Abstract
Depression and chronic diseases are closely linked, but the combined impact of multiple chronic diseases on depression is not well understood due to limited research on their interaction. This study aimed to examine how the interaction of chronic diseases influences depression in middle-aged and elderly individuals, and to identify high-risk factors for depression related to these disease interactions. In this study, depression among middle-aged and elderly individuals was designated as the dependent variable. The dataset from the 2015 China Health and Retirement Longitudinal Study (CHARLS) underwent both univariate and multivariate analyses. Subsequently, a dual interaction analysis was performed to examine the significant impact of the number of chronic diseases on depression, complemented by an attribution analysis. Among the 8163 participants, depression was more common in females, unmarried individuals, rural residents, and non-retired (P < 0.05, 0.01 or 0.001). Higher education correlate with lower depression rates. Participants with chronic diseases show higher depression rates than those without (P < 0.05, 0.01, or 0.001). The depression group exhibited lower episodic memory, cognitive ability, and sleep duration (P < 0.05, 0.01, or 0.001). Various factors significantly contribute to depression in middle-aged and elderly individuals (P < 0.05, 0.01 or 0.001). Finally, the majority of chronic diseases have a significant contribution to the occurrence of depression in middle-aged and elderly individuals after dual interaction. Chronic diseases significantly influence depression in middle-aged and elderly individuals, with their dual interaction having a complex effect. While most chronic disease indicators aren’t useful for diagnosing depression, memory and cognitive function indicators can help. These should be considered alongside other chronic disease indicators when diagnosing depression.
Similar content being viewed by others
Introduction
A greater focus must be placed on the health of middle-aged and elderly Chinese due to the aging population1. The current prevalence of depression among middle-aged and elderly people in China is around 22.7% and depression rates in this group have risen annually, and chronic diseases, a key public health issue, are increasingly studied by scholars globally2. Chronic diseases, while not infectious, are long-lasting and incurable, often leading to disability, reduced quality of life, economic strain, and significant use of medical resources3. Therefore, prevention and treatment of depression and chronic diseases is the focus of many scholars.
The etiology and pathogenesis of depression are still unclear. According to reports, the occurrence of depression is closely related to chronic diseases, and there may even be a bidirectional relationship between depression and chronic diseases4. A Study show that depression is more common in patients with chronic conditions, and factors like endocrine changes, inflammation, and psychological fluctuations can influence its onset5. Depression is a chronic disease affecting both physical and mental health and should be managed similarly to other chronic illnesses6. However, unlike degenerative chronic diseases caused by organic lesions or aging, depression is a psychiatric disorder with distinct evaluation and treatment methods. Despite their close relationship, they should not be conflated. In addition, The combined presence of multiple chronic diseases significantly affects depression7. However, the overall impact and interaction between chronic diseases and depression remain unclear, with limited quantitative research on their risk factors, particularly in middle-aged and elderly individuals. For a long time, the occurrence of depression has been closely related to functional health examination indicators, and there is no relevant discussion on whether the relevant detection indicators in chronic diseases can provide a reference value for the diagnosis of depression.
This study seeks to integrate a broad spectrum of general health conditions, chronic diseases, functional assessments, and blood biochemical markers, employing a comprehensive array of variables to predict and evaluate the determinants of depression in middle-aged and elderly populations. The objective is to elucidate the critical factors contributing to the onset of depression and to offer insights for its prevention and treatment. Our research aims to elucidate the relationship between chronic diseases and the incidence of depression in middle-aged and elderly individuals aged 45 and above, with a particular focus on examining the bidirectional interaction between chronic diseases and the progression of depression. Specifically, we focus on the following issues: (1) How do the general demographic characteristics, chronic diseases, functional examination results, and blood biochemical indicators differ between middle-aged and elderly individuals with depression and their non-depressed counterparts? To what extent can these indicators be directly used to assess the occurrence of depression? (2) What is the contribution of these influencing factors to the occurrence of depression in middle-aged and elderly individuals? (3) In what manner does chronic disease impact the occurrence of depression in middle-aged and elderly individuals? (4) What is the relationship between the dual interaction of chronic diseases and the occurrence of depression in middle-aged and elderly individuals?
Materials and methods
Data source and sample selection
Raw data for this study is taken from the 2015 China Health and Retirement Longitudinal Study8, managed by Peking University’s National Development Institute and funded by the National Natural Science Foundation of China. The data, representing individuals aged 45 and above, was collected through multi-stage stratified sampling of 21,038 respondents across 28 provinces, 150 counties, and 450 communities. This study employed a structured questionnaire to gather baseline demographic information, health status, functional assessments, blood biochemical markers, and other pertinent data from the population. The analysis focused on individuals aged 45 years and older. After excluding records with missing or erroneous data pertaining to demographic information, health status, functional assessments, and blood biochemical markers, a total of 8163 participants with complete datasets were included in the cross-sectional analysis. The research design framework for this cross-sectional survey is structured as follows: Initially, we performed statistical descriptions and univariate analyses on the general demographic characteristics, chronic disease prevalence, functional assessments, and blood biochemical indicators of 8163 participants. Subsequently, we conducted multivariate analyses to examine the individual factors that may influence the incidence of depression in middle-aged and elderly populations, aiming to ascertain the contribution of each factor to depression occurrence. Following this, we identified the number of chronic diseases that significantly impact depression incidence and investigated the effects of the dual interaction of chronic diseases on depression occurrence. Finally, we performed attribution analysis on the incidence of depression, considering the dual interaction of chronic diseases and relevant indicators. The detailed research methodology and conceptual framework are illustrated in Fig. 1.
Variables and definitions
Dependent variable
In this study, depression was utilized as the outcome variable, and its occurrence was qualitatively assessed using the widely recognized CESD10 scale9. The CESD10 comprises 10 categories of items, with a total score ranging from 0 to 30 points, where lower scores signify lower levels of depressive symptoms. Prior research has demonstrated that thresholds below 10 exhibit good sensitivity and specificity for middle-aged and elderly populations in China10. Accordingly, 2589 participants, who scored 10 or more on the CESD10 test, were classified as depressed, and 5574 participants were classified as non-depressed.
Independent variables
This study examines general demographic characteristics, chronic disease prevalence, physical and functional examination results, and blood biochemical indicators as independent variables influencing the incidence of depression in middle-aged and elderly individuals. Assessments of memory and cognitive abilities, as well as depression, were conducted using the MMSE scale11 and the CESD10 scale, both of which were integrated into the CHARLS questionnaire. The specific indicators included are as follows: (1) general demographic characteristics: gender, age, married, location of residential address, nationality, retired, level of education; (2) scope of chronic diseases: this study defined 15 types of diseases including diabetes, dyslipidemia, hypertension, apoplexy, memory disorders, psychosis, cardiopathy, lung disease, asthma, gastritis, hepatopathy, neuropathy, arthritis, disability, and cancer as chronic diseases, and included chronic diseases as disease variables in the independent variables; (3) functional examination results: general physical examination variables: mean systolic blood pressure, mean diabetic blood pressure; memory and cognitive ability test (score) variables: episode memory (0–10 points, the higher the score, the better), mind test (0–11 points, the higher the score, the better), cognitive ability (0–21 points, the higher the score, the better), CESD10 (0–30 points, the higher the score, the worse), sleep duration; (4) blood biochemical criteria variables: WBC in thousands, MCV, PLT, hematocrit, hemoglobin, BUN, creatinine, uric acid, cystatin c, blood glucose, glycated hemoglobin, total cholesterol, triglyceride, HDL, LDL, CRP. The assignment of variables and definitions is detailed in Table 1.
Statistical analysis
We utilized Microsoft Excel and SPSS version 23.0 for data processing and analysis. In the univariate analysis, P–P (probability–probability) plots or Q–Q (quantile–quantile) plots were employed to preliminarily assess the normal distribution of grouped continuous data. The central tendency and dispersion of the data were subsequently expressed as mean ± standard deviation (\({\overline{\text{X}}}\) ± S). For the comparison of two independent continuous data samples, the t-test was applied. In cases where the variance between two independent continuous data samples was unequal, the approximate t-test (tʹ test) was used. The comparison of ratios is performed using the chi-square test (χ2 test), while the multiple comparisons of ratios are performed using the chi-square split test (Bonferroni calibration level adjustment method). Incorporate variables exhibiting statistically significant differences in the univariate analysis into a multivariate binary logistic regression model. Assess the contribution of each variable to the dependent variable. Subsequently, reintroduce multiple chronic disease variables with notable contributions into the binary logistic regression model to examine dual interactions, thereby evaluating the impact of chronic disease comorbidities on the dependent variable. The relevant results were represented by odds ratios [OR = (number of exposed individuals in the case group/number of non-exposed individuals)/(number of exposed individuals in the control group/number of non-exposed individuals)] and 95% confidence intervals [95% CI = sample mean ± (critical value * standard error), critical value = 1.96], this OR value defines the multiplier of the risk of depression in middle-aged and elderly individuals under different factors in this study. The preceding analysis indicates statistically significant differences in test levels, with a p-value of less than 0.05. Utilizing the Bonferroni correction for level adjustment, the test level is determined by Pʹ < P/C2 n, where n denotes the number of chi-square test groups.
Moral statement
The raw data from the CHARLS is publicly accessible to researchers globally. Ethical and moral approvals for CHARLS procedures have been granted by the Institutional Review Committee of Peking University. Additionally, the Biomedical Ethics Review Committee of Peking University has conducted a comprehensive ethical review of the data collection process. Participation in CHARLS was entirely voluntary, with all participants providing informed consent through the signing of two consent forms prior to their involvement. The Institutional Review Board (IRB) approval number for this study is IRB00001052-11015. All content of this study strictly adheres to the above standards and requirements.
Results
The impact of the general feature distribution of the dataset on the occurrence of depression
The prevalence of depression was significantly higher among females compared to males (χ2 = 154.593, P < 0.001), unmarried individuals compared to married individuals (χ2 = 56.379, P < 0.001), rural residents compared to urban residents (χ2 = 80.153, P < 0.001), and non-retired individuals compared to retired individuals (χ2 = 109.757, P < 0.001). Additionally, an inverse relationship was observed between education level and the prevalence of depression (χ2 = 230.508, P < 0.001), with higher education levels associated with lower prevalence rates. The prevalence of chronic diseases is significantly higher among patients with chronic conditions compared to those without (χ2 = 131.479, P < 0.001), Furthermore, patients diagnosed with diabetes, dyslipidemia, hypertension, apoplexy, memory disorders, psychosis, cardiopathy, lung disease, asthma, gastrointestinal disorders, hepatopathy, nephropathy, arthritis, disability, and cancer exhibit a significantly higher prevalence of depression compared to those without these conditions (P < 0.001). For detailed information, refer to Table 2.
Descriptive characteristics of 8163 participants in the CHARLS 2015
In the general physical examination indicators, the depression group demonstrated higher mean systolic and diastolic blood pressure than the non-depressed group (P < 0.05). In assessments of memory and cognitive ability, the depression group showed significantly lower levels of episodic memory, mental test scores, and overall cognitive ability compared to the non-depressed group (P < 0.001). Additionally, the depression group exhibited a significantly higher CESD10 score compared to the non-depressed group (P < 0.001), and demonstrated reduced sleep duration relative to the non-depressed group (P < 0.001). Regarding blood biochemical indicators, the depression group had lower levels of hematocrit and hemoglobin compared to the non-depressed group (P < 0.001). Conversely, the depression group presented with elevated levels of creatinine, uric acid, HDL, and CRP in comparison to the non-depressed group (P < 0.05, 0.01 or 0.001). These differences are statistically significant. For detailed information, refer to Table 3.
The results of binary logistic regression analysis on the influencing factors of depression in middle-aged and elderly individuals
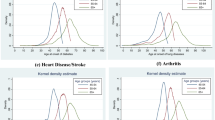
The results in Table 4 showed that gender, marriage, education level, chronic disease, diabetes, hypertension, apoplexy, memory disorders, psychosis, cardiopathy, asthma, hepatopathy, nephropathy, arthritis, disability, cancer, episodic memory, mind test, cognitive ability, CESD10, and sleep duration were significantly related to depression (P < 0.05). Among the significant categorical variables, being female, unmarried and having a low level of education are identified as high-risk factors for depression. Additionally, the presence of diabetes, hypertension, apoplexy, memory disorders, psychosis, cardiopathy, asthma, hepatopathy, nephropathy, arthritis, disability, and cancer are also significant high-risk factors. Conversely, among the significant continuous variables, episodic memory, cognitive test performance, cognitive ability, and sleep duration are identified as protective factors against depression. The prevalence of depression is 2.078 times higher in females compared to males (P < 0.001). Unmarried individuals are more likely to experience depression compared to their married counterparts (P < 0.001). Furthermore, individuals with higher educational attainment, including those who have completed elementary school, middle school, high school, or higher levels of education, exhibit a lower likelihood of developing depression compared to those with less than an elementary school education (P < 0.001). Among the overall participants, those with chronic diseases are 1.233 times more likely to develop depression compared to those without chronic diseases (P < 0.05). People with diabetes, hypertension, apoplexy, memory disorders, psychosis, cardiopathy, asthma, hepatopathy, nephropathy, arthritis, disability, and cancer are more likely to suffer from depression (P < 0.05, 0.01 or 0.001). Higher levels of episodic memory, cognitive performance, and sleep duration are associated with a decreased risk of depression (P < 0.001).
The binary logistic regression analysis results of the dual interaction of chronic diseases on the occurrence of depression in middle-aged and elderly individuals.
Finally, we correlated the diagnosed chronic diseases of middle-aged and elderly populations with each other to test whether such an effect would have an additional impact on the occurrence of depression. The results presented in Table 5 illustrate the impact of the dual interaction of chronic diseases on the occurrence of depression. The impact of comorbidity of most chronic diseases on the occurrence of depression is significant (OR > 1, P < 0.05, 0.01 or 0.001).
Discussion
According to the WHO, women experience depression at a rate 50% higher than men12. This study confirmed this, finding the incidence of depression in middle-aged and elderly women to be 50.59% higher than in men, with their risk being 2.078 times greater. The results of this study suggest that depression is more prevalent among unmarried, rural, non-retired, non-Han Chinese individuals, those with a history of falls, and those with low education. Key factors linked to depression include marital status, residence, gender, and education. Married, highly educated urban men show lower depression scores13. Ethnic customs also influence depression rates. Unmarried middle-aged and elderly individuals tend to experience more loneliness and depression. The absence of companionship and care can cause psychological issues in middle-aged and elderly individuals. Without someone to confide in, they are more susceptible to emotional problems and depression, especially when facing challenges. Experiences like widowhood and divorce, which are negative emotional events, further increase the risk of depression. The non-retired population often experiences greater work pressure and life challenges than retirees. Additionally, larger cities tend to have lower depression rates, suggesting urbanization protects against depression14. Higher education levels, which correlate with cognitive abilities, also significantly influence depression onset. A study has found that individuals most likely to believe false information exhibit higher levels of bias and depression, as well as lower levels of education, which has become an established fact15. In China, illiteracy has not been entirely eradicated. In remote rural areas, underdeveloped economic conditions often coincide with inadequate educational resources, and scientific interventions are markedly insufficient. These factors remain significant contributors to the prevalence of depression. The results of the attribution analysis indicate that marital status and higher educational attainment are significantly associated with a reduced risk of depression among middle-aged and elderly individuals. These findings are consistent with the themes discussed earlier.
Our study thoroughly examined how different chronic diseases and related factors influence depression. Findings suggest that managing chronic diseases is crucial to prevent depression. Notably, middle-aged and elderly individuals with hypertension have a higher incidence of depression and elevated systolic and diastolic blood pressure. A recent meta-analysis16 found that hypertension patients frequently suffer from depression, aligning with our study’s finding of a 0.147-fold increase in depression among middle-aged and elderly hypertensive patients compared to non-hypertensive ones. Additionally, hypertension, a condition linked to cardiovascular disease, is associated with related ailments like cardiopathy and apoplexy, which also contribute to depression. We discovered that middle-aged and elderly patients with depression exhibit elevated CRP levels, indicating a higher risk of cardiovascular disease and increased inflammation. Additionally, these patients tend to have high HDL levels, which may be linked to chronic inflammatory conditions like hepatopathy, diabetes, cardiopathy, and apoplexy17. We found that middle-aged and elderly patients with depression have lower hematocrit and hemoglobin levels, which are key indicators for diagnosing anemia. Untreated anemia increases the risk of depression by 2.6 times18, potentially due to inflammation. Inflammatory anemia, linked to conditions like cancer, arthritis, nephropathy, and gastrosis, results in chronic inflammation and reduced red blood cell production. Our research shows nephropathy increases creatinine and uric acid levels. Depression has diverse causes, with chronic diseases and related indicators playing a complex role. This study found that middle-aged and elderly patients with depression have higher rates of dyslipidemia, lung disease, asthma, disability, and cancer compared to their non-depressed counterparts. Adolescents with significant depressive symptoms also show similar dyslipidemia levels as healthy adolescents, which can increase cardiovascular disease risk19, dyslipidemia can increase the risk of cardiovascular disease in patients with depression20. There is also a noted association between lung disease and depression21. Scholars have found a complex relationship between depression and asthma22. Asthma can cause anxiety, which may lead to depression, and both anxiety and depression can affect asthma control23. Inflammation is a key factor in this relationship24. Higher severity of depression and anxiety correlates with greater disability25. Additionally, cancer and depression often co-occur, necessitating preventive measures26. Chronic diseases have long-term and serious damage, not only tormenting patients’ physical and mental health for a long time, reducing their quality of life, but also leading to the occurrence of depression. More interestingly, we found that only 12 chronic diseases were included in the framework, and all associated indicators were excluded. Then, surprisingly, all indicators related to memory and cognitive ability tests were included in the binary logistic regression model, including episode memory, mind test, cognitive ability, CESD10, sleep duration. We were pleasantly surprised to find that apoplexy, memory disorders, and psychosis, which correspond to these indicators, have a higher contribution to the occurrence of depression compared to other diseases included in the model, and have a higher risk. Therefore, the risk of depression caused by similar diseases cannot be underestimated, and their corresponding test indicators can also serve as auxiliary diagnostic indicators for depression.
A study has elucidated the impact of chronic comorbidities on the occurrence of depression. Chronic comorbidities have a higher risk than single non-communicable diseases lead to depression27. The occurrence of depression in the population over 45 years old is related to the number of chronic diseases in a dose–response manner28. However, these discussions have not yet been quantitatively focused on, and these studies mainly describe the impact of comorbidities on the occurrence of depression in chronic diseases. However, there is insufficient evidence regarding the potential interactive effects of these diseases on the risk of depression. This study aims to investigate whether interactions between chronic diseases contribute to the incidence of depression, and to elucidate the nature of such interactions. This research represents the first exploration of the relationship between the dual interactions of various chronic diseases and the development of depression. We separately attributed the possibility of depression occurrence to 12 chronic diseases that have outstanding contributions in the binary logistic regression model through dual interaction, and compared the risk of depression occurrence by adding or multiplying the risk of depression occurrence for each individual chronic disease. The most interesting thing is that from the comparison of research results, we were shocked to find that the dual interaction of chronic diseases is not a traditional synergistic effect, and chronic diseases may not necessarily have a joint effect on the occurrence of depression. The dual interaction between chronic diseases is mostly an enhancing effect, and we have also found that dual interaction with apoplexy, memory disorders, and psychosis poses a higher risk of depression. It should be emphasized here that the risk of depression is not changed by the interaction of chronic diseases. The significance of the dual interaction lies in studying whether the combination of multiple chronic diseases themselves can provide additional contributions to the occurrence of depression after studying the impact of multiple chronic diseases on depression. If chronic diseases exist in multiple comorbidities, the possibility of interaction is greater, and the risk of depression is increased.
The limitations of this study are as follows: First, the research design is cross-sectional, which precludes the establishment of causal relationships. Second, the questionnaire’s information settings were inadequate, resulting in a limited range of indicators that did not encompass all relevant diseases. This necessitates further investigation into the use of indirect indicators for determining depression. Additionally, the self-reported nature of the questionnaire introduces a potential bias. Lastly, the study’s focus on individuals aged 45 and older does not provide a comprehensive representation of the entire population.
Conclusion
The occurrence of depression in middle-aged and elderly individuals is a product of multiple factors. This study supports the view that the occurrence of chronic diseases has a significant impact on the occurrence of depression and indicates that the dual interaction of chronic diseases has a complex effect on the occurrence of depression. In addition, most of the relevant indicators used to diagnose chronic diseases cannot be directly used to diagnose depression. In contrast, indicators related to memory and cognitive function have certain reference values for the diagnosis of depression, which can be referred to according to actual situations. Also, if other indicators related to chronic diseases point to the occurrence of one or more chronic diseases, it is necessary to be vigilant about the occurrence of depression. The mechanism and causes of depression still need further improvement and in-depth research.
Data availability
All raw data is sourced from CHARLS. https://charls.charlsdata.com/
Abbreviations
- BUN:
-
Blood urea nitrogen
- BMI:
-
Body mass index
- CESD10:
-
Center for epidemiologic studies depression scale 10
- CHARLS:
-
China health and retirement longitudinal study
- CRP:
-
C-reactive protein
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- MCV:
-
Mean corpuscular volume
- PLT:
-
Platelet
- WBC:
-
White blood cell
References
Jiang, C. H., Zhu, F. & Qin, T. T. Relationships between chronic diseases and depression among middle-aged and elderly people in China: A prospective study from CHARLS. Curr. Med.Sci. 40, 858–870. https://doi.org/10.1007/s11596-020-2270-5 (2020).
Hong, A. L. sharpening our focus on chronic disease, access, and equity. Popul. Health Manag. 26, S1. https://doi.org/10.1089/pop.2023.0124 (2023).
Wang, Y. et al. Association of the depressive scores, depressive symptoms, and conversion patterns of depressive symptoms with the risk of new-onset chronic diseases and multimorbidity in the middle-aged and elderly Chinese population. EClinicalMedicine 52, 101603. https://doi.org/10.1016/j.eclinm.2022.101603 (2022).
Sharp, M. et al. Exploring the bidirectional relationship between chronic disease and depression among female Syrian refugees and Jordanians: A qualitative analysis. East Mediterr. Health J. 27, 1153–1161. https://doi.org/10.26719/emhj.21.017 (2021).
Yao, H. et al. The microbiota-gut-brain axis in pathogenesis of depression: A narrative review. Physiol. Behav. 260, 114056. https://doi.org/10.1016/j.physbeh.2022.114056 (2023).
Kingstone, T., Chew-Graham, C. A. & Corp, N. Interventions to identify and manage depression delivered by “nontraditional” providers to community-dwelling older adults: A realist review. Health Expect. 25, 2658–2679. https://doi.org/10.1111/hex.13594 (2022).
Lee, J. M. & Ryan, E. J. The relationship between muscular strength and depression in older adults with chronic disease comorbidity. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17186830 (2020).
CHARLS (2015). 2015 CHARLS Wave 3. https://charls.charlsdata.com/pages/Data/2015-charls-wave4/zh-cn.html.
Larsen, A. et al. Comparing depression screening tools (CESD-10, EPDS, PHQ-9, and PHQ-2) for diagnostic performance and epidemiologic associations among postpartum Kenyan women: Implications for research and practice. J. Affect Disord. 324, 637–644. https://doi.org/10.1016/j.jad.2022.12.101 (2023).
Wang, R. et al. The association between urbanization and depression in the elderly: A network analysis from the complexity science perspective. J. Affect Disord. 356, 72–79. https://doi.org/10.1016/j.jad.2024.04.026 (2024).
Obbels, J. et al. MMSE changes during and after ECT in late-life depression: A prospective study. Am. J. Geriatr. Psychiatry 27, 934–944. https://doi.org/10.1016/j.jagp.2019.04.006 (2019).
WHO (2023). Depressive disorder (depression). https://www.who.int/zh/news-room/fact-sheets/detail/depression.
Hsu, M. Y. et al. The interaction between exercise and marital status on depression: A cross-sectional study of the Taiwan biobank. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19031876 (2022).
Stier, A. J. et al. Evidence and theory for lower rates of depression in larger US urban areas. Proc. Natl. Acad. Sci. USA https://doi.org/10.1073/pnas.2022472118 (2021).
Delmastro, M. & Paciello, M. Depression, reduced education, and bias perceptions as risk factors of beliefs in misinformation. Sci. Rep. 12, 16408. https://doi.org/10.1038/s41598-022-20640-7 (2022).
Gan, Q. et al. Unraveling the link between hypertension and depression in older adults: a meta-analysis. Front Public Health 11, 1302341. https://doi.org/10.3389/fpubh.2023.1302341 (2023).
Manuals, M. (2024). Elevated HDL cholesterol. https://www.msdmanuals.cn/home/hormonal-and-metabolic-disorders/cholesterol-disorders/elevated-hdl-cholesterol.
Ahmed, T., Lamoureux-Lamarche, C., Berbiche, D. & Vasiliadis, H. M. The association between anemia and depression in older adults and the role of treating anemia. Brain Behav. 13, e2973. https://doi.org/10.1002/brb3.2973 (2023).
Khalfan, A. F., Campisi, S. C., Lo, R. F., McCrindle, B. W. & Korczak, D. J. The association between adolescent depression and dyslipidemia. J. Affect Disord. 338, 239–245. https://doi.org/10.1016/j.jad.2023.06.017 (2023).
Kim, J. A., Choi, S., Choi, D. & Park, S. M. Pre-existing depression among newly diagnosed dyslipidemia patients and cardiovascular disease risk. Diabetes Metab. J. 44, 307–315. https://doi.org/10.4093/dmj.2019.0002 (2020).
Holland, A. E. et al. Dyspnoea and comorbidity contribute to anxiety and depression in interstitial lung disease. Respirology 19, 1215–1221. https://doi.org/10.1111/resp.12360 (2014).
Gerald, J. K. & Moreno, F. A. Asthma and depression: It’s complicated. J. Allergy Clin. Immunol. Pract. 4, 74–75. https://doi.org/10.1016/j.jaip.2015.11.020 (2016).
Licari, A. et al. Anxiety and depression in adolescents with asthma: A study in clinical practice. Acta Biomed. 93, e2022021. https://doi.org/10.23750/abm.v93i1.10731 (2022).
Hou, R. et al. The role of inflammation in anxiety and depression in the European U-BIOPRED asthma cohorts. Brain Behav. Immun. 111, 249–258. https://doi.org/10.1016/j.bbi.2023.04.011 (2023).
Wang, L. Y., Fu, T. S., Tsia, M. C. & Hung, C. I. The associations of depression, anxiety, and insomnia at baseline with disability at a five-year follow-up point among outpatients with chronic low back pain: a prospective cohort study. BMC Musculoskelet. Disord. 24, 565. https://doi.org/10.1186/s12891-023-06682-6 (2023).
Carlson, L. E. et al. Integrative oncology care of symptoms of anxiety and depression in adults with cancer: Society for integrative oncology-ASCO guideline. J. Clin. Oncol. 41, 4562–4591. https://doi.org/10.1200/jco.23.00857 (2023).
Liu, X. et al. Association of chronic diseases with depression, anxiety and stress in Chinese general population: The CHCN-BTH cohort study. J. Affect Disord. 282, 1278–1287. https://doi.org/10.1016/j.jad.2021.01.040 (2021).
Bi, Y. H., Pei, J. J., Hao, C., Yao, W. & Wang, H. X. The relationship between chronic diseases and depression in middle-aged and older adults: A 4-year follow-up study from the China Health and Retirement Longitudinal Study. J. Affect Disord. 289, 160–166. https://doi.org/10.1016/j.jad.2021.04.032 (2021).
Acknowledgements
Thanks for providing us with data for the CHARLS.
Funding
This study was funded by Youth Science Foundation of Guangxi Medical University (GXMUYSF202332).
Author information
Authors and Affiliations
Contributions
DYL: Conceptualization, Formal analysis, Methodology, Visualization, Data analysis, Model building, Writing-original draft. XC: Software, Data curation, Validation. KHL: Project administration, Resources, Supervision, Funding acquisition, Writing-review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, Dy., Chen, X. & Li, Kh. CHARLS insights into the impact of dual interactions of chronic diseases on depression in middle-aged and elderly individuals. Sci Rep 15, 12433 (2025). https://doi.org/10.1038/s41598-025-95340-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95340-z