Abstract
This study aimed to assess the prevalence, severity, and progression of swallowing impairments in head and neck cancer (HNC) patients before and after treatment, using videofluoroscopy with the Modified Barium Swallow Impairment Profile (MBSImP) protocol. We retrospect survey 90 HNC patients was divided into rehabilitation (receiving swallowing rehabilitation) and non-rehabilitation groups. All participants underwent a videofluoroscopic swallowing study with MBSImP, the Penetration-Aspiration Scale (PAS), and the Swallowing Performance Status (SPS) scale, along with assessments using the EAT-10 and Functional Oral Intake Scale (FOIS) at baseline, and at 1 and 3 months post-treatment. In all patients, MBSImP, PAS, and FOIS scores worsened one month after therapy. However, patients who performed swallow exercises demonstrated statistically significant improvements in swallowing function (FOIS and EAT-10) and related quality of life (EAT-10, Reflux Symptom Index) after three months of rehabilitation. High aspiration rates (poor PAS scores) were observed in all HNC patients post-treatment, peaking at 1 month and persisting over time. Notably, the rehabilitation group showed recovery of swallowing function to pre-treatment levels. Dysphagia is a significant and enduring side effect that impacts the quality of life in HNC patients undergoing multimodal treatment. The study suggests that a proactive swallowing rehabilitation program can positively influence outcomes, particularly after 3 months of rehabilitation.
Similar content being viewed by others
Introduction
Dysphagia impacts nutrition and the overall health of patients with head and neck cancer. Swallowing function can be impaired not only by the cancer itself but also by treatments such as chemoradiation therapy and surgery1,2. Head and neck cancers include oral cavity, oropharyngeal, laryngeal, and hypopharyngeal cancers, with the tumor location influencing which phase of swallowing is affected (oral, oropharyngeal, or pharyngeal-esophageal phase). Early intervention to restore swallowing function before, during, and after cancer treatment is crucial for preventing the worsening of dysphagia, improving patients’ quality of life, enhancing disease control, and increasing survival rates3,4. Tailored swallowing rehabilitation protocols, such as those based on the Modified Barium Swallow (MBS), are important for managing dysphagia in head and neck cancer patients5. However, the effectiveness of early rehabilitation in preserving and recovering swallowing function remains unclear.
In addition, dysphagia in oral cavity cancer primarily affects the oral preparation and oral phases, while in non-oral cavity cancers (such as laryngeal and hypopharyngeal cancers), dysphagia mainly affects the pharyngeal phase or the pharyngeal-esophageal segment1. However, studies comparing the effects of tailor-made functional restoration protocols, designed based on Modified Barium Swallow (MBS) evaluations, on patients’ subjective, physician’s subjective, and objective outcomes are rare. Therefore, we investigated changes in swallowing outcomes before and after the implementation of a functional restoration protocol to assess its impact on swallowing function. The evaluation tools included patients’ subjective assessments, such as the Eating Assessment Tool-10 (EAT-10) and the Reflux Symptom Index (RSI), as well as physicians’ objective evaluations using the Functional Oral Intake Scale (FOIS) via flexible endoscopic evaluation of swallowing (FEES), the Penetration-Aspiration Scale (PAS), and the Modified Barium Swallow Impairment Profile (MBSImP). Given that the treatment area frequently involves the pharyngeal constrictor muscles, reflux is commonly observed but seldom thoroughly assessed. We also evaluated reflux conditions using the RSI to determine whether the tailor-made functional restoration protocol could reduce reflux and improve related quality of life. The aim of this study was to investigate the effects of a tailor-made functional restoration protocol by comparing changes in EAT-10, RSI, FOIS, PAS, and MBSImP scores at baseline, 1 month, and 3-month post-intervention.
Methods
This is a retrospective study, and the medical charts of advanced head and neck cancer (HNC) were reviewed. The patients were divided into rehabilitation (receiving swallowing rehabilitation) and non-rehabilitation groups. Both groups had been treated at the department of rehabilitation medicine or otolaryngology. The data were corrected before treatment (baseline), 1-month, and 3-month. The protocol of MBSImP with videofluoroscopic swallowing study (VFSS), clinical objective and subjective evaluations were assessed. A rehabilitation physician in 20 years of experience and a senior laryngologist performed MBS swallowing studies and assessed the results. Two senior laryngologists performed FEES to assess. Intra-judge reliability was assessed the records by comparing each judge’s ratings across two consecutive days. Inter-judge reliability was evaluated the records by comparing the ratings between the two judges. No significant intra and intra-judge and reliability of assessments in MBS (Cohen’s kappa = 0.92 and 0.90, respectively) and FEES (Cohen’s kappa = 0.89 and 0.88, respectively) were noted (p < 0.05), Clinical subjective and objective evaluations were assessed by a speech therapist in 8 years of experience. All methods were carried out comply with the ethical standards of Helsinki declaration. The waiver approval for all clinical data and laboratory results was approved by the Institutional Review Boards of China Medical University Hospital (CMUH110-REC3-037).
Swallowing rehabilitation
The rehabilitation program is all designed according to the defects of swallowing function of each patient by MBS. Once the rehabilitation program is planned, the swallow exercises were carried out twice daily by assistant of rehabilitation physician. In the swallowing rehabilitation program is described in Table 1. Each session lasted at least 90 min and was conducted by speech therapists under the guidance of a physician. All patients received rehabilitation at the tertiary referral hospital, specifically in the Voice and Swallow Center. Patients were required to attend therapy sessions twice a week at the hospital, with therapists documenting their progress during each visit. The rehabilitation group underwent therapy at least twice a week for a duration of four weeks. These exercises were designed for each patient according to the disability showed on MBS. Once the rehabilitation program was designed, then it was completed twice weekly therapy by the assistant of CCC-SLP in the hospital, and twice daily therapy is done by patient themselves at home under telecom guided therapy of speech therapists.
Assessments
Clinical subjective evaluations
Ten-item eating assessment tool
The EAT-10 is a subjective questionnaire for self-reported swallowing impairment. The scale consisted of 10 components, and used 5-point score for the patients to assess their severity of swallowing difficulties6.
Reflux symptom index
Reflux symptom index (RSI) is a 9-items questionnaire for self-reported the symptoms of laryngopharyngeal reflux. It is often used to compare the changes on difficult swallowing on laryngopharyngeal reflux. RSI was scored from 0 (no problem) to 8 (severe), and total of score was 457.
Clinical objective evaluations
Functional oral intake scale
Functional Oral Intake Scale (FOIS) is a 7-point assessment scale for swallowing ability. Physician used FOIS to assess the swallowing function during feeding the daily diet. The lower FOIS score represented the severe impairment of swallowing function8. The swallowing ability was assessed using the FOIS.
Penetration-aspiration scale
Penetration-aspiration scale (PAS) is objectively a clinical assessment, and physician used PAS to evaluate the severity of dysphagia. PAS was scored from 1 (no penetration and aspiration) to 8 (aspiration), and the high PAS score was meant as high dysphagia severity9. If patient suffered from choking, dyspnea, unstable condition (desaturation or unstable vital sign), the MBS was immediately stopped.
Modified barium swallow impairment profile
Modified Barium Swallow Impairment Profile (MBSImP) is a standardized tool to assess the swallowing impairment. The MBS (SIEMENS™ ARCADIS Avantic C-arm) is used to record patient’s swallow 30 frames in a second, and MBSImP with 17 physiological swallowing parameters in a semi-quantitative evaluation is applied to measure all phases of swallowing10. It included swallowing assessments of the lips, tongue, soft palate, larynx, epiglottis, pharynx, and esophagus, scored on a scale of 0 (no impairment), to a maximum of 2, 3, or 4, depending on the severity of the impairment in each specific component. Further, three functional domains of oral, pharyngeal, and esophageal impairment are calculated to evaluate the swallowing impairment. A rehabilitation physician in 20 years of experience performing MBS swallowing studies and a senior laryngologist performed FEES, then the two senior doctors and two CCC-SLP grading the results.
Undergoing MBSImP, the Oral Impairment Score (OIS) ranges from 0 to 22, Pharyngeal Impairment Score (PIS) from 0 to 28, higher score in OIS, PIS signified poor swallow function11. Oral transit time (OTT) from tongue movement begins till the bolus to lower edege of mandible, pharyngeal delay time (PDT) from hyoid bursts till the bolus passing through cricopharyngeal muscle area, and pharyngeal transit time (PTT) from end of OTT till the pharyngeal swallowing trigger all measured by patient swallow 5 ml thin barium bolus12,13.
Statistical analysis
In the statistical analysis, all measured data were showed as mean ± standard deviation. A repeated-measures ANOVA (group × time) following the post-hoc of Bonferroni test was used to compare the differences in the variables between the rehabilitation and non-rehabilitation groups and assessed times (baselines, 1-month or 3-month). In subgroup analysis, the repeated-measures ANOVA (subgroup × time) was also used to compare between the sub-groups (OSCC + rehabilitation, non-OSCC + rehabilitation, OSCC + non-rehabilitation, and non-OSCC + non-rehabilitation) and assessed times (base-lines, 1-month or 3-month). We used SPSS version 25.0 (IBM Corp., Armonk, NY, USA) for statistical analyses. All significance levels were set at p < 0.05.
Results
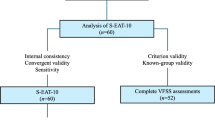
There were 124 patients with advanced head and neck cancer (HNC) were reviewed. Seventy-eight advanced stage oral cavity squamous cell carcinoma patients, all of them underwent surgical treatment with post operational chemoradiotherapy with cisplatin and 5 FU. In Fig. 1, there were 46 non-OSCC group which include 20 patients were oropharyngeal cancer and 26 patients hypopharyngeal cancer). In OSCC group, 18 of them did not have pre-treatment or post-treatment swallow evaluation. In non-OSCC group, 16 of them did not have pre-treatment or post-treatment swallow evaluation. Finally, there 90 advanced head and neck cancer patients enrolled in this study. Since we had arranged every patient proactive swallow therapy, however, some patients chose not to participate in swallow rehabilitation programs either before or during cancer therapy but they had pre and post therapy swallow evaluation, and they were finally as the control group.
There were 90 patients enrolled in our study and 66 of them were OSCC, and 24 of them were non-OSCC (oropharynx, hypopharynx) All 90 HNC patients underwent VFSS with the MBSImP protocol at 3 evaluation points: pre-treatment, and 1-month post-treatment and over 1 month after treatment. There were 42 male and 3 female patients. The average age is 51.32 ± 8.75 year-old. All of them had advanced tumor stage, there were 28 patients with T3 stage and 62 patients with T4 stage. For baseline, 6.46 ± 0.21 in FOIS, 4.24 ± 2.39 in RSI, is 0.38 ± 0.27 in OTT, and 0.16 ± 0.31 in PDT, 0.63 ± 0.29 in PTT, 4.27 ± 2.27 in OIS, 3.78 ± 3.07 in PIS, and 0.33 ± 0.67 in Esophageal Impairment Score were noted (Table 2). There were 44 patients with OSCC receiving early rehabilitation therapy and 22 patients with OSCC were not. There were also 12 patients with non-OSCC received early rehabilitation therapy but 12 patients with non-OSCC were not.
All swallowing physiology OTT, PTT, PDT in whole patient group didn’t have statistically significant between pre-treatment, short term post-treatment and long-term post-treatment (Table 3). There were also no significant OTT, PTT, PDT improvement in rehabilitation and non-rehabilitation group. The time period changes of improvement of OTT, PTT, also showed no significant difference between rehabilitation and non-rehabilitation groups excepting PDT.
All of the patients had deteriorated swallowing score in FOIS, RSI, EAT-10 and PAS before treatment (baseline), 1 month and 3 months after treatment. And all of the enrolled HNC patients who received swallowing therapy protocol therapy (individualized tailor-made rehabilitation program showed in Table 1). After 1 month period, there were significant improvement in FOIS. However, after 3 month rehabilitation there were significant improvement swallow scores in FOIS, RSI, EAT-10 and PAS, PDT. There were also found significant improvement in OSCC (oral cancer) and non-OSCC patients (oropharyngeal, hypopharyngeal cancer patients) who underwent over 1month period tailor made proactive rehabilitation in the FOIS, RSI, EAT-10 and PAS. Relationship between functional factors and PDT in rehabilitation group were statistically better than non-rehabilitation group (p < 0.05; Fig. 1).
The EAT-10 score is questionnaire which is a self-administered, symptom-specific outcome measure for dysphagia. In rehabilitation group, the score is significant recovered after over 1-month rehabilitation and will be not getting worse if re-habilitation going on to 3-month post treatment showed in Fig. 2A. In non-rehabilitation group, 1-month post-treatment EAT-10 was significant (p < 0.05) deterioration of swallowing was noted, which reached its peak at 1 month. However, 3-month post treatment EAT-10 score was statistically significant improved.
In rehabilitation group, 1-month post-treatment FOIS was significant (p < 0.001) deterioration of swallowing was noted, which reached its low at 1 month in Fig. 2B. There-after, 3-month post treatment FOIS statistically significant (p < 0.001) improvement in swallowing was observed. In non-rehabilitation group, FOIS score was lower than patients in rehabilitation group.
The scores of PAS at each evaluation time point are provided in Fig. 2C. In rehabilitation group, significant improvement of PAS was revealed between pre-treatment but not in non-rehabilitation group (Fig. 2C). The scores of RSI were significant change over time in both groups with Friedman test (p = 0.0215; Fig. 2D).
Discussion
Dysphagia is common occurred in patients with head and neck cancer. There were reported 70% head and neck cancer patients with swallow difficulties and higher gastric tube dependence is noted in oropharyngel cancer underwent concurrent chemoradiotherapy14. The dysphagia includes, oral, oropharyngeal and pharyngoesphageal segments in oral cavity cancer, oropharyngeal cancer, and hypopharyngeal cancer patients14. In this study, we enrolled 90 patients with HNC receiving treatment. We quantitatively investigated the change in swallowing after treatment for HNC patients and the impact of rehabilitation on it.
We assessed each of the patient’s swallowing function by functional oral intake scale, EAT-10, RSI, FOIS, and PAS score as well as swallow physiology (OTT, PTT, and PDT) in Table 3. The FOIS is not only the tool of evaluation patient’s dysphagia subjectively, but also the tool to show the current nasopharyngeal tube dependent condition for each patient. On the other hand, PAS could be an evaluation tool for evaluate the patient aspiration. We also applied EAT-10 as a tool to check oral dysphagia. We found that patients who were randomized to do rehabilitation had statistically significant better recovery in swallowing function (EAT-10, RSI, FOIS, and PAS), and had a better swallow physiology, i.e. PDT, recovery in Table 3.
Regarding swallowing physiology, most patients with dysphagia showed a problem in the pharyngeal phase. In our study, there was no statistically significant change in EAT10, OTT, PTT, PDT in both rehabilitation and control groups after 1 month rehabilitation (Table 3), but EAT10, FOIS, PAS and PDT change in rehabilitation group significantly improved after 3 months rehabilitation. These results suggested the better swallowing function will be gained after longer rehabilitation. Therefore, steadfastly offering the rehabilitation program in the peri-treatment periods is crucial for patients with head and neck cancer including oral cancer and non-oral cancer (oropharyngeal, hypopharyngeal cancer patients).
The PDT reached significant improvement after 3 months rehabilitation might be relating to the improvement of laryngeal suspension. Rehabilitation rescue the deterioration of swallowing function and prevent aspiration and improve quality of life. The rescue effect is found since 1 month of rehabilitation. The prominent improvement is noted after 3-month rehabilitation. The radiation or treatment affects the dysfunction of pharyngeal constriction muscle, surgery related muscle injury, microsites, neuropathy affect swallowing pharyngeal muscle strength which could be recover after 3-month treatment. However, the significant improvement in rehabilitation group. Concerning the mechanism, PDT is related to pharyngeal phase during swallowing and this is much related to the laryngeal elevation and lead to laryngeal arytenoid closure, the rehabilitation for laryngeal elevation as Mendelsohn maneuver rescue the deterioration for pharyngeal phase dysfunction12. Concerning about Esophageal Impairment Score, PIS, measured by MBSimp also revealed no significant change. One thing interesting is that, we hardly found the oral cancer itself will cause dysphagia, the same condition is also showed in non-OSCC since the cancer itself rarely cause dysphagia before treatment. However, all of the enrolled patients had deteriorated swallowing function after 1month treatment. In addition, the dysphagia is very common in hypopharyngeal cancer patients after treatment15. And dysphagia had also impact hypopharyngeal cancer patient’s quality of life16.
Another interesting finding is that the EAT-10, RSI, FOIS, PAS not associated with MBS findings. The possible explanation is rehabilitation that will lead to patient’s subjective improvement (not only physiologic functional but also mentally and socially) which showed by EAT-10, RSI, FOIS and PAS. However, the change of Oral, Pharyngeal, Esophageal Impairment Score, OTT, PDT is not significant deferred after early rehabilitation but resulted in PDT improvement after the rehabilitation. EAT-10, RSI, FOIS and PAS non-associated with MBSImp is also related to the small sample size.
Early swallow rehabilitation can significantly aid in the recovery of swallowing function after treatment for advanced head and neck cancer17. Treatments like surgery, radiation, and chemoradiation often cause substantial damage to the structures involved in swallowing, leading to dysphagia (difficulty swallowing)18. This can severely impact nutrition, quality of life, and even survival. Early intervention with swallow rehabilitation is crucial to mitigate these effects. Concerning about early rehabilitation (1 month) in oral cavity cancer, early intervention is considered for early recovery not only for oral eat phase but also pharyngeal phase. The three segments rehabilitation (oral, pharyngeal and pharyngoesophageal segments) not only improve oral cancer but non-oral cancer patients. In addition, early rehabilitation (rehabilitation 3 month after treatment) is not only applied and resulted in less severity of dysphagia for oral cancer but also non-OSCC as cancer patients. The recovery of swallowing function is also significant improved in 3-month rehabilitation both in oral and non-oral cancer patients since all swallowing function rehabilitation is beneficial to all of treated head and neck cancer.
In our study, we surely found that 1 to 3-month rehabilitation not only improved FOIS, PAS, EAT-10, RSI in oral cavity cancer but also in non-oral cavity cancer (oropharyngeal cancer, hypopharyngeal cancer). Therefore, early rehabilitation (1 month) is necessary to patients not only to OSCC but also to non-OSCC (oropharyngeal cancer, hypo-pharyngeal cancer) The possible cause of dysphagia followed by treatment of HNC patient might related to neck disability15, cervical and pharyngeal lymphedema coordination of laryngeal and pharyngeal muscles that will induce penetration and aspiration19.
Timely and early detection of dysphagia and tailor made proactive swallow therapy is recommended but remains challenge in the real world, since only the worst swallow handicapped patients could have had intention to treat their dysphagia but most of the HNSCC patients aware not20. Swallowing disorder usually attack 3 weeks since cancer treatment and we also found all head and neck patients in our study got worse swallowing function in 1 month after treatment in our study. But short term early individualized proactive swallowing therapy provided by a speech-language pathologist is very helpful in HNC (OSCC and non-OSCC) since treated and could reach to significant swallowing improvement after long term 3-month rehabilitation.
Conclusions
Early rehabilitation is not only suggested for patients with oral cavity cancer patient but also indicated for non-oral cavity cancer. Prominent improvement is noted after 1-month rehabilitation and prevent swallow function deterioration if rehabilitation goes on for 3 months.
Data availability
Data relative to this work will be available upon reasonable request to the corresponding author.
References
Pezdirec, M., Strojan, P. & Boltezar, I. H. Swallowing disorders after treatment for head and neck cancer. Radiol. Oncol. 53, 225–230 (2019).
Patterson, J. M. & Lawton, M. Dysphagia advances in head and neck cancer. Curr. Otorhinolaryngol. Rep. 1–8 (2023).
Messing, B. P. et al. Prophylactic swallow therapy for patients with head and neck cancer uder-going cemoradiotherapy: a randomized trial. Dysphagia 32, 487–500 (2017).
Greco, E. et al. Dysphagia treatment for patients with head and neck cancer undergoing radiation therapy: a meta-analysis review. Int. J. Radiat. Oncol. Biol. Phys. 101, 421–444 (2018).
Govender, R., Smith, C. H., Barratt, H., Gardner, B. & Taylor, S. A. SIP SMART: a parallel group randomised feasibility trial of a tailored pre-treatment swallowing intervention package compared with usual care for patients with head and neck cancer. BMC Cancer. 20, 360 (2020).
Belafsky, P. C. et al. Validity and reliability of the eat-ing Assessment Tool (EAT-10). Ann. Otol Rhinol Laryngol. 117, 919–924 (2008).
Belafsky, P. C., Postma, G. N. & Koufman, J. A. Validity and reliability of the reflux symptom index (RSI). J. Voice. 16, 274–277 (2002).
Crary, M. A., Mann, G. D. & Groher, M. E. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch. Phys. Med. Rehabil. 86, 1516–1520 (2005).
Rosenbek, J. C., Robbins, J. A., Roecker, E. B., Coyle, J. L. & Wood, J. L. A penetration-aspiration scale. Dysphagia 11, 93–98 (1996).
Krekeler, B. N. et al. Determining swallowing biomechanics underlying modified Barium Swallow Impairment Profile Scoring using computational analysis of swallowing mechanics. J. Speech Lang. Hear. Res. 65, 3798–3808 (2022).
Martin-Harris, B. et al. MBS measurement tool of swallow impairment- MBSImp: establishing a standard. Dysphagia 23, 392–405 (2008).
Kweon, S., Koo, B. S. & Jee, S. Change of swallowing in patients with head and neck cancer after concurrent chemoradiotherapy. Ann. Rehabil Med. 40, 1100–1107 (2016).
Terk, A. R., Leder, S. B. & Burrell, M. I. Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia 22, 89–93 (2007).
Hutcheson, K. A. et al. Late dysphagia after radi-otherapy-based treatment of head and neck cancer. Cancer 118, 5793–5799 (2012).
Harris, A. et al. Neck disability and swallowing function in posttreatment head and neck cancer patients. Otolaryngol. Head Neck Surg. 163, 763–770 (2020).
Kaae, J. K., Spejlborg, M. L., Spork, U., Bjørndal, K. & Eriksen, J. G. Reducing late dysphagia for head and neck cancer survivors with oral gel: a feasibility study. Dysphagia 35, 231–241 (2020).
Govender, R., Smith, C. H., Taylor, S. A., Barratt, H. & Gardner, B. Swallowing interventions for the treatment of dysphagia after head and neck cancer: a systematic review of behavioural strategies used to promote patient adherence to swallowing exercises. BMC Cancer. 17, 43 (2017).
van der Molen, L., van Rossum, M. A., Burkhead, L. M., Smeele, L. E. & Hilgers, F. J. Functional outcomes and rehabilitation strategies in patients treated with chemoradiotherapy for advanced head and neck cancer: a systematic review. Eur. Arch. Otorhinolaryngol. 266, 889–900 (2009).
Queija, D. D. S. et al. Cervicofacial and pharyngolaryngeal lymphedema and deglutition after head and neck cancer treatment. Dysphagia 35, 479–491 (2020).
Meng, N. H. et al. Longitudinal changes in swallowing function after surgery and proactive swallowing therapy for oral cancer. Head Neck. 45, 1632–1642 (2023).
Author information
Authors and Affiliations
Contributions
Study conception and design: Y.A.T. and N.H.M.; Data analysis and interpretation: Y.A.T., C.H.H. and N.H.M.; Drafting the article: Y.A.T. and W.D.C; Critically editing and revising the article: Y.A.T. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tsou, YA., Meng, NH., Chang, WD. et al. Does swallow rehabilitation improve recovery of swallow function after treatment for advanced head and neck cancer. Sci Rep 15, 8300 (2025). https://doi.org/10.1038/s41598-025-87877-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87877-w
Keywords
This article is cited by
-
Pre- and Rehabilitation of Swallowing in Head and Neck Cancer Patients
Current Otorhinolaryngology Reports (2025)