Abstract
Hospital organisations aim to restore patients’ health and improve their comfort. Furthermore, nurses are obligated to provide quality nursing care to patients. A hospital’s positive culture, interpersonal caring behaviour, and organisational health are important factors related to nursing quality. This study aimed to identify the factors that affected the quality of nursing care and verify the mediating effect of hospital organisational health on the relationship between positive nursing organisational culture, caring behaviour, and quality of nursing care. Data were collected from 190 clinical nurses who had worked for over 6 months in a tertiary hospital located in C city, South Korea. Descriptive statistics, independent t-test and one-way analysis of variance, Scheffe’s post-hoc test, Pearson’s correlation coefficient, hierarchical regression, and Baron and Kenny’s 3-stage procedures were calculated via SPSS version 25.0. Mediating effects were verified via bootstrapping. Hospital organisational health (β = 0.47, p < 0.001), ‘satisfied’ in departmental satisfaction (β = 0.26, p = 0.034), ‘surgical ward’ (β = 0.15, p = 0.017), ‘operating room/delivery room’ (β = 0.13, p = 0.023), ‘neonatal intensive care unit/nursery’ (β = 0.13, p = 0.039), and ‘outpatient department’ (β = 0.14, p = 0.018) in department of work were all factors that affected the quality of nursing care. Furthermore, these had significant effects, with an explanatory power of 57.2% (F = 10.70, p < 0.001). Hospital organisational health had a full mediating effect on the relationship between positive nursing organisational culture and quality of nursing care (B = 0.27, 95% BootCI = 0.18–0.37), as well as between caring behaviours among nurses and quality of nursing care (B = 0.21, 95% BootCI = 0.14–0.28). Practical measures to enhance nursing quality based on these findings should improve work and environmental conditions at the organisational level. In addition, measures to foster and manage a positive nursing organisational culture and promote various caring behaviour enhancement programs to improve hospital organisational health are recommended.
Similar content being viewed by others
Introduction
Nursing quality, defined as excellence in care whereby nurses provide patients with individualized and appropriate attention (Liu, 2014), is crucial in healthcare. It directly impacts patient outcomes and safety indicators, such as mortality, patient satisfaction falls, hospital-acquired infections, and medication administration errors, which collectively serve as important markers of a hospital’s performance (McHugh and Stimpfel, 2012; Tvedt et al. 2014; Yu et al. 2021). In addition, improving nursing quality not only enhances professionalism (Kim et al. 2003) but also builds trust in the nursing profession among patients, healthcare managers, and medical staff (Shin et al. 2017).
Several factors influence nursing quality, including the individual capabilities of organizational members, the physical environment, nursing organizational culture, and hospital policies (Klopper et al. 2012). Among these, nursing organizational culture stands out as a key factor, enabling efficient organizational management through shared values and behaviours among nurses to achieve the organization’s goals (Shin et al. 2017; Srimulyani and Hermanto, 2022). A positive nursing organizational culture, characterized by behaviour patterns, norms, and expectations that positively shape members’ thoughts and actions (Kim and Kim, 2021), enhances job satisfaction, self-development, and proactive job performance at the individual level, while at the organizational level it leads to more effective delivery of high-level medical services (Yom et al. 2014).
Care is fundamental to nursing (Coates, 2002). The Quality Caring Model by Duffy and Hoskins (2003) provides a comprehensive framework that encompasses four caring relationships—self, patients and families, each other, and communities—along with various caring factors like encouraging manners, mutual problem solving, affiliation needs, a healing environment, and human respect (Edmundson, 2012). Understanding the relationship between care and nursing practice, and its impact on nursing outcomes, is critical for expanding knowledge in the field and demonstrating the significance and value of care (Kim et al. 2016). Caring behaviours among nurses are crucial, as they directly influence the quality of patient care (Labrague, 2021). Moreover, caring and helping behaviours within the organization foster interdisciplinary collaboration and facilitate conflict resolution, convey positive energy, and promote personal growth and self-realization, which in turn enhances patient recovery and satisfaction (Kong, 2007; Jeong, 2023). These caring behaviours can contribute to improving the quality of nursing care by encouraging job satisfaction and the retention of experienced nurses who are capable of providing high-quality care (Boykin and Schoenhofer, 2013; Kim, 2006; Longo, 2009).
In a hospital setting, organizational health reflects effective functioning and adaptability (Lee and Jung, 2017). A healthy organization fosters emotional bonds among its members, facilitates adaptation to the environment, and encourages active engagement in tasks (Han and Jung, 2017). Managing organizational health is a powerful strategy for enhancing personnel management efficiency, particularly in healthcare organizations where it plays a vital role for nurses (Lee, 2015). Studies suggest that nurses who perceive their hospital as healthy are more engaged in their duties, which in turn improves patient safety and the quality of nursing care provided (Han and Jung, 2017). Positive interactions within the organization, such as a nursing organizational culture that promotes cooperation and satisfaction, along with caring and supportive behaviours, contribute to the improvement of organizational health (Lee, 2015). Thus, it follows that a supportive work environment is a critical factor influencing the provision of quality nursing care (Lake et al. 2016; Luxford et al. 2011).
Given the integral role of organizational health in enhancing nursing quality, it is anticipated to mediate the relationship between positive nursing organizational culture, caring behaviours, and nursing care quality. Through previous research, the quality of nursing care has been associated with various factors, such as nurses’ work engagement (Wei et al. 2023), nurse staffing, missed care and adverse events (Nantsupawat et al. 2022), workload and job satisfaction (Maghsoud et al. 2022; Yu et al. 2021; Khan and Muhammad, 2022), occupational fatigue and individualized nursing care (Cho et al. 2022), nurses’ turnover intentions and job satisfaction (Al Sabei et al. 2020; Yu et al. 2021), workplace incivility and patient safety outcomes (Cho et al. 2020), and nursing work environment as well as job burnout (Al Sabei et al. 2020; Khan and Muhammad, 2022). Despite the identified associations between various factors and nursing care quality, there has been limited exploration of the specific relationships between positive nursing organizational culture, caring behaviours, and nursing care quality. Additionally, studies on the mediating effects of hospital organizational health in these relationships are scarce.
Literature review for the framework development
Positive nursing organisational culture
A positive organizational culture, specifically within nursing organizations, is characterized by an environment that prioritizes employee recognition, fosters development, and empowers nurses to perform at their highest capabilities (Parent and Lovelace, 2015). This culture promotes learning, inclusion, and well-being among employees, aligning with the organization’s core values and goals. In nursing, a positive organizational culture is reflected in the behavioural patterns, norms, and expectations that positively influence nurses’ thinking and actions, creating a healthy work environment conducive to professional autonomy and collaborative relationships with other healthcare professionals (Mrayyan, 2019; Yom et al. 2014). Positive interactions within the organization, such as a nursing organizational culture that promotes cooperation and satisfaction, along with caring and supportive behaviours, contribute to improving organizational health (Lee, 2015). This positive culture is not just a supportive backdrop but is crucial for improving healthcare quality. Flexible organizational cultures that adapt to changing conditions and support nursing management practices have been shown to enhance the quality of nursing care (Bernardes et al. 2020). Studies have demonstrated a close relationship between positive nursing organizational culture and outcomes such as productivity, job satisfaction, and reduced turnover intentions among nurses (Aiken et al. 2002; Choi et al. 2014). Moreover, fostering a positive nursing organizational culture has been linked to maintaining high-quality nursing performance and sustainability in nursing tasks (Park et al. 2014). Therefore, positive nursing organizational culture is closely related to hospital organizational health and caring behaviour among colleagues, ultimately enabling the provision of high-quality nursing care.
Caring behaviour
Caring behaviour in nursing is the technical act of assisting individuals through protective actions that demonstrate concern for their needs, well-being, and survival (Leininger, 1985). This behaviour is vital in nursing as it forms the basis of the nurse-patient relationship and contributes to the overall quality of care provided. Caring behaviour extends beyond interactions with patients; it includes relationships with other nurses, nursing managers, and colleagues (Kong and Kim, 2017). Acts of caring within a nursing team can enhance patient care competencies, reduce stress, and alleviate conflicts among nurses (Longo, 2011). Therefore, caring behaviour is expected to play a role in creating a healthy organization.
Caring behaviour also plays a significant role in determining the quality of nursing care, which is a standard measure of the value and effectiveness of nursing practice (Kim and Park, 2014). Research indicates that caring behaviours, particularly from first-line nurse managers, promote professional growth and job satisfaction among nurses, ultimately leading to improved patient care (Peng et al. 2015; Putra et al. 2021). Peer support and caring behaviours among nursing staff have been shown to reduce job stress and increase job commitment, thereby mitigating the negative impacts of high turnover rates on organizational efficiency and nursing care quality (AbuAlRub, 2004; Longo, 2009; Kong and Kim, 2017). Thus, strategies that promote caring behaviour are essential for maintaining a high quality of nursing care.
Hospital organisational health
Hospital organizational health refers to the overall well-being and functionality of a hospital as perceived by its members, particularly nurses. This concept is similar to the health of an individual, encompassing both physical and mental aspects (Quick et al. 2007). A healthy organization is characterized by high productivity, performance, and the ability to maintain competitiveness (Keller and Price, 2011). In a hospital setting, organizational health involves creating a conducive environment that supports adaptation to work and fosters positive, collaborative relationships among staff (Kim and Yu, 2011). Therefore, it can be understood that hospital organizational health is closely related to a positive nursing organizational culture and caring behaviours among colleagues.
The health of a hospital organization is crucial for achieving its goals, particularly in providing high-quality nursing care. Healthy hospital organizations are more likely to engage in open cultural changes that enhance patient safety, reduce nursing errors, and improve overall healthcare quality (Brittain and Carrington, 2021). Moreover, hospital organizational health is significantly influenced by the quality of relationships within the organization. Strong teamwork and supportive relationships between managers and colleagues are essential for maintaining organizational health, particularly in rapidly changing hospital environments (Hadian et al. 2023; Hussein, 2014). These supportive relationships contribute to better organizational performance, patient safety, and nursing quality.
Relationships between the three concepts
The literature indicates that there are interrelated and potentially overlapping relationships between positive nursing organizational culture, caring behaviour, and hospital organizational health. A positive nursing organizational culture sets the foundation for caring behaviours by creating an environment that supports and values these behaviours. In turn, these caring behaviours contribute to the overall health of the hospital organization by promoting job satisfaction, reducing stress, and enhancing the quality of care provided. The health of the hospital organization, as perceived by its members, acts as a mediating factor that can amplify or diminish the effects of the nursing culture and caring behaviours on the quality of nursing care. Understanding the overlapping nature of these concepts is crucial for the development of a persuasive mediation model. The positive organizational culture and caring behaviours within nursing do not operate in isolation; they collectively contribute to the health of the hospital organization, which in turn influences the quality of nursing care. This integrative approach provides a more comprehensive understanding of how these factors interact to impact nursing outcomes.
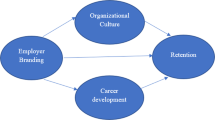
The objectives of the current study were to explore the relationship between positive nursing organizational culture, caring behaviour, and quality of nursing care, and to examine the mediating role of hospital organizational health between the positive nursing organizational culture, caring behaviour, and nursing care quality. Based on the proposed pathways, along with the results of previous studies, it was hypothesized that (Fig. 1):
-
1.
Positive nursing organisational culture and caring behaviour would be associated with hospital organisational health;
-
2.
Positive nursing organisational culture and caring behaviour, and hospital organisational health would be associated with quality of nursing care; and
-
3.
Hospital organisational health could serve as a mediating factor between a positive nursing organisational culture, caring behaviour, and the quality of nursing care.
Methods
Participants
Nurses who worked at a tertiary general hospital in City C, South Korea, were targeted. The sample size was determined via the software G-Power version 3.1.9.4 (Faul et al. 2009). A multiple regression analysis was employed with a medium effect size (f2) of 0.15 (Cho, 2022), significance level (α) of 0.05, and power (1-β) of 0.80. Based on 28 input explanatory variables (general characteristics including dummy variables, positive nursing organisational culture, caring behaviours, and hospital organisational health), the minimum sample size was 181. We considered a potential dropout rate of approximately 5–10% during data collection. Hence, 200 participants were randomly selected and surveyed via questionnaires. Collected data comprised 196 responses (recovery rate: 98%). After six unreliable responses were excluded, 190 responses were analysed. Data were collected via self-administered questionnaires between 2022 and 2023. The researcher distributed the questionnaires directly and explained the study’s purpose, data collection procedures, participants’ anonymity and confidentiality, voluntary nature of participation, and right to withdraw consent. Completed questionnaires were sealed in individual envelopes to maintain anonymity and collected directly by the researcher.
Measurements
General characteristics
We obtained data on 15 variables that reflected nurses’ demographic and sociological characteristics, such as gender, age, educational level, and clinical career.
Positive nursing organisational culture
The Positive Nursing Organizational Culture (PNOC) scale, created by Kim and Kim (2021), included four factors and 26 items: pursuit of common values (seven items), formation of organisational relationships based on trust (eight items), a fair management system (four items), and positive leadership of the nursing unit manager (seven items). PNOC refers to the behaviours, norms, and expectations that positively influence the thoughts and actions of nursing organization members (Kim and Kim, 2021). Each item was rated on a 5-point Likert scale that ranged from ‘Strongly Agree (5)’, ‘Agree (4)’, ‘Neutral (3)’, ‘Disagree (2)’, to ‘Strongly Disagree (1 point)’. A higher score indicated a stronger positive perception of the nursing organisational culture. Cronbach’s alphas (reliability) were α = 0.95 in the original study describing the scale (Kim and Kim, 2021) and 0.97 in the current study.
Caring behaviour
The modified and validated Korean versions of the Organizational Climate of Caring Questionnaire (OCCQ) (Longo, 2009) and Peer Group Caring Interaction Scale (PGCIS) (Hughes, 1998) known as the Organizational Climate of Caring Scale (OCCS) and PGCIS-K (Peer Group Caring Interaction Scale-Korean), respectively, were used. These have been validated by Kong and Kim (2017).
The OCCS, a tool to measure nursing managers’ caring behaviours within a nursing unit organisation, was structured into four factors with 17 items: modelling (seven items), dialogue (three items), practice (four items), and confirmation (three items). Each item was rated on a 6-point Likert scale that ranged from ‘Always True (6)’, ‘Often True (5)’, ‘Usually True (4)’, ‘Sometimes True (3)’, ‘Rarely True (2)’, to ‘Never True (1 point)’. A higher score indicated a more positive perception by nurses of nursing managers’ caring behaviours. Cronbach’s alphas were 0.98 (Longo, 2009) and 0.98, (Kong and Kim, 2017) in previous studies, and 0.98 in the current study.
The PGCIS-K, a tool to measure caring behaviours among peer nurses within a nursing organisation unit, was structured into two factors with 16 items: modelling (nine items) and providing assistance (seven items). Each item was rated on a 6-point Likert scale that ranged from ‘Always True (6)’, ‘Often True (5)’, ‘Usually True (4)’, ‘Sometimes True (3)’, ‘Rarely True (2)’, to ‘Never True (1 point)’. Higher scores indicated a more positive perception of caring behaviours among peer nurses. Cronbach’s alphas were 0.94 at the time of development (Hughes, 1998), 0.95 in a more recent study (Kong and Kim, 2017), and 0.98 in the current study.
Hospital organisational health
We utilised the Hospital Organizational Health (HOH) measurement tool, developed by Kim and Yu (2014). It was modified and complemented by Lee and Jung (2017) for nursing organisations.
Hospital organizational health refers to the perceived suitability and well-being of the organization as experienced by clinical nurses within the hospital (Lee and Jung, 2017).
The tool comprised four factors with 31 items: environmental fit (eight items), workflow fit (nine items), vitality (eight items), and community orientation (six items). Each item was rated on a 5-point Likert scale that ranged from ‘Strongly Agree (5)’, ‘Agree (4)’, ‘Neutral (3)’, ‘Disagree (2)’, to ‘Strongly Disagree (1 point)’. A higher score indicated a higher perception of organisational health by the hospital. Cronbach’s alphas were 0.96 in the original study describing the tool (Kim and Yu, 2014), 0.94 for the modified version (Lee and Jung, 2017), and 0.97 in the current study.
Quality of nursing care
We utilised the nurse-reported Quality of Care (QNC) measurement tool developed by Havaei et al. (2019), which was translated into Korean by the researcher and a nursing professor. Following the translation, the items’ meaning and understanding were validated by three registered nurses with over 20 years of experience and master’s degrees or higher qualifications. The QNC refers to the extent to which nurses provide appropriate care that meets the patient’s needs, leading to the achievement of the patient’s health goals and excellence in the level of care provided. The tool comprised 4 items. Each item was rated on a 4-point Likert scale that ranged from ‘Very High Level (4)’, ‘High Level (3)’, ‘Low Level (2)’, to ‘Very Low Level (1 point)’. Higher scores indicated a higher perception of nursing quality. Cronbach’s alphas were 0.80 in the original study describing the tool (Havaei et al. 2019) and 0.87 in the current study.
Data analysis
Data were analysed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY, USA). Descriptive analyses, which included frequency, percentage, mean, and standard deviation, were performed for the participants’ general characteristics, PNOC, CB, HOH, and QNC results. Differences were analysed via independent samples t-tests and one-way analysis of variance (ANOVA), with Scheffé’s post-hoc tests conducted where applicable. Pearson’s correlation coefficients were calculated to examine the correlations among variables. A hierarchical linear regression was used to analyse the factors that influenced the quality of nursing care. Multiple regression analysis, based on Baron and Kenney’s (1986) three-step technique, was conducted to examine the mediating effect of hospital organisational health on the relationship between positive nursing organisational culture, caring behaviour, and nursing quality. The significance of the mediation effect was assessed using a 95% bootstrapped confidence interval (CI) with 5000 bootstrap replications. The indirect effect is considered as significant if the zero is not included in the 95%CI.
Results
Nurses’ general characteristics and differences in quality of nursing care according to participants’ characteristics
Table 1 presents the nurses’ general characteristics and differences in quality of nursing care according to the participants’ general characteristics. Before differences in quality of nursing care according to the participants’ characteristics were analysed, a normality check confirmed that data were normally distributed. Characteristics that showed differences in the QNC scores were age (F = 3.71, p = 0.013), department of work (F = 6.07, p < 0.001), current hospital work experience (F = 3.50, p = 0.017), total clinical experience (F = 4.83, p = 0.003), nursing job satisfaction (F = 11.19, p < 0.001), department satisfaction (F = 33.07, p < 0.001), intention to leave (t = −2.53, p = 0.012), and the level of job stress (F = 8.35, p < 0.001). Regarding age, those under 25 years showed higher nursing quality than those aged 25–29 and 30–34 years. Regarding the department of work, nursing quality was higher in the neonatal intensive care unit (NICU) and nursery compared to the intensive care unit (ICU) and emergency room. Current hospital work experience revealed that those with less than two years of experience had higher nursing quality than those with 5–10 years. Total clinical experience indicated higher nursing quality for those with less than two years of experience than those with 2–5 years, 5–10 years, or over 10 years of experience. Nursing job and department satisfaction showed higher nursing quality as ‘satisfied’, neutral’, and ‘dissatisfied’ sequentially. No intention of leaving resulted in higher nursing quality than intention to leave. Level of job stress indicated a higher nursing quality for those who reported ‘low’ stress than those who reported ‘high’ stress (Table 1).
Scores of variables and correlations among the variables
The scores for the QNC, positive nursing organisational culture, caring behaviours, and hospital organisational health were 2.92 ± 0.45 (out of 4 points), 3.60 ± 0.59 (out of 5 points), 4.23 ± 0.73 (out of 6 points), and 3.40 ± 0.57 (out of 5 points), respectively. The QNC was significantly correlated with the PNOC (r = 0.61, p < 0.001), caring behaviour (CB) (r = 0.59, p < 0.001), and HOH (r = 0.67, p < 0.001; Table 2).
Influence of participants’ characteristics, positive nursing organisational culture, caring behaviour, and hospital organisational health on quality of nursing care
To investigate the impact of participants’ general characteristics, PNOC, CB, and HOH scores on QNC scores, a hierarchical linear regression analysis was calculated. Model 1 included the general characteristic variables identified as affecting QNC scores. Model 2 added PNOC and CB scores to Model 1, whereas Model 3 added the HOH scores to Model 2.
Before analysis, we checked for autocorrelation among the error terms via the Durbin-Watson statistic, which resulted in a value close to 2 (1.849). This indicated that there was no autocorrelation. Furthermore, we examined the distribution of the residuals through standardised residuals to assess the assumption of normal distribution. All values, except for one case, fell within ±3 standard deviations of the mean. Even the one exception was close to this threshold, with a value of −3.177, suggesting that the assumption of a normal distribution for the error terms was valid.
We examined the presence of multicollinearity among the input-independent variables via tolerance and variance inflation factors (VIF). Tolerance ranged from 0.176–0.732, which exceeded 0.10, and VIF ranged from 1.366 to 5.671, all below 10 (Kutner et al. 2004). These results indicated the absence of multicollinearity.
In Model 1, the variables that significantly influenced the quality of nursing care were the surgical ward (β = 0.21, p = 0.004) and other (outpatient) departments (β = 0.16, p = 0.027) for work, satisfaction (β = 0.57, p < 0.001) and average satisfaction (β = 0.32, p = 0.006) for department satisfaction, and average stress level (β = 0.15, p = 0.026) for job stress. Therefore, nursing care quality tended to be higher in the surgical and other (outpatient) departments compared to intensive care units and emergency rooms regarding work department. Regarding department satisfaction, nursing care quality was higher in satisfied and moderately satisfied conditions compared to dissatisfied conditions. Additionally, nursing care quality was higher when the level of job stress was average compared to high stress. The explanatory power of Model 1 was 38.0% (F = 5.83, p < 0.001, R2 = 0.380, Adj R2 = 0.315).
In Model 2, among the additional variables, a positive nursing organisational culture had a significant impact on quality of nursing care (β = 0.33, p = 0.001). Meanwhile, caring behaviour (β = 0.15, p = 0.140) did not show a significant influence. Hence, higher levels of positive nursing organisational culture were associated with higher quality of nursing care. The proportion of additional explanatory power in Model 2 was 10.4%, and the total explanatory power was 48.4% (F = 7.92, p < 0.001, R2 = 0.484, Adj R2 = 0.423).
In Model 3, the added variable, hospital organisational health, showed a significant impact on quality of nursing care (β = 0.47, p < 0.001). Thus, higher levels of hospital organisational health were associated with higher quality of nursing care. The proportion of additional explanatory power in Model 3 was 8.8%, and the total explanatory power was 57.2% (F = 10.70, p < 0.001, R2 = 0.572, Adj R2 = 0.519; see Table 3).
Mediating effect of hospital organisational health
To examine the mediating effect of hospital organisational health on the relationship between positive nursing organisational culture, caring behaviours, and quality of nursing care, a regression analysis was conducted using Baron and Kenny’s three-step procedure (Baron and Kenny, 1986) after controlling for general characteristic variables that showed significant differences in association with the quality of nursing care. Additionally, significance of the indirect effects of the mediating variable was assessed via bootstrapping. Before the analysis, the absence of autocorrelation among the error terms was confirmed via the Durbin-Watson statistic, which ranged from 1.885–1.944 and indicated no autocorrelation. Examination of the standardised residuals suggested normal distribution assumptions, and all cases fell within ± 3 standard deviations of the mean, except for one, which implied that the assumption of normal distribution for the error terms was reasonable. We assessed multicollinearity among the independent input variables, performed via tolerance and VIF, and revealed tolerance and VIF values between 0.181–0.821 (above 0.10) and 1.218–5.538 (below 10), respectively, which indicated the absence of multicollinearity.
Mediating effect of hospital organisational health on the relationship between positive nursing organisational culture and quality of nursing care
In the first step, the PNOC scores had significant direct effect on HOH scores (β = 0.73, p < 0.001). In the second step, PNOC scores had a significant impact on QNC scores (β = 0.45, p < 0.001). In the final third step, HOH scores significantly influenced QNC scores (β = 0.48, p < 0.001), while the PNOC scores demonstrated no significant effect on QNC scores (β = 0.08, p = 0.380). Therefore, HOH scores fully mediated the relationship between PNOC and QNC scores. The test for the significance of the indirect effect of HOH scores on the relationship between PNOC and QNC scores showed that the mediating effect was significant, as the 95% confidence interval did not include zero (B = 0.27, 95% CI = 0.18–0.37; Table 4, Fig. 2).
Mediating effect of hospital organisational health on the relationship between caring behaviour and quality of nursing care
In the first step, CB had a significant direct effect on HOH scores (β = 0.66, p < 0.001). In the second step, CB scores had a significant impact on QNC scores (β = 0.38, p < 0.001). In the final third step, HOH scores significantly influenced QNC scores (β = 0.50, p < 0.001), while CB scores had no significant effect on QNC scores (β = 0.04, p = 0.649). Therefore, HOH scores fully mediated the relationship between CB and QNC scores. The result for the indirect effect of HOH scores on the relationship between CB and QNC scores was significant (B = 0.21, 95% CI = 0.14–0.28; Table 5, Fig. 2).
Discussion
This study aimed to examine the relationships among positive nursing organisational culture, caring behaviour, and quality of nursing care among clinical nurses. Additionally, this study also investigated the mediating effect of hospital organisational health on the relationship between positive nursing organisational culture, caring behaviour, and the quality of nursing care. We aimed to provide foundational data for exploring strategies for establishing an appropriate nursing culture that could enhance the quality of nursing care.
Our results indicated that the QNC scores for the study participants averaged 11.67 points out of 16 (mean rating of 2.92 out of 4). In Havaei et al.’s (2019) study, which used the same instrument and focused on surgical ward nurses, the average score was 10.7. Additionally, in Ji’s (2017) study, which targeted ICU nurses albeit with a different instrument to assessed nursing quality, the mean rating was 2.47 out of 4. Thus, compared to previous studies, our results indicated higher quality of nursing care.
Ji’s (2017) study found that as nurses’ competence increased or their working environment improved, the quality of nursing care also increased. Furthermore, Yu et al.’s (2021) study targeted neonatal ICU nurses in three tertiary general hospitals and reported that 47.5% responded that the quality of nursing care was either average or low. They emphasised the need for appropriate staffing, improved nursing work environment, and establishment of measures to enhance job satisfaction to improve nursing care quality. Aiken et al.‘s (2011) research focused on Asian countries and revealed that 68%, 60%, and 30% of nurses in Korea, China, and Japan, respectively, responded that the quality of nursing care was deteriorating. Among Asian countries, Korea was reported as having a particularly low quality of nursing care compared with other nations. Labrague’s (2021) study on Filipino nurses revealed that nursing managers’ toxic leadership behaviours influenced deteriorations in nursing care quality. Additionally, Van Bogaert et al.’s (2017) study on Belgian nurses indicated differences in patient conditions and quality of nursing care based on high job demands. Hence, the quality of nursing care was influenced by both nurses’ individual competence and various other factors, such as nursing staff, work environment, job demands, nursing organisational culture, and hospital organisational policies. Our results focused on the general characteristics and organisational factors that influenced the quality of nursing.
In this study, the most significant factor that influenced the quality of nursing care was hospital organisational health. If the hospital organisation was perceived to be healthy, the quality of nursing care tended to be higher. A healthy hospital organisation was associated with increased autonomy among members, enhanced morale, and maximized effectiveness, which contributed to goal achievement (Ha, 2013). Direct comparisons were limited due to a scarcity of studies on the relationship between hospital organisational health and the quality of nursing care. However, Han and Jung (2017) examined the relationship between hospital organisational health and patient safety nursing activities, suggesting that a higher level of organisational health could enhance patient safety nursing activities.
Patient safety nursing activities encompass the overall realm of nursing activities, including patient safety and nursing-specific tasks, and can be considered a driving force for improving the quality of healthcare services (Han and Jung, 2017). This study identified enhancement of hospital organisational health as a means of improving the quality of nursing care. However, lack of direct research on the relationship between hospital organisational health and the quality of nursing care made it challenging to create a clear comparison. To this end, further studies are required.
Second, among participants’ characteristics, department satisfaction was identified as a factor that influenced the quality of nursing care. The higher the satisfaction with the current department, the higher the quality of nursing care. Kim (2021) focused on novice nurses and revealed that those placed in their preferred department had higher job satisfaction compared to those who were not placed in their preferred department. Additionally, Bang and Kim (2014) examined the relationship between job stress and job performance among novice nurses and found that nurses placed in their preferred department exhibited better job performance than those in other departments. Hence, satisfaction with the current department could be associated with increased job satisfaction and job performance. Furthermore, department satisfaction could positively influence improvement in nursing care quality. Therefore, in hospital organisations, efforts should be made to consider nurses’ individual preferences, such as deploying personnel to their desired departments whenever possible. This efficient workforce management approach could assist nurses in adapting to their roles and contribute to enhancing the quality of patient care. The working department was also a factor that influenced nursing care quality. Participants perceived that nursing care quality was higher when they worked in surgical wards, operating rooms/delivery rooms, neonatal ICUs, and outpatient departments compared to in critical care/emergency rooms. Previous studies indicated that nurses who worked in urgent care settings, such as emergency rooms, experienced higher levels of stress due to the need for constant alertness (Oh et al. 2011; Lee and Ahn, 2015). Nurses in intensive care units, who require advanced skills and deal with critically unwell patients, experience higher job stress (Sung, 2006; Oh et al. 2016; Ha et al. 2016). Nurses in outpatient departments with irregular shift schedules have been shown to experience higher job stress than those in departments with regular shifts (Sung et al. 2007). We observed that the quality of nursing care was lower in association with high job stress. Elevated job stress has been associated with decreased job satisfaction and increased burnout (Kwon et al. 2021), which makes effective and efficient task performance challenging and ultimately leads to a decline in the quality of patient care (Kim and Yu, 2014; Kim and Lee, 2006). Therefore, development of a differentiated compensation system based on departments or work types and exploration of various programs to manage nurses’ job stress and enhance the quality of nursing care are essential. Furthermore, since this study was conducted in a tertiary hospital, the observed results may be attributed to the higher acuity and complexity of tasks compared with smaller hospitals or medical centres. Therefore, additional research in hospitals of different sizes is necessary to validate and extend our findings.
In this study, positive nursing organizational culture and caregiving behaviour did not directly impact the quality of nursing care. However, our analysis revealed that HOH scores completely mediated the relationship between positive nursing organizational culture and nursing care quality. This indicates that while a positive nursing organizational culture may not have a direct effect on nursing care quality, it exerts its influence through the mediation of hospital organizational health. The quality of nursing care is a multifaceted outcome influenced by various factors. The direct impact of positive nursing organizational culture and caring behaviours may be overshadowed when more immediate or stronger factors are present. Instead, these influences on nursing care quality primarily occur through intermediary processes, such as improving job satisfaction, reducing stress, or enhancing teamwork. These indirect pathways, as highlighted by the mediating role of hospital organizational health, suggest that while the direct effects may be less visible, they remain crucial to the overall quality of care. Lee (2015) examined organizational culture and health among nurses in university hospitals and found that a human-centred organizational culture based on mutual trust established healthy relationships and made the organization healthier. This, in turn, enhanced job performance and satisfaction. Similarly, improved hospital organizational health can enhance nurses’ job satisfaction and organizational commitment (Lee and Jung, 2017). These factors—job satisfaction and organizational commitment—are critical to providing high-quality nursing care (Lake et al. 2016). Therefore, improving hospital organizational health through positive enhancements in nursing culture could lead to better nursing care quality. Consequently, cultivating a positive organizational culture, such as fostering a sense of community among members and creating a culture of mutual support, should be prioritized to promote hospital organizational health.
Furthermore, when analysing the mediating effect of hospital organisational health in the relationship between caring behaviour and nursing quality, hospital organisational health completely mediated the relationship between caring behaviour and nursing quality. Mutual care and respect exhibited among organisational members positively impact patient safety and enhance healthcare quality (Kim, 2012). Through caring and considerate behaviours, nurses’ nursing performance and caregiving capabilities can be increased (Shin et al. 2020), which facilitates the growth of nurses’ caregiving skills resulting in improved proficiency in patient caregiving practices (Longo, 2011). Ultimately, highly skilled nurses contribute to hospital organisational health, enable effective task performance, and enhance the quality of nursing (Lee and Jung, 2017). Therefore, the promotion of caregiving and considerate behaviour among nurses should raise awareness of hospital organisational health and positively influence the quality of nursing care. However, it was challenging to directly compare the relationship between caring behaviour, hospital organisational health, and nursing quality in the current study, as prior research on these associations was scarce. Thus, further studies are warranted. Although this study found that caring behaviour did not directly impact nursing quality, it did influence nursing quality indirectly through the mediating variable of hospital organisational health. Therefore, efforts promoting caring behaviours at the nursing organisational level, encouraging nurse participation, and fostering a culture that normalises caring behaviour among members are essential for enhancing the awareness of hospital organisational health.
This study’s scope was limited to tertiary hospitals, which may restrict the generalisability of the results. Additionally, the data collection relied on self-reported surveys, which included the assessment of nursing quality, which could pose limitations regarding objectivity. Caution is advised when interpreting the results. In addition, data collected during a specific timeframe may not capture long-term changes or trends. However, our results indicated that hospital organisational health was a crucial direct factor that influenced nursing quality and a significant mediating factor between positive nursing organisational culture, caring behaviour, and nursing care quality. Additionally, hospital organisational health was influenced by a positive nursing organisational culture and caring behaviour. By providing insights into the significant predictors of QNC, these findings can contribute to improving the quality of care in Korean hospitals.
Conclusion
The following practical suggestions are provided based on the findings of the current study: 1) There should be a focus on improving hospital organizational health, which significantly influences nursing care quality. This can be achieved by promoting teamwork, fostering supportive relationships among staff, and creating a positive work environment. Regular assessments and targeted interventions to address weaknesses could be beneficial. 2) Hospitals should emphasize mutual trust, collaboration, and shared values. Leadership training for nurse managers can promote positive cultural practices, thereby enhancing overall organizational health. 3) Programs that encourage caring behaviours, such as peer support systems and regular team-building activities, should be implemented to help maintain a healthy work environment. Recognizing and rewarding caring behaviours among staff can reinforce these practices. 4) Work and environmental conditions should be improved at the organizational level to further support nursing quality. This includes fostering a positive nursing organizational culture and managing stress effectively.
Going forward, the scope of the current study should be broadened to include a wider range of healthcare institutions and regions. Future studies should also confirm the relationship between hospital organizational health and nursing quality, and investigate whether raising awareness of organizational health through interventions based on caring behaviour leads to improvements in nursing quality.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to containing personal information such as the participant’s work place but are available from the first author on reasonable request.
References
AbuAlRub RF (2004) Job stress, job performance, and social support among hospital nurses. J Nurs Scholarsh 36(1):73–78. https://doi.org/10.1111/j.1547-5069.2004.04016.x
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH (2002) Hospital staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 288(16):1987–1993. https://doi.org/10.1001/jama.288.16.1987
Aiken LH, Sloane DM, Clarke S et al. (2011) Importance of work environments on hospital outcomes in nine countries. Int J Qual Health Care 23(4):357–364. https://doi.org/10.1093/intqhc/mzr022
Al Sabei SD, Labrague LJ, Miner Ross A et al. (2020) Nursing work environment, turnover intention, job burnout, and quality of care: the moderating role of job satisfaction. J Nurs Scholarsh 52(1):95–104. https://doi.org/10.1111/jnu.12528
Bang SS, Kim IO (2014) Relationship among essentials of fundamental nursing skills performance, stress from work and work capability of new clinical nurses. J Korean Acad Soc Nurs Educ 20(4):628–638. https://doi.org/10.5977/jkasne.2014.20.4.628
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J Pers Soc Psychol 51:1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173
Bernardes A, Gabriel CS, Cummings GG et al. (2020) Organizational culture, authentic leadership and quality improvement in Canadian healthcare facilities. Rev Bras Enferm 73(5):e20190732. https://doi.org/10.1590/0034-7167-2019-0732
Boykin A, Schoenhofer SO (2013) Nursing as caring: a model for transforming practice. NLN Press
Brittain AC, Carrington JM (2021) Organizational health and patient safety: a systematic review. J Hosp Manag Health Policy 5:2. https://doi.org/10.21037/jhmhp-20-57
Cho H, Pavek K, Steege L (2020) Workplace verbal abuse, nurse-reported quality of care and patient safety outcomes among early-career hospital nurses. J Nurs Manag 28(6):1250–1258. https://doi.org/10.1111/jonm.13071
Cho H, Sagherian K, Scott LD, Steege LM (2022) Occupational fatigue, individualized nursing care, and quality of nursing care among hospital nurses. J Nurs Scholarsh 54(5):648–657. https://doi.org/10.1111/jnu.12768
Choi SH, Jang IS, Park SM, Lee HY (2014) Effects of organizational culture, self-leadership and empowerment on job satisfaction and turnover intention in general hospital nurses. J Korean Acad Nurs Adm 20(2):206–214. https://doi.org/10.11111/jkana.2014.20.2.206
Coates C (2002) The evolution of measuring caring: moving toward construct validity. In: Sitzman KL, Watson J (eds) Assessing and Measuring Caring in Nursing and Health Science, 3rd edn. Springer Publishing: New York, p 297–302. https://doi.org/10.1891/9780826195425.0026
Duffy JR, Hoskins LM (2003) The quality-caring model: blending dual paradigms. Adv Nurs Sci 26(1):77–88
Edmundson E (2012) The quality caring nursing model: a journey to selection and implementation. J Pediatr Nurs 27(4):411–415. https://doi.org/10.1016/j.pedn.2011.09.007
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(40):1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Hadian SA, Yarmohammadian MH, Shaarbafchizadeh N (2023) The organizational health components for small-sized health-care organizations: a systematic review. J Edu Health Promot 12(1):37. https://doi.org/10.4103/jehp.jehp_1307_21
Ha HJ, Choe JS, Oh MS et al. (2016) Hospital nurses’ job stress, sleep disturbance, and fatigue. J Korea Soc Med Inform 22(1):13–25
Ha NS (2013) The relationship between the head nurse’s decision-making style perceived by nurses and job satisfaction, role conflict and the organizational health in nurses. Stress Korean J Stress Res 21(1):61–71
Han MY, Jung MS (2017) Effect of hospital nurses’ perceptions of organizational health and patient safety culture on patient safety nursing activities. J Korean Acad Nurs Adm 23(2):127–138. https://doi.org/10.11111/jkana.2017.23.2.127
Havaei F, MacPhee M, Dahinten VS (2019) The effect of nursing care delivery models on quality and safety outcomes of care: a cross‐sectional survey study of medical‐surgical nurses. J Adv Nurs 75(10):2144–2155. https://doi.org/10.1111/jan.13997
Hughes LC (1998) Development of an instrument to measure caring peer group interactions. J Nurs Educ 37(5):202–207. https://doi.org/10.3928/0148-4834-19980501-05
Hussein AHM (2014) Relationship between nurses’ and physicians’ perceptions of organizational health and quality of patient care. East Mediterr Health J 20(10):634–642
Jeong BH (2023) The influence of compassion competence, communication skills and peer group caring behaviors of general hospital nurses on patient-centered nursing. Dissertation, Chungnam National University
Ji HR (2017) Effect of ICU nurses’ competence and work environment on the quality of nursing care. Dissertation, ChungAng National University
Khan A, Muhammad D (2022) Perspective of nurses regarding factors affecting quality of nursing care in intensive care units: a qualitative study. Rehman J Health Sci 4(2):121–130. https://doi.org/10.52442/rjhs.v4i2.289
Keller S, Price C (2011) Organizational health: the ultimate competitive advantage. McKinsey Quarterly. https://www.operatingpartners.com/wp-content/uploads/2020/08/OMS-1a-People-Organization.pdf Accessed 12 December 2023
Kim CW, Park YJ (2014) An exploratory study of the discourse on the desirable elderly caring culture. J Crit Soc Welf 44:82–115
Kim HR (2012) Impact of healthcare accreditation on patient safety and improvement of healthcare quality, organizational culture, hospital administrative activities. Dissertation, Yonsei University
Kim JE, Yu GC (2014) A study on conceptual model of organizational health and development of its measurement (OHQ) and construct validation. J Bus Adm 43(6):1875–1904
Kim JE, Yu GC (2011) The meaning of healthy organization and an integrated model of organizational health. Korean J Bus Adm 24(5):2641–2673
Kim JH, Kong MY, Oh YH (2016) Validity and reliability of the peer group caring interaction scale-korean version. J Korean Acad Nurs 46(3):431–442. https://doi.org/10.4040/jkan.2016.46.3.431
Kim MJ (2006) The effect of nursing organizational culture on nurses’ intention of retention. Dissertation, Hanyang University
Kim MJ, Kim JK (2021) Development of a positive nursing organizational culture measurement tool. J Korean Acad Nurs 51(3):305–319. https://doi.org/10.4040/jkan.21014
Kim NY, Jang KS, Ryu SA, Kim YM (2003) The analysis of nursing research in Korea in relation to the evaluation of quality of nursing. J Korean Acad Nurs Adm 3(2):337–352
Kim SH, Lee MA (2006) A study of the reward and the job satisfaction perceived by nurses. J Korean Acad Nurs Adm 12(1):122–130
Kim YW (2021) Differences in job satisfaction, job stress and turnover intention according to the placement of new nurses desired department. Dissertation, Hanyang University
Klopper HC, Coetzee SK, Pretorius R, Bester P (2012) Practice environment, job satisfaction and burnout of critical care nurses in South Africa. J Nurs Manag 20(5):685–695. https://doi.org/10.1111/j.1365-2834.2011.01350.x
Kong BH (2007) Art of caring in nursing. Philos Med 3:97–116
Kong MY, Kim JH (2017) Influence of nurse manager and peer group caring behaviors as perceived by nurses on intention to retention. J Korean Acad Nurs Adm 23(2):191–200. https://doi.org/10.11111/jkana.2017.23.2.191
Kwon SY, Son MS, Kang IS (2021) Effect of interpersonal stress of emergency room nurses on burnout and job satisfaction: mediating effect of resilience. Glob Health Nurs 11(1):21–31. https://doi.org/10.35144/ghn.2021.11.1.21
Kutner MH, Nachtsheim CJ, Neter J (2004) Applied linear regression models, 4th ed. McGraw-Hill/Irwin, New York
Labrague LJ (2021) Influence of nurse managers’ toxic leadership behaviours on nurse-reported adverse events and quality of care. J Nurs Manag 29(4):855–863. https://doi.org/10.1111/jonm.13228
Lake ET, Hallowell SG, Kutney-Lee A et al. (2016) Higher quality of care and patient safety associated with better NICU work environments. J Nurs Care Qual 31(1):24–32. https://doi.org/10.1097/NCQ.0000000000000146
Lee GH (2015) The effects of organizational culture and middle manager leadership on organizational health and the mediating effects of self-efficacy. Dissertation, Kosin University
Lee JH, Jung MS (2017) Effects of organizational health on job satisfaction and organizational commitment in hospital nurses. J Humanit Soc Sci 8(2):499–516. https://doi.org/10.22143/HSS21.8.2.27
Lee YL, Ahn SH (2015) Impact of job stress on turnover intention among emergency room nurses. J Muscle Jt Health 22(1):30–39. https://doi.org/10.5953/JMJH.2015.22.1.30
Leininger MM (1985) Transcultural care diversity and universality: a theory of nursing. Nurs Health Care 6(4):208–212
Liu Y (2014) Factors influencing nurse-assessed quality of nursing care in Chinese hospitals. Dissertation, Chulalongkorn University, Thailand. p 8
Longo J (2009) The relationships between manager and peer caring to registered nurses’ job satisfaction and intent to stay. Int J Hum Caring 13(2):27–34. https://doi.org/10.20467/1091-5710.13.2.26
Longo J (2011) Acts of caring: nurses caring for nurses. Holist Nurs Pr 25(1):8–16. https://doi.org/10.1097/HNP.0b013e3181fe2627
Luxford K, Safran DG, Delbanco T (2011) Promoting patient-centered care: a qualitative study of facilitators and barriers in healthcare organizations with a reputation for improving the patient experience. Int J Qual Health Care 23(5):510–515. https://doi.org/10.1093/intqhc/mzr024
Maghsoud F, Rezaei M, Asgarian FS, Rassouli M (2022) Workload and quality of nursing care: the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion by using structural equations modeling approach. BMC Nurs 21(1):273. https://doi.org/10.1186/s12912-022-01055-1
McHugh MD, Stimpfel AW (2012) Nurse reported quality of care: a measure of hospital quality. Res Nurs Health 35(6):566–575. https://doi.org/10.1002/nur.21503
Mrayyan MT (2019) Nurses’ views on hospital organizational characteristics. Nurs Forum 54:650–660. https://doi.org/10.1111/nuf.12390
Nantsupawat A, Poghosyan L, Wichaikhum OA et al. (2022) Nurse staffing, missed care, quality of care and adverse events: A cross‐sectional study. J Nurs Manag 30(2):447–454. https://doi.org/10.1111/jonm.13501
Oh EW, Yang SM, Kim SH et al. (2016) Compare the level of job stress, burn-out and job satisfaction between intensive care unit nurses and general unit nurses. J Korea Inst Med Inform 22(1):27–36
Oh MO, Sung MH, Kim YW (2011) Job stress, fatigue, job satisfaction and commitment to organization in emergency department nurses. J Korean Clin Nurs Res 17(2):215–227
Parent JD, Lovelace KJ (2015) The impact of employee engagement and a positive organisational culture on an individual’s ability to adapt to organization change. 2015 Eastern academy of management proceedings: organization behavior and theory track 1-20. Available via https://scholarworks.merrimack.edu/mgt_facpub/10/. Accessed 10 Jan 2024
Park KO, Park SH, Yu M (2014) Review of research on nursing organizational culture in Korea. J Korea Contents Assoc 14(2):387–395. https://doi.org/10.5392/JKCA.2014.14.02.387
Peng X, Liu Y, Zeng Q (2015) Caring behavior perceptions from nurses of their first-line nurse managers. Scand J Caring Sci 29(4):708–715. https://doi.org/10.1111/scs.12201
Putra KR, Andayani T, Ningrum EH (2021) Job satisfaction and caring behavior among nurses in a military hospital: a cross-sectional study. J Public Health Res 10(2):2212. https://doi.org/10.4081/jphr.2021.2212
Quick JC, Macik-Frey M, Cooper CL (2007) Managerial dimensions of organizational health: the healthy leader at work. J Manag Stud 44(2):189–205. https://doi.org/10.1111/j.1467-6486.2007.00684.x
Shin ES, An MJ, Choi ML et al. (2017) Factors influencing quality of nursing service among clinical nurses: focused on resilience and nursing organizational culture. J Korean Clin Nurs Res 23(3):302–311
Shin NY, Yu SY, Kang SS et al. (2020) Influence of nurse manager and peer group caring behaviors as perceived by nurses on organizational socialization and nursing performance. J Korean Acad Nurs Adm 26(2):110–119. https://doi.org/10.11111/jkana.2020.26.2.110
Srimulyani VA, Hermanto YB (2022) Organizational culture as a mediator of credible leadership influence on work engagement: empirical studies in private hospitals in East Java, Indonesia. Humanit Soc Sci Commun 9(1):274. https://doi.org/10.1057/s41599-022-01289-z
Sung MH (2006) A comparative study on role conflict and job satisfaction between nurses in ICU and nurses in general ward. J Korean Acad Nurs Adm 12(1):104–112
Sung MH, Kim HJ, Han YM (2007) A study of health status and job satisfaction of nurses on day shift and nurses on night shift. J Korean Acad Nurs Adm 13(1):32–39
Tvedt C, Sjetne IS, Helgeland J, Bukholm G (2014) An observational study: Associations between nurse-reported hospital characteristics and estimated 30-day survival probabilities. BMJ Qual Saf 23(9):757–764. 10/1136/bmjqs-2013-002781
Van Bogaert P, Peremans L, Van Heusden D et al. (2017) Predictors of burnout, work engagement and nurse reported job outcomes and quality of care: a mixed method study. BMC Nurs 16:5. https://doi.org/10.1186/s12912-016-0200-4
Wei H, Horsley L, Cao Y et al. (2023) The associations among nurse work engagement, job satisfaction, quality of care, and intent to leave: a national survey in the United States. Int J Nurs Sci 10(4):476–484. https://doi.org/10.1016/j.ijnss.2023.09.010
Yom YH, Noh SM, Kim KH (2014) Clinical nurses’ experience of positive organizational culture. J Korean Acad Nurs Adm 20(5):469–480. https://doi.org/10.11111/jkana.2014.20.5.469
Yu M, Park C, Lee S (2021) Predictors of nurse-reported quality of care in neonatal intensive care units in Korea. J Pediatr Nurs 60:e24–e30. https://doi.org/10.1016/j.pedn.2021.02.015
Author information
Authors and Affiliations
Contributions
These authors contributed equally to this work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Approval was obtained from the ethics committee of Samsung Changwon Medical Center (no. SCMC 2022-07-015, SCMC 2022-07-015-001, SCMC 2022-07-015-003). Our procedures adhere to the principles of the Declaration of Helsinki and its future amendments.
Informed consent
Informed consent was obtained from all the participants before data collection.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ku, B.R., Yu, M. Hospital organisational health as a mediator between positive nursing organisational culture, caring behaviour, and quality of nursing care. Humanit Soc Sci Commun 11, 1203 (2024). https://doi.org/10.1057/s41599-024-03731-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1057/s41599-024-03731-w