Abstract
The Information Technology (IT) sector is a leading industry that fuels India’s economic growth. However, the work culture in this sector often promotes sedentary lifestyle, inadequate physical activity, and unhealthy dietary patterns which are risk factors for various non-communicable disease (NCD). This study aims to assess the prevalence of metabolic dysfunction-associated fatty liver disease (MAFLD) among IT employees and its association with behavioural and biological risk factors. This cross-sectional study involved 345 IT employees in Hyderabad, India, who responded to a questionnaire on their occupational sitting, shift work, stress, sleep duration, smoking, physical activity, and food habits. Anthropometric, biochemical, metabolic, and liver function parameters were evaluated. MAFLD was diagnosed using a Vibration-Controlled Transient Elastography FibroScan. Chi-square test and Spearman’s rank correlation were performed to analyse the associations and correlations between risk factors. The median age of the employees was 38 years (34–43 years) with a body mass index (BMI) of 244 (70.72%) obese. Approximately, 248 (71.88%), 89 (25.80%), 241 (69.86%) and 131 (37.97%) of employees were found to sit for long hours at work, had shift work, sleep deprivation and stress, respectively. Almost 72 (20.87%) of IT employees had elevated fasting blood glucose (FBG) and 264 (76.52%) had high low-density lipoprotein (LDL-C). Metabolic Syndrome (MetS) was present in 118 (34.20%) of the employees. A total of 290 (84.06%) employees had increased liver fat accumulation indicating MAFLD. There is high prevalence of MAFLD among IT employees, highlighting the urgent need for workplace interventions and health promotion initiatives addressing MAFLD risk in the IT workforce.
Similar content being viewed by others
Introduction
The Information Technology (IT) sector in India is one of the leading growth catalysts for the Indian economy, accounting for about 7% of India’s Gross Domestic Product in fiscal year 2023–2024. In India, the IT industry currently employs 5.43 million employees, including 36% women1. According to the National Association of Software and Services Companies (NASSCOM), an estimated revenue of 227 billion US dollars was generated from the Indian IT sector in 2021–22. By 2026, the country’s IT sector will need almost 9.5 million skilled IT workers, leading India towards its potential to become a trillion-dollar digital economy2. Among the IT hubs in India, Hyderabad is one of the major IT metropolises with around 1500 IT companies and over 5.8 lakh professionals employed3.
The IT sector is known for adapting to a work culture involving a sedentary lifestyle, physical inactivity, and changing dietary habits, linking it to a higher risk of developing non-communicable diseases (NCDs) including metabolic dysfunction-associated fatty liver disease (MAFLD)4,5.
The metabolic risk factors include visceral adiposity, hypertension, hyperglycemia, lowered levels of high-density lipoprotein cholesterol (HDL-C), and increased triglycerides (TG). These risk factors can get aggravated in occupations with sedentary lifestyle and consumption of unhealthy, obesogenic diet. Additionally, food rich in refined carbohydrates, fructose, saturated fats, and sugar sweetened beverages (SSBs) increase the risk of obesity6,7,8. Various studies across India have reported the prevalence of metabolic and behavioural risk factors such as overweight, hyperglycemia, high blood pressure (BP), dyslipidemia, stress, insomnia, and depression among IT employees9,10,11. A recent study conducted among IT employees in South India investigated lifestyle-associated risk factors contributing to NCDs and estimated the prevalence of metabolic syndrome (MetS) to be 29.87%, with 44.02% of the subjects being overweight, 16.85% obese, 3.86% diabetic, and 64.93% having low HDL-C levels12.
The risk factors associated with MetS are also implicated as a cause or consequence of MAFLD13,14. The presence of more than 5% fat in the hepatocytes, in the absence of secondary causes of fat accumulation in liver either due to alcohol consumption, medication, diseases, or hereditary causes is defined as MAFLD. The metabolic risk factors are commonly associated with MAFLD, which ranges from the spectrum to the inflammatory state of metabolic dysfunction-associated steatohepatitis (MASH), advances to fibrosis, and later to liver cirrhosis and hepatocellular carcinoma8,14. Various factors, including genetic predisposition, sex, age, race or ethnicity, obesity, dietary patterns, insulin resistance, diabetes, hypertension, and sleep deprivation, influence the development of MAFLD8,14. Apart from overweight individuals, a considerable proportion of people with body mass index (BMI) < 23 kg/m2 have MAFLD, addressed as lean MAFLD, found in the Asian population15. Lean MAFLD is closely linked to MetS16 with a global prevalence of 5.1%15. Due to the common causal pathways for NCDs, MetS and MAFLD, the Government of India included MAFLD in its National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke in 2021, and renamed the National Programme for Prevention and Control of Non-Communicable Diseases in 202317,18.
Epidemiological studies among the Indian population revealed the prevalence of MAFLD to be approximately 9% to 32%, with higher prevalence rates in obese and diabetic individuals18. In a large cohort of patients with MAFLD from South Asia, the prevalence of lean MAFLD was 10.6%19. In a systematic review published by Shalimar et al. the prevalence of MAFLD among adults and children was 38.6% and 35.4%, respectively20. A cross-sectional study reported higher BMI and increasing age as significant predictors of MAFLD21. A substantially high prevalence of MAFLD was observed in both urban and rural Indian populations, signifying the need for urgent public health interventions and control measures22. However, few studies have determined the prevalence of MAFLD, specifically in a high-stress, highly sedentary workforce with more hours of occupational sitting and jobs involving shift work20.
Despite reporting metabolic and lifestyle risk factors among IT employees in India, no study has assessed the prevalence of MAFLD in this group. If not screened at an early stage in the working-age group, the disease may go undiagnosed and become a huge public health burden. Hence, this study aimed to determine the prevalence of MAFLD and the associated behavioural and metabolic risk factors among IT employees in India.
Methods
Study design and participants recruitment
A cross-sectional study was conducted in Hyderabad, India from July, 2023 to July, 2024. The IT employees were randomly selected through wide publicity in the IT Hub situated in Hi-tech city locality of Hyderabad. Initially, a list of alumni students’ email with the IT companies that employed them was procured from the placement cell of the University of Hyderabad. Emails were sent to the Human Resource section of the IT companies located in Hyderabad describing the purpose of our study and seeking their participation. Information about the study was communicated to IT employees through text messages, emails, leaflets, banners, posters, and also by conducting camps. The link and QR codes for registration of participants were provided in all modes of communication. The consent form and study questionnaire were made available online and the research team also administered the questionnaire face-to-face to some IT employees. Their contact details were sought to follow up for biochemical tests.
Sample size Sample size was determined by considering a previous prevalence rate of 32%16, with a precision level of 5%, a sample size of 348 was determined by using the formula 4pq/L2. Given p = Prevalence rate 32%, q = 100–32 = 68, Level of precision (L) is 5% (absolute) 4(32 × 68)/5 × 5 = 8704/25 = 348.
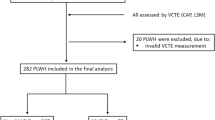
Inclusion and exclusion IT employees working in Hyderabad, India for at least one year and those aged between 30 and 60 years with minimal or no reported alcohol consumption (< 30 g/day for men or < 20 g/day for women) were included in the study. The participation was voluntary and we received 558 online responses and 200 offline responses. The research team reached out to all the participants who responded both online and offline. Based on the eligibility criteria and willingness to participate in the biochemical, metabolic and liver scan tests, 363 IT employees visited Asian Institute of Gastroenterology (AIG) Hospital, Hyderabad located in close proximity to the IT Hub. The recruitment rate in the study was 363 (47.88%). The anthropometric measurements, biochemical, metabolic, liver function tests and liver fibroscan were carried out at AIG Hospital, Hyderabad. All the tests were carried out after an overnight fasting of 8–12 h. The research team coordinated the scheduled visits and walked the study participants through the screening process. Participants who tested positive for hepatitis B (HbsAg), hepatitis C (HCV), and autoimmune diseases were excluded from the study. A total of 345 employees were included in the final data analysis (Fig. 1).
Data collection
Information related to history of tobacco and alcohol use, diet (food frequency questionnaire), 24-h dietary recall, physical activity, and medication use were gathered using a modified WHO surveillance (STEPS) questionnaire for NCDs23. Details of sleep duration, stress and occupational sitting were obtained through modified Pittsburgh Sleep Quality Index (PSQI)24, Perceived Stress Scale (PSS4)25, and Occupational Sitting and Physical Activity Questionnaire (OSPAQ)26, respectively.
Anthropometric and blood pressure measurements
The weight and height of all participants were measured using Quick Vital Sign-QVS-105 (Vortex Med Solutions Pvt. Ltd). Waist and hip circumferences were measured using standard techniques with a non-stretchable flexible tape with readings in centimetres, separately for men and women. The BP of each participant was measured in a sitting position using the Quick Vital Sign- QVS-105 (Vortex Med Solutions Pvt. Ltd). Hypertension was classified based on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines27.
Evaluation of biochemical parameters
After an overnight fast of 8–12 h, a total of 15 ml of venous blood was drawn from each participant by trained phlebotomy technicians and subjected to specific biochemical tests. Fasting blood glucose (FBG) levels were analysed using the hexokinase method in the Abbott Alinity c diagnostic system, and fasting insulin levels were analysed using the electrochemiluminescence immunoassay method in the Abbott Alinity i diagnostic system. The fasting lipid profile- Total cholesterol (TC) was evaluated using the cholesterol oxidase–peroxidase method, HDL-C was assayed using the enzymatic colorimetric method, and TG was analysed using the glycerol phosphate oxidase–peroxidase method in Beckman Coulter AU5800. Low-density lipoprotein cholesterol (LDL-C) was calculated using the formula LDL-C = (TC)—(HDL-C)—(TG)/5, and very-low-density lipoprotein cholesterol (VLDL-C) was calculated using the formula (TG)/5. Liver function test- Total bilirubin was determined using the 3,5-dichlorophenyl diazonium method, and alanine aminotransferase (ALT) was analysed using the International Federation of Clinical Chemistry and Laboratory Medicine reference method for measuring ALT activity without Pyridoxal-5'-Phosphate, aspartate aminotransferase (AST) was assayed using the IFCC reference method for measuring AST activity without P5P, alkaline phosphatase (ALP) was evaluated using the 2-Amino-2-methyl-1-propanolbuffer method after optimization to International Federation of Clinical Chemistry and Laboratory Medicine using Beckman Coulter AU500. The presence of viral markers-HbsAg, and anti-HCV was investigated using Enhanced Chemiluminescence Immunoassay method in VITROS 3600.
Assessment of liver steatosis and liver fibrosis
Liver biopsy the “gold standard” for diagnosing MAFLD and assessing its severity has limitations of histological staging and is not applicable on large scale for screening. Hence, non-invasive imaging techniques such as vibration-controlled transient elastography (VCTE) and magnetic resonance elastography (MRE) are used to evaluate hepatic steatosis and fibrosis. A trained technician at AIG Hospital performed VCTE with FibroScan 502 Touch (ECHOSENS, Paris, France) using an M probe in participants with BMI < 30 kg/m2 and an XL probe in participants with BMI ≥ 30 kg/m2 for the measurement of the controlled attenuated parameter (CAP) and liver stiffness measurement (LSM) for liver steatosis and liver stiffness, respectively.
Statistical analysis
The analysis was performed using Microsoft Excel 2019, IBM SPSS 25.0 (SPSS, Inc., Chicago IL, USA), and GraphPad Prism 9.5. The normality of the data was checked using Kolmogorov–Smirnov Tests of Normality. As most of the data were skewed, median values, 25th (P25) and 75th (P75) percentile were considered. Associations between categorical variables were assessed using the chi-square test. The correlation between various anthropometric, behavioural, and biochemical parameters and MAFLD was evaluated using Spearman’s correlation coefficient (rs). A probability level of alpha < 0.05 was considered as significant.
Ethical considerations
The study protocol was approved by the Institutional Ethics Committee (IEC) of the University of Hyderabad (approval number: UH/IEC/2022/412) and AIG Hospital, Hyderabad (approval number: AIG/IEC-BH&R43/03.2023–06). All research was performed in accordance with relevant guidelines/regulations and informed consent was obtained from all participants. Participation in the study was voluntary and there were no financial incentives. As a benefit to study participation, their biochemical and FibroScan test reports were shared with them, providing health insights without compromising the integrity of the study.
Results
A total of 363 IT employees were initially enrolled in the study through a voluntary recruitment process. Participants with secondary causes of liver steatosis like alcohol consumption, hepatitis B, hepatitis C or autoimmune diseases and those not meeting the inclusion criteria for age 30–60 years were excluded. After exclusion for secondary causes of liver steatosis and missing data, 345 IT employees included in the final analysis, of which 294 (85.20%) were men and 51 (14.80%) were women. Most 327 (94.80%) belonged to the age group of 30–49 years with a small proportion (5%) over 50 years. All the participants were literate and had graduation or post-graduation degrees. The median number of years of work was 14 years (9.8–18.0 years) and the work pattern was 125 (36.23%) worked in office, 165 (47.80%) worked in hybrid mode and 55 (15.90%) worked from home (WFH) (Table 1).
Description of Anthropometric characteristics of participants
The height, weight was measured and the BMI was calculated as per Asian population cut-off: < 18.5 kg/m2 (underweight), 18.5–22.9 kg/m2 (normal), 23.0–24.9 kg/m2 (overweight), and ≥ 25.0 kg/m2 (obese)28. BMI was normal among 51 (14.78%) [95% CI 11.20—19.00], overweight 50 (14.49%) [95% CI 11.00—18.70] and obese 244 (70.72%) [95% CI 65.60—75.50]. Men with waist circumference (WC) ≥ 90 cm were 253 (73.33%), while women with WC ≥ 80 cm were 43 (12.46%) (Table 1).
Behavioural risk factors among IT employees
Behavioural risk factors, such as sitting for long hours, shift work, sleep deprivation, stress, and smoking were assessed. A total of 248 (71.88%) were engaged in sedentary work (sitting > 8 h/day). Out of 345 employees, 256 (74.20%) reported working in general shift (9.00 am to 5.00 pm) and 89 (25.80%) worked in non-general shift (outside of 9.00 am to 5.00 pm). About 241 (69.86%) reported inadequate sleep (< 7 h/day). About 131 (37.97%) reported work-related stress, as assessed using the PSS-4. Less than 10% of them reported having ever smoked 34 (9.86%) (Fig. 2a).
Behavioural, biochemical parameters, and metabolic risk factors. (a) Occupation related behaviour –sitting > 8 h/day; Shift work (outside 9.00 AM to 5.00 PM); sleeping < 7 h/ day; Perceived Stress Score (PSS-4) ≥ 10; (b) Unhealthy diet and physical inactivity – Consumption of SSBs, High-Fat Diet, High-Salt Diet, High-Sugar Diet and Low-Fibre consumption; Physical Inactivity: having < 150 min of moderate-intensity physical activity/week. (c) Biochemical parameters – HOMA-IR Ratio > 2.529; TC ≥ 200 mg/dL; LDL-C ≥ 100 mg/dL; VLDL-C > 30 mg/dL; Fasting Insulin > 24.9 mlU/L; TC/HDL Ratio > 3.5; TG/HDL Ratio > 2.530. (d) Liver enzymes and proteins – Total Bilirubin > 1.0 mg/dL; Direct Bilirubin > 0.2 mg/dL; ALT > 34 U/L; AST > 31 U/L; ALP > 105 U/L; Total Proteins > 8.3 gm/dL; Albumin > 5.3 gm/dL; Globulin > 3.5 gm/dL31. (e) Metabolic risk factors (MetS) – BP ≥ 130/85 mmHg; HDL-C in Men: < 40 mg/dL and Women: < 50 mg/dL; TG ≥ 150 mg/dL; FBG ≥ 100 mg/dL; WC in Men: ≥ 90 cm and Women: ≥ 80 cm32.
Unhealthy diet consumption of SSBs like soft drinks, energy drinks, tea, and coffee reported by 98 (28.41%) participants, high fat diet like meat, dairy, and oils by 91 (26.38%), high-salt diet like consumption of fried items by 41 (11.88%), high-sugar diet by 126 (36.52%) and low-fibre diet by 134 (38.84%) participants. Intentional daily physical activity reported by 194 (56.23%) participants, while 78 (22.61%) reported < 150 min of moderate-intensity physical activity per week (Fig. 2b).
High LDL-C in 264 (76.52%) [95% CI 71.70—80.90], TC/HDL ratio in 294 (85.21%), and TG/HDL ratio in 196 (56.81%) were found among the study participants. An elevated homeostatic model assessment for insulin resistance (HOMA-IR) ratio was observed in 180 (52.17%) [95% CI 46.80—57.60] participants. (Fig. 2c).
Liver function parameters showed increased total bilirubin in 86 (24.92%) participants. The liver enzymes among the participants, 71 (20.57%) had elevated ALT levels, 52 (15.07%) had increased AST levels, and 51 (14.78%) had elevated ALP levels (Fig. 2d).
The prevalence of MetS (metabolic risk factors ≥ 3) was found in 118 (34.20%) [95% CI 29.20—39.50] participants. The high WC was 296 (85.80%) [95% CI 81.70—89.30], followed by elevated BP 129 (37.83%) [95% CI 32.30—42.70], and low HDL-C levels 121 (35.07%) [95% CI 30.0—40.40]. Twenty (5.80%) participants had no metabolic risk factors, while 6 (1.76%) participants had all five risk factors associated with MetS (Fig. 2e).
Biochemical, liver function parameters and metabolic risk factors:
The median (P25-P75) values of the biochemical and liver function parameters of the participants are presented in Table 2.
Prevalence of MAFLD among the IT employees
The overall prevalence of MAFLD among IT employees revealed that 290 (84.06%) [95% CI 78.80—87.80] out of 345 participants had liver steatosis. The age-specific prevalence of MAFLD between the age of 30–40 years was 50.14% and 33.91% between the ages of 41–60 years. The prevalence of MAFLD was high in men 255 (73.91%) than in women 35 (10.14%) (Fig. 3a). Liver steatosis: Grade-S1 (11–33% Liver Fat) CAP score 238–259 dB/m; Grade-S2 (34–66% Liver Fat) CAP score 260–289 dB/m; Grade-S3 (> 67% Liver Fat) CAP score > 290 dB/m, indicating mild to severe steatosis33. While 55 employees (15.94%) [95% CI 12.20—20.20] had Grade-S0 (0–10% Liver Fat) CAP score between 150 and 237 dB/m indicating no liver steatosis and 70 (20.29%) [95% CI 16.20—24.90] had Grade-S1, 103 (29.86%) [95% CI 25.10—35.00] had Grade S2 and 117 (33.91%) [95% CI 28.90—39.20] had Grade-S3 liver steatosis (Fig. 3b). Liver fibrosis was assessed using fibrosis score ranging from F0 to F433,34. Fibrosis was absent in most participants, with 336 (97.39%) having score F0 and F1 (kPa < 8.0), suggesting no to mild fibrosis. Eight participants (2.32%) had moderate fibrosis (F2) (kPa 8.0–10.0) and severe fibrosis with a score of F3 (kPa 11.0–16.0) was seen only in one participant (0.29%) (Fig. 3c).
Prevalence of MAFLD among the IT employees. (a) Age specific prevalence of MAFLD among men and women (b) Prevalence of MAFLD – Grade-S0 (0–10% Liver Fat) CAP score – 150–237 dB/m; Grade-S1 (11–33% Liver Fat) CAP score—238–259 dB/m; Grade-S2 (34–66% Liver Fat) CAP score—260–289 dB/m; Grade-S3 (> 67% Liver Fat) CAP score—> 290 dB/m33. (c) Prevalence of liver fibrosis – F0-F1 (kPa < 8.0)—normal; F2 (kPa 8.0–10.0)—moderate scarring; F3 (kPa 11.0–16.0)—severe scarring; F4 (kPa > 16.0) – cirrhosis33,34.
The study examined the occupation related behavioural risk factors namely sedentary work, shift work, sleep deprivation, stress, and smoking. No behavioural risk was reported by 18 (5.22%) participants yet, MAFLD was observed in 14 (4.06%) of them. Presence of at least one risk factor was reported in 59 (17.10%) participants and the prevalence of MAFLD was 49 (14.20%). Two risk factors were found in 153 (44.35%) participants of whom 129 (37.39%) had MAFLD followed by 84 (24.35%) who had three risk factors with 70 (20.29%) MAFLD. All five risk factors were present in two participants and both had MAFLD. (Fig. 4a).
Clustering of behavioural risk factors, unhealthy diet, physical inactivity, metabolic risk factors, and prevalence of MAFLD among IT employees. (a) Clustering of behavioural risk factors and prevalence of MAFLD – sitting for long hours, shift work, sleep deprivation, stress, and smoking constituting the five risk factors and the associated prevalence of MAFLD. (b) Clustering of unhealthy diet and physical inactivity and prevalence of MAFLD – Reported consumption of SSBs, and diets with high-fat, high-salt, high-sugar, and low-fibre diet, and physical inactivity constituting the six risk factors and the associated prevalence of MAFLD. (c) Clustering of metabolic risk factors and prevalence of MAFLD – raised WC, elevated FBG, increased BP, low-HDL-C, and high TG.
Unhealthy dietary intake and physical inactivity were assessed for the presence of MAFLD. A total of 107 (31.01%) participants, had at least one risk factor, and MAFLD was observed in 85 (24.64%) participants. Two risk factors were observed in 101 (29.28%) participants, with 81 (23.48%) having MAFLD. The presence of all six risk factors was found in 11 participants (3.19%), with 10 (2.90%) having MAFLD (Fig. 4b).
Metabolic risk factors were assessed for the presence of MAFLD among the participants. The presence of one metabolic risk factor (increased WC, elevated FBG, increased BP, low-HDL-C, and high TG) was reported in 85 (24.64%) participants, with MAFLD found in 65 (19.84%). At least two of the five metabolic risk factors were observed in 122 (35.36%) participants, and 108 (31.30%) had MAFLD. All metabolic risk factors were seen in six (1.74%), of which five (1.45%) of them had MAFLD. Despite a meagre 20 (5.80%) participants with no metabolic risk factors, six (1.74%) of them had MAFLD (Fig. 4c).
Association of behavioural and metabolic risk factors with MAFLD
MAFLD was associated with age (p = 0.036). Shift work was associated with elevated FBG, HOMA-IR, TC, LDL-C, and BMI (p < 0.05). Low HDL-C levels and inadequate sleep hours had association (p = 0.036). Physical activity of < 150 min/week showed association with overweight and obesity (p = 0.004) and MAFLD (p = 0.009). Consumption of low-fibre diet was associated with TC (p = 0.001). Intake of SSBs and smoking were associated with MAFLD (p = 0.012) and (p = 0.029), respectively. The behavioural risk factors were associated with the MetS among participants. Higher BMI, WC, elevated HOMA-IR, FBG, and BP showed a significant association with MAFLD (p < 0.001) (Table 3).
Correlation of anthropometric and metabolic risk factors with MAFLD
WC and BMI showed a significantly positive correlation with MAFLD rs = 0.66 (p = < 0.0001), followed by waist-to-hip ratio (W/H) rs = 0.50 (p = < 0.0001). Elevated fasting insulin, HOMA-IR, and FBG showed a significant positive correlation with MAFLD, rs = 0.53, 0.52, and 0.18, respectively (p = < 0.0001). TG levels were also positively correlated with MAFLD rs = 0.27 (p = < 0.0001). The liver enzymes ALT and AST had a positive correlation with MAFLD rs = 0.38 and rs = 0.23 respectively (p = < 0.0001) (Fig. 5).
Spearman correlation plots for the correlation of anthropometric, biochemical, and metabolic risk factors with MAFLD. Correlation of (a) WC vs MAFLD; (b) BMI vs MAFLD; (c) W/H ratio vs MAFLD; (d) Fasting Insulin vs MAFLD; (e) HOMA-IR vs MAFLD; (f) TG vs MAFLD; (g) TC/HDL ratio vs MAFLD; (h) ALT vs MAFLD.
Discussion
This study aimed to assess the prevalence of MAFLD and its associated behavioural and metabolic risk factors among IT employees in India. The study revealed an alarming 84.06% prevalence of MAFLD among the IT employees. A systematic review recorded the prevalence of MAFLD in the general Indian population at 38.6%20. The recent large cross-sectional study in the capital city of Delhi, India among general population has revealed a higher prevalence of 56.4%35. A city in western region of India, Goa has for a long time reported alcoholic liver disease but a recent study has reported 34.8% prevalence of MAFLD36. As per a survey conducted by Asian Institute of Gastroenterology in Telangana region, fatty liver diseases were 20% and 25% in rural and urban population respectively37. As there are no comparable studies in the region our study is the first to report MAFLD prevalence in among IT employees. The Indian population has predilection for lean MAFLD and we found 20 IT employees (5.80%) from our study participants with BMI < 23 kg/m2 had MAFLD. The study findings by Sarin et al., showed a prevalence of lean MAFLD at 11.3%35. MAFLD was more prevalent among males and older individuals that is reflected in our study also with73.91% males and 10.14% females having MAFLD21,35,36. The sex differential in our study could be due to the paucity of women in the age group of 30–60 years in the Indian IT sector38. The work culture in the IT industry often involves engagement in sedentary activities for extended periods, shift work and irregular work hours, sleep deprivation, stress, and smoking, combined with unhealthy food options, creating the perfect storm for the development of MetS and MAFLD. Occupational sitting for > 8 h in a workday, inadequate sleep hours, high perceived stress, and physical inactivity as the major behavioural risk factors leading to the development of MAFLD. Reports on the impact of sedentary behaviour, shift work, and lack of exercise on metabolic parameters are fairly evident6,7,39. Studies have also reported the prevalence of behavioural and metabolic risk factors among IT professionals in India9,10,12. To our knowledge, this study is the first in India to report the association of behavioural risk with MAFLD in IT employees.
The prevalence of MetS in our study was 34.3%, which is in line with observations by Banerjee et al. study12. The high prevalence of MetS among the participants was driven primarily by elevated WC, BMI, BP, and dyslipidaemia. The two parameters of BMI and WC indicating abdominal obesity is associated with highest risk for MAFLD. Reducing the abdominal obesity provides MAFLD remission12,40. Though elevated WC is associated with a sedentary work life, factors other than abdominal obesity can also lead to MetS7. The common covariates for MAFLD, like BP, FBG, TG, and TC, were associated with the long working hours in workers < 60 years41. This is on par with our observation that MAFLD correlates to age, along with other metabolic parameters- FBG, HOMA-IR, fasting insulin, TG, and TC. There is paucity of studies among various occupational groups. However, two studies examined workplace MAFLD among steel workers in Korea and China using abdominal ultrasound and found high prevalence42,43. Our study brings to fore the occupational context that is a critical factor in understanding the prevalence of MAFLD. This study has significant public health implications given the natural progression of the disease to fibrosis and cirrhosis that are irreversible and have no cure. As the progressive form of MASH (liver fibrosis) in the MAFLD spectrum was found in only few participants, there is a scope to prevent the progression to the severe form. Further longitudinal studies are required to establish the causal relationship and also fill in the research gap that exists.
Limitations The study sample predominantly had males (85.2%) and hence we did not extensively analyze female subgroup due to the paucity of women in the age group of 30–60 years in the Indian IT sector. Further research is needed to understand the unique risk factors and mechanisms in subgroups with MAFLD in participants with normal BMI. The study lacks a comparison between IT employees and the general Indian population regarding behavioral and metabolic risk factors which can help determine whether the observed risk factors are unique to the IT sector or prevalent across the broader population. There could be both selection and information bias as the behavioural information obtained relied on voluntary participants’ self-reported behavioural pattern as there was no means of verification.
Conclusion and recommendations
This study highlights the high prevalence of MAFLD (84.06%) among IT employees in India, linked to sedentary lifestyles, unhealthy diets, and metabolic risk factors. Therefore, we recommend urgent and appropriate interventions to increase their physical activity and reduce sedentary lifestyle. Considering dietary modification by reducing HFSS (High fat, sugar and salt), consuming diet low in calories and rich in fibre may aid in reducing their abdominal obesity. It is worth noting that occupational risk factors involving prolonged sitting, shift work and physical inactivity among IT employees puts them at specific risk for MAFLD and therefore, routine periodic screening for MAFLD is required. As IT employees are not addressed in India’s National Programme for Non-Communicable Diseases programme, urgent workplace interventions are needed to address MAFLD and its associated risks, emphasizing the need for routine liver function screenings in this population.
Abbreviations
- ALP:
-
Alkaline Phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate Aminotransferase
- BMI:
-
Body Mass Index
- BP:
-
Blood Pressure
- CAP:
-
Controlled Attenuated Parameter
- FBG:
-
Fasting Blood Glucose
- HbsAg:
-
Hepatitis B surface antigen
- HCV:
-
Hepatitis C virus
- HDL-C:
-
High-Density Lipoprotein Cholesterol
- HOMA-IR:
-
Homeostatic Model Assessment for Insulin Resistance
- IEC:
-
Institutional Ethics Committee
- IT:
-
Information Technology
- LDL-C:
-
Low-Density Lipoprotein Cholesterol
- MAFLD:
-
Metabolic Dysfunction-Associated Fatty Liver Disease
- MASH:
-
Metabolic Dysfunction-Associated Steatohepatitis
- MetS:
-
Metabolic Syndrome
- MRE:
-
Magnetic Resonance Elastography
- NCDs:
-
Non-Communicable Diseases
- OSPAQ:
-
Occupational Sitting and Physical Activity Questionnaire
- PSQI:
-
Pittsburgh Sleep Quality Index
- PSS4:
-
Perceived Stress Scale
- SSBs:
-
Sugar-Sweetened Beverages
- TC:
-
Total Cholesterol
- TG:
-
Triglycerides
- VLDL-C:
-
Very-Low-Density Lipoprotein Cholesterol
- W/H:
-
Waist-to-Hip Ratio
- WC:
-
Waist Circumference
References
Ministry of Electronics and Information Technology, Government of India. IT/Software Sector; 2024. https://www.meity.gov.in/content/software-and-services-sector [accessed01 October 2024].
Press Information Bureau. Government of India, Ministry of Electronics & IT. Number of employees in IT; 2022.https://www.pib.gov.in/Pressreleaseshare.aspx?PRID=1847841 [accessed 01 October 2024].
Department of Industries and Commerce, Government of Telangana. IT/ITeS. https://invest.telangana.gov.in/it-ites-sector/ [accessed 04 October 2024].
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 73(1), 202–209. https://doi.org/10.1016/j.jhep.2020.03.039 (2020).
Eslam, M. et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: An international expert consensus statement. Lancet Gastroenterol. Hepatol. 6(10), 864–873. https://doi.org/10.1016/S2468-1253(21)00183-7 (2021).
Hamilton, M. T., Hamilton, D. G. & Zderic, T. W. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 56(11), 2655–2667. https://doi.org/10.2337/db07-0882 (2007).
Honda, T. et al. Sedentary bout durations and metabolic syndrome among working adults: A prospective cohort study. BMC Public Health. 16(1), 888. https://doi.org/10.1186/s12889-016-3570-3 (2016).
Rinella, M. E. et al. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. 77(5), 1797–1835. https://doi.org/10.1097/HEP.0000000000000323 (2023).
Limaye, T. Y., Kulkarni, R. L., Deokar, M. R. & Kumaran, K. High prevalence of cardiometabolic risk factors in young employees of Information Technology industry. Indian J. Occup. Environ. Med. 20(1), 64–67. https://doi.org/10.4103/0019-5278.183848 (2016).
Padma, V. et al. Health problems and stress in information technology and business process outsourcing employees. J. Pharm. Bioallied Sci. 7(Suppl1), S9-13. https://doi.org/10.4103/0975-7406.155764 (2015).
Babu, G. R., Mahapatra, T. & Detels, R. Job stress and hypertension in younger software professionals in India. Indian J. Occup. Environ. Med. 17(3), 101–107. https://doi.org/10.4103/0019-5278.130848 (2013).
Banerjee, P. et al. Diets, lifestyles and metabolic risk factors among corporate information technology (IT) employees in South India. Nutrients. 15(15), 3404. https://doi.org/10.3390/nu15153404 (2023).
Radu, F. et al. The link between NAFLD and metabolic syndrome. Diagnostics. 13(4), 614. https://doi.org/10.3390/diagnostics13040614 (2023).
Chalasani, N. et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the study of liver diseases. Hepatology. 67(1), 328–357. https://doi.org/10.1002/hep.29367 (2018).
Wang, W. et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD) and the development of metabolic syndrome: a retrospective study. Sci. Rep. 12(1), 10977. https://doi.org/10.1038/s41598-022-14701-0 (2022).
Sinha, N., Mukhopadhyay, S. & Sau, M. Metabolic syndrome is not uncommon among lean non-alcoholic fatty liver disease patients as compared with those with obesity. Indian J. Gastroenterol. 39, 75–83. https://doi.org/10.1007/s12664-020-01020-3 (2020).
Ministry of Health and Family Welfare, Government of India. Operational Guidelines National Programme for Prevention and Control of Non-Communicable Diseases (2023–2030); 2023. https://mohfw.gov.in/sites/default/files/NP-NCD%20Operational%20Guidelines_0.pdf [accessed 13 October 2024].
Ministry of Health and Family Welfare, Government of India. Dr. Harsh Vardhan launches Operational Guidelines for integration of Non-Alcoholic Fatty Liver Disease (NAFLD) with NPCDCS;2021. https://www.pib.gov.in/www.pib.gov.in/Pressreleaseshare.aspx?PRID=1699904 [accessed 03 October 2024].
Duseja, A. et al. Clinicopathological profile and outcome of a large cohort of patients with nonalcoholic fatty liver disease from South Asia: Interim results of the Indian consortium on nonalcoholic fatty liver disease. Metab Syndr Relat Disord. 20(3), 166–173. https://doi.org/10.1089/met.2021.0104 (2022).
Shalimar, et al. Prevalence of non-alcoholic fatty liver disease in India: A systematic review and meta-analysis. J. Clin. Exp. Hepatol. 12(3), 818–829. https://doi.org/10.1016/j.jceh.2021.11.010 (2022).
Anton, M. C., Shanthi, B. & Sridevi, C. Prevalence of non-alcoholic fatty liver disease in urban adult population in a tertiary care center, Chennai. Indian J. Commun. Med. 48(4), 601–604. https://doi.org/10.4103/ijcm.ijcm_437_22 (2023).
Asadullah, M. et al. Rural-Urban differentials in prevalence, spectrum and determinants of non-alcoholic fatty liver disease in North Indian population. PLOS ONE. 17(2), e0263768. https://doi.org/10.1371/journal.pone.0263768 (2022).
World Health Organization (WHO). STEPwise approach to NCD risk factor surveillance (STEPS). https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps [accessed 15 December 2022].
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4 (1989).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 24(4), 385–396 (1983) (PMID:6668417).
Maes, I., Ketels, M., Van Dyck, D. & Clays, E. The occupational sitting and physical activity questionnaire (OSPAQ): a validation study with accelerometer-assessed measures. BMC Public Health. 20(1), 1072. https://doi.org/10.1186/s12889-020-09180-9 (2020).
Chobanian, A. V. et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 42(6), 1206–1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2 (2003).
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 363(9403), 157–163. https://doi.org/10.1016/S0140-6736(03)15268-3 (2004).
Singh, Y., Garg, M. K., Tandon, N. & Marwaha, R. K. A study of insulin resistance by HOMA-IR and its cut-off value to identify metabolic syndrome in urban Indian adolescents. J. Clin. Res. Pediatr. Endocrinol. 5(4), 245–251. https://doi.org/10.4274/Jcrpe.1127 (2013).
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. PMID:12485966.
Alam, S. et al. Prevalence of elevated liver enzymes and its relationship with type 2 diabetes mellitus in North Indian adults. Metabol Open. 12, 100130. https://doi.org/10.1016/j.metop.2021.100130 (2021).
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
Kamali, L., Adibi, A., Ebrahimian, S., Jafari, F. & Sharifi, M. Diagnostic performance of ultrasonography in detecting fatty liver disease in comparison with fibroscan in people suspected of fatty liver. Adv Biomed Res. 8(1), 69. https://doi.org/10.4103/abr.abr_114_19 (2019).
Kanwal, F., Neuschwander-Tetri, B. A., Loomba, R. & Rinella, M. E. Metabolic dysfunction-associated steatotic liver disease: Update and impact of new nomenclature on the American Association for the Study of Liver Diseases practice guidance on nonalcoholic fatty liver disease. Hepatology. 79(5), 1212–1219. https://doi.org/10.1097/HEP.0000000000000670 (2024).
Prabhakar, T. et al. High prevalence of MAFLD in general population: A large cross-sectional study calls for concerted public health action. Aliment PharmacolTher. 59(7), 843–851. https://doi.org/10.1111/apt.17892 (2024).
Vagurmekar, P. A. et al. Prevalence of non-alcoholic fatty liver disease (NAFLD) among adults in urban Goa. Natl Med J India. 36, 401–404. https://doi.org/10.25259/NMJI_37_2022 (2023).
Fatty Liver on the rise in Urban and Rural population in the country – Latest survey reports Telangana today.2022 https://telanganatoday.com/fatty-liver-disease-on-rise-in-urban-rural-areas-aig-survey [accessed 24December 2024].
Parimalam EJ, Sudheer S, Babu RR. Women in Indian IT sector: Gender inequality. SELP J Soc Sci, 2024; 15(55).
Schettini, M. A. S., Passos, R. F. D. N. & Koike, B. D. V. Shift work and metabolic syndrome updates: A systematic review. Sleep Sci. 16(2), 237–247. https://doi.org/10.1055/s-0043-1770798 (2023).
Sogabe, M. et al. Association of variabilities in body mass index and waist circumference with newly achieved remission of metabolic dysfunction-associated fatty liver disease. Diabetes MetabSyndr. 18(5), 103036. https://doi.org/10.1016/j.dsx.2024.103036 (2024).
Song, E. et al. Long working hours and risk of nonalcoholic fatty liver disease: Korea national health and nutrition examination survey VII. Front Endocrinol (Lausanne). 12, 647459. https://doi.org/10.3389/fendo.2021.647459 (2021).
Kim, K. et al. Correlation between shift work and non-alcoholic fatty liver disease among male workers in the steel manufacturing company of Korea: a cross-sectional study. Ann. Occup. Environ. Med. 34, e33. https://doi.org/10.35371/aoem.2022.34.e33 (2022).
Meng, R. et al. Analysis of factors affecting nonalcoholic fatty liver disease in Chinese steel workers and risk assessment studies. Lipids Health Dis. 22(1), 123. https://doi.org/10.1186/s12944-023-01886-0 (2023).
Acknowledgements
The University of Hyderabad provided resources such as infrastructure, library and logistics under the Institute of Eminence program of the Ministry of Education, Government of India. BB was the recipient of a non-NET fellowship from University of Hyderabad. NP is the recipient of Project Research Scientist-1 funds from the ICMR project (F. No. 52/10/2020-BIO/BMS). The investigators would like to thank Dr. Barry J. Goldstein, former Vice-President—Drug Development, Labcorp Drug Development and Merck Company for critically reading the manuscript and providing comments. The investigators would like to thank Dr. Pramod Rajaram for discussion on statistics. The investigators would like to thank Mr. Amith Chaudhary, Mr. Danish Quamar and Mr. Govardhan for the recruitment of participants, collection of serum samples and all those who participated in this study.
Funding
This work was supported by the University of Hyderabad – Institute of Eminence program, Ministry of Education, Government of India grant—UoH-IoE-RC5-22–005.
Author information
Authors and Affiliations
Contributions
BB participated in data collection, curation, formal analysis, validation, visualization, writing- original draft, review and editing. PNR, AVK and RV participated in project administration, methodology and investigation. NP participated in writing- original draft, review and editing. CTA participated in investigation, methodology, project administration, resources, funding acquisition, supervision, validation, visualization, writing the original draft, review and editing. KM participated in conceptualisation, funding acquisition, investigation, methodology, project administration, data curation, formal analysis, resources, supervision, validation, visualization, writing the original draft, review and editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Ethics Committee (IEC) of the University of Hyderabad (approval number: UH/IEC/2022/412) and Asian Institute of Gastroenterology Hospital, Hyderabad (approval number: AIG/IEC-BH&R43/03.2023-06). Participation in the study was voluntary and there were no financial incentives. As a benefit to participants, their biochemical and FibroScan test reports were shared with them, providing health insights without compromising the integrity of the study. Written informed consent obtained from all the participants.
Consent for publication
Consent for publication obtained from all the study participants.
Availability of data and materials
The data used in this study are presented here. The raw data underlying this article cannot be shared publicly because of privacy concerns of the participants and the legal regulations of the Institutional Ethical Committee of the University of Hyderabad and the Asian Institute of Gastroenterology. Raw data were stored and analysed only on designated computers at the University of Hyderabad. The data that support the findings of this study are available from the corresponding authors, KM and CTA, upon reasonable request.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bhargava, B., Rao, P.N., Kulkarni, A.V. et al. Prevalence of metabolic dysfunction-associated fatty liver disease among information technology employees in India. Sci Rep 15, 10124 (2025). https://doi.org/10.1038/s41598-025-91482-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91482-2