Abstract
Preventing venous thromboembolism (VTE) in obstetrics remains challenging, with cases still occurring despite preventive measures. The aim of this study is to investigate the underlying causes by analyzing potential issues in current postpartum VTE prevention strategies in China. This retrospective study was conducted in our hospital from May 2021 to August 2024. VTE risk was assessed using the Chinese Expert Consensus on VTE Prevention and Treatment during Pregnancy and Puerperium (Chinese Consensus), and preventive measures were implemented accordingly. Clinical variables, timing of prophylaxis, and the predictive accuracy of the Chinese Consensus were analyzed. The VTE group had higher D-dimer levels and longer hospital stays and shorter gestational ages (P < 0.05). Significant differences were observed in postpartum hemorrhage (PPH), premature birth, autoimmune diseases, and cesarean delivery (P < 0.05). Despite 65.4% receiving thromboprophylaxis, 25.2% developed VTE, with higher incidences in those without prophylaxis. Pneumatic therapy and LMWH were effective in high-risk patients (P < 0.05). Early VTE occurred 6 h postpartum, with 41.8% within 48 h. Most preventive measures were initiated at 24–48 h postpartum, potentially delaying optimal protection. The ROC analysis showed an AUC of 0.497 (P = 0.937), indicating limited predictive efficacy of the Chinese Consensus. Current postpartum VTE prevention is inadequate, as some at-risk patients still miss the opportunity for pneumatic therapy and LMWH anticoagulation after delivery. Initiating LMWH prophylaxis 24 h postpartum appears to be delayed. The predictive ability of the Chinese Consensus for assessing VTE risk is limited. Future research is essential to optimize prevention strategies and reduce the incidence of postpartum VTE.
Similar content being viewed by others
Introduction
Venous thromboembolism (VTE), encompassing pulmonary embolism (PE) and deep vein thrombosis (DVT), is a common condition with an incidence of 1 to 2 cases per 1000 pregnancies1,2. Compared to non-pregnant women, the risk of VTE is 3–10 times higher during pregnancy and 12–35 times higher in the postpartum period2,3. Despite being a potentially preventable condition, the morbidity of obstetric VTE has been increasing annually in China3. Currently, significant controversies persist regarding thromboprophylaxis in postpartum women.
Thrombosis prevention strategies include pharmacological prophylaxis, mechanical prophylaxis (e.g., pneumatic therapy and graduated compression stockings), early mobilization, hydration, and patient education4,5,6. Low-molecular-weight heparin (LMWH) has proven particularly effective in preventing VTE; however, there remains inconsistency regarding the optimal timing for initiating LMWH after delivery.
Freedman et al. reported that severe postpartum hemorrhage (PPH) is rare when enoxaparin is administered to hemostatically stable women 5–24 h after vaginal delivery or 12–36 h after cesarean section7. The American Society of Regional Anesthesia (ASRA) recommends starting LMWH prophylaxis 12 h after vaginal delivery and 24 h after cesarean delivery in high-risk thrombotic patients8. Similarly, the American College of Obstetricians and Gynecologists (ACOG) suggests initiating LMWH 4–6 h after vaginal delivery and 6–12 h postoperatively in their Practice Bulletins9. More recently, Saad et al. proposed initiating a prophylactic dose of LMWH 12 h after anesthesia, while the therapeutic dose should begin 24 h after anesthesia10. These variations highlight the need for further clinical trials to determine the optimal timing for initiating anticoagulation in the postpartum period.
Appropriate risk assessment models (RAMs) are essential for preventing thrombosis. Several VTE RAMs for obstetric patients have been proposed, including the Royal College of Obstetricians and Gynecologists (RCOG) guidelines5, the Queensland Clinical (QLD) Guideline4 and the Chinese Consensus11. The Chinese Consensus excludes certain risk factors, such as preterm birth, diabetes mellitus, assisted reproductive technology (ART), vaginal delivery transfer cesarean section, hysterectomy, and stillbirth. However, it does not account for antiphospholipid antibody syndrome (APS), which is strongly associated with thrombosis12,13. According to the Chinese Consensus, LMWH anticoagulation should be restarted 4–6 h after vaginal delivery and 6–12 h after cesarean delivery in patients with a history of pre-pregnancy VTE, provided there is no significant bleeding risk. For other patients with a VTE risk score ≥ 2, LMWH prophylaxis should begin 24 h postpartum (Supplementary Table S1).
The primary objective of this study was to evaluate the insufficiencies in postpartum VTE prevention at our hospital, with a focus on determining the optimal timing for initiating LMWH prophylaxis in Chinese women and assessing the predictive accuracy of the Chinese Consensus for VTE risk.
Methods
Study design
This retrospective study was conducted at our hospital from May 2021 to August 2024. All women diagnosed with puerperal VTE during hospitalization were assigned to the VTE group. Controls were randomly selected at a 1:3 ratio from women without puerperal VTE during the same recruitment period, given the extensive number of risk factor indicators incorporated in the Chinese Consensus. Informed consent was obtained from each participant, and the study was approved by the Medical Ethics Committee of the West China Women’s and Children’s Hospital of Sichuan University (approval number: 2024195). All methods were performed in accordance with the relevant institutional and national guidelines and regulations.
Inclusion criteria
VTE occurring after delivery and during hospitalization at our institute. Control group: Postpartum women who did not develop VTE during the study period.
Exclusion criteria
① VTE diagnosed during pregnancy; ② Suspicious but undiagnosed PE or DVT; ③ Patients with incomplete clinical data; ④ Superficial venous thrombosis (SVT) occurring during hospitalization; ⑤Patients who terminated at outside hospitals. Control group: Patients who underwent induced labor due to medical or obstetric complications after hospital admission.
Diagnosis standard
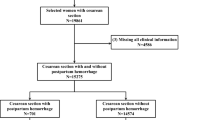
PE was confirmed by computed tomography pulmonary angiography (CTPA), while DVT was diagnosed by color Doppler ultrasonography. The selection process is shown in Fig. 1
Data collection
Demographic and clinical data were collected for each participant, including age, body mass index (BMI) before delivery, length of hospital stay, gestational age at delivery, history of VTE, and family history of VTE. Data on pregnancy-associated risk factors was also collected, including multiple pregnancies, preeclampsia, parity ≥ 3, PPH (≥ 1000 ml or blood transfusion), postnatal infection and prolonged labor (≥ 24 h), premature birth and delivery mode (vaginal delivery, elective cesarean delivery, emergency cesarean delivery and vaginal delivery transfer cesarean delivery). Maternal comorbidities were also recorded, including cancer, heart failure, severe pulmonary disease, inflammatory bowel disease and sickle cell anemia, as well as autoimmune diseases such as antiphospholipid syndrome (APS), systemic lupus erythematosus (SLE) and Sjögren’s syndrome. Antenatal immobility (defined as bed rest for ≥ 7 days) was also included. Lastly, D-dimer after delivery was also collected.
The Chinese Consensus was applied to all participants within 24 h postpartum to assess their risk of VTE. The risk was categorized into four levels: low risk (score = 0–1), medium risk (score = 2), high risk (score > 3), and very high risk (score ≥ 4). Due to the limited number of patients classified as very high risk, this group was combined with the high-risk group for the final statistical analysis. Data were subsequently collected on the initiation time of pneumatic compression therapy and LMWH prophylaxis postpartum, as well as the timing of VTE occurrence.
Statistical analysis
Results were tabulated and analyzed using the Statistical Package for Social Sciences (SPSS, version 25.0, IBM, United States). Continuous variables were tested for normality using the Shapiro–Wilk test. Quantitative data were expressed as mean ± standard deviation and compared using the Mann–Whitney U-test. Categorical data were expressed as percentages and assessed with the chi-square test or Fisher’s exact test. The Kruskal–Wallis test was applied for pairwise comparisons of multiple groups of data. The prediction effects of all the Chinese Consensus was evaluated by the AUC of ROC. For all tests, a P value < 0.05 was considered to indicate statistical significance.
Results
A total of 141 patients were included in the VTE group, comprising 69 cases of PE and 72 cases of DVT. A further 423 women without VTE were recruited as the control group (Fig. 1).
The baseline characteristics and risk factors for the VTE and control groups are summarized in Table 1. The length of stay and D-dimer were higher in the VTE group (P < 0.05) compared to the control group, while the gestational age was shorter (P < 0.001). Significant differences were also observed between the VTE and control groups for PPH, premature birth, autoimmune diseases, and delivery mode (P < 0.05). Specifically, the proportion of women undergoing elective cesarean delivery and vaginal delivery transfer cesarean were all higher in the VTE group (P < 0.05), while the proportion of women undergoing emergency cesarean delivery was higher in the control group (P < 0.05). No significant differences were found between the two groups, including age, BMI, multiple pregnancies, preeclampsia, parity ≥ 3 times, score after delivery, and other evaluated factors.
Further analysis was shown that although the differences were not statistically significant, the incidence of VTE tended to increase with higher risk scores. Meanwhile, as post-delivery risk scores increased, age and BMI also showed a corresponding increase. Women with scores ≥ 2 had significantly higher age, BMI, and length of stay compared to those with scores = 0–1, while their gestational age at delivery was significantly earlier (P < 0.001) (Table 2).
From Table 3, it can be seen that 65.4% of patients overall received thromboprophylaxis, yet 25.2% still developed VTE. Among patients who received prophylaxis, women with score = 1 experienced a higher incidence of VTE (34.1%) compared to those with score ≥ 2 (P < 0.05). In contrast, for patients who did not receive prophylaxis, there was no significant difference in VTE incidence across the various risk score groups. For patients with score ≥ 2, thromboprophylaxis appears to reduce the incidence of VTE compared to those without prophylaxis, but the difference was not statistically significant. These results are similar to those observed in clinical practice; therefore, we will continue to analyze the possible related causes.
We then explored the preventive effects of pneumatic therapy and LMWH on postpartum VTE. The results revealed that patients who did not undergo compression therapy had a significantly higher incidence of VTE, particularly among high-risk patients (43.5%) compared to women in the low risk group (14%) and medium-risk group (26.1%) (P < 0.05). Conversely, among patients who received compression therapy, the incidence of VTE was higher in the low-risk group (38.5%) compared to the medium- risk group (20.5%) and high-risk group (24.7%) (P < 0.05). This discrepancy may be attributed to the fact that patients in the medium- and high-risk groups were more likely to have received LMWH prophylaxis (Table 4).
Similarly, in the high-risk group, women who did not receive LMWH prophylaxis showed a significantly higher VTE incidence compared to moderate-risk patients (38.9% vs. 17.8%, P < 0.05). This finding highlights the important role of these two preventive strategies from another perspective. Among patients who received LMWH prophylaxis, there was no significant difference in the incidence of VTE between the medium-risk group (23.7%) and the high-risk group (27.2%) (Table 5).
Additionally, three cases of subcutaneous hematomas were reported as adverse reactions to LMWH prophylaxis (Table 5), indicating that LMWH prophylaxis is generally safe and well-tolerated.
Next, we examined the time distribution of VTE occurrence. As shown in Fig. 2, the earliest VTE event was observed at 6 h postpartum. The incidence of VTE at different time intervals was as follows: ≤ 48 h (59 cases, 41.8%), ≤ 24 h (38 cases, 27%), ≤ 72 h (32 cases, 22.7%), > 72 h (6 cases, 4.3%), and ≤ 12 h (6 cases, 4.3%), in descending order. Among them, both the low-risk and medium-risk groups showed a higher incidence of VTE within 48 h compared to other time periods (P < 0.001), while the high-risk group exhibited a higher proportion of VTE occurrences within 48 h and 72 h compared to other time periods (P < 0.001). Notably, 6 cases of VTE occurred within 12 h postpartum, even in the low-risk group, including 2 cases of PE.
Time distribution of VTE occurrence postpartum and its relationship with VTE risk scores. Time intervals represent independent periods (e.g., ≤ 24 h refers to VTE occurring between 12 and 24 h postpartum, and ≤ 48 h refers to VTE occurring between 24 and 48 h postpartum). * Indicates a statistical difference, P < 0.05.
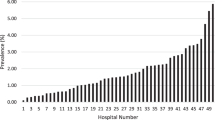
Subsequently, the timing of initiating postpartum preventive measures was investigated. The results showed that most women who received pneumatic compression therapy started within 24 h postpartum, with very few initiating therapy within the first 12 h (Fig. 3). For those who received LMWH, the majority of women in the medium-risk group (30.7%) began prophylaxis within 48 h postpartum, whereas most women in the high-risk group (40.4%) initiated treatment within 24 h postpartum (almost at the 24-h mark). Notably, only 0.4% of women in the medium-risk group started LMWH prophylaxis within 12 h postpartum (Fig. 4). The results suggest that the initiation of preventive measures appears to be delayed.
Finally, an AUC curve evaluation was conducted on 369 patients who were administered corresponding preventive measures according to the Chinese Consensus. The results indicated that the AUC value was only 0.497 (P = 0.937) (Fig. 5).
Discussion
VTE is a serious maternal complication that can occur during the antenatal or postpartum period. Despite significant advancements in the prevention of obstetric VTE, its incidence continues to rise annually14,15,16. Alarmingly, many women still develop VTE even when preventive measures are implemented. In this study, we retrospectively investigated postpartum VTE cases during hospitalization and analyzed potential shortcomings in current preventive strategies.
It has been indicated elevated D-dimer levels, PPH, autoimmune diseases, preterm birth, and cesarean delivery are closely related to thrombosis. Notably, APS, anti-phospholipid antibody positivity and SLE have been shown to significantly increase the risk of thrombosis17,18. APS and antiphospholipid antibody positivity are included as risk factors in both the RCOG guideline, and the Caprinin scoring system19,20, while the Chinese Consensus only considers active autoimmune diseases. In this study, the autoimmune diseases observed in patients were primarily APS, with few cases of SLE, none of which were active. On the other hand, the proportion of vaginal delivery transfer cesarean was significantly higher in this study. This raises concerns about the appropriateness of excluding preterm birth and vaginal delivery transfer cesarean as risk factors in the Chinese Consensus. These results indicated that the omission of these risk factors could be one of the reasons for its inadequate ability to predict VTE risk.
Previous studies have identified maternal age ≥ 35 years and BMI ≥ 30 kg/m2 as critical risk factors for VTE21,22,23. Our analysis found no significant differences in age or BMI between the VTE group and the control group overall. Nevertheless, upon stratifying patients by risk, both age and BMI increased with VTE risk level. This suggests that age and BMI remain important risk factors, but their specific cutoff values require further refinement. In addition, although our analysis found that preeclampsia had a weak association with thrombosis, consistent with previous studies14,20, its impact should not be underestimated given its distinct pathophysiological mechanisms24.
Regardless of VTE risk level, most VTE events in this study occurred within the first 24 to 48 h postpartum, with DVT and PE diagnosed as early as 6 and 9 h postpartum, respectively. However, it was observed that pneumatic therapy was generally initiated 24 h after delivery, while LMWH prophylaxis was primarily started nearly at the 24–48 h mark postpartum—aligning closely with the peak incidence of thrombosis, given the timing of VTE occurrence. Considering the low incidence of adverse reactions to LMWH and existing evidence on the timing of anticoagulation initiation7,8,9, we believe that initiating LMWH prophylaxis at 12 h postpartum may be more appropriate for patients with a low risk of bleeding. However, this recommendation requires further validation through prospective clinical studies.
Unexpectedly, despite the well-recognized importance of barometric therapy and LMWH prophylaxis, some patients at high risk of VTE still missed the appropriate preventive measures, underlying the insufficiency in postpartum VTE prevention management. In particular, adequate pneumatic therapy is relatively challenging to implement. Each session lasts only 30 min, and due to the need for abundant equipment and staff, it is often limited to once a day. Additionally, many high-risk patients did not initiate LMWH anticoagulation promptly. These may explain why some patients still develop VTE despite receiving preventive measures. Therefore, support from management is essential to enhance the effectiveness of barometric therapy and ensure timely initiation of LMWH anticoagulation.
As demonstrated in the study, 27.7% of women classified as low risk still developed VTE, highlighting the limited recognition capability of the Chinese Consensus to some extent. Effective clinical decision-making relies heavily on an accurate assessment of VTE risk. To evaluate the identification ability of the Chinese Consensus, we analyzed its performance and found that the AUC was only 0.497, with no statistically significant difference. Moreover, a comparison between the Chinese Consensus and ROCG risk stratification revealed that the stratification ability of ROCG was also suboptimal (Supplementary Table 2). This reveals the inadequate of current RAMs and emphasizes the necessity of developing a new model.
Generally, factors such as elevated D-dimer levels, PPH, autoimmune diseases, preterm birth, and cesarean delivery are significantly associated with an increased risk of VTE. However, there are notable deficiencies in VTE prevention. Pneumatic therapy and LMWH prophylaxis should be implemented whenever possible to minimize the risk of oversight. For patients with a low risk of bleeding, initiating LMWH prophylaxis at 12 h postpartum may be more appropriate. But the most appropriate timing for initiating anticoagulation still requires further exploration. The predictive ability of the Chinese Consensus for VTE remains inadequate, emphasizing the need for a new, optimized RAM to improve the prevention and management of VTE during the puerperium.
Several limitations should be considered when interpreting the results of this retrospective study. First, the characteristics of the control group are critical and may vary depending on the definition used, thus potentially introducing bias. Second, the sample size was relatively small, thereby reducing the statistical power to detect differences. Third, the study was conducted at a single center, which may limit the generalizability of the findings to other healthcare settings.
Conclusions
This study highlights substantial deficiencies in current postpartum VTE prevention strategies among Chinese women, including delayed initiation of LMWH prophylaxis and the limited predictive ability of the Chinese Consensus. Importantly, some patients at risk of thrombosis still did not receive appropriate preventive measures. Early initiation of LMWH at 12 h postpartum may be more appropriate for patients with a low risk of bleeding, but further prospective studies are needed to validate this approach. Additionally, the development of an optimized risk assessment model is essential to improve the prevention and management of VTE during the puerperium.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request. Please contact [zhusha_hxey@163.com] for access to the data.
Abbreviations
- VTE:
-
Venous thromboembolism
- LMWH:
-
Low molecular weight heparin
- PE:
-
Pulmonary embolism
- DVT:
-
Deep vein thrombosis
- RAMs:
-
Risk assessment models
- Chinese Consensus:
-
Chinese Expert Consensus on the Prevention and Treatment of VTE during Pregnancy and Puerperium
- QLD:
-
Queensland Clinical Guideline
- ASRA:
-
American Society of Regional Anesthesia
- ACOG:
-
American College of Obstetricians and Gynecologist
- RCOG:
-
Royal College of Obstetricians and Gynecologists
- BMI:
-
Body mass index
- AUC:
-
Area under the curve
- ROC:
-
Receiver operating characteristic
- ART:
-
Assisted reproductive technology
- APS:
-
Antiphospholipid syndrome
- PPH:
-
Postpartum hemorrhage
References
Bates, S. M., Middeldorp, S., Rodger, M., James, A. H. & Greer, I. Guidance for the treatment and prevention of obstetric-associated venous thromboembolism. J Thromb Thrombolysis. 41, 92–128 (2016).
Maughan, B. C. et al. Venous thromboembolism during pregnancy and the postpartum period: Risk factors, diagnostic testing, and treatment. Obstet Gynecol Surv. 77, 433–444 (2022).
Zhao, Z., Zhou, Q. & Li, X. Missed opportunities for venous thromboembolism prophylaxis during pregnancy and the postpartum period: evidence from mainland China in 2019. BMC Pregnancy Childbirth. 21, 1–7 (2021).
Queensland Clinical Guidelines. Maternity and Neonatal Clinical Guideline Venous thromboembolism (VTE) prophylaxis in pregnancy and the puerperium. Queensl Gov. 2014;1–25. www.health.qld.gov.au/qcg.
(RCOG) Royal College of Obstetricians and Gynaecologists. Reducing the Risk of Venous Thromboembolism during Pregnancy and the Puerperium Green-top Guideline No. 37a. 2015; 40. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg-37a.pdf.
Oakes, M. C. et al. Efficacy of postpartum pharmacologic thromboprophylaxis: A systematic review and meta-analysis. Obstet Gynecol. 141, 697–710 (2023).
Freedman, R. A., Bauer, K. A., Neuberg, D. S. & Zwicker, J. I. Timing of postpartum enoxaparin administration and severe postpartum hemorrhage. Blood Coagul Fibrinolysis. 19, 55–59 (2008).
Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp SL, Benzon HT, et al. Regional Anesthesia in the patient receiving antithrombotic or thrombolytic therapy; American Society of Regional Anesthesia and Pain Medicine evidence-based guidelines (Third Edition). Reg Anesth Pain Med. 2010;35:64–101.
ACOG Practice Bulletin No. 197: Inherited Thrombophilias in Pregnancy. Obstet Gynecol. 2018;132:e18–34.
Saad, A., Safarzadeh, M. & Shepherd, M. Anticoagulation regimens in pregnancy. Obstet Gynecol Clin North Am. 50, 241–249. https://doi.org/10.1016/j.ogc.2022.10.010 (2023).
The Obstetrics and Gynecology Group of Chinese Medical Association. Expert consensus on the prevention and diagnosis of venous thromboembolism during pregnancy and the puerperium. Chin J of Obstet and Gynecol. 2021;56:236–43.
Soto-Peleteiro, A., Gonzalez-Echavarri, C. & Ruiz-Irastorza, G. Obstetric antiphospholipid syndrome. Med Clin (Barc). 163(Suppl), S14-21 (2024).
Sammaritano, L. R. Antiphospholipid syndrome. Best Pract Res Clin Rheumatol. 34, 101463 (2020).
Chen, X., Peng, W., Zhang, Y., Zhou, H. & Zhang, M. Development and validation of a facile rapid assessment scale for perinatal venous thromboembolism in puerperium in Chinese women. BMC Pregnancy Childbirth. 23, 1–10 (2023).
Chen, M. et al. Benefits and risks of low molecular weight heparin use on reproductive outcomes: A retrospective cohort study. Taiwan J Obstet Gynecol. 61, 812–817. https://doi.org/10.1016/j.tjog.2022.05.015 (2022).
Merriam, A. A. et al. Postpartum thromboembolism prophylaxis during delivery hospitalizations. Am J Perinatol. 35, 873–881 (2018).
Branch, D. W. & Lim, M. Y. How I diagnose and treat antiphospholipid syndrome in pregnancy. Blood 143, 757–768 (2024).
You H, Zhao J, Zhang M, Jin Z, Feng X, Tan W, et al. Development and external validation of a prediction model for venous thromboembolism in systemic lupus erythematosus. RMD Open. 2023;9.
Cronin, M. A., Dengler, N., Krauss, E. S., Segal, A., Wei, N., Daly, M., et al. Completion of the updated Caprini risk assessment model (2013 Version). Clin. Appl. Thromb. 2019;25.
Liu, H., Li, L. & Zhao, Z. Values of Caprini risk assessment scale and D-dimer for predicting venous thromboembolism during puerperium. Int J Womens Health. 2024(16), 47–53 (2023).
Bates, S. M. et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: Venous thromboembolism in the context of pregnancy. Blood Adv. 2, 3317–3359 (2018).
Lian, Y., Li, J., Liang, W. & Zhong, M. Comparison and validation of different risk assessment models in patients with venous thromboembolism during pregnancy and postpartum: A retrospective study in China. Int J Gen Med. 2023(16), 95–106 (2022).
Blondon, M., Skeith, L. Preventing postpartum venous thromboembolism in 2022: A narrative review. Front. Cardiovasc. Med. 2022;9 April:1–7.
Havers-Borgersen, E. et al. Preeclampsia and long-term risk of venous thromboembolism. JAMA Netw Open. 6, e2343804 (2023).
Acknowledgements
The authors are grateful to all the doctors who performed the VTE scores by Chinese Consensus.
Author information
Authors and Affiliations
Contributions
Sha Zhu and Yonghui Xu led the study design, data collection and results interpretation. Yonghui Xu conducted data cleaning, data analysis and manuscript writing. Fei Xiao and Xinsheng Xue led protocol development and results interpretation. Ji He and Yngting Li provided partial important advices. All authors critically reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Medical Ethics Committee of the West China Women’s and Children’s Hospital of Sichuan University (approval number: 2024195).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, Y., Xiao, F., He, J. et al. Analysis on the causes of unsatisfactory prevention effect of postpartum VTE in Chinese women. Sci Rep 15, 11029 (2025). https://doi.org/10.1038/s41598-025-95790-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95790-5