Abstract
This study investigated the in vitro antimicrobial activity of cephamycins and novel β-lactam/β-lactamase inhibitor combinations, against extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Klebsiella pneumoniae isolates. ESBL-producing blood isolates were obtained between January and May 2023. The antibiotic susceptibility of the isolates was determined by broth microdilution method using standard (105 CFU/mL) and high (107 CFU/mL) inoculum sizes. Two randomly selected ESBL-producing isolates were subjected to time-kill assays for cephamycin. More than 80% of the isolates exhibited susceptibility to cefoxitin, cefmetazole, flomoxef, ceftazidime/avibactam, cefepime/enmetazobactam and imipenem/relebactam. Ceftolozane/tazobactam demonstrated in vitro efficacy against 62.1% of the ESBL-producing isolates. At the higher inoculum size, cefoxitin, cefmetazole, flomoxef, ceftolozane/tazobactam, ceftazidime/avibactam, cefepime/enmetazobactam, and imipenem/relebactam demonstrated in vitro efficacy against 48.3%, 75.9%, 70.0%, 0%, 82.8%, 100%, 89.7% of the ESBL-producing isolates. The frequencies of the inoculum effect with cefoxitin (3.7%), cefmetazole (14.8%), flomoxef (88.9%), ceftolozane/tazobactam (96.0%), ceftazidime/avibactam (34.5%), cefepime/enmetazobactam (10.3%), and imipenem/relebactam (10.3%) were identified. With standard inoculum, cephamycins reduced bacterial growth within 2–24 h. However, high inoculum resulted in regrowth after 12 h of cephamycin exposure. Cephamycins demonstrated high in vitro activity against ESBL-producing isolates at standard inoculum sizes. However, the in vitro time-kill experiments revealed that the efficacy of cephamycins is not fully maintained at high inoculum sizes.
Similar content being viewed by others
Introduction
The emergence and dissemination of extended-spectrum β-lactamase (ESBL)-producing Enterobacterales have led to increased reliance on carbapenems as a treatment option, raising concerns about the rising carbapenem consumption and its potential consequences1. Therefore, carbapenem-sparing antimicrobial options are needed not only to treat ESBL-producing isolates, but also to reduce the rapid emergence of carbapenem resistant pathogens1.
Cephamycins, a subgroup of second-generation cephalosporins, include cefotetan, cefoxitin, cefmetazole, and flomoxef. These antibiotics, along with temocillin and β-lactam/β-lactamase inhibitor combinations, are stable to hydrolysis by ESBLs1,2. The stability of cephamycins to ESBL hydrolysis is attributed to their unique molecular structure, which includes a 7-α-methoxy group. This structural feature provides steric hindrance, making it difficult for ESBLs to hydrolyse the β-lactam ring3. While the minimum inhibitory concentrations (MICs) of β -lactam/β-lactamase inhibitor combinations can increase as the bacterial inoculum size increases4, cephamycins demonstrate in vitro antibacterial efficacy even against high inoculum concentrations5. Understanding the impact of inoculum size on antibiotic efficacy is crucial for optimizing treatment strategies and predicting clinical outcomes. Moreover, the increasing prevalence of ESBL-producing organisms in both hospital and community settings has raised concerns about the limited treatment options available6. This situation has renewed interest in older antibiotics like cephamycins as potential alternatives to carbapenems. However, the clinical efficacy of cephamycins against ESBL-producing organisms remains a subject of debate, with some studies reporting favourable outcomes7 and others highlighting potential limitations8.
Therefore, we aimed to evaluate the in vitro activities of cephamycins versus comparator agents, including recently approved β-lactam/β-lactamase inhibitor combinations, against ESBL-producing isolates obtained from blood cultures. Additionally, we investigated the impact of high inoculum sizes on minimum inhibitory concentrations (MICs) to identify which antibiotics retain their effectiveness against ESBL-producing bacteria, regardless of the bacterial load.
Materials and methods
Bacterial isolates
Forty-eight E. coli and 68 K. pneumoniae clinical isolates were obtained from the Korean National Culture Collection for Pathogens (KNUH-NCCP). These isolates were originally collected from three Korean hospitals (Kyungpook National University Chilgok Hospital (Daegu), Kyungpook National University Hospital (Daegu), and Samsung Changwon Hospital (Changwon)) between January 2023 and May 2023. The thirty isolates exhibiting an ESBL phenotype by automated antimicrobial susceptibility testing (VITEK 2) were selected for further analysis. The phenotypic confirmatory test for ESBL production was performed by the disk diffusion method according to the recommendations of the Clinical and Laboratory Standards Institute (CLSI)9. Briefly, disks containing cefotaxime (30 μg) and ceftazidime (30 μg), with and without clavulanic acid (10 μg), were placed on Mueller–Hinton agar plates inoculated with the test organism. After overnight incubation at 35 °C, an increase of ≥ 5 mm in the zone diameter for either antimicrobial agent tested in combination with clavulanic acid versus its zone when tested alone confirmed the ESBL phenotype9. The Xpert Carba-R assay is a qualitative in vitro real-time PCR assay designed to detect five carbapenemase gene families: blaIMP, blaVIM, blaOXA-48, blaNDM, and blaKPC, according to the manufacturer’s instructions. The following ESBL-related genes were tested: TEM-type, CTX-M-1 group, CTX-M-9 group, and SHV-type, which were amplified by PCR from clinical isolates with primers as described in a previous study10. All PCR products were examined using 2% agarose gel electrophoresis.
Ethical approval
This study was conducted in agreement with the principles of the Declaration of Helsinki and was approved by the ethics committee of the Daegu Joint Institutional Review Board (DGIRB 2024-03-001). Informed consent was waived by DGIRB because this study utilized bacterial isolates from the KNUH-NCCP repository without any direct handling of human samples or patient data. All the experiments were performed in accordance with relevant guidelines and regulations.
Antimicrobial susceptibility testing
The MICs of ertapenem, imipenem, amikacin, ceftazidime, aztreonam, cefepime, cefotaxime, piperacillin/tazobactam, and trimethoprim/sulfamethoxazole were determined using automated antimicrobial susceptibility testing (VITEK 2), while the MIC of cefoxitin, cefmetazole, flomoxef, colistin, and the recently approved β-lactam/β-lactamase inhibitor combinations ceftazidime/avibactam, ceftolozane/tazobactam, cefepime/enmetazobactam and imipenem/relebactam were determined using the microdilution method at standard 105 CFU/mL or high 107 CFU/mL inoculum sizes. Susceptibility was interpreted according to the CLSI breakpoints9. There is no MIC breakpoint available for flomoxef from CLSI or EUCAST. Following current clinical practice in countries where flomoxef is available, we used the CLSI latamoxef (moxalactam) breakpoints9: susceptible at ≤ 8 mg/L, intermediate at 16 mg/L, and resistant at ≥ 32 mg/L. However, it should be noted that recent data suggests these breakpoints may not be adequate for high-burden severe infections such as bacteremia11. For cefepime/enmetazobactam, the FDA susceptibility breakpoint (≤ 8/8 mg/L) was applied. An inoculum effect was defined as an ≥ eightfold increase in the MIC at the higher inoculum size. E. coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 served as quality control strains.
In vitro time-kill studies
For the time-kill curves, two ESBL-producing E. coli isolates that were susceptible to cephamycins were chosen. The time-kill experiments for cefoxitin, cefmetazole, and flomoxef were conducted according to a previously described method with slight modifications12. Briefly, colonies from overnight cultures were suspended in LB broth and adjusted to a 0.5 McFarland standard (approximately 1.5 × 108 CFU/mL). The suspensions were then diluted to achieve final concentrations of 5 × 105 CFU/mL and 5 × 107 CFU/mL in a total volume of 10 mL, and these concentrations were confirmed by dilution plating. Cefoxitin, cefmetazole, and flomoxef were added to the prepared bacterial suspensions to final concentrations of 16 μg/mL, 4 μg/mL, and 1 μg/mL, respectively, each corresponding to 2 × MIC. Antibiotic-free cultures served as growth controls. All cultures were incubated at 35 °C with continuous shaking. Viable cell counts were determined at 0, 2, 4, 8, 12, and 24 h by plating serial dilutions on blood agar plates. Following overnight incubation at 35 °C, colony-forming units (CFU) were enumerated. The detection limit was established at 10 CFU/mL. Time-kill curves were generated by plotting log10 CFU/mL against time. Bactericidal activity was defined as a ≥ 3-log10 reduction in CFU/mL relative to the initial inoculum. All experiments were performed in duplicate. When discrepancies greater than 0.5 log10 CFU/mL were observed between paired results, the experiments were repeated in duplicate until consistent results (within 0.5 log10 CFU/mL variation) were obtained.
Results
Antimicrobial susceptibility of E. coli and K. pneumoniae blood isolates
Among the 116 blood isolates of E. coli and K. pneumoniae, more than 80% exhibited susceptibility to ertapenem (90.5%), imipenem (90.5%), amikacin (96.6%), gentamicin (83.6), piperacillin/tazobactam (80.2%), and cefoxitin (87.1%). All carbapenem resistance was found exclusively in K. pneumoniae isolates. Among these 11 carbapenem-resistant K. pneumoniae isolates, 10 were confirmed to produce KPC carbapenemase, while one isolate was a non-carbapenemase-producing strain that exhibited resistance through other mechanisms including ESBL production. All the 48 E. coli isolates were susceptible to ertapenem, imipenem, amikacin, and piperacillin/tazobactam, while 47 (97.9%) and 39 (81.3%) isolates were susceptible to cefoxitin and gentamicin, respectively. K. pneumoniae isolates demonstrated susceptibility to ertapenem (83.8%), imipenem (83.8%), amikacin (94.1%), gentamicin (85.3%), cefoxitin (79.4%), and piperacillin/tazobactam (66.2%). The susceptibility rates of E. coli isolates were 68.8%, 72.9%, 70.8%, 68.8%, 62.5%, and 66.7% for cefotaxime, ceftazidime, cefepime, aztreonam, amoxicillin/clavulanic acid, and trimethoprim/sulfamethoxazole, respectively. Among K. pneumoniae isolates, 61.8% (cefotaxime), 63.2% (ceftazidime), 72.1% (cefepime), 64.7% (aztreonam), 61.8% (amoxicillin/clavulanic acid), and 75.0% (trimethoprim/sulfamethoxazole) were susceptible to antibiotics (Supplement Table 1).
Among the isolates, 30 (15 E. coli and 15 K. pneumoniae) exhibited the ESBL-positive phenotype. One K. pneumoniae isolate demonstrated both the ESBL-positive phenotype and carbapenem resistance. This isolate was excluded from further analysis, resulting in a final study population of 29 ESBL-producing isolates.
In vitro activity of antimicrobial agents against ESBL-producing isolates
The susceptibility of the 29 ESBL-producing isolates to nineteen antimicrobial agents is presented in Table 1. More than 80% of the isolates exhibited susceptibility to ertapenem, imipenem, amikacin, cefoxitin, cefmetazole, flomoxef, ceftazidime/avibactam, cefepime/enmetazobactam and imipenem/relebactam. Ceftolozane/tazobactam demonstrated in vitro efficacy against 62.1% (18/29) of the ESBL-producing isolates. Interestingly, E. coli isolates showed a higher susceptibility rate of 93.3% (14/15) compared to K. pneumoniae isolates, which had a lower susceptibility rate of 28.6% (4/14).
Antimicrobial susceptibility of ESBL-producing isolates to cephamycins and new β-lactam/β-lactamase inhibitor combinations with different inoculum sizes
Tables 2 and 3 shows the antimicrobial susceptibility of ESBL blood isolates to three cephamycins and three new β-lactam/β-lactamase inhibitor combinations with standard (105 CFU/mL) or high (107 CFU/mL) inoculum size. The most ESBLs belonged to the CTX-M-1 group. At the higher inoculum size, cefoxitin, cefmetazole, flomoxef, ceftolozane/tazobactam, ceftazidime/avibactam, cefepime/enmetazobactam, and imipenem/relebactam demonstrated in vitro efficacy against 48.3% (n = 14), 75.9% (n = 22), 70.0% (n = 20), 0% (n = 0), 82.8% (n = 24), 100% (n = 29), 89.7% (n = 26) of the ESBL-producing isolates. The frequencies of the inoculum effect with cefoxitin (3.7%, 1/27), cefmetazole (14.8%, 4/27), flomoxef (88.9%, 24/27), ceftolozane/tazobactam (96.0%, 24/25), ceftazidime/avibactam (34.5%, 10/29), cefepime/enmetazobactam (10.3%, 3/29), and imipenem/relebactam (10.3%, 3/29) were identified.
Killing effects of cefoxitin, cefmetazole, and flomoxef on ESBL blood isolates
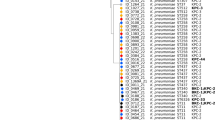
For the time-kill curves, two ESBL-producing E. coli isolates that were susceptible to cephamycins were chosen. The curves were generated using standard (5 × 105 CFU/mL) and high (5 × 107 CFU/mL) inocula. Figure 1 depicts the impact of cephamycins at concentrations corresponding to 2 × MIC. When the standard inoculum was used, cephamycins reduced bacterial growth within 2–24 h. However, one isolate (ECO-2) exhibited regrowth at 24 h under cefoxitin treatment (Fig. 1A). In contrast, when high inocula was employed, both isolates demonstrated regrowth after 12 h of exposure to cephamycins (Fig. 1B, 1D).
Time-kill curves of two cephamycin-susceptible ESBL-producing E. coli exposed to cefoxitin, cefmetazole, and flomoxef. (A) ECO-2, inoculum 5 × 105 CFU/mL; (B) ECO-2, inoculum 5 × 107 CFU/mL; (C) ECO-8, inoculum 5 × 105 CFU/mL; (B) ECO-8, inoculum 5 × 107 CFU/mL. The lower limit of detection for this assay was 10 CFU/mL.
Discussion
Our study revealed that cephamycins exhibited high susceptibility rates against ESBL-producing E. coli and K. pneumoniae clinical isolates (cefoxitin 82.8%, cefmetazole 93.1%, flomoxef 89.7%), with their efficacy maintained to a certain extent at high inoculum sizes. The study further showed that cefmetazole and flomoxef maintained high activity (75.9% and 70.0% susceptibility, respectively) even at high inoculum, while cefoxitin’s efficacy decreased more substantially (from 80.0 to 48.3%). Among the β-lactam/β-lactamase inhibitor combinations, ceftazidime/avibactam, cefepime/enmetazobactam, and imipenem/relebactam showed the most robust activity across both inoculum sizes, maintaining over 80% susceptibility even at high inoculum. Ceftolozane/tazobactam, however, showed a dramatic loss of efficacy at high inoculum. These findings suggest that cephamycins can retain their efficacy against ESBL-producing strains even at high inoculum sizes. However, the in vitro time-kill experiments revealed that bacterial regrowth was observed after 12 h of cephamycin exposure at high inoculum size. This indicates that the efficacy of cephamycins is not fully maintained at high inoculum sizes.
A previous study of 102 MDR K. pneumoniae isolates revealed a high prevalence (> 90%) of resistance to most β-lactam antibiotics, with carbapenems and cephamycins being notable exceptions, as the isolates remained susceptible to these agents13. In that investigation, cephamycins including cefoxitin and cefotetan showed better efficacy (40.2% and 68.6%, respectively) compared to carbapenems (23.5 to 34.3%) against K. pneumoniae isolates13. Our findings indicated that over 80% of ESBL-producing E. coli and K. pneumoniae isolates were susceptible to cephamycins (cefoxitin (82.8%), cefmetazole (93.1%), and flomoxef (89.7%)). Flomoxef had a lower MIC50 value (0.5 µg/mL) compared to cefoxitin (8 µg/mL) and cefmetazole (2 µg/mL). In addition, flomoxef maintained its activity against 92.8% of the isolates, even with a high inoculum size, despite showing an inoculum effect of 88.9%. These results are consistent with studies conducted in China, Japan, and Korea, which demonstrated the potent activity of flomoxef against ESBL-producing isolates14,15,16. Additionally, flomoxef exhibited excellent activity against ESBL-producing bacteria, including an isolate with an MIC eight times the MIC90 value17.
Ceftazidime-avibactam, cefepime/enmetazobactam and imipenem-relebactam also exhibited potent activity inhibiting 100% of ESBL-isolates at the standard inoculum, supporting their potential to preserve carbapenem efficacy. However, inoculum effects abrogating susceptibility were noteworthy for ceftolozane/tazobactam against most isolates, especially K. pneumoniae with SHV-type enzymes. This result is consistent with that ceftolozane/tazobactam inhibits 92.9% of the isolates harbouring CTX-M group but exhibited limited activity against isolates carrying SHV group (61.1%)18. This contrasts with the superior efficacy of cephamycins like flomoxef, which maintained activity against 86.7% isolates even at high inoculum despite exhibiting an inoculum effect in 88.9%. These findings suggest cephamycins could be advantageous over ceftolozane/tazobactam for treating high burden ESBL infections not amenable to carbapenem therapy. On the other hand, ceftazidime/avibactam, cefepime/enmetazobactam or imipenem/relebactam may be an option for the treatment of infections caused by ESBL-producing organisms but should be used judiciously to preserve its activity against carbapenem-resistant organisms.
Notwithstanding the efficacy if cephamycin against ESBL-producing organisms demonstrated in this paper, cephamycin has several limitations to use in the clinical setting. Currently, there are no established MIC breakpoints for flomoxef. Lee et al. observed comparable mortality rates between flomoxef and carbapenems when the flomoxef MIC was ≤ 1 mg/L, but flomoxef performed worse than carbapenem at MICs of 4–8 mg/L8. In our study, when considering a susceptibility threshold of 1 mg/L, the percentage of isolates susceptible to flomoxef dropped from 86.7 to 83.3%. Furthermore, a previous study discovered that cefmetazole was only effective against isolates with MICs ≤ 2 μg/mL, and the currently approved dosing might be suboptimal for isolates with higher MICs17. These observations emphasize the importance of establishing updated susceptibility breakpoint of cephamycins.
The findings of this study have several potential implications for clinical practice and antimicrobial stewardship. Our results suggest that cephamycins may serve as carbapenem-sparing alternatives for the treatment of certain ESBL-producing infections19,20. The demonstrated in vitro efficacy of cephamycins against ESBL-producing isolates supports their potential integration into antimicrobial stewardship programs, which could contribute to reducing carbapenem usage, thereby preserving the efficacy of these crucial antibiotics for infections caused by more resistant organisms21. Furthermore, the observed inoculum effect underscores the critical importance of considering bacterial load when selecting antimicrobial agents for severe infections. This insight may inform clinical decision-making processes, particularly in guiding the selection of appropriate empiric therapy for high-inoculum infections, such as those associated with osteomyelitis or endocarditis.
Conclusions
Our study suggested that cephamycins represent promising alternatives against ESBL-producing bacteria based on their in vitro activity. Cephamycins exhibited persistent in vitro activity against ESBL-producing isolates irrespective of the inoculum size. However, bacterial regrowth was observed when high inoculum size was employed, and caution should be required when using cephamycins in high-inoculum infections caused by ESBL-producing Enterobacterales. Further clinical studies are needed to confirm that the observed in vitro efficacy and inoculum independence of cephamycins translate into clinical effectiveness.
Data availability
The data of this study are available on request from the corresponding author.
References
Tamma, P. D. et al. Infectious Diseases Society of America 2022 guidance on the treatment of extended-spectrum β-lactamase producing enterobacterales (ESBL-E), carbapenem-resistant enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin. Infect. Dis. 75, 187–212 (2022).
Karaiskos, I. & Giamarellou, H. Carbapenem-sparing strategies for ESBL producers: When and how. Antibiotics (Basel) 9, 61 (2020).
Cun, W. Y., Keller, P. A. & Pyne, S. G. Synthesis of 7α-methoxy-7-(4-phenyl-1H-1,2,3-triazol-1-yl)acetamino-3’-arylthio-cephalosporic acid derivatives from 7-aminocephalosporic acid. Molecules 28, 7338 (2023).
Thomson, K. S. & Moland, E. S. Cefepime, piperacillin-tazobactam, and the inoculum effect in tests with extended-spectrum beta-lactamase producing Enterobacteriaceae. Antimicrob. Agents Chemother. 45, 3548–3554 (2001).
Soriano, F., Edwards, R. & Greenwood, D. Effect of inoculum size on bacteriolytic activity of cefminox and four other beta-lactam antibiotics against Escherichia coli. Antimicrob. Agents Chemother. 36, 223–226 (1992).
Pitout, J. D. & Laupland, K. B. Extended-spectrum β-lactamase-producing Enterobacteriaceae: An emerging public-health concern. Lancet Infect Dis. 8, 159–166 (2008).
Lee, C. H., Su, L. H., Tang, Y. F. & Liu, J. W. Treatment of ESBL-producing Klebsiella pneumoniae bacteraemia with carbapenems or flomoxef: A retrospective study and laboratory analysis of the isolates. J. Antimicrob. Chemother. 58, 1074–1077 (2006).
Lee, C. H. et al. Comparative effectiveness of flomoxef versus carbapenems in the treatment of bacteraemia due to extended-spectrum β-lactamase-producing Escherichia coli or Klebsiella pneumoniae with emphasis on minimum inhibitory concentration of flomoxef: A retrospective study. Int. J. Antimicrob. Agents 46, 610–615 (2015).
CLSI. CLSI supplement M100. In performance standards for antimicrobial susceptibility testing 33rd edn. (Clinical and Laboratory Standards Institute, 2023).
Kim, J., Lim, Y. M., Jeong, Y. S. & Seol, S. Y. Occurrence of CTX-M-3, CTX-M-15, CTX-M-14, and CTX-M-9 extended-spectrum beta-lactamases in Enterobacteriaceae clinical isolates in Korea. Antimicrob. Agents Chemother. 49, 1572–1575 (2005).
World Health Organization. Application for the Inclusion of Flomoxef Sodium on the WHO Model List of Essential Medicines (EML) and Model List of Essential Medicines for Children (EMLc). https://cdn.who.int/media/docs/default-source/essential-medicines/2023-eml-expert-committee/applications/flomoxef-sodium.pdf?sfvrsn=d23dd782_4 (2023).
Wi, Y. M. et al. Antimicrobial effects of β-lactams on imipenem-resistant ceftazidime-susceptible Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 61, e00054-e117 (2017).
Oliveira, R. et al. Exploring the antibiotic resistance profile of clinical Klebsiella pneumoniae Isolates in Portugal. Antibiotics (Basel) 11, 1613 (2022).
Miyazaki, M. et al. Change in the antimicrobial resistance profile of extended-spectrum β-lactamase-producing Escherichia coli. J. Clin. Med. Res. 11, 635–641 (2019).
Jung, Y., Lee, S. S., Song, W., Kim, H. S. & Uh, Y. In vitro activity of flomoxef against extended-spectrum β-lactamase–producing Escherichia coli and Klebsiella pneumoniae in Korea. Diagn. Microbiol. Infect. Dis. 94, 88–92 (2019).
Yang, Q. et al. In vitro activity of flomoxef and comparators against Escherichia coli, Klebsiella pneumoniae and Proteus mirabilis producing extended-spectrum β-lactamase in China. Int. J. Antimicrob. Agents 45, 485–490 (2015).
Yamashiro, H., Kasamatsu, Y., Anan, N., Takemura, M. & Yamano, Y. In vitro efficacy of humanized regimen of flomoxef against extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae. Antimicrob. Agents Chemother. 67, e0025823 (2023).
Castanheira, M., Doyle, T. B., Mendes, R. E. & Sader, H. S. Comparative activities of ceftazidime-avibactam and ceftolozane-tazobactam against Enterobacteriaceae isolates producing extended-spectrum β-lactamases from U.S. Hospitals. Antimicrob. Agents Chemother. 63, 10–1128 (2019).
Tamma, P. D. & Rodriguez-Bano, J. The use of noncarbapenem β-lactams for the treatment of extended-spectrum β-lactamase infections. Clin. Infect. Dis. 64, 972–980 (2017).
Rodríguez-Baño, J., Gutiérrez-Gutiérrez, B., Machuca, I. & Pascual, A. Treatment of infections caused by extended-spectrum-beta-lactamase-, AmpC-, and carbapenemase-producing Enterobacteriaceae. Clin. Microbiol. Rev. 31, e00079-e117 (2018).
Barlam, T. F. et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. 62, e51–e77 (2016).
Funding
This study was supported by a Korea National Institute of Health research project (2022-ER2503-02).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Wi YM, Choi JY, Lee DE, Jun SH, Kwon KT, Ko KS. The first draft of the manuscript was written by Wi YM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wi, Y.M., Choi, J.Y., Lee, D.E. et al. Antimicrobial activity of cephamycins and β-lactam/β-lactamase inhibitors against ESBL-producing Escherichia coli and Klebsiella pneumoniae under standard and high bacterial inocula. Sci Rep 15, 9785 (2025). https://doi.org/10.1038/s41598-025-90762-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90762-1