Abstract
Jiangfangbaoxin (JFBX) has been used to attenuate essential hypertension (EH) for over 20 years. Here, we aimed to examine the blood composition and toxicological effects of JFBX using 40 and 10 male age-matched spontaneously hypertensive rats (SHRs) and Wistar–Kyoto, respectively. After 12 weeks of intervention, blood pressure and left ventricular hypertrophy were measured. Subsequently, their organs were harvested for pathological examination. Ultra-high-performance liquid chromate- graphy with quadrupole time-of-flight mass spectrometry was used to explore the components of JFBX in blood. Low and high-doses of JFBX attenuated both systolic and diastolic blood pressure in the SHRs. The high- and low-dose JFBX groups showed significantly reduced endothelin-1 and increased nitric oxide levels. The myocardial tissue levels of tumor necrosis factor-α, interleukin (IL)-1β, and IL-6 in the JFBX-high-dose group were significantly decreased. Furthermore, superoxide dismutase and malonaldehyde levels significantly increased and decreased, respectively. The toxicological results showed that JFBX did not cause particularly severe side effects when administered after 12 weeks. In total, 87 precursor compounds, including alkaloids, iridoid glycosides, flavonoids, siterpenoids, volatile components, and organic phenols/acids, were detected in the blood. JFBX attenuated EH. No serious organ damage was observed after 12 weeks of oral administration.
Similar content being viewed by others
Introduction
Essential hypertension (EH) is a common chronic diseases that threatens human life and health1. EH is primarily characterized by increased arterial blood pressure (BP), leading to various cardiovascular syndromes and damage to target organs, such as the heart, brain, and kidneys, often occurring in a continuous hyperdynamic circulatory state2. In addition, patients with EH are often diagnosed with other cardiovascular diseases, which serve as critical risk factors damaging crucial organs such as the heart and brain3. Currently, EH is predominantly attributed to genetic and environmental factors4. The latest survey showed that the incidence of adult hypertension in China is 27.9%. Furthermore, the population with high normal BP is increasing annually5. End-stage hypertension is often accompanied by multiple organ dysfunction syndrome and ultimately results in death. Most patients require long-term or even lifelong medication to maintain their BP within a stable range6.
According to the 2020 International Society of Hypertension Global Hypertension Practice Guidelines, hypertension is the most important risk factor for ischemic or hemorrhagic stroke, and over 50% of individuals with hypertension exhibit additional cardiovascular risk factors7. The guidelines emphasize the importance of achieving the basic standards for BP control. Evidence-based medicine and clinical research have shown that the Western medicine approach involves regulating BP and reducing target organ damage. Traditional Chinese medicine (TCM) has gradually played a role in the prevention and treatment of hypertension and could improve the quality of life of patients and reduce associated cardiovascular risk factors8,9.
According to the clinical symptoms, signs, syndromes, and other characteristics of hypertension, EH is categorized by “headache,” “dizziness,” “stroke,” or other syndromes based on the TCM theory10. Physicians practicing TCM believe that the lingering course of this disease can be primarily attributed to an interplay involving factors such as improper diet, emotional disorders, congenital constitution, blood stasis, and internal resistance. TCM is used to attenuate EH, primarily by promoting blood circulation and removing blood stasis8. In our previous study, liver depression, blood stasis, and heart vessel blockage were identified as the factors involved in the fundamental pathogenesis of EH, and the application of Jiangfangbaoxin (JFBX) showed good therapeutic efficacy11,12. JFBX was developed by M.D. Shu, a renowned Chinese medicine doctor practicing in Jiangsu Province and national Chinese medicine expert who was also an academic inheritance program instructor in China13,14. It is composed of nine Chinese herbs: Stephniae Tetrandrae Radix (Fangji), Rehmanniae Radix (Dihuang), Angelicae Sinensis Radix (Danggui), Paeoniae Radix Rubra (Chishao), Chuanxiong Rhizoma (Chuanxiong), Cyperi Rhizoma (Xiangfu), Puerariae Lobatae Radix (Gegen), Dalbergiae Odoriferae Lignum (Jiangxiang), and Paeoniae Radix Alba (Baishao). JFBX reduced BP in rats with renal vascular hypertension and decreased left ventricular weight and body-specific gravity15. It significantly reduced BP and fasting insulin levels in patients undergoing clinical trials for the treatment of hypertension with insulin resistance13. JFBX can restore and protect vascular endothelial cell function in patients with EH16. Chinese herbs and chemicals in JFBX improve cardiovascular function or reduces BP. The total glucosides of paeony have exhibited a potential protective effect in rats with chronic heart failure, along with remarkable anti-inflammatory and immunosuppressive effects17,18. Tetrandrine, a bisbenzylisoquinoline alkaloid extracted from the roots of Fangji, can inhibit the STING/TBK1/NF-κB signaling pathway to reduce inflammation in oxidized low-density lipoprotein-challenged macrophages and alleviate atherosclerosis in high-fat diet-fed ApoE-/-mice19. Kaempferol is the active component of Xiangfu. Furthermore, Baishao exhibits lipid-lowering, antioxidant, and anti-inflammatory effects and is associated with cardiovascular disease20.
Although JFBX has long been used in the clinical treatment of mild-to-moderate hypertension, fundamental research on its mechanisms and effects remains limited. Spontaneously hypertensive rats (SHRs), developed by Okamoto in 1963 via selective mating of Wistar rats, exhibited a 100% incidence of spontaneous hypertension. Wistar-Kyoto rats (WKYs) were initially bred from the same unit as SHRs and inbred with rats with normal BP; therefore, they are often used as controls for SHRs21. SHRs exhibit a very similar pathology to human EH, whose pathogenesis is primarily driven by genetic factors. Hence, they are ideal animal models to study cardiovascular diseases. The BP elevation begins at 6-weeks-of-age, and left ventricular hypertrophy is observed at 14 weeks-of-age in SHRs. Therefore, SHR and WKY rats were selected as study subjects to analyze the mechanisms and drug interventions of hypertension22.
No consensus has been established regarding the toxicity of S.Tetrandrae23,24. According to previous reports, the main chemical components of tetrandrine are alkaloids25. However, the hepatotoxicity and nephrotoxicity of tetrandrine have raised concerns regarding its safety26. In TCM, the purpose of reducing toxicity and increasing effects is emphasized by herbcompatibility27,28. Therefore, when conducting pharmacodynamic research, additional toxicology observation of the long-term use of JFBX is important for clinical application. This study aimed to observe the effect of JFBX on BP and analyze blood components in SHRs and observe the toxicological effects in SHRs 12 weeks after administration.
Results
High-performance liquid chromatography (HPLC)
JFBX (S01–S10) was selected for determination according to chromatographic conditions (Chemstation C.01.10 of Agilent, USA), and the chromatographic fingerprint similarity evaluation system (2012 edition, Chinese Pharmacopoeia Commission) was used for analysis. After multipoint correction of the chromatographic peaks, automatic matching was performed to generate control fingerprints (R; Fig. 1)29. Ten common peaks were identified, with peak 4 corresponding to acromial peaks. The other nine common peaks were well-separated morphologically and identified by reference products as follows: peak 1, gallic acid; peak 2, chlorogenic acid; peak 3, puerarin; peak 5, paeoniflorin; peak 6, ferulic acid; peak 7, fangchinoline; peak 8, tetrandrine; peak 9, ligustrone I; and peak 10, benzoyl paeoniflorin (Fig. 2). The area of peak 5 (paeoniflorin) was moderate, and the peak type was suitable; thus, when this peak was used as the reference peak, the similarity between the fingerprints of each batch of samples and control was between 0.98 and 0.99, indicating that each batch of samples exhibited good consistency (Fig. 3)30.
Identification of components in blood by ultra-high performance liquid chromatography with quadrupole time-of-flight mass spectrometry (UPLC-QTOF-MS/MS)
In the total ion flow diagram of the JFBX serum samples (Figs. 4 and 5), the obtained components were searched and compared with the mass spectrum data of the blank serum and administered serum31. Based on the retention time, primary mass number, and secondary mass spectrum data, 87 blood components were identified (Table 1).
The extracted molecular ion peak [M + H]+ (623.3116) and fragment ions at m/z 580, 381, and 122 were consistent with the fragment ions of tetrandrine in vitro(Fig. 6). The compound was identified based on the retention time of reference of tetrandrine32.
The molecular ion peak [M + H]+ (609.2966) of fangchinoline was observed in the primary MS peak. Secondary MS data were obtained corresponding to the extraction of the molecular ion peaks [M + H]+ 566, 367, and 191 of fangchinoline. These data represent the characteristic mass spectrum cleavage law of glucuronic acid replacing triterpenoid acid (Fig. 7). The ingredients were identified by comparison with the reference fangchinoline33.
The primary secondary fragment peak of [M + H]+ (342) was observed at m/z 192. Based on previous reports, the compound was identified as cyclanoline. In contrast, the secondary fragment peak of [M + H]+ (447, RT = 14.69 min)was noted at m/z 381, 297, and 255, and its cleavage was similar to that of puerarin34. According to the results of previous reports, the compound was identified as 3’-methoxypuerarin35. An analysis of the cleavage pathway in positive ion mode is shown in Fig. 8.
Secondary fragment peaks of [M + H]+ (255) were observed at m/z 237, 145, and 137. According to the literature, this compound was identified as Daidzein36. The secondary fragment peaks of [M + H]+ (463) were observed at m/z 381, 325, 279, 179, and 151, and the compound was identified as lactiflorin37. The secondary fragment peaks of [M + H]+ (481) were observed at m/z 417, 255, 179, and 105,and the compound was identified as albiflorin38. Benzoylpaeoniflorin exhibited a strong molecular ion peak at [M + H]+ (585), and the fragment ions showed m/z 315, 255, and 87, aligning with previous reports39. Kaempferol exhibited a strong molecular ion peak at [M + H]+ (287.0541), with corresponding fragment ions at m/z 255 and 111. The amounts of the ingredients were confirmed as per a previous study40.
The secondary fragment peaks of [M + H]+ (137) were at m/z 121 and 91, and the compound was identified as 2’-hydroxyacetophenone, according to a previous report41. The secondary fragment peaks of [M + H]+ (181) were at m/z 162 and 109, and the compound was identified as caffeic acid by comparison with the reference42. Secondary fragment peaks of [M + H]+ (447, retention time = 9.16 min) were observed at m/z 429 and 327, and the compound was identified as calycosin-7-O-glucoside43. Secondary fragment peaks of [M + H]+ (301) were observed at m/z 264 and 172,and the compound was identified as methylnissolin33.
The main secondary fragment peaks of [M + H]+ (371) were observed at m/z 185, 109, and 95, and the compound was identified as riligustilide44. The main secondary fragment peak of [M + H]+ (315) was noted at m/z 299, and the compound was identified as nepetoidin B45. The main secondary fragment peaks of [M + H]+ (130) were observed at m/z 116 and 84, and the compound was identified as DL-pyroglutamic acid46. The main secondary fragment peak of [M + H]+ (301) was noted at m/z 285, and the compound was identified as 3’-hydroxymelanettin47. The secondary fragment peaks of [M + H]+ (285) were observed at m/z 270 and 137, and the compound was identified as xenognosin B48. The main secondary fragment peak of the [M + H]+ (273) was noted at m/z 137, and the compound was identified as naringenin49. The main secondary fragment peak of the [M + H]+ (317) was atm/z 163, and the compound was identified as violanone50. The secondary fragment peaks of [M + H]+ (331) were observed at m/z 267, 149, and 133,and the compound was identified as melilotocarpan C49. The secondary fragment peaks of [M + H]+ (285) were noted at m/z 255 and 149, and the compound was identified as stevein48. The main secondary fragment peak of [M + H]+ (237) was noted at m/z 81, and the compound was identified as cyperolone51. The secondary fragment peak of [M + H]+ (137) was recorded at m/z 109,83, and 71, and the compound was identified as alpha-phellandrene51. The secondary fragment peaks of [M + H]+ (219) were observed at m/z 121 and 93, and the compound was identified as alpha-cyperone51.
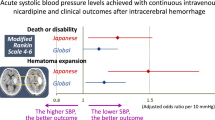
BP
The systolic BP (SBP) and diastolic BP (DBP) levels in the normal saline SHR group were significantly higher than those in the WKY control group at each time point pre-and post-administration (P < 0.05, Fig. 9). After 4weeks of administration, SBP and DBP levels (161.36 ± 5.12 mmHg vs. 128.71 ± 4.97 mmHg) in the irbesartan hydro- chlorothiazide capsule (IHC) group and JFBX-low (175.62 ± 5.78mmHg vs. 121.47 ± 5.82 mmHg) and high groups (171.25 ± 5.34 mmHg vs. 131.42 ± 5.28 mmHg) were all significantly decreased compared to those in the SHR untreated group (182.38 ± 6.65 mmHg vs. 142.50 ± 6.59 mmHg; P < 0.05). No significant differences were noted in SBP or DBP between the JFBX and IHC groups (P > 0.05).
Effects of JFBX on tail systolic blood pressure (SBP) and diastolic blood pressure (DBP) in normotensive Wistar–Kyoto (WKY) rats and spontaneously hypertensive rats (SHRs). The results are expressed as the mean ± SEM. N = 10. *p < 0.05 versus the WKY-Saline group; ∆p < 0.05 vs. the SHR-Saline group.
After 8weeks of treatment, the SBP and DBP levels in the IHC (150.37 ± 4.97 mmHg vs. 121.71 ± 4.86 mmHg), JFBX-low (168.23 ± 5.57 mmHg vs. 134.52 ± 5.29 mmHg), and JFBX-high (157.29 ± 5.15 mmHg vs. 124.82 ± 4.75 mmHg) groups were significantly lower than those in the SHR untreated group (191.35 ± 6.94 mmHg vs. 152.60 ± 6.95 mmHg; P < 0.05). No significant differences were noted in SBP or DBP between the JFBX and IHC groups (P > 0.05).
After 12weeks of administration, the SBP and DBP levels in the IHC (147.82 ± 5.02 mmHg vs. 110.35 ± 4.99 mmHg), JFBX-low (171.63 ± 5.93 mmHg vs. 138.92 ± 5.84 mmHg), and JFBX-high groups (157.99 ± 5.47 mmHg vs. 132.59 ± 5.30 mmHg) were significantly lower than those in the SHR untreated group (209.57 ± 7.05 mmHg vs. 153.60 ± 7.23 mmHg; P < 0.05). Compared with the IHC group, DBP levels were significantly different between the JFBX-low (SHR-3 L) and high (SHR-4 H) groups (P < 0.05); however, the SBP levels did not show significant differences (P > 0.05). The results showed that early intervention with both low- and high-doses of JFBX effectively reduced SBP and DBP levels in SHRs (Fig. 9).
JFBX alleviated oxidative stress-induced damage
Compared to the normal control group, superoxide dismutase (SOD) levels in the myocardium of the model group (SHRs) were reduced with an increase in malondialdehyde (MDA) levels, and the differences were statistically significant (P < 0.05; Fig. 10). Compared with the untreated group, SOD activity was significantly increased, and MDA content was significantly decreased after the administration of a high-dose of JFBX (P < 0.05). No significant changes were observed in the low-dose JFBX group (P > 0.05).
Effects of JFBX on different indices in normotensive Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHRs). Cardiac micro-CT images: A-WKY rats; B-SHRs; C-JFBX-Low group; D-JFBX-High group. Values are presented as the mean and standard deviation. The values were considered to be significantly different at p < 0.05; (*) vs. normal; (#) vs. model.
JFBX improved endothelial cell dysfunction
Endothelin (ET)-1 levels in the untreated group were significantly higher than those in the normal group, and NO levels were significantly lower than those in the normal group (P < 0.05; Fig. 10). The high- and low-dose JFBX groups showed significantly reduced ET-1 levels and increased NO levels (P < 0.05).
Effects of JFBX on levels of tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6 in rat myocardial tissue
Compared with the normal group, the levels of TNF-α, IL-1β, and IL-6 in the myocardial tissues of the untreated group (SHRs) were significantly increased (P < 0.05, Fig. 10). Compared with the untreated group, the levels of TNF-α, IL-1β, and IL-6 in the myocardial tissue of the JFBX-high-dose group were significantly decreased (P < 0.05). The levels of TNF-α and IL-6 of the myocardial tissue in the JFBX-low-dose group were significantly decreased (P < 0.05), in contrast to those of IL-1β, which did not show any significant differences (P > 0.05).
The micro-computed tomography (CT) images indicated that, compared with the WKY rats, the SHRs showed significant signs of left ventricular thickening after 12 weeks; however, left ventricular hypertrophy was not significant in the SHRs in the JFBX-high-dose group (Fig. 10). Compared to the WKY-saline group, white blood cells (WBC), red blood cells (RBC), and hemoglobin concentration (HGB) levels were significantly increased in the SHR-saline group (P < 0.05, Fig. 11–S1). Compared to the SHR-saline group, WBC and HGB levels were significantly decreased in both the JFBX-low and JFBX-high groups (P < 0.05). The RBC count was significantly decreased in the JFBX-High group (P < 0.05) but not in the JFBX-low group (P > 0.05). Morphological results showed that in the control group, the myocardial structure was intact, myocardial cells were normal, myocardial fibers were neatly arranged, and no cell swelling was observed (yellow arrows, Fig. 11). In the untreated group, abnormal hypertrophy of cardiomyocytes, disordered orientation of myocardial fibers, increased transverse diameter, porosity, edema, hyperplasia of connective tissue between myocardial fibers, and increased infiltration of inflammatory cells were observed. Compared with the untreated group, the high- and low-dose JFBX groups showed slightly larger and moderately arranged cardiomyocytes, reduced hypertrophy of cardiomyocytes, porosity, edema, hyperplasia of connective tissue, and inflammatory cell infiltration; the improvement was more significant in the high-dose group (P < 0.05, Fig. 11–S2).
Toxicology
After 12weeks of administration, the major organs of the high- and low-dose JFBX groups (n = 10), including the heart, liver, spleen, lung, bladder, kidney, adrenal gland, testis, and epididymis were observed, and no obvious lesions were recorded upon gross examination. Histopathological examinations of the heart, liver, spleen, lung, kidney, adrenal gland, testis, epididymis, and other major organs revealed no apparent abnormal changes (Fig. 12). Among them, two lung tissues, two liver tissues, and one kidney tissue that were observed under a microscope showed mild abnormalities: two cases (H2 and H5) demonstrated local lung tissue bleeding, whereas the terminal bronchus and bronchial cavity were normal, and the other lung tissues did not show exudation, edema, or other changes. The color of the liver tissue appeared slightly yellow to the naked eye (H3). Under a microscope, the liver lobular structure was still intact, liver cord structure was mildly disorganized, liver cells showed scattered necrosis in many places, and liver lobular proliferation, false lobular formation, liver cell fibrosis, and cancer were not observed. In the kidney tissue (H1), the proximal convoluted tubule was swollen, the distal convoluted tubule epithelium was slightly exfoliated, and no other changes, such as steatosis, hyalinosis, or necrosis, were recorded. Furthermore, the bristles were still intact, and no various types of tubes were observed in the collecting tubules.
Discussion
In this study, pharmacological results showed that early intervention with low- or high-doses of JFBX effectively attenuated both SBP and DBP levels in SHRs. JFBX reduced ET-1 levels, increased NO levels, and decreased the myocardial tissue levels of TNF-α, IL-1β, and IL-6. It also increased SOD activity and decreased MDA content. The toxicological results showed that JFBX did not exhibit particularly severe side effects when administered for 12 weeks.
The component array of TCM compounds is diverse, and the chemical components involved are highly complex, making it difficult to characterize all chemical components using a single technical method31. The rapid development of modern science and technology has improved the quality and pharmacology of Chinese medicinal compounds to a certain extent. TCM fingerprinting is an effective means to mitigate the limitations of single-quality components in evaluating compound preparations and, to a certain extent, it is an effective means to reflect the intrinsic quality of TCM compounds. In this study, an HPLC fingerprint quality control method was established to ensure the uniformity of the quality of JFBX preparations for clinical applications30. In the established control fingerprint, a total of 10 common peaks were labeled, and nine common peaks were identified by comparison with the reference products, namely, peak 1, gallic acid; peak 2, chlorogenic acid; peak 3,puerarin; peak 5, paeoniflorin; peak 6, ferulic acid; peak 7, tetrandrine; peak 8, tetrandrine; peak 9, ligustrone I; and peak 10 benzoyl paeoniflorin.
Then, UPLC-QTOF-MS combined with serum pharmaco-chemistry analyses were performed to explore the components of JFBX in blood, and 26 prototype compounds were detected, including alkaloids (tetrandrine, fangchinoline, and cyclanoline), iridoid glycosides (lactiflorin, albiflorin, and benzoyl-paeoniflorin), flavonoids (Kaempferol, Daidzein, and 3’-hydroxymelanettin), siterpenoids (alpha-phellandrene and alpha-cyperone), volatile components (riligustilide, xenognosin B, and 2’-hydroxyacetophenone), and organic phenols/acids (caffeic acid, DL-pyroglutamicacid). These components may attenuate EH in vivo, and our results provide a basis for further studies on the pharmacological mechanisms of action. Huang et al. found that tetrandrine significantly inhibited blood pressure in SHRs, which may be related to calcium channel blockade52. Tetrandrine exhibits a clear effect in a rat model of portal and pulmonary hypertension, and its antihypertensive mechanism may be related to direct cardiovascular expansion, improvement of microcirculation, inhibition of vascular collagen synthesis, and reduction of calmodulin activity53. Kakarla et al. found that kaempferol and caffeic acid have strong antioxidant activities54. Yu et al. reported that benzoylpaeoniflorin inhibits cardiomyocyte apoptosis in a rat model of acute myocardial infarction and is instrumental in protecting heart function via the nuclear factor E2-related factor 2/heme oxygenase 1 pathway55.
During oxidative stress, the body produces numerous harmful free radicals, such as reactive nitrogen species and reactive oxygen species (ROS)56. During left ventricular hypertrophy, excessive ROS are released, which directly leads to peroxidation damage of membrane lipids, ultimately resulting in MDA production. Therefore, the MDA level is an important indicator of the degree of oxidative stress in the body. SOD is a major cellular antioxidant that removes free radicals and prevents membrane lipid peroxidation. In a state of physiological equilibrium, SOD can be produced by myocardial microvascular endothelial cells, and only SOD can eliminate superoxide anions in ROS via a catalytic disproportionation reaction, thereby blocking their toxic effect. Therefore, increasing the level of SOD and decreasing the levels of MDA and NO could effectively prevent oxidative stress-induced myocardial ischemic injury. The results of this study showed that the SOD level of rats in the JFBX high-dose group was significantly increased and the MDA level was significantly decreased, suggesting that JFBX could reduce MDA and NO levels by increasing the SOD level in the serum of SHRs, further protecting against oxidative stress-induced cerebral ischemic injury. Irbesartan is a long-acting angiotensin receptor antagonist with promising anti-hypertensive properties57. In this study, irbesartan was used as a positive control drug. Irbesartan significantly reduced serum MDA and significantly increased SOD, which is consistent with literatures58,59.
NO and ET-1 are vasoactive substances secreted by endothelial cells, and under normal circumstances exist in dynamic balance: NO inhibits myocardial hypertrophy by dilating blood vessels, reducing cardiac load, reducing myocardial oxygen consumption, inhibiting vascular smooth muscle proliferation, and scavenging oxygen free radicals60. Additionally, ET-1 inhibits myocardial hypertrophy primarily by activating mitogen-activated protein kinase and Ca2+/calmodulin-de-pendent protein kinase-II(CaMKIL). CaMKIL signaling promotes cardiomyocyte hypertrophy and antagonizes endogenous pathways, whereas the physiological vasodilatory effector surface aggravates myocardial hypertrophy61. In the present study, ET-1 levels in the model group were significantly higher than those in the control group, whereas NO levels were lower than those in the control group, suggesting that JFBX can improve ventricular diastolic dysfunction and myocardial injury in rats with left ventricular hypertrophy by alleviating myocardial vascular dysfunction.
TNF-α-, IL-1β-, and IL-6-induced inflammation, promotes cardiomyocyte apoptosis and causes myocardial tissue necrosis62. The results of this study showed that after intervention with JFBX for 12 weeks, the levels of TNF-α, IL-1β, and IL-6 in the myocardial tissues of rats were significantly reduced. Further pathological studies showed that the cardiomyocytes of rats were slightly larger and moderately arranged, the degree of cardiomyocyte hypertrophy and porosity, edema, and hyperplasia of connective tissue were reduced, and the infiltration of inflammatory cells was reduced22. These results suggest that JFBX improved myocardial hypertrophy in hypertensive rats by inhibiting the expression of TNF-α, IL-1β, and IL-6.
Moreover, recently, the safety of S.Tetrandrae as a substitute for Aristolochiafangchi has been questioned, prompting research on the efficacy and toxicity of S.Tetrandrae63. S.Tetrandrae and its main component alkaloids (such as tetrandrine) exhibited apparent liver and kidney toxicity, with liver toxicity appearing early, alongside serious symptoms63. According to TCM theory, prescriptions include monarchs, ministers, assistants, and guides. A certain compatibility relationship exists between the herbs. With reasonable compatibility, drug bias can be corrected to enhance efficacy and reduce toxicity64.
Nevertheless, as JFBX contains S.Tetrandrae, toxicological studies are necessary. In this study, we observed lesions in organs, including the liver and kidneys, after 12 weeks of oral JFBX administration by upright optical microscope (Olympus Corporation, Japan, CX43) with image Analysis System11.0 software. Abnormalities in the two lung tissues, two liver tissues, and one kidney tissue were observed under a microscope in the high-dose group, including local lung tissue hemorrhage, slight disturbance in the hepatic cord structure, scattered necrosis of liver cells at several locations, swelling of the proximal convoluted tubules of the kidney, and slight exfoliation of the distal convoluted tubule epithelium. In the low-dose group, only one lung and one kidney showed mild abnormalities under the microscope. No significant abnormalities were observed in the liver, including local lung tissue bleeding, proximal convoluted tubule swelling, or slight distal convoluted tubule epithelial exfoliation. However, the toxicity and mechanism of action of S.Tetrandraein JFBX and relationship between its effects and the main alkaloids require further study.
Conclusion
The pharmacological results showed that early intervention with low- or high-doses of JFBX effectively attenuated both SBP and DBP levels in SHRs. JFBX reduced ET-1 levels, increased NO levels, decreased the myocardial tissue levels of TNF-α, IL-1β, and IL-6, increased SOD activity, and decreased MDA content. The toxicological results showed that JFBX did not cause particularly severe side effects when administered for12 weeks.
Materials and methods
All procedures were approved by the Experimental Animal Care and Use Committee of the Wuxi TCM Hospital (approval number: 2024A003-01) and conducted in accordance with the Guide for the Care and Use of Laboratory Animals (NIH publication No. 85 − 23, revised 1996).
Materials
Tetrandrine (Lot: A03HB190411), tetrandronoline (Lot: O18GB16436), gallic acid (Lot: J05GB153704), trans-caffeic acid (Lot: M27GB143417), chlorogenic acid (Lot: A22GB158496), puerarin (Lot: S02M9B54875), paeoniflorin (Lot: M28GB143089), Ligustrone I (Lot: M21HB178706), ferulic acid (Lot: G13S11L124423), and benzoyl paeoniflorin (Lot: O10HB197203) were purchased from Shanghai Yuanyet Biotechnology Co., Ltd. (China). Irbesartan hydrochlorothiazide tablets (lot: 211106) were obtained from Nanjing Zhengda Tianqing Co., Ltd. (China). SOD (Lot: 20240322012), MDA (Lot: 20240426121), ET-1 (Lot: 240117112), NO (Lot: 20240321114), TNF-α (Lot: 20240321028), IL-1β (Lot: 20240321036), and IL-6 kits (Lot: 20240321032) were all provided by Nanjing Jiancheng Institute of Biological Engineering. JBFX capsules (Lot: S01-20230411, S02-20230310, S03-20230206, S04-20221215, S05-20220914, S06-20220506, S07-20220304, S08-20211228, S09-20211125, and S10-20211024) were provided by the Preparation Room Department of Pharmacy in the Wuxi Hospital of Traditional Chinese Medicine, and the quality was determined using HPLC (Agilent 1200, USA).
Animal experiments
In total, forty 4-week-old male SHRs and ten 4-week-old male WKY rats, which were used as controls, were obtained from Weitong Lihua Experimental Animal Technology Co., LTD, Zhejiang Province (laboratory animal permit number: SCXK2024-0001). All rats were housed in a temperature-controlled room under a 12-h light/dark cycle with ad libitum access to standard chow and tap water. The 40 SHRs were divided in to untreated, JFBX-low, JFBX-high, and IHC groups.
After adaptive feeding for 1week, the rats were randomly assigned to five groups (n = 10 per group).
(1) Group 1: WKY rats without treatment (WKY group);
(2) Group 2: Untreated SHRs (SHR-M group);
(3) Group 3: JFBX-low group; rats received 0.8 g/kg of JFBX per day (SHR-3 L group);
(4) Group 4: JFBX-high group; rats received 1.6 g/kg of JFBX per day (SHR-4 H group);
(5) Group 5: Rats received 16 mg/kg of IHC (I: H = 12:1) per day (IHC group)65,66.
The rats in each treatment group were intragastrically administered each treatment for 12 weeks, and the SHR-M and WKY control groups were administered equal volumes of sterile distilled water.
Measurement of tail artery BP
BP was measured in conscious rats using the indirect tail-cuff method (BP-2000; VisitechSystems, Inc., Apex, NC, USA) after the rats were systematically trained at 4, 6, 8, 10, and 12 weeks of age. BP was measured after 12 weeks of intervention. Before measurement, the rats were maintained at 28 ℃ to detect the pulse of the tail artery and ensure its stabilization. To minimize stress-induced function, BP fitness measurements were performed daily for at least a week pre-experiment52.
Measurement of left ventricular hypertrophy by micro-CT
The rats were anesthetized using isoflurane and placed on a micro-CT scanner (Life Medical Technology Co., LTD, Kunshan, China). The scanning resolution, voltage, and current values were 8.5 μm, 60 kV, and 500 Å, respectively. Avatar Research Workplace software version 2.0.10.0 (Life Medical Technology Co., LTD, Kunshan, China) was used to reconstruct the region of interest and analyze the parameters.
Thereafter, the rats in all groups were anesthetized using 2% pentobarbital sodium (80 mg/kg, intraperitoneally). The blood was collected from the abdominal aorta67. Subsequently, all rats were euthanized by cervical dislocation under anesthesia. A comprehensive judgment of death was made by observing signs such as respiration, heartbeat, pupils, and nerve reflexes (no fluctuation of the chest, whitening of the eyelids, and no visual response)68. The organs were removed for pathological examination, and blood samples were collected for compositional analyses.
Hematological study
Blood samples were analyzed using an automatic Veterinary blood cell analyzer (Mindray, China). Hematological parameters including WBC, RBC, and HGB, were investigated69.
Preparation of serum samples
Blood samples were collected and centrifuged at 3500 rpm for 10 min to obtain serum samples. Overall, 200 µL of serum was obtained and 800 µL of iced acetonitrile was added, then the mixture was vortexed for 1 min and centrifuged at 12,000 rpm for 10 min with a centrifugation radius of 8.6 cm to obtain the supernatant for composition analysis. The supernatant was blown dry with nitrogen, and 100 µL of the initial mobile phase was added for re-dissolution70.
HPLC
The JFBX fingerprint was established using HPLC (Agilent 1200, USA) before administration to ensure consistency in the quality of JFBX samples used for clinical application and animal experiments71. The chromatographic analysis was performed on Kromasil-C18 column (4.6 × 250 mm, 5 μm; Sweden) with a detection wavelength of 280 nm and column temperature of 25℃. The flow rate was 1.0 mL/min, sample size was 5 µL, and mobile phase was acetonitrile 0.1% phosphate solution. The mobile phase comprised 0.1% phosphoric acid in water (A) and acetonitrile (B). The elution conditions were set as follows: 0–25 min, 5–15% B; 25–34 min, 15–18% B; 34–44 min, 18–20% B; 44–54 min, 20% B; 54–65 min, 20–35% B; 65–66 min, 35–47% B; 66–73 min, 47–80% B; 73–78 min, 80–95% B; 78–79 min, 80–95% B; and 79–87 min, 95% B. Data processing was performed using Chemstations Analysis Data System version C.01.10 (Agilent, USA).
UPLC-QTOF-MS/MS72
Chromatographic conditions
Waters Acquity UPLC HSS T3 column (100 mm×2.1 mm, 1.8 μm); flow rate 0.25 mL/min; column temperature 40 ℃; and sample size 10 µL. The mobile phase consisted of 0.1% formic acid in water (A) and acetonitrile (B). The elution conditions were set as follows: 0–8 min, 5–15% B; 8–11 min, 15–18% B; 11–15 min, 18–20% B; 15–18 min, 20% B; 18–21 min, 20–35% B; 21–23 min, 35–47% B; 23–25 min, 47–80% B; 25–28 min, 80–95% B; 25–28 min, 80–95% B; and 28–29 min, 95–5% B.
Conditions of mass spectrum analysis
The ion source was electrospray ionization (ESI), and the samples were scanned in the positive ion mode. The ionization voltage was 3500 V, capillary temperature was 320 ℃, heater temperature was 300 ℃, sheath gas pressure was 35 psi, and auxiliary gas pressure was 10 arb. The data collection range was 50–1500 m/z, and the ions of the components absorbed into the plasma were observed using ESI-QTOF-MS in both positive and negative modes, and the fragmentation behavior was determined via MS/MS by Masslynx software version 4.1 (Waters, USA). The components were subsequently identified based on accurate molecular weight and molecular formula information obtained from literature reviews.
Morphological observation
The heart, liver, spleen, lung, bladder, kidney, adrenal gland, testis, epididymis, brain, spinal cord, stomach, duodenum, and other tissue Sect. (5 μm) were harvested from the rats, fixed with 4% paraformaldehyde solution, embedded, sliced, and stained with Hematoxylin and eosin73.
(1) Fixed tissue dehydration: Fixed tissue blocks were placed in 70%, 80%, 90%, 95%, and 100% ethanol I and II for gradient dehydration for 1 h.
(2) For fixed tissue transparency, dehydrated fixed tissues were immersed in xylene I and II for 50 min.
(3) Wax dipping and embedding of the samples: The tissues were immersed in waxes I and II for 50 min, and then embedded in melted paraffin for 10 min.
(4) Paraffin block section: The tissues were sliced at a thickness of 5 μm, stuck to slides, baked at 60 ℃ for 1 h, and stored at 4 ℃.
(5) Dewaxing: Paraffin sections were immersed twice in xylene for 10 min and in 1/2 xylene + 1/2 pure ethanol for 10 min, 100% ethanol for 5 min, 95% ethanol for 5 min, 85% ethanol for 5 min, 70% ethanol for 5 min, and 50% ethanol for 5 min. Subsequently, the sections were washed with distilled water for 3 min.
(6) Hematoxylin staining: The sections were stained with hematoxylin for 10 min, rinsed with tap water until the color of the sections turned blue, and stained with 1% hydrochloric ethanol for color separation. The sections were again rinsed with tap water for 15 min until the sections turned blue and immersed in 50%, 70%, and 80% ethanol for 3–5 min.
(7) Eosin staining: The slices were incubated in 0.5% eosin-ethanol solution for 1–3 min and in 95% ethanol and anhydrous ethanol for 3–5 min for dehydration and differentiation, respectively.
(8) Transparency and fixation: The slices were incubated in xylene I and II for 3–5 min each to ensure transparency and sealed with neutral gum for microscopic observation. Three to five random fields (around 30–50 cells per field) were selected from per sections for observation under a light microscope (Olympus Corporation). Images were analyzed using the Image-Pro Plus software version 6.0 (Media Cybernetics Inc., MD, USA)74.
Determination of serum SOD and MDA levels
The levels of SOD and MDA in the rat serum were measured according to the manufacturer’s instructions (Nanjing Jiancheng Bioengineering Research Institute)75. In brief, the 96-well plate coated with SOD antibody were added to the samples, standard products, and horseradish peroxidase (HRP) labeled detection antibodies, which were warmed by the constant temperature incubator and thoroughly washed. Substrate 3,3’, 5,5’-tetramethylaniline was added for color development, absorbance (OD value) was determined at 450 nm wavelength by enzyme-labeled instrument, and SOD concentration was calculated. The serum to be tested was mixed with thiobarbituric acid solution and heated in a boiling water bath for 10–15 min. The solution was quickly cooled to room temperature, followed by centrifugation to remove the protein precipitate, and the clarified supernatant was obtained. The absorbance of the reaction product was determined at 532 nm wavelength, and then SOD concentration was calculated.
Determination of serum ET-1 and NO levels
ET-1 levels were determined by enzyme-linked immunosorbent assay (ELISA), and NO levels were measured using the microplate method (Nanjing Jiancheng Bioengineering Research Institute)60.
Determination of TNF-α, IL-1β and IL-6 levels in rat myocardial tissues
The levels of TNF-α, IL-1β, and IL-6 in the rat myocardial tissue were detected using ELISA. One frozen myocardium sample was collected from each group, washed with normal saline, and ground in an ice bath to prepare a 10% myocardial homogenate. The tissue homogenate was centrifuged at 10,000 rpm for 15 min, and the supernatant was obtained according to the instructions of the ELISA kit manufacturer (Nanjing Jiancheng Bioengineering Research Institute). The levels of TNF-α, IL-1β, and IL-6 in the rat myocardial tissue were determined using an enzyme-labeling instrument at 450 nm22.
Statistical analyses
Data are presented as the mean ± standard error of the mean. Statistical significance among multiple groups was evaluated by one-way analysis of variance with the Bonferroni post-hoc test using SPSS version 21.0 (IBM Corp., Armonk, NY, USA), Statistical significance was defined as a two-tailed P-value < 0.0522
Data availability
All data generated or analyzed during this study are included in this published article.
References
Ferdinand, K. C. & Nasser, S. A. Management of essential hypertension. Cardiol. Clin. 35, 231–246. https://doi.org/10.1016/j.ccl.2016.12.005 (2017).
Messerli, F. H., Williams, B. & Ritz, E. Essential hypertension. Lancet 370, 591–603. https://doi.org/10.1016/S0140-6736(07)61299-9 (2007).
Bruno, R. M., Masi, S., Taddei, M., Taddei, S. & Virdis, A. Essential hypertension and functional microvascular ageing. High. Blood Press. Cardiovasc. Prev. 25, 35–40. https://doi.org/10.1007/s40292-017-0245-9 (2018).
Forouzanfar, M. H. et al. Global Burden of Hypertension and systolic blood pressure of at least 110 to 115 mm hg, 1990–2015. JAMA 317, 165. https://doi.org/10.1001/jama.2016.19043 (2017).
Wang, Z. et al. Status of hypertension in China. Circulation 137, 2344–2356. https://doi.org/10.1161/CIRCULATIONAHA.117.032380 (2018).
Sudano, I., Roas, S. & Noll, G. Vascular abnormalities in essential hypertension. Curr. Pharm. Des. 17, 3039–3044. https://doi.org/10.2174/138161211798157766 (2011).
Unger, T. et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 75, 1334–1357. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026 (2020).
Liu, T. et al. Network Pharmacology Identifies the Mechanisms of Action of TaohongSiwu Decoction against Essential Hypertension. Med. Sci. Monit. 26, e920682. https://doi.org/10.12659/MSM.920682 (2020).
Xie, P. et al. The effect of Taohong Siwu decoction combined with antihypertensive medicine in the treatment of hypertension: Meta-analysis. Med. (Baltim). 101, e32133. https://doi.org/10.1097/MD.0000000000032133 (2022).
Li, J. et al. The mechanism of acupuncture in treating essential hypertension: a narrative review. Int. J. Hypertens. 2019, 1–10. https://doi.org/10.1155/2019/8676490 (2019).
Shu, L., Xinyu, W., Xiaosheng, W., Lihua, Z. & Shaoyu, G. Effects of JiangFangBaoXin tablets on left ventricular hypertrophy in hypertension. J. Nanjing Unverisity TCM. 14, 17–19 (1998).
Shu, L. et al. Effects of Jiangfangbaozhong herbal compound on left ventricular hypertrophy in renovascular hypertensive rats. Chin. J. Integr. Med. 19, 13–14 (1999).
Zhibin, Z., Shu, L., Ping, L., Chengxia, X. & Shaoyu, G. Regulation of JiangFangBaoXin Capsule to insulin resistance of essential hypertension patients. J. Liaoning Univ. TCM. 11, 78–79 (2009).
Shu, L. et al. Effect of JiangFangBaoXin Decotion on Renin Angiotension System in Renovascular Hypertensive rats. Chin. J. Expertimental Traditional Med. Formula. 5, 28–32 (1999).
Shu, L., Di, Y., Xiaosheng, W., Jinxing, G. & Hong, X. Effect of Jiangfang Baoxin Decoction on renin angiotensin system in renovascular hypertensive rats. Chin. J. Exp. Trad. Med. Formula 28–32 (1999).
Zhibin, Z., Shu, L. & Chungang, Z. Regulation of JiangFangBaoXin Capsule to vascular endothelial cell dysfunction in essential hypertension patients. Chin. J. Experimental Traditional Med. Formula. 17, 254–257 (2011).
Wei, W. et al. Total glucosides of paeony ameliorate myocardial injury in chronic heart failure rats by suppressing PARP-1. J. Cardiovasc. Transl Res. https://doi.org/10.1007/s12265-023-10440-3 (2023).
Liu, B. et al. Clinical safety of total glucosides of paeony adjuvant therapy for rheumatoid arthritis treatment: a systematic review and meta-analysis. BMC Complement. Med. Ther. 21 https://doi.org/10.1186/s12906-021-03252-y (2021).
Li, W. et al. Tetrandrine alleviates atherosclerosis via inhibition of STING-TBK1 pathway and inflammation in macrophages. Int. Immunopharmacol. 119, 110139. https://doi.org/10.1016/j.intimp.2023.110139 (2023).
Xiao, Y. et al. Quercetin and kaempferol increase the intestinal absorption of isorhamnetin coexisting in Elaeagnus rhamnoides (L.) A. Nelson (Elaeagnaceae) extracts via regulating multidrug resistance-associated protein 2. Phytomedicine 154–162. https://doi.org/10.1016/j.phymed.2018.09.028 (2019).
Tsai, C., Kuo, H., Hsu, C., Huang, L. & Tain, Y. Metformin reduces asymmetric dimethylarginine and prevents hypertension in spontaneously hypertensive rats. Transl Res. 164, 452–459. https://doi.org/10.1016/j.trsl.2014.07.005 (2014).
Diego, L. M. et al. Modulation of TNF -α, interleukin‐6, and interleukin‐10 by nebivolol–valsartan and nebivolol–lisinopril polytherapy in SHR rats. Pharmacol. Res. Perspect. 12 https://doi.org/10.1002/prp2.1189 (2024).
Friese, J. et al. Aconitum sp. alkaloids: the modulation of voltage-dependent Na+ channels, toxicity and antinociceptive properties. Eur. J. Pharmacol. 337, 165–174. https://doi.org/10.1016/s0014-2999(97)01268-5 (1997).
Tankeu, S., Vermaak, I., Chen, W., Sandasi, M. & Viljoen, A. Differentiation between two Fang Ji herbal medicines, Stephania Tetrandra and the nephrotoxic Aristolochia Fangchi, using hyperspectral imaging. Phytochemistry 122, 213–222. https://doi.org/10.1016/j.phytochem.2015.11.008 (2016).
Zhang, Y. et al. History of uses, phytochemistry, pharmacological activities, quality control and toxicity of the root of Stephania Tetrandra S. Moore: a review. J. Ethnopharmacol. 260, 112995. https://doi.org/10.1016/j.jep.2020.112995 (2020).
Bhagya, N. & Chandrashekar, K. R. Tetrandrine – a molecule of wide bioactivity. Phytochemistry 125, 5–13. https://doi.org/10.1016/j.phytochem.2016.02.005 (2016).
Han, M., Wang, Z., Li, Y., Song, Y. & Wang, Z. The application and sustainable development of coral in traditional medicine and its chemical composition, pharmacology, toxicology, and clinical research. Front. Pharmacol. 14, 1230608. https://doi.org/10.3389/fphar.2023.1230608 (2023).
Huang, L., Yu, Q., Peng, H. & Zhen, Z. Network pharmacology and molecular docking technology for exploring the effect and mechanism of Radix Bupleuri and Radix Paeoniae Alba herb-pair on anti-hepatitis: a review. Med. (Baltim). 102, e35443. https://doi.org/10.1097/MD.0000000000035443 (2023).
Xiao, Y. et al. Spectrum-effect relationship between HPLC fingerprint and antioxidant of San-Bai decoction extracts. J. Chromatogr. B. 1208, 123380. https://doi.org/10.1016/j.jchromb.2022.123380 (2022).
Xiao, D. et al. Study on HPLC fingerprint, network pharmacology, and antifungal activity of Rumex japonicus Houtt. J. AOAC Int. 105, 1741–1754. https://doi.org/10.1093/jaoacint/qsac079 (2022).
Xue, J. et al. An integrated strategy for characterization of chemical constituents in Stephania Tetrandra using LC–QTOF–MS/MS and the target isolation of two new biflavonoids. J. Pharm. Biomed. Anal. 226, 115247. https://doi.org/10.1016/j.jpba.2023.115247 (2023).
Li, S. et al. Preparation, characterization, Pharmacokinetics and tissue distribution of solid lipid nanoparticles loaded with Tetrandrine. AAPS PharmSciTech. 12, 1011–1018. https://doi.org/10.1208/s12249-011-9665-3 (2011).
Cui, W. et al. Rapid quantitative analysis of 19 bioactive components in fangji huangqi decoction based on UHPLC–MS/MS. J. Chromatogr. Sci. 61, 852–862. https://doi.org/10.1093/chromsci/bmac085 (2023).
Zhang, L. et al. Comparative pharmacokinetic analysis of six major bioactive constituents using UPLC-MS/MS in samples isolated from normal and diabetic nephropathy rats after oral administration of Gushen Jiedu capsule. J. Pharm. Biomed. Anal. 235, 115638. https://doi.org/10.1016/j.jpba.2023.115638 (2023).
Tao, Y., Chen, X., Jiang, Y. & Cai, B. A UPLC–MS/MS approach for simultaneous determination of eight flavonoids in rat plasma, and its application to pharmacokinetic studies of Fu-Zhu‐Jiang‐Tang tablet in rats. Biomed. Chromatogr. 31 https://doi.org/10.1002/bmc.3828 (2017).
Yao, D. et al. Integrated UHPLC–QE/MS, transcriptomics and network pharmacology reveal the mechanisms via which Liang-Yan‐Yi‐Zhen‐San promotes the browning of white adipose tissue. Biomed. Chromatogr. 37 https://doi.org/10.1002/bmc.5734 (2023).
Gao, X. et al. Exploration of chemical composition and absorption characteristics of Chaigui granules based on UHPLC-Q-orbitrap-MS/MS. J. Pharm. Biomed. Anal. 187, 113293. https://doi.org/10.1016/j.jpba.2020.113293 (2020).
Mei, Y. et al. Chemical profiling of Shen-Wu-Yi-Shen tablets using UPLC-Q-TOF-MS/MS and its quality evaluation based on UPLC-DAD combined with Multivariate Statistical Analysis. J. Chromatogr. Sci. https://doi.org/10.1093/chromsci/bmae001 (2024).
Seo, C. S. & Lee, M. Y. Simultaneous determination of fourteen marker compounds in the traditional herbal prescription, Geumgwesingihwan, using Ultra-performance Liquid Chromatography-Tandem Mass Spectrometry. Molecules 27 https://doi.org/10.3390/molecules27123890 (2022).
Ndhlala, A. R., Işık, M., Kavaz Yüksel, A. & Dikici, E. Phenolic content analysis of two species belonging to the Lamiaceae Family: antioxidant, anticholinergic, and Antibacterial activities. Molecules 29, 480. https://doi.org/10.3390/molecules29020480 (2024).
Xie, X. et al. Profiling and annotation of carbonyl compounds in Baijiu Daqu by chlorine isotope labeling-assisted ultrahigh-performance liquid chromatography-high resolution mass spectrometry. J. Chromatogr. A. 1703, 464110. https://doi.org/10.1016/j.chroma.2023.464110 (2023).
Bayer, J. & Högger, P. Development and validation of a LC–MS/MS method for the quantification of phenolic compounds in human saliva after intake of a procyanidin-rich pine bark extract. J. Pharm. Biomed. Anal. 239, 115914. https://doi.org/10.1016/j.jpba.2023.115914 (2024).
Wang, F. et al. Chemical characterisation and quantification of the major constituents in the Chinese herbal formula Jian-Pi‐Yi‐Shen pill by UPLC‐Q‐TOF‐MS/MS and HPLC‐QQQ‐MS/MS. Phytochem Anal. 31, 915–929. https://doi.org/10.1002/pca.2963 (2020).
Li, S. L. et al. Simultaneous analysis of seventeen chemical ingredients of Ligusticum Chuanxiong by on-line high performance liquid chromatography-diode array detector-mass spectrometry. Planta Med. 69, 445–451. https://doi.org/10.1055/s-2003-39709 (2003).
Kostic, O. et al. The phytoremediation potential and physiological adaptive response of Tamarix tetrandra Pall. Ex M. Bieb. During the restoration of Chronosequence fly Ash deposits. Plants (Basel) 11 https://doi.org/10.3390/plants11070855 (2022).
Chen, L. et al. Identification of metabolite biomarkers in Salmonella enteritidis-contaminated chickens using UHPLC-QTRAP-MS-based targeted metabolomics. Food Chemistry: X. 20, 100966. https://doi.org/10.1016/j.fochx.2023.100966 (2023).
Abdelaziz, S. et al. Phytochemical profile, antioxidant and cytotoxic potential of Parkinsonia aculeata L. growing in Saudi Arabia. Saudi Pharm. J. 28, 1129–1137. https://doi.org/10.1016/j.jsps.2020.08.001 (2020).
Chan, S. C., Chang, Y. S., Wang, J. P., Chen, S. C. & Kuo, S. C. Three new flavonoids and antiallergic, anti-inflammatory constituents from the heartwood of Dalbergia odorifera. Planta Med. 64, 153–158. https://doi.org/10.1055/s-2006-957394 (1998).
Dossou, S. et al. Comparative metabolomics analysis of different Perilla varieties provides insights into variation in seed metabolite profiles and antioxidant activities. Foods https://doi.org/10.3390/foods12234370 (2023).
Liu, R. et al. Simultaneous determination of 10 major flavonoids in Dalbergia odorifera by high performance liquid chromatography. J. Pharm. Biomed. Anal. 39, 469–476. https://doi.org/10.1016/j.jpba.2005.04.007 (2005).
Liu, P. et al. Simultaneous determination of bioactive components in essential oil of Xiang–Fu–Si–Wu Formula in Beagle dog plasma by UPLC–MS/MS and its application to pharmacokinetics. J. Chromatogr. B. 929, 63–69. https://doi.org/10.1016/j.jchromb.2013.04.022 (2013).
Huang, Y. et al. Tetrandrine, an alkaloid from S. tetrandra exhibits anti-hypertensive and sleep-enhancing effects in SHR via different mechanisms. Phytomedicine 23, 1821–1829. https://doi.org/10.1016/j.phymed.2016.10.021 (2016).
Iturriaga-Vásquez, P., Miquel, R., Ivorra, M. D., D’Ocon, M. P. & Cassels, B. K. Simplified tetrandrine congeners as possible antihypertensive agents with a dual mechanism of action. J. Nat. Prod. 66, 954–957. https://doi.org/10.1021/np030022 (2003).
Kakarla, L. et al. Free radical scavenging, alpha-glucosidase inhibitory and anti-inflammatory constituents from Indian sedges, Cyperus Scariosus R.Br and Cyperus rotundus L. Pharmacogn. Mag. 12, S488–S496. https://doi.org/10.4103/0973-1296.191467 (2016).
Li, Y. & Wang, W. Effects of Benzoyl paeoniflorin on Cardiac function in rats with myocardial infarction via promoting Nrf2/ho-1 pathway. Lab. Anim. Sci. 39, 44–48 (2022).
Pang, H., Han, B., Yu, T. & Peng, Z. The complex regulation of tanshinone IIA in rats with hypertension-induced left ventricular hypertrophy. PLoS ONE 9, e92216. https://doi.org/10.1371/journal.pone.0092216 (2014).
Hao, S., He, Q., Yuan, Y. & Mu, Q. The protective effects of Irbesartan in cognitive impairment in hypertension. Aging (Albany NY). 16, 5065–5076. https://doi.org/10.18632/aging.205589 (2024).
Al-kuraishy, H., Al-Gareeb, A. & Al-nami, M. Irbesartan attenuates gentamicin-induced nephrotoxicity in rats through modulation of oxidative stress and endogenous antioxidant capacity. Int. J. Prev. Med. 11, 16. https://doi.org/10.4103/ijpvm.IJPVM_567_18 (2020).
Zhao, X., Yang, D., Xu, W., Xu, W. & Guo, Z. Effect of Irbesartan on oxidative stress and serum inflammatory factors in renal tissues of type 2 Diabetic rats. J. Coll. Physicians Surg. Pak. 29, 422–425. https://doi.org/10.29271/jcpsp.2019.05.422 (2019).
Li, J. et al. Salidroside enhances NO bioavailability and modulates arginine metabolism to alleviate pulmonary arterial hypertension. Eur. J. Med. Res. https://doi.org/10.1186/s40001-024-02016-x (2024).
Wu, J., Nakashima, S., Nakamura, S. & Matsuda, H. Effects of Sanoshashinto on left ventricular hypertrophy and gut microbiota in spontaneously hypertensive rats. J. Nat. Med. 74, 482–486. https://doi.org/10.1007/s11418-020-01387-9 (2020).
Bednarski, T. K., Duda, M. K. & Dobrzyn, P. Alterations of lipid metabolism in the heart in spontaneously hypertensive rats precedes left ventricular hypertrophy and Cardiac Dysfunction. Cells 11, 3032. https://doi.org/10.3390/cells11193032 (2022).
Schütz, R. et al. Synthesis, biological evaluation and toxicity of novel tetrandrine analogues. Eur. J. Med. Chem. 207, 112810. https://doi.org/10.1016/j.ejmech.2020.112810 (2020).
Jiang, M. et al. An efficient approach addressing the chemical complexity of Jiawei Fangji Huangqi decoction by integrating ultra-high‐performance liquid chromatography/ion mobility‐quadrupole time‐of‐flight mass spectrometry and intelligent data processing workflows. J. Sep. Sci. 46 https://doi.org/10.1002/jssc.202300374 (2023).
Dudhipala, N., Ettireddy, S., Youssef, A. A. A. & Puchchakayala, G. Development and In vivo pharmacokinetic and pharmacodynamic evaluation of an oral innovative cyclodextrin complexed lipid nanoparticles of Irbesartan Formulation for enhanced bioavailability. Nanotheranostics 7, 117–127. https://doi.org/10.7150/ntno.78102 (2023).
Zhang, D., Huang, Q., Li, Y. & Wang, J. Incident Hyperuricemia in relation to antihypertensive therapy with the irbesartan/hydrochlorothiazide combination. Blood Press. Monit. 26, 413–418. https://doi.org/10.1097/MBP.0000000000000554 (2021).
Xiang, L. et al. Ethanol extract of Paridis rhizoma attenuates carrageenan-induced paw swelling in rats by inhibiting the production of inflammatory factors. BMC Complement. Med. Ther. 23, 437. https://doi.org/10.1186/s12906-023-04264-6 (2023).
Shi, Z., Xu, F., Xia, T., Bian, Z. & Li, S. Pharmacokinetics and anti-ulcerogenic effects of Zuojin gastric floating bio-adhesive pellets in rats with acetic acid-induced gastric ulcer. Phytomed. Plus 3, 100442. https://doi.org/10.1016/j.phyplu.2023.100442 (2023).
Cai, T. et al. Subacute dermal toxicity study of bensulfuron-methyl in Sprague-Dawley rats. Cutan. Ocul Toxicol. 41, 162–167. https://doi.org/10.1080/15569527.2022.2077750 (2022).
Liu, Q., Liu, L., Yuan, Y. & Xie, F. A validated UHPLC–MS/MS method to quantify eight antibiotics in quantitative dried blood spots in support of pharmacokinetic studies in neonates. Antibiotics 12, 199. https://doi.org/10.3390/antibiotics12020199 (2023).
Mykhailenko, O. et al. Bio-guided bioactive profiling and HPLC-DAD fingerprinting of Ukrainian saffron (Crocus sativus stigmas): moving from correlation toward causation. BMC Complement. Med. Ther. https://doi.org/10.1186/s12906-021-03374-3 (2021).
Liu, M., Su, X., Li, G., Zhao, G. & Zhao, L. Validated UPLC–MS/MS method for simultaneous determination of simvastatin, simvastatin hydroxy acid and berberine in rat plasma: application to the drug–drug pharmacokinetic interaction study of simvastatin combined with berberine after oral administration in rats. J. Chromatogr. B. 1006, 8–15. https://doi.org/10.1016/j.jchromb.2015.09.033 (2015).
Zeng, Z. et al. Myocardial hypertrophy is improved with berberine treatment via long non-coding RNA MIAT‐mediated autophagy. J. Pharm. Pharmacol. 71, 1822–1831. https://doi.org/10.1111/jphp.13170 (2019).
Yadav, G. et al. Utility of bone marrow examination in retinoblastoma and their correlation with hematological features. J. Med. Life. 16, 1245–1250. https://doi.org/10.25122/jml-2023-0156 (2023).
Abdelrahman, A. M., Al Suleimani, Y. M., Ashique, M., Manoj, P. & Ali, B. H. Effect of infliximab and tocilizumab on fructose-induced hyperinsulinemia and hypertension in rats. Biomed. Pharmacother. 105, 182–186. https://doi.org/10.1016/j.biopha.2018.05.118 (2018).
Acknowledgements
None.
Funding
This project was supported by the National Natural Science Foundation of China (Grant Number: 82274427), Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (Grant Number: HB2023076), Taihu Talent Program for senior medical team project of Wuxi City (Grant Number: Talent Office of Wuxi [p2021] No.9), Traditional Chinese Medicine Bureau of Jiangsu Province and National Clinical base of Traditional Chinese Medicine open subject (Grant Number: JD2023SZ20), and Natural Science Foundation of Nanjing University of Traditional Chinese Medicine (Grant Number: XZR2023092).
Author information
Authors and Affiliations
Contributions
Z. Q. S. and Q.W. conceptualized this studyand should be considered as co-first authors. Z.Q.S., F.J., Q.L., and Q.W. conducted experiments. Z.Q.S. and S.L. analyzed the data and contributed to the writing of the paper. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was conducted in compliance with the ARRIVE guidelines. The experimental protocols and treatments were approved by the Ethics Committee of Wuxi Hospital of Traditional Chinese Medicine. All methods were performed in accordance with the Jiangsu Province Laboratory Animal Care and Use Guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shi, Z., Wang, Q., Jia, F. et al. Pharmacological and toxicological effects of Jiangfangbaoxin and determination of its components in the blood of spontaneously hypertensive rats. Sci Rep 15, 4934 (2025). https://doi.org/10.1038/s41598-025-88009-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88009-0