Abstract
Background
Emotional distress (ED) has been demonstrated to compromise immune responses against tumors; however, few clinical studies have explored its influence on the efficacy of immune checkpoint inhibitors (ICIs) in cancer patients, especially those with gastroesophageal cancer (GEC). Additionally, reliable biomarkers for predicting the response to immunotherapy remain elusive. This study was aimed at investigating whether ED affects the outcomes of immunotherapy in advanced GEC patients and identifying potential biomarkers predictive of immunotherapy efficacy.
Methods
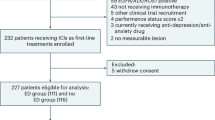
This prospective observational cohort study enrolled 84 patients with advanced, treatment-naïve, and inoperable GEC. ED was evaluated at baseline using the Patient Health Questionnaire-9 and the Generalized Anxiety Disorder 7-item Scale. The primary endpoint was Progression-Free Survival (PFS), while the secondary endpoint was Disease Control Rate (DCR).
Results
Patients with baseline ED exhibit significantly shorter median PFS (7.8 months vs. 14.0 months, HR = 2.59, 95% CI: 1.35-4.97, P = 0.004) and a lower DCR (39.5% vs. 68.3%, OR = 3.21, 95% CI: 1.29–7.98, P = 0.012) compared to those without ED. Exploratory analyses further demonstrate that both pre- and post-treatment peripheral inflammatory markers (PIMs) are independently and jointly associated with survival outcomes in combination with ED.
Conclusions
This prospective study demonstrates that ED and elevated PIMs significantly impair ICI efficacy in advanced GEC. The synergistic interaction between ED and PIMs suggests underlying psycho-inflammatory mechanisms affecting treatment outcomes. These findings establish the clinical importance of integrating routine psychological assessment and PIMs monitoring in cancer patients receiving immunotherapy.
Plain language summary
This study explored how stress and inflammation affect treatment outcomes in patients with advanced stomach or esophageal cancer receiving a type of treatment called immunotherapy. We aimed to understand why some patients respond better to these drugs and whether emotional health plays a role. We followed 84 patients, using questionnaires and blood tests to measure stress and inflammation before treatment. Patients with high stress before treatment saw faster cancer progression (7.8 vs. 14 months) and poorer responses to immunotherapy. High inflammation levels further worsened outcomes, especially when combined with stress. These results highlight that reducing stress and monitoring inflammation before treatment could help doctors tailor immunotherapy plans, potentially improving survival and quality of life for cancer patients.
Similar content being viewed by others
Data availability
The source data underlying the figures are provided as Supplementary Data 2 alongside this manuscript. Specifically, the source data for Fig. 3 are available in “PFS by pretreatment ED”, for Fig. 4 in “PFS subgroup analysis” and for Fig. 5 in “PFS by each significant biomark”. Additional supporting data not included in Supplementary Data 2, as well as the complete datasets generated and/or analysed during this study, are not publicly available due to patient confidentiality requirements and institutional data protection policies. Deidentified individual patient-level clinical data are available under restricted access upon reasonable request. All requests for datasets should be directed to the corresponding author, CH (chd1975ay@126.com) and will be responded to within 2 weeks. Requests will be reviewed to determine whether the request is subject to any intellectual property or confidentiality obligations. Patient-related data requires the requesting researcher to sign a data access agreement, and data will be shared in aggregate form if there is no reasonable likelihood of participant reidentification.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. (2024).
Shah, M. A. et al. Immunotherapy and targeted therapy for advanced gastroesophageal cancer: ASCO guideline. J. Clin. Oncol. 41, 1470–1491 (2023).
Janjigian, Y. Y. et al. Nivolumab (Nivo) plus chemotherapy (chemo) or ipilimumab (Ipi) vs chemo as first-line (1l) treatment for advanced gastric cancer/gastroesophageal junction cancer/esophageal adenocarcinoma (Gc/Gejc/Eac): checkmate 649 study. Annals Oncol. 32, S1329–S1330 (2021).
Shitara, K. et al. Pembrolizumab versus paclitaxel for previously treated, advanced gastric or gastro-oesophageal junction cancer (KEYNOTE-061): a randomised, open-label, controlled, phase 3 trial. Lancet 392, 123–133 (2018).
Ken, K. et al. First-line pembrolizumab plus chemotherapy for advanced/metastatic esophageal cancer: 1-year extended follow-up in the Japanese subgroup of the phase 3 KEYNOTE-590 study. Esophagus (2024).
Wang, P. et al. Prognostic and predictive factors in advanced upper gastrointestinal cancer treated with immune checkpoint inhibitors: a systematic review and meta-analysis of the current evidence. BMC Cancer 24, 1249 (2024).
Wanting, H., Yaqin, Z. & Hong, Z. Predictive Biomarkers for Immunotherapy in gastric cancer: current status and emerging prospects. Int. J. Mol. Sci. (2023).
Mino-Kenudson, M. et al. Predictive biomarkers for immunotherapy in lung cancer: perspective from the International Association for the Study of Lung Cancer Pathology Committee. J. Thorac. Oncol. 17, 1335–1354 (2022).
Yang, M. et al. Psychological intervention to treat distress: an emerging frontier in cancer prevention and therapy. Biochim Biophys. Acta Rev. Cancer 1877, 188665 (2022).
Hellstadius, Y. et al. Aspects of emotional functioning following oesophageal cancer surgery in a population-based cohort study. Psychooncology 24, 47–53 (2015).
Kim, G. M. et al. Prevalence and prognostic implications of psychological distress in patients with gastric cancer. BMC Cancer 17, 283 (2017).
Xin Shelley, W. et al. Patient-reported symptom burden and functioning in patients with advanced esophageal, gastroesophageal junction (GEJ), and gastric cancer undergoing chemotherapy. J. Clin. Oncol. 39, 183 (2021).
Ma, Y. & Kroemer, G. The cancer-immune dialogue in the context of stress. Nat. Rev. Immunol. 24, 264–281 (2023).
Morales-López, C. et al. Abstract 6120: The effect of chronic stress in T-cell population and function in ovarian cancer. Cancer Res. 82, 6120–6120 (2022).
Ciliberti, M. G. et al. Peripheral blood mononuclear cell proliferation and cytokine production in sheep as affected by cortisol level and duration of stress. J. Dairy Sci. 100, 750–756 (2017).
Yin, W. et al. Unique brain endothelial profiles activated by social stress promote cell adhesion, prostaglandin E2 signaling, hypothalamic-pituitary-adrenal axis modulation, and anxiety. Neuropsychopharmacology 47, 2271–2282 (2022).
Cui, B. et al. Stress-induced epinephrine enhances lactate dehydrogenase A and promotes breast cancer stem-like cells. J. Clin. Investig. 129, 1030–1046 (2019).
Sastry, K. S. et al. Epinephrine protects cancer cells from apoptosis via activation of cAMP-dependent protein kinase and BAD phosphorylation. J. Biol. Chem. 282, 14094–14100 (2007).
Sullivan, D. R. et al. Longitudinal changes in depression symptoms and survival among patients with lung cancer: a National Cohort Assessment. J. Clin. Oncol. 34, 3984–3991 (2016).
Wang, Y. H. et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol. Psychiatry 25, 1487–1499 (2020).
Eckerling, A., Ricon-Becker, I., Sorski, L., Sandbank, E. & Ben-Eliyahu, S. Stress and cancer: mechanisms, significance and future directions. Nat. Rev. Cancer 21, 767–785 (2021).
Yi, G. et al. Combined systemic immune-inflammatory index and prognostic nutritional index predicts the efficacy and prognosis of ES-SCLC patients receiving PD-L1 inhibitors combined with first-line chemotherapy. Front. Oncol. 14, 1485849 (2024).
Qilin, H. et al. Peripheral blood inflammatory biomarkers dynamics reflect treatment response and predict prognosis in non-small cell lung cancer patients with neoadjuvant immunotherapy. Cancer Sci. 114, 4484-4498 (2023).
Maodong, F. Prognostic value of peripheral blood neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, pan-immune-inflammation value and systemic immune-inflammation index for the efficacy of immunotherapy in patients with advanced gastric cancer. Immunotherapy 16, 551–563 (2024).
Liangshan, D. et al. Prognostic value of inflammatory markers and clinical features for survival in advanced or metastatic esophageal squamous cell carcinoma patients receiving anti-programmed death 1 treatment. Front. Oncol. (2023).
Beurel, E., Toups, M. & Nemeroff, C. B. The bidirectional relationship of depression and inflammation: double trouble. Neuron 107, 234–256 (2020).
Kiecolt-Glaser, J. K., Derry, H. M. & Fagundes, C. P. Inflammation: depression fans the flames and feasts on the heat. Am. J. Psychiatry 172, 1075–1091 (2015).
Marazziti, D. et al. Neutrophil/lymphocyte, platelet/lymphocyte, and monocyte/lymphocyte ratios in mood disorders. Curr. Med. Chem. 29, 5758–5781 (2022).
Nai-Fei, C. et al. Serum albumin as a prognostic predictor reflecting host immunity in patients with non–small cell lung cancer. J. Nutr. Oncol. (2023).
Ke, Z. et al. Potential metabolic monitoring indicators of suicide attempts in first episode and drug naive young patients with major depressive disorder: a cross-sectional study. BMC Psychiatry (2020).
Bisgaard, T. H., Allin, K. H., Keefer, L., Ananthakrishnan, A. N. & Jess, T. Depression and anxiety in inflammatory bowel disease: epidemiology, mechanisms and treatment. Nat. Rev. Gastroenterol. Hepatol. 19, 717–726 (2022).
Deshields, T. L. et al. Addressing distress management challenges: recommendations from the consensus panel of the American Psychosocial Oncology Society and the Association of Oncology Social Work. CA Cancer J. Clin. 71, 407–436 (2021).
Andersen, B. L. et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J. Clin. Oncol. 32, 1605–1619 (2014).
Levis, B., Benedetti, A., Thombs, B. D. & Collaboration, D. E. S. D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ 365, l1476 (2019).
Yang, Y. et al. Network connectivity between fear of cancer recurrence, anxiety, and depression in breast cancer patients. J. Affect. Disord. 309, 358–367 (2022).
Grapp, M., Terhoeven, V., Nikendei, C., Friederich, H. C. & Maatouk, I. Screening for depression in cancer patients using the PHQ-9: the accuracy of somatic compared to non-somatic items. J. Affect Disord. 254, 74–81 (2019).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097 (2006).
Esser, P. et al. The Generalized Anxiety Disorder Screener (GAD-7) and the anxiety module of the Hospital and Depression Scale (HADS-A) as screening tools for generalized anxiety disorder among cancer patients. Psychooncology 27, 1509–1516 (2018).
Kroenke, K. et al. Patient health questionnaire anxiety and depression scale: initial validation in three clinical trials. Psychosom. Med 78, 716–727 (2016).
Zeng, Y. et al. Association between pretreatment emotional distress and immune checkpoint inhibitor response in non-small-cell lung cancer. Nat. Med. 30, 1680–1688 (2024).
Tang, Y. MOVER confidence intervals for a difference or ratio effect parameter under stratified sampling. Stat. Med. 41, 194–207 (2022).
Hosmer, D. W. & Lemeshow, S. Confidence interval estimation of interaction. Epidemiology 3, 452–456 (1992).
Yu, S. et al. Depression decreases immunity and PD-L1 inhibitor efficacy via the hypothalamic-pituitary-adrenal (HPA) axis in triple-negative breast cancer. Biochim. Biophys. Acta Mol. Basis Dis. 1871, 167581 (2024).
Bucsek, M. J. et al. β-adrenergic signaling in mice housed at standard temperatures suppresses an effector phenotype in CD8(+) T cells and undermines checkpoint inhibitor therapy. Cancer Res. 77, 5639–5651 (2017).
Marwah, R. et al. Social media insights into disease burden in patients and caregivers of myelodysplastic syndrome: subcohort analysis of high-risk patients. J. Med. Internet Res. 27, e65460 (2025).
Ding, X. et al. The association of adverse reactions and depression in cervical cancer patients treated with radiotherapy and/or chemotherapy: moderated mediation models. Front. Psychol. 14, 1207265 (2023).
Huai, Q. et al. Peripheral blood inflammatory biomarkers dynamics reflect treatment response and predict prognosis in non-small cell lung cancer patients with neoadjuvant immunotherapy. Cancer Sci. 114, 4484–4498 (2023).
Fu, M., Zhang, X., Shen, F., Ma, J. & Li, Z. Prognostic value of peripheral blood neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, pan-immune-inflammation value and systemic immune-inflammation index for the efficacy of immunotherapy in patients with advanced gastric cancer. Immunotherapy (2024).
Fu, M., Li, Z., Ma, J., Shen, F. & Zhang, X. Study on the predictive value of pretreatment peripheral blood inflammatory markers regarding immunotherapy in patients with inoperable advanced or locally advanced oesophageal squamous cell carcinoma. Scand. J. Gastroenterol. 59, 722–729 (2024).
Kim, R. et al. Immune factors associated with the pathological and therapeutic effects of preoperative chemotherapy in patients with breast cancer. Transl. Oncol. 14, 100927 (2021).
Minici, R. et al. Prognostic role of neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-C reactive protein ratio (LCR) in patients with hepatocellular carcinoma (HCC) undergoing Chemoembolizations (TACE) of the liver: The Unexplored Corner Linking Tumor Microenvironment, Biomarkers and Interventional Radiology. Cancers 15 (2022).
Reichman, H. et al. Activated Eosinophils Exert Antitumorigenic Activities in Colorectal Cancer. Cancer Immunol. Res 7, 388–400 (2019).
Carretero, R. et al. Eosinophils orchestrate cancer rejection by normalizing tumor vessels and enhancing infiltration of CD8+ T cells. Nat. Immunol. 16, 609–617 (2015).
Kao, C.-C., et al. 261. The prognostic impact of pre-operative nutritional indicators of the patients with esophageal cancer. Diseases Esophagus 36(2023).
Cheng, H., Lu, D., Yin, C. & Fang, Y. Prognostic value of peripheral blood fibrinogen-to-albumin ratio and neutrophil-to-lymphocyte ratio in patients with locally advanced or metastatic pancreatic cancer. Am. J. Transl. Res. 16, 7165–7175 (2024).
Duivis, H. E., Vogelzangs, N., Kupper, N., de Jonge, P. & Penninx, B. W. Differential association of somatic and cognitive symptoms of depression and anxiety with inflammation: findings from the Netherlands Study of Depression and Anxiety (NESDA). Psychoneuroendocrinology 38, 1573–1585 (2013).
Mehta, N. D. et al. Inflammation, amygdala-ventromedial prefrontal functional connectivity and symptoms of anxiety and PTSD in African American women recruited from an inner-city hospital: Preliminary results. Brain Behav., Immun. 105, 122–130 (2022).
Cox, C. Fieller’s theorem, the likelihood and the delta method. Biometrics 46, 709–718 (1990).
Rodin, G. et al. Managing cancer and living meaningfully (CALM): a randomized controlled trial of a psychological intervention for patients with advanced cancer. J. Clin. Oncol. 36, 2422–2432 (2018).
Huang, R. et al. Effect of behavioral activation on stigma and quality of life in patients with advanced esophageal and gastric cancer: a randomized controlled trial. Psycho Oncol. 33 (2024).
Wang, K. et al. Long-term anti-inflammatory diet in relation to improved breast cancer prognosis: a prospective cohort study. NPJ Breast Cancer 6, 36 (2020).
Dominik, N. et al. Smoking Aggravates Inflammation, Fibrogenesis, Angiogenesis and Cancer Risk in Patients With Cirrhosis. Liver Int 45, e70314 (2025).
Cao, G. et al. Physical activity reduces cancer risk by lowering C-reactive protein: a dual-cohort study in the Chinese population. Chin. Sci. Bullet. (2025).
Liu, X. et al. Loratidine is associated with improved prognosis and exerts antineoplastic effects via apoptotic and pyroptotic crosstalk in lung cancer. J. Exp. Clin. Cancer Res 43, 5 (2024).
Jang, J. Y., Jeong, S. Y. & Kim, S.-T. Tumor mutational burden as a potential predictive marker for the efficacy of immunotherapy in advanced gastric cancer. J. Clin. Oncol. (2023).
Acknowledgements
We would like to thank all the patients who participated in the study. This work was supported by the National Natural Science Foundation of China (grant no. 82573690 to H.D. Cheng), the Health Research Project of Anhui Province (grant no. AHWJ2023A20149 to L. Cheng), and the 2024 Take-Off Project of Shenzhen Hospital of Southern Medical University (grant no. 23H3ATF01 to H.D. Cheng).
Author information
Authors and Affiliations
Contributions
H.R., N.G. and L.A. planned the study. N.G., L.A., G.H., C.J., J.Y., L.L. and H.Z. took part in the process of data collection. H.R. carried out analysis, interpreted results and drafted the manuscript. D.X., L.M., C.L., Y.S., H.Z., C.H. and Z.M. revised it for critically important intellectual content. All authors gave final approval of the version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Yu Jiang and Konstantinos Kamposioras for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, R., Nie, G., Li, A. et al. Pretreatment emotional distress and peripheral biomarkers predict immune checkpoint inhibitor response in people with advanced inoperable gastroesophageal cancer. Commun Med (2026). https://doi.org/10.1038/s43856-025-01358-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-025-01358-9