Abstract
Sustained engagement and promotion by healthcare professionals are essential for the advancement of telemedicine. Post coronavirus disease 2019 (COVID-19) pandemic, the preference for in-person care highlights the need for research on healthcare professionals’ sustained telemedicine attitudes. This study assessed healthcare professionals’ continued willingness to participate in and recommend telemedicine post-pandemic and identified factors influencing their decisions. From September to October 2023, a cross-sectional study was conducted among 560 healthcare professionals, with samples recruited from 230 hospitals across 11 provinces in China using a multi-stage sampling method. Overall, 518 (92.5%) of 560 respondents expressed their willingness to continue participating in telemedicine, and nearly all respondents (93.5%) displayed a willingness to recommend telemedicine to those in need. The results showed that perceived usefulness, subjective norms, patient coverage, and satisfaction were positively associated with healthcare professionals’ willingness to continue participating in and recommend telemedicine. Satisfaction and subjective norms play a partial mediating role in the effect of usefulness on willingness to continue participating in and recommend telemedicine. Patient coverage partially mediates relationship between usefulness and willingness to recommend telemedicine. Chinese healthcare professionals exhibited a generally high level of willingness to continue participating in and to recommend telemedicine. To further enhance this willingness, it is essential to improve their perceptions of telemedicine’s usefulness, increase their satisfaction with the technology, and emphasize the roles of subjective norms. Moreover, broadening patient access to telemedicine services will be crucial in promoting healthcare professionals’ recommendations.
Similar content being viewed by others
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) has significantly sped up the rapid development and deployment of telemedicine, both in China and globally1,2,3. Amidst the global health crisis, telemedicine has promptly emerged as a crucial adjunct to medical services, owing to its convenience, safety, and efficiency4,5. It effectively reduces the risk of virus transmission by minimizing direct contact between patients and healthcare facilities6, highlighting its enormous potential and importance in the healthcare industry.
Telemedicine in China began in the mid-1980s, and its development was greatly accelerated following the release of the “Opinions on Promoting Telemedicine Services in Medical Institutions” by the Chinese government in 20147. Since then, a series of policies have been introduced to further promote telemedicine, with the goal of improving primary healthcare and medical conditions in remote areas8. In the post-pandemic era, telemedicine in China is advancing from a provisional solution to a staple of healthcare delivery9. An increasing number of medical institutions are beginning to incorporate telemedicine into their daily operations, offering patients more convenient, efficient, and personalized healthcare services10,11,12. By 2023, telemedicine services have covered all residents in Chinese prefecture-level cities13. This not only caters to the varied medical needs of patients and improves medical resource utilization but also provides expanded avenues for career growth within medical institutions and for their staff11.
Healthcare professionals play a vital role in telemedicine services. They serve as the crucial connection between patients and medical resources, employing their knowledge and technological skills to offer timely and effective medical advice, diagnoses, and treatment recommendations14. The continuous involvement of healthcare professionals is crucial to ensuring the sustained and stable development of telemedicine15. Previous research indicates that a lack of understanding, insufficient awareness, and limited technological skills and experience may hinder healthcare professionals from adopting telemedicine16,17. During the COVID-19 pandemic, the widespread application and remarkable effectiveness of telemedicine heightened healthcare professionals’ awareness of it18, and these constraints are expected to have a significantly reduced impact on their participation in telemedicine.
While the pandemic accelerated global telemedicine adoption, healthcare professionals’ willingness to continue engaging in telemedicine post-pandemic varies across healthcare systems worldwide. In some countries and regions, healthcare professionals have shown increased interest in telemedicine19,20. However, challenges persist in many countries, particularly the continued preference for in-person consultations among both healthcare professionals21 and the public22, primarily due to the limitations of telemedicine in fully assessing patient conditions. This variation highlights the need to understand the unique characteristics of the Chinese healthcare system in the context of telemedicine adoption.
A significant amount of previous research has examined patients’ perspectives on telemedicine participation and usage23,24,25, while relatively little attention has been given to healthcare professionals’ involvement, particularly concerning their sustained willingness to engage in telemedicine in the post-pandemic era. Given the continuous advancement of telemedicine technologies and the broadening of their application scenarios, there is an increasing importance in examining the experiences and perceptions of healthcare professionals during the utilization of telemedicine technologies. It is essential to comprehend their willingness to engage in telemedicine services and to analyze the factors that either facilitate or impede their engagement. This understanding is pivotal for optimizing the quality of telemedicine services and for propelling their further advancement.
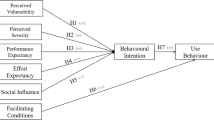
Therefore, the purpose of this study is to explore healthcare professionals’ willingness to engage in telemedicine in the post-pandemic era, with a focus on their willingness to continue participating in and recommend telemedicine, and to further analyze the potential influencing factors. To ensure a comprehensive understanding of the variables that may affect patients’ perspectives on telemedicine, this study adopted the extended Technology Acceptance Model (TAM)26 and the Theory of Planned Behavior (TPB)27 as conceptual frameworks, while considering the impact of telemedicine on patient accessibility. These models are frequently employed in evaluating the adoption and acceptance of technological innovations by users.
Methods
Study design and setting
The 2023 Chinese National Survey of Telemedicine Development in Hospitals (CNSTDH) was conducted from September to October 2023 across 230 hospitals in 11 provinces in China to investigate the current status of telemedicine development. Data for the survey were collected through a joint effort between the Telemedicine Informationization Professional Committee of China (TIPC) and the National Telemedicine Center of China (NTCC). This study, part of the 2023 CNSTDH, specifically focused on examining the willingness of healthcare professionals to continue engaging in telemedicine services post-pandemic. In this study, “healthcare professionals” refers to a broad range of roles, including doctors, medical technologists, and public health practitioners, all of whom play a role in the delivery of healthcare services. The study primarily focused on general medicine, with a smaller proportion of participants from specialties such as psychiatry, neurology, or dermatology. Telemedicine is discussed not only in the context of patient visits (e.g., remote consultations) but also in relation to other interactions, such as remote diagnosis, remote surgical guidance, and remote teaching.
A multi-stage sampling method was employed to recruit the respondents. First, eleven survey provinces were purposefully chosen from the eastern, central, and western regions based on previous collaborative efforts. Then, one TIPC member from each province was selected to oversee the survey process, with responsibility for both hospital selection and coordination. In terms of hospital sampling, we referred to the overall distribution of hospitals in China in 202328. Given the importance of tertiary hospitals in telemedicine, we emphasized their representation and also allowed flexibility for each provincial TIPC member to adjust the proportion of tertiary hospitals based on local conditions, ensuring balanced and adaptable representation across hospital levels. After obtaining consent from selected hospitals, a staff member was assigned to each hospital by TIPC members to manage participant recruitment, and all of these staff members were trained by three experienced researchers from NTCC. Finally, electronic questionnaires, along with quick-response codes and instructions, were distributed by staff members in each hospital to healthcare professionals participating in telemedicine services. Participation was voluntary, allowing participants to withdraw at any time. Anonymity and confidentiality of data were ensured, and no financial compensation was provided. Researchers from NTCC periodically reviewed data during the survey, provided timely feedback, and conducted unified data cleaning afterward to ensure the effectiveness of the data.
Sample size was calculated using the standard formula for a cross-sectional study29:
With a 95% confidence interval (Zα/2 = 1.96), a margin of error of 5%, and a response rate of 50%, a sample size of 385 healthcare professionals was determined. Considering a 10% potential for non-response or invalid questionnaires, the minimum required sample size was set at 424 participants.
Data collection
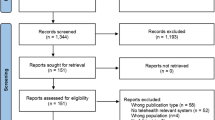
According to the 2023 CNSTDH, TIPC members reported that, in total, 1200 healthcare professionals were initially contacted by the staff members and themselves through WeChat, telephone, and text message. Finally, a total of 996 questionnaires were received, with a response rate of 83.0%. After excluding 135 invalid questionnaires due to incomplete responses, highly repetitive answers, or obvious logical errors, there were 831 questionnaires left (effective rate 83.4%). As the main purpose of 2023 CNSTDH was to investigate the current development status of telemedicine in China, the sub-questionnaire on willingness to continue engaging in telemedicine was not set as mandatory. Healthcare professionals were free to decide whether to participate in the sub-questionnaire. Therefore, after excluding participants who did not respond to the sub-questionnaire on willingness, 560 valid samples were retained (Fig. 1). The sample size was set higher than the estimated minimum to ensure representativeness, adequate statistical power, and reduced bias, thereby enhancing the reliability of the results.
Ethics approval and consent to participate
Ethics approval for this study was obtained from the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. All participants were fully informed of the research purpose and were asked to provide informed consent before the participation. All methods were performed in accordance with the relevant guidelines and regulations.
Measures
Dependent variables
There are two dependent variables in this study, one of which measures healthcare professionals’ willingness to continue participating in telemedicine post COVID-19 pandemic (“I am willing to continue participating in telemedicine”), and the other measures their willingness to recommend telemedicine (“I am willing to recommend telemedicine to those in need”). The responses are rated on a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating stronger willingness.
Independent variables
Based on the extended TAM-TPB theoretical model, this study assessed a range of independent variables concerning participants’ perceptions and attitudes toward telemedicine: (1) The TAM includes two primary variables: perceived ease of use (technological ease, equipment accessibility, connection stability, etc.) and perceived usefulness (effectiveness, cost reduction, convenience, etc.) of telemedicine. (2) The TPB includes two major components: subjective norms (participants’ perception of social pressure and attitudes toward the expectations of others regarding telemedicine) and perceived behavioral control (participants’ perception of their ability and the resources available to them for engaging in telemedicine services within their work context). (3) Patient Accessibility, including perceived patient profile accessibility and perceived patient coverage by telemedicine. (4) Overall satisfaction of telemedicine, assessed by one single item: “Overall, I am satisfied with the telemedicine services I have engaged with.” Each variable, except satisfaction, was measured using three or four scale items. Most items were retrieved and adapted from previously tested and validated research15,30,31. Measurement of Cronbach’s alpha showed good internal consistency reliability for each of the scales: 0.86 for ease of use, 0.93 for usefulness, 0.94 for subjective norms, 0.94 for perceived behavioral control, 0.87 for patient profile accessibility, and 0.95 for patient coverage. Face and content validity were assessed through panel discussions with experts (academics and clinicians in the field) and a small-scale pilot study involving 25 healthcare professionals from the target population, who were not part of the main study sample. All items were rated on 5-point Likert scales, with responses ranging from 1 (strongly disagree) to 5 (strongly agree). Scores for each variable were calculated by averaging across all items within that variable.
Socio-demographic variables
Sociodemographic characteristics examined include age, gender, region, education level, professional title, participatory roles, hospital level, department, years of working, and years of telemedicine experience. The participatory roles in telemedicine are defined as either “inviter” or “invitee” based on their responsibilities. The “inviter” is the healthcare institution requesting support for diagnosis and treatment, while the “invitee” provides the support using information technologies.
Data analysis
The statistical analysis was conducted with SPSS version 24.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were presented as frequencies with percentages. Age was presented as means with standard deviation (SD), whereas other continuous variables were mainly presented as median (inter quartile range). Hierarchical multiple linear regression models with a “Stepwise” approach were used to identify the primary correlates of willingness to continue participating in and to recommend telemedicine, respectively. In Model 1, all socio-demographic variables were included except for years of work experience to mitigate potential collinearity. Model 2 added TAM constructs (ease of use and usefulness), and Model 3 added TPB constructs (subjective norms and perceived behavioral control). Patient Accessibility variables (patient profile accessibility and patient coverage) were entered in Model 4, and finally, overall satisfaction was entered in Model 5. “Perceived behavioral control” variable was removed from the models due to variance inflation factor (VIF) values > 5 and tolerance values < 0.2, indicating significant multicollinearity. All assumptions for linear regression models were examined graphically and analytically (linearity, normality, independence, and homoscedasticity) and were fulfilled. Further, based on the results of linear regression, mediation analyses were performed using the PROCESS version 4.2 macro designed for SPSS. We examined the mediation effects of satisfaction, subjective norms, and patient coverage on the association between usefulness and both willingness to continue participating in telemedicine and willingness to recommend telemedicine.
Results
Characteristics of the participants
In total, 560 healthcare professionals were included in this study. The sample characteristics are outlined in Table 1. The average age of participants was 37.14 (± 8.50) years, with a median of 3 (IQR 2–6) years of working experience in telemedicine. Slightly over half of the sample (52.7%) was female, and the majority came from the central region (48.9%) and the western region (45.2%). There were 43.2% of the respondents who took on the role of the inviter in telemedicine services, while 38.8% simultaneously served as both the inviter and the invitee. Approximately 43.0% were from tertiary hospitals, and most (75.4%) were from clinical departments. The largest number of participants had junior and intermediate titles, accounting for 38.9% and 32.7% respectively, and over 60% had a bachelor degree.
Perceptions, attitudes and willingness to continue participating in and recommend telemedicine
Overall, 518 (92.5%) of 560 respondents expressed their willingness to continue participating in telemedicine, and nearly all respondents (93.5%) displayed a willingness to recommend telemedicine to those in need. Healthcare professionals generally perceived the telemedicine services they participate in with a high level of ease of use and usefulness. They also reported a high level of subjective norms and perceived behavioral control in participating in telemedicine, as well as a high level of perceived profile accessibility and patient coverage through telemedicine. Moreover, participants expressed considerable satisfaction with the telemedicine services they engaged in (Table 2). The correlation matrix with main variables can be found in supplementary files (Supplementary Table 1).
Predictors associated with willingness to continue participating in telemedicine
Table 3 displays the hierarchical multiple linear regression results predicting willingness of healthcare professionals to continue participating in telemedicine. Demographic variables (Model 1) were generally non-significant predictors of variance. Professional title was negatively associated with healthcare professionals’ willingness to continue participating in telemedicine. Compared to respondents with a junior professional title, those with intermediate (β = -0.10, P = 0.040) and senior professional (β = -0.15, P = 0.001) titles had lower willingness to continue participating in telemedicine. Years of telemedicine experience was positively associated with willingness to continue participating in telemedicine (β = 0.09, P = 0.030). In model 2, the inclusion of TAM constructs accounted for a significant increase in variance explained (ΔR2 = 0.667, P < 0.001), and usefulness (β = 0.82, P < 0.001) was positively associated with willingness to continue participating in telemedicine. Furthermore, the addition of TPB constructs in Model 3 was positively and significantly associated with willingness. Healthcare professionals with greater perceived subjective norms (β = 0.64, P < 0.001) were more willing to continue participating in telemedicine. The inclusion of TPB constructs accounted for an additional 13.1% of the variance (P < 0.001), increasing the adjusted R2 to 82.1%. In Model 4, the inclusion of patient accessibility variables explained an additional 0.3% of the variance (P = 0.004). In Model 5, greater overall satisfaction with telemedicine was associated with stronger willingness to continue participating in telemedicine (β = 0.24, P < 0.001), an effect that explained an additional 1.2% (P < 0.001) of the variance and the model accounted for 83.5% of adjusted total variance.
Predictors of willingness to recommend telemedicine
Results of multiple linear regression examining predictors of willingness to recommend telemedicine are shown in Table 4. Socio-demographic predictors in Model 1 only explained an adjusted total variance of 0.7%, and having a higher professional title was associated with lower willingness to recommend telemedicine. Years of telemedicine experience was positively associated with willingness to recommend telemedicine (β = 0.09, P = 0.045). In model 2, TAM constructs accounted for 67.0% of added variance to the model (Adj R2 = 0.689, P < 0.001). Usefulness was positively associated with willingness to recommend telemedicine (β = 0.83, P < 0.001). In Model 3, subjective norms (β = 0.56, P < 0.001) was positively associated willingness to recommend telemedicine, accounting for 10.0% of added variance to the model (Adj R2 = 0.789, P < 0.001). Furthermore, patient coverage in Model 4 explained an additional 0.6% (Adj R2 = 0.795, P < 0.001) of the variance, and satisfaction in Model 5 explained an additional 1.9% of the variance (P < 0.001). In Model 5, participants who perceived higher levels of patient coverage (β = 0.12, P = 0.001) and satisfaction (β = 0.30, P < 0.001) with telemedicine reported greater willingness to recommend telemedicine. Ultimately, the final model explained approximately 81.4% of the variance in willingness to recommend telemedicine.
Mediation analysis
Finally, we further examined the mediating effects of satisfaction, subjective norms, and patient coverage in the models (see Figs. 2 and 3). As depicted in Table 5, usefulness was associated with willingness to continue participating in telemedicine directly (β = 0.18, 95% CI [0.10, 0.25]), and indirectly through satisfaction (β = 0.19, 95% CI [0.10, 0.29]) and subjective norms (β = 0.39, 95% CI [0.28, 0.51]). We also found that usefulness was associated with willingness to recommend telemedicine directly (β = 0.20, 95% CI [0.12, 0.27]), and indirectly through satisfaction (β = 0.23, 95% CI [0.14, 0.34]), subjective norms (β = 0.28, 95% CI [0.16, 0.39]), and patient coverage (β = 0.10, 95% CI [0.03, 0.19]).
Mediation effect model of satisfaction, subjective norms, and patient coverage between usefulness and willingness to continue participating in telemedicine. Usefulness was both directly and indirectly (through satisfaction and subjective norms) associated with willingness to continue participating in telemedicine.
Mediation effect model of satisfaction, subjective norms, and patient coverage between usefulness and willingness to recommend telemedicine. Usefulness was both directly and indirectly (through satisfaction, subjective norms, and patient coverage) associated with willingness to recommend telemedicine.
Discussion
In the post-pandemic era, with traditional face-to-face medical care fully resumed, the sustained and active engagement of healthcare professionals in telemedicine remains critical for its stable development. Given the irreplaceable advantages of face-to-face consultations, it is uncertain whether healthcare professionals will sustain their willingness for active telemedicine engagement. The factors influencing healthcare professionals’ willingness to engage in telemedicine identified during the pandemic may not apply to the current multi-model medical landscape. This nationwide survey examined the willingness of Chinese healthcare professionals to engage in telemedicine post-pandemic, with a focus on their willingness to continue participating in and recommend telemedicine, using an extended TAM-TPB model.
Overall, more than 90% of healthcare professionals in this study expressed willingness to continue participating in and recommend telemedicine. This suggests a general recognition of its value and significant role in enhancing the quality and accessibility of medical services. The adoption of telemedicine and willingness to engage in it vary significantly across different countries. Our results are similar to the high levels of acceptance and willingness observed in some high-income countries32,33, but are higher than those reported among healthcare professionals in resource-limited settings34,35. A previous study in Saudi Arabia found that most participants across all subgroups were willing to use digital tools in patient care, with acceptance rates ranging from 75.6 to 87.1% among physicians and nurses and 66.1–80.0% among nursing and medical students32. In contrast, only 53.42% of health professionals in Ethiopia held positive attitudes towards telemedicine, indicating moderate acceptance34. Furthermore, we note that the willingness in our study was slightly lower than that in nationwide studies conducted both before and during the pandemic15. As the pandemic subsides and daily life returns to normal, healthcare professionals may reduce their demand and expectations for telemedicine. Face-to-face communication is integral for healthcare professionals in diagnosing conditions and fostering patient trust36. Despite the convenience of telemedicine during the pandemic, its constraints in communication and diagnostic capabilities, such as the inability to monitor patients’ vital signs in person or perform physical exams on location37,38, may limit its use in certain contexts. This could lead healthcare professionals to prefer traditional face-to-face services, potentially reducing their willingness to participate in and recommend telemedicine.
In this study, we found that healthcare professionals with higher professional titles (intermediate and senior levels) were less willing to continue participating in and recommend telemedicine compared to those with junior titles. This reluctance may stem from multiple factors. First, senior healthcare professionals may have a stronger preference for traditional in-person consultations, which rely heavily on physical examinations and personal interactions that are difficult to replicate in virtual settings39. Second, their years of experience in traditional practice may create cognitive inertia, making them less inclined to adapt to newer modalities40. According to Rogers’ Diffusion of Innovations theory, later adopters often require higher compatibility between technologies and existing workflows41, and telemedicine may be perceived as a challenge to their established practice patterns. Additionally, the time investment required for technology adoption may disproportionately affect senior healthcare professionals. While junior healthcare professionals, often trained in the digital era, tend to have higher e-health literacy42, senior healthcare professionals may face a steeper learning curve, further exacerbated by their existing clinical workload43. Finally, concerns over the technological aspects of telemedicine, such as usability and reliability, may further reduce their willingness to adopt it44. Our results also showed that years of telemedicine experience were positively associated with willingness to continue participating in and recommend telemedicine. This further emphasizes the importance of familiarity and comfort in driving the adoption of new technologies. As healthcare professionals gain more exposure to telemedicine, they become more confident in its benefits and effectiveness, leading to increased acceptance and utilization. It also suggests that ongoing education and hands-on experience may help overcome initial barriers to telemedicine adoption. These findings highlight the need for tailored strategies, such as targeted training, technical support, and incentives, to encourage greater participation in telemedicine across all professional levels. Further research should focus on identifying the specific barriers faced by senior healthcare professionals and exploring effective ways to address these challenges to promote broader telemedicine adoption.
The results suggested that the extended TAM-TPB frameworks have a better predictive effect on healthcare professionals’ willingness to continue participating in telemedicine and their intention to recommend it. Two multiple linear regression models explained 86.0% and 82.8% of the total variance in healthcare professionals’ willingness to continue participating in and recommend telemedicine, respectively. Previous research has confirmed the validity and effectiveness of TAM and TPB in understanding technology acceptance45,46. However, relying solely on a single theoretical model may not fully capture the complex relationship between behavioral intention and actual behavior. The integration of multiple theoretical models can enhance the accuracy and comprehensiveness of predictions47,48. Future research could explore the significant role of integrating multiple theoretical models in predicting health behaviors and intentions related to telemedicine.
When analyzing the factors associated with healthcare professionals’ willingness to continue participating in and recommend telemedicine, our results showed that usefulness, subjective norm, patient coverage, and satisfaction were key drivers. Usefulness has been identified as one of the key determinants for the adoption of telemedicine49. When telemedicine systems offer practical benefits to healthcare professionals, such as improving diagnostic efficiency and streamlining resource management, they are more willing to participate in and recommend these technologies39. The usefulness of such systems is not only reflected in their technical features but also in their enhancement of the patient’s medical experience50. Interestingly, we found that greater subjective norms were associated with higher willingness to continue participating in and recommend telemedicine. Previous research has focused on individuals’ telemedicine usage experiences51,52, with little attention paid to the normative influences on healthcare professionals’ participation and promotion of telemedicine. However, it is important to note that healthcare professionals’ participation in and promotion of telemedicine is not just an individual choice but also has significant social interaction characteristics53. This suggests that future efforts to encourage healthcare professionals to engage more actively in telemedicine should leverage the positive influence of peer effects or social norms. Beyond using telemedicine technology, healthcare professionals’ perception of its benefits to patients is crucial for their sustained engagement and promotion54. Our results indicated that patient coverage was positively associated with the willingness to recommend telemedicine. This suggests that healthcare professionals consider patients’ needs when deciding whether to recommend telemedicine, thereby ensuring those who are unable or find it difficult to access traditional healthcare services can conveniently obtain necessary medical care. In the future, enhancing patients’ access to telemedicine will not only facilitate the equitable distribution and optimal allocation of medical resources but also effectively boost healthcare professionals’ willingness to recommend it. Consequently, this will further promote the widespread adoption of telemedicine, thereby improving the quality and efficiency of medical care.
We found that higher overall satisfaction of telemedicine increases healthcare professionals’ willingness to continue participating in and recommend telemedicine, which is consistent with previous findings55,56. This indicates that satisfaction is a key factor influencing the usage and promotion of telemedicine. Satisfaction with telemedicine may arise from its convenience, efficient patient communication, and expanded service reach57. Further analysis revealed that satisfaction acts as a mediating variable between usefulness and intention, suggesting that in the future promotion of telemedicine, continuously optimizing service quality and user experience, and maintaining and enhancing healthcare professionals’ satisfaction with telemedicine remain key to driving their sustained participation and promotion.
This study explored the willingness of Chinese healthcare professionals to continue participating in and recommend telemedicine in the post-pandemic era. It revealed the key factors influencing their engagement and endorsement of telemedicine, offering empirical support for advancing telemedicine services in China. The findings suggest that by enhancing healthcare professionals’ perceptions of telemedicine’s usefulness, increasing their satisfaction with engaging in telemedicine, emphasizing the influence of subjective norms on participation, and expanding patient access to telemedicine, healthcare professionals’ willingness to participate in and promote telemedicine will be significantly bolstered. With cautious interpretation, these results may provide reference for similar healthcare settings in other middle-income countries.
Policymakers and hospital administrators should implement targeted training programs to enhance healthcare professionals’ confidence and competence in telemedicine, focusing specifically on improving their satisfaction and perceived usefulness. This is especially important for senior staff who may face technological barriers. For example, training modules could include hands-on workshops, simulation exercises, and ongoing technical support to ensure proficiency in using telemedicine platforms. Offering financial incentives and career development opportunities, such as telemedicine specialization or certification, can further motivate participation and boost overall satisfaction. Additionally, improving the user experience by streamlining telemedicine platforms and ensuring seamless integration into existing workflows will be crucial in enhancing perceived usefulness. This includes optimizing user interfaces, reducing technical glitches, and providing clear guidelines for both healthcare professionals and patients. Strengthening technological infrastructure, particularly in rural or underserved areas, is essential for broader telemedicine adoption. This involves investing in high-speed internet connectivity, upgrading hardware, and ensuring reliable access to telemedicine tools. Promoting patient awareness and trust in telemedicine through public health campaigns and educational initiatives will also play a significant role in its success. These efforts will ultimately strengthen healthcare professionals’ involvement and improve the quality and accessibility of telemedicine nationwide.
This study has certain limitations that should be acknowledged. First, the study was cross-sectional, and while we examined the associations between usefulness, satisfaction, subjective norms, and willingness to continue participating in and recommend telemedicine, we cannot determine the causality or the temporal direction of the observed associations. This limitation is particularly relevant in mediation analyses, where the sequence of effects is crucial for accurate interpretation. Specifically, while satisfaction and subjective norms partially mediate the effect of usefulness on willingness to continue participating in and recommend telemedicine, the cross-sectional data cannot establish the direction of these effects. It is possible that higher satisfaction and subjective norms may increase perceived usefulness, rather than usefulness driving satisfaction and subjective norms. Similarly, patient coverage partially mediates the relationship between usefulness and willingness to recommend telemedicine, but this relationship could also be bidirectional. Therefore, future longitudinal studies are needed to establish causal relationships by tracking changes in these variables over time and their impact on continued participation and recommendation of telemedicine. Second, self-reported willingness to participate in and recommend telemedicine may be influenced by social desirability bias. Third, although this study was conducted nationwide, the sample size lacks sufficient diversity, so caution should be exercised when generalizing to other populations and regions. Future studies should aim for more comprehensive population coverage. Additionally, while our findings may be useful to similar healthcare settings, applying them to other middle-income countries may not be appropriate due to significant differences in healthcare systems and population health profiles. Fourth, participation was voluntary, and data from non-respondents or incomplete surveys were excluded. This may introduce selection bias, as individuals who chose to participate and complete the survey may have had more positive experiences or attitudes towards telemedicine, potentially overestimating the reported willingness to engage in telemedicine. Consequently, the generalizability of our results may be limited, which should be carefully considered during interpretation. Future studies should consider strategies to minimize selection bias, such as employing techniques to account for missing data. Finally, this study included a limited number of potential influencing factors. The sustained participation and recommendation of telemedicine are affected by various factors. For example, we did not account for potential regional disparities in telemedicine infrastructure and policy implementation. Differences in healthcare resources, internet penetration, and policy support across regions could affect the accessibility and utilization of telemedicine services, potentially biasing our findings. Future research needs to consider a broader range of potential influences.
Conclusions
The sustained engagement and promotion by healthcare professionals are essential for the advancement of telemedicine. Our findings indicated that Chinese healthcare professionals have a generally high willingness to continue participating in and recommend telemedicine in the post-pandemic era. Perceived usefulness, subjective norms, satisfaction, and patient coverage of telemedicine are key factors in enhancing healthcare professionals’ continued engagement and promotion of telemedicine. Future research could benefit from longitudinal studies that track changes in willingness over time, as well as studies that explore the perspectives of both patients and healthcare professionals to better understand the dynamics that influence telemedicine participation and recommendation.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to reasons of privacy and ethical considerations. The instruments are available from the corresponding author upon reasonable request.
References
Monaghesh, E. & Hajizadeh, A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public. Health. 20, 1193. https://doi.org/10.1186/s12889-020-09301-4 (2020).
Hong, Z. et al. Telemedicine during the COVID-19 pandemic: experiences from Western China. J. Med. Internet Res. 22, e19577. https://doi.org/10.2196/19577 (2020).
Barney, A., Buckelew, S., Mesheriakova, V. & Raymond-Flesch, M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J. Adolesc. Health. 67, 164–171. https://doi.org/10.1016/j.jadohealth.2020.05.006 (2020).
Smolić, S., Blaževski, N. & Fabijančić, M. Remote healthcare during the COVID-19 pandemic: findings for older adults in 27 European countries and Israel. Front. Public. Health. 10, 921379. https://doi.org/10.3389/fpubh.2022.921379 (2022).
Serper, M. et al. Positive early patient and clinician experience with telemedicine in an academic gastroenterology practice during the COVID-19 pandemic. Gastroenterology 159, 1589–1591. https://doi.org/10.1053/j.gastro.2020.06.034 (2020).
Paffenholz, P. et al. Impact of the COVID-19 pandemic on urologists in Germany. Eur. Urol. Focus. 6, 1111–1119. https://doi.org/10.1016/j.euf.2020.06.001 (2020).
The State Council. The People’s Republic of China. Opinions on Promoting Telemedicine Services in Medical Institutions. https://www.gov.cn/gongbao/content/2014/content_2792664.htm (2014).
Zhang, W., He, D., Wang, G., Zhu, C. & Evans, R. Analyzing National telemedicine policies in China from the perspective of policy instrument (1997–2020). Int. J. Med. Inf. 166, 104854. https://doi.org/10.1016/j.ijmedinf.2022.104854 (2022).
Ye, J., He, L. & Beestrum, M. Implications for implementation and adoption of telehealth in developing countries: a systematic review of China’s practices and experiences. NPJ Digit. Med. 6, 174. https://doi.org/10.1038/s41746-023-00908-6 (2023).
Fu, H., Cheng, T. C., Zhan, J., Xu, D. & Yip, W. Dynamic effects of the COVID-19 pandemic on the demand for telemedicine services: evidence from China. J. Econ. Behav. Organ. 220, 531–557. https://doi.org/10.1016/j.jebo.2024.02.015 (2024).
Gao, J. et al. Telemedicine is becoming an increasingly popular way to resolve the unequal distribution of healthcare resources: evidence from China. Front. Public. Health. 10, 916303. https://doi.org/10.3389/fpubh.2022.916303 (2022).
Cheng, T. C. & Yip, W. Progress, policies and prospects for internet telemedicine in China. https://www.hsph.harvard.edu/takemi/wp-content/uploads/sites/114/2023/10/TakemiSymposium_Cheng.pdf (2023).
The State Council. The People’s Republic of China. Telemedicine services cover all Chinese cities. https://english.www.gov.cn/news/202307/30/content_WS64c62185c6d0868f4e8de35b.html (2023).
Abdelghany, I. K., AlMatar, R., Al-Haqan, A., Abdullah, I. & Waheedi, S. Exploring healthcare providers’ perspectives on virtual care delivery: insights into telemedicine services. BMC Health Serv. Res. 24, 1. https://doi.org/10.1186/s12913-023-10244-w (2024).
Ma, Q. et al. Usage and perceptions of telemedicine among health care professionals in China. Int. J. Med. Inf. 166, 104856. https://doi.org/10.1016/j.ijmedinf.2022.104856 (2022).
Houlding, E. et al. Barriers to use of remote monitoring technologies used to support patients with COVID-19: rapid review. JMIR Mhealth Uhealth. 9, e24743. https://doi.org/10.2196/24743 (2021).
Kruse, C. & Heinemann, K. Facilitators and barriers to the adoption of telemedicine during the first year of COVID-19: systematic review. J. Med. Internet Res. 24, e31752. https://doi.org/10.2196/31752 (2022).
Assaye, B. T. et al. Perception towards the implementation of telemedicine during COVID-19 pandemic: a cross-sectional study. BMC Health Serv. Res. 23, 967. https://doi.org/10.1186/s12913-023-09927-1 (2023).
Reingold, S. M. et al. COVID-19 era effect on pandemic and Post-pandemic pediatric telemedicine use: A survey of the European academy of pediatrics research in ambulatory settings network. Front. Pediatr. 9, 713930. https://doi.org/10.3389/fped.2021.713930 (2021).
Mohammadi, E. et al. Post-pandemic paradigm shift toward telemedicine and tele-education; an updated survey of the impact of Covid-19 pandemic on neurosurgery residents in united States. World Neurosurg. X. 23, 100326. https://doi.org/10.1016/j.wnsx.2024.100326 (2024).
Jung, S. E., Kwon, Y., Kwon, S., Kim, Y. & Park, H. Satisfaction survey of medical staff for telemedicine after the COVID-19 pandemic: A comparison between the COVID-Pandemic and Post-COVID pandemic periods. Telemed J. E Health. 31, 50–58. https://doi.org/10.1089/tmj.2024.0142 (2025).
Chandrasekaran, R. Telemedicine in the Post-Pandemic period: Understanding patterns of use and the influence of socioeconomic demographics, health status, and social determinants. Telemed J. E Health. 30, 480–489. https://doi.org/10.1089/tmj.2023.0277 (2024).
Moulaei, K., Sheikhtaheri, A., Fatehi, F., Shanbehzadeh, M. & Bahaadinbeigy, K. Patients’ perspectives and preferences toward telemedicine versus in-person visits: a mixed-methods study on 1226 patients. BMC Med. Inf. Decis. Mak. 23, 261. https://doi.org/10.1186/s12911-023-02348-4 (2023).
Splinter, M. J. et al. Patient perspectives on telemedicine during the COVID-19 pandemic: a mixed-methods community-based study. BMC Health Serv. Res. 23, 803. https://doi.org/10.1186/s12913-023-09794-w (2023).
Kruse, C. S. et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 7, e016242. https://doi.org/10.1136/bmjopen-2017-016242 (2017).
Davis, F. D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS QUART. 13, 319–340. https://doi.org/10.2307/249008 (1989).
Schifter, D. E. & Ajzen, I. Intention, perceived control, and weight loss: an application of the theory of planned behavior. J. Pers. Soc. Psychol. 49, 843–851. https://doi.org/10.1037/0022-3514.49.3.843 (1985).
The State Council. The People’s Republic of China. 2023 Statistical Bulletin on the Development of Health and Wellness in China. https://www.gov.cn/lianbo/bumen/202408/content_6971241.htm (2023).
Kish, L. Sampling organizations and groups of unequal sizes. Am. Sociol. Rev. 30, 564–572 (1965).
Hah, H., Goldin, D. & Ha, S. The association between willingness of frontline care providers’ to adaptively use telehealth technology and virtual service performance in provider-to-provider communication: quantitative study. J. Med. Internet Res. 21, e15087. https://doi.org/10.2196/15087 (2019).
Albarrak, A. I. et al. Assessment of physician’s knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia. J. Infect. Public. Health. 14, 97–102. https://doi.org/10.1016/j.jiph.2019.04.006 (2021).
Thapa, S., Nielsen, J. B., Aldahmash, A. M., Qadri, F. R. & Leppin, A. Willingness to use digital health tools in patient care among health care professionals and students at a university hospital in Saudi Arabia: quantitative Cross-sectional survey. JMIR Med. Educ. 7, e18590. https://doi.org/10.2196/18590 (2021).
Muehlensiepen, F., Petit, P., Knitza, J., Welcker, M. & Vuillerme, N. Factors associated with telemedicine use among German general practitioners and rheumatologists: secondary analysis of data from a nationwide survey. J. Med. Internet Res. 24, e40304. https://doi.org/10.2196/40304 (2022).
Chereka, A. A. et al. Attitudes towards telemedicine services and associated factors among health professionals in Ethiopia: a systematic review and meta-analysis. BMC Health Serv. Res. 24, 1505. https://doi.org/10.1186/s12913-024-11979-w (2024).
Ahmed, M. H. et al. Willingness to use telemedicine during COVID-19 among health professionals in a low income country. Inf. Med. Unlocked. 27, 100783. https://doi.org/10.1016/j.imu.2021.100783 (2021).
Sutherland, B. L., Pecanac, K., LaBorde, T. M., Bartels, C. M. & Brennan, M. B. Good working relationships: how healthcare system proximity influences trust between healthcare workers. J. Interprof Care. 36, 331–339. https://doi.org/10.1080/13561820.2021.1920897 (2022).
Ftouni, R., AlJardali, B., Hamdanieh, M., Ftouni, L. & Salem, N. Challenges of telemedicine during the COVID-19 pandemic: a systematic review. BMC Med. Inf. Decis. Mak. 22, 207. https://doi.org/10.1186/s12911-022-01952-0 (2022).
Almathami, H. K. Y., Win, K. T. & Vlahu-Gjorgievska, E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J. Med. Internet Res. 22, e16407. https://doi.org/10.2196/16407 (2020).
Antonacci, G. et al. Healthcare professional and manager perceptions on drivers, benefits, and challenges of telemedicine: results from a cross-sectional survey in the Italian NHS. BMC Health Serv. Res. 23, 1115. https://doi.org/10.1186/s12913-023-10100-x (2023).
Mareš, J. Resistance of health personnel to changes in healthcare. Kontakt 20, e262–e272. https://doi.org/10.1016/j.kontakt.2018.04.002 (2018).
Escobar-Rodríguez, T. & Romero-Alonso, M. The acceptance of information technology innovations in hospitals: differences between early and late adopters. Behav. Inf. Technol. 33, 1231–1243. https://doi.org/10.1080/0144929X.2013.810779 (2013).
Kuek, A. & Hakkennes, S. Healthcare staff digital literacy levels and their attitudes towards information systems. Health Inf. J. 26, 592–612. https://doi.org/10.1177/1460458219839613 (2020).
Scott Kruse, C. et al. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed Telecare. 24, 4–12. https://doi.org/10.1177/1357633X16674087 (2018).
Breton, M. et al. Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. BMC Fam Pract. 22, 192. https://doi.org/10.1186/s12875-021-01543-4 (2021).
Domingos, C., Costa, P., Santos, N. C. & Pêgo, J. M. Usability, acceptability, and satisfaction of a wearable activity tracker in older adults: observational study in a real-life context in Northern Portugal. J. Med. Internet Res. 24, e26652. https://doi.org/10.2196/26652 (2022).
Sora, B., Nieto, R., Del Campo, M., Armayones, M. & A. & Acceptance and use of telepsychology from the clients’ perspective: questionnaire study to document perceived advantages and barriers. JMIR Ment Health. 8, e22199. https://doi.org/10.2196/22199 (2021).
Lee, S. J., Choi, M. J., Rho, M. J., Kim, D. J. & Choi, I. Y. Factors affecting user acceptance in overuse of smartphones in mobile health services: an empirical study testing a modified integrated model in South Korea. Front. Psychiatry. 9, 658. https://doi.org/10.3389/fpsyt.2018.00658 (2018).
Gagnon, M. et al. Electronic health record acceptance by physicians: testing an integrated theoretical model. J. Biomed. Inf. 48, 17–27. https://doi.org/10.1016/j.jbi.2013.10.010 (2014).
Harst, L., Lantzsch, H. & Scheibe, M. Theories predicting end-user acceptance of telemedicine use: systematic review. J. Med. Internet Res. 21, e13117. https://doi.org/10.2196/13117 (2019).
Shen, Y. T., Chen, L., Yue, W. W. & Xu, H. X. Digital technology-based telemedicine for the COVID-19 pandemic. Front. Med. 8, 646506. https://doi.org/10.3389/fmed.2021.646506 (2021).
Odendaal, W. A. et al. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst. Rev. 3, CD011942. https://doi.org/10.1002/14651858.CD011942.pub2 (2020).
Alqurashi, H., Mohammed, R., AlGhanmi, A. S. & Alanazi, F. The perception of health care practitioners regarding telemedicine during COVID-19 in Saudi Arabia: mixed methods study. JMIR Form. Res. 7, e47065. https://doi.org/10.2196/47065 (2023).
Seuren, L. M., Ilomäki, S., Dalmaijer, E., Shaw, S. E. & Stommel, W. J. P. Communication in telehealth: a state-of-the-art literature review of conversation-analytic research. Res. Lang. Soc. Interact. 57, 73–90. https://doi.org/10.1080/08351813.2024.2305045 (2024).
Ahmed, A. et al. A systematic review of publications on perceptions and management of chronic medical conditions using telemedicine remote consultations by primary healthcare professionals April 2020 to December 2021 during the COVID-19 pandemic. Med. Sci. Monit. 30, e943383. https://doi.org/10.12659/MSM.943383 (2024).
Alashek, W. A. & Ali, S. A. Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review. Libyan J. Med. 19, 2301829. https://doi.org/10.1080/19932820.2024.2301829 (2024).
Nguyen, M., Waller, M., Pandya, A. & Portnoy, J. A review of patient and provider satisfaction with telemedicine. Curr. Allergy Asthma Rep. 20, 72. https://doi.org/10.1007/s11882-020-00969-7 (2020).
Shi, J. et al. Implementation, service effectiveness and satisfaction with teleconsultation services in China during the COVID-19 pandemic: from the perspective of primary health care professionals. Int. J. Med. Inf. 178, 105202. https://doi.org/10.1016/j.ijmedinf.2023.105202 (2023).
Acknowledgements
The authors are extremely grateful to all the participants who took part in this study.
Funding
This research was supported by grants from the National Key Research and Development Program of China (Grant No. 2022ZD0160704); the Science and Technology Research Program in Henan Province (Grant No. 232102311057 and 242102311021); and the Joint Construction Project of Henan Province Medical Science and Technology Research Plan (Grant NO. LHGJ20230178 and LHGJ20220433).
Author information
Authors and Affiliations
Contributions
WW: Conceptualization, Methodology, Investigation, Funding acquisition, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. XH: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing. XZ: Investigation, Formal analysis, Writing – review & editing. YC: Conceptualization, Methodology, Investigation, Data curation, Writing – review & editing. CL: Conceptualization, Project administration, Writing – review & editing. BC: Conceptualization, Writing – review & editing. JZ: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, W., He, X., Zhang, X. et al. Willingness of healthcare professionals in China to continue participating in and recommend telemedicine post COVID-19 pandemic. Sci Rep 15, 9581 (2025). https://doi.org/10.1038/s41598-025-93801-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-93801-z