Abstract
Sarcopenia has become a critical health concern in the global older population. However, limited studies have investigated the epidemiological characteristics and potential risk factors of sarcopenia in older individuals residing in rural coastal areas of China. This cross-sectional study involving sarcopenia screening was conducted in Ningbo City, including body composition measurements, and questionnaire surveys. Sarcopenia was diagnosed using the criteria outlined in the Asian Working Group for Sarcopenia 2019 Consensus. A total of 902 older adults aged ≥ 60 years (average age: 69.76 years) were included using a two-stage random sampling method from three villages in Ningbo. The prevalence of sarcopenia was 11.53%, with men (16.36%) exhibiting higher rates than women (7.93%). Multivariate logistic regression analysis identified age (odds ratio [OR]: 6.708, 95% confidence interval [CI]: 2.520–17.855), stroke (OR: 9.232, 95% CI: 1.917–44.447), and waist circumference (OR: 1.095, 95% CI: 1.030–1.165) as factors positively correlated with the occurrence of sarcopenia. Conversely, body mass index (OR: 0.347, 95% CI: 0.270–0.445) was negatively correlated with sarcopenia development. These findings underscore the need for specific health education, the collaborative prevention of comorbidities, and active screening for sarcopenia in the older population to reduce its disease burden.
Similar content being viewed by others
Introduction
Sarcopenia, an age-associated syndrome, is characterized by the progressive loss of skeletal muscle mass, muscle strength, and physical function in older adults1. Sarcopenia, recognized as a significant health concern, was officially incorporated into the International Classification of Diseases in 20162,3. The global prevalence of sarcopenia varies significantly due to the differences in age, region, and diagnostic criteria. The prevalence among community-dwelling individuals aged ≥ 50 years ranges from 1 to 29%4. Furthermore, approximately 10% of individuals over 60 years are affected by sarcopenia, with rates of 21% in men and 18% in women aged over 705,6. A study in China reported that 17.4% of community-dwelling older participants aged ≥ 65 years had sarcopenia7. Sarcopenia has been associated with various adverse health outcomes, including falls, fractures8, cardiovascular diseases9, cognitive impairments10, and an increased risk of mortality11,12. Additionally, it often coexists with other conditions, such as cardiovascular diseases, dementia, diabetes, and respiratory diseases, with respective prevalence rates of 31.4%, 26.4%, 31.1%, and 26.8%13. These associations highlight the critical need for timely screening for sarcopenia.
Several studies have investigated the risk factors associated with sarcopenia. A survey in the United Kingdom involving 396,283 individuals aged 38–73 years identified sex, age > 65 years, low body weight, and rheumatoid arthritis as the primary risk factors14. Similarly, a study in the United States involving 1,700 residents aged 55–98 years linked sarcopenia to older age, sedentary lifestyle, and smoking15. In China, research involving 1,407 urban older individuals aged ≥ 65 years identified age, male sex, and depression as risk factors for sarcopenia16. The majority of studies on sarcopenia in China have been conducted in urban areas, while limited studies have focused on rural areas17,18,19. Whether the significant factors associated with sarcopenia in urban groups are consistent with those in the rural elderly population is an issue of concern.
To address this gap, we conducted a screening initiative for sarcopenia among older individuals aged ≥ 60 years across three villages in Fenghua, a district in Ningbo City. The findings of this study would help identify the risk factors for sarcopenia in this rural region, providing a foundation for targeted health education and the development of regional health policies for this underserved population.
Methods
Study population
Fenghua, a district in Ningbo City, is located in the coastal area of Eastern Zhejiang Province, China. The district comprises eight subdistricts and four towns, with a registered population of 475,028 (Fig. 1). In 2020, the older population aged ≥ 60 years totaled 137,600, accounting for 28.67% of the total population. Moreover, the proportion of older individuals increases annually, emphasizing the growing burden of preventing and controlling sarcopenia in this demographic.
From August to December 2021, we conducted a survey in Qiucun Town, part of Fenghua District. Using a two-stage random sampling method, we selected three villages: Cao, Yingjia Peng, and Yang. Participants were eligible if they met the following criteria: (1) aged ≥ 60 years; (2) permanent residents of the three villages for at least 6 months per year; and (3) absence of specific conditions, such as Parkinson’s disease, muscle atrophy, speech or hearing impairments, and cognitive dysfunctions. We calculated the sample size using the formula N = [ (Z2) P (1-P) ] / d2 (where Z = 1.96, P = 0.10, and d = 0.02) and recruited 931 older participants to consider the possibility of loss to follow-up. All participants provided informed consent before the study began.
Data collection
Data were collected through face-to-face interviews. The process included administering a questionnaire and assessing a combination of grip strength, gait speed, and body composition. The questionnaire gathered demographic information, chronic disease history, smoking and alcohol consumption habits, and physical activity levels. Body composition measurements included height, weight, waist circumference and appendicular skeletal muscle mass (ASM).
Assessment of muscle mass
We employed a body composition analyzer (Model MC780, TANITA, Japan) to assess body weight and ASM. The ASM was calculated as the sum of the lean tissue mass of all four limbs using bioelectrical impedance analysis (BIA) at a precision of up to 0.1 kg. The ASM index (ASMI) was calculated as ASMI = ASM/height2 (kg/m2).
Assessment of grip strength
Grip strength was measured using a grip strength dynamometer (Xiangshan, China). Participants exerted the maximum grip strength with their dominant hand, with the highest value from three attempts recorded to the nearest 0.1 kg.
Assessment of gait speed
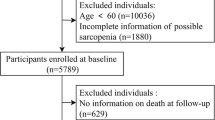
Gait speed was determined by measuring the time required for participants to walk a distance of 6 m using a stopwatch (Lining, China). In total, 902 older individuals were included in this study. Details of participant recruitment and selection are shown in Fig. 2.
Definition of sarcopenia
Sarcopenia was diagnosed following the criteria established by the Asian Working Group for Sarcopenia (AWGS) in 201920. A diagnosis required either low grip strength or low gait speed combined with low muscle mass. Low grip strength was defined as < 28 kg for men and < 18 kg for women; low gait speed was defined as < 1.0 m/s; and low muscle mass was defined as an ASMI < 7.0 kg/m2 for men and < 5.7 kg/m2 for women.
Physical exercise was defined as vigorous activities, such as brisk walking or jogging, for more than 150 min per week21. Smoking status was categorized into three groups: non-smoker, prior smoker, and current smoker. A prior smoker was defined as an individual who had quit smoking for at least 1 year, While a current smoker had smoked for 6 months or more cumulatively. Drinking status was similarly categorized: non-drinker, prior drinker, and current drinker. A current drinker was defined as someone who consumed alcohol at least once a week every month. While a prior drinker was an individual who abstained for at least 1 year. Participants’ medical history was assessed, including diagnoses of chronic diseases such as cancer, hypertension, diabetes, chronic respiratory diseases, and stroke.
Statistical analysis
Continuous variables following a normal distribution were expressed as mean ± standard deviation. Independent sample t-tests were used to compare normally distributed quantitative data between groups, while the Mann–Whitney U test was applied for non-normally distributed data. Categorical variables are expressed as counts and percentages, with comparisons between groups conducted using the chi-square test. Logistic regression models were employed to analyze potential influencing factors for sarcopenia after testing for collinearity among included variables. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. Statistical significance was set at a two-sided P < 0.05. All analyses were conducted using R software version 4.0.5 (https://www.r-project.org/)22.
Results
Basic characteristics of participants
This study included 902 older individuals aged ≥ 60 years with a mean age of 69.76 years. Among them, 385 were men (mean age: 70.81 years), and 517 were women (mean age: 68.98 years), yielding a male-to-female ratio of 1:1.34. Women had a higher average body mass index (BMI) and were more likely to engage in physical exercise than men (Table 1). In contrast, smoking and alcohol consumption rates were significantly higher among men. Chronic disease prevalence varied by sex, with diabetes being more prevalent in women and stroke more prevalent in men. Men exhibited significantly higher grip strength, gait speed, and ASMI values than women.
Prevalence of sarcopenia and its components by sex
The overall prevalence of sarcopenia among older adults in the rural coastal areas of Ningbo was 11.53% (104/902). Sarcopenia was more prevalent in men (16.36%) than in women (7.93%, P < 0.001). When comparing the components of sarcopenia according to sex, men had significantly higher rates of low grip strength and muscle mass than women (Table 2).
Analysis of factors influencing the prevalence of sarcopenia
Age was strongly associated with sarcopenia prevalence. Individuals aged ≥ 70 years were at a significantly higher risk of developing sarcopenia, with an adjusted odds ratio (aOR) of 6.708 (95% CI: 2.520–17.855) compared to those aged 60–64 years. Participants who had experienced a stroke had a significantly increased risk of sarcopenia (aOR: 9.232, 95% CI: 1.917–44.447). Waist circumference was also positively associated with sarcopenia, as indicated by an aOR of 1.095 (95% CI: 1.030–1.165). Conversely, BMI showed an inverse correlation with sarcopenia incidence (aOR: 0.347, 95% CI: 0.270–0.445). Detailed results of the logistic regression analysis are presented in Table 3.
Discussion
In 2023, China’s population aged ≥ 60 years reached 297.44 million, accounting for 21.1% of its total population, making it the country with the largest older population in the world23. As societies age, sarcopenia has garnered increasing research attention. This study found that the prevalence of sarcopenia in the rural coastal region of Ningbo City was 11.53% among individuals aged ≥ 60 years. Aging, stroke, waist circumference, and BMI were identified as significant factors influencing sarcopenia occurrence. To our knowledge, this is the first cross-sectional study to explore sarcopenia prevalence among older individuals in the rural coastal region of Ningbo, providing insights for targeted interventions and effective policymaking for vulnerable populations.
A recent meta-analysis in China reported a sarcopenia prevalence of 20.7% among individuals aged ≥ 60 years24, while the global prevalence based on the AWGS criteria was 18%25. In neighboring countries, the prevalence in the same age group was 13.1% in Korea26, 19% in Thailand27, and 32% in Vietnam28. Variations in prevalence across countries and regions are likely due to differences in diet, lifestyle, healthcare access, and economic conditions. Low protein intake could increase the sarcopenia risk29,30. However, residents of coastal regions of China, like Fenghua, generally have relatively adequate protein intake, especially from seafood31, potentially lowering their sarcopenia risk.
Urban-rural disparities in sarcopenia prevalence show higher rates in rural areas than in urban areas, both globally and in China32,33,34. Older adults in rural areas face greater challenges related to malnutrition, which may contribute to reduced muscle mass and strength34,35,36. Additionally, osteoarthritis is more prevalent among older adults in rural areas, significantly affecting their grip strength and ability to perform daily activities37,38,39. Limited health education and awareness about sarcopenia in rural areas result in missed opportunities for early intervention, leading to disease progression. Therefore, enhancing nutritional support and health education for older adults in rural areas is crucial to addressing this issue.
Consistent with previous studies40,41,42, we found that age is a significant risk factor for sarcopenia, particularly in individuals aged ≥ 70 years. Human muscle mass declines by 3–8% per decade after age 35, accelerating to 25% per decade after age 70 43. Muscle strength peaks between 25 and 35 years of age, then declines slightly until 49 years, followed by significant decreases of 12–14% per decade44. These progressive losses of muscle mass and strength can lead to various adverse health outcomes, including falls, increased healthcare costs, and higher mortality45,46. Special health education and early screening for sarcopenia in individuals aged > 70 years should be prioritized to mitigate these risks.
This study identified a negative correlation between BMI and sarcopenia development, consistent with findings from a study in Bengbu City47, Taiwan, and South Korea48,49. In older adults, BMI is associated with nutritional status, and malnutrition can lead to weight and skeletal muscle loss. Inadequate nutritional intake can lead to sarcopenia50,51. Although no causal relationship has been established, maintaining an appropriate BMI and avoiding malnutrition are critical for older adults. Future cohort studies are needed to explore the causal association between sarcopenia and BMI.
We also observed a significant positive correlation between stroke and sarcopenia. Previous studies reported that sarcopenia was more common in individuals with a history of stroke52,53. Stroke-related muscle atrophy and weakness might reduce physical activity, increasing sarcopenia risk54,55,56. Additionally, dysphagia in patients with stroke often leads to malnutrition. Meanwhile, malnutrition can further accelerate muscle mass loss and muscle weakness, worsening sarcopenia symptoms. Stroke and sarcopenia exacerbate each other, significantly affecting an individual’s quality of life. Considering our previous finding of a high stroke incidence in Fenghua District57, monitoring the occurrence of sarcopenia in patients with a history of stroke is essential. Joint health education for both diseases should be implemented, and cost-effective sarcopenia screening methods should be explored.
The relationship between waist circumference and sarcopenia was inconsistent with some previous studies. A study in Bengbu City found no association between waist circumference and sarcopenia47, whereas a study in Taiwan found a negative correlation49. Our findings align with studies in the United States58 and Japan59, which observed a positive correlation. Several factors may explain this discrepancy. Increased waist circumference suggests visceral fat accumulation risk, which may induce the secretion of inflammatory cytokines like TNF-α and IL-6 through the mechanism of glycolysis in skeletal muscle, contributing to sarcopenia development60. Besides, TNF-α could activate muscle atrophy gene expression via the NF-κB signaling pathway, further increasing sarcopenia risk61. Visceral fat is also closely associated with insulin resistance, impairing skeletal muscle’s ability to absorb and utilize insulin and negatively affecting protein synthesis and muscle quality62. It also further compromised skeletal muscle function by exacerbating inflammatory responses and oxidative stress63. Therefore, we recommend that older adults maintain healthy waist circumference levels to reduce the risk of sarcopenia.
Our study has several strengths. First, the study population comprised community-dwelling individuals aged ≥ 60 years from a rural coastal area, differing from most sarcopenia studies conducted in urban areas. This distinction helps address a knowledge gap and provides reference data for older adults in rural coastal areas of China. Second, we used the latest sarcopenia diagnostic criteria of AWGS 2019, which have been used in a few studies to date. Third, given the high prevalence of stroke in older individuals in the Fenghua District, our study explored the relationship between stroke and sarcopenia occurrence, offering a new perspective on comorbidity interventions. However, this study also has limitations. First, it was conducted at a single location with a limited sample size, potentially affecting the generalizability of the findings. Second, chronic disease prevalence was self-reported, possibly leading to underestimating actual disease prevalence. Third, excluding individuals with conditions such as Parkinson’s disease, muscle atrophy, speech and hearing impairments, and cognitive dysfunction may have influenced the generalizability of our findings. Fourth, some vital variables, such as diet, were not considered in our study, which might influence the comprehensive exploration of sarcopenia. Last, due to the cross-sectional design of this study, definitive causal relationships between sarcopenia and the identified factors could not be established.
Conclusion
The prevalence of sarcopenia in older individuals in rural coastal areas of Ningbo is relatively low. Waist circumference was positively correlated with sarcopenia occurrence, while BMI was negatively correlated. Individuals with a history of stroke should be particularly vigilant about developing sarcopenia. Comprehensive prevention programs, including targeted health education, collaborative management of comorbidities, and early detection policies in older adults, are necessary to reduce the disease burden of sarcopenia in this population.
Data availability
All data and materials pertinent to this study are detailed in this paper. The corresponding author (Dr. Wei Feng) is willing to provide all data upon reasonable request.
References
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing. 39, 412–423 (2010).
Anker, S. D., Morley, J. E. & von Haehling, S. Welcome to the Icd-10 code for sarcopenia. J. Cachexia Sarcopenia Muscle. 7, 512–514 (2016).
Cao, L. & Morley, J. E. Sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (Icd-10-Cm) code. J. Am. Med. Dir. Assoc. 17, 675–677 (2016).
Cruz-Jentoft, A. J. et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (Ewgsop and Iwgs). Age Ageing. 43, 748–759 (2014).
Kim, M. & Won, C. W. Sarcopenia in Korean community-dwelling adults aged 70 years and older: application of screening and diagnostic tools from the Asian Working Group for sarcopenia 2019 update. J. Am. Med. Dir. Assoc. 21, 752–758 (2020).
Shafiee, G. et al. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J. Diabetes Metab. Disord. 16, 21 (2017).
Ren, X. et al. Prevalence of sarcopenia in Chinese community-dwelling elderly: a systematic review. Bmc Public. Health. 22, 1702 (2022).
Yeung, S. et al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle. 10, 485–500 (2019).
Chin, S. O. et al. Sarcopenia is independently associated with cardiovascular disease in older Korean adults: the Korea National Health and Nutrition Examination Survey (Knhanes) from 2009. Plos One. 8, e60119 (2013).
Fhon, J. et al. Association between Sarcopenia, Falls, and cognitive impairment in older people: a systematic review with Meta-analysis. Int. J. Environ. Res. Public. Health 20, (2023).
Saaksjarvi, K. et al. Probable sarcopenia, obesity, and risk of all-cause mortality: a pooled analysis of 4,612 participants. Gerontology 69, 706–715 (2023).
Petermann-Rocha, F., Gray, S. R., Pell, J. P., Ho, F. K. & Celis-Morales, C. The Joint Association of Sarcopenia and Frailty with incidence and mortality health outcomes: a prospective study. Clin. Nutr. 40, 2427–2434 (2021).
Pacifico, J. et al. Prevalence of sarcopenia as a comorbid disease: a systematic review and meta-analysis. Exp. Gerontol. 131, 110801 (2020).
Petermann-Rocha, F. et al. Factors associated with sarcopenia: a cross-sectional analysis using Uk Biobank. Maturitas 133, 60–67 (2020).
Castillo, E. M. et al. Sarcopenia in elderly men and women: the Rancho Bernardo Study. Am. J. Prev. Med. 25, 226–231 (2003).
He, X. et al. Prevalence and factors influencing sarcopenia among community-dwelling older adults using the Asian Working Group for sarcopenia definition. Clin. Interv Aging. 17, 1707–1727 (2022).
Yang, J. et al. Prevalence of sarcopenic obesity among older adults in communities of China: a multicenter, cross-sectional study. Nutr. Clin. Pract. 39, 1375–1387 (2024).
Wang, B. et al. Prevalence and associated body composition factors of sarcopenia in community-dwelling older adults. Eur. J. Med. Res. 29, 598 (2024).
Qiu, W., Cai, A., Li, L. & Feng, Y. Trend in prevalence, associated risk factors, and longitudinal outcomes of sarcopenia in China: A National Cohort Study. J. Intern. Med. 296, 156–167 (2024).
Chen, L. K. et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21, 300–307 (2020).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462 (2020).
Team, R. C. A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2023).
Statistics, N. B. O. 2023 National Economic and Social Development Bulletin of the People’s Republic of China. https://www.stats.gov.cn/sj/zxfb/202402/t20240228_1947915.html (Accessed October spetember 2024) (2024).
Meng, S. et al. The prevalence of sarcopenia and risk factors in the older adult in China: a systematic review and meta-analysis. Front. Public. Health. 12, 1415398 (2024).
Petermann-Rocha, F. et al. Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle. 13, 86–99 (2022).
Choo, Y. J. & Chang, M. C. Prevalence of sarcopenia among the elderly in Korea: a meta-analysis. J. Prev. Med. Public. Health. 54, 96–102 (2021).
Lawongsa, K. & Tepakorn, J. Sarcopenia prevalence and risk factors among older adults in Bangkok, Thailand: a cross-sectional study. Cureus J. Med. Sci. 16, e63483 (2024).
Pham, L. T. et al. Community-based prevalence and associated factors of sarcopenia in the Vietnamese elderly. Sci. Rep. 14, 17 (2024).
Pang, B. et al. Prevalence and associated factors of sarcopenia in Singaporean adults-the Yishun Study. J. Am. Med. Dir. Assoc. 22, 881–885 (2021).
Lin, C. C., Shih, M. H., Chen, C. D. & Yeh, S. L. Effects of adequate dietary protein with whey protein, leucine, and vitamin D supplementation on sarcopenia in older adults: an open-label, parallel-group study. Clin. Nutr. 40, 1323–1329 (2021).
Jiao, Y. et al. Analysis of differentiated regional dietary patterns of adults aged 18–64 years in 15 provinces (autonomous regions, municipalities) in 2018. Wei Sheng Yan Jiu. 52, 11–19 (2023).
Li, X., Wang, R., Hou, Z. & Sun, Q. Urban-rural differences in the prevalence and associated factors of Sarcopenia: a systematic review and meta-analysis. Arch. Gerontol. Geriatr. 122, 105390 (2024).
Wu, X. et al. Sarcopenia prevalence and associated factors among older Chinese population: findings from the China health and retirement longitudinal study. Plos One. 16, e247617 (2021).
Gao, L. et al. Prevalence of sarcopenia and associated factors in Chinese community-dwelling elderly: comparison between rural and urban areas. J. Am. Med. Dir. Assoc. 16, 1001–1003 (2015).
Crichton, M. et al. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: associations with geographical region and sex. Age Ageing. 48, 38–48 (2019).
Koopman, J. J., van Bodegom, D., van Heemst, D. & Westendorp, R. G. Handgrip strength, ageing and mortality in rural Africa. Age Ageing. 44, 465–470 (2015).
Li, D., Li, S., Chen, Q. & Xie, X. The prevalence of symptomatic knee osteoarthritis in relation to Age, Sex, Area, Region, and body Mass Index in China: a systematic review and Meta-analysis. Front. Med. 7, 304 (2020).
Stoffer-Marx, M. A. et al. Functional consultation and exercises improve grip strength in osteoarthritis of the hand - a randomised controlled trial. Arthritis Res. Ther. 20, 253 (2018).
Boring, M. A. et al. Prevalence of arthritis and arthritis-attributable activity limitation by urban-rural county classification - United States, 2015. Mmwr-Morb Mortal. Wkly. Rep. 66, 527–532 (2017).
Chen, X., Hou, L., Zhang, Y. & Dong, B. Analysis of the prevalence of sarcopenia and its risk factors in the elderly in the Chengdu community. J. Nutr. Health Aging. 25, 600–605 (2021).
Wagenaar, C. A., Dekker, L. H. & Navis, G. J. Prevalence of sarcopenic obesity and sarcopenic overweight in the general population: the lifelines cohort study. Clin. Nutr. 40, 4422–4429 (2021).
Therakomen, V., Petchlorlian, A. & Lakananurak, N. Prevalence and risk factors of primary sarcopenia in community-dwelling outpatient elderly: a cross-sectional study. Sci. Rep. 10, 19551 (2020).
Mitchell, W. K. et al. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front. Physiol. 3, 260 (2012).
Doherty, T. J. The influence of aging and sex on skeletal muscle mass and strength. Curr. Opin. Clin. Nutr. Metab. Care. 4, 503–508 (2001).
Cruz-Jentoft, A. J. & Sayer, A. A. Sarcopenia Lancet 393, 2636–2646 (2019).
Beaudart, C., Zaaria, M., Pasleau, F., Reginster, J. Y. & Bruyere, O. Health outcomes of sarcopenia: a systematic review and meta-analysis. Plos One. 12, e169548 (2017).
Yao, J. et al. Prevalence of possible sarcopenia in community-dwelling older Chinese adults: a cross-sectional study. Bmj Open. 12, e67425 (2022).
Hwang, J. & Park, S. Gender-specific risk factors and prevalence for sarcopenia among community-dwelling young-old adults. Int. J. Environ. Res. Public. Health 19, (2022).
Kuo, Y. H. et al. Epidemiology of sarcopenia and factors associated with it among community-dwelling older adults in Taiwan. Am. J. Med. Sci. 357, 124–133 (2019).
Otsuka, Y. et al. Dietary intake of vitamin e and fats associated with sarcopenia in community-dwelling older Japanese people: a cross-sectional study from the fifth survey of the road study. Nutrients 13, (2021).
Karlsson, M., Becker, W., Michaelsson, K., Cederholm, T. & Sjogren, P. Associations between dietary patterns at age 71 and the prevalence of sarcopenia 16 years later. Clin. Nutr. 39, 1077–1084 (2020).
Su, Y., Yuki, M. & Otsuki, M. Prevalence of stroke-related sarcopenia: a systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 29, 105092 (2020).
Inoue, T. et al. Trajectories of the prevalence of sarcopenia in the pre- and post-stroke periods: a systematic review. Nutrients 15, (2022).
Hunnicutt, J. L. & Gregory, C. M. Skeletal muscle changes following stroke: a systematic review and comparison to healthy individuals. Top. Stroke Rehabil. 24, 463–471 (2017).
Arasaki, K., Igarashi, O., Machida, T., Hyodo, A. & Ushijima, R. Reduction in the Motor Unit Number Estimate (MUNE) after cerebral infarction. Suppl. Clin. Neurophysiol. 60, 189–195 (2009).
Harris, M. L., Polkey, M. I., Bath, P. M. & Moxham, J. Quadriceps muscle weakness following acute hemiplegic stroke. Clin. Rehabil. 15, 274–281 (2001).
Wei, F. E. N. G. Occurrence of stroke in one chronic demonstration area of Zhejiang Province in China: a retrospective study from 2009–2015. Iran. J. Public. Health. 49, 503–511 (2020).
Brown, J. C., Harhay, M. O. & Harhay, M. N. Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J. Cachexia Sarcopenia Muscle. 7, 290–298 (2016).
Sanada, K. et al. A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur. J. Appl. Physiol. 110, 57–65 (2010).
Bian, A. L. et al. A study on relationship between elderly sarcopenia and inflammatory factors Il-6 and tnf-alpha. Eur. J. Med. Res. 22, 25 (2017).
Remels, A. H., Gosker, H. R., Verhees, K. J., Langen, R. C. & Schols, A. M. Tnf-Alpha-Induced Nf-Kappab activation stimulates skeletal muscle glycolytic metabolism through activation of Hif-1Alpha. Endocrinology 156, 1770–1781 (2015).
Cleasby, M. E., Jamieson, P. M. & Atherton, P. J. Insulin resistance and sarcopenia: mechanistic links between common co-morbidities. J. Endocrinol. 229, R67–R81 (2016).
Savage, D. B., Petersen, K. F. & Shulman, G. I. Disordered lipid metabolism and the pathogenesis of insulin resistance. Physiol. Rev. 87, 507–520 (2007).
Acknowledgements
Thanks to Professor Guozhang Xu, Deputy Director of Ningbo University Medical Science Center and Dean of School of Public Health, for his guidance and help in this article.
Funding
This study was supported by the Social Development Scientific Research Project of Fenghua District (No. 202303203), the Traditional Chinese Medicine Science and Technology Plan Project of Zhejiang Province (No. 2023ZL669) and the Science and Technology Project of Yinzhou District (No. 2022AS033).
Author information
Authors and Affiliations
Contributions
Shuaishuai Huang, Wei Feng and Kui Liu designed and drafted the study. Shuaishuai Huang, Wei Feng, Kui Liu and Chen Wu revised the manuscript. Fujun Zhou and Yinfen Zhou performed data collection, curation and formal analysis. Chen Wu, Jiaqi Zhong, Hang Hong and Guobin Weng designed and implemented the methodology, formal analysis, software and interpretation of results. All authors approved the final version for submission.
Corresponding authors
Ethics declarations
Ethical statement and consent
This study was approved by the ethics committee of the Zhejiang Provincial Center for Disease Control and Prevention (No.2021-034-01). Prior to the survey, participants were provided with a standard informed consent form that outlined the objectives of the research. In accordance with the principles of the Declaration of Helsinki, all personal data obtained in this study were handled confidentially, and the research procedures followed ethical guidelines.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, S., Zhou, F., Zhou, Y. et al. Prevalence and influencing factors of sarcopenia among older adults in rural coastal areas of Ningbo City. Sci Rep 15, 6037 (2025). https://doi.org/10.1038/s41598-025-90017-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90017-z