Abstract
Atopic dermatitis (AD) is a chronic inflammatory skin condition that significantly impacts patients’ quality of life and imposes substantial economic burdens due to direct medical costs and indirect costs such as absenteeism and loss of productivity. This study aimed to quantify the economic impact of AD in Portugal. A cross-sectional study was conducted on AD-diagnosed Portuguese residents using a 70-question survey, distributed between June 2019 and January 2020, including DLQI, EQ-5D, and VAS scales, to assess AD’s 12 months impact. Statistical analysis included univariate and bivariate methods with post-stratification by disease severity. Findings revealed a mean DLQI score of 9.4 and a 24% productivity loss equating to 50 workdays annually. The economic impact calculated from the participation in the labor market totaled €1.477 million, including €43 million from absenteeism, €1.295 million from presenteeism, and €139 million of missed days by family members. The economic value of time spent treating the disease amounts to €311 million. The total annual cost of treating the disease is shared between the NHS (€218 million) and the patient out-of-pocket cost (€800 million). These results highlight AD’s significant economic burden in Portugal, underscoring the need for comprehensive strategies to improve disease management, access to dermatological care, and quality of life. This study emphasizes the importance of investing in AD health services and promoting access to effective treatments to achieve economic and societal benefits.
Similar content being viewed by others
Introduction
Atopic dermatitis (AD), also known as eczema, is the most common chronic inflammatory skin disease affecting both infants and adults, with approximately 80% of cases beginning in infancy or childhood1,2. Its manifestation is particularly diverse, with symptoms including sensitive, dry skin, eczematous lesions, and intense itching, all of which have a significant impact on patients’ quality of life1,3,4. AD has a strong heritability component and is associated with other atopic disorders such as food allergy, asthma, and allergic rhinitis, and it frequently marks the beginning of the “atopic march” that leads to later allergic conditions3,5.
While its exact cause remains unknown, a combination of skin barrier defects, environmental and infectious agents, and immunological dysregulation seem to contribute to AD manifestations3,6. Its treatment typically involves a complex multimodal approach that targets both skin barrier restoration and immunological dysregulation, highlighting the importance of effective and accessible approaches to alleviate symptoms and improve overall health of those who suffer from these disease1,3.
Over the past three decades, there has been a notable increase in AD prevalence, presenting a substantial challenge for healthcare systems worldwide2. According to the Global Report on Atopic Dermatitis 2022, AD affects approximately 20% of children and 10% of adults7. The burden of this disease ranks 15th globally for non-fatal diseases and first for skin diseases based on disability-adjusted life years (DALYs)7,8. In Europe, AD affects 8.4–18.6% of children and adolescents and 4.4% of people over the age of 187, which is consistent with Portugal’s reality, where the prevalence of AD in the adult population is also reported to be around 4.4%9.
Beyond the physical implications of the disease, AD has a substantial impact on patients’ emotional and psychological well-being, often called humanistic burden10,11,12. The visible symptoms of AD, along with stigma and itching, worsen the condition, causing social isolation and discomfort, ultimately contributing to unfavorable psychosocial repercussions2,4. In turn, emotional factors, stress, and sleep deprivation are also reported triggers for AD symptoms, potentially leading to decreased work/school productivity and increased absenteeism6,7,11.
Moreover, the significant economic burden of AD cannot be overlooked. The annual costs per patient can range from €1572 to €6993 in some European countries per year13,14. However, these expenses seem to vary depending on the health system used, the severity of the disease and how it is managed7,15,16. The overall annual costs of adult moderate-to-severe AD in Europe is estimated to be €30 billion11. These costs include both direct costs, such as expenses for medications, medical consultations, and complementary treatments, and indirect costs due to presenteeism, absenteeism and loss of work11.
When socioeconomic differences are considered, these impacts become even more complex8,17,18. These differences significantly influence access to appropriate healthcare, exposure to environmental triggers, and access to preventative and self-care education6.
The global socioeconomic impact of AD is a noticeable public health issue that requires attention given the substantial and increasing burden it represents on both patients and the economy8,11,17,19. It is therefore necessary to recognize AD as a significant health problem and to raise awareness among policymakers, health professionals and payers of its long-term financial and humanistic implications. Although the impact of this disease on health and quality of life has been gaining growing interest, there is clearly a lack of research about its economic impacts20,21,22,23. In particular, these economic effects have been mostly unknown in Portugal.
Hence, conducting comprehensive economic analyses is crucial for assessing the impact of AD on the labor market and society. These analyses facilitate the development of health policies and optimizing resource allocation, enabling stakeholders to make well-informed decisions21. By addressing the evident gap in the Portuguese context about this subject, this research not only provides valuable local insights but also establishes a benchmark for Europe and beyond. This paper, therefore, focuses on quantifying the economic impact of AD on patients and society within Portugal.
Results
Demographic characterization of the study population
A total of 204 valid questionnaire responses were collected, with a mean age of 31 years old and a proportion of 64% of females. The sociodemographic characteristics of the participants, categorized by self-reported disease severity, are presented in Table 1.
Dermatology life quality index—DLQI
73% of participants scored 6 or higher on DLQI, with 36% scoring above 10, resulting in an average score of 9.4. The average score was 6.6 for light cases, 12.3 for moderate and 18.7 for severe forms of the disease, with statistically significant severity effect over DLQI (Pr > F < 0.001).
Employment situation
Around 64% of respondents are employed, and 13% missed at least one working day in the previous year due to AD. Mean number of missed working days is 2.
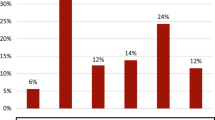
The impact of AD on productivity and absenteeism varies significantly with disease severity. In severe cases, productivity losses (presenteeism) reach 47.5%, equivalent to approximately 109 missed working days annually, and 9 lost days due to absenteeism. Moderate cases show a productivity loss of 37.9%, corresponding to 87 missed working days and 3 days of absenteeism. In contrast, mild cases demonstrate much lower productivity losses at 11.1% (about 26 days lost) and minimal absenteeism (1.5 days annually). Globally, AD leads to a productivity loss of 23.1% across all severities, translating to approximately 53 missed working days annually and an absenteeism of 2.3 days (Table 2). It is noticeable that at any severity level the impact of AD on productivity is significantly larger than the one on absenteeism.
The economic burden of AD in Portugal, considering absenteeism and productivity losses at an estimated daily work cost of €79, could amount to €43 million, with productivity losses alone contributing €1.295 million (Fig. 1). Severe cases represent the greatest share of this burden due to their disproportionately higher productivity losses (Table 2).
Annual economic impact of missed workdays due to Atopic Dermatitis (AD). This figure illustrates the annual economic impact of lost workdays due to AD, encompassing costs attributed to absenteeism, reduced productivity (presenteeism), and the involvement of family members. It summarizes the overall economic impact through labor market participation in terms of wages, with additional consideration given to productivity losses.
AD also significantly impacts students and families. Students with severe AD miss an average of 4 school days annually, while those with moderate AD miss around 3 days. Family members providing support for individuals with severe AD experience an average of 4 days of absenteeism, adding to the indirect economic burden. Collectively, these additional costs of family members contribute to an additional economic impact of €139 million annually (Fig. 1). These findings highlight the substantial individual, social, and economic burdens of AD, particularly in severe cases (Table 2).
As a result, considering an estimated prevalence of 440.000 patients with AD in Portugal24, the annual economic impact measured through the participation in labor market is €1.477 million through wages. Considering the relationship between productivity and cost of work, i.e. potential loss of added value due to the missed working days, the economic impact of the disease thorough the labor market amounts to €2.216 million (Fig. 1).
Healthcare systems
Public sector - NHS
It was estimated that 39% of the population used the NHS to treat their AD. Of these, 93% scheduled appointments, while only 16% used emergency care (Table 3).Scheduled appointments were predominantly with general practitioners (74%), followed by dermatologists (60%) and allergists (25%). The average waiting time for dermatology appointments was 4 months, and for allergology appointments, it was 2 months (Table 3).Scheduled appointments cost an average of €97 and take 9 h per year, whereas emergency appointments cost €18 and take about 4 h (including travel time) (Table 3).Overall, considering travel to healthcare facilities, patients spent €163 on transportation expenses (Table 3).
Private sector
The estimate of the proportion of patients that used the private health system to treat their AD is 50%. The main reasons provided were “shorter waiting times” (86%), “convenience” (53%) and “choice of health professional” (49%). Dermatology was the specialty most frequently accessed (94%), followed by allergology (22%). All respondents using the private health system had doctor’s appointments and only 5% used emergency services (Table 3). The yearly cost of these appointments was €165, with a total duration of 5 h per consultation (including travel time). The cost with the use of emergency services is €33 per year and a time loss of just 2 h (Table 3).Travel expenses for health services amount to €65 (Table 3).
Medicines and complementary treatments
The average cost out-of-pocket per year of these patients with medicines is €797. Additionally, patients report significant costs with complementary therapies not classifiable and health products or services (e.g. Gloves, special clothing, phototherapy, special detergent, bandages) leading to an average of €480 per per year (Fig. 3).
AD-related costs
The economic impact of time spent with AD is estimated to be €311 million per year. This estimate includes the time spent in consultations and emergency care, both in the public and private sectors, as well as the hours spent caring for AD every day, such as applying creams. On average, each patient dedicate approximately 267 h per year (equivalent to 12 days) to managing AD (Fig. 2).
Time and Economic Burden of Atopic Dermatitis (AD) on Patients. This figure illustrates the cumulative time spent by AD patients on healthcare appointments and personal care, contributing to the total economic burden of the disease. Time invested includes 9 h for NHS appointments and 4 h for emergency visits, and 5 h for appointments and 2 h for emergencies in the private sector, alongside 267 h annually dedicated to managing AD at home (e.g., applying creams). Each patient spends an average of 287 h (equivalent to 12 days) per year on AD-related care. This time commitment translates to an estimated economic impact of €311 million per year, calculated through the marginal cost of patients’ time.
The yearly costs out-of-pocket per patient in health products and services is €1100. These costs include consultations, emergencies, and medication, resulting in a total annual expenditure on AD of around €488 million.
Considering additional expenses related to traveling and complementary therapies, the total expenditure per patient amounts to €1818, leading to a total annual cost of €800 million (Fig. 3).
Total costs of patients with Atopic Dermatitis (AD). This figure illustrates the comprehensive costs associated with AD for patients. It includes expenses such as consultations, emergency care, travel to access services in both public and private sectors, as well as costs for medications and complementary treatments. Each patient bears annual costs of €1,818 for health products and services, contributing to a total annual expenditure of €800 million.
Furthermore, the NHS’s estimated costs for AD are around €218 million per year, which includes consultations, emergencies, and co-participation in medications (Fig. 4).
Total costs of National Health Service (NHS) with Atopic Dermatitis (AD). This figure illustrates the comprehensive costs associated with AD for the NHS. It includes expenses such as consultations, emergency care and co-participation in medications. NHS expenditures for AD are estimated at €218 million per year.
These findings offer valuable insights into the direct costs associated with health products and services for the treatment of AD for patients and the NHS, estimated at around €706 million per year, being the balance of the costs of 69% for the patient and 31% for the NHS. When including the additional costs with other products and services the annual cost rises to €1.018 million, with an even more unbalanced distribution (79% for the patient and 21% for the NHS). Contrary to what happens with other diseases, AD is clearly a disease where the economic burden is mostly on the side of the patient. This is partially explained due to the significant use of private sector and the cost of complementary treatments not supported by NHS.
Economic impact
The economic impact of the disease may be assessed under different perspectives. The impact obtained through the participation in the labor market (absenteeism and presenteeism) was already established in €1.477 million. Of course, there is an economic value that may be attributed to the degradation of health status and quality of life that affects all patients independently of their level of participation in the labor market. We have assessed this value using the yearly willing to pay, i.e. the yearly economic value that patients would be willing to spend in order to avoid the disease and its symptoms. We have estimated an average willing to pay 3117 per patient, leading to a total economic value of €1359 million.
Discussion
In this study, we have carried out an assessment of the economic burden of AD on patients and society, with a specific focus on its impact on Portuguese labor market. The study reinforces that AD is a disease with a significant impact on patients’ quality of life, affecting personal and professional lives, resulting in a substantial economic repercussion for both the Public Healthcare System and the patients, but also to society in general. This contradicts some general perceptions in society that tend to underestimate this disease25,26,27.
It is estimated that AD costs patients and the NHS approximately one thousand million Euros annually. This value includes healthcare products and services (such as emergencies, appointments, and medications), as well as travel expenses and complementary treatments. A significant portion of this cost is assumed entirely by patients (€800 million). The impact of this chronic inflammatory skin disease on Portuguese society also includes indirect costs related to absenteeism and loss of productivity, estimated at €1.477 million (when including impacts to family members and friends). The prevalence of reduced productivity due to AD highlights the hidden costs of presenteeism, despite the low rates of absenteeism recorded. These figures accentuate the substantial impact that this disease has on both the economy and the well-being of those affected12,28.
The total costs of AD are also the subject of analysis in other European studies on the burden of disease and the cost of illness. For example, a German study reported annual costs (including treatment, complementary therapies, travel costs and indirect costs) of €1,466 for mild AD and €5,229 for moderate to severe AD29. On the other hand, a Dutch cohort study revealed higher direct costs of €15,23130, and a French study found average outlay costs of €462.1 for severe AD and €247.4 for moderate AD31. In Spain, annual costs reached €9.3 million of which 75.5% were health care costs and 24.5% non-health care costs (loss of productivity), which is consistent with our result of 24% productivity loss13. Likewise, the costs of a Hungarian study of €1,881 per patient per year are also similar to ours28. While our study’s average costs align with the European average, it’s important to recognize the specific nuances of each healthcare system when interpreting and comparing results, given the variability in healthcare systems and general price levels across countries.
Disparities in waiting times and costs between public and private healthcare sectors exacerbate the issue. Our findings suggest that individuals accessing public healthcare experience longer waits and higher financial burdens compared to those utilizing private sector services. About 70% of respondents resort to the private sector due to AD, citing shorter waiting times for appointments—eight times faster than in the NHS, particularly in dermatology. These discrepancies highlight systemic issues within healthcare systems, including resource distribution and access to specialized care32. Access to care for AD patients is challenging due to the disorder’s chronic nature and high healthcare needs21,33. AD patients often delay care due to costs and face longer hospital stays21. The introduction of expensive biologic treatments for severe cases could exacerbate access challenges over time21. Addressing these disparities is crucial to ensure equitable and timely access to dermatological services, reducing delays in effective treatment, mitigating condition severity, and improving health and economic outcomes32,34.
The cost burden to the patients is very significant (80%) when compared to NHS costs. These unbalanced costs are surely tributary from the need the many patients feel to use the private systems due a lack of response in the NHS, but also the need to purchase different products and services that are not considered P&S health and do not have a public co-participation35,36. Simultaneously, out-of-pocket costs can significantly affect household budgets, varying depending on the patient’s insurance status and disease severity14,37,38.
Overall, AD imposes significant economic burdens in Portugal, requiring comprehensive strategies for improved disease management, access to dermatological care, enhanced quality of life and work performance.
Strengths and limitations
One major limitation of this study is the sample size, which, while sufficient for estimating population characteristics (average DLQI with 1.1 points accuracy at a 95% confidence level), could be inadequate for accurately estimating characteristics with more than three categories. Another limitation is the use of a cross-sectional design instead of a longitudinal one, which would better measure changes over time. Additionally, the reliance on self-reported data, though mitigated by detailed definitions and a support line, is another limitation.
However, a key strength of this study is its detailed analysis of the economic and quality of life impacts of AD on patients. By quantifying direct and indirect costs, including personal expenses, absenteeism, and productivity loss, the study provides a comprehensive understanding of the financial burden of AD. This robust quantitative approach supports arguments for policy changes and better resource allocation in healthcare. Moreover, these findings offer valuable insights for future cost-effectiveness evaluations and contribute to the development of patient-centered policies aimed at reducing costs and improving quality of life—an area previously overlooked in adult AD research in Portugal.
Implications of the results for clinical practice, policy, and future research
The disparities between public and private healthcare sectors, particularly the prolonged waiting times in the public sector, exacerbate the financial and health burdens on patients. This calls for systemic improvements in resource allocation, access to care, and the efficiency of the public healthcare system to ensure equitable and timely treatment for all patients. Ensuring fair and equitable access to healthcare for patients with AD, particularly dermatology consultations, is crucial regardless of the healthcare system used.
The reliance on private healthcare highlights a critical issue of inequity in healthcare access. Addressing these disparities is crucial to ensure all patients have fair access to necessary dermatological services, thereby reducing delays in treatment and improving health outcomes. AD imposes a substantial economic burden, with direct and indirect costs estimated to exceed one thousand million Euros annually. The significant personal expenditure (€800 million) and the extensive costs related to absenteeism and loss of productivity (€1.477 billion) found in this study highlight the extensive financial strain on patients and society. Comprehensive strategies to manage and mitigate these costs effectively are necessary, emphasizes the need to invest in preventative measures, allocate resources and implement effective treatments to mitigate its impact on health systems and the economy.
The study also emphasizes the significant impact of AD on patients’ quality of life, affecting both personal and professional aspects. The hidden costs of presenteeism, despite low absenteeism rates, highlight the need for supportive workplace policies and interventions to maintain productivity and minimize the disease’s impact on work performance. The positive ROI from treating AD, as indicated by the societal perspective, reinforces the importance of viewing healthcare expenditures not just as costs but as investments with significant returns in terms of improved health and economic productivity.
These findings provide a strong basis for advocating for policy changes and healthcare reforms aimed at better managing AD. Policies should focus on reducing patient out-of-pocket expenses, improving public healthcare response times, and enhancing overall access to care.
For future research, there is potential to expand the study to focus on pediatric patients and explore the economic value of successful therapeutic strategies. Following up with a longitudinal sample could validate results and provide insights into successful management pathways. Extending the research to other dermatological diseases with significant impacts would broaden the understanding of their economic and quality of life impacts.
Methods
Study design, study population and questionnaire
We conducted a cross-sectional study with a quantitative approach. The questionnaire was distributed between June 2019 and January 2020, both in print and online, targeting Portuguese residents diagnosed with AD. The study only included patients (adults and non-adults) diagnosed by a medical specialist. The sample was collected from the database of patients registered with the National Atopic Dermatitis Association (ADERMAP), and patients were encouraged to share the questionnaire with others. Data were also collected through a sample of dermatologists that disseminated the questionnaire.
To assess the self-reported impacts of AD on affected patients, we developed a 70-question survey comprising seven main themes with “sub-questions” covering the following topics: sociodemographic characteristics, disease characterization, daily life impact, employment situation, healthcare system (public and private sectors) and treatment strategy.
The rating instruments were developed in collaboration with AD medical specialists and incorporated metrics validated in previous studies, including the Dermatology Life Quality Index—DLQI39 and EQ-5D40 scales, along with the Visual Analog Scale (VAS), all previously validated in Portuguese41,42. Patients answered considering the previous 12 months.
The questionnaire was pre-tested in a convenience sample of 20 AD medical specialists from Portuguese Society of Dermatology and Venerology (SPDV). Accordingly, the changes suggested by the experts were incorporated to improve the clarity and validity of the survey questions.
In order to increase response rate and mitigate possible non-response bias the data collection used up to 3 callbacks to non-responds.
Respondents were informed about the context and objectives of the study and were asked to provide voluntarily consent for their participation. Informed consent was obtained from all subjects and/or their legal guardian(s).
This research was approved by NOVA IMS ethical committee. All methods used in this research are in line with relevant guidelines and regulations, particularly the ethical principles in the declaration of Helsinki.
For the purposes of this economic analysis, this article will focus solely on questionnaire topics relating to employment situation, as well as different types of costs and economic impacts of the disease.
Data sources
The National Statistics Institute (INE) provided official data on the economic worth of working days. Costs for the Portuguese National Health Service (NHS) (public sector) were derived from official data provided by the Central Administration of the Health System (ACSS). The average cost of medicines was determined using data from the National Institute of Pharmacy and Medicines (INFARMED) and recommended dosages provided by specialists. Additional data was self-reported by respondents.
Data analysis
Univariate and bivariate analysis consisting in estimates of central tendency measures and frequency distribution for key variables was performed. Estimation weights were based on post-stratification by disease severity. All continuous variables were expressed using means, while categorical variables were expressed using proportions. Group effects over means were tested using F tests associated with one-way ANOVA.
The annual economic impact of absenteeism and presenteeism due to AD was calculated based on daily average income in Portugal obtained from INE, combined with the declared working missed days and loss of productivity.
The AD-related costs results were obtained using data provided by respondents and reference values obtained from ACSS, INFARMED and Base.Gov.
Data were analyzed using Statistical Analysis System software.
Data availability
The data used in this study are available upon request. Researchers interested in accessing the data can contact the corresponding author (A.S.C) for further information (acunha@novaims.unl.pt).
References
Bieber, T. Atopic dermatitis: an expanding therapeutic pipeline for a complex disease. Nat. Rev. Drug Discov. 21, 21–40 (2022).
Langan, S. M., Irvine, A. D. & Weidinger, S. Atopic dermatitis. Lancet 396, 345–360 (2020).
Kapur, S., Watson, W. & Carr, S. Atopic dermatitis. Allergy Asthma Clin. Immunol. 14, 52 (2018).
Coelho, P. S. et al. The burden of atopic dermatitis in Portuguese patients: an observational study. Sci. Rep. 14, 5181 (2024).
Weidinger, S., Beck, L. A., Bieber, T., Kabashima, K. & Irvine, A. D. Atopic dermatitis. Nat. Rev. Dis. Primers. 4, 1 (2018).
Jelousi, S., Sharma, D., Alexis, A. & Murase, J. E. The impact of global health disparities on atopic dermatitis in displaced populations: narrowing the health equity gap for patients with skin of color. Dermatol. Ther. (Heidelb). 12, 2679–2689 (2022).
House, W. Global Report on Atopic Dermatitis 2022. www.atopicdermatitisatlas.org. (2022).
Xue, Y. et al. Global burden, incidence and Disability-Adjusted Life-Years for dermatitis: A systematic analysis combined with socioeconomic development status, 1990–2019. Front. Cell. Infect. Microbiol. 12, 1–10 (2022).
Carvalho, D., Aguiar, P., Ferrinho, P., Mendes-Bastos, P. & Palma-Carlos, A. Eczema and urticaria in the adult population in Portugal: a prevalence study. Actas Dermo-Sifiliográficas (English Edition). 110, 744–751 (2019).
Luger, T. et al. Clinical and humanistic burden of atopic dermatitis in Europe: analyses of the National health and wellness survey. Dermatol. Ther. (Heidelb). 12, 949–969 (2022).
Augustin, M. et al. Unveiling the true costs and societal impacts of moderate-to‐severe atopic dermatitis in Europe. J. Eur. Acad. Dermatol. Venereol. 36, 3–16 (2022).
Fasseeh, A. N. et al. Burden of atopic dermatitis in adults and adolescents: a systematic literature review. Dermatol. Ther. (Heidelb). 12, 2653–2668 (2022).
Sicras-Mainar, A., Navarro-Artieda, R. & Carrascosa Carrillo, J. M. Impacto económico de La dermatitis atópica En Adultos: estudio de base poblacional (estudio IDEA). Actas Dermosifiliogr. 109, 35–46 (2018).
Ariëns, L. et al. Economic burden of adult patients with moderate to severe atopic dermatitis indicated for systemic treatment. Acta Derm. Venereol. 99, 762–768 (2019).
Sicras-Mainar, A., Navarro-Artieda, R. & Carrascosa Carrillo, J. M. Economic impact of atopic dermatitis in adults: A Population-Based study (IDEA study). Actas Dermo-Sifiliográficas (English Edition). 109, 35–46 (2018).
Simpson, E. L. et al. Association of inadequately controlled disease and disease severity with Patient-Reported disease burden in adults with atopic dermatitis. JAMA Dermatol. 154, 903 (2018).
Bajwa, H. et al. Mixed evidence on the relationship between socioeconomic position and atopic dermatitis: A systematic review. J. Am. Acad. Dermatol. 86, 399–405 (2022).
Perry, T. T., Grant, T. L., Dantzer, J. A., Udemgba, C. & Jefferson, A. A. Impact of socioeconomic factors on allergic diseases. J. Allergy Clin. Immunol. 153, 368–377 (2024).
Chung, J. & Simpson, E. L. The socioeconomics of atopic dermatitis. Ann. Allergy Asthma Immunol. 122, 360–366 (2019).
Sach, T. H., McManus, E. & Levell, N. J. Understanding economic evidence for the prevention and treatment of atopic eczema. Br. J. Dermatol. 181, 707–716 (2019).
Adamson, A. S. The Economics Burden of Atopic Dermatitis. in Advances in experimental medicine and biology vol. 1027 79–92 (2017).
Birdi, G., Cooke, R. & Knibb, R. C. Impact of atopic dermatitis on quality of life in adults: a systematic review and meta-analysis. Int. J. Dermatol. 59, e75–e91 (2020).
Drucker, A. M., Wang, A. R. & Qureshi, A. A. Research gaps in quality of life and economic burden of atopic dermatitis. JAMA Dermatol. 152, 873 (2016).
Barbarot, S. et al. Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy 73, 1284–1293 (2018).
Silverberg, J. I. et al. Patient perspectives of atopic dermatitis: comparative analysis of terminology in social media and scientific literature, identified by a systematic literature review. J. Eur. Acad. Dermatol. Venereol. 36, 1980–1990 (2022).
Magin, P. J., Pond, C. D., Smith, W. T., Watson, A. B. & Goode, S. M. Correlation and agreement of self-assessed and objective skin disease severity in a cross‐sectional study of patients with acne, psoriasis, and atopic eczema. Int. J. Dermatol. 50, 1486–1490 (2011).
Wei, W. et al. Discordance between Physician- and Patient-Reported disease severity in adults with atopic dermatitis: A US Cross-Sectional survey. Am. J. Clin. Dermatol. 18, 825–835 (2017).
Beretzky, Z. et al. Societal costs and health related quality of life in adult atopic dermatitis. BMC Health Serv. Res. 23, 859 (2023).
Mohr, N. et al. Cost-of‐illness of atopic dermatitis in Germany: data from dermatology routine care. J. Eur. Acad. Dermatol. Venereol. 35, 1346–1356 (2021).
Thyssen, J. et al. Societal costs of Moderate-to-severe atopic dermatitis occurring in adulthood: A Danish Register-based study. Acta Derm. Venereol. 101, adv00538 (2021).
Launois, R. et al. Importance of out-of‐pocket costs for adult patients with atopic dermatitis in France. J. Eur. Acad. Dermatol. Venereol. 33, 1921–1927 (2019).
Yardman-Frank, J. M. & Nambudiri, V. Ending the pandemic of inaccessibility in dermatology. Clin. Dermatol. 41, 280–283 (2023).
Manjelievskaia, J. et al. The direct and indirect costs of adult atopic dermatitis. J. Manag Care Spec. Pharm. 27, 1416–1425 (2021).
Lee, H., Kim, D., Lee, S. & Fawcett, J. The concepts of health inequality, disparities and equity in the era of population health. Appl. Nurs. Res. 56, 151367 (2020).
Wan, G. & Wang, Q. Two-tier healthcare service systems and cost of waiting for patients. Appl. Stoch. Models Bus. Ind. 33, 167–183 (2017).
Chovatiya, R., Begolka, S., Thibau, W., Silverberg, J. & I. & Atopic dermatitis polypharmacy and Out-Of-Pocket healthcare expenses. J. Drugs Dermatol. 22, 154–164 (2023).
Zink, A. et al. Out-of-pocket costs for individuals with atopic eczema: A Cross-sectional study in nine European countries. Acta Derm. Venereol. 99, 263–267 (2019).
Chovatiya, R., Begolka, W. S., Thibau, I. J. & Silverberg, J. I. Impact and associations of atopic dermatitis Out-of-Pocket health care expenses in the united States. Dermatitis 33, S43–S51 (2022).
FINLAY, A. Y. & KHAN, G. K. Dermatology life quality index (DLQI)-a simple practical measure for routine clinical use. Clin. Exp. Dermatol. 19, 210–216 (1994).
Rabin, R. & de Charro, F. EQ-SD: a measure of health status from the EuroQol group. Ann. Med. 33, 337–343 (2001).
Martins, G. A., Arruda, L. & Mugnaini, A. S. B. Validação de questionários de Avaliação Da qualidade de Vida Em Pacientes de psoríase. Bras. Dermatol. 79, 521–535 (2004).
Ferreira, P. L., Ferreira, L. N. & Pereira, L. N. Contributos Para a Validação Da Versão Portuguesa do EQ-5D. Acta Med. Port. 26, 664–675 (2013).
Acknowledgements
The study was conducted with the support SPDV and ADERMAP and was funded by Sanofi.
Funding
This work was supported by national funds through FCT (Fundação para a Ciência e a Tecnologia), under the project UIDB/04152/2020 (DOI: https://doi.org/10.54499/UIDB/04152/2020) - Centro de Investigação em Gestão de Informação (MagIC)/NOVA IMS.
Author information
Authors and Affiliations
Contributions
P.S.C., J.M.S. and G.V. jointly designed the study, contributed to the design and implementation of the data collection model. A.S. C. and P.S.C. were primarily responsible for drafting the manuscript, with contributions from G.V.P.S.C. supervised the analysis of the data. A.S.C. and P.S.C. generated insights based on the analytic model. All authors contributed to reviewing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cunha, A.S., Vitorino, G., Silva, J.M.e. et al. Economic burden of atopic dermatitis in Portugal: a cross-sectional study. Sci Rep 15, 7717 (2025). https://doi.org/10.1038/s41598-025-91896-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91896-y