Abstract
With the rapid aging of China’s population, the number of empty-nest elderly who have no children or whose children have left home is increasing, and empty nests are gradually becoming a family life pattern for the elderly population. This change has implications for their mental health. The research data were sourced from the 2020 China health and retirement longitudinal study. The center for epidemiologic studies depression scale was used to assess the prevalence of depression among this population. Logistic regression was employed to analyze the influencing factors of depressive symptoms. The overall prevalence of depression symptoms among empty-nest elderly is 40.2%. Multivariate logistic regression results show that higher education, having a spouse, living in an urban area, self-rated good health, frequent contact with children, high life satisfaction, and having a pension are protective factors against depressive symptoms among empty-nest elderly. Conversely, being female, having difficulties with activities of daily living, chronic diseases, physical pain, short sleep duration, frequent drinking, and living in impoverished households are risk factors in this population. It is crucial to prioritize the prevention and treatment of depression in empty-nest elderly, particularly among groups such as female elderly, those in rural areas, and those with poorer economic conditions.
Similar content being viewed by others
Introduction
Among the various social issues arising from the aging population trend, the mental health of the elderly is likely the most prominent. This concern is particularly pressing in China, given the country’s rapid aging process. By the end of 2023, the population aged 60 and above in China had reached 297 million, accounting for 21.1% of the total population1. Meanwhile, due to China’s former one-child policy2 and the rapid urbanization process3, there have been significant changes in family structures, with empty-nest living becoming a predominant family lifestyle for the elderly. In the past, due to traditional filial piety norms, elderly people in many East Asian countries, including China, often lived with their children4. However, recent years have seen a growing trend where more young people are choosing to move out, no longer living with their parents, and instead opting for independent living5,6. This move away from family life can be driven by various factors, including the pursuit of employment or education, marriage, or simply the desire to gain independence from parents as a symbol of adulthood7.
Empty-nest elderly refers to older adults who live alone or with a spouse, without children or whose children have already left home8,9. According to data from the China National Committee on Aging, the number of empty-nest elderly in China reached 118 million in 2020, and it is expected that by 2030, the proportion of empty-nest families will reach 90%, with over 200 million empty-nest elderly10. Empty-nest elderly have lower levels of general health, role physical, role emotional, and vitality11. As a vulnerable group12, they not only undergo a personal life cycle transition from middle age to old age but also a family cycle shift from a nuclear or extended family to an empty-nest family13. This dual transition makes them more susceptible to various adverse conditions and age-related issues, particularly mental health problems such as depression symptoms14,15. Therefore, it is crucial to prioritize the mental health of this population.
Among the various mental health issues affecting the elderly, depression symptoms are a common psychiatric disorder. An increasing number of studies report a high prevalence of depression symptoms in the elderly population16,17,18, making it a significant public health issue19. Depression symptoms severely impact the mental health and quality of life of the elderly, imposing a substantial burden on families and society20,21, and also elevating the risk of suicide among the elderly22,23. Additionally, depression symptoms are often associated with an increased risk of other diseases and higher mortality rates in the elderly24,25.
Despite the availability of effective treatments for mental disorders, over 75% of individuals in low-income and middle-income countries do not receive treatment26. In particular, Asia ranks second among continents in terms of depression prevalence, with many patients potentially not receiving adequate treatment27. In China, there is a shortage of mental health professionals and an uneven distribution across regions28 resulting in limited access to mental health services29. For the mental health issues of empty-nest elderly in China, it is crucial to implement early identification and intervention to ensure they are addressed timely and in effective manner.
Research on depressive symptoms among empty-nest elderly in China has largely been confined to specific regions or to either urban or rural settings. Reported prevalence varies substantially across locations, ranging from 47% in coastal cities of Zhejiang Province30, 64.2% in Shanxi Province31, to 79.7% in rural Yongzhou, Hunan Province32. In Xi’an City, Shaanxi Province, depressive symptoms were reported in 28.4% of urban and 36.2% of rural empty-nest elderly33. Given China’s vast geographic diversity and regional disparities in socio-economic development and policy contexts, these findings are not readily generalizable to the national level. Therefore, the present study draws on a nationally representative sample to examine depressive symptoms among this population.
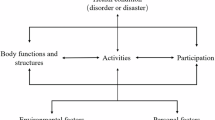
To develop effective interventions for depression symptoms among empty-nest elderly, it is essential to understand their influencing factors. Existing research has primarily focused on sociodemographic and health-related factors, including gender, age, and education level34; marital status, chronic diseases, economic status, relationships with children, and social support35; as well as sleep duration, activities of daily living, self-rated health, and place of residence36. Other factors such as social security37, life satisfaction38, and physical pain39 have also been linked to depressive symptoms. Importantly, depression cannot be explained by individual factors alone, as welfare systems, cultural contexts, and socioeconomic conditions also play a significant role40. Accordingly, our study incorporates a comprehensive set of variables to assess the risk of depression symptoms in this unique population.
The main contributions of this study are: (1) assessing the prevalence of depression symptoms among empty-nest elderly; (2) examining the within-group correlates of depression; (3) further enriching the understanding of mental health issues in this specific population, and providing insights to inform effective intervention and prevention strategies, ultimately promoting their mental health and supporting healthy aging.
Data and methods
Data source
The data used in this study comes from the fifth wave (2020) of CHARLS, which was released by the National School of Development at Peking University in 2023. CHARLS was designed with reference to a series of international aging studies, including the Health and Retirement Study, the English Longitudinal Study of Ageing, and the Survey of Health, Ageing and Retirement in Europe, employing a multi-stage stratified Probability Proportional to Size (PPS) sampling method.
PPS sampling is a method in which the probability of selecting a sampling unit is proportional to its size, such as population or household count. The CHARLS baseline survey used stratification by region, urban/rural status, and per capita GDP. In the first stage, 150 counties and districts across eight regions were randomly selected with probability proportional to population size. In the second stage, three villages or communities per selected county/district were similarly chosen. The resulting sample covered 28 provinces, 150 counties/districts, and 450 villages/communities, ensuring national and regional representativeness. The CHARLS official dataset used in this study has already been processed to account for sampling weights and the complex survey design. Therefore, no additional survey weights, strata, or clustering were applied in our analyses.
The CHARLS questionnaire collects detailed information on family, health, work, retirement, and pensions among China’s middle-aged and elderly population41, providing a reliable micro-level data source for this study. The survey was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015), and all participants provided written informed consent before completing the interviews.
Based on the research requirements, we selected empty-nest elderly aged 60 and above as the study subjects. After variable screening and data cleaning, a total of 4,007 empty-nest elderly were included in the final data sample, with 2,062 males and 1,945 females. The sample selection process of this study is shown below (Fig. 1).
Variable description
The dependent variable is measured by the presence of depression symptoms. The depression symptom scale used in this study is the simplified version of the Center for Epidemiological Studies Depression Scale42. This scale has been validated for use with older respondents in China using CHARLS data43 and demonstrates high reliability and validity. According to the guidelines for the Chinese version of CES-D10, the scale is rated on a 4-point scale with options “<1 day,” “1–2 days,” “3–4 days,” and “5–7 days,” which are coded as 0, 1, 2, and 3, respectively. Items “I feel hopeful about the future” and “I feel cheerful” are scored in reverse. The total score ranges from 0 to 30, with higher scores indicating more severe depression symptoms. Based on existing research standards for depression assessment44,45, a CES-D10 score of ≥ 10 is defined as having depression symptoms. In our study, the Cronbach’s alpha for the depression scale is 0.7940.
Based on previous studies46,47,48, this study included individual, health-related, child-related, and other related variables. Individual characteristics comprised gender, age, education level, marital status, and place of residence. Health-related variables included self-rated health status, activities of daily living (ADL), chronic diseases, physical pain, sleep duration, drinking, and smoking. Child-related variables included frequency of contact with children and satisfaction with children. Other variables included life satisfaction, social activities, exercise, household economic status, medical insurance, and pension insurance. The definitions of the variables are presented in Table 1.
In CHARLS, ADL were assessed using the Katz Index of Activities of Daily Living49, which evaluates six basic self-care activities: dressing, bathing, eating, getting in and out of bed, using the toilet, and continence. Participants reporting difficulty in at least one activity were classified as having ADL impairment. For chronic disease, participants were classified as having chronic disease if they reported at least one of the three specified conditions. Ordinal variables such as life satisfaction and satisfaction with children were measured using five-point Likert scales in CHARLS. Based on previous studies, these variables were recoded into three ordinal categories: dissatisfied, fair, and satisfied, with dissatisfied serving as the reference group.
Statistical analysis
All statistical analyses were conducted using Stata 18.0. Logistic regression models were employed to explore factors associated with depressive symptoms among empty-nest elderly, with all covariates entered simultaneously into the models. The results are presented as odds ratios (ORs) with 95% confidence intervals (CIs), indicating the risk of experiencing depressive symptoms associated with various characteristics. A p-value of less than 0.05 was considered statistically significant.
In addition, model goodness of fit was assessed using the Pearson chi-square goodness-of-fit test following logistic regression. The results showed no evidence of lack of fit (χ² = 3714.00, df = 3750, p = 0.6588), indicating that the model appeared to fit the data appropriately.
Research results
Basic characteristics of depression symptoms in empty-nest elderly
Table 2 presents the basic characteristics of empty-nest elderly stratified by the presence or absence of depression symptoms. The overall prevalence of depression symptoms among empty-nest elderly is 40.15%, 16.62% of which are males and 23.53% are females. The remaining characteristics and corresponding chi-square test results are shown in the table.
Influencing factors of depression symptoms in empty-nest elderly
The results of the multivariable logistic regression for depression symptoms among the entire empty-nest elderly sample are shown in Table 3. Compared with male empty-nest elderly, females had a higher likelihood of depressive symptoms (OR = 1.366, 95% CI: 1.090–1.713). Higher educational attainment was associated with a lower likelihood of depressive symptoms; compared with illiterate participants, those with junior high school education or below (OR = 0.793, 95% CI: 0.655–0.960) and those with high school education or above (OR = 0.437, 95% CI: 0.319–0.599) had significantly lower risks. Being married (OR = 0.782, 95% CI: 0.633–0.965) and living in urban areas (OR = 0.644, 95% CI: 0.541–0.767) were also associated with reduced likelihood.
Compared with those reporting poor health, participants with fair (OR = 0.553, 95% CI: 0.461–0.664) or good self-rated health (OR = 0.304, 95% CI: 0.236–0.390) had substantially lower likelihood. More frequent contact with children (OR = 0.734, 95% CI: 0.617–0.874), higher life satisfaction (OR = 0.144, 95% CI: 0.102–0.203), and satisfaction with children (OR = 0.385, 95% CI: 0.253–0.586) were also associated with lower likelihood of depressive symptoms.
In contrast, several health-related and socioeconomic factors increased the likelihood of depressive symptoms, including difficulties in ADL (OR = 1.689, 95% CI: 1.411–2.021), chronic diseases (OR = 2.361, 95% CI: 1.616–3.449), physical pain (OR = 1.830, 95% CI: 1.541–2.174), short sleep duration (OR = 1.542, 95% CI: 1.315–1.808), drinking (OR = 1.275, 95% CI: 1.070–1.520) and living in impoverished households (OR = 1.356, 95% CI: 1.092–1.683). Having a pension was associated with a lower likelihood of depressive symptoms (OR = 0.829, 95% CI: 0.706–0.975), whereas age, social activities, smoking, exercise, and medical insurance showed no significant associations.
Discussion
Prevalence of depression symptoms in empty-nest elderly
The study found that the prevalence of depression symptoms among empty-nest elderly in China is 40.15%. This finding differs from the prevalence of depression symptoms reported in recent literature. These results should be interpreted with caution, as they may be influenced by differences in the time period of the data and regional variations in the study populations.
Specifically, the CHARLS data used in this study were collected during the COVID-19 pandemic, a period that may have posed additional psychological challenges for empty-nest elderly. Previous research suggests that the pandemic had a negative impact on the mental health of the elderly in China and may have increased the risk of depressive symptoms50. Moreover, eastern regions of China generally have higher levels of economic development51, and elderly individuals in these areas tend to have better economic conditions, which are associated with better health status and higher life satisfaction, potentially lowering the likelihood of depressive symptoms30. In contrast, this study includes urban and rural samples from central and western regions with greater socioeconomic heterogeneity, which may help explain the observed prevalence of depressive symptoms.
There may be differences in the causal mechanisms of depression between the empty-nest elderly population and the general elderly population. Within the empty-nest elderly population, the lack of companionship from children results in reduced daily interaction and emotional support, leading to higher levels of loneliness, which has been identified as a prominent risk factor for the development of depression52,53. In contrast, the general elderly population usually benefits from the companionship of their children and receives more stable emotional support, which can buffer psychological stress and thereby attenuate the causal role of loneliness in depression. In addition, individuals in the empty-nest elderly population often need to manage daily activities independently. When functional limitations or declining health occur, the absence of timely assistance from family members may increase feelings of helplessness and psychological stress, consequently elevating the risk of depression. By comparison, the general elderly population is more likely to receive care and support from children or other family members. As a result, the psychological impact of declining functional ability is relatively smaller, leading to a lower risk of depression.
Analysis of influencing factors
Female empty-nest elderly have a higher likelihood of experiencing depressive symptoms compared to their male counterparts, which aligns with previous research findings31,46. This gender disparity in depression symptoms may be linked to distinct physiological and psychological factors in women54. Higher education, having a spouse, and living in urban areas are each independently associated with a lower prevalence of depressive symptoms among empty-nest elderly. More educated elderly generally have better socioeconomic status, greater knowledge, and more active cognitive skills, which help them cope with life’s challenges and manage stress effectively55. According to marital resource theory, spouses provide economic support, emotional companionship, and daily assistance, and their loss, known as the “widowhood effect,” significantly increases depression risk, especially in China, where elderly largely rely on pensions and support from children56,57. In empty-nest families, a spouse plays a critical role in providing daily care and emotional support. Urban residents benefit from higher economic development, better infrastructure, more social support, and easier access to healthcare, whereas rural elderly face underdeveloped infrastructure, limited healthcare access, lower social support, and poorer quality of life, all of which elevate depression risk58,59.
A higher frequency of contact with children, greater satisfaction with children, and higher life satisfaction are all associated with a lower likelihood of depressive symptoms among empty-nest elderly. Studies have shown that infrequent contact with children is linked to a gradual deterioration in mental health, largely due to increased feelings of loneliness following the transition to an empty-nest status15. Loneliness may adversely affect mental health to some extent, whereas increasing contact with children can strengthen family support, reduce loneliness, and thereby lower the likelihood of depressive symptoms60. In Confucian culture-oriented countries such as China and Korea, family factors play a central role in both life satisfaction and depression among the elderly61. The family, as the most important social bond, provides a sense of belonging, security, and support. Strong family support and financial or emotional assistance from children can enhance satisfaction and life satisfaction among empty-nest elderly, thereby protecting against depressive symptoms62,63. Conversely, difficulty in establishing close and reciprocal parent–child relationships, lack of family support, or dysfunctional family dynamics can intensify loneliness, reduce life satisfaction, and increase vulnerability to depressive symptoms.
Among health-related factors, self-rated good health is associated with a lower likelihood of depressive symptoms among empty-nest elderly, whereas difficulties in ADL, chronic diseases, physical pain, short sleep duration, and drinking are each independently associated with a higher likelihood of depressive symptoms. Self-reported health status is a key indicator of overall health64 and reflects the psychological well-being of older adults to some extent. Those who report better health tend to have greater confidence in their health and are more likely to adopt a positive attitude towards life65, which can serve as a protective factor against depression. However, this relationship may be bidirectional, as depression can lead individuals to perceive their health more negatively, further impacting their mental well-being.
Limitations in ADL are significantly associated with depressive symptoms and show a cumulative effect66. Basic self-care abilities help maintain mental health and support social integration, while partial or severe dependency may cause social and psychological strain, worsening mood and increasing vulnerability to depression67,68. Inability to participate in social activities or fulfill social roles can further heighten feelings of social disconnection, adversely affecting mental health69. Among empty-nest elderly, these relationships are likely bidirectional, as depression may impair motivation, energy, and cognitive functioning, which in turn affects ADL performance and further contributes to declines, particularly given their limited social support.
Research shows that those with one chronic condition have a 13% higher likelihood of experiencing depressive symptoms, while those with two or more chronic conditions have a 20% higher likelihood70. The duration of chronic disease also increases the risk of depressive symptoms71. Chronic diseases often limit social interactions, preventing individuals from alleviating loneliness and fear of illness, which can eventually lead to depressive feelings72. Conversely, depression may negatively affect disease management and immune function, exacerbating chronic disease symptoms and creating a mutually reinforcing negative cycle.
There is a bidirectional longitudinal association between pain and depressive symptoms, with individuals experiencing physical pain at an increased risk of developing depression, while depression may also amplify pain perception or increase pain sensitivity73. From a pathological perspective, this may be related to the key role of neuroinflammation in the development of both depression and chronic pain74. Additionally, physical pain can substantially impair daily living activities in older adults, heightening negative emotions and potentially triggering further depressive symptoms75. For empty-nest elderly, the impact of physical pain is further intensified by the lack of daily caregiving from children, worsening the situation.
Sleep duration has been widely recognized as an important determinant of mental health in later life. The mechanisms underpinning this association can be explained from biological perspectives, including disruption of circadian rhythms, hormonal dysregulation, and elevated levels of chronic inflammation76. In addition, shorter sleep duration may further exacerbate depressive symptoms77. However, it should also be noted that the relationship is likely bidirectional, as depression can contribute to various sleep problems, such as difficulty initiating or maintaining sleep, early-morning awakening, and poor sleep quality. Therefore, maintaining adequate sleep is crucial for preventing and alleviating depressive symptoms among empty-nest elderly.
Research has identified a U-shaped association between alcohol consumption and depressive symptoms, suggesting that both abstinence and excessive drinking are linked to higher depression risk, whereas moderate drinking may have a protective effect in older adults78,79. In this study, most empty-nest elderly report frequent drinking. Prolonged excessive drinking and alcohol dependence can elevate blood alcohol levels and increase the likelihood of adverse health outcomes. Given their reduced tolerance and heightened sensitivity to alcohol, older adults are particularly vulnerable to its negative health effects80, which may in turn heighten the risk of depressive symptoms. Conversely, depression may also lead empty-nest elderly to rely on alcohol as a coping mechanism, as a way to manage stress or negative emotions, thereby reinforcing harmful drinking behaviors.
Among other influencing factors, economic conditions significantly affect the risk of depressive symptoms in empty-nest elderly. Those from impoverished households, which in China are defined as families with income below the national poverty line, poor living conditions, and registration to receive government aid, face a higher risk of depression46. In addition, elderly individuals living in areas of greater income inequality are more likely to experience depressive symptoms compared to those in lower inequality contexts81. Limited financial resources also reduce access to health care, as older adults from low-income families exhibit lower rates of inpatient service utilization82, further increasing vulnerability to depression. Conversely, having a pension serves as a protective factor against depressive symptoms83, likely due to the financial stability it provides, enabling access to health care and other resources. From a public health perspective, pensions help cover relatively affordable medical services, addressing health care needs84. Economically, they provide a stable and reliable income to meet basic living needs, thereby reducing depression risk85. Therefore, policies and interventions should prioritize improving the economic conditions of empty-nest elderly to support their physical and mental health.
Conclusion
With the increasing aging population in China, the number of empty-nest elderly experiencing depression symptoms is anticipated to rise, which will put pressure on families and society. It is necessary to prioritize empty-nest elderly in the prevention and treatment of depression symptoms. Considering the factors influencing depression symptoms in empty-nest elderly, we recommend enhancing family support, improving healthcare services, expanding pension coverage, and giving special attention to female, rural, and economically disadvantaged members of this group to lower their risk of developing depressive symptoms.
Limitations and Future Research: First, this study uses cross-sectional data, which only allows for exploring the associations between depressive symptoms in empty-nest elderly and their influencing factors, without establishing causation. Second, the measurement of chronic diseases was limited to three self-reported conditions, which may underestimate the true prevalence and introduce measurement bias. Additionally, with the advancement of information technology and the application of smart healthcare technologies, our study did not examine the potential impact of participation in online social platforms or access to emotional counseling on depressive symptoms among empty-nest elderly. Finally, future research should consider including a control group to enable comparative analyses and examine the differences in depressive symptoms between empty-nest elderly and the general elderly.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
National Bureau of Statistics. Statistical Bulletin of National Economic and Social Development of the People’s Republic of China 2023. https://www.stats.gov.cn/xxgk/jd/sjjd2020/202401/t20240118_1946711.html (2024).
Hesketh, T., Lu, L. & Xing, Z. W. The effect of china’s one-child family policy after 25 years. N Engl. J. Med. 353, 1171–1176. https://doi.org/10.1056/NEJMhpr051833 (2005).
Liu, L. J. & Guo, Q. Loneliness and health-related quality of life for the empty nest elderly in the rural area of a mountainous County in China. Qual. Life Res. 16, 1275–1280. https://doi.org/10.1007/s11136-007-9250-0 (2007).
You, K. S. et al. Spirituality, depression, living alone, and perceived health among Korean older adults in the community. Arch. Psychiatr Nurs. 23, 309–322. https://doi.org/10.1016/j.apnu.2008.07.003 (2009).
Chen, T. Living arrangement preferences and realities for elderly chinese: implications for subjective wellbeing. Ageing Soc. 39, 1557–1581. https://doi.org/10.1017/S0144686X18000041 (2019).
Zhang, H. H. et al. Prevalence of depression among empty-nest elderly in china: A meta-analysis of observational studies. Front. Psychiatry. 11, 608. https://doi.org/10.3389/fpsyt.2020.00608 (2020).
Beaupre, P., Turcotte, P. & Milan, A. When is junior moving out? Transitions from the parental home to independence. Can. Soc. Trends. 82, 9–15 (2006). https://www150.statcan.gc.ca/n1/pub/11-008-x/2006002/9274-eng.htm
Wang, Z., Shu, D., Dong, B., Luo, L. & Hao, Q. Anxiety disorders and its risk factors among the Sichuan empty-nest older adults: a cross-sectional study. Arch. Gerontol. Geriatr. 56, 298–302. https://doi.org/10.1016/j.archger.2012.08.016 (2013).
Gao, Y. L., Wei, Y. B., Shen, Y. D., Tang, Y. Y. & Yang, J. R. China’s empty nest elderly need better care. J. Am. Geriatr. Soc. 62, 1821–1822. https://doi.org/10.1111/jgs.12997 (2014).
Mu, G. & Yin, S. Respectful care for the elderly: the dilemmas and solutions in the construction of elderly-friendly care institutions. Jiang Huai Trib. 6, 94–102. https://doi.org/10.16064/j.cnki.cn34-1003/g0.2023.06.019 (2023).
He, W. et al. Quality of life of empty-nest elderly in china: a systematic review and meta-analysis. Psychol. Health Med. 25, 131–147. https://doi.org/10.1080/13548506.2019.1695863 (2020).
Zhou, C. et al. Non-use of health care service among empty-nest elderly in Shandong, china: a cross-sectional study. BMC Health Serv. Res. 15, 294. https://doi.org/10.1186/s12913-015-0974-1 (2015).
Liu, M. & Wang, A. H. Community care of senile people with empty nest syndrome. Chin. Nurs. Res. 20, 2811–2812 (2006).
Wang, J. & Zhao, X. Empty nest syndrome in China. Int. J. Soc. Psychiatry. 58, 110. https://doi.org/10.1177/0020764011418406 (2012).
Gao, M. et al. Does an empty nest affect elders’ health? Empirical evidence from China. Int. J. Environ. Res. Public. Health. 14, 463. https://doi.org/10.3390/ijerph14050463 (2017).
Almeida, O. P. Prevention of depression in older age. Maturitas 79, 136–141. https://doi.org/10.1016/j.maturitas.2014.03.005 (2014).
Szymkowicz, S. M., Gerlach, A. R., Homiack, D. & Taylor, W. D. Biological factors influencing depression in later life: role of aging processes and treatment implications. Transl Psychiatry. 13, 160. https://doi.org/10.1038/s41398-023-02464-9 (2023).
Kim, K. M., Kim, J. H., Rhee, H. S. & Youn, B. Y. Development of a prediction model for the depression level of the elderly in low-income households: using decision trees, logistic regression, neural networks, and random forest. Sci. Rep. 13, 11473. https://doi.org/10.1038/s41598-023-38742-1 (2023).
Thirthahalli, C. et al. Proportion and factors associated with depressive symptoms among elderly in an urban slum in Bangalore. J. Urban Health. 91, 1065–1075. https://doi.org/10.1007/s11524-014-9903-6 (2014).
König, H., König, H. H. & Konnopka, A. The excess costs of depression: a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 29. https://doi.org/10.1017/S2045796019000180 (2019).
Liu, J. et al. China health and retirement longitudinal study: depressive symptoms and related factors among middle-aged and elderly disabled people. Chin. J. Behav. Med. Brain Sci. 30, 273–278. https://doi.org/10.3760/cma.j.cn371468-20201009-01774 (2021).
Yi, S. W. Depressive symptoms on the geriatric depression scale and suicide deaths in older middle-aged men: A prospective cohort study. J. Prev. Med. Public. Health. 49, 176–182. https://doi.org/10.3961/jpmph.16.012 (2016).
Marwaha, S. et al. Novel and emerging treatments for major depression. Lancet 401, 141–153. https://doi.org/10.1016/S0140-6736(22)02080-3 (2023).
Alexopoulos, G. S. Depression in the elderly. Lancet 365, 1961–1970. https://doi.org/10.1016/S0140-6736(05)66665-2 (2005).
Xue, Y., Liu, G. & Geng, Q. Associations of cardiovascular disease and depression with memory-related disease: A Chinese National prospective cohort study. J. Affect. Disord. 266, 187–193. https://doi.org/10.1016/j.jad.2020.01.054 (2020).
Evans-Lacko, S. et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO world mental health (WMH) surveys. Psychol. Med. 48, 1560–1571. https://doi.org/10.1017/S0033291717003336 (2018).
Lim, G. Y. et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 8, 2861. https://doi.org/10.1038/s41598-018-21243-x (2018).
Liu, J. et al. Mental health system in china: history, recent service reform and future challenges. World Psychiatry. 10, 210–216. https://doi.org/10.1002/j.2051-5545.2011.tb00059.x (2011).
Zhang, M. Major depressive disorder treatment guidelines in China. J. Clin. Psychiatr.. 71. https://doi.org/10.4088/JCP.9058se1c.06gry (2010).
Yao, Y. et al. Risk factors for depression in empty nesters: a cross-sectional study in a coastal City of Zhejiang Province and China. Int. J. Environ. Res. Public. Health 16, 4106. https://doi.org/10.3390/ijerph16214106 (2019).
Zhang, C. et al. Prevalence and related influencing factors of depressive symptoms among empty-nest elderly in Shanxi, China. J. Affect. Disord. 245, 750–756. https://doi.org/10.1016/j.jad.2018.11.045 (2019).
Xie, L. Q., Zhang, J. P., Peng, F. & Jiao, N. N. Prevalence and related influencing factors of depressive symptoms for empty-nest elderly living in the rural area of YongZhou, China. Arch. Gerontol. Geriatr. 50, 24–29. https://doi.org/10.1016/j.archger.2009.01.003 (2010).
Zhang, H. & Zhang, Y. Comparative analysis on healthy living related factors of empty-nest elderly in rural and urban areas. China J. Health Psychol. 26, 1725–1729. https://doi.org/10.13342/j.cnki.cjhp.2018.11.033 (2018).
Zhai, Y. et al. Association of empty nest with depressive symptom in a Chinese elderly population: A cross-sectional study. J. Affect. Disord. 187, 218–223. https://doi.org/10.1016/j.jad.2015.08.031 (2015).
Song, C., Yao, L., Chen, H., Song, Y. & Liu, L. Prevalence and factors influencing depression among empty nesters in china: A meta-analysis. BMC Geriatr. 23, 333. https://doi.org/10.1186/s12877-023-04064-0 (2023).
Fu, C., Cao, L. & Yang, F. Prevalence and determinants of depressive symptoms among community-dwelling older adults in China based on differences in living arrangements: a cross-sectional study. BMC Geriatr. 23, 640. https://doi.org/10.1186/s12877-023-04339-6 (2023).
Shao, M., Chen, J. & Ma, C. Research on the relationship between Chinese elderly health Status, social Security, and depression. Int. J. Environ. Res. Public. Health. 19, 7496. https://doi.org/10.3390/ijerph19127496 (2022).
Lee, S. W., Choi, J. S. & Lee, M. Life satisfaction and depression in the oldest old: A longitudinal study. Int. J. Aging Hum. Dev. 91, 37–59. https://doi.org/10.1177/0091415019843448 (2020).
Ye, X. & Wang, X. Associations of Multimorbidity with body pain, sleep duration, and depression among middle-aged and older adults in China. Health Qual. Life Outcomes. 22, 23. https://doi.org/10.1186/s12955-024-02238-x (2024).
Conde-Sala, J. L., Garre-Olmo, J., Calvó-Perxas, L., Turró-Garriga, O. & Vilalta-Franch, J. Course of depressive symptoms and associated factors in people aged 65 + in europe: a two-year follow-up. J. Affect. Disord. 245, 440–450. https://doi.org/10.1016/j.jad.2018.10.358 (2019).
Zhao, Y., Hu, Y., Smith, J. P., Strauss, J. & Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int. J. Epidemiol. 43, 61–68. https://doi.org/10.1093/ije/dys203 (2014).
Andresen, E. M., Malmgren, J. A., Carter, W. B. & Patrick, D. L. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for epidemiologic studies depression Scale). Am. J. Prev. Med. 10, 77–84. https://doi.org/10.1016/S0749-3797(18)30622-6 (1994).
Chen, H. & Mui, A. C. Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. Int. Psychogeriatr. 26, 49–57. https://doi.org/10.1017/S1041610213001701 (2014).
Qian, J., Li, N. & Ren, X. Obesity and depressive symptoms among Chinese people aged 45 and over. Sci. Rep. 7, 45637. https://doi.org/10.1038/srep45637 (2017).
Chang, H., Zhou, J. & Wang, Z. Multidimensional factors affecting successful aging among empty-nesters in China based on social-ecological system theory. Int. J. Environ. Res. Public. Health 19 (19), 11885. https://doi.org/10.3390/ijerph191911885 (2022).
Wang, L., Liu, W., Liang, Y. & Wei, Y. Mental health and depressive feeling of empty-nest elderly people in China. Am. J. Health Behav. 43 (6), 1171–1185. https://doi.org/10.5993/AJHB.43.6.14 (2019).
Su, D. et al. Effect of social participation on the physical functioning and depression of empty-nest elderly in china: evidence from the China health and retirement longitudinal survey (CHARLS). Int. J. Environ. Res. Public. Health. 17 (24), 9438. https://doi.org/10.3390/ijerph17249438 (2020).
Xu, M. & Yang, W. Depressive symptoms among older empty nesters in china: the moderating effects of social contact and contact with one’s children. Aging Ment Health. 27 (1), 54–69. https://doi.org/10.1080/13607863.2021.2019190 (2023).
Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A. & Jaffe, M. W. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA 185 (12), 914–919. https://doi.org/10.1001/JAMA.1963.03060120024016 (1963).
Liang, W. et al. Precautionary behavior and depression in older adults during the COVID-19 pandemic: an online cross-sectional study in Hubei, China. Int. J. Environ. Res. Public. Health. 18 (4), 1853. https://doi.org/10.3390/ijerph18041853 (2021).
Tan, J. et al. Research on the current situation and influencing factors of depression among empty nesters in Hangzhou. Chin. J. Health Stat. 38 (04), 593–596. https://doi.org/10.3969/j.issn.1002-3674.2021.04.030 (2021).
Shankar, A. & Kidd, T. Loneliness in older Indian dyads. Int. J. Environ. Res. Public. Health. 19 (9), 5302. https://doi.org/10.3390/ijerph19095302 (2022).
Son, H., Cho, H. J., Cho, S., Ryu, J. & Kim, S. The moderating effect of social support between loneliness and depression: differences between the young-old and the old-old. Int. J. Environ. Res. Public. Health. 19 (4), 2322. https://doi.org/10.3390/ijerph19042322 (2022).
Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry. 4 (2), 146–158. https://doi.org/10.1016/S2215-0366(16)30263-2 (2017).
Xie, Y. et al. Factors associated with depressive symptoms among the elderly in china: structural equation model. Int. Psychogeriatr. 33 (2), 157–167. https://doi.org/10.1017/S1041610220001398 (2021).
Schmitz, A. Gendered experiences of widowhood and depression across europe: the role of loneliness and financial resources from a longitudinal perspective. J. Affect. Disord. 280 (Pt A), 114–120. https://doi.org/10.1016/j.jad.2020.11.091 (2021).
Pang, J., Liang, D. & Wu, Y. The effect of widowhood on depression of caregivers. BMC Health Serv. Res. 23 (1), 722. https://doi.org/10.1186/s12913-023-09746-4 (2023).
Liu, L. J., Sun, X., Zhang, C. L. & Guo, Q. Health-care utilization among empty-nesters in the rural area of a mountainous County in China. Public. Health Rep. 122 (3), 407–413. https://doi.org/10.1177/003335490712200315 (2007).
Brenes, G. A. et al. Barriers to mental health treatment in rural older adults. Am. J. Geriatr. Psychiatry. 23 (11), 1172–1178. https://doi.org/10.1016/j.jagp.2015.06.002 (2015).
Sheng, B. et al. Elucidating the influence of Familial interactions on geriatric depression: a comprehensive nationwide multi-center investigation leveraging machine learning. Acta Psychol. 246, 104274. https://doi.org/10.1016/j.actpsy.2024.104274 (2024).
Chai, H. W. & Jun, H. J. Relationship between ties with adult children and life satisfaction among the middle-aged, the young-old, and the oldest-old Korean adults. Int. J. Aging Hum. Dev. 85 (4), 354–376. https://doi.org/10.1177/0091415016685834 (2017).
Gu, H. X. The empty nesters’ life quality, mentality, and social support. Chin. J. Health Psychol. 23 (08), 1218–1222. https://doi.org/10.13342/j.cnki.cjhp.2015.08.028 (2015).
Wu, Y. et al. Financial transfers from adult children and depressive symptoms among mid-aged and elderly residents in china: evidence from the China health and retirement longitudinal study. BMC Public. Health. 18 (1), 882. https://doi.org/10.1186/s12889-018-5794-x (2018).
Al-Hanawi, M. K. Self-reported health inequalities among older adults in Saudi Arabia. Healthcare 12 (1), 72. https://doi.org/10.3390/healthcare12010072 (2023).
Liu, L. et al. Analysis of the status quo of ADL, self-rated health, and depression among Chinese elderly. Med. Soc. 33 (6), 90–94. https://doi.org/10.13723/j.yxysh.2020.06.022 (2020).
Meltzer, H. et al. Physical ill health, disability, dependence and depression: results from the 2007 National survey of psychiatric morbidity among adults in England. Disabil. Health J. 5 (2), 102–110. https://doi.org/10.1016/j.dhjo.2012.02.001 (2012).
Lenze, E. J. et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am. J. Geriatr. Psychiatr. 9 (2), 113–135. https://doi.org/10.1176/appi.ajgp.9.2.113 (2001).
Carr, D., Cornman, J. C. & Freedman, V. A. Do family relationships buffer the impact of disability on older adults’ daily mood? An exploration of gender and marital status differences. J. Marriage Fam. 81 (3), 729–746. https://doi.org/10.1111/jomf.12557 (2019).
Santini, Z. I. et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 5 (1), e70. https://doi.org/10.1016/S2468-2667(19)30230-0 (2020).
Wang, Z., Yang, H., Sun, C. & Hong, S. Estimating causal effects of physical disability and number of comorbid chronic diseases on risk of depressive symptoms in an elderly Chinese population: a machine learning analysis of cross-sectional baseline data from the China longitudinal ageing social survey. BMJ Open 13 (7). https://doi.org/10.1136/bmjopen-2022-069298 (2023).
Tel, H. Anger and depression among the elderly people with hypertension. Neurol. Psychiatry Brain Res. 19 (3), 109–113. https://doi.org/10.1016/j.npbr.2013.05.003 (2013).
Xue, Y. Q. et al. Depression status and influencing factors of empty-nest elderly based on structural equation modeling. Chin. J. Dis. Control Prev. 23 (10), 1181–1185. https://doi.org/10.16462/j.cnki.zhjbkz.2019.10.005 (2019).
Qiu, Y., Ma, Y. & Huang, X. Bidirectional relationship between body pain and depressive symptoms: a pooled analysis of two National aging cohort studies. Front. Psychiatry. 13, 881779. https://doi.org/10.3389/fpsyt.2022.881779 (2022).
Zis, P. et al. Depression and chronic pain in the elderly: links and management challenges. Clin. Interv Aging. 12, 709–720. https://doi.org/10.2147/CIA.S113576 (2017).
Singh, A. et al. Impact of pain on activities of daily living in older adults: a cross-sectional analysis of Korean longitudinal study of aging (KLoSA). Geriatrics 9 (3), 65. https://doi.org/10.3390/geriatrics9030065 (2024).
Li, Y. et al. Longitudinal association of sleep duration with depressive symptoms among middle-aged and older Chinese. Sci. Rep. 7 (1), 11794. https://doi.org/10.1038/s41598-017-12182-0 (2017).
Tian, X. et al. Temporary relationship between sleep duration and depression and its impact on future risk of cardiovascular disease. J. Affect. Disord. 350, 559–564. https://doi.org/10.1016/j.jad.2024.01.185 (2024).
Yun, M. & Kim, E. Gender difference in the association between alcohol consumption and depressive symptoms among the elderly in rural areas. J. Ethn. Subst. Abuse. 21 (1), 36–54. https://doi.org/10.1080/15332640.2019.1704336 (2022).
Bots, S. et al. Lifestyle- and diet-related factors in late-life depression—a 5-year follow-up of elderly European men: the FINE study. Int. J. Geriatr. Psychiatry. 23 (5), 478–484. https://doi.org/10.1002/gps.1919 (2008).
Tevik, K., Bergh, S., Selbæk, G., Johannessen, A. & Helvik, A. S. A systematic review of self-report measures used in epidemiological studies to assess alcohol consumption among older adults. PLoS One 16 (12). https://doi.org/10.1371/journal.pone.0261292 (2021).
Patel, V. et al. Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry. 17 (1), 76–89. https://doi.org/10.1002/wps.20492 (2018).
Luo, J., Zhang, X., Jin, C. & Wang, D. Inequality of access to health care among the urban elderly in Northwestern China. Health Policy. 93 (2–3), 111–117. https://doi.org/10.1016/j.healthpol.2009.06.003 (2009).
He, H., Xu, L. & Fields, N. Pensions and depressive symptoms of older adults in china: the mediating role of intergenerational support. Int. J. Environ. Res. Public. Health. 18 (7), 3725. https://doi.org/10.3390/ijerph18073725 (2021).
Lloyd-Sherlock, P. & Agrawal, S. Pensions and the health of older people in South africa: is there an effect? J. Dev. Stud. 50 (11), 1570–1586. https://doi.org/10.1080/00220388.2014.936399 (2014).
Chen, X., Wang, T. & Busch, S. H. Does money relieve depression? Evidence from social pension expansions in China. Soc. Sci. Med. 220, 411–420. https://doi.org/10.1016/j.socscimed.2018.12.004 (2019).
Acknowledgements
The authors sincerely thank the China Health and Retirement Longitudinal Study team for providing the research dataset.
Funding
This study was funded by the Postgraduate Scientific Research Innovation Project of Hunan Province (Grant No. CX20240632).
Author information
Authors and Affiliations
Contributions
D.L. contributed to writing the original draft, formal analysis, validation, data curation and funding acquisition. Z.L. was responsible for conceptualization, writing review and editing, methodology. All authors have read, approved, and consented to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
No animal studies are presented in this manuscript. No potentially identifiable human images or data are presented in this study. Ethical approval for all the waves of the China Health and Retirement Longitudinal Study (CHARLS) was granted by the Institutional Review Board at Peking University. The IRB approval number is IRB00001052-11015.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, D., Long, Z. Prevalence and related influencing factors of depression symptoms among empty-nest elderly in China. Sci Rep 16, 4494 (2026). https://doi.org/10.1038/s41598-025-34565-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-34565-4