Abstract
Osteoarthritis (OA) is a prevalent musculoskeletal condition leading to functional limitations, especially among the elderly. Current treatments focus on pain relief and functional improvement, however there is a lack of approaches which slow disease progression. A promising approach focusses on reducing knee joint loading, as excessive loading contributes to knee OA progression. This study explores kinematic variations in the knee OA population, utilizing principal component analysis (PCA) to examine gait variations (primitives) in both healthy individuals and those with knee osteoarthritis (KOA) and their implications for knee joint loading. The KOA population exhibited 14 modes of variation representing 95% of the cumulative variance, compared to 20 in the healthy population, indicating lower variability with KOA. The relation between identified gait primitives and knee loading parameters, revealed complex relationships. Surprisingly, modes with the largest kinematic variations did not consistently correspond to the highest variations in knee loading parameters revealing degrees of freedom which may have a larger role in determining joint loading. Moreover, potential gait-retraining strategies for KOA, associating specific kinematic combinations with altered knee loading were identified. The results showed a good agreement with previously applied strategies. However, this study highlights the importance of analyzing whole-body kinematics for effective gait retraining, as opposed to focusing on one single joint variation. The study’s insights contribute to understanding the intricate interplay between gait pattern variations and knee joint loading changes in healthy and KOA populations, offering practical applications for guiding interventions and estimating loading parameters.
Similar content being viewed by others
Introduction
Osteoarthritis (OA), is a prevalent and complex musculoskeletal condition, accounting for a large societal and economical burden on both individuals and healthcare systems worldwide. It is considered a major cause of impaired functionality, especially among the aging population1,2,3 and is associated with joint pain and stiffness, leading to reduced mobility. While age is a risk factor, other mechanical factors such as obesity, joint misalignment, and overuse also play crucial roles in disease development and progression. With an aging population and lifestyle changes, the prevalence of knee OA is increasing, posing substantial socioeconomic challenges2,3. At present, conservative knee OA treatments, focusing on improving knee function and slowing down joint damage via pharmacological and/or physical therapy approaches are missing4. As such, effective interventions to slow down disease progression represent an unmet clinical need, that, if successful, offer evident societal and economic benefits2. Avoiding mechanical risk factors by e.g. reducing knee joint loading towards a healthier condition, has been suggested to be a promising strategy to slow down disease progression5,6,7. Healthy physiological knee joint loading is needed to preserve structural integrity for absorbing and distributing loads during motion and plays a crucial role in maintaining cartilage homeostasis. Alterations to either the magnitude and/or location of knee joint loading have been suggested to contribute to degeneration8,9. Moreover, factors like trauma, misalignment, or joint instability are recognized as contributing factors that can induce changes in knee movement. These changes can consequently lead to further alterations in knee joint loading associated with osteoarthritis10,11.
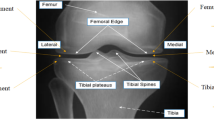
Gait kinematics in healthy and knee OA populations have extensively been studied12,13,14,15,16. Specifically, patients with KOA reported decreased walking speed and step length, reduced range of motion (ROM) in knee flexion (6–10°) but increased ROM in knee adduction (2–8°) compared to healthy individuals17,18. Furthermore, aberrant joint moments have been reported whereby the knee adduction moment (KAM) and ankle adduction moment were (up to 19%) higher compared to healthy individuals. Additionally, hip, knee and ankle flexion moments were reported to be reduced in the knee OA group17. In particular, KAM and knee flexion moment (KFM) exhibit a significant variation with medial knee OA severity7,8,13. These previously reported alterations in gait pattern have been suggested to likely induce altered knee joint loading13,19,20,21 in this population.
Direct measurement of knee joint loading in-vivo requires invasive measurement techniques via instrumented knee implants that measure the forces transmitted through implants22,23,24. However, this approach is costly, invasive, and not feasible in large cohorts. Thus, musculoskeletal (MSK) model-based simulations based on 3D motion capture (MoCap) data represent the state-of-the-art method to estimate in-vivo joint loading24,25. Several groups have reported good agreement between MSK model-based and instrumented knee implant joint loading parameters26,27, hence making it a feasible alternative to instrumented prosthesis26,28 with the advantage of being able to be applied to larger clinicial cohorts.
Using these MSK modeling-based workflows, literature specifically reports differences in loading distribution in the medial and lateral knee compartments in the KOA population. Knee joint loading is frequently increased compared to the healthy population (up to 22%), with elevated loading rates29 and an imbalanced load distribution that results in increased loading of the medial compartment. This, in turn, leads to excessive cartilage loading and potential damage27,28. Moreover, an association between elevated knee contact forces during walking and the three-year radiographic progression of knee osteoarthritis has been demonstrated, which underlines the importance of mitigating knee load by reducing the compressive knee contact forces30.
While the above-mentioned studies are useful in documenting differences in kinematics and in knee loading distribution between the two populations (healthy and KOA), they are based on small sample size (few gait cycles per individual) or cross-sectional data. Consequently, the sampled knee joint loading landscape does not account for the overall inter-subject variability in the gait pattern. Furthermore, no causal relation between gait variability and knee joint loading can be established. This is indeed relevant as gait pattern variability constitutes coordinated movements of different segments of the legs and trunk, which each by themselves but also in combination will affect knee joint loading. Additionally, gait pattern adaptations may serve as compensatory mechanisms for the purpose of avoiding knee pain, which in turn alters the loading and disease state.
Therefore, it is essential to improve the current cross-sectional data on knee joint loading by incorporating insights from natural variations in gait patterns observed in both healthy individuals and those with KOA. This can be achieved by integrating population-specific analysis of gait kinematics with MSK modeling to provide a more comprehensive understanding of the landscape of knee joint loading. Principal component analysis (PCA) has been previously used to enhance motion characterization at a population scale, identifying primary gait pattern variations31,32,33,34. Whereas kinematics was already characterized in healthy and KOA individuals34, an analysis of the impact of kinematics variations on knee joint loading in patients with knee OA is currently missing in literature. Furthermore, in combination with MSK modeling, PCA would allow to investigate how dominant variations in gait pattern affect knee joint loading. Investigating the gait patterns variations within populations and their impact on knee joint loading can potentially define movement primitives (i.e., the main joint kinematic variations observed in the population) that predispose to altered knee joint loading. As gait retraining strategies are a feasible and increasingly popular therapeutic approach in patients with KOA, this analysis may offer the conceptual basis for defining the gait characteristics to target in order to impact knee joint loading and hence impact pain and functional impairments35,36.
This study presents a population-specific analysis of joint kinematics and knee joint loading using PCA-based gait primitives of healthy and knee OA individuals to (1) identify primary kinematics variations in healthy and knee OA populations and determine if these variations are unique to each population and (2) investigate how these primary gait pattern variations contribute to changes in knee joint loading parameters. We hypothesize that, given the observed cross-sectional disparities between KOA and healthy gait patterns, the primary modes (principal components) of variation would differ between these two populations. It is further proposed that specific movement characteristics that reduce knee loading in a knee OA can be identified. These unique movement characteristics may serve as the foundation for future gait retraining strategies. The potential of these strategies in slowing down the progression of knee OA needs to be investigated in larger cohorts and confirmed with measured biomechanical data.
Results
Gait pattern variations
We identified the gait primitives underlying the gait characteristics of KOA and healthy individuals. To this end, the modes (principal components) that represent 95% of the observed cumulative variance in each population were separately considered for further analysis. Twenty modes were required for the healthy population, but only 14 modes for knee OA population, potentially indicative of reduced gait variability in the knee OA population (Fig. 1 and Tab. S1). Based on the selected modes, we synthesized kinematics during an entire gait cycle for each of the considered 14 degrees of freedom (i.e., a gait pattern representative of each mode). This allows us to identify specific kinematic variations compared to the mean gait pattern, which are representative of the specific mode. Figures 2 and 3 show examples of two different synthesized gait patterns from a single mode, in this case, mode 1.
Joint kinematic variations of the synthesized gait pattern described by Mode 1 (22.96% of explained variance) with ± 1 standard deviation from the mean gait pattern with positive (red), and negative (blue) standard deviation for healthy population dataset—ipsilateral leg. Solid black line shows the mean of the dataset and the grey regions shows the standard deviation of the input dataset (2553 gait cycles), and grey dashed line defines the stance phase. Medial and lateral knee contact force (KCF) (bottom panel) assessed based on mean (black) and Mode 1 ± 1 standard deviation (red, blue respectively) kinematic patterns. Mean and standard deviation of measured knee contact forces in healthy population (grey solid line and area).
Joint kinematic variations of the synthesized gait pattern described by Mode 1 (29.67% of explained variance) with ± 1 standard deviation from the mean gait pattern with positive (red), and negative (blue) standard deviation for knee OA population dataset—affected leg. Solid black line shows the mean of the kinematic dataset, the grey regions show the standard deviation of the input dataset (1754 gait cycles), and grey dashed line defines the stance phase. Medial and lateral knee contact force (KCF) (bottom panel) assessed based on mean (black) and Mode 1 ± 1 standard deviation (red, blue respectively) kinematic patterns. Mean and standard deviation of measured knee contact forces in knee OA population (grey solid line and area).
We subsequently summarized the contribution of each individual degree of freedom (DOF) to each mode’s variation (Fig. 4) by illustrating which DOFs are responsible for the first 50% of entire mode variation. Mode 1, accounting for 23% and 30% of the total variation in healthy and in knee OA individuals respectively, is associated with changes in sagittal plane angles in both populations, however there are contributions from individual joints. Specifically, it reveals that in both populations, the highest variation is observed in hip flexion/extension and pelvic anterior–posterior tilt movements. The third joint differs between the populations; it involves lumbar flexion/extension for the healthy population but knee flexion/extension for the knee OA population. Mode 2, accounting 19% and 17% of the total variation in healthy and in knee OA individuals respectively, is primarily associated with hip int/external rotation and knee flexion/extension in both populations. However, the relevant joint DOFs start to differ, introducing hip flexion/extension and knee int/external rotation for healthy and lumbar flex/extension, lumbar lateral bending and subtalar inversion/eversion for knee OA. Mode 3, accounting for 10% and 14% of the total variation in healthy and knee OA individuals respectively, introduces ankle dorsiflexion/plantarflexion in both populations. In the healthy population, knee internal/external rotation becomes more relevant, while in the knee OA population, the subtalar inversion/eversion. Further analysis of the different joints identified as most involved for each subsequent mode (4 to 20—less than 8% and 9% of the total variation in healthy and knee OA individuals respectively, see Fig. 1,) revealed that the overall kinematic variations are quite distinct with a different number of joints.
Comparison of joint variations contribution percentage (1–100%) of each mode over stance phase for healthy (white background) and knee OA (grey background) populations. Each bar color represents a different joint degree of freedom and its width denotes its contribution (%) to the kinematic variation of the mode. Only joints that contribute to the top 50% (when sorted from largest to smallest) are highlighted with text. Mode 15 to 20 for healthy population are illustrated in supplementary materials (Fig. S1).
Knee contact force variations
We investigated the effect of the observed gait primitives on estimated knee contact force defined by the modes from the healthy and KOA population. Specifically, each single unique gait pattern for each unique mode was used as input in a previously developed MSK modeling workflow37 to estimate the knee contact forces (Figs. 2 and 3 bottom right panel). As such, we can examine how the joint variations illustrated in Fig. 4 affect the estimated contact force peaks in the two populations (Figs. 5 and 6) with the intention of defining relevant changes in knee contact force peaks (increases/decreases). For simplicity, we described only the modes that resulted in functionally relevant changes in contact forces peaks (changes exceeding ± 10% BW, see Methods section). Modes with functionally relevant medial contact force peak changes are illustrated in Figs. 5 and 6. Complete modes with medial and lateral contact forces peaks changes are illustrated in supplementary materials (Fig. S2.1-20, S3.1-14).
Functionally relevant changes (changes exceeding ± 10% BW) as result of kinematic variations in medial (MED) compartment knee contact forces and relative changes in lateral (LAT) compartment (relevant changes are depicted with filled red and blue circle) expressed as a % difference in body weight (BW) compared to knee contact forces estimated using the mean healthy gait pattern (black dotted lines), at the top. Solid grey lines are the cut-off/threshold for functionally relevant knee contact force changes (see Material and Methods section “Methods”). Dotted grey lines define peak 1 (P1) and peak 2 (P2) of the gait cycle. Below (bottom) are the kinematics of the different joints contributing to the top 50% (see Fig. 4) of the observed variation for each specific mode depicted as ± 1 STD (red, blue respectively). Grey dashed line defines the stance phase.
Functionally relevant changes (changes exceeding ± 10% BW) as result of kinematic variations in medial (MED) compartment knee contact forces and relative changes in lateral (LAT) compartment (relevant changes are depicted with filled red and blue circle) expressed as a % difference in body weight (BW) compared to knee contact forces estimated using the mean knee OA gait pattern (black dotted lines), at the top. Solid grey lines are the cut-off/threshold for functionally relevant knee contact force changes (see Material and Methods section “Methods”). Dotted grey lines define peak 1 (P1) and peak 2 (P2) of the gait cycle. Below (bottom) are the kinematics of the different joints contributing to the top 50% (see Fig. 4) of the observed variation for each specific mode depicted as ± 1 STD (red, blue respectively). Grey dashed line defines the stance phase.
Healthy population
Gait primitives/kinematics affecting medial compartment loading
Overall, no functionally relevant increases (> 10% BW) in medial contact force were observed for either the 1st or 2nd peaks in any of the modes. However, a number of different modes showed a functionally relevant decrease (< 10% BW) in either or both the first and second peaks of knee joint loading. In the analysis, joints were categorized based on the number of associated modes. The ankle joint, specifically ankle plantarflexion (modes 3, 6, 7, 10, 13, 15, 18, 19), exhibited the most common involvement across healthy population modes. The hip joint, including hip flexion (modes 2, 13, 15), hip extension (modes 3, 10), hip internal rotation (modes 2, 3, 15), was observed in multiple modes, along with hip external rotation (mode 7), hip abduction (mode 15), and adduction (mode 19). The knee joint, including knee extension (modes 6, 10, 18), and knee external rotation (modes 6, 7, 15, 19), also showed functionally relevant variations across different modes. The lumbar joint, including lumbar internal rotation (modes 10, 13), lumbar external rotation (modes 6, 18), along with lumbar extension (mode 19) and ipsilateral bending (mode 7), showed functionally relevant variations. The pelvis degrees of freedom, specifically pelvic internal rotation (mode 13), external rotation (modes 6), and anterior tilt (mode 13), were present but less frequently across the relevant modes. Subtalar eversion was observed only in mode 19.
Knee OA population
Gait primitives/kinematics affecting medial compartment loading
In the knee OA population, different modes demonstrated functionally relevant increases (> 10% BW) in either or both the first and second peaks of medial knee contact forces. Notably, the hip joint exhibited the most common involvement across various modes, including hip extension (modes 1, 3, 7), internal rotation (modes 3, 5, 8), external rotation (mode 2, 10), flexion (modes 7), abduction (mode 7), and adduction (mode 7). The lumbar joint showed consistent involvement across various modes, including lumbar ipsilateral bending (modes 5, 8, 10), contralateral bending (mode 2, 6), extension (mode 2, 5), external rotation (8), and flexion (7). The knee joint, including extension (modes 1, 2, 3), internal rotation (mode 5), and flexion (6), also exhibited functionally relevant increases in knee joint loading across different modes. Similar to the healthy case, pelvic joint movements such as internal rotation (mode 10), downward obliquity (6), upward obliquity (mode 7), and posterior tilt (mode 2) were present but less frequently across the relevant modes. In contrast to the healthy population, where the ankle joint showed the most common involvement across various modes, the knee OA population exhibited relevant increases primarily during ankle plantarflexion (mode 3, 8, 10). Furthermore, subtalar eversion was observed in mode 3, 6 and 7.
Functionally relevant decreases (< 10% BW) in either or both the first and second peaks of medial knee contact forces were observed. The hip joint exhibited the highest involvement across various modes, including hip extension (modes 3, 7), internal rotation (modes 3, 5), external rotation (mode 10), and abduction (mode 7); however, hip flexion and adduction did not show any decrease in knee joint loading. The lumbar joint, including lumbar ipsi/contralateral bending (modes 5, 10) and flex/extension (modes 5 and 7), showed notable decrease in knee joint loading. Similarly to the increase case, hip and lumbar joints contributed to reducing loading when combined with other joints depending on their direction. The knee joint showed functionally relevant decreases across different modes, including knee extension (modes 1, 2, 3), and flexion (mode 6). Notably, in the case of knee internal rotation (mode 5), a similar reduction in loading was observed, highlighting a consistent trend across various modes. Examining the pelvic joint, combination of internal rotation (mode 10) and downward obliquity (mode 7) showed always relevant decreases in knee joint loading. The ankle joint demonstrated less involvement across various modes compared to the healthy population, including only plantarflexion in only two modes 3 and, 10). Additionally, subtalar eversion was observed in mode 3 and 7, respectively.
Joint combinations associated to relevant loading changes
The results showed relevant increases or decreases in medial contact force peaks in both healthy and knee OA populations, based on variations in kinematic patterns defined by the assessed modes (Figs. 5 and 6). However, upon focusing on functionally relevant changes in medial contact force peak alterations irrespective of population, interestingly, some recurrent kinematic pattern variations emerge, inducing consistently an increase or decrease in medial knee contact force peaks (Fig. 7).
Functionally relevant changes as result of kinematic variations in first (top) and second peak (bottom) medial compartment knee contact forces (KCF) expressed as a % difference in body weight (BW) compared to knee contact forces estimated using the mean gait pattern. Each colored bubble represents a different joint degree of freedom and its dimension denotes its contribution (%) to the kinematic variation of the mode with ± 1 STD (HS: healthy in blue label; KOA: knee OA in red label). The “+” and “−“ signs next to the mode numbers denote the direction of the STD. Only joints contributing to the top 50% are displayed as illustrated in Fig. 4.
It was observed that combinations of joint variations with lumbar internal rotation (light green) consistently leads to a decrease in both medial peaks, and combinations with lumbar external rotation, lead to an increase on the second peak. Combinations with knee flexion (light brown) consistently resulted in peak decreases; however, knee extension, which mainly leads to second peak increases, could lead to decrease if combined with lumbar internal rotation (light green) and/or ankle plantarflexion (bright blue). Combinations of knee internal rotation (dark green) consistently resulted in decreases in both peaks. In addition, subtalar eversion and inversion (purple) consistently leads to increases and decreases in both peaks, respectively. However, other kinematic variations, such as hip int/external rotation (dark grey) and lumbar ipsi/contralateral bending (light blue) (i.e. found to have a functionally relevant impact on medial knee loading changes in modes 2 and 3), influence changes in medial contact force peaks depending on the combination with other joints. These combinations can either increase or decrease medial contact forces peaks.
Discussion
This study aimed to identify population-specific kinematic variations, also so-called gait primitives, and potential whole-body movement strategies, as well as their effects on knee contact forces, in both healthy and knee osteoarthritis (OA) populations. The PCA was applied to a comprehensive set of gait kinematic data from both populations to synthesize new kinematic data, which are often challenging to discern in human cross-sectional experiments where multiple factors can change simultaneously. The new synthesized kinematic data were then integrated with a previously established musculoskeletal (MSK) modeling workflow to estimate knee contact forces37.
Unique gait primitives, i.e., gait kinematics variations, were identified for each population. The knee OA population analysis showed 14 modes of variation compared to the 20 of the healthy population to account for a cumulative 95% of population variation. A higher number of modes may indicate larger movement pattern variability within the studied population. Larger movement pattern variability should not be interpreted as a larger magnitude of kinematic variation (e.g., standard deviation of each degree of freedom), instead, as a higher number of variations or coordination strategies within a specific population. These vaqueryriations do not necessarily represent the magnitude of total variations within or between modes but instead the entire populations movement pattern variability. Mode 1, accounting for the highest total variability (23% for healthy and 30% for knee OA), was associated with variations in hip flexion/extension and pelvic anterior/posterior tilt for both populations. In addition, lumbar flexion/extension was observed in healthy, while knee flexion/extension in knee OA, highlighting differences between the two populations. Notably, despite the knee OA population, showing reduced range of motion (ROM) in the knee kinematics (approximately 6–10 degrees) compared to healthy population, (Figs. 2 and 3), similar to previous studies12,17,21,38, it showed higher knee flexion/extension variability in mode 1 (Fig. 3). This suggests a larger relevance for the knee OA population than the healthy one in the primary mode. An interesting observation is that, as we advance through the modes, mode 2, 3, 4 etc., an increasing number of degrees of freedom (DOFs) are required to account for a cumulative 50% variation for each mode (Fig. 4), varying distinctly between the two populations. This indicates that a greater number of degrees of freedom (DOFs) is necessary to characterize each mode. In contrast to earlier modes, where only a few DOFs dominated the modes (i.e., mode 1 and 2), the importance or contribution of each DOF is more similar and/or distributed across multiple DOFs. This greater number of DOFs is required to represent the complex behavior of the whole-body kinematics more accurately.
The second objective of this study was to investigate how the joint variations defined by the different modes in the two populations contributed to changes in knee joint loading parameters (i.e. contact forces peaks). Interestingly, modes presenting the largest variations in kinematics (i.e. hip flexion/extension, pelvic tilt in mode 1) did not translate into modes presenting the highest variation in knee joint loading parameters. In fact, mode 2 and mode 6 in knee OA with total explained variance of 17% and 5%, respectively, showed the highest increase for both medial contact force peaks (6% for peak 1 and 23% for peak 2). Mode 7, with total explained variance of 5%, showed the highest decrease for medial contact forces (17% for peak 1 and 3% for peak 2). Surprisingly, Mode 3, with total explained variance of 14%, revealed a maximal decrease in peak 1 (23%) but a maximal increase in peak 2 (29%) of medial contact forces.
Interestingly, opposite changes in kinematics (i.e. knee flexion or extension) did not consistently result in opposite changes in knee joint loading parameters. For instance, both combinations of knee flexion and ankle dorsiflexion (mode 6) and knee extension and ankle plantarflexion (mode 18) corresponded to relevant decreases in knee loading in healthy population. However, joint variation combinations with lumbar internal rotation or knee flexion or knee internal rotation resulted in relevant decreases, and combinations with knee extension or subtalar eversion consistently resulted in relevant increases in contact forces peak (i.e. mode 6 10, 18, Fig. 7 from the KOA group). However, other joint combinations with hip internal/external rotation and lumbar ipsi/contralateral bending resulted in either increased or decreased medial contact forces peaks dependent on the specific kinematics combination (i.e. mode 2, 5, Fig. 7). Likely, only a combination of a select number of kinematic changes (comprising the identified PC) results in the observed loading changes– rather than all those identified to change. Indeed, one joint variation may be identified as dominant in a specific PC. However, its direct result on the knee joint loading cannot be dissected. While it is possible to only vary one single joint at a time to evaluate its individual effect, it may be that this kinematic change is only influential when coupled with the other kinematic changes observed within the specific PC. Despite this, we believe the PCA based approach still holds a stronger potential to dissect the relationship between kinematics changes and changes in knee joint loading compared to single joint/DOF perturbations, by better aligning with the observed joint kinematics in patients with KOA.
Based on the population-specific analyses, specific movement characteristics could be identified that are already targeted in currently implemented gait-retraining strategies13,39. For example, previous studies have demonstrated that trunk leaning, particularly ipsilateral trunk leaning, can decrease medial knee contact force peaks10,20,40,41,42,43. Indeed, we observed relevant changes in contact force peaks associated with modes related to lumbar flexion/extension or ipsi/contralateral bending (i.e., mode 4 and 5 in knee OA), suggesting their potential utility in gait retraining. However it should be noted that in some cases, they could result in either increased or decreased medial contact force peaks dependent on the combination of whole-body kinematics (i.e. mode 5, Fig. 7). Also, other modes associated with combinations in ankle dorsi/plantarflexion, subtalar inversion/eversion and hip internal/external rotation (i.e. mode 3, Fig. 7) showed relevant contact force peak increases/decreases. This described joint combination can be associated with changes in foot progression angle, toe-in, toe-out strategies. These alterations have been previously associated with significant changes in knee moments (flexion and adduction moment) and contact force peaks21,44,45. Overall, our findings align with literature, providing consistency with reported gait pattern modification outcomes. This strengthens the potential practical application of our study’s findings in guiding and validating specific gait retraining interventions. However, additional relevant changes were observed in mode 15 for healthy population and in mode 11 for knee OA associated with variation in hip adduction/abduction during walking, which did impact the distribution of knee loading between the medial and lateral compartments. It has been shown that walking with increased hip abduction, which is moving the foot outward, can lead to higher knee loading on the medial compartment10. Potentially, based on our results, combinations involving either lumbar internal rotation (mode 10) or knee internal rotation (mode 5) and knee flexion (mode 3) may be further explored as strategies to decrease knee contact force peaks.
This study underscores identifies which joints are important in modifying medial contact forces, with a particular focus on the ankle, hip, and lumbar joints across various movement modes. In the healthy population, ankle plantarflexion was the most frequently observed movement, occurring in multiple modes. Additionally, all hip movements were prominently featured. In contrast, the knee OA population consistently showed involvement of the lumbar region across all modes, indicating its substantial impact on medial contact forces regardless of movement direction. Conversely, the ankle joint demonstrated less involvement compared to the healthy subjects, with plantarflexion and subtalar eversion present in fewer modes. These differences in joint engagement between the healthy and OA populations highlight how various movement models influence loading changes and emphasize the distinct contributions of specific joints to altered loading patterns in each population.
The population-specific kinematics variations could potentially serve as a foundation for defining the combined joint variations for healthy and knee OA populations that lead to either reduced or excessive knee loading conditions20,46. Importantly, this study results showed that knee loading changes are dependent on the whole-body kinematic variations. Consequently, it is crucial not to only consider gait pattern modifications in isolation at the single-joint level. Such isolated changes often result in kinematic alterations in other joints, which previous studies have not addressed41. Conversely, this study emphasizes that focusing on a single joint’s kinematic change may not represent an optimal approach for significantly influencing joint loading. Gait retraining should consider changes in multiple joints. Indeed, the described modes do not exclusively define changes in one degree of freedom; instead, they define combined kinematic changes in all joints, involving variations in pelvic, lumbar, hip, knee, and ankle joints21. Therefore, evaluating the impact of whole-body kinematics on knee joint loading with MSK modeling and expanding biomechanics measurement systems for use in more ecological contexts is crucial to evaluate the effect execution of the whole-body kinematic strategy needed to effectively reduce knee loading.
In our study, we limited the description of each mode to a restricted number of degrees of freedom (up to six), adopting a highly selective approach. A more comprehensive understanding of each mode would require a detailed comparison of whole-body kinematics, which is a limitation of our study. Furthermore, we analyzed pelvis residuals during inverse dynamics to assess the potential for unrealistic gait patterns resulting from PCA-derived kinematics. The analysis revealed elevated residual forces and normal residual moments, indicating that pelvis residual forces can significantly affect the observed contact forces (see Tab. S2). This discrepancy can likely be attributed to errors in estimating ground reaction forces and the center of pressure. The manner in which these parameters were estimated was consistent across all modes—and therefore we assume any error in these estimates is systematic and effect each simulations equally. According to Hicks47 acceptable residual ranges were not consistently met, suggesting that the ground reaction forces and moments (GRFM) prediction models may have introduced additional errors that could impact knee contact force estimates. Additional analysis using techniques such as the Residual Reduction Algorithm (RRA) could help mitigate the impact of modeling and processing errors, which can accumulate and result in significant non-physical compensatory forces; however, this was beyond the scope of the current study.
For calculating the impact of the PCA-based kinematics on the knee joint loading, a generic MSK models that was scaled based on the average scaling factor of each population (one MSK model for healthy and one MSK model for KOA) and the associated GRF and GRM were calculated using the probabilistic PCA (PPCA)37. This approach intentionally minimizes the impact of anthropometric and geometric variability on the knee contact force parameters. In particular, the generic knee model used in OpenSim JAM includes a generic geometry of the bones, cartilage surfaces, and knee ligaments28. The selective impact of anatomical variations in knee joint geometry on knee contact forces was reported in our previous work48 but is beyond the scope of the study.
Moreover, it was observed that the knee OA population exhibited a greater variation in knee contact forces, with both relevant increases and decreases across various modes (Fig. S9). This variation showed a range of up to 32%, in comparison to the healthy population where only decreases of up to 21% were observed. As such, our PCA analysis fails to identify specific kinematic patterns in the healthy population that could lead to functionally relevant increases in medial contact forces. A key observation in our simulations of healthy subjects is the general decrease in knee contact forces when modifying kinematics, particularly in first peak knee loads. As noted in prior studies49,50, first peak knee loads tend to be less variable than second peak loads, primarily due to their dependence on quadriceps forces, which are channeled through the patellar tendon with limited redistribution potential. This suggests that kinematic modifications may have less impact on first peak loading than expected. Additionally, a likely explanation for the observed trends is that the variability in knee flexion angle among healthy individuals was relatively small, meaning that perturbations within ± 1 standard deviation may not have been sufficient to meaningfully alter knee moments and, consequently, knee contact forces. The asymmetry in load changes across perturbations further suggests that other compensatory mechanisms—such as changes in internal/external rotation or other joints —may have overridden the expected effects of knee flexion moment variations. This reinforces the need for a deeper examination of kinematic and kinetic interdependencies when assessing contact force modulation.
Finally, gait data were collected during treadmill walking to facilitate the acquisition of a large number of trials. It is known that treadmill walking kinematics differ subtly from overground walking. This should be considered when interpreting the identified kinematic strategies and transferring them to overground conditions. Moreover, there are notable differences in gait speed and age between healthy and knee OA datasets (see Table 1). These differences reflect well-known and inherent characteristics of the populations, with the KOA population being generally older and exhibiting lower gait speed51. Slower gait speeds in the OA population are associated with different movement patterns (such as reduced stride length and range of motion) compared to the faster gait speeds observed in the healthy population52. Although differences in gait speed impact kinematic patterns, these alterations underscore the natural variations in movement dynamics between the two populations. As highlighted by Rowe et al.53, gait kinematics can vary significantly with age. Age-related differences in knee function are exacerbated in knee OA subjects, with older individuals presenting a more reduced knee flexion range of motion11. Consequently, the gait speed and age differences between the healthy and OA populations may have influenced the number of principal components identified through PCA, potentially affecting the reported differences in knee contact forces between the two groups. Nonetheless, both age and gait speed variations during self-selected gait are inherent characteristics of the OA population. The comparison between measured mean knee contact forces and those estimated from the modes remains relevant and illustrates their natural gait variation.
In conclusion, this study offers insights into the relationship between gait pattern variations and knee joint loading changes in healthy and knee osteoarthritis populations. Through principal component analysis, specific movement characteristics associated with altered knee loading were identified, highlighting unique gait characteristics and loading changes for both populations. The findings demonstrate the importance of analyzing the whole gait kinematics to optimize knee loading reduction, taking population biomechanical factors into account. Moreover, the study suggests the potential use of synthesized gait patterns (PCA-based) to estimate loading parameters. This innovative approach opens up possibilities for future applications, particularly through the utilization of machine learning techniques to predict distinct gait patterns and establish correlations with knee loading variations during everyday activities. This not only promises a practical and easily accessible solution but also represents an alternative to complex data collection in motion capture laboratories and musculoskeletal modeling workflows.
Methods
Dataset
3D MoCap collected at Laval University, Quebec City, Canada from twenty-three healthy adults and seventeen patients diagnosed with medial knee OA walked on instrumented treadmill at self-selected speed for ~ 2 min, see Table 1 (between 65 and 167 gait cycles per participant—2553 and 1754 cycles in total for healthy and knee OA population, respectively).
The 3D position of the 74 reflective markers, 42 attached to anatomical landmarks of the different body segments54,55 and 32 cluster markers was recorded using 9 infrared camera system (VICON, Oxford Metrics Group, UK, 100 Hz) while walking on an instrumented treadmill (Bertec, Columbus, OH, US, 1000 Hz) recording ground reaction forces. All participants provided written informed consent, prior to data collection. This research was in accordance with the ethical guidelines provided by the ethical research committee Centre Intégré Univeritaire de santé et de services sociaux de la Capitale-National, Quebec (MP-13-2020-1954).
Data processing
Filtered, labelled and gap-filled MoCap data (marker trajectories, ground reaction forces and center of pressure) were exported as .trc and .mot files from Nexus 2.12. Joint kinematics were calculated using the inverse kinematics tool in OpenSim Joint Articular Mechanics (JAM) using a validated musculoskeletal model with combined 12 degrees of freedom for the tibiofemoral (6DOF) and patellofemoral (6DOF) joints28. All trials were processed and time-normalized to 100% of the gait cycle (101 time points) using custom-built MATLAB scripts. Moreover, OpenSim JAM56,57 with the integrated concurrent optimization of muscle activations and kinematics (COMAK) algorithm57 was used to solve the muscle activation distribution problem, compute the resultant secondary knee kinematics and knee contact forces26 for all measured data.
Data analysis
After completing the data processing, joint kinematics were parameterized using a PCA-based framework19,34,58. Principal Component Analysis (PCA) of 2553 gait cycles for healthy and 1756 gait cycles for KOA were separately applied to extract the mean as well as dominant features in the modelling kinematic curves. Only the modes that represented >= 95% of the population variation were considered (20 for healthy and 14 for knee OA) for further analysis and MSK modelling (Tab. S1).
The PCs representing 95% of the cumulative variance showed the ability to reconstruct measured gait kinematics with an average RMSE of 3° across all 14 DOF. In this way, we believe these PCs appropriately represent the measured input data’s variability. A cumulative variance of 95% was also chosen based on previous studies58. Moreover, this study focused on the primary modes of variation, i.e., show the largest variance compared to the mean gait pattern for each population. The last 5% of cumulative variance components in PCA are generally excluded to prevent overfitting by disregarding noise and potentially random variability. This approach enhances model interpretability by prioritizing the most informative components that capture the underlying data variations.
Moreover, the gait variations of the final 5% showed only an average difference of less than 1 degree across all DOF compared to the mean gait pattern. This is particularly low compared to PC1 where an average difference of 10 degrees was observed (see Fig. S4 and S5). Therefore, the selection of 95% is sufficient to inform which variations are most common in each of the two populations and most relevant for further analysis. The investigated gait patterns were synthesized for each mode with a standard deviation of ± 1 from the average gait pattern. The choice of ± 1 standard deviation was motivated by the fact that a higher standard deviation (e.g. ± 2 or 3) could lead to gait kinematics that are representative of outliers/non-physiological gait patterns.
This approach allowed a targeted and isolated analysis of each mode and its effect on the knee loading parameters. Each synthesized gait pattern, represented by each mode with a standard deviation of +/−1, was utilized as kinematics in a musculoskeletal (MSK) modeling workflow. Specifically, two different MSK models, a healthy and a KOA MSK model, were scaled based on the mean scale factors of the 23 healthy and 18 knee OA individuals, respectively. Subsequently, the synthesized kinematics were imposed at the average population speed (1.28 m/s for healthy and 0.75 m/s for KOA), and the population-specific MSK model was utilized as inputs in a previously developed pipeline. This pipeline integrated probabilistic principal component analysis (PPCA)37,59 and zero moment point (ZMP) methods60,61 to estimate ground reaction forces and moments (GRFM), and the center of pressure (COP). These inputs are combined to estimate the knee joint loading parameters of interest (i.e., pressure, contact force, contact area)26,28,57. Thus, the impact of the synthesized gait patterns, represented by each individual mode, on the change in knee contact force (KCF) peaks was investigated. Relevant changes in knee contact force peaks were reported if greater than ± 10% body weight difference (ΔBW) from the mean knee contact force peaks of the medial knee compartments. In general, previously reported differences in KCF peaks between healthy and KOA population were found to be at least 10% BW62,63.
To identify which DOF contribute to each PC mode (Fig. 4), the area defined between the synthesized kinematic +/1 STD, (i.e. mode 1, mode 2, etc.…) (red and blue area Fig. 2) and the mean curve (solid black line) during the entire stance phase was used. To identify primary kinematics variations in healthy and knee OA populations and determine if these variations are unique to each population, the contribution of the kinematics was determined based on the variation throughout the whole stance phase, rather than solely during Peak 1 and Peak 2 of knee joint contact forces. Despite kinematic variation being examined across the entire stance phase, only two instants of contact forces were considered, as known differences between KOA and HS have been reported in literature62. These peaks offer essential insights into the maximum loading during loading response and pre-swing stance phases. While this approach seemingly creates a discrepancy in the data analysis, by imposing the PCA-derived kinematics over the entire stance phase, we ensure imposing continuous changes in gait cycle kinematics and dynamics. Consequently, the impact of the kinematic changes on the knee loading was evaluated based on the contribution value of the joints defined in Fig. 4. Furthermore, in the context of potential applications for gait retraining, it is essential to consider the joint variations at both peaks as well as the entire stance phase, to enforce continuity. This approach should permit considering all potential combinations of the degrees of freedom (DOFs) during the retraining session.
Data availability
The workflow and data will be made available on RDR—the KU Leuven repository.
References
Konrath, J. M. et al. Estimation of the knee adduction moment and joint contact force during daily living activities using inertial motion capture. Sensors (Switzerland) 19(7), 1681. https://doi.org/10.3390/s19071681 (2019).
O. R. S. International. Osteoarthritis: A Serious Disease, Submitted to the U. S. Food and Drug Administration. Oarsi, 1–103 (2016).
McAlindon, T. E. et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 22(3), 363–388. https://doi.org/10.1016/j.joca.2014.01.003 (2014).
Li, M. H., Xiao, R., Li, J. B. & Zhu, Q. Regenerative approaches for cartilage repair in the treatment of osteoarthritis. Osteoarthr. Cartil. 25(10), 1577–1587. https://doi.org/10.1016/j.joca.2017.07.004 (2017).
Chang, A. et al. The relationship between toe-out angle during gait and progression of medial tibiofemoral osteoarthritis. Ann. Rheum. Dis. 66(10), 1271–1275. https://doi.org/10.1136/ard.2006.062927 (2007).
Sharma, L. et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama 286(2), 188–195. https://doi.org/10.1001/jama.286.2.188 (2001).
Ulrich, B. et al. Diverse parameters of ambulatory knee moments differ with medial knee osteoarthritis severity and are combinable into a severity index. Front. Bioeng. Biotechnol. 13(11), 1176471. https://doi.org/10.3389/fbioe.2023.1176471 (2023).
Vincent, K. R., Conrad, B. P., Fregly, B. J. & Vincent, H. K. The pathophysiology of osteoarthritis: A mechanical perspective on the knee joint. PM R 4(5 SUPPL), S3. https://doi.org/10.1016/j.pmrj.2012.01.020 (2012).
Heijink, A. et al. Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg. Sports Traumatol. Arthrosc. 20(3), 423–435. https://doi.org/10.1007/s00167-011-1818-0 (2012).
Iijima, H., Shimoura, K., Ono, T., Aoyama, T. & Takahashi, M. Proximal gait adaptations in individuals with knee osteoarthritis: A systematic review and meta-analysis. J. Biomech. 87, 127–141. https://doi.org/10.1016/j.jbiomech.2019.02.027 (2019).
Favre, J. & Jolles, B. M. Gait analysis of patients with knee osteoarthritis highlights a pathological mechanical pathway and provides a basis for therapeutic interventions. EFORT Open Rev. 1(10), 368–374. https://doi.org/10.1302/2058-5241.1.000051 (2016).
Kubo, T. et al. Association between foot posture and tibiofemoral contact forces during barefoot walking in patients with knee osteoarthritis. BMC Musculoskelet. Disord. 23(1), 1–10. https://doi.org/10.1186/s12891-022-05624-y (2022).
Astephen, J. L., Deluzio, K. J., Caldwell, G. E. & Dunbar, M. J. Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J. Orthop. Res. 26(3), 332–341. https://doi.org/10.1002/jor.20496 (2008).
Lopen, T. Afwijkende mechanische belasting van het kniegewricht bij artrose. PQDT - UK Irel. (2017).
Meireles, S. et al. Knee contact forces are not altered in early knee osteoarthritis. Gait Posture 45, 115–120. https://doi.org/10.1016/j.gaitpost.2016.01.016 (2016).
Halim, H. N. A., Azaman, A. & Yahya, A. Gait characteristics and pain assessment of symptomatic knee osteoarthritis. IFMBE Proc. 82, 301–307. https://doi.org/10.1007/978-3-030-66169-4_37 (2021).
Ro, D. H. et al. Effects of knee osteoarthritis on hip and ankle gait mechanics. Adv. Orthop. https://doi.org/10.1155/2019/9757369 (2019).
Lebleu, J. et al. Lower limb kinematics using inertial sensors during locomotion: Accuracy and reproducibility of joint angle calculations with different sensor-to-segment calibrations. Sensors (Switzerland) 20(3), 715. https://doi.org/10.3390/s20030715 (2020).
Yamagata, M., Taniguchi, M., Tateuchi, H., Kobayashi, M. & Ichihashi, N. The effects of knee pain on knee contact force and external knee adduction moment in patients with knee osteoarthritis. J. Biomech. 123, 110538. https://doi.org/10.1016/j.jbiomech.2021.110538 (2021).
Uhlrich, S. D., Silder, A., Beaupre, G. S., Shull, P. B. & Delp, S. L. Subject-specific toe-in or toe-out gait modifications reduce the larger knee adduction moment peak more than a non-personalized approach. J. Biomech. 66, 103–110. https://doi.org/10.1016/j.jbiomech.2017.11.003 (2018).
Gerbrands, T. A., Pisters, M. F. & Vanwanseele, B. Individual selection of gait retraining strategies is essential to optimally reduce medial knee load during gait. Clin. Biomech. 29(7), 828–834. https://doi.org/10.1016/j.clinbiomech.2014.05.005 (2014).
Zhang, L. et al. A subject-specific musculoskeletal model to predict the tibiofemoral contact forces during daily living activities. Comput. Methods Biomech. Biomed. Eng. 26(8), 972–985. https://doi.org/10.1080/10255842.2022.2101889 (2023).
DeMers, M. S., Pal, S. & Delp, S. L. Changes in tibiofemoral forces due to variations in muscle activity during walking. J. Orthop. Res. 32(6), 769–776. https://doi.org/10.1002/jor.22601 (2014).
Curreli, C., Di Puccio, F., Davico, G., Modenese, L. & Viceconti, M. Using musculoskeletal models to estimate in vivo total knee replacement kinematics and loads: Effect of differences between models. Front. Bioeng. Biotechnol. 9, 703508. https://doi.org/10.3389/fbioe.2021.703508 (2021).
Jung, Y., Phan, C. B. & Koo, S. Intra-articular knee contact force estimation during walking using force-reaction elements and subject-specific joint model. J. Biomech. Eng. 138(2), 021016. https://doi.org/10.1115/1.4032414 (2016).
Smith, C. R., Won Choi, K., Negrut, D. & Thelen, D. G. Efficient computation of cartilage contact pressures within dynamic simulations of movement. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 6(5), 491–498. https://doi.org/10.1080/21681163.2016.1172346 (2018).
Benoit, D. L. et al. In vivo knee kinematics during gait reveals new rotation profiles and smaller translations. Clin. Orthop. Relat. Res. 454(454), 81–88. https://doi.org/10.1097/BLO.0b013e31802dc4d0 (2007).
Lenhart, R. L., Kaiser, J., Smith, C. R. & Thelen, D. G. Prediction and validation of load-dependent behavior of the tibiofemoral and patellofemoral joints during movement. Ann. Biomed. Eng. 43(11), 2675–2685. https://doi.org/10.1007/s10439-015-1326-3 (2015).
Meireles, S. et al. Medial knee loading is altered in subjects with early osteoarthritis during gait but not during step-up-and-over task. PLoS One 12(11), e0187583. https://doi.org/10.1371/journal.pone.0187583 (2017).
Amiri, P. et al. High tibiofemoral contact and muscle forces during gait are associated with radiographic knee OA progression over 3 years. Knee 41, 245–256. https://doi.org/10.1016/j.knee.2023.01.012 (2023).
De Roeck, J., Duquesne, K., Van Houcke, J. & Audenaert, E. A. Statistical-shape prediction of lower limb kinematics during cycling, squatting, lunging, and stepping—Are bone geometry predictors helpful?. Front. Bioeng. Biotechnol. 9, 585. https://doi.org/10.3389/fbioe.2021.696360 (2021).
De Roeck, J. et al. Statistical modeling of lower limb kinetics during deep squat and forward lunge. Front. Bioeng. Biotechnol. 8, 233. https://doi.org/10.3389/fbioe.2020.00233 (2020).
Deluzio, K. J., Wyss, U. P., Zee, B., Costigan, P. A. & Sorbie, C. Principal component models of knee kinematics and kinetics: Normal vs. pathological gait patterns. Hum. Mov. Sci. 16(2–3), 201–217. https://doi.org/10.1016/S0167-9457(96)00051-6 (1997).
Federolf, P. A., Boyer, K. A. & Andriacchi, T. P. Application of principal component analysis in clinical gait research: Identification of systematic differences between healthy and medial knee-osteoarthritic gait. J. Biomech. 46(13), 2173–2178. https://doi.org/10.1016/j.jbiomech.2013.06.032 (2013).
Erhart-Hledik, J. C., Favre, J. & Andriacchi, T. P. New insight in the relationship between regional patterns of knee cartilage thickness, osteoarthritis disease severity, and gait mechanics. J. Biomech. 48(14), 3868–3875. https://doi.org/10.1016/j.jbiomech.2015.09.033 (2015).
Favre, J., Erhart-Hledik, J. C., Chehab, E. F. & Andriacchi, T. P. General scheme to reduce the knee adduction moment by modifying a combination of gait variables. J. Orthop. Res. 34(9), 1547–1556. https://doi.org/10.1002/jor.23151 (2016).
Di Raimondo, G. et al. Peak tibiofemoral contact forces estimated using IMU-based approaches are not significantly different from motion capture-based estimations in patients with knee osteoarthritis. Sensors 23(9), 4484. https://doi.org/10.3390/s23094484 (2023).
Laudanski, A., Brouwer, B. & Li, Q. Measurement of lower limb joint kinematics using inertial sensors during stair ascent and descent in healthy older adults and stroke survivors. J. Healthc. Eng. 4(4), 555–576. https://doi.org/10.1260/2040-2295.4.4.555 (2013).
Gerbrands, T. A., Pisters, M. F., Theeven, P. J. R., Verschueren, S. & Vanwanseele, B. Lateral trunk lean and medializing the knee as gait strategies for knee osteoarthritis. Gait Posture 51, 247–253. https://doi.org/10.1016/j.gaitpost.2016.11.014 (2017).
Hunt, M. A. & Takacs, J. Effects of a 10-week toe-out gait modification intervention in people with medial knee osteoarthritis: A pilot, feasibility study. Osteoarthr. Cartil. 22(7), 904–911. https://doi.org/10.1016/j.joca.2014.04.007 (2014).
Shull, P. B. et al. Toe-in gait reduces the first peak knee adduction moment in patients with medial compartment knee osteoarthritis. J. Biomech. 46(1), 122–128. https://doi.org/10.1016/j.jbiomech.2012.10.019 (2013).
Bennour, S., Ulrich, B., Legrand, T., Jolles, B. M. & Favre, J. A gait retraining system using augmented-reality to modify footprint parameters: Effects on lower-limb sagittal-plane kinematics. J. Biomech. 66, 26–35. https://doi.org/10.1016/j.jbiomech.2017.10.030 (2018).
Aminiaghdam, S., Epro, G., James, D. & Karamanidis, K. Leaning the trunk forward decreases patellofemoral joint loading during uneven running. J. Strength Cond. Res. 36(12), 3345–3351. https://doi.org/10.1519/JSC.0000000000004128 (2022).
Karatsidis, A. et al. Validation of wearable visual feedback for retraining foot progression angle using inertial sensors and an augmented reality headset. J. Neuroeng. Rehabil. 15(1), 1–12. https://doi.org/10.1186/s12984-018-0419-2 (2018).
Seagers, K. et al. Changes in foot progression angle during gait reduce the knee adduction moment and do not increase hip moments in individuals with knee osteoarthritis. J. Biomech. 141, 111204. https://doi.org/10.1016/j.jbiomech.2022.111204 (2022).
Shull, P. B. et al. Six-week gait retraining program reduces knee adduction moment, reduces pain, and improves function for individuals with medial compartment knee osteoarthritis. J. Orthop. Res. 31(7), 1020–1025. https://doi.org/10.1002/jor.22340 (2013).
Hicks, J. L., Uchida, T. K., Seth, A., Rajagopal, A. & Delp, S. L. Is my model good enough? Best practices for verification and validation of musculoskeletal models and simulations of movement. J. Biomech. Eng. 137(2), 020905. https://doi.org/10.1115/1.4029304 (2015).
Willems, M. et al. Population-based in silico modeling of anatomical shape variation of the knee and its impact on joint loading in knee osteoarthritis. J. Orthop. Res.® 42(2024), 2473–2484 (2024).
Navacchia, A., Myers, C. A., Rullkoetter, P. J. & Shelburne, K. B. Prediction of in vivo knee joint loads using a global probabilistic analysis. J. Biomech. Eng. 138(3), 4032379. https://doi.org/10.1115/1.4032379.PMID:26720096;PMCID:PMC4844089 (2016).
DeMers, M. S., Pal, S. & Delp, S. L. Changes in tibiofemoral forces due to variations in muscle activity during walking. J. Orthop. Res.® 32(6), 769–776. https://doi.org/10.1002/jor.22601 (2014).
Bejek, Z. et al. Gait parameters of patients with osteoarthritis of the knee joint. Facta Universitatis: Series Phys. Educ. Sport 4(1), 9 (2006).
Milner, C. E. et al. Walking velocity and step length adjustments affect knee joint contact forces in healthy weight and obese adults. J. Orthop. Res.® 36(10), 2679–2686 (2018).
Rowe, E., Beauchamp, M. K. & Wilson, J. A. Age and sex differences in normative gait patterns. Gait & Posture 88, 109–115. https://doi.org/10.1016/j.gaitpost.2021.05.014 (2021).
Wu, G. et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 35(4), 543–548. https://doi.org/10.1016/S0021-9290(01)00222-6 (2002).
Wu, G. et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 38(5), 981–992. https://doi.org/10.1016/j.jbiomech.2004.05.042 (2005).
Delp, S. L. et al. OpenSim: Open-source software to create and analyze dynamic simulations of movement. IEEE Trans. Biomed. Eng. 54(11), 1940–1950. https://doi.org/10.1109/TBME.2007.901024 (2007).
Smith, C. R., Vignos, M. F., Lenhart, R. L., Kaiser, J. & Thelen, D. G. The influence of component alignment and ligament properties on tibiofemoral contact forces in total knee replacement. J. Biomech. Eng. 138(2), 021017. https://doi.org/10.1115/1.4032464 (2016).
Warmenhoven, J. et al. PCA of waveforms and functional PCA: A primer for biomechanics. J. Biomech. 116, 110106. https://doi.org/10.1016/j.jbiomech.2020.110106 (2021).
Tanghe, K. et al. A probabilistic method to estimate gait kinetics in the absence of ground reaction force measurements. J. Biomech. 96, 109327. https://doi.org/10.1016/j.jbiomech.2019.109327 (2019).
Dijkstra, E. J. & Gutierrez-Farewik, E. M. Computation of ground reaction force using Zero Moment Point. J. Biomech. 48(14), 3776–3781. https://doi.org/10.1016/j.jbiomech.2015.08.027 (2015).
Gupta, D., Donnelly, C. & Reinbolt, J. Physics-based guidelines for accepting reasonable dynamic simulations of movement. IEEE Trans. Biomed. Eng. 69(3), 1194–1201. https://doi.org/10.1109/TBME.2021.3119773 (2022).
Meireles, S., De Groote, F., Van Rossom, S., Verschueren, S. & Jonkers, I. Differences in knee adduction moment between healthy subjects and patients with osteoarthritis depend on the knee axis definition. Gait Posture 53, 104–109. https://doi.org/10.1016/j.gaitpost.2017.01.013 (2017).
Van Rossom, S. et al. Knee joint loading in healthy adults during functional exercises: Implications for rehabilitation guidelines. J. Orthop. Sports Phys. Ther. 48(3), 162–173. https://doi.org/10.2519/jospt.2018.7459 (2018).
Funding
This research was supported by KU Leuven—PhD project nr. 3M200591 as well as the Re- search Foundation Flanders (FWO) grant G0E4521N for collaboration with Laval University.
Author information
Authors and Affiliations
Contributions
Conceptualization, G.D.R., B.A.K., B.V., I.J.; Data collection, S.H. and K.T.; Data curation, M.W. and G.D.R.; Formal analysis, G.D.R, B.A.K.; Funding acquisition, K.T. and I.J.; Investigation, M.W., G.D.R. and B.A.K.; Methodology, G.D.R., B.A.K.; Software, G.D.R.; Supervision, B.A.K., B.V. and I.J.; Validation, G.D.R., and B.A.K.; Writing original draft, G.D.R., B.A.K. and I.J.; Writing—review and editing, M.W., B.A.K., B.V. and I.J.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent was obtained from all individuals involved in the study.
Institutional review board statement
The ethical committee of Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale, Québec (MP-13-2020-1954) gave ethical approval for this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Di Raimondo, G., Willems, M., Killen, B.A. et al. The impact of PCA derived gait kinematic variations on estimated medial knee contact forces in a knee osteoarthritis population. Sci Rep 15, 18342 (2025). https://doi.org/10.1038/s41598-025-90804-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90804-8