Abstract
With the popularity of breast screening, more and more intraductal papillary lesions (IDPL)were detected by ultrasound or mammography, which is a spectrum of diseases ranging from benign to malignant lesions. Patients with pathological nipple discharge (PND) may indicate IDPL, but it is difficult to clarify their biological characteristics before the operation. As to patients with IDPL without PND, it is even an enormous challenge to differentiate their benign or malignant characteristics. Therefore, to avoid inadequate treatment, it is necessary to analyze the clinicopathological and imaging characteristics of patients with papillary lesions before surgery for the preliminary diagnosis of benign or malignant papillary lesions. 267 cases of IDPL with or without PND, namely PND group and non-PND group, were studied using continuous clinical data from October 2020 to September 2023. We analyzed the clinicopathological and imaging characteristics in the two groups of patients with malignancy compared with benign patients. Meanwhile, these characteristics were analyzed in malignant papillary patients with PND or not. 267 patients were pathologically diagnosed with IDPL during three years, accounting for 15.4% of surgical cases of the same period. There were 55 patients with malignant lesions (20.6%), including 28 cases in the PND group (16.5%) and 27 cases in the non-PND group (27.8%), and the incidence of malignant lesions was higher in the non-PND group than that of the PND group. There was a close correlation between age and malignant lesions in the two groups; the number of patients older than 50 years in malignant patients (74.5%) exceeded that of benign patients (42.5%). There were nearly one-third of malignancies in patients with nipple bloody discharge, and the rate increased to 50% when the patient was older than 50 years, but the malignant rate was meager in patients without bloody discharge. There were some factors relating to malignancy in non-PND patients, including age, lesion size, the distance from the nipple to the lesson (DFNL), and abnormal mammogram; there was a significant difference in this positive manifestation between benign and malignant patients. In malignant intraductal papillary lesions, 40.8% of the cases were invasive carcinoma in the non-PND group, higher than in the PND group (10.7%). Meanwhile, immunohistochemistry was more likely to be hormone receptor-positive (92.6%) and Her-2 negative in the non-PND group, compared with the PND group. Breast IDPL is a common disease, among which malignant lesions are higher than reports in previous literature. There are some clinical and imaging manifestations indicating malignancy; patients more than 50 years old with bloody nipple discharge are at high risk of malignancy. When old non-PND patients have more significant lesions, remote DFNL, and abnormal mammograms, there is a high probability of malignancy in them. Although there are different biological characteristics in malignant IDPL with or without PND, they are all low-grade malignancies compared with traditional breast cancer.
Similar content being viewed by others
Introduction
WHO (2012) Classification of breast tumors named intraductal papillary tumors as intraductal papillary lesions, which is a spectrum of diseases ranging from benign lesions to malignant lesions, and is recognized as a diagnostic difficulty in the field of breast surgery1. According to the international classification of tumors, intraductal papilloma (IDP), intraductal papilloma with usual ductal hyperplasia (UDH), intraductal papilloma with atypical ductal hyperplasia (ADH), intraductal papillomatosis are classified as benign lesions. The intraductal papillary carcinoma with ductal carcinoma in situ (DCIS), intraductal papillary carcinoma (IPC), encapsulated papillary carcinoma (EPC), solid papillary carcinoma (SPC), DCIS with micro-invasion and DCIS with invasion are classified as malignant lesions1,2. Clinically, it is often difficult to distinguish benign from malignant papillary lesions because these lesions have overlapping clinical symptoms and imaging features3,4. Pathologically, there are some challenges to diagnose papillary lesion even after core needle biopsy (CNB), because of lesions heterogeneity5.
Patients with intraductal papillary lesions may present with pathological nipple discharge (PND) and/or palpable mass. PND is defined as spontaneous bloody or serous discharge in unilateral breast, caused by a single duct6. When the patient presents with PND, we may associate it with papillary lesions, but it is difficult to differentiate papillary lesions from other lesions in patient with non-PND. Because of extensive breast screening, more and more nodules, including some papillary lesions without PND, were detected by ultrasound or mammography. As its malignant tendency in papillary lesion, it is important to preliminary determining benign or malignant lesion in these patients before surgery, so as to avoid over-treatment and underestimation7.
Few studies have evaluated the clinicopathological or imaging features of intraductal papillary lesions with or without PND. In this study, we analyzed the data of 267 serial cases of intraductal papillary lesions confirmed pathologically in the past 3 years, and evaluated the relationship between the biological characters and clinicopathological or imaging features in these patients with PND or not.
Materials and methods
Study population
Clinicopathological data of patients undergoing breast surgery in Qingdao, Qilu Hospital of Shandong University during a 3-year period from October 2020 to September 2023 were retrospectively collected. During this period, 1736 patients underwent surgical resection of breast lesions, of which 267 patients with intraductal papillary lesions were found(15.4%). Inclusion criteria: Inpatients who complained of nipple discharge or breast nodules found by physical examination, complete clinical, imaging and postoperative pathological data were obtained. Exclusion criteria: physiological nipple discharge (pregnancy, lactation, oral contraceptives or sedatives, etc.), Clinical, imaging and postoperative pathological data were incomplete, pathology was associated with non-intraductal lesions (breast fibroadenoma, lobular tumor, invasive lobular carcinoma, breast cyst, breast adenopathy and mastitis). Finally, 267 female patients with a total of 280 papillary lesions were included in the study. For patients with bilateral lesions at the same time, when one breast was diagnosed as malignant lesions, they were classified as malignant lesions. Our institution’s ethics committee approved the retrospective study and waived the requirement of informed consent for patients whose medical records and imaging images were reviewed.
Observation indicators and definitions
Clinical, ultrasonic, molybdenum target and paraffin pathological data of enrolled patients were collected and sorted out, such as patient age, disease course, presence or absence of discharge, imaging characteristics of lesions. We used a mammogram camera (Siemens Erlangen, Germany) to perform a standard craniocaudal and mediolateral oblique mammogram of each breast. Molybdenum positive findings included high-density mass shadow, cluster and gravel calcification, and presence or absence of filling defect after galactography. The ultrasound was performed in a Philips iU22 unit (Philips Medical Systems, Bothell, WA) using a Philips L12-5 high-frequency linear ultrasound probe. The ultrasound features evaluated were presence or absence of nodules, distance from lesion to nipple (DFLN), nodule size, shape, direction, edge, echo, duct dilation, and vascular signals. The operators of the machines are radiologists and sonographers with at least 5 years of experience in scanning and interpreting breast ultrasound. Static and color Doppler images of the lesions are generated and stored in the hospital’s PACS. The pathological data of paraffin included the number of nodules, single or multiple, benign or malignant lesions. According to the clinical manifestations, the patients were divided into two groups, namely PND group and non-PND group.
Surgical method
Preoperative localization of the discharge ducts was performed by galactography or color ultrasound. The lacrimal passage irrigation needle was inserted into the discharge duct, and 0.2 mL methylene blue was injected into the discharge duct. The discharge duct and surrounding breast tissue were removed (segmental resection) under general anesthesia. As to papillary lesions without PND, Vacuum assisted excison was used to lesions ≤ 2 cm, and lesions more than 2 cm were removed with open surgery. If malignant lesions were verified with intraoperative frozen pathology or postoperative routine pathological examination, radical mastectomy were performed with or without sentinel lymph node biopsy.
Statistical method
SPSS 23.0 (IBM Corp. Armonk, NY) was used to process the data. The statistical data were expressed as percentage or number of cases. The Chi-square test or Fisher exact probability method was used for comparison between groups. When the p-value was less than 0.05, it was considered to be statistically significant.
Results
General clinicopathological characteristics of patients with papillary lesions
In serial 1736 patients underwent surgical resection of breast lesions during 3 years, 267 patients (15.4%) were diagnosed as intraductal papillary lesions, aged 13–95 years. Patients with bilateral lesions simultaneously were classified into the malignant lesion group when one breast was diagnosed as malignant lesion, and 13 patients had bilateral papillary lesions. The postoperative pathological diagnosis was 212 patients with benign lesions and 55 patients with malignant lesions(20.6%).
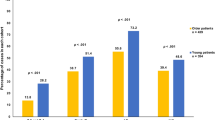
There were 170 papillary lesions in PND group, including 28 malignancy (16.5%). In non-PND group, 27 cases were malignancy (27.8%) among the total 97 cases of papillary lesions. The incidence of malignant lesions was higher in non-PND group (27.8%) than that of PND group (16.5%, P < 0.05, Table 1). Meanwhile, there was close correlation between age and malignant lesions in the two groups, the number of patients older than 50 years in malignant patients (74.5%) exceed the benign patients (42.5%) (P < 0.05).
The PND cases (170) accounted for 63.7% of total patients with papillary lesions, among of them, 84 cases with bloody discharge (49.4%). There were 28 malignant patients with bloody discharge, account for 29.8% of total patients with bloody discharge. However, the malignant rate was only 3.5% in patients with serous or clear nipple discharge (Table 1).
Clinical and imaging characteristics of PND patient group with benign or malignant lesions
In PND group, patient age with malignant papillary lesions was older than that of benign patients, and the number of cases>50 years were more than benign cases (57.1% vs. 28.9%,P = 0.004, Table 2), it was consistent with the overall age trend of malignant patients in this study. Notably, the rate of nipple bloody discharge was higher in malignant patients than those with benign lesions, there were nearly one-thirds of malignancy in patients with nipple bloody discharge, but the malignant rate was very low in patients without bloody discharge (P < 0.001, Table 2). The lesion size was usually less than 1 cm in PND patients, and couldn’t be palpated, and there was no difference in lesion size between benign and malignant groups. Other factors, including duct abnormality and blood flow signal showed in color Doppler ultrasound, even abnormal galactography, had no significant difference between the two groups (Table 2). In general, the age older than 50 years and bloody discharge were risk factors indicating malignancy in PND patient group (14/28, 50.0%).
Clinical and imaging characteristics of non-PND patients with benign or malignant lesions
Like the PND patients with malignant papillary lesions, the age of non-PND malignant patients was also older than that of benign patients (P = 0.003, Table 3). As to the difference in lesion size between malignant and benign patients, it was not alike the PND patients. The lesion size was usually more than 1 cm in non-PND malignant patients, and could be palpated, but there were more lesions size less than 1 cm in benign patients, and could’t be palpated (P < 0.001, Table 3). There was significant difference in the distance from nipple to lesion(DFNL) between the two groups, the number of patients with malignant lesions more than 2 cm in DFNL exceed to those with benign lesions (P < 0.001,Table 3). Other factors, including irregular shape, duct abnormality and blood flow signal showed on ultrasound, had no significant difference between the benign and malignant patients. However, abnormal mamogram in malignant patients was common, including mass, calcification, distortion and asymmetry, and these positive manifestation were rare in benign patients, there was significant difference between benign and malignant patients (P < 0.001, Table 3). Meanwhile, The patients who were assigned as BI-RADS (Breast Imaging- Reporting and Data system) 4B-5 were diagnosed more malignancies than the patients who were assigned as BI-RADS 3–4 A) (Table 3).
Comparison of clinicopathological and imaging features of malignant patients with PND or not
In our data, although old age had positive relationship with malignancy in both PND and non-PND groups, there were more patients older than 50 years in non-PND group, compared with PND group (P = 0.003, Table 4). Meanwhile, the number of lesion size>1 cm in non-PND group was more than PND group, as is the case in palpable mass (P < 0.001). Other factors including the DFNL, blood flow signal on ultrasound were not significantly different between the PND and non-PND groups (Table 4).
Pathologically, DCIS including EPC, SPC, accounted for 74.5% in the two groups, but the number of DCIS in PND group (89.3%) was higher than that in non-PND group (59.3%), and vice versa in IDC (P = 0.011, Table 4)). In terms of immunohistochemistry, 25 in 27 cases of non-PND patients (92.6%) highly expressed ER and PR, it was higher than that in PND group (18/28, 64.3%, p = 0.0111). However, the positive rate of Her-2 expression in non-PND group (3.7%) was lower than that in PND group (28.6%, p = 0.013). There was no significant difference in Ki67 expression between the two groups.
Discussion
Breast cancer is one of the most common malignancies in women and the leading cause of cancer-related death among women worldwide, and early detection and treatment is the key to improving survival rates for breast cancer patients8. In breast screening, more and more nodules were detected by ultrasound or mammography, and some nodules were verified as papillary lesions pathologically. Our serial data suggested that intraductal papillary lesion had a high incidence of 15.4% in breast lesions after surgery, among which malignant lesions account for 20.6%, which was higher than the 10–15% incidence reported in previous literatures more than 20 years ago9,10. Therefore, we believe that the diagnosis and treatment of intraductal papillary lesions is essential for the early detection of breast cancer and the reduction of breast cancer mortality.
Nipple discharge is a common symptom in women, accounting for about 5% of the symptoms of female breast visits6. PND is mostly manifested as spontaneous, bloody or serous discharge in unilateral breast, caused by a single duct11. PND often suggests duct papillary lesions, however, some patients with breast papillary lesions don’t present PND, as in our study, 36.3% of papillary lesions were not associated with PND. No matter papillary lesions with PND or not, the most importance is to differentiate malignancy from benign lesions. We found there was close correlation between age and malignant lesions in both PND and non-PND patient groups, like the common characteristics of malignancy incidence, nearly 75% of malignant patients was older than 50 years, but in benign patients only 43%. Our findings were similar to Seltzer’s reports, they proposed that the likelihood of cancer increased dramatically in women older than 50 years12.
In our serial data, the PND cases accounted for almost 64% of total patients with papillary lesions, among of them, 50% of cases with bloody discharge. Morrogh et al. reported that 33% of patients with DCIS and 25% with ductal hyperplasia when they presented bloody discharge13, but the absence of bloody discharge didn’t rule out malignancy14. Like Morrogh et al. report, we found that there were nearly one-thirds of malignancy in patients with nipple bloody discharge, but the malignancy was rare in patients with serous or clear nipple discharge(3.5%). Furthermore, the malignant incidence rate was higher in older patients, and there were 50% malignancy in bloody discharge patients older than 50 years. These data remind us when a patient is older than 50 years, with bloody nipple discharge, she has high probability of suffering from malignancy.
Clinically, when patient presents with PND, we may associate it with papillary lesion, but the papillary lesions in patient with non-PND is difficult to differentiate from other lesions, especially to determine benign or malignant lesion in these patients. Because of extensive breast screening, more and more papillary lesions without PND were detected by ultrasound or mammography. In our study, like the PND patients, the age of non-PND malignant patients was also older than that of benign patients, it means the papillary lesion in patients older than 50 years should be paid more attention. It was reported that intraductal papillary lesion larger than 1 cm was at high risk for malignancy15, in our non-PND malignant patients, we also found the lesion size was larger than that in benign cases, and could be palpated. Literature reports suggested that the lesion biological characters had relationship with the distance from nipple to lesion(DFNL), the peripheral lesion, namely remote DFNL, tend to be malignant15,16. Our research showed there was significant difference in the DFNL in non-PND patients with benign or malignant lesions, the number of patients with malignant lesions more than 2 cm in DFNL exceed to those with benign lesions. Sometimes, it is difficult to diagnosed papillary lesion pathologically even after core needle biopsy (CNB), because of its heterogeneity17,18. It suggests that open resection should be used to avoid underestimate after diagnosis of papillary lesions on CNB19, especially when the patient has these risk factors, including older than 50 years, lesion size more than 1 cm, remote DFNL etc.
From the above data, we could find there were different clinicopathological and imaging characters between benign and malignant papillary lesions with PND or not, whether there were differences in malignant lesions with PND or not. We found the age was older and the lesion size was larger in non-PND patients group, compared with PND group. Except for galactography, rare abnormality manifested on mammogram in PND group, but in non-PND group, abnormal imaging were often found on mammogram. The reasons may be that the lesions are larger and the age are older in non-PND patients, these factors facilitate the abnormal imaging to show on mammogram.
Pathologically, in the PND group, we found there were more DCIS cases, including SPC and EPC, but more IDC cases in non-PND group. It mean the malignant degree in PND patients with cancer is lower than that in non-PND patients. However, the expression of ER/PR were higher, the expression of Her-2 were lower in the non-PND malignant group, compared with those in the PND malignant group. The immunochemical expression of ER, PR, Her-2 in PND patients with malignant lesions was similar to documental data. But the expression of ER/PR was higher and Her-2 expression was lower in non-PND malignant patients, it was similar to Rehman’s reports in EPC and SPC of breast20. This suggests that non-PND malignant patients might have good prognosis, although accompany with invasive lesions21.
In conclusion, our serial data suggested that malignancy accounted for 20.6% of papillary lesions, higher than reports in previous literature. There was close correlation between age and malignant lesions in both PND and non-PND patients, nearly 75% of malignant patients was older than 50 years. When a patient was older than 50 years, with bloody nipple discharge, her probability of suffering from malignancy was 50% or so. Attentions should be paid to these non-PND patients when they had these risk factors including older than 50 years, lesion size more than 1 cm, DFNL more than 2 cm. There were more DCIS in patients with PND, but more IDC in non-PND patients, however, their biological characters were good in the two groups, might indicate good prognosis.
Data availability
The datasets are available from corresponding author on reasonable request.
References
Cserni, G. Histological type and typing of breast carcinomas and the WHO classification changes over time. Pathologica 112 (1), 25–41 (2020).
Kulka, J., Madaras, L., Floris, G. & Lax, S. F. Papillary lesions of the breast. Virchows Arch. 480 (1), 65–84 (2022).
Rakha, E. A. & Ellis, I. O. Diagnostic challenges in papillary lesions of the breast. Pathology 50 (1), 100–110 (2018).
Elfgen, C. et al. Third International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Virchows Arch. 483 (1), 5–20 (2023).
Qiu, L. et al. Diagnosis of papillary breast lesions on Core Needle Biopsy: upgrade Rates and Interobserver Variability. Int. J. Surg. Pathol. 27 (7), 736–743 (2019).
Dolan, R. T., Butler, J. S., Kell, M. R., Gorey, T. F. & Stokes, M. A. Nipple discharge and the efficacy of duct cytology in evaluating breast cancer risk. Surgeon 8 (5), 252–258 (2010).
Makita, M., Akiyama, F., Gomi, N. & Iwase, T. Mammary ductoscopy and watchful follow-up substitute microdochectomy in patients with bloody nipple discharge. Breast Cancer. 23 (2), 242–251 (2016).
Sung, H. et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 (3), 209–249 (2021).
Van Zee, K. J., Ortega Pérez, G., Minnard, E. & Cohen, M. A. Preoperative galactography increases the diagnostic yield of major duct excision for nipple discharge. Cancer 82 (10), 1874–1880 (1998).
Grillo, M., Lehmann-Willenbrock, E. & Gent, H. J. Chromogalactography preceding ductal-lobular unit excision for nipple discharge–with special reference to diagnostic galactography and histology. Ann. Chir. Gynaecol. 79 (1), 6–9 (1990).
Patel, B. K., Falcon, S. & Drukteinis, J. Management of nipple discharge and the associated imaging findings. Am. J. Med. 128 (4), 353–360 (2015).
Seltzer, M. H. Breast complaints, biopsies, and cancer correlated with age in 10,000 consecutive new surgical referrals. Breast J. 10 (2), 111–117 (2004).
Morrogh, M., Park, A., Elkin, E. B. & King, T. A. Lessons learned from 416 cases of nipple discharge of the breast. Am. J. Surg. 200 (1), 73–80 (2010).
Patel, B. K. et al. Nipple discharge: imaging variability among U.S. Radiologists. AJR Am. J. Roentgenol. 211 (4), 920–925 (2018).
Kuehner, G. et al. Benign papillary breast Mass lesions: favorable outcomes with Surgical Excision or Imaging Surveillance. Ann. Surg. Oncol. 26 (6), 1695–1703 (2019).
Oh, J. & Park, J. Y. Clinicopathological and Imaging features of breast papillary lesions and their association with pathologic nipple discharge. Diagnostics (Basel). 13 (5), 878 (2023).
Abbassi-Rahbar, S., Amin, A. L., Reflections, A. S. O. A. & De-escalation of Surgical Excision for Intraductal Papilloma of the breast. Ann. Surg. Oncol. 29 (Suppl 3), 593–594 (2022).
Liu, C. et al. Risk of malignancy in papillary neoplasms of the breast. Breast Cancer Res. Treat. 178 (1), 87–94 (2019).
Chen, P. et al. Treatment and outcome of 341 papillary breast lesions. World J. Surg. 43 (10), 2477–2482 (2019).
Rehman, B. et al. Papillary carcinoma of breast: clinicopathological characteristics, management, and Survival. Int. J. Breast Cancer. 2022, 5427837 (2022).
Morgan, S., Dodington, D., Wu, J. M. & Turashvili, G. Solid Papillary Carcinoma and Encapsulated Papillary Carcinoma of the breast: clinical-pathologic features and basement membrane studies of 50 cases. Pathobiology 88 (5), 359–373 (2021).
Acknowledgements
This work is supported by the Flexible talent guidance project, Qilu Hospital of Shandong University (Qingdao), No. QDKY2022RX01.
Author information
Authors and Affiliations
Contributions
QP drafted the work. MHS and PL collected data. DZG designed the work and revised it. All authors have read and approved the final manuscript, and ensure that this is the case.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pu, Q., Li, P., Su, M. et al. Analysis of the clinicopathological and imaging features in breast intraductal papillary lesions with or without pathological nipple discharge. Sci Rep 15, 2478 (2025). https://doi.org/10.1038/s41598-025-87278-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87278-z