Abstract
To investigates the current status of mindfulness in patients with Wilson’s disease (WD) and to explore the effects of psychological resilience, perceived social support, and acceptance of illness on their mindfulness. By using the convenient sampling method, 136 patients with WD were selected from May 2019 to January 2023 in 12 tertiary hospitals in Chengdu. General information questionnaire, five facet mindfulness scale, resilience scale, acceptance of illness and perceived social support scale were used to conduct the investigation. Structural equation model was used to analyze the data. The score of mindfulness of patients with WD was (128.63 ± 22.62), and there were statistically significant differences in different courses of disease, clinical classification, and hospitalization times (P < 0.05). Perceived social support (β = 0.18, P < 0.01) and psychological resilience (β = 0.36, P < 0.05) directly affected mindfulness, perceived social support (β = 0.21, P < 0.01), and acceptance of illness (β = 0.11, P < 0.05) indirectly affected mindfulness through psychological resilience. Patients with WD have moderate levels of mindfulness, psychological resilience, perceived social support and acceptance of illness directly or indirectly affect their mindfulness. Nursing staff can help patients improve their mental defense ability, actively seek more social support, dialectical view, and accept the disease to improve their level of mindfulness to promote physical and mental health.
Similar content being viewed by others
Introduction
Hepatolenticular degeneration (HLD), also known as Wilson’s disease (WD), is a rare genetic systemic disease caused by a decrease in a copper-transporting ATP enzyme encoded by the ATP7B gene due to mutation. This results in abnormal copper transport and accumulation in various organs, such as the liver and brain, leading to characteristic clinical manifestations such as acute or chronic liver disease symptoms, progressively worsening extra-pyramidal symptoms, psychiatric symptoms, and corneal pigmentation rings1. Once diagnosed, WD requires lifelong treatment. However, early-stage symptoms are nonspecific, and patients are often in the late stage of the disease when diagnosed. Moreover, the clinical manifestations are complex and diverse, and no effective cure exists2. Therefore, treatment mainly focuses on symptomatic relief to delay disease progression. As the prognosis of WD cannot be predicted, patients may develop negative emotions and poor compliance with medical recommendations, hindering disease recovery.
Wilson disease typically manifests during childhood and early adulthood. The most common age of presentation is between 10 and 20 years3,4. However, patients may present at an earlier age, below 5 years5,6 or at a later age, above 70 years7. In one study, 3.8% of 1223 patients with genetically confirmed WD became symptomatic at 40 years of age or later8. Therefore, although the majority of patients present early in life, WD could still be considered in the differential diagnosis for patients presenting in middle age. Several studies have indicated that patients with primarily hepatic presentations tend to be younger than those with neurological presentations, although both can occur at any age9.
WD is a rare disorder, with a prevalence that has been reported to vary depending on the study, with the most widely cited prevalence of 1 in 30,00010. More recent studies in China11 and France12 indicate a lower prevalence of 1 in 56,000 to 1 in 66,000, respectively. The frequency of individuals carrying pathogenic mutations is higher than anticipated. This finding has been corroborated in multiple populations in France13, the United Kingdom14 and China15. Furthermore, one study demonstrated a higher-than-expected prevalence of WD in the offspring of patients with WD16. Despite the absence of national epidemiological survey data in China, domestic scholars have conducted two consecutive surveys in three counties in Anhui Province, a total of 153,370 individuals. This has led to the identification of nine cases of WD patients, with an estimated prevalence rate of 0.587 per 10,00017. It is postulated that the actual prevalence in the Chinese population may be higher, given that some asymptomatic patients have no clinical manifestations and no abnormalities in biochemical indicators.
Mindfulness was initially introduced into psychology as an intervention method that involves conscious focus of an individual’s attention on various internal and external experiences occurring in the present moment through practices such as meditation18. Subsequently, with further research, mindfulness began to be recognized as a relatively stable trait commonly possessed by individuals19. Following Kabat-Zinn’s definition20, mindfulness is understood as an individual’s ability to consciously focus their attention on the present moment without passing judgment on subsequent unfolding experiences. Mindfulness is the awareness arising from conscious, non-judgmental attention to the present moment. Relevant interventions serving specific goals are non-religious and bring about physical and mental improvement21. Mindfulness can enhance individuals’ self-awareness of their current cognition, thoughts and emotions22. It can also reduce issues such as distraction and inattention23, and improve individuals’ self-control ability, thereby decreasing the likelihood of self-regulation failure24. Extensive research has focused on mindfulness in the context of various chronic illnesses. Mindfulness exercises can serve the purpose of cultivating mindfulness. A body of evidence from empirical studies indicates that mindfulness practices can positively impact individuals’ mental and physical well-being by reducing stress, anxiety, and depression, and enhancing coping mechanisms25. Additionally, mindfulness-based therapy has been shown to have a beneficial impact on both physical and psychological aspects of chronic diseases, promoting the disease recovery and improving the patients’ quality of life and well-being of patients. Mindfulness can assist patients in coping with illness-related pain, relieving psychological stress, and ultimately promoting the formation of self-compassion and self-acceptance26.
Previous studies have shown that psychological resilience, perceived social support, and disease acceptance are related to mindfulness. Psychological resilience is a positive quality that promotes the healthy development of an individual’s body and mind. It refers to an individual’s ability to adapt and rebound psychologically in the face of adversity, trauma, threat and stressful events27. Psychological resilience not only helps individuals adjust their own state and overcome difficulties, but also enables them to reshape themselves28. The process model of psychological resilience posits that individuals use resources to maintain physical and mental equilibrium in response to stressful events29. Patients with high psychological resilience levels cope actively with their own illness, maintain an optimistic outlook on life, and have a lower incidence of depression compared to those with low levels of resilience.
Perceived social support is the subjective emotional experience of feeling supported, respected and understood30. The use of resources is dependent on the individual’s internal psychological traits, such as their awareness of social support and self-esteem31. According to the cognitive basis model of psychological resilience, when an individual experiences prolonged stress or negative emotions, psychological resilience can activate the individual’s internal and external resources. This activation occurs through assessment and metacognitive processes, allowing the individual to make behavioral and psychological responses that protect them from potential negative emotions32. Psychological resilience is positively correlated with an individual’s ability to cope with stressful events and negative emotions, making them less susceptible to defeat and negative emotions. Studies have found a strong association between psychological resilience and emotions. Psychological resilience can alleviate the adverse effects of stress on individual emotions and reduce the incidence of stress-related negative emotions, thus reducing the risk of individuals suffering from depression. It is an internal and stable psychological trait33. Perceived social support can reduce psychological distress during stressful events34, and improve their levels of psychological resilience35. According to the main effect model of social support, good social support is a crucial element in helping individuals establish hope. When patients fall ill, they often experience fear of the disease and confusion about their future. By receiving support and care from the outside world, patients can stimulate their internal motivation and further improve their hope and confidence in overcoming the disease36. Perceived social support can assist patients in utilizing available support resources to solve life problems, reduce fear of disease, and increase confidence in their ability to cope with the adverse outcomes. This can lead to greater psychological benefits and improved mental health37.
Disease acceptance is the extent to which a patient refrains from seeking a definitive solution to the physical distress and instead focuses on positive daily activities and other aspects of life38. The concept of disease acceptance implies that the patient maintains a positive awareness of the disease and regains a sense of personal control over it by integrating the experience into their lifestyle39. Disease acceptance is a crucial factor in patients’ psychosocial adjustment. It directly affects their disease management behavior, and has a significant predictive effect on their mental health and quality of life40,41. As per the symptom experience model, patients’ self-perception influences their ability to accept the disease. Accepting a disease can help patients improve their social courage and confidence, and alleviate feelings of alienation42,43. Positive social support can also enhance the acceptance and coping ability of chronic patients44. According to research45, accepting a disease can help patients come to terms with their illness, accept the changes it brings, and remain optimistic about moving forward with their lives. The quality of life of patients with chronic diseases is positively correlated with their acceptance of the disease. Improving disease acceptance can effectively enhance patients’ quality of life46,47.
Previous studies have investigated the interrelationships between psychological resilience, perceived social support, and disease acceptance and mindfulness. Studies on similar populations have shown that psychological resilience, disease acceptance, and perceived social support are essential factors affecting mindfulness. These findings provide valuable insights into promoting overall well-being in patient populations facing chronic health conditions. Furthermore, Kuang et al. discovered that negative emotions in cancer patients not only directly predicted the level of mindfulness but also had an indirect impact on mindfulness through perceived social support and psychological resilience48. Berdida et al. reported that social support mediated the influence of stress on resilience, mindfulness and psychological well- being among nursing students49. The impact of WD on a patient’s life is significant, with negative effects that can exacerbate the patient’s condition. Previous studies have demonstrated the efficacy of mindfulness interventions in reducing psychological distress and promoting health in patients with chronic diseases. However, there is a paucity of research examining the potential benefits of mindfulness in patients with WD. Although some chronic conditions have demonstrated correlations between perceived social support, mental resilience, disease acceptance, and mindfulness, it remains unclear whether these effects are also present in individuals with WD. To the best of our knowledge, no previous studies have investigated the link between perceived social support, mental resilience, illness acceptance, and mindfulness in people with WD. Therefore, a thorough understanding of this relationship is essential to identify specific measures to improve the health of people with WD. Furthermore, our study can provide a theoretical basis and practical reference for the formulation of mindfulness interventions and specific measures for WD patients.
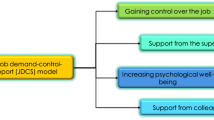
In this study, we used a structural equation model to investigate the relationships between perceived social support, psychological resilience, disease acceptance and mindfulness in patients with WD. Our hypotheses, as shown in Fig. 1, were developed based on a review of the literature. (1) The level of perceived social support has a direct impact on psychological resilience, disease acceptance and mindfulness. (2) Perceived social support can also indirectly affect mindfulness through psychological resilience or disease acceptance. (3) Psychological resilience has a direct impact on mindfulness. (4) Disease acceptance has both direct and indirect effects on mindfulness through psychological resilience.
The study
Design
This study used a cross-sectional and questionnaire-based design.
Participants
This study used convenience sampling to select 136 patients with HLD who were admitted to outpatient and inpatient departments of 12 tertiary hospitals in Sichuan Province from May 2019 to January 2023. Inclusion criteria were: (1) aged 18 years or older; (2) diagnosed clinically with HLD50; (3) participation in other clinical trials. The Medical Ethics Committee of West China Fourth Hospital, Sichuan University, has approved this study (HXSY-EC-2019003), and informed consent has been obtained from the patients. In accordance with the Kendall estimation method51, the requisite sample size is 5–10 times the total number of variables under investigation. In this study, the general data encompass 8 variables and 4 scales, resulting in a total of 14 dimensions. Therefore, the number of variables is 22. With a 10% loss rate factored in, the optimal sample size is calculated to be 121–242 cases. The final sample size for this study was 136.
Instruments
Demographic
The researchers designed the general information survey form themselves, which included general sociodemographic data about the patients and treatment of the disease.
Five facet mindfulness scale (FFMS)
The FFMS was developed by Baer et al.52 and it includes 39 items across five dimensions: observing, describing, acting with awareness, non-judging, and non-reacting. The Likert 5-point scale ranges from “completely inconsistent” to “completely consistent,” and scores are calculated from 1 to 5. The total score ranges from 39 to 195, with higher scores indicating higher levels of mindfulness. The Chinese version of this scale has been extensively used in various settings and has demonstrated good psychometric properties. Confirmatory factor analysis in this study indicated that the questionnaire had good structural validity (χ2 /df = 4.78, GFI = 0.908, CFI = 0.913, RMSEA = 0.066), and the Cronbach’s alpha coefficient was 0.85.
Connor-Davidson resilience scale (CD-RISC)
The CD-RISC was developed by Connor and Davidson53 to measure an individual’s psychological resilience. This study used the CD-RISC scale revised by Yu et al.54, which shows good reliability and validity and has been widely used in China. The CD-RISC scale includes 23 items across three dimensions: toughness, self-improvement, and optimism. The Likert 5-point scale ranges from 0 to 4, with higher scores indicating higher levels of psychological resilience. The total score ranges from 0 to 40. Confirmatory factor analysis in this study demonstrated good structural validity of the questionnaire (χ2/df = 4.45, GFI = 0.905, CFI = 0.904, RMSEA = 0.062), and the Cronbach’s alpha coefficient was 0.93.
Acceptance of illness scale (AIS)
The AIS was developed by Felton et al.55 to measure an individual’s acceptance of illness. It includes eight items on disease-related limitations, decreased or lost self-sufficiency, and dependence on others. This study used the Chinese version of the AIS scale56, with a Likert 5-point scale ranging from 1, “strongly agree,” to 5, “strongly disagree.” The total score ranges from 8 to 40, with higher scores indicating higher levels of acceptance of illness. The scale showed strong internal consistency (Cronbach’s α = 0.88) and test-retest reliability (0.91)57. Confirmatory factor analysis in this study indicated that the questionnaire had good structural validity (χ2/df = 4.76, GFI = 0.950, CFI = 0.878, RMSEA = 0.065), and the Cronbach’s alpha coefficient was 0.81.
Perceived social support scale (PSSS)
The PSSS was developed by Zimet et al.58 to evaluate an individual’s perceived social support. This study used the Chinese version of the PSSS scale translated by Zhang Fan et al.59. It includes 12 items across two dimensions: internal and external support. A Likert 7-point scale ranges from 1, “completely disagree,” to 7, “completely agree.” The total score ranges from 12 to 84, with higher scores indicating higher levels of social support. The total scale’s Cronbach’s α and test-retest reliability were 0.90 and 0.88, respectively60. The questionnaire demonstrated good structural validity in this study, as confirmed by the results of the confirmatory factor analysis (χ2/df = 4.29, GFI = 0.889, CFI = 0.917, RMSEA = 0.070), and the Cronbach’s alpha coefficient was 0.91.
Data collection method
Before the survey, the researchers provided training to the surveyors on using the questionnaires and survey plan. During the survey, one surveyor used uniform instructional language to provide the patients with instructions on the purpose and significance of the survey and how to complete the questionnaire. After obtaining the patient’s consent, the survey was distributed to the patient to be completed without collecting personal information. On-site collection was conducted and completed surveys with missing information, or smudged answers were excluded. A total of 136 survey questionnaires were distributed, 136 were completed, and the effective response rate was 100%.
Data analysis
Data were double-entered using Epidata 3.1 software and analyzed using SPSS 25.0 and AMOS 25.0 software. For normally distributed measurement data, mean and standard deviation were used, while frequency and percentage were used to describe count data. Two independent sample t-tests and variance analysis were used for inter-group comparisons. For non-normally distributed measurement data, median and quartile were used to describe and inter-group comparisons were conducted using Mann-Whitney U-test and Kruskal-Wallis H-test. Pearson correlation analysis was used to analyze the correlation between study variables. Harman single-factor analysis and latent variable method were used to test for common method bias in the data. Structural equation modeling was used to examine relationships between study variables, and bootstrap resampling was used to obtain more stable and accurate estimates of standard errors. The path analysis method was used to identify direct and indirect effects in the model. The following fit indices61 were used to evaluate model fit: chi-square/degree of freedom (χ2/df) < 2 (P > 0.05), goodness of fit index (GFI) > 0.90, adjusted goodness of fit index (AGFI) > 0.90, comparative fit index (CFI) > 0.90, Tucker-Lewis index (TLI) > 0.90, and root mean square error of approximation (RMSEA) < 0.06. The Akaike information criterion (AIC) was used to compare modified models with initial models. Statistical significance was set at P < 0.05.
Validity, reliability and rigor
All questionnaires used in this study have been adopted for and used previously in China, and the reliability and internal consistency were found to be acceptable.
Results
General information of participants
The demographic characteristics of the participants are presented in Table 1. The sample consists of predominantly 18–34-year-old participants (59.56%). The majority were male (58.09%) and unmarried (65.44%).
Test for common method bias
Results of Harman’s single-factor analysis showed that there were 23 factors with eigenvalues greater than 1. However, the variation explained by the first factor was only 17.41%, which is lower than the critical standard of 40%62. The latent variable method indicated that the chi-square difference value of the fit index for the baseline model (χ2/df = 1.599, GFI = 0.963, AGFI = 0.950, CFI = 0.938, TLI = 0.954, RMSEA = 0.052) and the control model (χ2/df = 1.600, GFI = 0.962, AGFI = 0.949, CFI = 0.937, TLI = 0.954, RMSEA = 0.051) was not statistically significant [△df = 1, △χ2 = 0.716, P = 0.400 > 0.01, n = 136, α = 0.01 as the critical value63. Therefore, it can be concluded that there is no significant common method bias in the data of this study.
Robustness analysis
In order to test the robustness of this study, we divided the sample into a male group (n = 79) and a female group (n = 57). The results are shown in Tables 2 and 3. Minor changes are observed between the two groups, but the interpretation of the results remains essentially unchanged.
Analysis of the correlation among research variables
The results of the analysis of the correlation among research variables are presented in Table 4. The scores of mindfulness, social support, psychological resilience, and illness acceptance were (128.63 ± 22.62), (65.51 ± 10.37), (28.62 ± 9.64), and (29.58 ± 8.92), respectively. Mindfulness was significantly positively correlated with social support, psychological resilience, and illness acceptance (r = 0.39, 0.48, 0.35, all P < 0.01), while social support was significantly positively correlated with psychological resilience and illness acceptance (r = 0.52, 0.47, both P < 0.01). Moreover, psychological resilience was positively correlated with illness acceptance (r = 0.58, P < 0.01). The disease course was significantly negatively correlated with mindfulness, psychological resilience, and illness acceptance (r = -0.61,-0.51, -0.58, all P < 0.01). Hospitalization times were significantly negatively correlated with mindfulness, social support, and illness acceptance (r = -0.53, -0.60, -0.57, all P < 0.01), while clinical classification was positively correlated with social support (r = 0.15, P < 0.05).
Structural equation modeling
After controlling for disease course and hospitalization times, which showed significant correlations with research variables (Fig. 2), the initial model showed good fit indices (χ2/df = 1.853, P = 0.121; GFI = 0.987, AGFI = 0.949, CFI = 0.988, TLI = 0.962, RMSEA = 0.053). However, this study found that the path coefficient from illness acceptance to mindfulness and clinical classification to social support were insignificant. After deleting insignificant paths and controlling for disease course and hospitalization times, the modified model showed better fit indices (χ2/df = 1.225, P = 0.374; GFI = 0.990, AGFI = 0.952, CFI = 0.999, TLI = 0.971, RMSEA = 0.040). Comparing AIC values between the two models suggested that the modified model had a better fit (AIC for the initial model = 52.685 vs. AIC for the modified model = 36.579). The path coefficients among the research variables are shown in Fig. 1.
The results of the mediation effect test (Table 5) showed that social support had a positive predictive effect on illness acceptance (β = 0.43, P < 0.05), psychological resilience (β = 0.40, P < 0.01), and mindfulness (β = 0.18, P < 0.01). Social support indirectly influenced mindfulness through psychological resilience (β = 0.21, P < 0.01) and indirectly influenced psychological resilience through illness acceptance (β = 0.13, P < 0.01). Psychological resilience had a direct impact on mindfulness (β = 0.36, P < 0.05), and illness acceptance had an indirect effect on mindfulness through psychological resilience (β = 0.11, P < 0.05). The disease course was directly and indirectly associated with mindfulness, while social support was associated with hospitalization times, and both disease course and hospitalization times had direct and indirect effects on mindfulness.
Discussion
This study presents evidence on the relationships between perceived social support, psychological resilience, acceptance of illness and mindfulness among patients with HLD, offering insights into factors that could potentially enhance their mindfulness. The structural model indicates that perceived social support and psychological resilience are important predictors of mindfulness in patients with HLD. Furthermore, perceived social support had a direct impact on psychological resilience and acceptance of illness, and an indirect impact on mindfulness through psychological resilience. Acceptance of illness indirectly influenced mindfulness through psychological resilience. The hypotheses concerning the relationships among study variables are supported, except for the direct impact of acceptance of illness on mindfulness.
This study found that the mean score for mindfulness among the HLD population was approximately 65% of the total score, indicating insufficient mindfulness. This is consistent with previous research64,65,66. It is recommended that mindfulness be promoted in patients with HLD. As hypothesized, perceived social support was found to be an important factor influencing mindfulness among patients with HLD. Appropriate support is significantly associated with improved physical and psychological health outcomes. This can help patients feel more at ease with their surroundings and better cope with the physical and psychological discomfort caused by their illness67. Our findings are consistent with previous research that has shown a positive correlation between perceived social support and mindfulness in cancer survivors and pregnant individuals68. According to a study, cancer patients who perceive greater social support also exhibit higher levels of mindfulness48. Cancer patients can better understand their negative emotions and biases towards them when they receive kindness and care from family, friends, and others. This understanding allows them to adjust their state of mind and adopt a tolerant and accepting attitude towards all physical and mental events. Such an attitude can improve an individual’s negative emotions, enhance their physical and psychological indicators, and promote self-management of behavior and lifestyle69. Patients with HLD may develop unclear feelings about the disease due to its repeated episodes, complex clinical manifestations, and chronic nature. As a result, they may frequently suffer from negative emotions, face social stigma, and experience substantial psychosocial stress3, which may affect their ability to receive adequate support. Our study revealed that patients with HLD did not receive sufficient support from their social networks. Therefore, it is crucial to help enhance their support from families, healthcare providers, communities, and other sources to help them cope with the illness and increase their mindfulness.
In the modified model, perceived social support also indirectly influenced mindfulness through psychological resilience. This suggests that patients with better perceived social support may have higher resilience when performing mindfulness. A possible explanation may be that patients with Wilson’s disease have relatively closed thoughts and behaviors due to the characteristics of the disease. Additionally, traditional Chinese culture and disease stigma may make patients reluctant to seek help from others for fear of discrimination70, resulting in a lack of social interaction and social support. Over time, this can lead to severe social and psychological stress, which can reduce an individual’s chances of obtaining social support. It is important to note that this is a possible explanation and further research is needed to confirm this hypothesis. According to the theory of social support, helping behaviors from others are important resources in the social support system and can help individuals cope with setbacks or difficulties. However, understanding social support is even more important in enhancing an individual’s psychological health and future development25. When patients lack social support, they may struggle to observe and accept themselves well, resulting in lower levels of cognitive insight and self-healing. Therefore, social stigma associated with HLD may reduce the size of a patient’s support network and limit their ability to express their feelings and concerns, ultimately reducing their resilience and ability to increase mindfulness levels. Additionally, perceived social support appears to play a significant role in the acceptance of illness related about HLD. These results suggest that interventions aimed at enhancing perceived social support may benefit patients in improving their disease status in hepatolenticular disease.
Furthermore, previous research has supported the notion that psychological resilience is a significant predictor of mindfulness, as evidenced by this study71. This suggests that patients with greater psychological resilience are better able to acknowledge their current experiences and achieve internal balance, leading to improved mental well-being. Additionally, the study found that perceived social support affects mindfulness by mediating psychological resilience. According to research, patients with greater levels of social support demonstrate a greater ability to cope with illness, maintain a positive attitude, and gain confidence in self-regulation and healing72. Social support functions as an external protective factor for psychological resilience. When transformed into an internal cognitive factor, it can help individuals enhance their psychological resilience73. Additionally, it can reduce their experience of stress and psychological pain, and help them effectively cope with life challenges74. High levels of perceived social support can help patients to manage disease-related stress, increase their confidence in overcoming the disease, and improve their physical and mental well-being. This can ultimately lead to greater relaxation and a reduction in the negative effects of the disease. Additionally, the structural equation model shows that disease acceptance can indirectly impact the level of mindfulness in patients with Wilson’s disease through psychological resilience. This finding further highlights the significance of psychological resilience in mindfulness among patients with HLD. Previous studies have shown that psychological resilience acts as a mediator between certain factors (such as academic procrastination and negative emotions) and mindfulness75. Psychological resilience interventions have been successful in improving mindfulness in cancer patients. Our study assessed psychological resilience and found that patients did not have enough resilience to cope with HLD, which in turn affected their mindfulness of the illness. These results suggest that psychological resilience is a useful intervention target for HLD patients.
Contrary to our hypothesis, the direct path from acceptance of illness to mindfulness in the initial model was not significant. This indicates that accepting of illness alone does not lead to a change in mindfulness. Instead, acceptance of illness indirectly affects mindfulness through psychological resilience, which is consistent with another study76. Another study also found no significant association between acceptance of illness and mindfulness77. The study found that, similar to previous research, most patients with HLD had inadequate acceptance of illness78. Therefore, interventions to improve acceptance of illness should be provided to these patients due to its indirect effect on mindfulness.
Our study also identified the impact of disease course and hospitalization times on mindfulness. Patients with HLD who were hospitalized more frequently tended to have lower perceived social support. This may affect their acceptance of illness, psychological resilience, and mindfulness. Previous studies have reported that patients with atrial fibrillation who have had more hospitalizations have lower medication adherence, poorer self-reported outcomes79, and lower mindfulness levels80 and Chi Lin-Lin81. During the long-term treatment process for Wilson’s disease, patients may become concerned about treatment effects and prognosis, which can lead to a negative attitude towards the disease. This negative attitude can result in reduced treatment compliance, which can seriously affect their physical health and harm their psychological state. In this situation, patients may struggle to manage their attention and cognitive insight effectively, and fail to use their internal resources and energy to actively focus on themselves, resulting in lower levels of mindfulness82. These findings suggest that particular attention should be given to patients with longer disease courses or more hospitalization times, as they may be even less adherent to mindfulness.
This study is the first to investigate the factors influencing mindfulness among patients with HLD using a structural equation model. The findings provide valuable information for healthcare providers working with HLD. However, the study has some limitations. First, the cross-sectional design could introduce result bias, and longitudinal studies are still needed to confirm the findings. Second, this study was conducted in 12 tertiary hospitals in Sichuan. Therefore, caution should be exercised when generalizing our findings to hospitals at different levels or in other provinces. Future research studies should aim to include a larger sample size and intervention designs.
The study revealed that the mean score for mindfulness among patients with WD was 128.63 ± 22.62, indicating a moderate level of mindfulness57. Moderate levels of mindfulness have been demonstrated to exert a partial influence on patients’ illness and health outcomes57. Prior research has indicated that patients with moderate levels of mindfulness tend to exhibit reduced treatment compliance and heightened psychological distress compared to those with high levels of mindfulness83. Our findings have practical implications for healthcare providers involved in HLD care. The model suggests developing a multifaceted intervention to reduce potential barriers to mindfulness for this population. First, mindfulness interventions should be provided and strengthened extensively for patients with HLD. Nurses can enhance patients’ mental health by using mindfulness cognitive therapy and mindfulness-based stress reduction techniques, such as relaxation, mindful breathing, and meditation. Additionally, mindfulness interventions based on networks and smartphones can be utilized25. These techniques can help patients become aware of their thoughts and emotions, avoid automatic responses and rumination, provide positive guidance, and relieve negative feelings such as anxiety and depression during challenging situations84. This can increase patients’ confidence in their resources and potential, enabling them to better regulate their physical and mental changes better, achieve freedom from anxiety, and enhance their ability to cope with the disease. Second, perceived social support plays a crucial role in mindfulness among patients with HLD. Therefore, strategies to enhance perceived social support should be incorporated into mindfulness measures to facilitate more effective mindfulness interventions for patients with HLD. Additionally, nurses can use social support resources to assist these individuals in coping with difficulties and enhancing their social support, respect and understanding. It is important to note that patients should seek support and help from all parties, communicate with family members and colleagues, and actively participate in disease management. They should internalize external support as self-perceived energy, reducing or decentralizing negative emotions and thoughts to better cope with the disease. Third, interventions should include behavior change strategies aimed at improving psychological resilience. Nurses must attend to patients’ needs, value their emotions, and assist them in adjusting their feelings. They should encourage patients to maintain a positive and optimistic attitude. Further, Nursing staff can also help patients set achievable self-improvement goals and facilitate communication among them. Recommending high-quality WeChat public accounts or apps about Wilson’s disease can effectively help patients better understand the condition. In addition, nurses should encourage patients to objectively view their disease, avoiding the magnification of negative effects and affirming their internal traits and abilities. Patients should not compare their shortcomings with those of others25, as this can enhance their resilience and confidence in coping with setbacks, promoting self-support and self-healing, and help them accept their disease better.
Conclusion
This study found that perceived social support and psychological resilience are important predictors of mindfulness in patients with Wilson’s disease. Perceived social support directly affects psychological resilience and disease acceptance and indirectly affects mindfulness through psychological resilience. Disease acceptance itself cannot affect mindfulness but indirectly affects mindfulness through psychological resilience. Therefore, it is essential to improve the psychological resilience, perceived social support, and disease acceptance of patients with Wilson’s disease, especially psychological resilience, to promote improving their mindfulness level. Nursing staff can dynamically assess and pay attention to the psychological status of this group, and develop scientific and targeted intervention measures to improve patients’ mindfulness levels and promote disease recovery.
Data availability
The data sets used and analyzed in this study can be made available by the corresponding author at reasonable request.
References
Poujois, A. & Woimant, F. Challenges in the diagnosis of Wilson disease. Ann. Transl Med. 7 (Suppl 2), S67 (2019).
Bandmann, O., Weiss, K. H. & Kaler, S. G. Wilson’s disease and other neurological copper disorders. Lancet Neurol. 14 (1), 103–113 (2015).
Mulligan, C. & Bronstein, J. M. Wilson Disease: An Overview and Approach to Management. Neurol. Clin. 38 (2), 417–432 (2020).
Walshe, J. M. & Yealland, M. Wilson’s disease: the problem of delayed diagnosis. J. Neurol. Neurosurg. Psychiatry. 55 (8), 692–696 (1992).
Kim, J. W. et al. Genetically confirmed Wilson disease in a 9-month old boy with elevations of aminotransferases. World J. Hepatol. 5 (3), 156–159 (2013).
Beyersdorff, A. & Findeisen, A. Morbus Wilson: Case report of a two-year-old child as first manifestation. Scand. J. Gastroenterol. 41 (4), 496–497 (2006).
Ala, A., Borjigin, J., Rochwarger, A. & Schilsky, M. Wilson disease in septuagenarian siblings: raising the bar for diagnosis. Hepatology 41 (3), 668–670 (2005).
Ferenci, P. et al. Late-onset Wilson’s disease. Gastroenterology 132 (4), 1294–1298 (2007).
Saito, T. Presenting symptoms and natural history of Wilson disease. Eur. J. Pediatr. 146 (3), 261–265 (1987).
Kulkarni, A. & Sharma, V. K. Wilson’s Disease: Elsevier.
Cheung, K. S. et al. Epidemiology and natural history of Wilson’s disease in the Chinese: a territory-based study in Hong Kong between 2000 and 2016. World J. Gastroenterol. 23 (43), 7716–7726 (2017).
Poujois, A. et al. Characteristics and prevalence of Wilson’s disease: a 2013 observational population-based study in France. Clin. Res. Hepatol. Gastroenterol. 42 (1), 57–63 (2018).
Collet, C. et al. High genetic carrier frequency of Wilson’s disease in France: discrepancies with clinical prevalence. BMC Med. Genet. 19 (1), 143 (2018).
Coffey, A. J. et al. A genetic study of Wilson’s disease in the United Kingdom. Brain 136 (Pt 5), 1476–1487 (2013).
Jang, J. H., Lee, T., Bang, S., Kim, Y. E. & Cho, E. H. Carrier frequency of Wilson’s disease in the Korean population: a DNA-based approach. J. Hum. Genet. 62 (9), 815–818 (2017).
Dziezyc, K., Litwin, T., Chabik, G., Gramza, K. & Czlonkowska, A. Families with Wilson’s disease in subsequent generations: clinical and genetic analysis. Mov. Disord. 29 (14), 1828–1832 (2014).
Zhang, S. et al. Clinical and genetic characterization of a large cohort of patients with Wilson’s disease in China. Transl Neurodegener. 11 (1), 13 (2022).
Lindsay, E. K. & Creswell, J. D. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clin. Psychol. Rev. 51, 48–59 (2017).
Park, T., Reilly-Spong, M. & Gross, C. R. Mindfulness: a systematic review of instruments to measure an emergent patient-reported outcome (PRO). Qual. Life Res. 22 (10), 2639–2659 (2013).
Kabat-Zinn, J. Mindfulness-based interventions in context: past, present, and future. Clin. Psychol. Sci. Pract., 10(2):144–156 (2003).
Houghton, L. C. et al. Free Time for Wellness: a co-designed intervention utilizing social networks to encourage physical activity for cancer prevention among low resourced mothers. BMC Public. Health. 21 (1), 1805 (2021).
Lutz, J., Bruhl, A. B., Scheerer, H., Jancke, L. & Herwig, U. Neural correlates of mindful self-awareness in mindfulness meditators and meditation-naive subjects revisited. Biol. Psychol. 119, 21–30 (2016).
Verhaeghen, P. Mindfulness as attention training: Meta-analyses on the links between attention performance and mindfulness interventions, long-term Meditat ion practice, and Trait Mindfulness. Mindfulness, 12(3):564–581 (2021).
Leyland, A., Rowse, G. & Emerson, L. M. Experimental effects of mindfulness inductions on self-regulation: systematic review and meta-analysis. Emotion 19 (1), 108–122 (2019).
Al-Ghabeesh, S.H., Mahmoud, M., Rayan, A., Alnaeem, M. & Algunmeeyn, A. Mindfulness, Social Support, and Psychological Distress Among Jordanian Burn Patients. J Burn Care Res 45, 685-691, https://doi.org/10.1093/jbcr/irad195(2024).
Labrague, L. J. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J. Nurs. Manag. 29 (7), 1893–1905 (2021).
Delcea, C., Rad, D., Toderici, O. F. & Bululoi, A. S. Posttraumatic Growth, Maladaptive Cognitive Schemas and Psychological Distress in Individuals Involved in Road Traffic Accidents-A Conservation of Resources Theory Perspective. Healthcare (Basel) 11(22). (2023).
Fletcher, D. & Sarkar, M. A grounded theory of psychological resilience in olympic champions. Psychol. Sport Exerc., 13(5):669–678 (2012).
Balikji, J., Hoogbergen, M. M., Garssen, J. & Verster, J. C. Mental Resilience, Mood, and quality of life in young adults with self -reported impaired Wound Healing. IJERPH, 19(5):2542 .
Uchino, B. N. et al. Perceived social support and ambulatory blood pressure during daily life: a meta-analysis. J. Behav. Med. 45 (4), 509–517 (2022).
Hagger, M. S. Conservation of resources theory and the ‘strength’ model of self-control: conceptual overlap and commonalities. Stress Health. 31 (2), 89–94 (2015).
Wang, J. L., Zhang, D. J. & Zimmerman, M. A. Resilience theory and its implications for Chinese adolescents. Psychol. Rep. 117 (2), 354–375 (2015).
Eagle, D. E., Hybels, C. F. & Proeschold-Bell, R. J. Perceived social support, received social support, and depression amon g clergy. J. Social Personal Relationships, 36(7):2055–2073 (2019).
Karaca, A., Yildirim, N., Cangur, S., Acikgoz, F. & Akkus, D. Relationship between mental health of nursing students and coping, sel f-esteem and social support. Nurse Educ. Today, 76:44–50 (2019).
Berdida, D. J. E., Lopez, V. & Grande, R. A. N. Nursing students’ perceived stress, social support, self-efficacy, res ilience, mindfulness and psychological well‐being: A structural equati on model. Int. J. Mental Health Nurs., 32(5):1390–1404 (2023).
Daniel, L. C. et al. 1041 Sleep Quality mediates the relationship between fear of Cancer re currence and psychological distress in young adults with Cancer. Sleep, 43(Supplement_1):A395–A396 (2020).
Yaghoobzadeh, A. et al. Role of sex, socioeconomic status, and emotional support in Predicting Aging Perception among older adults. Int. J. Aging Hum. Dev. 87 (1), 77–89 (2018).
McCracken, L. M. & Eccleston, C. Coping or acceptance: what to do about chronic pain? Pain 105(1–2):197–204. (2003).
Karademas, E. C., Tsagaraki, A. & Lambrou, N. Illness acceptance, hospitalization stress and subjective health in a sample of chronic patients admitted to hospital. J. Health Psychol. 14 (8), 1243–1250 (2009).
Qiu, C., Zhang, X., Zang, X. & Zhao, Y. Acceptance of illness mediate the effects of health literacy on self-management behaviour. Eur. J. Cardiovasc. Nurs. 19 (5), 411–420 (2020).
Obieglo, M., Uchmanowicz, I., Wleklik, M., Jankowska-Polanska, B. & Kusmierz, M. The effect of acceptance of illness on the quality of life in patients with chronic heart failure. Eur. J. Cardiovasc. Nurs. 15 (4), 241–247 (2016).
Graboyes, E. M. et al. Body image disturbance in surgically treated Head and Neck Cancer patients: a prospective cohort pilot study. Otolaryngol. Head Neck Surg. 161 (1), 105–110 (2019).
Haggerty, B. B., Bradbury, T. N. & Karney, B. R. The disconnected couple: intimate relationships in the context of social isolation. Curr. Opin. Psychol. 43, 24–29 (2022).
Jordan, S. R., Geiger, C. L., Fischer, S. M. & Kessler, E. R. Care planning priorities of older patients with advanced bladder cance r. J. Geriatric Oncol., 13(4):432–439 (2022).
Uchmanowicz, I., Jankowska-Polanska, B., Chabowski, M., Uchmanowicz, B. & Fal, A. M. The influence of frailty syndrome on acceptance of illness in elderly patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct Pulmon Dis. 11, 2401–2407 (2016).
Chabowski, M., Juzwiszyn, J., Bolanowska, Z., Brzecka, A. & Jankowska-Polanska, B. Acceptance of Illness Associates with Better Quality of Life in patients with Nonmalignant Pulmonary diseases. Adv. Exp. Med. Biol. 1176, 19–24 (2019).
Pompey, C. S., Ridwan, M. N., Zahra, A. N. & Yona, S. Illness acceptance and quality of life among end state renal disease p atients undergoing hemodialysis. Enfermería Clínica, 29:128–133 (2019).
Lei, H. et al. The chain mediating role of social support and stigma in the relations hip between mindfulness and psychological distress among Chinese lung cancer patients. Support Care Cancer, 29(11):6761–6770 (2021).
Berdida, D. J. E., Lopez, V. & Grande, R. A. N. Nursing students’ perceived stress, social support, self-efficacy, resilience, mindfulness and psychological well-being: a structural equation model. Int. J. Ment Health Nurs. 32 (5), 1390–1404 (2023).
European Association for Study of L. EASL Clinical Practice guidelines: Wilson’s disease. J. Hepatol. 56 (3), 671–685 (2012).
Forthofer, R. N. & Lehnen, R. G. Rank Correlation Methods: Springer US.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J. & Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 13 (1), 27–45 (2006).
Connor, K. M. & Davidson, J. R. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety. 18 (2), 76–82 (2003).
Yu, X. & Zhang, J. Factor Analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behav. Personality Int. J. 35 (1), 19–30 (2007).
Felton, B. J., Revenson, T. A. & Hinrichsen, G. A. Stress and coping in the explanation of psychological adjustment among chronically ill adults. Soc. Sci. Med. 18 (10), 889–898 (1984).
WW, Z. Reliability and validity evaluation of the Chinese version of the disease Acceptance Scale. Chin. J. Mod. Nurs. 024 (022), 2652–2655 (2018).
Sierpinska, L. E. Assessment of the degree of illness acceptance in patients diagnosed with hepatitis C. Ann. Agric. Environ. Med. 29 (2), 224–231 (2022).
Zimet, G. D., Powell, S. S., Farley, G. K., Werkman, S. & Berkoff, K. A. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 55 (3–4), 610–617 (1990).
Fan, Z., Shuzhen, Z. & Pingji, D. Evaluation of Perceived Social Support Scale used in study of social support among hospitalized patients in China. Chin. Nurs. Res. 32(2018).
Kong, L. N. et al. Self-management behaviors in adults with chronic hepatitis B: a structural equation model. Int. J. Nurs. Stud. 116, 103382 (2021).
Wolf, M. G. & McNeish, D. Dynamic: an R Package for deriving dynamic fit Index Cutoffs for Factor Analysis. Multivar. Behav. Res. 58 (1), 189–194 (2023).
Podsakoff, P. M., MacKenzie, S. B. & Podsakoff, N. P. Sources of method bias in social science research and recommendations on how to control it. Annu. Rev. Psychol. 63, 539–569 (2012).
Wen, Z. L., Hau, K. T., Marsh, H. W. & STRUCTURAL EQUATION MODEL TESTING: CUTOFF CRITERIA FOR GOODNESS OF FIT INDICES AND CHI-SQUARE TEST. : Acta Physiol. Sinica 36(2):186–194. (2004).
Dunning, D. L. et al. Research Review: the effects of mindfulness-based interventions on cognition and mental health in children and adolescents - a meta-analysis of randomized controlled trials. J. Child. Psychol. Psychiatry. 60 (3), 244–258 (2019).
Zebdi, R. et al. Emotion regulation scale and mindfulness scale in school aged children: construction and validation of French versions. Child. Psychiatry Hum. Dev. 53 (5), 1004–1017 (2022).
Ameli, R. et al. Effect of a brief mindfulness-based program on stress in Health Care professionals at a US Biomedical Research Hospital: a Randomized Clinical Trial. JAMA Netw. Open. 3 (8), e2013424 (2020).
Dai, Z. et al. Mindfulness-based online intervention on mental health among undergraduate nursing students during coronavirus disease 2019 pandemic in Beijing, China: a randomized controlled trial. Front. Psychiatry. 13, 949477 (2022).
Sanchez Hernandez, H., Urizar, G. G. Jr. & Yim, I. S. The influence of mindfulness and social support on stress reactivity during pregnancy. Stress Health. 35 (3), 330–340 (2019).
Li, X. L. S. Q., Wang, L., Xie, J. F. & Zheng, S. J. Progress in the application of mindfulness intervention in nurses’ negative emotions. Chin. J. Nurs. 55 (2), 5 (2020).
Dan, L., Zheng, L., Qiugui, B., Nuo, X. U. & Meifeng, W. Perceived stigma in patients with inflammatory bowel disease and its effect on psychology,medication compliance and quality of life. Chin. J. Nurs. (2018).
Grbic, D., Jayas, A., McOwen, K. S., Shaull, L. & Andriole, D. A. Graduating medical students’ experiences with away (In-Person and virt ual) rotations during COVID-19: analysis of the Association of America N Medical Colleges (AAMC) 2021 Graduation Questionnaire (GQ). J. Surg. Educ., 80(5):646–656 (2023).
Al-Ghabeesh, S. H. Coping strategies, social support, and mindfulness improve the psychological well-being of Jordanian burn survivors: a descriptive correlational study. Burns 48 (1), 236–243 (2022).
Yan, H. X. C., Qi, M. Y., Zhang, S. X. & Li, R. Correlation between post traumatic growth, social support and resilience in patients with breast cancer. Chin. J. Mod. Nurs. 25 (21), 6 (2019).
Friborg, O. et al. Resilience as a moderator of pain and stress. J. Psychosom. Res. 61 (2), 213–219 (2006).
Wang, S., Bao, J., Liu, Y. & Zhang, D. The impact of online learning engagement on college students’ academic performance: the serial mediating effect of inquiry learning and refl ective learning. Innovations Educ. Teach. Int. :1–15 (2023).
Thompson, R. W., Arnkoff, D. B. & Glass, C. R. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma. Violence Abuse. 12 (4), 220–235 (2011).
Chinh, K. et al. Relations of Mindfulness and Illness Acceptance with Psychosocial Func tioning in patients with metastatic breast Cancer and caregivers. ONF, 47(6):739–752 (2020).
Kong, L. & Zhang, H. Latent profile analysis of depression in non-hospitalized elderly pati ents with hypertension and its influencing factors. J. Affect. Disord., 341:67–76 (2023).
Doshi, R. et al. Frequency, trends, and outcomes of cerebrovascular events Associated W Ith Atrial Fibrillation hospitalizations. Am. J. Cardiol., 138:53–60 (2021).
SS, L. Correlation of Mindfulness Level, Coping Style and Health Behavior in Patients with Coronary Atherosclerosis (Jinzhou Medical University, 2018).
LL, C. Investigation of Mindfulness Level in Patients with Chronic Obstructive Pulmonary Disease at home and Construction of Mindfulness Intervention Scheme (Qingdao University, 2018).
Roche, L., Dawson, D. L., Moghaddam, N. G. & Abey, A. An Acceptance and Commitment Therapy (ACT) intervention for chronic fatigue syndrome (CFS): a case series approach. J. Context. Behav. Sci. 6:S2212144717300315 (2017).
Hoge, E. A. et al. Mindfulness-based stress reduction vs Escitalopram for the treatment of adults with anxiety disorders: a Randomized Clinical Trial. JAMA Psychiatry. 80 (1), 13–21 (2023).
Yang, J., Tang, S. & Zhou, W. Effect of mindfulness-based stress reduction therapy on work stress and Mental Health of Psychiatric nurses. Psychiatr Danub. 30 (2), 189–196 (2018).
Acknowledgements
We would like to thank all participants for their involvement in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TW, YL: Conceived and designed the experiments, analyzed and interpreted the data, wrote the paper; TW, NW: Analyzed and interpreted the data, wrote the paper; SW: wrote the paper; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Participation in this study was voluntary and anonymous. Before signing the informed consent form, all patients were informed of the purpose and content of the survey. This study was approved by the institutional review board of the investigator’s affiliate hospital and all procedures were performed in accordance with the Declaration of Helsinki and written informed consent was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, T., Wu, N., Wang, S. et al. The relationship between psychological resilience, perceived social support, acceptance of illness and mindfulness in patients with hepatolenticular degeneration. Sci Rep 15, 1622 (2025). https://doi.org/10.1038/s41598-025-85956-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-85956-6