Abstract
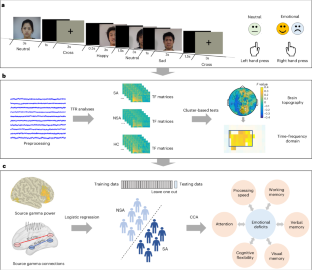
Altered neural oscillations in response to negative or positive emotional stimuli may be related to severe clinical symptoms in patients with major depressive disorder, particularly high suicidality. However, the underlying neurobiological mechanisms of this aberrant oscillatory activity and its potential emotional and cognitive functions remain unclear. Here we conducted a cross-sectional study of 107 participants, including 40 healthy controls and 67 patients with major depressive disorder (33 with suicide attempts and 34 without). All participants underwent an emotional expression recognition task during the magnetoencephalography scanning and completed neurocognitive assessments. Time–frequency characteristics and phase connections were analysed and compared between groups in sensor and source space using cluster-based permutation tests. The association between abnormal oscillatory features and neurocognitive performance was also evaluated. We found that increased gamma oscillations (50–70 Hz) of the visual cortices were considerably associated with suicide attempts in depression. Moreover, gamma-band source power in happy or sad conditions could predict individualized suicide risk. Gamma-band phase connections under the happy or sad condition were related to deficits in large-scale cognitive functions. Overall, gamma oscillations of the visual areas induced by the emotional stimuli were reliable biomarkers for identifying suicide attempts in depressive patients. Abnormal gamma-band connection involving visual cortex under both happy and sad expressions were significantly correlated with broad cognitive deficits.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the key findings are available from the Open Science Framework (https://osf.io/q5zyg/). For any inquiries regarding the data, requests can be made to the corresponding authors.
Code availability
MEG data were preprocessed and analysed with the MATLAB r2016b based Fieldtrip (v.2017) toolbox (https://github.com/fieldtrip/fieldtrip)55. The sample size was estimated with G*Power_3.1.9.7 software (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower)47. The statistical comparisons involving demographic variables, behavioral data were conducted with SPSS software (v.22)59. The data distribution plots were conducted with GraphPad Prism software (8.0.2)60. The brain maps were plotted with the BrainNet Viewer (v.2017) toolbox (https://github.com/mingruixia/BrainNet-Viewer)32. The custom codes are available from the Open Science Framework (https://osf.io/q5zyg/).
References
Millner, A. J., Robinaugh, D. J. & Nock, M. K. Advancing the understanding of suicide: the need for formal theory and rigorous descriptive research. Trends Cogn. Sci. 24, 704–716 (2020).
Séguin, M. Review of suicide risk management: a manual for health professionals. Can. Psychol. 53, 255–257 (2012).
Jung, J. et al. Alterations in functional brain networks in depressed patients with a suicide attempt history. Neuropsychopharmacology 45, 964–974 (2020).
Ruhe, H. G. et al. Emotional biases and recurrence in major depressive disorder. Results of 2.5 years follow-up of drug-free cohort vulnerable for recurrence. Front. Psychiatry 10, 145 (2019).
Stuhrmann, A., Suslow, T. & Dannlowski, U. Facial emotion processing in major depression: a systematic review of neuroimaging findings. Biol. Mood Anxiety Disord. 1, 10 (2011).
Dai, Z. et al. Attenuated alpha-gamma coupling in emotional dual pathways with right-amygdala predicting ineffective antidepressant response. CNS Neurosci. Ther. 28, 401–410 (2022).
Li, Y., Cao, D., Wei, L., Tang, Y. & Wang, J. Abnormal functional connectivity of EEG gamma band in patients with depression during emotional face processing. Clin. Neurophysiol. 126, 2078–2089 (2015).
Atallah, B. V. & Scanziani, M. Instantaneous modulation of gamma oscillation frequency by balancing excitation with inhibition. Neuron 62, 566–577 (2009).
Touboul, J. & Destexhe, A. Can power-law scaling and neuronal avalanches arise from stochastic dynamics? PLoS ONE 5, e8982 (2010).
Gladding, C. M., Fitzjohn, S. M. & Molnár, E. Metabotropic glutamate receptor-mediated long-term depression: molecular mechanisms. Pharmacol. Rev. 61, 395–412 (2009).
Uhlhaas, P. J. & Singer, W. Abnormal neural oscillations and synchrony in schizophrenia. Nat. Rev. Neurosci. 11, 100–113 (2010).
Arikan, M. K., Gunver, M. G., Tarhan, N. & Metin, B. High-gamma: a biological marker for suicide attempt in patients with depression. J. Affect. Disord. 254, 1–6 (2019).
Gilbert, J. R., Ballard, E. D., Galiano, C. S., Nugent, A. C. & Zarate, C. A. Jr Magnetoencephalographic correlates of suicidal ideation in major depression. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 5, 354–363 (2020).
Fitzgerald, P. J. & Watson, B. O. Gamma oscillations as a biomarker for major depression: an emerging topic. Transl. psychiatry 8, 177 (2018).
Dai, Z. et al. Disrupted fronto-parietal network and default-mode network gamma interactions distinguishing suicidal ideation and suicide attempt in depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 113, 110475 (2022).
Dai, Z. et al. Hampered gamma oscillations induced by sad emotion underlying suicide attempt in major depressive disorder. Psychiatry Clin. Neurosci. 77, 20–29 (2023).
Shestyuk, A. Y., Deldin, P. J., Brand, J. E. & Deveney, C. M. Reduced sustained brain activity during processing of positive emotional stimuli in major depression. Biol. Psychiatry 57, 1089–1096 (2005).
Silton, R. L. et al. Regulating positive emotions: implications for promoting well-being in individuals with depression. Emotion 20, 93–97 (2020).
Grent-‘t-Jong, T. et al. Association of magnetoencephalographically measured high-frequency oscillations in visual cortex with circuit dysfunctions in local and large-scale networks during emerging psychosis. JAMA Psychiatry 77, 852–862 (2020).
Liu, S. & Parvizi, J. Cognitive refractory state caused by spontaneous epileptic high-frequency oscillations in the human brain. Sci. Transl. Med. 11, eaax7830 (2019).
Lan, X. et al. Association between cognition and suicidal ideation in patients with major depressive disorder: a longitudinal study. J. Affect. Disord. 272, 146–151 (2020).
Fazakas-DeHoog, L. L., Rnic, K. & Dozois, D. J. A cognitive distortions and deficits model of suicide ideation. Eur. J. Psychol. 13, 178–193 (2017).
Westheide, J. et al. Executive performance of depressed suicide attempters: the role of suicidal ideation. Eur. Arch. Psychiatry Clin. Neurosci. 258, 414–421 (2008).
Gujral, S. et al. Impaired executive function in contemplated and attempted suicide in late life. Am. J. Geriatr. Psychiatry 22, 811–819 (2014).
Manor, I. et al. Possible association between attention deficit hyperactivity disorder and attempted suicide in adolescents—a pilot study. Eur. Psychiatry 25, 146–150 (2010).
Balazs, J. & Kereszteny, A. Attention-deficit/hyperactivity disorder and suicide: a systematic review. World J. Psychiatry 7, 44–59 (2017).
Ram, D., Chandran, S., Sadar, A. & Gowdappa, B. Correlation of cognitive resilience, cognitive flexibility and impulsivity in attempted suicide. Indian J. Psychol. Med. 41, 362–367 (2019).
Saffer, B. Y. & Klonsky, E. D. Do neurocognitive abilities distinguish suicide attempters from suicide ideators? A systematic review of an emerging research area. Clin. Psychol. 25, e12227 (2018).
Yin, Y. et al. Suicidal ideation, suicide attempts, and neurocognitive dysfunctions among patients with first‐episode schizophrenia. Suicide Life Threat. Behav. 50, 1181–1188 (2020).
Siems, M., Pape, A.-A., Hipp, J. F. & Siegel, M. Measuring the cortical correlation structure of spontaneous oscillatory activity with EEG and MEG. NeuroImage 129, 345–355 (2016).
Muthukumaraswamy, S. D. & Singh, K. D. Visual gamma oscillations: the effects of stimulus type, visual field coverage and stimulus motion on MEG and EEG recordings. Neuroimage 69, 223–230 (2013).
Xia, M., Wang, J. & He, Y. BrainNet Viewer: a network visualization tool for human brain connectomics. PLoS ONE 8, e68910 (2013).
Lewis, D. A., Curley, A. A., Glausier, J. R. & Volk, D. W. Cortical parvalbumin interneurons and cognitive dysfunction in schizophrenia. Trends Neurosci. 35, 57–67 (2012).
Murray, J. D. et al. Linking microcircuit dysfunction to cognitive impairment: effects of disinhibition associated with schizophrenia in a cortical working memory model. Cereb. Cortex 24, 859–872 (2014).
Schreiner, M. W., Klimes-Dougan, B. & Cullen, K. R. Neural correlates of suicidality in adolescents with major depression: resting-state functional connectivity of the precuneus and posterior cingulate cortex. Suicide Life Threat. Behav. 49, 899–913 (2019).
Vanderlind, W. M., Millgram, Y., Baskin-Sommers, A. R., Clark, M. S. & Joormann, J. Understanding positive emotion deficits in depression: from emotion preferences to emotion regulation. Clin. Psychol. Rev. 76, 101826 (2020).
Dai, Z. et al. Sub-second transient activated patterns to sad expressions in major depressive disorders discovered via hidden Markov model. J. Neurosci. Res. 99, 3250–3260 (2021).
Atlas, L. Y. How instructions shape aversive learning: higher order knowledge, reversal learning, and the role of the amygdala. Curr. Opin. Behav. Sci. 26, 121–129 (2019).
Farzan, F. et al. Evidence for gamma inhibition deficits in the dorsolateral prefrontal cortex of patients with schizophrenia. Brain 133, 1505–1514 (2010).
Yang, Y. et al. Atrophy of right inferior frontal orbital gyrus and frontoparietal functional connectivity abnormality in depressed suicide attempters. Brain Imag. Behav. 14, 2542–2552 (2020).
Zhu, R. et al. Discriminating suicide attempters and predicting suicide risk using altered frontolimbic resting-state functional connectivity in patients with bipolar II disorder. Front. Psychiatry 11, 1352 (2020).
Santamarina-Perez, P. et al. Visual memory improvement in adolescents at high risk for suicide who are receiving psychotherapy at a community clinic. Psychiatry Res. 298, 113796 (2021).
Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62 (1960).
Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 32, 50–55 (1959).
Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR (American Psychiatric Association, 2003).
Beck, A. T., Steer, R. A. & Ranieri, W. F. Scale for suicide ideation: psychometric properties of a self‐report version. J. Clin. Psychol. 44, 499–505 (1988).
Faul, F., Erdfelder, E., Buchner, A. & Lang, A.-G. Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160 (2009).
Du, J., Yao, Z., XIE, S., Shi, J. & Teng, G. The primary development of Chinese facial expression video system. Chin. Ment. Health J. 21, 333–337 (2007).
Zhao, S. et al. Sex differences in the association between symptom profiles and cognitive functioning in patients with depressive disorder. J. Affect. Disord. 287, 1–7 (2021).
Reitan, R. M. Validity of the Trail Making Test as an indicator of organic brain damage. Percept. Mot. Skills 8, 271–276 (1958).
Wechsler, D. Wechsler Memory Scale-Revised (Psychological Corporation, 1987).
Wechsler, D. Manual for the Wechsler Adult Intelligence Scale (Psychological Corporation, 1955).
Wechsler, D. WMS-III: Wechsler Memory Scale Administration and Scoring Manual (Psychological Corporation, 1997).
Liu, J. et al. Exploration of major cognitive deficits in medication-free patients with major depressive disorder. Front. Psychiatry 12, 836 (2019).
Oostenveld, R., Fries, P., Maris, E. & Schoffelen, J.-M. FieldTrip: open source software for advanced analysis of MEG, EEG, and invasive electrophysiological data. Comput. Intell. Neurosci. 2011, 156869 (2011).
Tallon-Baudry, C., Bertrand, O., Delpuech, C. & Pernier, J. Stimulus specificity of phase-locked and non-phase-locked 40 Hz visual responses in human. J. Neurosci. 16, 4240–4249 (1996).
Gross, J. et al. Dynamic imaging of coherent sources: studying neural interactions in the human brain. Proc. Natl Acad. Sci. USA 98, 694–699 (2001).
Vinck, M., Oostenveld, R., Van Wingerden, M., Battaglia, F. & Pennartz, C. M. An improved index of phase-synchronization for electrophysiological data in the presence of volume-conduction, noise and sample-size bias. Neuroimage 55, 1548–1565 (2011).
SPSS Statistics for Windows v.22.0 (IBM, 2013).
GraphPad v.8.0.2. (GraphPad Software, 2019).
Maris, E. & Oostenveld, R. Nonparametric statistical testing of EEG-and MEG-data. J. Neurosci. Methods 164, 177–190 (2007).
Acknowledgements
This research received support from the National Natural Science Foundation of China (grants 81871066, 81571639 and 81701784) awarded to Q.L.; the Fundamental Research Funds for the Central Universities (2242021k30014, 2242021k30059) awarded to Q.L.; the Jiangsu Provincial Medical Innovation Team of the Project of Invigorating Health Care through Science, Technology, and Education (grant CXTDC2016004) awarded to Z.Y.; and the Jiangsu Provincial key research and development program (grant BE2018609) awarded to Z.Y.; Z.D. was supported by the Chinese Scholarship Council. We are grateful to O. Jensen from the University of Birmingham and H. Jiang from Zhejiang University for their valuable comments on this work. We would also like to express our appreciation to Y. Pan and T. Ghafari from the University of Birmingham for their helpful suggestions. Additionally, we acknowledge the editing and proofreading services provided by American Journal Experts, which substantially contributed to improving the clarity and language of this paper.
Author information
Authors and Affiliations
Contributions
Q.L. and Z.Y. were responsible for conceptualization. Z.D., W.Z. and S.Z. were responsible for methodology. Z.D., H.Z. and W.Z. were responsible for formal analysis. Z.D., H.Z., Z.C. and W.Z. were responsible for investigation. Z.D. wrote the orignal draft; Z.D., Q.L., H.Z. and S.Z. reviewed and edited the paper. Z.D. was responsible for visualization. Q.L. and Z.Y. supervised the project and acquired funding.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks the, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–15 and Table 1.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dai, Z., Zhang, W., Zhou, H. et al. Gamma oscillations of visual cortex underlying emotion and cognition deficits associated with suicide attempt in major depressive disorder. Nat. Mental Health 2, 924–934 (2024). https://doi.org/10.1038/s44220-024-00269-3
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-024-00269-3
This article is cited by
-
Uncovering oscillatory dysregulation associated with suicide risk in major depressive disorder: a narrative review
Translational Psychiatry (2026)
-
Tai Chi modulating multimodal connectivity patterns and cognitive function in cerebral small vessel disease
GeroScience (2026)
-
Brain structural and functional aberrant of hippocampal subregions was associated with somatic depression
BMC Psychiatry (2025)