Abstract
Evidence on the association between the non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and Helicobacter pylori (H. pylori) infection remains limited. This study investigates this correlation based on the U.S. population. This cross-sectional research included data on 834 U.S. participants from the National Health and Nutrition Examination Survey 1999–2000. The association between the NHHR and H. pylori infection was examined using logistic regression models, restricted cubic spline (RCS) curve and subgroup analyses. Individuals with H. pylori infection exhibited significantly higher NHHR value. A significant positive association between NHHR and H. pylori infection was observed across all three models, even after adjusting for potential confounders, with a stronger association noted in males, individuals under 60 years of age, and non-Hispanic White participants. These findings suggest NHHR may act as a non-invasive biomarker for detecting H. pylori infection in U.S. populations.
Similar content being viewed by others
Introduction
Helicobacter pylori (H. pylori), a prevalent Gram-negative bacterium, classified as a Group I carcinogen by the World Health Organization1. Recent statistics estimate the global prevalence of H. pylori infection at approximately 43.9% over the past decade2. H. pylori can persistently colonize the human stomach, resulting in chronic gastric mucosal inflammation, potentially progressing to severe gastroduodenal conditions3,4. H. pylori has been linked to a range of systemic diseases5, including metabolic disorders, gut dysbiosis, and cardiovascular conditions6,7,8. Therefore, given the wide-reaching implications of H. pylori infection, identifying modifiable, noninvasive potential indicators for its detection is critical for reducing the incidence of both gastroduodenal and systemic associated diseases9. Given that blood tests are simple and routinely used in clinical practice, identifying novel biomarkers from the blood to assess an individual’s infection status is important for improving current strategies for H. pylori prevention and treatment.
Previous research has indicated that H. pylori infection may influence nutrient absorption and contribute to dyslipidemia10, particularly in studies focusing on high-density lipoprotein cholesterol (HDL-C), which plays a vital role in immune regulation as an anti-inflammatory and antioxidant plasma lipoprotein11,12. However, there is controversy regarding the correlation between H. pylori infection and HDL-C levels, with some studies reporting significantly lower HDL-C levels in infected individuals, and others find no such association13,14. Additionally, the effect of eliminating H. pylori on HDL-C has been inconsistent, leaving the relationship unclear10,15.
Recently, the non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) has become a composite marker of lipid metabolism compared with other traditional indices. It has a superior predictive capacity compared with HDL-C in various diseases, such as cardiovascular diseases, urinary stones, metabolic disease, and psychological disorders16,17,18,19. Nevertheless, nothing is known about the possible relationship between H. pylori infection and the NHHR.
This study aims to investigate the relationship between the NHHR and H. pylori infection by analyzing dataset from the National Health and Nutrition Examination Survey (NHANES) carried out in U.S. between 1999 and 2000. Clarifying this association could provide insight into the connection between H. pylori infection and lipid metabolism disorders, potentially aiding in early H. pylori infection detection and prevention of its associated diseases.
Materials and methods
Study design and population
The National Center for Health Statistics (NCHS) conducts the publicly available, cross-sectional NHANES survey, which collects data representative of the U.S. noninstitutionalized civilian population20. Numerous data categories are encompassed in the scope of NHANES database, including demographic, dietary, laboratory, examination and questionnaire-based information. Written informed agreements were obtained from all participants, and the research procedures and methods were approved by NCHS Research Ethics Review Board.
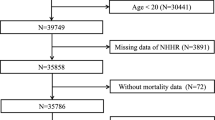
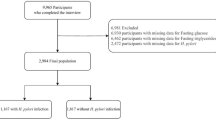
In this study, data from 9965 U.S. individuals were derived from the NHANES 1999–2000, as the assessment of H. pylori serological infection status was limited to this cycle. After excluding 2472 participants without H. pylori serology infection status data, a cohort of 7493 individuals with relevant serological data was established. Following further exclusion screening, 834 participants were ultimately selected for analysis. These individuals were further stratified into two categories, “H. pylori-seronegative” and “H. pylori-seropositive”, based on the results of enzyme-linked immunoassay (ELISA) for the detection of H. pylori immunoglobulin G (IgG) antibodies. Figure 1 showed the flowchart of U.S. participants participating in the study.
Assessment of H. pylori infection status
For U.S. participants, H. pylori IgG antibodies were assessed via ELISA on serum samples (Wampole Laboratories, Cranbury, NJ). Based on standard ELISA thresholds, participants were classified as “H. pylori-seropositive” [optical density (OD) value ≥ 1.1] or “H. pylori-seronegative” (OD value < 0.9), with individuals showing ambiguous OD values (0.9–1.1) excluded to minimize bias21.
Assessment of NHHR
The NHHR served as a primary exposure variable and calculated as follows: Non-HDL-C level/HDL-C level16. Among them, the HDL-C level was subtracted from total cholesterol (TC) level to obtain Non-HDL-C level22. The NHHR was investigated as continuous and categorical variable. All individuals were stratified into quartiles (Quartile 1–4), with Quartile 1 serving as the reference. Additionally, triglycerides (TG), remnant cholesterol (RC), low-density lipoprotein-cholesterol (LDL-C) and TC were selected as continuous variables to evaluate lipid metabolism status.
Covariates
A multitude of factors linked to H. pylori infection and lipid metabolism were identified in previous studies. In this study for the U.S. participants, covariates included sex, age, race, education, body mass index (BMI), income-to-poverty ratio (PIR), waist circumference (WC), smoking, drinking, diabetes, hypertension and physical activity. Among them, sex, race, education, smoking and drinking behavior, hypertension, diabetes mellitus and physical activity were applied as categorical variables; age, PIR, WC, and BMI were applied as continuous variables. Additional comprehensive details on the aforementioned covariates and the methodology for their measurement is available in open-access format from the NHANES webpage.
Statistical analyses
Student’s t-test was employed to compare normally distributed continuous variables, which were reported as means ± standard deviations (SD). Frequencies and percentages representing categorical variables were displayed, and chi-square or Fisher’s exact tests were applied for comparisons as applicable. The relationship between H. pylori positive and the NHHR was evaluated by logistic regression model, with results reported as odds ratios (ORs) and 95% confidence intervals (CIs). Three models with varying degrees of progression were established in order to adjust for confounding variables. Model 1 remained unadjusted; Model 2 was adjusted for gender, age and ethnicity; and Model 3 further adjusted for gender, age, ethnicity, education, PIR, diabetes, hypertension, smoking and alcohol behavior, WC, BMI and physical activity. Furthermore, the linear relationship between H. pylori seropositivity and NHHR was analyzed with the restricted cubic spline (RCS) plots. Additionally, according to the aforementioned adjustment models, subgroup analyses were conducted by sex, gender, and ethnicity. A statistically significant result was defined as a two-sided P < 0.05. R software version 4.1.1 (www.rproject.org) and SPSS software version 26.0 (IBM, Chicago, IL, USA) were employed for statistical analyses.
Results
Baseline characteristics of individuals stratified by H. pylori infection status
A final sample of 834 U.S. individuals was analyzed. Among these individuals, 487 (58.39%) were H. pylori-seronegative, whereas 347 (41.61%) were H. pylori-seropositive (Fig. 1). The average age of the total individuals was 48.51 ± 17.84 years, and 50.48% were male. Age, race, educational attainment, PIR, alcohol behavior, and physical activity all presented the statistically significant differences between the two groups. Participants who were H. pylori-seropositive exhibited lower HDL-C levels and higher TG and RC levels compared to their H. pylori-seronegative counterparts (P < 0.05). Moreover, the NHHR was significantly elevated among H. pylori-seropositive participants (P < 0.05). Table 1 presented a detailed summary of the baseline characteristics of U.S. participants categorized by H. pylori infection status.
Baseline characteristics of individuals stratified by the NHHR quartile
To further evaluate distributional disparities, individuals were divided into four quartiles (Q) based on their NHHR values (Table 2). Those in higher NHHR quartiles presented an increased H. pylori infection prevalence compared to individuals in lower quartiles (P < 0.05). Additionally, participants in the higher quartiles were more probable to be elder males with lower levels of educational, were more frequently smokers, and demonstrated higher WC, BMI, TC, Non-HDL-C, LDL-C, TG and RC levels (P < 0.05).
Associations between the NHHR and H. pylori infection
Among the U.S. participants (Table 3), the NHHR demonstrated a statistically significant positive correlation with H. pylori infection across all three models when considered as a continuous variable (P < 0.05). Similarly, each of the three models showed a remarkable positive relationship between H. pylori infection and the highest quartile (Quartile 4) of the NHHR when it was analyzed as a categorical variable (P < 0.05).
RCS analysis
RCS method was employed to investigate the potential nonlinear relationship between NHHR and H. pylori infection. A positive linear association between NHHR and H. pylori infection was observed across all three models (Fig. 2).
Subgroup analyses
To further explore the link between the NHHR and H. pylori infection, participants were subgroup analyzed by sex, age, and race. For the U.S. participants in all three models (Table 4), a statistically remarkable positive association between the NHHR and H. pylori infection was observed in males when stratified by sex (P < 0.05). In individuals aged < 60 years, the positive association was also significant (P < 0.05). Additionally, stratified by race, a statistically positive association was identified in non-Hispanic White individuals in all three models, whereas a remarkable negative association was found in other Hispanic individuals in Model 2 and 3 (P < 0.05).
Discussion
Based on large sample sizes of NHANES 1999–2000 databases, this study is the first to find that higher NHHR values were positively associated with H. pylori infection. Furthermore, subgroup analysis indicated that this association remained significantly positive among male participants under the age of 60 and non-Hispanic, White participants among U.S. participants.
The NHHR is a novel lipid parameter developed to predict the risk of lipid metabolism-related diseases, such as nonalcoholic fatty liver disease, diabetes and atherosclerosis23,24,25. By comprehensively incorporating information regarding both protective and harmful lipid particles, the NHHR may more accurately represent the balance between these two types of lipoproteins than traditional lipid indices. Recent studies have increasingly linked an elevated NHHR to inflammatory diseases such as sepsis, periodontitis and chronic obstructive pulmonary disease26,27,28. H. pylori persistently colonize in the stomach, eliciting chronic immune responses and inflammation within the gastrointestinal tract. However, the link between the NHHR and H. pylori infection remains unexplored.
While direct evidence linking the NHHR and H. pylori infection is lacking, several studies have identified associations between various traditional lipid-related parameters and H. pylori infection. A meta-analysis by Upala et al. in 2016 reported a strong association between H. pylori infection and lower HDL-C levels29. Additionally, prior studies reported that individuals with H. pylori infection had elevated LDL-C, TC, and TG levels compared to uninfected individuals, with a positive link between LDL-C and TC levels and H. pylori density30,31. Furthermore, successful H. pylori eradicating has been shown to partially restore the imbalanced lipid profiles mentioned above32,33. Despite various studies demonstrating the significant relationships between lipid-related parameters and H. pylori infection, some recent studies have yielded inconsistent conclusions34,35. In 2024, Ozturk et al. performed a retrospective observational study and revealed no significant associations between H. pylori infection and conventional lipid-related parameters35. Similarly, another study conducted in China found no significant differences in lipid parameters, including TC, HDL-C, LDL-C and TG, between individuals with and without H. pylori infection36. Nontraditional lipid-related parameters, including RC and LDL-C/HDL-C, were also found to have no significant correlation with H. pylori infection35. In this investigation, it was discovered that H. pylori infection was substantially related to higher levels of TC, LDL-C, Non-HDL-C, RC and TG in U.S. populations, along with lower HDL-C levels. For the novel composite lipid-related index NHHR, a strong positive link with H. pylori infection was observed. These results imply that the correlation between lipid metabolism and H. pylori infection may vary by ethnicity, warranting further exploration through larger sample studies in the future.
Although the precise association between the NHHR and H. pylori infection remains unclear, several potential pathogenic hypotheses may help elucidate this correlation. H. pylori infection may affect the lipid metabolism through the upregulation of inflammation-related cytokines, which can inhibit lipoprotein lipase activity, leading to the decreased HDL-C levels and increased TG levels37,38. Additionally, various studies shown that gastric mucosal atrophy induced by H. pylori disrupts the homeostasis of leptin and ghrelin, contributing to nutritional absorption imbalances and blood lipid profiles dysregulation, including Non-HDL-C and HDL-C39. Nevertheless, the effect of lipid metabolism disorders on H. pylori infection has not yet been reported. Previous researches have indicated that obesity might increase the risk of H. pylori infection by dampening immune response40. It was hypothesized that lipid disorders may also lead to a weakened immune response, increasing susceptibility to H. pylori infection, suggesting a bidirectional correlation between lipid metabolism disorders and H. pylori infection.
Subgroup analyses in this research indicated the adjusted correlation between the NHHR and H. pylori infection was significantly stronger among males, those aged < 60 years and non-Hispanic White individuals, whereas it was less pronounced among other Hispanic individuals within the U.S. cohort. Previous studies have shown that H. pylori infection varies by sex, age and ethnicity, with higher susceptibility in older, male and non-Hispanic, Black individuals41. Seo et al. reported that H. pylori may influence lipid profiles with potential sex-specific differences42. Given that the NHHR is a new composite lipid-related predictor of atherosclerosis, a comparative investigation in 2019 suggested that H. pylori infection specifically increases the risk of carotid atherosclerosis among young males43. This study aligns with this finding, revealing a significantly higher NHHR level with H. pylori infection in young males in the U.S. population. Nonetheless, research addressing ethnic-specific differentiation on correlation between H. pylori infection and lipid profiles is lacking, highlighting an area for future exploration.
At present, this study firstly investigates the relationship between the NHHR and H. pylori infection. Based on U.S. population cohort with large sample size, it was concluded that the NHHR was positively correlated with H. pylori infection, providing new evidence for the relationship between lipid metabolism disorders and H. pylori infection. These findings suggest that NHHR could serve as a potential biomarker for identifying individuals at higher risk of H. pylori infection, particularly in specific demographic subgroups such as young males and non-Hispanic White individuals. If validated in future studies, NHHR could be integrated into clinical practice for risk stratification and early intervention strategies aimed at reducing the burden of H. pylori-related diseases.
There were several limitations considered in the study. First of all, as serological data for H. pylori infection were accessible solely during the NHANES 1999–2000, the data for U.S. participants were limited to this timeframe. Moreover, since the NHANES database provides only serological data, it was difficult to differentiate between past and current infection statuses among H. pylori-seropositive participants. However, serological testing remains a widely adopted and practical method for evaluating H. pylori infection in large-scale epidemiological studies, given its non-invasive characteristics, cost-efficiency, and applicability in extensive population-based research. Third, as this was a retrospective study, it was not feasible to assess changes in the NHHR following H. pylori eradication. Finally, it is challenging to prove a causal relationship between the NHHR and H. pylori infection for this study is cross-sectional. Despite these limitations, our findings provide a foundation for future longitudinal studies to explore the causal mechanisms underlying the observed associations and to validate the utility of NHHR as a predictive marker across diverse populations.
Conclusion
In conclusion, the NHHR was positively associated with H. pylori infection in U.S. populations, highlighting the potential role of lipid metabolism in the pathogenic mechanism of H. pylori infection. These findings suggest that NHHR testing could serve as a valuable tool for clinicians in assessing H. pylori infection risk and mitigating associated diseases. Future research should investigate causal mechanisms through longitudinal studies, validate the predictive value of NHHR in different populations, such as across diverse ethnic groups, and explore its utility in intervention strategies.
Data availability
The NHANES and clinical datasets used in this study are available upon the National Health and Nutrition Examination Survey website (http://www.cdc.gov/nchs/nhanes/).
References
Malfertheiner, P. et al. Helicobacter pylori infection. Nat. Rev. Dis. Primers. 9, 19 (2023).
Chen, Y. C. et al. Global prevalence of Helicobacter pylori infection and incidence of gastric cancer between 1980 and 2022. Gastroenterology 166, 605–619 (2024).
Denic, M., Touati, E., De Reuse, H. & Review Pathogenesis of Helicobacter pylori infection. Helicobacter 25 (Suppl 1), e12736 (2020).
Malfertheiner, P. et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut 66, 6–30 (2017).
Kuo, C. H., Chen, Y. H., Goh, K. L. & Chang, L. L. Helicobacter pylori and systemic disease. Gastroenterol. Res. Pract. 358494 (2014).
Chen, C. C. et al. The interplay between Helicobacter pylori and Gastrointestinal microbiota. Gut Microbes. 13, 1–22 (2021).
Wang, F. et al. Research progress on Helicobacter pylori infection related neurological diseases. Ageing Res. Rev. 99, 102399 (2024).
He, J. et al. Helicobacter pylori and unignorable extragastric diseases: mechanism and implications. Front. Microbiol. 13, 972777 (2022).
Boubrik, F. & Belmouden, A. El Kadmiri, N. Potential Non-invasive biomarkers of Helicobacter pylori-Associated gastric cancer. J. Gastrointest. Cancer. 53, 1113–1120 (2021).
Shiotani, A., Miyanishi, T., Uedo, N. & Iishi, H. Helicobacter pylori infection is associated with reduced Circulating Ghrelin levels independent of body mass index. Helicobacter 10, 373–378 (2005).
Fernandes das Neves, M., Batuca, J. R. & Delgado Alves, J. The role of high-density lipoprotein in the regulation of the immune response: implications for atherosclerosis and autoimmunity. Immunology 164, 231–241 (2021).
Navab, M., Anantharamaiah, G. M. & Fogelman, A. M. The role of high-density lipoprotein in inflammation. Trends Cardiovasc. Med. 15, 158–161 (2005).
Shimamoto, T. et al. The association of Helicobacter pylori infection with serum lipid profiles: an evaluation based on a combination of meta-analysis and a propensity score-based observational approach. PLoS One. 15, e0234433 (2020).
Sun, Y., Fu, D., Wang, Y. K., Liu, M. & Liu, X. D. Prevalence of Helicobacter pylori infection and its association with lipid profiles. Bratisl Lek Listy. 117, 521–524 (2016).
Upala, S., Sanguankeo, A., Saleem, S. A. & Jaruvongvanich, V. Effects of Helicobacter pylori eradication on insulin resistance and metabolic parameters: a systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 29, 153–159 (2017).
Yu, B. et al. The non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) as a predictor of all-cause and cardiovascular mortality in US adults with diabetes or prediabetes: NHANES 1999–2018. BMC Med. 22, 317 (2024).
Du, Y. Z. et al. A cross-sectional analysis of the relationship between the non-high density to high density lipoprotein cholesterol ratio (NHHR) and kidney stone risk in American adults. Lipids Health Dis. 23, 158 (2024).
Tan, M. Y. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio with type 2 diabetes mellitus: recent findings from NHANES 2007–2018. Lipids Health Dis. 23, 151 (2024).
Qi, X. et al. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and risk of depression among US adults: A cross-sectional NHANES study. J. Affect. Disord. 344, 451–457 (2024).
Wu, W. T. et al. Data mining in clinical big data: the frequently used databases, steps, and methodological models. Mil Med. Res. 8, 44 (2021).
Meier, H. C. S. et al. Helicobacter pylori seropositivity is associated with antinuclear antibodies in US adults, NHANES 1999–2000. Epidemiol. Infect. 148, e20 (2020).
Raja, V. et al. Non-HDL-cholesterol in dyslipidemia: review of the state-of-the-art literature and outlook. Atherosclerosis 383, 117312 (2023).
Yang, S. et al. Association between the non-HDL-cholesterol to HDL-cholesterol ratio and non-alcoholic fatty liver disease in Chinese children and adolescents: a large single-center cross-sectional study. Lipids Health Dis. 19, 242 (2020).
Sheng, G. et al. Utility of Non-High-Density lipoprotein cholesterol to High-Density lipoprotein cholesterol ratio in evaluating incident diabetes risk. Diabetes Metab. Syndr. Obes. 15, 1677–1686 (2022).
Wang, A. et al. Non-HDL-C/HDL-C ratio is associated with carotid plaque stability in general population: A cross-sectional study. Front. Neurol. 13, 875134 (2022).
Wu, R. & Gong, H. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio and chronic obstructive pulmonary disease: the mediating role of dietary inflammatory index. Front. Nutr. 11, 1427586 (2024).
Hou, K., Song, W., He, J. & Ma, Z. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and prevalence of periodontitis among US adults: a cross-sectional NHANES study. Sci. Rep. 14, 5558 (2024).
Zhang, Y. & Zheng, X. Association of 28-day mortality with non-high-density lipoprotein cholesterol and the high-density lipoprotein cholesterol ratio (NHHR) in patients with sepsis: results of MIMIC-IV database analysis. Lipids Health Dis. 23, 255 (2024).
Upala, S., Jaruvongvanich, V., Riangwiwat, T., Jaruvongvanich, S. & Sanguankeo, A. Association between Helicobacter pylori infection and metabolic syndrome: a systematic review and meta-analysis. J. Dig. Dis. 17, 433–440 (2016).
Kucukazman, M. et al. The relationship between updated Sydney system score and LDL cholesterol levels in patients infected with Helicobacter pylori. Dig. Dis. Sci. 54, 604–607 (2008).
Xie, J., Wang, J., Zeng, R. & Xie, Y. Association between Helicobacter pylori infection and triglyceride levels: a nested cross-sectional study. Front. Endocrinol. 14, 1220347 (2023).
Wang, Z. et al. Eradication of Helicobacter pylori alleviates lipid metabolism deterioration: a large-cohort propensity score-matched analysis. Lipids Health Dis. 21, 34 (2022).
Iwai, N. et al. Helicobacter pylori eradication increases the serum high density lipoprotein cholesterol level in the infected patients with chronic gastritis: A single-center observational study. PLoS One. 14, e0221349 (2019).
Eslami, O., Shahraki, M., Shahraki, T. & Ansari, H. Association of Helicobacter pylori infection with metabolic parameters and dietary habits among medical undergraduate students in southeastern of Iran. J. Res. Med. Sci. 22, 12 (2017).
Ozturk, S. et al. Traditional and nontraditional lipid parameters in Helicobacter pylori infection. Biomark. Med. 18, 291–300 (2024).
Fang, Y., Fan, C., Li, Y. & Xie, H. The influence of Helicobacter pylori infection on acute coronary syndrome and lipid metabolism in the Chinese ethnicity. Front. Cell. Infect. Microbiol. 14, 1437425 (2024).
Makoveichuk, E., Vorrsjo, E., Olivecrona, T. & Olivecrona, G. TNF-alpha decreases lipoprotein lipase activity in 3T3-L1 adipocytes by up-regulation of angiopoietin-like protein 4. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids. 1862, 533–540 (2017).
Sheu, W. H. H., Lee, W. J., Chang, R. L. & Chen, Y. T. Plasma tumor necrosis factor alpha levels and insulin sensitivity in hypertensive subjects. Clin. Exp. Hypertens. 22, 595–606 (2000).
Roper, J. et al. Leptin and Ghrelin in relation to Helicobacter pylori status in adult males. J. Clin. Endocrinol. Metab. 93, 2350–2357 (2008).
Yang, G. H. et al. Obesity associated with increased risk of gastric Helicobacter pylori infection in an elderly Chinese population. J. Am. Geriatr. Soc. 62, 190–192 (2014).
Shah, S. C. et al. Helicobacter pylori burden in the united States according to individual demographics and geography: A nationwide analysis of the veterans healthcare system. Clin. Gastroenterol. Hepatol. 22, 42–50 (2024). e26.
Seo, K. I. et al. Sex differences betweenHelicobacter pyloriinfection and cholesterol levels in an adult health checkup program. Helicobacter 25, e12704 (2020).
Zhang, L. et al. Helicobacter pylori infection selectively increases the risk for carotid atherosclerosis in young males. Atherosclerosis 291, 71–77 (2019).
Acknowledgements
This work was supported by the Key Laboratory Project of Digestive Diseases in Jiangxi Province (2024SSY06101), and Jiangxi Clinical Research Center for Gastroenterology (20223BCG74011).
Funding
This manuscript was supported by the National Natural Science Foundation of China (No. 82270593 and No. 82200628), and China Postdoctoral Science Foundation (No. 2023M731495).
Author information
Authors and Affiliations
Contributions
JQ, DL, CW and HC collected data, analyzed relevant information, and drafted the manuscript. JX, SC, YW and FZ contributed to statistical analysis. JF and QL contributed to manuscript revision. RZ and YX designed the study, critically revised the paper and approved the final submission. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qiu, J., Liu, D., Wu, C. et al. Association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio and Helicobacter pylori infection. Sci Rep 15, 12560 (2025). https://doi.org/10.1038/s41598-025-96851-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-96851-5