Abstract
Assessment of the quality of orthodontic care in a UAE-based orthodontic postgraduate training institution was conducted using multiple indices, including the Peer Assessment Rating (PAR), American Board of Orthodontics Objective Grading System (ABO-OGS), and Index of Complexity Outcome and Need (ICON). Retrospective evaluation of pre- and post-treatment records of patients (n = 201) treated with fixed orthodontic appliances was performed by two examiners Statistical analysis assessed the influence of gender, type of malocclusion, need for extraction, missed appointments and number of treating residents on treatment duration. The average numerical reduction of the PAR and ICON scores at the start and end of the treatment were 17.2 and 30.3, respectively, while the ABO-OGS post-treatment score was 14.8. The average PAR score reduction (84.5%) showed that the majority of the patients showed significant improvement at the end of treatment. Treatment duration correlated positively with ICON case complexity (p = 0.003), number of treating residents (r = 0.572, p < 0.001), and missed appointments (r = 0.671, p < 0.001) and negatively with age at treatment initiation (r = − 0.165, p = 0.019). The study findings indicated favorable outcomes for the quality of orthodontic care delivered by residents in a postgraduate training institution, though there were areas needing improvement. Optimizing the number of treating residents and minimizing missed appointments could further enhance clinical care.
Similar content being viewed by others
Introduction
Evaluating the effectiveness of orthodontic treatment and providing high-quality care to patients requires a thorough assessment of treatment needs, difficulties, and outcomes. Occlusal indices hold a significant importance across various aspects of orthodontics, including resource allocation, and the establishment of treatment standards1. Indices of treatment outcome also serve as a means of evaluating the quality of orthodontic care provided, thereby facilitating enhancements in education, research, and audit2,3. Information from these indices also offers valuable perceptions of the profiles of practitioners and healthcare systems prevailing within a nation4. Consequently, validated and reliable indices, such as the Peer Assessment Rating (PAR), American Board of Orthodontics Objective Grading System (ABO-OGS), and Index of Complexity Outcome and Need (ICON), have been widely used worldwide to assess standards of orthodontic care5,6,7,8,9,10,11,12,13.
These indices have become integral in assessing the standards of orthodontic care in both research and clinical practice. The PAR index is a widely utilized measure to assess orthodontic treatment outcomes by evaluating dental occlusion. It incorporates weighted scores for several occlusal components including alignment, buccal occlusion, overjet, overbite, and midline discrepancy. PAR enables an objective assessment of the severity of malocclusion and the improvement following treatment. The ABO-OGS is an assessment tool developed by the American Board of Orthodontics to objectively evaluate treatment quality by focusing on specific criteria, such as alignment, marginal ridges, buccolingual inclination, and overjet. The ICON is a comprehensive index designed to assess the complexity of malocclusion, predict treatment need, and evaluate outcomes. It combines five weighted components (esthetic assessment, upper arch crowding or spacing, crossbite, overbite/open bite, and buccal occlusion) to provide a single score and helps in determining treatment priority and assessing effectiveness.
The effectiveness of orthodontic treatment has been examined in a range of settings, including state-funded hospitals5,7,8,9, private practices6,10,11,12,13, educational programs14,15, and among practitioners with varying levels of expertise such as specialists and residents16. In graduate orthodontic programs, residents often provide a high standard of clinical care14, with reports showing that approximately half of the resident-treated cases meet the requirements for board certification15. The orthodontic outcomes for resident-treated cases are reported to be similar to those of board-certified practitioners17. In addition, the orthodontic outcomes for patients treated by residents and specialists in the same setting were not found to be significantly different16. However, when the orthodontic treatment outcomes of university orthodontic clinics were compared to private practices, some studies showed no differences18,19, whereas others reported suboptimal occlusal results for cases treated in a university setting20.
Although individual variations exist, the average duration of treatment with fixed orthodontic appliances lasts for approximately 2 years21. Malocclusion characteristics, patient-related, and operator-related factors can contribute to longer orthodontic treatment duration22,23. An increase in orthodontic treatment duration is associated with problems such as greater cost24, and a prolonged need for lifestyle modifications25. Additionally, the likelihood of root resorption26,27, gingival recession28, and enamel decalcification29 also increases with longer orthodontic treatment duration. It is unclear whether treatment duration varies based on the treatment setting, as some reports suggest a longer treatment duration in private practices19, while others indicate significant increases in treatment duration in educational settings30. Considering duration is also important when assessing the quality of orthodontic care provided, as it helps to evaluate the overall success of the treatment. Studies evaluating the quality of orthodontic care provided in academic settings in the UAE are sparse31. Therefore, this study aims to fill this gap by evaluating the quality of treatment provided by residents in an educational institute in the UAE using multiple indices, while simultaneously investigating possible correlations between treatment duration and patient- and operator-related variables.
Materials and Methods
Ethical considerations
This study was approved by the Mohammed Bin Rashid University—Institutional Review Board (MBRU IRB-2022-163). All research was performed in accordance with relevant guidelines/regulations of the institute. General consent to use the data for scientific purposes was obtained from the patients and/or their legal guardians at the time of registration. Due to the retrospective nature of the study, the Mohammed Bin Rashid University—Institutional Review Board waived the need of obtaining informed consent.
Sample size
Calculations using software (G*Power, Ver. 3.1.9.7) to determine the study sample size indicated that a sample size of 200 subjects was needed to represent the population for a power of 80% and a significance level of 0.05.
Inclusion and exclusion criteria
Patients who completed comprehensive orthodontic treatment with fixed appliances, with high-quality pre- and post-treatment records (photographs, dental casts with no chipping or breakage of any teeth and dental panoramic radiographs with no technical or patient-related artifacts), and a minimum retention time of six months were included in the study. Patients who received limited or adjunctive orthodontic treatment, with craniofacial syndromes, or with incomplete records were excluded.
Resident and faculty profile
The three year orthodontic residency program has a yearly intake of six residents (total = 18). The clinical faculty includes both full-time (n = 4) and part-time (n = 2) members, with a cumulative experience of over fifty years.
Dataset
The pre- and post-treatment orthodontic records of patients who underwent comprehensive orthodontic treatment with fixed appliances (22 slot, Roth prescription, stainless steel, American Orthodontics Mini Master® brackets; Sheboygan, USA) between 2015 and 2022 were included in this study. Information regarding sex, age at the start of treatment, category of malocclusion, whether extractions were a part of treatment, duration of active treatment, number of missed appointments as well as number of residents treating were obtained from the electronic dental records of the hospital. All patient information was de-identified before being made available to the investigators.
Measurement indices and calibration
The PAR, ABO-OGS and ICON were the three indices used in this study. Prior to commencing the study, the two investigators involved in the measurements (KG and AT) participated in multiple calibration sessions. Randomly selected casts (n = 25) were scored independently by two investigators (KG and AT) to assess inter-observer reliability, and the measurements were repeated after a two-week interval on the same set of casts to assess intra-observer reliability.
Data analysis
Data was analyzed in SPSS version 28 (IBM, SPSS Inc., Chicago, IL, USA). Descriptive data were collected and summarized from orthodontic records. The Shapiro–Wilk test was used to assess data normality. Spearman’s rank correlation was used to measure the strength and direction of association between the patient- and treatment-related variables. Mann–Whitney and Kruskal–Wallis tests were used for categorical variables. Statistical significance was set at p < 0.05 for all analyses. To create a visual representation of the distribution by nationality for those patients who underwent orthodontic treatment in this study, a spreadsheet application (Microsoft Excel 2022, https://www.microsoft.com/en-us/microsoft-365/excel) was utilized.
Results
Normality tests revealed that data were normally distributed. Patients (n = 201) included in the study were from over forty different nationalities (Fig. 1), a majority of which were females (Table 1). The majority of patients seeking treatment presented with Class II malocclusion, followed by Class I and Class III malocclusions (Table 1). The mean age at the start of orthodontic treatment was 19.8 ± 10.5 years (12–53 years). Orthodontic treatment was performed on a non-extraction basis in most patients (Table 2). Most patients received orthodontic care from a single resident and a small minority received care from more than two residents. The average duration of orthodontic treatment in this study was 816 ± 376.4 days with the mean number of visits to the orthodontic department being 28.8 ± 12.6, following a 3–4 weekly recall schedule. The average number of missed appointments was 3.3 ± 4.9 visits.
Nationality-wise distribution of patients who received orthodontic treatment at the institution. The visual map was generated using software (https://www.microsoft.com/en-us/microsoft-365/excel, Microsoft Excel 2022).
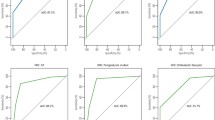
The inter- and intra-rater correlations for all indices were high (r ≥ 0.981), indicating excellent reliability. Assessment of treatment outcomes revealed significant improvements across all three measurement indices used in this study. The mean reduction in PAR score was 84.5%. PAR improvement scale and PAR score on a nomogram are outlined in Table 3 and Fig. 2 respectively for the patients included in this study. The ABO-OGS grade had a mean score of 14.8, with the majority classified as satisfactory (Table 3). Similarly, for the ICON scores, a reduction (30.3 points) was seen from the mean pre-treatment (42.1 points) to the post-treatment (11.8 points) with an acceptable orthodontic treatment outcome seen in all patients. Case complexity, as assessed by the ICON, revealed that a sizable proportion of patients seeking treatment were in the mild to moderate categories (Table 3). Treatment needs, as assessed by the ICON, revealed that 45.8% of the subject’s required treatment.
The correlations between orthodontic treatment duration and various patient- and operator-related factors investigated in this study are shown in Table 2. No correlation was observed between the malocclusion category (p = 0.121) or treatment modality (extraction/non-extraction) (p = 0.163) and treatment duration. However, a moderate positive correlation (r = 0.572, p < 0.001) was observed between the number of treating residents and treatment duration. Age at the start of treatment showed a mild positive correlation (p < 0.018, r = 0.165) with the treatment duration. Similarly, the number of missed appointments were also positively correlated (p < 0.001, r = 0.671) with treatment duration.
Discussion
This study reports original data on the outcomes of orthodontic treatment provided by residents within an educational setting in the UAE. The orthodontic outcomes of patients treated by residents within an educational setting have been previously documented but were outside the geographical region of this study14,15. Previous studies in the same geographical region investigated orthodontic treatment needs in a large sample of adolescents32,33 and examined orthodontic treatment outcomes31. Although the previous assessment of treatment outcomes was carried out in the same setting as in this study, the sample size was only one-tenth of the present study. In addition to the large sample size, the strengths of the current study also include the generalizability of the sample and use of multiple indices. Although this was a single-center study, the results are representative of diverse patient demographics (Fig. 1) owing to the multiethnic nature of the UAE population34.
At present, there is no universal assessment tool to evaluate orthodontic treatment outcomes. In this study, three indices were utilized, each serving to complement the other. For instance, the PAR index evaluates improvements in occlusion, establishes treatment standards35,36, and offers a detailed view of a single component, but falls short in assessing final outcomes37. The ABO-OGS index, on the other hand, quantifies finishing quality but fails to account for treatment complexity and needs38,39. Lastly, the ICON index assesses pre-treatment need and complexity in a more rigorous manner and incorporates an aesthetic standard in addition to the occlusal component40,41. Comparing scores among the aforementioned indices has also been done in the past1,42,43. The simultaneous use of three occlusal indices in this study enabled a comprehensive evaluation of the treatment results. Additionally, in this study, measurements of orthodontic study casts were used rather than those derived from lateral cephalograms, which are prone to measurement errors44. Advanced digital methods, including intraoral scanning and automated model analyses may also be incorporated in future studies.
The study limitations should also be considered. First, as this was a single-centre study, it is likely that the orthodontic treatment protocols followed were homogenous, thereby limiting the diversity of modalities available for patient treatment. The orthodontist’s choice of techniques and appliances can have varying effects on tooth movement with implications on treatment duration. Furthermore, the study focused on treatment assessment indices that are specifically of concern to clinicians, without assessing patients’ perceptions, satisfaction, and quality of life45. Also, only patients with complete records were included in the study, leading to a possible selection bias. Lastly, both assessors who evaluated the treatment outcomes were from the same academic setting, which may have introduced institutional biases that could potentially affect the outcome measures46. However, to mitigate this potential limitation, standardized measurement indices and a rigorous calibration process were utilized to ensure consistency in the data collection.
The PAR index was used to assess the pre- and post-treatment occlusal status of the patients in this study. The mean initial PAR score (19.3 ± 12.4) values in this study were similar to those reported from postgraduate training centers by Elshafee et al.31 and Firestone et al.47. On the other hand, the final PAR score (2.1 ± 4.7) in this study was relatively lower than postgraduate training centers in Europe12,47,48 but comparable to the centers in the United States49. The percentage reduction in the PAR score (84.59%) in this study was similar to that reported in a postgraduate training center in the United States49. The reported reduction in PAR score percentage ranges from 63 to 78% and includes diverse settings such as hospital orthodontic services7, public group practice9, and post-graduate training centers47,48. Only 5% of the cases (Fig. 2) were in the "worse/no different" category, suggesting a high standard of care provided by the residents. It should also be noted that the majority (61.2%) of orthodontic cases had an initial PAR score of less than 22 points. When the pre-treatment PAR score was higher, a trend towards longer treatment was also observed, similar to previously published literature by Birkeland et al.48.
ABO-OGS was also used to evaluate treatment outcomes and assess the quality of orthodontic treatment. Only 27 patients (13.4%) had unsatisfactory results, again indicative of a relatively high standard of care provided by the residents during their postgraduate training. The ABO-OGS score in this study (14.8 ± 9.8) was within the cutoff values reported in a multicenter study from China50. In this study, no significant correlation between treatment duration and the ABO-OGS score was observed. Interestingly, the ABO-Discrepancy Index (DI) has been reported to be useful for predicting orthodontic treatment time51. In addition to the ABO-OGS index, the ABO-DI is also a part of the ABO certification process. However, the focus of the ABO-DI is to quantify the starting difficulty and recognize clinician ability to treat cases of varying complexity.
The ICON was used to assess the complexity and the need for orthodontic treatment in this study. The international cutoff for orthodontic treatment needs using the ICON index is set at 43, but there are differing views (ICON cutoff of 52), which are population-specific52. Of the subjects seeking orthodontic treatment, 45.8% required treatment based on the pretreatment ICON score (> 43 points). Although the physical attributes of the ICON score are common, the subjectivity in perception of the esthetic component could possibly explain the variation observed. The mean ICON score obtained in this study was (42.1 ± 21.3) which was lower than a Norwegian study reported by King et al. (54.9)53 and a UK based study by Koochek et al. (69.0)54 respectively. It is also important to note that there is no waitlist for patients seeking orthodontic care in the UAE compared to other countries where orthodontic triage as a means of improving the appropriateness of referrals is common practice55.
The ICON results showed that all the patients in this study had acceptable results. This might be due to the fact that most of the cases had a low pre-treatment ICON score, in comparison to studies reporting (12–29%) unacceptable results9,13. The post-treatment ICON score (11.8 ± 4.5) was slightly lower than the value (15.8) reported by a general practice-based study in the UK54. Interestingly, problems associated with treating complex malocclusions in an educational setting have been highlighted in the past56. There was a significant difference between the ICON case complexity categories in terms of orthodontic treatment duration, indicating that complex cases took longer to treat. Overall, in this study, orthodontic treatment achieved a good treatment outcome, with a significant proportion of patients showing great or substantial improvement.
Without doubt, the outcome of orthodontic treatment is also influenced by patient compliance, including attendance at follow-up appointments57,58. In this study, a higher number of missed appointments was associated with longer treatment duration (Table 2), concurring with the findings reported by Kiyamehr et al.57. However, it must also be borne in mind that the study duration coincided with the social restrictions imposed by the pandemic59. A certain percentage of missed appointments in this study may have been due to the institution cancelling patient appointments to abide by local health authority regulations to prevent overcrowding in the clinics. However, the literature on the duration of orthodontic treatment due to the recent pandemic is inconclusive, as both increased59 and no differences60 have been reported. However, the reduced and irregular appointments during the pandemic did not have any effect on PAR score improvement60, which is similar to what we observed. No discernible impact on the length of orthodontic treatment was seen in this study on the basis of whether treatment was performed with or without extractions (Table 3), similar to the findings of Pariskou et al.14, but contrary to that of Holman et al.61.
Patient- and operator-related factors that contribute to longer treatment durations have been identified23,62. Factors such as sex and malocclusion category did not have any relationship with orthodontic treatment duration in this study. However, orthodontic treatment duration was observed to be longer in complex malocclusions, younger subjects, when patients missed appointments, and when multiple residents were involved in the treatment. Given the three-year duration of orthodontic resident training, patients are frequently transferred to junior residents during treatment63 which was also the case in this study. Residents tend to focus on patients who are progressing well in treatment resulting in finishing those cases by the time they graduate, and the patients who are not progressing as expected are often on the transfer list of the subsequent cohort of residents30,63. Diminished clinical outcomes are also seen in graduate orthodontic programs, particularly when the active treatment time is long63. This study found that when multiple residents were involved in providing care, treatment duration was longer. This is consistent with multiple retrospective studies that found significant increases in treatment duration resulting from changes in the operator across settings, including a teaching environment30, state-funded hospital64, and even private practice42. Interestingly, an increase in the treatment duration in an educational setting did not have a relationship with clinical outcomes62.
Conclusions
The findings of this study indicated favorable outcomes regarding the quality of orthodontic care delivered by residents in an academic environment. The duration of orthodontic treatment requires the establishment of fresh benchmarks to enhance clinical care.
Data availability
All data generated or analysed during this study are included in this published article.
References
Brown, R. & Richmond, S. An update on the analysis of agreement for orthodontic indices. Eur. J. Orthod. 27, 286–291. https://doi.org/10.1093/EJO/CJH078 (2005).
Shaw, W. C., Richmond, S. & O’Brien, K. D. The use of occlusal indices: a European perspective. Am. J. Orthod. Dentofac. Orthop. 107, 1–10. https://doi.org/10.1016/S0889-5406(95)70151-6 (1995).
Eliades, T. & Athanasiou, A. E. Advanced orthodontic education: Evolution of assessment criteria and methods to meet future challenges. Angle Orthod. 75, 143–143. https://doi.org/10.1043/0003-3219(2005)075%3c0143:AOEEOA%3e2.0.CO;2 (2005).
Roberts, C. T. & Richmond, S. The design and analysis of reliability studies for the use of epidemiological and audit indices in orthodontics. Br. J. Ortho 24, 139–147. https://doi.org/10.1093/ORTHO/24.2.139 (1997).
Richmond, S. et al. Orthodontics in the general dental service of England and Wales: a critical assessment of standards. Br. Dent. J. 174, 315–329. https://doi.org/10.1038/SJ.BDJ.4808166 (1993).
Younis, J. W., Vig, K. W. L., Rinchuse, D. J. & Weyant, R. J. A validation study of three indexes of orthodontic treatment need in the United States. Community Dent. Oral Epidemiol. 25, 358–362. https://doi.org/10.1111/J.1600-0528.1997.TB00955.X (1997).
O’Brien, K. D., Shaw, W. C. & Roberts, C. T. The use of occlusal indices in assessing the provision of orthodontic treatment by the hospital orthodontic service of England and Wales. Br. J. Orthod. 20, 25–35. https://doi.org/10.1179/BJO.20.1.25 (1993).
McMullan, R. E., Doubleday, B., Muir, J. D., Harradine, N. W. & Williams, J. K. Development of a treatment outcome standard as a result of a clinical audit of the outcome of fixed appliance therapy undertaken by hospital-based consultant orthodontists in the UK. Br. Dental J. 194, 81–84. https://doi.org/10.1038/SJ.BDJ.4809878 (2003).
Richmond, S. et al. Orthodontic treatment standards in a public group practice in Sweden. Swed. Dent. J. 25, 137–144 (2001).
Linder-Aronson, S., Fridh, G. & Jensen, R. Need of orthodontic treatment and orthodontic specialists in Sweden. Tandlakartidningen 68, 383–402 (1976).
Linder-Aronson, S. S. Orthodontics in the Swedish Public Dental Health Service. Eur. Orthod. Soc. 233–240 (1974).
Richmond, S. & Andrews, M. Orthodontic treatment standards in Norway. Eur. J. Orthod. 15, 7–15. https://doi.org/10.1093/EJO/15.1.7 (1993).
Richmond, S., Ikonomou, C., Williams, B. & Rolfe, B. Orthodontic treatment standards in Greece. Hellenic Orthod. 4, 9–20 (2001).
Pariskou, A. & Athanasiou, A. E. Assessing treatment outcomes of a graduate orthodontic program. Open Dent. J. 12, 896–903. https://doi.org/10.2174/1874210601812010896 (2018).
Santiago, J. J. & Martínez, C. J. Use of the objective grading system of the American Board of Orthodontics to evaluate treatment at the Orthodontic Graduate Program Clinic, University of Puerto Rico, 2007–2008. Puerto Rico Health Sci. J. 31, 29–34 (2012).
Tofeldt, L. N., Johnsson, A.-C. & Kjellberg, H. Evaluation of orthodontic treatment, retention and relapse in a 5-year follow-up: a comparison of treatment outcome between a specialist and a post-graduate clinic. Swed. Dent. J. 31, 121–127 (2007).
Dyken, R. A., Sadowsky, P. L. & Hurst, D. Orthodontic outcomes assessment using the peer assessment rating index. Angle Orthod. 71, 164–169 (2001).
Mislik, B., Konstantonis, D., Katsadouris, A. & Eliades, T. University clinic and private practice treatment outcomes in Class I extraction and nonextraction patients: A comparative study with the American Board of Orthodontics Objective Grading System. Am. J. Orthod. Dentofac. Orthop. 149, 253–258. https://doi.org/10.1016/J.AJODO.2015.10.012 (2016).
Mascarenhas, A. K. & Vig, K. Comparison of orthodontic treatment outcomes in educational and private practice settings. J. Dent. Educ. 66, 94–99. https://doi.org/10.1002/J.0022-0337.2002.66.1.TB03513.X (2002).
Yang-Powers, L. C., Sadowsky, C., Rosenstein, S. & Begole, E. A. Treatment outcome in a graduate orthodontic clinic using the American Board of Orthodontics grading system. Am. J. Orthod. Dentofac. Orthop. 122, 451–455. https://doi.org/10.1067/mod.2002.128464 (2002).
Tsichlaki, A., Chin, S. Y., Pandis, N. & Fleming, P. S. How long does treatment with fixed orthodontic appliances last? A systematic review. Am. J. Orthod. Dentofac. Orthop. 149, 308–318. https://doi.org/10.1016/j.ajodo.2015.09.020 (2016).
Prasad, S., Farella, M. & Melsen, B. In Adult Orthodontics 438–445 (2022).
Prasad, S. & Farella, M. Speed limits to orthodontic treatment: a review. N. Z. Dent. J. 117, 113–125 (2021).
Järvinen, S. & Widström, E. Determinants of costs of orthodontic treatment in the Finnish public health service. Swed. Dent. J. 26, 41–49 (2002).
Bernabé, E., Sheiham, A. & de Oliveira, C. M. Impacts on daily performances attributed to malocclusions by British adolescents. J. Oral Rehabil. 36, 26–31. https://doi.org/10.1111/j.1365-2842.2008.01899.x (2009).
Brezniak, N. & Wasserstein, A. Root resorption after orthodontic treatment: Part 1. Literature review. Am. J. Orthod. Dentofac. Orthop. 103, 62–66. https://doi.org/10.1016/0889-5406(93)70106-x (1993).
Segal, G. R., Schiffman, P. H. & Tuncay, O. C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod. Craniofac. Res. 7, 71–78. https://doi.org/10.1111/j.1601-6343.2004.00286.x (2004).
McComb, J. L. Orthodontic treatment and isolated gingival recession: a review. Br. J. Orthod. 21, 151–159. https://doi.org/10.1179/bjo.21.2.151 (1994).
Khalaf, K. Factors affecting the formation, severity and location of white spot lesions during orthodontic treatment with fixed appliances. J. Oral Maxillofac. Res. 5, e4. https://doi.org/10.5037/jomr.2014.5104 (2014).
McGuinness, N. J. & McDonald, J. P. The influence of operator changes on orthodontic treatment times and results in a postgraduate teaching environment. Eur. J. Orthod. 20, 159–167. https://doi.org/10.1093/EJO/20.2.159 (1998).
Elshafee, F. I., Naser-ud-Din, S., Khamis, A. H. & Athanasiou, A. E. Occlusal outcome assessment of orthodontic treatments performed at an educational institute in Dubai. J. Leban Dent. Assoc. 51, 60–70 (2017).
AlHammadi, H. A., Ferguson, D. J. & Makki, L. Index of complexity, outcome, and need (ICON) in Dubai school-aged adolescents. APOS Trends Orthod. 10, 32–37 (2020).
Al Jeshi, A., Al-Mulla, A. & Ferguson, D. J. Orthodontic treatment need in Dubai school adolescents: a study of 20,000 school-age adolescents in 66 public and private schools comparing orthodontic treatment need by gender and ethnicity. Oral Health Dent. Manag. 13, 857–865 (2014).
Baycar, H. Promoting multiculturalism and tolerance: Expanding the meaning of “unity through diversity” in the United Arab Emirates. Digest Middle East Stud. 32, 40–59. https://doi.org/10.1111/dome.12282 (2023).
Kerr, W. J., Buchanan, I. B. & McColl, J. H. Use of the PAR index in assessing the effectiveness of removable orthodontic appliances. Br. J. Orthod. 20, 351–357. https://doi.org/10.1179/BJO.20.4.351 (1993).
Richmond, S. et al. The development of the PAR Index (Peer Assessment Rating): reliability and validity. Eur. J. Orthod. 14, 125–139. https://doi.org/10.1093/EJO/14.2.125 (1992).
Hong, M. et al. The Improvement and Completion of Outcome index: A new assessment system for quality of orthodontic treatment. Korean J. Orthod. 46, 199–211. https://doi.org/10.4041/kjod.2016.46.4.199 (2016).
The American Board of Orthodontics Grading System for Dental Casts and Panoramic Radiographs. (The American Board of Orthodontics, 2012).
Casko, J. S. et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am. J. Orthod. Dentofac. Orthop. 114, 589–599. https://doi.org/10.1016/S0889-5406(98)70179-9 (1998).
Firestone, A. R., Michael Beck, F., Beglin, F. M., L Vig, K. W. & Orth, D. Validity of the index of complexity, outcome, and need (ICON) in determining orthodontic treatment need. Angle Orthod. 72 (2002).
Fox, N. A., Daniels, C. & Gilgrass, T. A comparison of the index of complexity outcome and need (ICON) with the peer assessment rating (PAR) and the index of orthodontic treatment need (IOTN). Br. Dent. J. 193, 225–230. https://doi.org/10.1038/SJ.BDJ.4801530 (2002).
Alsaeed, S. A. et al. Outcomes of orthodontic treatment performed by individual orthodontists vs 2 orthodontists collaborating on treatment. Am. J. Orthod. Dentofac. Orthop. 158, 59–67. https://doi.org/10.1016/j.ajodo.2019.07.015 (2020).
Onyeaso, C. O. & Begole, E. A. Relationship between index of complexity, outcome and need, dental aesthetic index, peer assessment rating index, and American Board of Orthodontics objective grading system. Am. J. Orthod. Dentofac. Orthop. 131, 248–252. https://doi.org/10.1016/J.AJODO.2005.04.045 (2007).
Houston, W. J. The analysis of errors in orthodontic measurements. Am. J. Orthod. 83, 382–390. https://doi.org/10.1016/0002-9416(83)90322-6 (1983).
Tsichlaki, A. & Fleming, P. S. Prioritising patients in research and practice—why and how?. J. Orthod. 46, 17–20. https://doi.org/10.1177/1465312519840032 (2019).
Prasad, S., Denotti, G. & Farella, M. Effect of prior knowledge about treatment on cephalometric measurements. J. Orthod. 49, 388–393. https://doi.org/10.1177/14653125221094333 (2022).
Firestone, A. R., Häsler, R. U. & Ingervall, B. Treatment results in dental school orthodontic patients in 1983 and 1993. Angle Orthod. 69, 19–26. https://doi.org/10.1043/0003-3219(1999)069%3c0019:TRIDSO%3e2.3.CO;2 (1999).
Birkeland, K., Furevik, J., Bøe, O. E. & Wisth, P. J. Evaluation of treatment and post-treatment changes by the PAR Index. Eur. J. Orthod. 19, 279–288. https://doi.org/10.1093/EJO/19.3.279 (1997).
Onyeaso, C. O. & Begole, E. A. Orthodontic treatment-improvement and standards using the peer assessment rating index. Angle Orthod. 76 (2006).
Song, G.-Y. et al. Validation of the American Board of Orthodontics Objective Grading System for assessing the treatment outcomes of Chinese patients. Am. J. Orthod. Dentofac. Orthop. 144, 391–397. https://doi.org/10.1016/j.ajodo.2013.04.018 (2013).
Aljehani, D. & Baeshen, H. A. Effectiveness of the American Board of Orthodontics Discrepancy Index in predicting Treatment Time. J. Contemp. Dent. Pract. 19, 647–650 (2018).
Louwerse, T. J., Aartman, I. H., Kramer, G. J. & Prahl-Andersen, B. The reliability and validity of the Index of Complexity, Outcome and Need for determining treatment need in Dutch orthodontic practice. Eur. J. Orthod. 28, 58–64. https://doi.org/10.1093/ejo/cji085 (2006).
King, G. J. & Brudvik, P. Effectiveness of interceptive orthodontic treatment in reducing malocclusions. Am. J. Orthod. Dentofac. Orthop. 137, 18–25. https://doi.org/10.1016/J.AJODO.2008.02.023 (2010).
Koochek, A. R., Shue-Te Yeh, M., Rolfe, B. & Richmond, S. The relationship between Index of Complexity, Outcome and Need, and patients’ perceptions of malocclusion: a study in general dental practice. Br. Dent. J. 191, 325–329, https://doi.org/10.1038/SJ.BDJ.4801175 (2001).
Willmot, D. R., Dibiase, D., Birnie, D. J. & Heesterman, R. A. The Consultant Orthodontists Group survey of hospital waiting lists and treated cases. Br. J. Orthod. 22, 53–57. https://doi.org/10.1179/BJO.22.1.53 (1995).
Campbell, C. L., Roberts, W. E., Hartsfield, J. K. & Qi, R. Treatment outcomes in a graduate orthodontic clinic for cases defined by the American Board of Orthodontics malocclusion categories. Am. J. Orthod. Dentofac. Orthop. 132, 822–829. https://doi.org/10.1016/J.AJODO.2006.05.036 (2007).
Kiyamehr, Z., Razeghinejad, M. H., Rahbar, M., Oskouei, S. G. & Vafaei, A. Factors affecting the duration of fixed orthodontic treatment in patients treated in a University Department between 2016 and 2020. Mædica 17, 380–380. https://doi.org/10.26574/MAEDICA.2022.17.2.380 (2022).
Nawarathna, L. Assessment of factors associated with patient’s compliance in orthodontic treatment. Sri Lanka Dent. J. 47, 1–12 (2017).
Santos, M., de Araujo Almeida, G. & Normando, D. The impact of COVID-19 pandemic on total treatment time of fixed appliances. Prog. Orthod. 23, 42. https://doi.org/10.1186/s40510-022-00437-0 (2022).
Meriç, P. & Naoumova, J. Did the coronavirus disease 2019 pandemic affect orthodontic treatment outcomes? A clinical evaluation using the objective grading system and Peer Assessment Rating index. Am. J. Orthod. Dentofac. Orthop. 162, e44–e51. https://doi.org/10.1016/j.ajodo.2021.12.017 (2022).
Holman, J. K., Hans, M. G., Nelson, S. & Powers, M. P. An assessment of extraction versus nonextraction orthodontic treatment using the peer assessment rating (PAR) index. Angle Orthod. 68, 527–534 (1998).
Vu, C. Q., Roberts, W. E., Hartsfield, J. K. & Ofner, S. Treatment complexity index for assessing the relationship of treatment duration and outcomes in a graduate orthodontics clinic. Am. J. Orthod. Dentofac. Orthop. 133(9), e1-9.e13. https://doi.org/10.1016/J.AJODO.2007.08.012 (2008).
Pinskaya, Y. B., Hsieh, T. J., Roberts, W. E. & Hartsfield, J. K. Comprehensive clinical evaluation as an outcome assessment for a graduate orthodontics program. Am. J. Orthod. Dentofac. Orthop. 126, 533–543. https://doi.org/10.1016/j.ajodo.2004.05.017 (2004).
Turbill, E. A., Richmond, S. & Wright, J. L. The time-factor in orthodontics: what influences the duration of treatments in National Health Service practices?. Community Dent. Oral Epidemiol. 29, 62–72 (2001).
Acknowledgements
Dr. Samira Diar-Bakirly for her help in the initial stages of the study, Dr. Angela Gonzalez, and Dr. Bayan Alyammahi for their support and contributions.
Funding
This study was supported by the Mohammed Bin Rashid University resident research fund.
Author information
Authors and Affiliations
Contributions
K.G.: Conceptualization, software, investigation, data curation, writing—original draft. A.Y.: Validation, investigation, visualization. R.A.: Formal analysis, resources, writing—review and editing. O.K.: Writing—review and editing. S.P.: Writing—review and editing, supervision, project administration, funding acquisition. A.G.: Resources.
Corresponding author
Ethics declarations
Human ethics and consent to participate
This study was approved by the Mohammed Bin Rashid University—Institutional Review Board (MBRU IRB-2022-163). In this retrospective study, data were collected from the records of patients who had provided consent for research purposes and we certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Due to the retrospective nature of the study, the Mohammed Bin Rashid University—Institutional Review Board waived the need of obtaining informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gyasudeen, K.S., Yousef, A.A., Alrubaiaan, R. et al. Quality of orthodontic care in an academic setting in the Middle East. Sci Rep 15, 3426 (2025). https://doi.org/10.1038/s41598-025-87927-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87927-3