Abstract
Background
Shortages in mental healthcare lead to long periods of inadequate support for many patients. While digital interventions offer a scalable solution to this unmet clinical need, patient engagement remains a key challenge. Generative artificial intelligence (genAI) presents an opportunity to deliver highly engaging, personalized mental health treatment at scale.
Methods
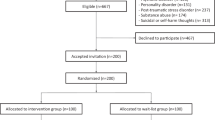
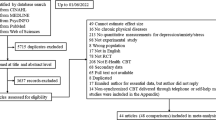
In a pre-registered (ClinicalTrials.gov: NCT06459128, 10 June 2024), parallel, 2-arm, unblinded, randomized controlled trial (N = 540), we evaluate whether a genAI-enabled cognitive behavioral therapy (CBT) app enhances engagement or symptom reduction compared with digital CBT workbooks. Eligible participants are adults residing in the United States with elevated self-reported symptoms of anxiety (GAD-7 ≥ 7) or depression (PHQ-9 ≥ 9), recruited online. After an online baseline assessment, participants are automatically randomly allocated (3:2) to receive either the genAI-enabled app or a digital workbook, both self-guided over six weeks. Primary outcomes are: 1) engagement frequency and duration, and 2) change in anxiety (GAD-7) and depression (PHQ-9) symptom severity. Secondary outcomes include adverse events and functional impairment. The study is unblinded to participants and researchers due to the nature of the digital interventions.
Results
A total of 540 participants are recruited and randomized to each group (intervention: n = 322, active control: n = 218). Nine participants from the control group are excluded from analysis due to protocol deviations. Over six weeks, the genAI solution (n = 322) increases engagement frequency (2.4×) and duration (3.8×) compared to digital workbooks (n = 209), with moderate to large effect sizes. We observe comparable outcomes for anxiety (GAD-7) and depression (PHQ-9) with no differences in adverse events. Moreover, exploratory analyses suggest that participants who choose to engage with clinical personalization features powered by genAI experience stronger anxiety symptom reduction and improved overall wellbeing.
Conclusions
Our findings suggest that, in self-directed usage, tailored genAI-enabled therapy safely enhances user engagement above and beyond static materials, without showing an overall enhancement in anxiety or depression symptom reduction.
Plain language summary
Access to mental health care is often limited, leaving many people without support while they wait for treatment to start or between therapy sessions. Self-help tools can help fill these gaps but users often struggle to stay engaged. Generative artificial intelligence (AI), a technology that can generate new content like text or images, could make these tools feel more personal and interactive. In this six-week randomized-controlled trial with 540 adults experiencing anxiety or depression symptoms, we compared an AI-enabled cognitive-behavioral therapy (CBT) app with digital workbooks. People using the AI app engaged more often and for longer, while safety and symptom reduction were similar across groups. Those who used the app’s more personalized features showed the greatest improvements, suggesting AI-powered therapy tools could safely help people stay engaged between therapy sessions.
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in Supplementary Data 3.
References
Peipert, A., Krendl, A. C. & Lorenzo-Luaces, L. Waiting lists for psychotherapy and provider attitudes toward low-intensity treatments as potential interventions: survey study. JMIR Form Res 6, e39787 (2022).
Punton, G., Dodd, A. L. & McNeill, A. ‘You’re on the waiting list’: An interpretive phenomenological analysis of young adults’ experiences of waiting lists within mental health services in the UK. PloS One 17, e0265542 (2022).
Anderson, K. K. et al. Access and health system impact of an early intervention treatment program for emerging adults with mood and anxiety disorders. Can. J. Psychiatry Rev. Can. Psychiatr. 64, 492–500 (2019).
Mausbach, B. T., Moore, R., Roesch, S., Cardenas, V. & Patterson, T. L. The relationship between homework compliance and therapy outcomes: an updated meta-analysis. Cogn. Ther. Res 34, 429–438 (2010).
Prasko, J. et al. Homework in cognitive behavioral supervision: theoretical background and clinical application. Psychol. Res. Behav. Manag. 15, 3809–3824 (2022).
Tran, Q. D. Going beyond waitlists in mental healthcare. Community Ment. Health J 60, 629–634 (2024).
Karyotaki, E., Furukawa, T. A., Efthimiou, O., Riper, H. & Cuijpers, P. Guided or self-guided internet-based cognitive–behavioural therapy (iCBT) for depression? Study protocol of an individual participant data network meta-analysis. BMJ Open 9, e026820 (2019).
Titov, N. et al. Treating anxiety and depression in older adults: randomised controlled trial comparing guided V. self-guided internet-delivered cognitive–behavioural therapy. BJPsych Open 2, 50–58 (2016).
Oewel, B., Areán, P. A. & Agapie, E. Approaches to Tailoring Between-Session Mental Health Therapy Activities.In Proc. 2024 CHI Conference on Human Factors in Computing Systems, 696 (2024).
Torous, J., Nicholas, J., Larsen, M. E., Firth, J. & Christensen, H. Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. Evid. Based Ment. Health 21, 116–119 (2018).
Malik, A. et al. Client perspectives on perceived barriers to homework adherence in psychotherapy: An exploratory study from India. Asian J. Psychiatry 75, 103206 (2022).
Gilbody, S. et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 351, h5627 (2015).
Kuhail, M. A., Alturki, N., Thomas, J., Alkhalifa, A. K. & Alshardan, A. Human-Human vs Human-AI Therapy: An Empirical Study. Int. J. Human–Computer Interact. 1–12 (2024) https://doi.org/10.1080/10447318.2024.2385001.
Meyer, S. & Elsweiler, D. Llm-Based Conversational Agents for Behaviour Change Support: A Randomized Controlled Trial Examining Efficacy, Safety, and the Role of User Behaviour. SSRN Scholarly Paper at https://papers.ssrn.com/abstract=4917769 (2024).
Rollwage, M. et al. Conversational AI facilitates mental health assessments and is associated with improved recovery rates. BMJ Innov. 10, (2024).
Rollwage, M. et al. Using conversational AI to facilitate mental health assessments and improve clinical efficiency within psychotherapy services: real-world observational study. JMIR AI 2, e44358 (2023).
Cabrera, J., Loyola, M. S., Magaña, I. & Rojas, R. Ethical Dilemmas, Mental Health, Artificial Intelligence, and LLM-Based Chatbots. in Bioinformatics and Biomedical Engineering (eds Rojas, I., Valenzuela, O., Rojas Ruiz, F., Herrera, L. J. & Ortuño, F.) 313–326 (Springer Nature Switzerland, Cham, 2023). https://doi.org/10.1007/978-3-031-34960-7_22.
Volkmer, S., Meyer-Lindenberg, A. & Schwarz, E. Large language models in psychiatry: Opportunities and challenges. Psychiatry Res 339, 116026 (2024).
Freyer, O., Wiest, I. C., Kather, J. N. & Gilbert, S. A future role for health applications of large language models depends on regulators enforcing safety standards. Lancet Digit. Health 6, e662–e672 (2024).
Rollwage, M. et al. The Limbic Layer: Transforming Large Language Models (LLMs) into Clinical Mental Health Experts. Preprint at https://doi.org/10.31234/osf.io/9d7tp (2024).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097 (2006).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med 16, 606–613 (2001).
Anwyl-Irvine, A. L., Massonnié, J., Flitton, A., Kirkham, N.Z. & Evershed, J. K. Gorilla in our midst: An online behavioral experiment builder. Behav Res. 52, 388–407 (2020).
Mundt, J. C., Marks, I. M., Shear, M. K. & Greist, J. H. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br. J. Psychiatry J. Ment. Sci 180, 461–464 (2002).
Natale, V., Fabbri, M., Tonetti, L. & Martoni, M. Psychometric goodness of the Mini Sleep Questionnaire. Psychiatry Clin. Neurosci. 68, 568–573 (2014).
Habicht, J. et al. Generative AI–enabled therapy support tool for improved clinical outcomes and patient engagement in group therapy: real-world observational study. J. Med. Internet Res. 27, e60435 (2025).
Limpanopparat, S., Gibson, E. & Harris, D. A. User engagement, attitudes, and the effectiveness of chatbots as a mental health intervention: A systematic review. Comput. Hum. Behav. Artif. Hum. 2, 100081 (2024).
Perski, O., Crane, D., Beard, E. & Brown, J. Does the addition of a supportive chatbot promote user engagement with a smoking cessation app? An experimental study. Digit. Health 5, 2055207619880676 (2019).
Dosovitsky, G., Pineda, B. S., Jacobson, N. C., Chang, C. & Bunge, E. L. Artificial intelligence chatbot for depression: descriptive study of usage. JMIR Form. Res 4, e17065 (2020).
Ng, M. M., Firth, J., Minen, M. & Torous, J. User engagement in mental health apps: a review of measurement. Reporting, and Validity. Psychiatr. Serv. Wash. DC 70, 538–544 (2019).
Karkosz, S., Szymański, R., Sanna, K. & Michałowski, J. Effectiveness of a Web-based and Mobile Therapy Chatbot on Anxiety and Depressive Symptoms in Subclinical Young Adults: Randomized Controlled Trial. JMIR Form. Res 8, e47960 (2024).
Richards, D. et al. A pragmatic randomized waitlist-controlled effectiveness and cost-effectiveness trial of digital interventions for depression and anxiety. NPJ Digit. Med. 3, 85 (2020).
Cheung, K. et al. Evaluation of a recommender app for apps for the treatment of depression and anxiety: an analysis of longitudinal user engagement. J. Am. Med. Inform. Assoc. JAMIA 25, 955–962 (2018).
Xu, J. et al. A scalable mental health intervention for depressive symptoms: evidence from a randomized controlled trial and large-scale real-world studies. NPJ Digit. Med. 8, 491 (2025).
Bhatt, S. Digital Mental Health: Role of Artificial Intelligence in Psychotherapy. Ann. Neurosci. 09727531231221612 (2024) https://doi.org/10.1177/09727531231221612.
Moshe, I. et al. Digital interventions for the treatment of depression: A meta-analytic review. Psychol. Bull. 147, 749–786 (2021).
Linardon, J., Cuijpers, P., Carlbring, P., Messer, M. & Fuller-Tyszkiewicz, M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry 18, 325–336 (2019).
Jonassaint, C. R. et al. Digital Cognitive Behavioral Therapy vs Education for Pain in Adults with Sickle Cell Disease. Blood Adv. bloodadvances. 2024013861 (2024) https://doi.org/10.1182/bloodadvances.2024013861.
Fitzsimmons-Craft, E. E. et al. Effects of Chatbot Components to Facilitate Mental Health Services Use in Individuals With Eating Disorders Following Online Screening: An Optimization Randomized Controlled Trial. Int. J. Eat. Disord. 57, 2204–2216 (2024).
Kim, Y., Kang, Y., Kim, B., Kim, J. & Kim, G. H. Exploring the role of engagement and adherence in chatbot-based cognitive training for older adults: memory function and mental health outcomes. Behav. Inf. Technol. 44, 2405–2417 (2025).
Acknowledgements
This research was funded by Limbic Limited. We would like to thank the research team at Limbic, particularly Dr Sashank Pisupati, George Prichard, Dr Keno Juchems, and Dr Annamaria Balogh, for their significant contributions to the development of the clinical AI used in this study. We also thank the wider Limbic team for their support throughout this work.
Author information
Authors and Affiliations
Contributions
J.H., M.R., R.H., L.D., J.M. and T.U.H. conceived the study idea J.H., J.M., M.R. and T.U.H. designed the study. J.M. and J.H. implemented the data collection. J.M. analysed the data and created manuscript figures. J.M., L.D., T.U.H. and M.R. wrote and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.M., J.H., L.D., R.H. and M.R. are employed by Limbic Limited and hold shares in the company. T.U.H. is working as a paid consultant for Limbic Limited and holds shares in the company.
Peer review
Peer review information
Communications Medicine thanks Nickolai Titov, Julia Ive and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McFadyen, J., Habicht, J., Dina, LM. et al. Increasing engagement with cognitive-behavioral therapy (CBT) using generative AI: a randomized controlled trial (RCT). Commun Med (2026). https://doi.org/10.1038/s43856-025-01321-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-025-01321-8