Abstract
Access to trustworthy artificial intelligence (AI) for clinical applications is uneven, especially in low-resource settings with limited and inconsistent data. Models from high-resource settings often fail to generalize. Transfer learning (TL) can adapt established models to new settings. Using neurological outcome prediction for out-of-hospital cardiac arrest (OHCA) as a proof of concept, we adapted a model trained on a large cohort to Vietnam (243 patients) and Singapore (15,916 patients) using the Pan-Asian Resuscitation Outcomes Study registry. The external model performed poorly on the Vietnam cohort, with an area under the receiver operating characteristic curve (AUROC) of 0.467 (95% CI: 0.141–0.785), but TL markedly improved performance (AUROC = 0.807, 95% CI: 0.626–0.948). In Singapore, TL yielded modest gains (AUROC = 0.955 vs. 0.945). These findings highlights the potential of TL to improve prediction accuracy across diverse healthcare contexts and to support equitable and safe global AI adoption.
Similar content being viewed by others
Introduction
Artificial Intelligence (AI) has become a powerful tool in supporting healthcare and clinical decision-making1, but its benefits are unevenly distributed due to significant healthcare inequities2. Much of health AI research has focused on high-income and upper-middle-income countries, raising concerns about the generalizability and applicability of AI solutions globally, particularly in low-resource settings2. Zyl et al.3 identified financial constraints as one of several factors contributing to challenges in low-data-resource settings (LDRS)3,4, where disparities are further compounded by systemic issues beyond financial pressures. This results in more pronounced healthcare inequities than reported in studies focusing solely on financial barriers, as the assumption that healthcare solutions in high-income countries can address all population needs may be unfounded3.
The demand for healthcare services worldwide is increasing due to factors like population aging and the growing complexity of medical conditions. In response, healthcare systems worldwide must find innovative strategies to manage limited resources effectively. Risk assessment, which prioritizes patients at higher risk of poor outcomes or requiring urgent intervention, is central to this process. However, the development of accurate and context-specific risk prediction models in LDRS is constrained by limited access to large, high-quality datasets, preventing the creation of tailored solutions for these populations.
In such settings, clinicians frequently rely on externally developed models trained on high-resource datasets5. However, these models often experience significant performance declines when applied to populations that differ from the original dataset6. For example, the HAS-BLED score7, a tool to assess bleeding risk in atrial fibrillation patients, was developed using a European cohort but dropped significantly in performance when validated in more diverse global cohorts8. Specifically, the area under the receiver operating characteristic curve (AUROC) decreased from 0.72 (95% CI: 0.65–0.79) to 0.65 (95% CI: 0.61–0.68)7,8, highlighting the need for adaptable AI models that can be localized to specific regions and populations.
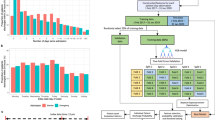
Transfer learning (TL) is an advanced AI technique designed to adapt pre-trained models, built on large datasets, to new settings with limited local data9,10. As illustrated in Fig. 1, this technique enables the reuse of existing model parameters to improve performance in new settings without the need for extensive new data collection10, making it particularly valuable in LDRS. For example, Hwang et al.11 demonstrated the effectiveness of TL by adapting an existing deep neural network model12, developed from the Korean National Health and Nutritional Examination Survey data, to predict low-density lipoprotein cholesterol levels, further refining it with local data from Wonju Severance Christian Hospital11. Despite its potential, the application of TL in clinical research, particularly in LDRS, remains underexplored, presenting an opportunity to address critical gaps in global healthcare equity10.
A source model, trained on large source data from high-resource settings, often performs poorly when applied to small target data from low-resource settings. A target model, trained only on target data, may also be suboptimal. TL improves predictive performance by adapting the source model using limited target data, producing a TL model better suited for low-data-resource settings (LDRS).
To demonstrate the applicability of TL, we aimed to address a clinical question requiring accurate risk assessment that is influenced by regional data variability due to epidemiological differences and other factors contributing to global healthcare disparities. Out-of-hospital cardiac arrest (OHCA) was chosen as proof of concept, as it is a life-threatening emergency where the heart suddenly stops functioning outside a hospital, and immediate medical intervention is crucial. Oxygen deprivation to the brain and other vital organs can cause irreversible damage within minutes13,14. Even when return of spontaneous circulation (ROSC) is achieved and patients receive intensive care, many OHCA patients suffer from poor neurological outcomes due to ischemic injury sustained during the arrest15,16. Predicting neurological recovery is therefore useful for guiding clinical decisions, such as whether to continue intensive care or withdrawing life-sustaining treatment15. However, in LDRS, where data collection is particularly challenging, large-scale datasets for OHCA studies are often unavailable, complicating the development of accurate predictive models.
In response to these challenges, we applied TL to develop a neurological outcome prediction model specifically tailored for regions with limited data, using an existing external model and the Pan-Asian Resuscitation Outcomes Study (PAROS) network17. Our goal is to demonstrate TL’s capacity to improve predictive accuracy for critical outcomes, such as OHCA, while also promoting its ethical deployment and scalable implementation in LDRS and beyond. Through this study, we aim to showcase how TL can drive global healthcare innovation by creating scalable, equitable AI models that can improve patient outcomes and help reduce healthcare disparities worldwide.
Results
The Vietnam and Singapore cohorts consisted of 243 and 15,916 patients, respectively. Figure 2 illustrates the cohort formation process, with a 6:4 split between training and testing datasets for both cohorts. Details on missing data proportions are available in Supplementary Table 1. The descriptive statistics are summarized in Table 1, with continuous variables presented as medians with interquartile ranges, and categorical variables reported as counts and percentages. Compared to the original Japanese study cohort, the Vietnam dataset featured significantly younger patients, contributing to greater data heterogeneity.
The flowchart details patient selection for (A) the Vietnam cohort, which was narrowed from 207,450 cases to 243, and (B) the Singapore cohort, which was narrowed from 28,660 cases to 15,916. Exclusions were primarily based on incident year, patient age, and completeness of neurological outcome data.
TL models were independently fitted using the training datasets for Vietnam and Singapore and evaluated on their respective testing datasets and compared with the external model. As shown in Supplementary Table 5, the TL model significantly outperformed the external model in both cohorts. The TL-Vietnam model, adapted using local data from Vietnam, improved performance compared to the external model, achieving an AUROC of 0.807 (95% CI: 0.626–0.948), up from the external model’s AUROC of 0.467 (95% CI: 0.141–0.785). Similarly, the TL-Singapore model, adapted using the local data from Singapore, achieved an AUROC of 0.955 (95% CI: 0.940–0.967), slightly outperforming the external model’s AUROC of 0.945 (95% CI: 0.929–0.958). The AUPRC also improved with the application of TL. On the Vietnam dataset, AUPRC increased from 0.428 for the external model to 0.889 for the TL-Vietnam model. On the Singapore dataset, AUPRC increased from 0.527 to 0.885. Specificity values at fixed sensitivity thresholds, detailed in Table 2, further confirmed that the TL models consistently outperformed the external model.
The parameters of the TL-Vietnam and TL-Singapore models are provided in Supplementary Tablse 2 and 3. These findings demonstrate the ability of TL to enhance model performance, particularly in adapting externally developed models to diverse geographic and resource-limited settings.
Discussion
This study demonstrates the feasibility and utility of TL in adapting existing predictive models to new clinical contexts, especially in LDRS. Using OHCA as a proof of concept, we showed that TL can significantly enhance model performance with smaller datasets, as observed in Vietnam, and provide incremental benefits with larger datasets, as seen in Singapore. These findings highlight TL’s broad applicability across diverse global healthcare settings, offering a scalable solution for developing robust predictive models and reducing healthcare disparities by tailoring models to specific regional contexts.
Healthcare research in LDRS faces numerous challenges, including small population sizes, low outcome prevalence, and disparities in epidemiological features and data collection systems. Importantly, even high-income regions are not immune to these issues. For example, in OHCA, where favorable neurological outcomes are rare (3–4%), large datasets are essential for robust model development. The external model used in this study was developed from 46,918 OHCA patients in Japan over 5–6 years18, providing a solid foundation for model development and validation. In contrast, Singapore, with only approximately 3000 annual OHCA cases, would require more than a decade to accumulate a comparable dataset. While both Singapore and Japan are considered developed countries, conducting such research in Singapore is more challenging due to differences in population size. The situation is even more difficult in data-constrained settings like Vietnam, where OHCA databases are still emerging. Despite approximately 4000 annual cases, it would still take over 10 years to collect enough data for robust model development. These prolonged timelines delay the implementation of predictive models that could improve patient outcomes and exacerbate global healthcare disparities, highlighting the urgent need for innovative solutions to address data gaps in LDRS.
AI techniques like TL provide an effective solution by adapting existing models to local populations, improving predictive performance even with scarce data. This study highlights the transformative potential of TL for developing accurate prediction models in LDRS, where socio-ecological factors, in addition to financial constraints3, influence healthcare outcomes. In Vietnam (n = 243), TL significantly enhanced model accuracy. In contrast, in Singapore (n = 15,916), TL provided more modest gains, illustrating its adaptability across different resource levels. Despite Singapore’s larger dataset, the annual OHCA case numbers remain insufficient to independently develop models comparable to those built with Japan’s extensive data. These findings underscore the utility of TL in leveraging external information to overcome local dataset limitations, enabling the development of clinically relevant models tailored to specific populations. By addressing heterogeneity in data distributions and clinical practices, TL enhances the reliability and applicability of predictive models, while supporting ethical AI deployment that respects contextual limitations and health equity concerns.
Analyzing the feature weights in Supplementary Tables 2 and 3 provides insight into the mechanism by which TL enhances model performance. In the data-scarce Vietnam cohort, a locally trained model shrunk the coefficients of clinically important predictors to zero, whereas the TL model retained these features with non-zero coefficients by leveraging knowledge from the source domain. In contrast, for the data-rich Singapore cohort, TL produced minor modifications to the coefficient values of an already robust model. This demonstrates that the function of TL is context-dependent: it preserves critical predictive information in low-resource settings and refines model parameters in high-resource ones.
As shown in Table 2, the benefits of TL were most pronounced with the Vietnam cohort, where the improvement in overall prediction performance was more significant than in Singapore. This supports the theoretical foundations of TL10, which is particularly effective when the source data (e.g., the Japanese cohort) has a large sample size and the target data (e.g., Vietnam and Singapore) is relatively limited. This study demonstrates the applicability of TL in challenging settings like LDRS, showing how researchers can directly leverage knowledge from external studies without requiring access to additional datasets or direct collaborations. Federated learning (FL)19, another relevant AI technique, addresses data privacy concerns in cross-site collaboration by enabling co-training of AI models without sharing data20. Unlike FL, which requires simultaneous participation from multiple data owners, TL allows independent adaptation of publicly available models. This makes TL particularly advantageous for researchers with limited access to external data or collaboration opportunities, offering a practical way to overcome barriers associated with data sharing and resource constraints10.
TL is a flexible AI approach applicable to a wide range of models and knowledge transfer scenarios10, such as transferring insights on drug sensitivity between different cancer types21or adapting knowledge of surgical complications across patient groups22. In LDRS, where collecting large, high-quality datasets is challenging, TL offers an efficient way to leverage existing models for improved predictive performance. Regardless of the clinical or biomedical domain, as Li et al.10 highlight, the successful implementation of TL depends on carefully selecting an appropriate external study and ensuring that the chosen TL framework aligns with the research question. It is also crucial to address potential privacy concerns when building or using external models. When co-training is required, FL can be integrated into TL frameworks to enable secure collaborations across multiple sites, ensuring data privacy while still facilitating knowledge transfer.
One reason for TL’s effectiveness in this study may be the standardized data format and consistent variable definitions under the PAROS study framework. The Utstein data format, adopted in this study, has been globally accepted since its establishment in 1995, and most countries utilize it for OHCA data collection23. Furthermore, the prehospital management pathways for OHCA cases follow similar protocols across the study countries—paramedics respond to an emergency call, perform resuscitation, and transport patients to hospitals. During this clinical pathway, prehospital OHCA data are systematically collected, which likely facilitated effective knowledge transfer using TL.
Another potential reason is that certain predictors, such as ROSC status, are expected to be strongly associated with patient outcomes, despite variability in unmeasured clinical factors like in-hospital care or hospital systems among the three countries24. Given these considerations, further research is essential to investigate the applicability of TL to the other clinical scenarios where unmeasured factors may significantly impact outcomes. For example, in patients with refractory VF, treatment strategies vary markedly across countries. In Japan, advanced invasive resuscitation procedures, such as extracorporeal cardiopulmonary resuscitation, are commonly performed and may contribute improved outcomes24. In contrast, such procedures are rarely utilized in Singapore and Vietnam24. It remains unclear whether TL would perform well in contexts where critical unmeasured factors, such as the treatment strategy or in-hospital care, vary substantially and may significantly affect patients’ outcomes.
Future research should explore strategies for handling ultra-small datasets, where outcome prevalence is extremely low or absent. In this study, the Vietnam dataset included 234 cases with only 13 positive outcomes, but settings with even fewer cases present greater challenges. In such instances, the TL method used here may not be directly applicable. To enhance model robustness and improve predictive reliability, alternative approaches—such as synthetic data generation and oversampling—should be integrated with TL. Combining these techniques within TL frameworks may further mitigate data scarcity in low-resource clinical settings.
Moreover, while TL has potential for application in data-scarce environments, practical implementation in low-income countries poses additional challenges. Foundational barriers such as the absence of reliable infrastructure for routine data collection can severely limit model development. Furthermore, the successful adoption of such AI-driven approaches also depends on whether local clinicians understand and accept the technology. Future efforts should consider capacity building, local context adaptation, and clinician training as key components of model deployment.
This study has several limitations. First, our primary limitation is the small Vietnam cohort, with only 13 positive neurological outcomes. This low event count results in insufficient statistical power, a finding confirmed by our results which yielded very wide 95% confidence intervals for the AUROC (see Table 2 and Supplementary Table 5). Consequently, the findings for this cohort must be considered exploratory rather than definitive. Second, while the Singapore data were derived from a nationwide population-based registry for OHCA patients and are likely representative of the Singapore population, the Vietnam data were collected from a limited number of hospitals in Ho Chi Minh, Hanoi, and Hue, which are relatively large urban areas in Vietnam. As a result, the Vietnam data may not be representative of the broader population, potentially limiting the generalizability of the model to current clinical settings in Vietnam and may have a concern about the applicability to the rural regions or settings where the different emergency medical system is working. Third, although the data from Vietnam, Singapore, and Japan were collected using an internationally standardized format with consistent definitions, differences in local clinical practices and resuscitation protocols may have influenced data collection and reporting. This might lead to a risk of measurement bias. Furthermore, in Vietnam, the lack of a centralized EMS system and the hospital-based nature of data collection make it difficult to capture some prehospital variables. For example, critical information such as the initial cardiac rhythm assessed by EMS and whether an AED was applied by a bystander is often missing or inconsistently reported. Finally, a critical limitation is the lack of prospective external validation, which is essential before any clinical prediction model can be considered for real-world deployment. Therefore, our models should be considered foundational and are not ready for clinical application. While such validation is crucial, suitable independent datasets from Vietnam or Singapore are not currently available. Future prospective studies are therefore a necessary next step.
In conclusion, this study demonstrates that TL has the potential to bridge regional resource disparities in healthcare. While applied here to OHCA, TL’s adaptability extends to other emergency conditions with low event rates, such as trauma, sepsis, heart failure, and stroke. Moreover, TL holds broader potential beyond emergency medicine, offering a scalable, efficient strategy to enhance clinical decision-making in LDRS globally. By reducing reliance on large-scale data collection, TL facilitates equitable global access to AI-driven predictive models, helping to reduce healthcare disparities and optimize patient outcomes in data-constrained environments.
Methods
Study design and setting
This study was a secondary and retrospective analysis of data from the PAROS registry17. PAROS is a collaborative clinical research initiative established by international emergency medical professionals and researchers to investigate the epidemiology of OHCA across the Asia-Pacific region17,25,26. Specifically, this analysis utilized data from the PAROS 2 international dataset, a prospective, observational registry encompassing OHCA cases from 13 regions27.
To ensure uniformity in outcome reporting, all PAROS participants adhered to a standardized taxonomy and data collection protocol. The registry included all OHCA cases reported by emergency medical services (EMS), defined as the absence of a pulse, unresponsiveness, and apnea within the participating regions. A wide range of variables was collected, including patient demographics (e.g., age, gender), event-specific information (e.g., location type, bystander cardiopulmonary resuscitation (CPR)), and EMS-related data (e.g., drug administration).
Study population
This study analyzed adult OHCA patients recorded in the PAROS database from January 2017 to December 2021 in Singapore and Vietnam. Pediatric patients (<18 years), those missing epinephrine data, or those without detailed neurological outcome records were excluded. Two local cohorts were formed to represent settings with different sample sizes: a small sample size cohort from Vietnam (Ho Chi Minh City, Hue, Hanoi) and a large sample size cohort from Singapore.
Variables
The variables selected for outcome predictions are consistent with those used in the Japan study21. These include: age (in years), gender (male/female), first recorded cardiac rhythm (ventricular fibrillation (VF)/pulseless ventricular tachycardia (pVT), pulseless electrical activity (PEA) or asystole), no flow time (duration between collapse and CPR start in minutes), low-flow time (time from initiation of CPR to return of spontaneous circulation (ROSC), in minutes), use of bystander automated external defibrillator (AED) (yes/no), prehospital defibrillation (yes/no), prehospital administration of epinephrine (yes/no) and cardiac rhythm at emergency department (ED) arrival (VF/pVT, PEA, asystole or ROSC). Details of these variables are available in Supplementary Table 4.
Outcomes
The primary outcome was binary, defined as survival with favorable neurological outcomes (Cerebral Performance Category (CPC) score of 1 or 2) at 30 days post-arrest or at discharge. The CPC score was assessed by the treating physician.
Data preprocessing
Missing values in the predictors were imputed using the missForest R package28, a nonparametric missing value imputation method widely used in clinical and biomedical studies28,29. For numerical predictors, additional data transformations were applied: age, no flow time, and low flow time were standardized, and a log transformation was applied to the low-flow time variable to align with the methodology of the Japanese study18.
Prediction modeling
The original model developed by Nishioka et al.18 used least absolute shrinkage and selection operator (Lasso) regression to predict neurological outcomes in Japanese OHCA patients, achieving an AUROC of 0.943 (95% confidence interval (CI): 0.934–0.953). This model was trained on the Osaka CRITICAL database18 (17,385 patients) and validated using the JAAM-OHCA registry18 (29,633 patients), providing a robust foundation for neurological outcome prediction.
To adapt this model to the PAROS datasets, we employed the Trans-Lasso30 algorithm, which integrates TL techniques tailored for Lasso regression models. The Trans-Lasso algorithm was initialized with the model parameters reported in the original Japanese study and then refined using data from the PAROS registry to create cohort-specific predictive models. For baseline comparisons, the performance of the original Japanese model (external model) was evaluated directly on both the Vietnam and Singapore cohorts. The implementation of the Trans-Lasso algorithm used in this study can be accessed at https://github.com/nliulab/Clinical-Transfer-Learning. The analysis was performed in R (version 4.3.1) and does not require specialized hardware; it can be executed on a standard laptop with a single CPU core.
The same predictors as the external model were used in our analysis, but the outcome of interest was redefined as good neurological outcomes. Model performance was assessed using the AUROC and the area under the precision-recall curve (AUPRC). Sensitivity and specificity values were also calculated to evaluate the model’s ability to correctly identify cases with and without good neurological outcomes. All statistical analyses were conducted using R software version 4.3.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Ethical statement
This retrospective analysis was approved by the relevant ethics committees at each participating PAROS site and by the Centralized Institutional Review Board and Domain Specific Review Board for Singapore (reference numbers: 2013/604/C, 2013/00929 and 2018/2937). Informed consent was waived due to the observational nature of the study, and all data were de-identified.
Data availability
The PAROS dataset contains confidential information and is governed by IRB restrictions. In accordance with these policies, the data are available to qualified researchers upon reasonable request, pending approval from the PAROS governing body.
Code availability
The R code is available at https://github.com/nliulab/Clinical-Transfer-Learning.
References
Okada, Y., Mertens, M., Liu, N., Lam, S. S. W. & Ong, M. E. H. AI and machine learning in resuscitation: ongoing research, new concepts, and key challenges. Resusc Plus 15, 100435 (2023).
Yang, R. et al. Disparities in clinical studies of AI enabled applications from a global perspective. Npj Digit. Med. 7, 1–3 (2024).
Van Zyl, C., Badenhorst, M., Hanekom, S. & Heine, M. Unravelling ‘low-resource settings’: a systematic scoping review with qualitative content analysis. BMJ Glob. Health 6, e005190 (2021).
Rowe, A. K., Savigny, D. de, Lanata, C. F. & Victora, C. G. How can we achieve and maintain high-quality performance of health workers in low-resource settings?. Lancet 366, 1026–1035 (2005).
Yang, C. et al. Trends in the conduct and reporting of clinical prediction model development and validation: a systematic review. J. Am. Med. Inform. Assoc. 29, 983–989 (2022).
Siontis, G. C. M., Tzoulaki, I., Castaldi, P. J. & Ioannidis, J. P. A. External validation of new risk prediction models is infrequent and reveals worse prognostic discrimination. J. Clin. Epidemiol. 68, 25–34 (2015).
Pisters, R. et al. A Novel User-Friendly Score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro heart survey. Chest 138, 1093–1100 (2010).
Lip, G. Y. H., Frison, L., Halperin, J. L. & Lane, D. A. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) Score. J. Am. Coll. Cardiol. 57, 173–180 (2011).
Day, O. & Khoshgoftaar, T. M. A survey on heterogeneous transfer learning. J. Big Data 4, 29 (2017).
Bridging Data Gaps in Healthcare: A Scoping Review of Transfer Learning in Structured Data Analysis. https://doi.org/10.34133/hds.0321.
Hwang, S. et al. A deep neural network for estimating low-density lipoprotein cholesterol from electronic health records: real-time routine clinical application. JMIR Med. Inform. 9, e29331 (2021).
Lee, T., Kim, J., Uh, Y. & Lee, H. Deep neural network for estimating low density lipoprotein cholesterol. Clin. Chim. Acta Int. J. Clin. Chem. 489, 35–40 (2019).
Myat, A., Song, K.-J. & Rea, T. Out-of-hospital cardiac arrest: current concepts. Lancet 391, 970–979 (2018).
Marijon, E. et al. The Lancet Commission to reduce the global burden of sudden cardiac death: a call for multidisciplinary action. Lancet Lond. Engl. 402, 883–936 (2023).
Nolan, J. P. et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 47, 369–421 (2021).
Semeraro, F. et al. European Resuscitation Council Guidelines 2021: Systems saving lives. Resuscitation 161, 80–97 (2021).
Ong, M. E. H. et al. Pan-Asian Resuscitation Outcomes Study (PAROS): rationale, methodology, and implementation. Acad. Emerg. Med. 18, 890–897 (2011).
Nishioka, N. et al. External validation of updated prediction models for neurological outcomes at 90 Days in patients with out-of-hospital cardiac arrest. J. Am. Heart Assoc. 13, e033824 (2024).
Li, S. et al. Federated learning in healthcare: a benchmark comparison of engineering and statistical approaches for structured data analysis. Health Data Sci. 4, 0196 (2024).
Li, S. et al. Federated and distributed learning applications for electronic health records and structured medical data: a scoping review. J. Am. Med. Inform. Assoc. ocad170 https://doi.org/10.1093/jamia/ocad170 (2023).
Kim, S., Kim, K., Choe, J., Lee, I. & Kang, J. Improved survival analysis by learning shared genomic information from pan-cancer data. Bioinformatics 36, i389–i398 (2020).
Lorenzi, E., Henao, R. & Heller, K. Hierarchical infinite factor models for improving the prediction of surgical complications for geriatric patients. Ann. Appl. Stat. 13, 2637–2661 (2019).
Jacobs, I. et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 110, 3385–3397 (2004).
Okada, Y. et al. Outcome assessment for out-of-hospital cardiac arrest patients in Singapore and Japan with initial shockable rhythm. Crit. Care Lond. Engl. 27, 351 (2023).
Ong, M. E. H. et al. Rationale, methodology, and implementation of a dispatcher-assisted cardiopulmonary resuscitation Trial in the Asia-Pacific (Pan-Asian Resuscitation Outcomes Study Phase 2). Prehosp. Emerg. Care 19, 87–95 (2015).
Doctor, N., Ahmad, N., Pek, P., Yap, S. & Ong, M. The Pan-Asian Resuscitation Outcomes Study (PAROS) clinical research network: what, where, why and how. Singap. Med. J. 58, 456–458 (2017).
Liu, N. et al. Development and validation of an interpretable prehospital return of spontaneous circulation (P-ROSC) score for patients with out-of-hospital cardiac arrest using machine learning: a retrospective study. eClinicalMedicine 48, 101422 (2022).
Stekhoven, D. J. & Bühlmann, P. MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics 28, 112–118 (2012).
Aracri, F., Giovanna Bianco, M., Quattrone, A. & Sarica, A. Imputation of missing clinical, cognitive and neuroimaging data of Dementia using missForest, a Random Forest based algorithm. in 2023 IEEE 36th International Symposium on Computer-Based Medical Systems (CBMS) 684–688 https://doi.org/10.1109/CBMS58004.2023.00300 (2023).
Li, S., Cai, T. T. & Li, H. Transfer Learning for High-Dimensional Linear Regression: Prediction, Estimation and Minimax Optimality. J. R. Stat. Soc. Ser. B Stat. Methodol. 84, 149–173 (2022).
Acknowledgements
We would like to express our gratitude to all the other participating members of the Pan-Asian Resuscitation Outcomes Study Clinical Research Network (PAROS CRN) for their invaluable contributions. Participating Site Investigators: H Tanaka (Kokushikan University); SD Shin (Seoul National University College of Medicine); MHM Ma (National Taiwan University Hospital Yunlin Branch); K Kajino (Kansai Medical University); CH Lin (National Cheng Kung University); CW Kuo (Chang-Gung Memorial Hospital); S Karim (Hospital Sungai Buloh); S Jirapong (Rajavithi Hospital); P Khruekarnchana (Rajavithi Hospital); RH Ho (Chonnam National University Medical School and Hospital); HW Ryoo (Kyungpook National University); Tagashi Tagami (Nippon Medical School Tama Nagayama Hospital); PCI Ko (National Taiwan University, Yun-Lin Branch Hospital); KD Wong (Hospital Pulau Pinang); N Sumetchotimaytha (Rajavithi Hospital); FJ Gaerlan (Southern Philippines Medical Center); B Velasco (East Avenue Medical Center), GV Ramana Rao (GVK Emergency Management and Research Institute Telangana); W Cai (Zhejiang Provincial People’s Hospital); S Fei (Beijing Chaoyang Hospital); N Khan (Aga Khan University); ME Sayed (American University of Beirut Medical Center); MI Abuamllouh (Dubai Corporation for Ambulance Services); CB Yang (Sarawak General Hospital); Vimal M (GVK Emergency Management and Research Institute); Rajanarsing Rao HV (GVK Emergency Management and Research Institute); M Khursheed (National Institute of Cardiovascular Diseases); PJ Tiglao (Corazon Locsin Montelibano Memorial Regional Hospital); Zhou SA (Zhejiang Provincial People's Hospital); A Alhumodi (Abu Dhabi Police GHQ). We would like to thank Ms Pin Pin Pek and Ms Nur Shahidah from the Prehospital and Emergency Care Research Centre, Duke-NUS Medical School for coordination of the study, and Ms Patricia Tay from the Singapore Clinical Research Institute for her role as Network Secretariat for the PAROS CRN. We also extend our sincere appreciation to Dr. Chuan Hong (Duke University) and Dr. Molei Liu (Peking University) for their invaluable expertise, support, and guidance in providing the source code for implementing the Trans-Lasso algorithm, which significantly contributed to the analytic framework of this study. This study was supported by grants from SingHealth Duke-NUS ACP Programme Funding (15/FY2020/P2/06-A79), National Medical Research Council, Clinician Scientist Awards, Singapore (NMRC/CSA/024/2010, NMRC/CSA/0049/2013 and NMRC/CSA-SI/0014/2017), Ministry of Health, Health Services Research Grant, Singapore (HSRG/0021/2012) and Laerdal Foundation (20040). The funders are not involved in the study design, collection, analysis, and interpretation of data, nor do they have a role in the writing of the paper and decision to submit the paper for publication. SL was supported by the KPFA scholarship (Duke-NUS-KPFA/2025/0081). YO was supported by the research grant from the ZOLL foundation, and the scholarship from JSPS-Overseas Scholarship and the KPFA scholarship (Duke-NUS-KPFA/2024/0073). The study funders had no role in the design, data collection, analysis, interpretation, or manuscript preparation.
Author information
Authors and Affiliations
Consortia
Contributions
S.L.: Conceptualization, Methodology, Analysis, Project administration, Writing – original draft, Writing—review & editing. Y.O.: Methodology, Analysis, Data curation, Writing—original draft, Writing—review & editing. W.G.: Analysis, Data curation, Writing—original draft, Writing—review & editing. M.H.C.: Data curation, Writing – review & editing. S.N.D.: Data acquisition, Writing—review & editing. Q.D.P.: Data acquisition, Writing—review & editing. Q.T.H.: Data acquisition, Writing—review & editing. M.E.H.O.: Investigation, Resources, Writing—review & editing. N.L.: Conceptualization, Project administration, Funding acquisition, Resources, Writing—review & editing. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
M.E.H.O. reports grants from the Laerdal Foundation, Laerdal Medical, and Ramsey Social Justice Foundation for funding of the Pan-Asian Resuscitation Outcomes Study; an advisory relationship with Global Healthcare Singapore (SG), a commercial entity that manufactures cooling devices. MEH Ong has a licensing agreement with ZOLL Medical Corporation and patent filed (Application no: 13/047,348) for a “Method of predicting acute cardiopulmonary events and survivability of a patient”. He is also the co-founder and scientific advisor of Technology Innovation in Medicine (TIIM) Healthcare, a commercial entity which develops real-time prediction and risk stratification solutions for triage. He is a member of the Editorial Board of Resuscitation. YO has received a research grant from the ZOLL Foundation and an overseas scholarship from the FUKUDA Foundation for Medical Technology and the International Medical Research Foundation. All other authors have no conflict of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, S., Okada, Y., Gu, W. et al. Leveraging AI and transfer learning to enhance out-of-hospital cardiac arrest outcome prediction in diverse setting. npj Digit. Med. 8, 716 (2025). https://doi.org/10.1038/s41746-025-02088-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-025-02088-x