Abstract
Background
The relative efficacies of nalmefene versus naltrexone for alcohol use disorder is the subject of intense and ongoing debate. The two pan-opioid receptor ligands differ primarily in actions at the kappa opioid receptor, where naltrexone acts as an antagonist and nalmefene acts as a partial agonist. Parallel clinical trials for nalmefene or naltrexone have produced widely disparate outcomes and a marked lack of consensus regarding which of the compounds should be used for the treatment of alcohol use disorder.
Methods
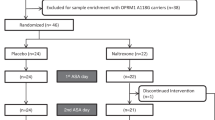
Here we leveraged a mouse model (n = 56 male C57BL/6 J) to directly compare the efficacy of nalmefene and naltrexone within-subject. After acquiring operant responding for ethanol, each subject underwent four treatment block conditions: nalmefene (0.1 mg/kg i.p.), naltrexone (1.0 mg/kg i.p.), the selective kappa opioid receptor agonist U50,488 (1.0 mg/kg i.p.) and placebo (saline 10 ml/kg i.p.). Each treatment block consisted of an ethanol self-administration session followed by two subsequent sessions of punished (quinine adulterated) ethanol self-administration sessions with treatment given 30 min prior to each session.
Results
We show that nalmefene and naltrexone have similar efficacy in reducing ethanol consumption, whereas U50,488 increases ethanol consumption. Despite similar effects in aggregate analyses, nalmefene- and naltrexone-induced reductions in drinking are driven by fully separate subpopulations which do not show any beneficial response to the non-preferred compound and display markedly different behavioral phenotypes prior to treatment. A predictive model based on circulating biogenic amines allows for high accuracy classification of nalmefene- versus naltrexone-responders.
Conclusion
Together, these results provide a roadmap for improving alcohol use disorder treatment outcomes via precision application of existing compounds.
Plain Language Summary
Nalmefene and naltrexone are two drug treatments for alcohol use disorder, but disagreement exists on which is more effective. Despite ongoing controversy, treatment outcomes have only been compared across separate studies, rather than head-to-head. Using a preclinical model where mice learn to press a lever for alcohol, we treated each mouse with nalmefene, naltrexone, and placebo control. While both drugs equally reduced alcohol consumption on average, individual-level analysis revealed two distinct subpopulations: one responding to nalmefene but not naltrexone, and vice versa. Using machine learning on a single blood sample, we could predict which treatment would be more effective for each individual. This work suggests treatment outcomes for alcohol use disorder could be improved by using predictive models to deliver the right treatment to the right person at the right time.
Similar content being viewed by others
References
Litten, R. Z. et al. Heterogeneity of alcohol use disorder: understanding mechanisms to advance personalized treatment. Alcohol Clin. Exp. Res. 39, 579–584 (2015).
American Psychiatric Association. American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (American Psychiatric Association, 2013).
Kiefer, F. et al. Long-term effects of pharmacotherapy on relapse prevention in alcohol dependence. Acta Neuropsychiatr. 16, 233–238 (2004).
Hunt, W. A., Barnett, L. W. & Branch, L. G. Relapse rates in addiction programs. J. Clin. Psychol. 27, 455–456 (1971).
Armor, D. J., Polich, J. M. & Stambul, H. B. Alcoholism and Treatment (Rand, 1976).
Barrick, C. & Connors, G. J. Relapse prevention and maintaining abstinence in older adults with alcohol-use disorders. Drugs Aging 19, 583–594 (2002).
Ashenhurst, J. R., Bujarski, S. & Ray, L. A. Delta and kappa opioid receptor polymorphisms influence the effects of naltrexone on subjective responses to alcohol. Pharm. Biochem. Behav. 103, 253–259 (2012).
Anton, R. F. et al. An evaluation of μ-opioid receptor (OPRM1) as a predictor of naltrexone response in the treatment of alcohol dependence: results from the combined pharmacotherapies and behavioral interventions for alcohol dependence (COMBINE) study. Arch. Gen. Psychiatry 65, 135–144 (2008).
Hinton, D. J. et al. Metabolomics biomarkers to predict acamprosate treatment response in alcohol-dependent subjects. Sci. Rep. 7, 2496 (2017).
Witkiewitz, K., Roos, C. R., Mann, K. & Kranzler, H. R. Advancing precision medicine for alcohol use disorder: replication and extension of reward drinking as a predictor of naltrexone response. Alcohol. Clin. Exp. Res. 43, 2395–2405 (2019).
Roos, C. R., Mann, K. & Witkiewitz, K. Reward and relief dimensions of temptation to drink: construct validity and role in predicting differential benefit from acamprosate and naltrexone. Addiction Biol. 22, 1528–1539 (2017).
Mann, K. et al. Nalmefene for the management of alcohol dependence: review on its pharmacology, mechanism of action and meta-analysis on its clinical efficacy. Eur. Neuropsychopharmacol. 26, 1941–1949 (2016).
Jonas, D. E. et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA 311, 1889–1900 (2014).
Selincro: Summary of Product Characteristics (Annex 1) (EMA, 2013).
Nalmefene for Reducing Alcohol Consumption in People with Alcohol Dependence, Technology Appraisal 325 (NICE, 2014).
Fitzgerald, N. et al. Weak evidence on nalmefene creates dilemmas for clinicians and poses questions for regulators and researchers. Addiction 111, 1477–1487 (2016).
van den Brink, W. et al. Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies. Alcohol Alcohol. 48, 570–578 (2013).
Spence, D. Bad medicine: nalmefene in alcohol misuse. BMJ 348, g1531 (2014).
Naudet, F., Fitzgerald, N. & Braillon, A. Nalmefene for alcohol dependence: a NICE decision. Lancet Psychiatry 3, 1104–1105 (2016).
Green, M., Veltri, C. A. & Grundmann, O. Nalmefene hydrochloride: potential implications for treating alcohol and opioid use disorder. Subst. Abus. Rehabilit. 15, 43–57 (2024).
Braillon, A.& Granger, B. Nalmefene and alcohol dependence: a new approach or the same old unacceptable marketing? SAR 75, https://doi.org/10.2147/SAR.S86007 (2015).
Drobes, D. J., Anton, R. F., Thomas, S. E. & Voronin, K. Effects of naltrexone and nalmefene on subjective response to alcohol among non-treatment-seeking alcoholics and social drinkers. Alcohol Clin. Exp. Res. 28, 1362–1370 (2004).
Drobes, D. J., Anton, R. F., Thomas, S. E. & Voronin, K. A clinical laboratory paradigm for evaluating medication effects on alcohol consumption: naltrexone and nalmefene. Neuropsychopharmacology 28, 755–764 (2003).
Palpacuer, C. et al. Pharmacologically controlled drinking in the treatment of alcohol dependence or alcohol use disorders: a systematic review with direct and network meta-analyses on nalmefene, naltrexone, acamprosate, baclofen and topiramate. Addiction 113, 220–237 (2018).
Raynor, K. et al. Pharmacological characterization of the cloned kappa-, delta-, and mu-opioid receptors. Mol. Pharm. 45, 330–334 (1994).
Kelly, E. et al. The opioid receptor pharmacology of GSK1521498 compared to other ligands with differential effects on compulsive reward-related behaviours. Psychopharmacology 232, 305–314 (2015).
Connor, M. & Traynor, J. Constitutively active μ-opioid receptors. Methods Enzymol. 484, 445–469 (2010).
Wang, D., Sun, X. & Sadee, W. Different effects of opioid antagonists on mu-, delta-, and kappa-opioid receptors with and without agonist pretreatment. J. Pharm. Exp. Ther. 321, 544–552 (2007).
Barnett, M. E., Knapp, B. I. & Bidlack, J. M. Unique pharmacological properties of the kappa opioid receptor signaling through Gαz as shown with bioluminescence resonance energy tranfer. Mol. Pharm. 98, 462–474 (2020).
Bart, G. et al. Nalmefene induced elevation in serum prolactin in normal human volunteers: partial kappa opioid agonist activity. Neuropsychopharmacology 30, 2254–2262 (2005).
Butelman, E. R., Harris, T. J. & Kreek, M. J. Apparent efficacy of κ-opioid receptor ligands on serum prolactin levels in rhesus monkeys. Eur. J. Pharm. 383, 305–309 (1999).
Gual, A., He, Y., Torup, L., van den Brink, W., Mann, K. & ESENSE 2 Study Group A randomised, double-blind, placebo-controlled, efficacy study of nalmefene, as-needed use, in patients with alcohol dependence. Eur. Neuropsychopharmacol. 23, 1432–1442 (2013).
Aubin, H. J. et al. Clinical relevance of as-needed treatment with nalmefene in alcohol-dependent patients. Eur. Addict. Res. 21, 160–168 (2015).
Nieto, S. J., Grodin, E. N. & Ray, L. A. On the path toward personalized medicine: implications of pharmacogenetic studies of alcohol use disorder medications. Expert Rev. Precis Med. Drug Dev. 5, 43–54 (2020).
George, O. & Koob, G. F. Individual differences in the neuropsychopathology of addiction. Dialogues Clin. Neurosci. 19, 217–229 (2017).
Litten, R. Z. et al. Medications development to treat alcohol dependence: a vision for the next decade. Addict. Biol. 17, 513–527 (2012).
Ray, L. A. et al. The future of translational research on alcohol use disorder. Addict. Biol. 26, e12903 (2021).
van der Stel, J. Precision in addiction care: does it make a difference?. Yale J. Biol. Med. 88, 415–422 (2015).
FDA. FDA Approves Prescription Nasal Spray to Reverse Opioid Overdose. https://www.fda.gov/news-events/press-announcements/fda-approves-prescription-nasal-spray-reverse-opioid-overdose (2023).
Fortinguerra, F., Pierantozzi, A. & Trotta, F. The use of medications approved for alcohol use disorders in Italy. Front. Public Health 11, 1110435 (2023).
Keenan, K. P. et al. The effects of diet, ad libitum overfeeding, and moderate dietary restriction on the rodent bioassay: the uncontrolled variable in safety assessment. Toxicol. Pathol. 24, 757–768 (1996).
National Research Council (US) Subcommittee on Laboratory Animal Nutrition. Nutrient Requirements of the Mouse (National Academies Press (US), 1995).
Laman-Maharg, A. et al. Sex differences in the effects of a kappa opioid receptor antagonist in the forced swim test. Front. Pharm. 9, 93 (2018).
Przybysz, K. R., Varlinskaya, E. I. & Diaz, M. R. Age and sex regulate kappa opioid receptor-mediated anxiety-like behavior in rats. Behav. Brain Res. 379, 112379 (2020).
Reichard, K. L. et al. Regulation of kappa opioid receptor inactivation depends on sex and cellular site of antagonist action. Mol. Pharm. 98, 548–558 (2020).
Robles, C. F. et al. Effects of kappa opioid receptors on conditioned place aversion and social interaction in males and females. Behav. Brain Res. 262, 84–93 (2014).
Russell, S. E. et al. Sex differences in sensitivity to the depressive-like effects of the kappa opioid receptor agonist U-50488 in rats. Biol. Psychiatry 76, 213–222 (2014).
Hartoff, E. H. & Mavrikaki, M. Sex differences in kappa opioid receptor function and their potential impact on addiction. Front. Neurosci. 9, 466 (2015).
Brown, A. R. et al. Structured tracking of alcohol reinforcement (STAR) for basic and translational alcohol research. Mol. Psychiatry 28, 1585–1598 (2023).
Walker, B. M. & Koob, G. F. Pharmacological evidence for a motivational role of kappa-opioid systems in ethanol dependence. Neuropsychopharmacology 33, 643–652 (2008).
Osborn, M. D., Lowery, J. J., Skorput, A. G. J., Giuvelis, D. & Bilsky, E. J. In vivo characterization of the opioid antagonist nalmefene in mice. Life Sci. 86, 624–630 (2010).
Divin, M. F., Holden Ko, M. C. & Traynor, J. R. Comparison of the opioid receptor antagonist properties of naltrexone and 6 beta-naltrexol in morphine-naïve and morphine-dependent mice. Eur. J. Pharm. 583, 48–55 (2008).
Robinson, S. A., Erickson, R. L., Browne, C. A. & Lucki, I. A role for the mu opioid receptor in the antidepressant effects of buprenorphine. Behav. Brain Res. 319, 96–103 (2017).
Butelman, E. R. et al. Effects of salvinorin A, a kappa-opioid hallucinogen, on a neuroendocrine biomarker assay in nonhuman primates with high kappa-receptor homology to humans. J. Pharm. Exp. Ther. 320, 300–306 (2007).
Rose J. H. et al. Supersensitive kappa opioid receptors promotes ethanol withdrawal-related behaviors and reduce dopamine signaling in the nucleus accumbens. Int. J. Neuropsychopharmacol. 19, https://doi.org/10.1093/ijnp/pyv127 (2016).
Siciliano, C. A. et al. A cortical-brainstem circuit predicts and governs compulsive alcohol drinking. Science 366, 1008–1012 (2019).
Jia, T. et al. Neural network involving medial orbitofrontal cortex and dorsal periaqueductal gray regulation in human alcohol abuse. Sci. Adv. 7, eabd4074 (2021).
Tolomeo, S., Macfarlane, J. A., Baldacchino, A., Koob, G. F. & Steele, J. D. Alcohol binge drinking: negative and positive valence system abnormalities. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 6, 126–134 (2021).
Zhao, Y., Constable, R. T., Hien, D., Chung, T. & Potenza, M. N. Brain anatomical covariation patterns linked to binge drinking and age at first full drink. NeuroImage Clin. 29, 102529 (2021).
Zhao, Y. et al. Brain structural covariation linked to screen media activity and externalizing behaviors in children. J. Behav. Addict. 11, 417–426 (2022).
Zhao, Y., Paulus, M. P. & Potenza, M. N. Brain structural co-development is associated with internalizing symptoms two years later in the ABCD cohort. J. Behav. Addict. 12, 80–93 (2023).
Pulcinelli, R. R. et al. Taurine enhances voluntary alcohol intake and promotes anxiolytic-like behaviors in rats. Alcohol 88, 55–63 (2020).
Miranda-Páez, A., Marichal-Cancino, B. A., Sánchez-Castillo, H. & Vázquez-León, P. Acute taurine reduced alcohol intake and preference in alcohol-experienced, but not in alcohol-näive rats by central mechanisms. Behav. Brain Res. 463, 114892 (2024).
Ferguson, L. B., Mayfield, R. D. & Messing, R. O. RNA biomarkers for alcohol use disorder. Front. Mol. Neurosci. 15, 1032362 (2022).
Setiawan, E., Pihl, R. O., Benkelfat, C. & Leyton, M. Influence of the OPRM1 A118G polymorphism on alcohol-induced euphoria, risk for alcoholism and the clinical efficacy of naltrexone. Pharmacogenomics 13, 1161–1172 (2012).
Schacht, J. P. et al. Interacting effects of naltrexone and OPRM1 and DAT1 variation on the neural response to alcohol cues. Neuropsychopharmacology 38, 414–422 (2013).
Oslin, D. W. et al. A functional polymorphism of the mu-opioid receptor gene is associated with naltrexone response in alcohol-dependent patients. Neuropsychopharmacology 28, 1546–1552 (2003).
McGeary, J. E. et al. Genetic moderators of naltrexone’s effects on alcohol cue reactivity. Alcohol Clin. Exp. Res. 30, 1288–1296 (2006).
Kim, S. G. et al. A micro opioid receptor gene polymorphism (A118G) and naltrexone treatment response in adherent Korean alcohol-dependent patients. Psychopharmacology 201, 611–618 (2009).
Oroszi, G. et al. OPRM1 Asn40Asp predicts response to naltrexone treatment: a haplotype-based approach. Alcohol Clin. Exp. Res. 33, 383–393 (2009).
Arias, A. J. et al. Effects of opioid receptor gene variation on targeted nalmefene treatment in heavy drinkers. Alcohol Clin. Exp. Res. 32, 1159–1166 (2008).
Karkhanis, A. N., Huggins, K. N., Rose, J. H. & Jones, S. R. Switch from excitatory to inhibitory actions of ethanol on dopamine levels after chronic exposure: role of kappa opioid receptors. Neuropharmacology 110, 190–197 (2016).
Siciliano, C. A. et al. Voluntary ethanol intake predicts κ-opioid receptor supersensitivity and regionally distinct dopaminergic adaptations in macaques. J. Neurosci. 35, 5959–5968 (2015).
Marinelli, P. W., Lam, M., Bai, L., Quirion, R. & Gianoulakis, C. A microdialysis profile of dynorphin A(1-8) release in the rat nucleus accumbens following alcohol administration. Alcohol Clin. Exp. Res. 30, 982–990 (2006).
Mathieu-Kia, A. M. & Besson, M. J. Repeated administration of cocaine, nicotine and ethanol: effects on preprodynorphin, preprotachykinin A and preproenkephalin mRNA expression in the dorsal and the ventral striatum of the rat. Brain Res. Mol. Brain Res. 54, 141–151 (1998).
McGonigle, C. E., Nentwig, T. B., Wilson, D. E., Rhinehart, E. M. & Grisel, J. E. Β-endorphin regulates alcohol consumption induced by exercise restriction in female mice. Alcohol 53, 51–60 (2016).
Roschina, O. V. et al. Beta-endorphin and oxytocin in patients with alcohol use disorder and comorbid depression. J. Clin. Med. 10, 5696 (2021).
de Waele, J. P., Kiianmaa, K. & Gianoulakis, C. Spontaneous and ethanol-stimulated in vitro release of beta-endorphin by the hypothalamus of AA and ANA rats. Alcohol Clin. Exp. Res. 18, 1468–1473 (1994).
Dai, X., Thavundayil, J. & Gianoulakis, C. Differences in the responses of the pituitary beta-endorphin and cardiovascular system to ethanol and stress as a function of family history. Alcohol Clin. Exp. Res. 26, 1171–1180 (2002).
Tuttle, A. H., Philip, V. M., Chesler, E. J. & Mogil, J. S. Comparing phenotypic variation between inbred and outbred mice. Nat. Methods 15, 994–996 (2018).
Acknowledgements
This work was supported by NIH grants R00 DA04510 (C.A.S), R01 AA030115 (C.A.S.), U01 AA029971 (C.A.S.), P60 AA031124 (C.A.S.), and the Whitehall Foundation (C.A.S). Z.Z.F. was supported by NIH fellowships T32 MH064913 and F31 DA056196. S.O.N. was supported by an NIH fellowship (F32 DA051136). S.M. was supported by a NARSAD Young Investigator Award from the Brain and Behavior Research Foundation.
Author information
Authors and Affiliations
Contributions
Z.Z.F., A.R.B., & C.A.S. conceived of the project. Z.Z.F. & C.A.S. designed experiments. Z.Z.F. & A.R.B. collected and analyzed data. Z.Z.F., A.R.B., S.O.N., & S.M. contributed to the execution of experiments. Z.Z.F., A.R.B., & C.A.S. wrote the manuscript. All authors read and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Jen Rinker and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farahbakhsh, Z.Z., Brown, A.R., Nolan, S.O. et al. Nalmefene and naltrexone reduce alcohol intake via selective efficacy in subpopulations distinguished by behavioral and blood-based biomarkers. Commun Med (2026). https://doi.org/10.1038/s43856-025-01369-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-025-01369-6