Abstract
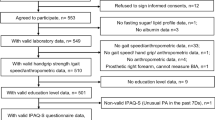
The Asian Working Group for Sarcopenia (AWGS) presents an updated 2025 consensus reframing sarcopenia management through a life-course approach to muscle health promotion. While aligning with the Global Leadership Initiative in Sarcopenia (GLIS), this update provides healthcare providers with Asia-specific guidance. The consensus introduces three key refinements: first, expanding sarcopenia diagnosis to middle-aged adults (50‒64 years) with validated diagnostic thresholds; second, simplifying the diagnostic algorithm to require only concurrent low muscle mass and strength, with physical performance as an outcome measure; and third, introducing an enhanced muscle health framework recognizing skeletal muscle as vital for healthy longevity, emphasizing cross-talk with brain, bone, adipose tissue and immune systems. This framework leverages the World Health Organization’s Integrated Care for Older People (ICOPE) implementation for enhanced case-finding through natural overlap between muscle health and ICOPE’s intrinsic capacity domains. The consensus provides evidence-based recommendations for multimodal interventions that combine resistance exercise with nutritional supplementation, representing advancement toward proactive muscle health promotion and establishing a framework for reducing age-related decline in Asian populations.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chen, L. K. Sarcopenia in the era of precision health: toward personalized interventions for healthy longevity. J. Chin. Med. Assoc. 87, 980–987 (2024).
Anker, S. D., Morley, J. E. & von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J. Cachexia Sarcopenia Muscle 7, 512–514 (2016).
Chen, L. K. et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 15, 95–101 (2014).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39, 412–423 (2010).
Chen, L. K. et al. Recent advances in sarcopenia research in Asia: 2016 update from the Asian Working Group for Sarcopenia. J. Am. Med Dir. Assoc. 17, 767.e1–7 (2016).
Chen, L. K. et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med Dir. Assoc. 21, 300–307 (2020).
Dhar, M. et al. South Asian Working Action Group on SARCOpenia (SWAG-SARCO) - a consensus document. Osteoporos. Sarcopenia 8, 35–57 (2022).
Baek, J. Y. et al. Korean Working Group on Sarcopenia Guideline: expert consensus on sarcopenia screening and diagnosis by the Korean Society of Sarcopenia, the Korean Society for Bone and Mineral Research, and the Korean Geriatrics Society. Ann. Geriatr. Med Res 27, 9–21 (2023).
Ji, S., Baek, J. Y., Lee, E., Jang, I. Y. & Jung, H. W. Phenotype validation of the Korean working group on sarcopenia guideline. Arch. Gerontol. Geriatr. 117, 105251 (2024).
Shim, G. Y., Jang, H. C., Kim, K. W. & Lim, J. Y. Impact of Sarcopenia on falls, mobility limitation, and mortality using the diagnostic criteria proposed in the Korean Working Group on Sarcopenia Guideline. Ann. Geriatr. Med. Res. 29, 38–44 (2025).
Peng, L. N. C. D. et al. Advancing Sarcopenia diagnosis and treatment: recommendations from the Taiwan Advisory Panel for Sarcopenia. Aging Med. Healthc. 15, 8–14 (2024).
Kirk, B. et al. The conceptual definition of sarcopenia: Delphi Consensus from the Global Leadership Initiative in Sarcopenia (GLIS). Age Ageing https://doi.org/10.1093/ageing/afae052 (2024).
World Health Organization. Integrated Care for Older People: Guidelines on Community-level Interventions to Manage Declines in Intrinsic Capacity https://iris.who.int/server/api/core/bitstreams/4639a0b9-f77e-48db-9617-987aabb143f2/content/ (WHO, 2017).
Weng, S. E. et al. The evolving landscape of sarcopenia in Asia: a systematic review and meta-analysis following the 2019 Asian Working Group for Sarcopenia (AWGS) diagnostic criteria. Arch. Gerontol. Geriatr. 128, 105596 (2025).
Yamada, M. et al. Clinical practice for sarcopenia in Asia: online survey by the Asian Working Group for Sarcopenia. Arch. Gerontol. Geriatr. 115, 105132 (2023).
Zhang, S. et al. Muscle function outweighs appendicular lean mass in predicting adverse outcomes: evidence from Asian longitudinal studies. J. Nutr. Health Aging 28, 100403 (2024).
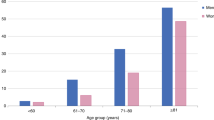
Chen, L. K. et al. Mapping normative muscle health metrics across the aging continuum: a multinational study pooling data from eight cohorts in Japan, Malaysia and Taiwan. J. Cachexia Sarcopenia Muscle 16, e13731 (2025).
Pedersen, B. K. & Febbraio, M. A. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 8, 457–465 (2012).
Hsu, P. S. et al. Safeguarding vitality and cognition: the role of sarcopenia in intrinsic capacity decline among octogenarians from multiple cohorts. J. Nutr. Health Aging 28, 100268 (2024).
McGregor, R. A., Cameron-Smith, D. & Poppitt, S. D. It is not just muscle mass: a review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev. Healthspan 3, 9 (2014).
Groeneveld, K. Muscle physiology and its relations to the whole body in health and disease. Acta Physiol. 240, e14131 (2024).
Riviati, N. & Indra, B. Relationship between muscle mass and muscle strength with physical performance in older adults: a systematic review. SAGE Open Med. 11, 20503121231214650 (2023).
Breen, L. & Phillips, S. M. Skeletal muscle protein metabolism in the elderly: interventions to counteract the ‘anabolic resistance’ of ageing. Nutr. Metab. 8, 68 (2011).
Andersen, J. L. Muscle fibre type adaptation in the elderly human muscle. Scand. J. Med. Sci. Sports 13, 40–47 (2003).
Ehrhardt, J. & Morgan, J. Regenerative capacity of skeletal muscle. Curr. Opin. Neurol. 18, 548–553 (2005).
Naranjo, J. D., Dziki, J. L. & Badylak, S. F. Regenerative medicine approaches for age-related muscle loss and sarcopenia: a mini-review. Gerontology 63, 580–589 (2017).
Roman, W. et al. Muscle repair after physiological damage relies on nuclear migration for cellular reconstruction. Science 374, 355–359 (2021).
Fujitani, M., Tarif, A. M. M. & Otani, Y. Regeneration mechanisms and therapeutic strategies for neuromuscular junctions in aging and diseases. Neural Regen. Res. 20, 193–194 (2025).
López-Otín, C., Blasco, M. A., Partridge, L., Serrano, M. & Kroemer, G. Hallmarks of aging: an expanding universe. Cell 186, 243–278 (2023).
Boccardi, V. Sarcopenia: a dive into metabolism to promote a multimodal, preventive, and regenerative approach. Mech. Ageing Dev. 219, 111941 (2024).
Lee, W. J. et al. Enhancing intrinsic capacity and related biomarkers in community-dwelling multimorbid older adults through integrated multidomain interventions: ancillary findings from the Taiwan Integrated Geriatric (TIGER) Trial. J. Am. Med. Dir. Assoc. https://doi.org/10.1016/j.jamda.2023.10.006 (2023).
Ali, S. R., Nkembo, A. T., Tipparaju, S. M., Ashraf, M. & Xuan, W. Sarcopenia: recent advances for detection, progression, and metabolic alterations along with therapeutic targets. Can. J. Physiol. Pharm. 102, 697–708 (2024).
Hu, P. et al. The effect of social isolation on sarcopenia: a longitudinal study among the middle-aged and older population in China. Gerontology 69, 748–756 (2023).
Izquierdo, M. et al. Global consensus on optimal exercise recommendations for enhancing healthy longevity in older adults (ICFSR). J. Nutr. Health Aging 29, 100401 (2025).
Lin, H. Y., Lin, Y. C., Chen, L. K. & Hsiao, F. Y. Untangling the complex interplay between social isolation, anorexia, sarcopenia, and mortality: insights from a longitudinal Study. J. Nutr. Health Aging 27, 797–805 (2023).
Peng, K. Y. et al. Vitality attributes and their associations with intrinsic capacity, resilience, and happiness in community-dwelling adults: results from Gan-Dau Healthy Longevity Plan Wave 2. J. Nutr. Health Aging 29, 100559 (2025).
Lee, W. J., Peng, L. N., Lin, M. H., Loh, C. H. & Chen, L. K. Letter to the editor: disentangling mortality associations: an in-depth comparative study of possible sarcopenia versus sarcopenia of AWGS 2019. J. Nutr. Health Aging 27, 685–686 (2023).
Lim, W. S. et al. Singapore clinical practice guidelines for sarcopenia: screening, diagnosis, management and prevention. J. Frailty Aging 11, 348–369 (2022).
Rose Berlin Piodena-Aportadera, M. et al. Calf circumference measurement protocols for sarcopenia screening: differences in agreement, convergent validity and diagnostic performance. Ann. Geriatr. Med. Res. 26, 215–224 (2022).
Malmstrom, T. K. & Morley, J. E. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J. Am. Med. Dir. Assoc. 14, 531–532 (2013).
Barbosa-Silva, T. G., Menezes, A. M., Bielemann, R. M., Malmstrom, T. K. & Gonzalez, M. C. Enhancing SARC-F: improving sarcopenia screening in the clinical practice. J. Am. Med. Dir. Assoc. 17, 1136–1141 (2016).
Tanaka, T., Takahashi, K., Akishita, M., Tsuji, T. & Iijima, K. Yubi-wakka” (finger-ring) test: a practical self-screening method for sarcopenia, and a predictor of disability and mortality among Japanese community-dwelling older adults. Geriatr. Gerontol. Int. 18, 224–232 (2018).
Tang, T. C. et al. FNIH-defined sarcopenia predicts adverse outcomes among community-dwelling older people in Taiwan: results from I-Lan Longitudinal Aging Study. J. Gerontol. A Biol. Sci. Med. Sci. 73, 828–834 (2018).
Kinoshita, K., Satake, S., Matsui, Y. & Arai, H. Association between sarcopenia and fall risk according to the muscle mass adjustment method in Japanese older outpatients. J. Nutr. Health Aging 25, 762–766 (2021).
Kinoshita, K., Satake, S., Matsui, Y. & Arai, H. Quantifying muscle mass by adjusting for body mass index is the best for discriminating low strength and function in Japanese older outpatients. J. Nutr. Health Aging 25, 501–506 (2021).
Beaudart, C. et al. Health outcomes of sarcopenia: a consensus report by the outcome working group of the Global Leadership Initiative in Sarcopenia (GLIS). Aging Clin. Exp. Res. 37, 100 (2025).
Lim, J. P. et al. Grip strength criterion matters: impact of average versus maximum handgrip strength on sarcopenia prevalence and predictive validity for low physical performance. J. Nutr. Health Aging 24, 1031–1035 (2020).
Auyeung, T. W., Arai, H., Chen, L. K. & Woo, J. Letter to the editor: normative data of handgrip strength in 26344 older adults - a pooled dataset from eight cohorts in Asia. J. Nutr. Health Aging 24, 125–126 (2020).
Negm, A. M., Lee, J., Hamidian, R., Jones, C. A. & Khadaroo, R. G. Management of sarcopenia: a network meta-analysis of randomized controlled trials. J. Am. Med. Dir. Assoc. 23, 707–714 (2022).
Geng, Q., Zhai, H., Wang, L., Wei, H. & Hou, S. The efficacy of different interventions in the treatment of sarcopenia in middle-aged and elderly people: a network meta-analysis. Medicine 102, e34254 (2023).
Shen, Y. et al. Exercise for sarcopenia in older people: a systematic review and network meta-analysis. J. Cachexia Sarcopenia Muscle 14, 1199–1211 (2023).
Zhu, L. Y. et al. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing 48, 220–228 (2019).
Lu, L. et al. Effects of different exercise training modes on muscle strength and physical performance in older people with sarcopenia: a systematic review and meta-analysis. BMC Geriatr. 21, 708 (2021).
Chen, Y. C. et al. Is moderate resistance training adequate for older adults with sarcopenia? A systematic review and network meta-analysis of RCTs. Eur. Rev. Aging Phys. Act. 20, 22 (2023).
Nunes, E. A. et al. Systematic review and meta-analysis of protein intake to support muscle mass and function in healthy adults. J. Cachexia Sarcopenia Muscle 13, 795–810 (2022).
Peng, L. N., Yu, P. C., Lee, H. F., Lin, M. H. & Chen, L. K. Protein-enriched diet improved muscle endurance and marginally reduced intramuscular adiposity: results from a randomized controlled trial among middle-aged and older adults. Arch. Gerontol. Geriatr. 96, 104436 (2021).
Kao, S. L. et al. Daily supplementation with protein-enriched lacto-vegetarian soups and muscle health in community-dwelling older adults: a randomized controlled trial. J. Nutr. Health Aging 29, 100477 (2025).
Bai, G. H., Tsai, M. C., Tsai, H. W., Chang, C. C. & Hou, W. H. Effects of branched-chain amino acid-rich supplementation on EWGSOP2 criteria for sarcopenia in older adults: a systematic review and meta-analysis. Eur. J. Nutr. 61, 637–651 (2022).
Peng, L. N. et al. Sarcojoint, the branched-chain amino acid-based supplement, plus resistance exercise improved muscle mass in adults aged 50 years and older: a double-blinded randomized controlled trial. Exp. Gerontol. 157, 111644 (2022).
Xu, Z. R., Tan, Z. J., Zhang, Q., Gui, Q. F. & Yang, Y. M. The effectiveness of leucine on muscle protein synthesis, lean body mass and leg lean mass accretion in older people: a systematic review and meta-analysis. Br. J. Nutr. 113, 25–34 (2015).
Gu, W. -T., Zhang, L. -W., Wu, F. -H. & Wang, S. The effects of β-hydroxy-β-methylbutyrate supplementation in patients with sarcopenia: a systematic review and meta-analysis. Maturitas 195, 108219 (2025).
Peng, L. N. et al. Oral nutritional supplement with β-hydroxy-β-methylbutyrate (HMB) improves nutrition, physical performance and ameliorates intramuscular adiposity in pre-frail older adults: a randomized controlled trial. J. Nutr. Health Aging 25, 767–773 (2021).
Phillips, S. M., Lau, K. J., D’Souza, A. C. & Nunes, E. A. An umbrella review of systematic reviews of β-hydroxy-β-methyl butyrate supplementation in ageing and clinical practice. J. Cachexia Sarcopenia Muscle 13, 2265–2275 (2022).
Bird, J. K., Troesch, B., Warnke, I. & Calder, P. C. The effect of long chain omega-3 polyunsaturated fatty acids on muscle mass and function in sarcopenia: a scoping systematic review and meta-analysis. Clin. Nutr. ESPEN 46, 73–86 (2021).
Tseng, P. T. et al. Omega-3 polyunsaturated fatty acids in sarcopenia management: a network meta-analysis of randomized controlled trials. Ageing Res. Rev. 90, 102014 (2023).
Prokopidis, K. et al. Impact of probiotics on muscle mass, muscle strength and lean mass: a systematic review and meta-analysis of randomized controlled trials. J. Cachexia Sarcopenia Muscle 14, 30–44 (2023).
Prokopidis, K. et al. Effect of vitamin D monotherapy on indices of sarcopenia in community-dwelling older adults: a systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 13, 1642–1652 (2022).
Widajanti, N. et al. The effect of vitamin D supplementation to parameter of sarcopenia in elderly people: a systematic review and meta-analysis. Can. Geriatr. J. 27, 63–75 (2024).
Cesari, M. et al. Challenges in the development of drugs for sarcopenia and frailty - report from the International Conference on Frailty and Sarcopenia Research (ICFSR) Task Force. J. Frailty Aging 11, 135–142 (2022).
Sumukadas, D., Witham, M. D., Struthers, A. D. & McMurdo, M. E. Effect of perindopril on physical function in elderly people with functional impairment: a randomized controlled trial. CMAJ 177, 867–874 (2007).
Burks, T. N. et al. Losartan restores skeletal muscle remodeling and protects against disuse atrophy in sarcopenia. Sci. Transl. Med. 3, 82ra37 (2011).
Yoshihara, T., Dobashi, S., Takaragawa, M. & Naito, H. Effect of losartan treatment on Smad signaling and recovery from hindlimb unloading-induced soleus muscle atrophy in female rats. Eur. J. Pharm. 931, 175223 (2022).
Papanicolaou, D. A. et al. A phase IIA randomized, placebo-controlled clinical trial to study the efficacy and safety of the selective androgen receptor modulator (SARM), MK-0773 in female participants with sarcopenia. J. Nutr. Health Aging 17, 533–543 (2013).
Golan, T. et al. LY2495655, an antimyostatin antibody, in pancreatic cancer: a randomized, phase 2 trial. J. Cachexia Sarcopenia Muscle 9, 871–879 (2018).
Rooks, D. et al. Bimagrumab vs optimized standard of care for treatment of sarcopenia in community-dwelling older adults: a randomized clinical trial. JAMA Netw. Open 3, e2020836 (2020).
Dao, T. et al. Sarcopenia and muscle aging: a brief overview. Endocrinol. Metab. 35, 716–732 (2020).
Ranjit, R., Van Remmen, H. & Ahn, B. Acylated ghrelin receptor agonist HM01 decreases lean body and muscle mass, but unacylated ghrelin protects against redox-dependent sarcopenia. Antioxidants 11, 2358 (2022).
Cheng, A. J., Ström, J., Hwee, D. T., Malik, F. I. & Westerblad, H. Fast skeletal muscle troponin activator CK-2066260 mitigates skeletal muscle weakness independently of the underlying cause. J. Cachexia Sarcopenia Muscle 11, 1747–1757 (2020).
Sabini, E., O’Mahony, A. & Caturegli, P. MyMD-1 improves health span and prolongs life span in old mice: a noninferiority study to rapamycin. J. Gerontol. A Biol. Sci. Med. Sci. 78, 227–235 (2023).
Chen, L. K. Crosstalk between bone and muscle for healthy aging. Aging Med. Healthc. 10, 51–52 (2019).
Florea, V., Bagno, L., Rieger, A. C. & Hare, J. M. Attenuation of frailty in older adults with mesenchymal stem cells. Mech. Ageing Dev. 181, 47–58 (2019).
Nissinen, T. A. et al. Muscle follistatin gene delivery increases muscle protein synthesis independent of periodical physical inactivity and fasting. FASEB J. 35, e21387 (2021).
Sciorati, C. et al. Pharmacological blockade of TNFα prevents sarcopenia and prolongs survival in aging mice. Aging 12, 23497–23508 (2020).
Oost, L. J., Kustermann, M., Armani, A., Blaauw, B. & Romanello, V. Fibroblast growth factor 21 controls mitophagy and muscle mass. J. Cachexia Sarcopenia Muscle 10, 630–642 (2019).
Reza, M. M. et al. Irisin is a pro-myogenic factor that induces skeletal muscle hypertrophy and rescues denervation-induced atrophy. Nat. Commun. 8, 1104 (2017).
Vinel, C. et al. The exerkine apelin reverses age-associated sarcopenia. Nat. Med. 24, 1360–1371 (2018).
Tung, H. H. et al. Efficacy of digital dance on brain imagery, cognition, and health: randomized controlled trial. J. Med. Internet Res. 26, e57694 (2024).
Makizako, H. et al. Effects of digital-based interventions on the outcomes of the eligibility criteria for sarcopenia in healthy older adults: a systematic review and meta-analysis. Ageing Res. Rev. 104, 102663 (2025).
Chan, K. O. W. et al. Effectiveness of telehealth in preventive care: a study protocol for a randomised controlled trial of tele-exercise programme involving older people with possible sarcopenia or at risk of fall. BMC Geriatr. 23, 845 (2023).
Donini, L. M. et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO Consensus Statement. Obes. Facts 15, 321–335 (2022).
Zhang, X. et al. Characterization of cellular senescence in aging skeletal muscle. Nat. Aging 2, 601–615 (2022).
Kedlian, V. R. et al. Human skeletal muscle aging atlas. Nat. Aging 4, 727–744 (2024).
Koliaki, C., Liatis, S., Dalamaga, M. & Kokkinos, A. Sarcopenic obesity: epidemiologic evidence, pathophysiology, and therapeutic perspectives. Curr. Obes. Rep. 8, 458–471 (2019).
Liu, C. et al. Deciphering the “obesity paradox” in the elderly: a systematic review and meta-analysis of sarcopenic obesity. Obes. Rev. 24, e13534 (2023).
Biltz, N. K. et al. Infiltration of intramuscular adipose tissue impairs skeletal muscle contraction. J. Physiol. 598, 2669–2683 (2020).
Tieland, M., Trouwborst, I. & Clark, B. C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 9, 3–19 (2018).
Yeung, S. S. Y., Kwok, T. & Woo, J. C-reactive protein and muscle-related measures over 14 years in Chinese community-dwelling older adults. Arch. Gerontol. Geriatr. 106, 104878 (2023).
Won, C. W., Kim, M. & Shin, H. E. From a solitary blood-derived biomarker to combined biomarkers of sarcopenia: experiences from the Korean Frailty and Aging Cohort Study. J. Gerontol. https://doi.org/10.1093/gerona/glae237 (2024).
Shin, H. E., Jang, J. Y., Jung, H., Won, C. W. & Kim, M. MicroRNAs as commonly expressed biomarkers for sarcopenia and frailty: a systematic review. Exp. Gerontol. 197, 112600 (2024).
Acknowledgements
We acknowledge the contributions of L. Kang (China), S. B. Kamaruzzaman (Malaysia) and S. Zhang (Japan) for their participation in consensus discussions and data provision. We also thank D. Neil, of Dr. Word Ltd, Taiwan, who provided editing and graphic design services, which were funded by the AWGS and the National Yang Ming Chiao Tung University, Taiwan. This research was funded by the National Science and Technology Council, the Interdisciplinary Research Center for Healthy Longevity of National Yang Ming Chiao Tung University from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan, Taiwan Association for Integrated Care, and Asian Association for Frailty and Sarcopenia.
Author information
Authors and Affiliations
Contributions
L.-K.C. wrote the first draft and was a major contributor in writing the manuscript. L.-K.C., J.W. and H.A. contributed to conception of the consensus update. L.-K.C. and F.-Y.H. performed systematic evidence review and prepared the figures/tables. L.-K.C., F.-Y.H. and H.A. revised subsequent drafts to address reviewer comments. All authors participated in consensus discussions, contributed to critical review of the manuscript for important intellectual content and approved the final version. All authors agree to be accountable for the accuracy and integrity of this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Marco Narici, who co-reviewed with Fabio Sarto; Alejandro Álvarez-Bustos; and Theresa Mau for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Table 1, Members of the Asian Working Group for Sarcopenia (AWGS); and Supplementary Table 2, Comparison of muscle assessment methods.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, LK., Hsiao, FY., Akishita, M. et al. A focus shift from sarcopenia to muscle health in the Asian Working Group for Sarcopenia 2025 Consensus Update. Nat Aging 5, 2164–2175 (2025). https://doi.org/10.1038/s43587-025-01004-y
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s43587-025-01004-y
This article is cited by
-
High-speed resistance training vs. low-speed resistance training on body composition and physical function in adults with sarcopenic obesity
European Review of Aging and Physical Activity (2026)