Abstract
Major depressive disorder (MDD) is a prevalent psychiatric illness marked by notable changes in mood, behavior and cognition. Emerging evidence indicates that depression can differ by sex in terms of onset, symptoms and treatment response. While modern psychiatry acknowledges sex differences in epidemiology, we are yet to identify biomarkers that could guide sex-specific interventions.
Recent discoveries in MDD research point towards alterations in functional brain network patterns. This Perspective highlights the rationale for using resting-state functional magnetic resonance imaging (rs-fMRI) to identify sex differences in MDD. We present preliminary evidence for sex-based differences in depression from the limited existing rs-fMRI literature. Although limited and heterogeneous in their design, the results point towards the need for larger research studies. Furthermore, in female individuals, hormonal fluctuations during specific life phases pose a substantial risk for the onset of depressive episodes.
We advocate that future studies integrate sex as an essential factor in MDD research and utilize resting-state functional connectivity to identify sex-specific neural features and biomarkers. We finally recommend ways to incorporate menstrual and reproductive cycle data into depression research to develop better diagnostic tools and personalized treatment strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lundberg, J. et al. Determinants and outcomes of suicidal behavior among patients with major depressive disorder. JAMA Psychiatry 80, 1218–1225 (2023).
Garnett, F. M. & Curtin C. S. Suicide Mortality in the United States, 2001–2021 Data Brief 464 (National Center for Health Statistics, 2023).
Cavanagh, A., Wilson, C. J., Kavanagh, D. J. & Caputi, P. Differences in the expression of symptoms in men versus women with depression: a systematic review and meta-analysis. Harv. Rev. Psychiatry 25, 29–38 (2017).
Mazure, C. M. What do we mean by sex and gender? Yale School of Medicine https://medicine.yale.edu/news-article/what-do-we-mean-by-sex-and-gender/ (2021).
Liu, M., Patel, V. R., Reisner, S. L. & Keuroghlian, A. S. Health status and mental health of transgender and gender-diverse adults. JAMA Intern. Med. 184, 984–986 (2024).
Villarroel, M. A. & Terlizzi, E. P. Symptoms of Depression Among Adults: United States, 2019 Data Brief 379 (National Center for Health Statistics, 2020).
Hyde, J. S. & Mezulis, A. H. Gender differences in depression: biological, affective, cognitive, and sociocultural factors. Harv. Rev. Psychiatry 28, 4–13 (2020).
Piccinelli, M. & Wilkinson, G. Gender differences in depression: critical review. Br. J. Psychiatry 177, 486–492 (2000).
Seedat, S. et al. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch. Gen. Psychiatry 66, 785–795 (2009).
Lui, S., Zhou, X. J., Sweeney, J. A. & Gong, Q. Psychoradiology: the frontier of neuroimaging in psychiatry. Radiology 281, 357–372 (2016).
Smallwood, R. F., Hutson, R. M. & Robin, D. A. in Pathobiology of Human Disease (eds McManus, L. M. & Mitchell, R. N.) 2522–2537 (Academic, 2014).
Kochunov, P. et al. Functional vs structural cortical deficit pattern biomarkers for major depressive disorder. JAMA Psychiatry 82, 582–590 (2025).
Whitfield-Gabrieli, S. et al. Association of intrinsic brain architecture with changes in attentional and mood symptoms during development. JAMA Psychiatry 77, 378–386 (2020).
Fox, M. D. et al. Resting-state networks link invasive and noninvasive brain stimulation across diverse psychiatric and neurological diseases. Proc. Natl Acad. Sci. USA 111, E4367–E4375 (2014).
Yamashita, A. et al. Unsupervised feature computation-based feature selection robustly extracted resting-state functional connectivity patterns related to mental disorders. Preprint at bioRxiv https://doi.org/10.1101/2025.04.14.648842 (2025).
Uddin, L. Q., Castellanos, F. X. & Menon, V. Resting state functional brain connectivity in child and adolescent psychiatry: where are we now? Neuropsychopharmacology 50, 196–200 (2025).
Norman, L. J. et al. Cross-sectional mega-analysis of resting-state alterations associated with autism and attention-deficit/hyperactivity disorder in children and adolescents. Nat. Mental Health 3, 709–723 (2025).
Zang, Y.-F., Zuo, X.-N., Milham, M. & Hallett, M. Toward a meta-analytic synthesis of the resting-state fMRI literature for clinical populations. BioMed Res. Int. 2015, e435265 (2015).
Kaiser, R. H., Andrews-Hanna, J. R., Wager, T. D. & Pizzagalli, D. A. Large-scale network dysfunction in Major Depressive Disorder: meta-analysis of resting-state functional connectivity. JAMA Psychiatry 72, 603–611 (2015).
Mitra, A., Raichle, M. E., Geoly, A. D., Kratter, I. H. & Williams, N. R. Targeted neurostimulation reverses a spatiotemporal biomarker of treatment-resistant depression. Proc. Natl Acad. Sci. USA 120, e2218958120 (2023).
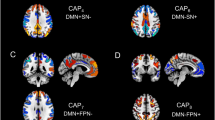
An, Z. et al. Aberrant resting-state co-activation network dynamics in major depressive disorder. Transl. Psychiatry 14, 1 (2024).
Buch, A. M. & Liston, C. Dissecting diagnostic heterogeneity in depression by integrating neuroimaging and genetics. Neuropsychopharmacology 46, 156–175 (2021).
Rechlin, R. K., Splinter, T. F. L., Hodges, T. E., Albert, A. Y. & Galea, L. A. M. An analysis of neuroscience and psychiatry papers published from 2009 and 2019 outlines opportunities for increasing discovery of sex differences. Nat. Commun. 13, 2137 (2022).
Duffy, K. A. & Epperson, C. N. Evaluating the evidence for sex differences: a scoping review of human neuroimaging in psychopharmacology research. Neuropsychopharmacology 47, 430–443 (2022).
Young, K. D., Bodurka, J. & Drevets, W. C. Functional neuroimaging of sex differences in autobiographical memory recall in depression. Psychol. Med. 47, 2640–2652 (2017).
Jenkins, L. M. et al. Considering sex differences clarifies the effects of depression on facial emotion processing during fMRI. J. Affect. Disord. 225, 129–136 (2018).
Dong, D. et al. Sex-specific neural responses to acute psychosocial stress in depression. Transl. Psychiatry 12, 2 (2022).
Orgo, L., Bachmann, M., Kalev, K., Hinrikus, H. & Järvelaid, M. Brain functional connectivity in depression: gender differences in EEG. In Proc. 2016 IEEE EMBS Conference on Biomedical Engineering and Sciences (IECBES) 270–273 (IEEE, 2016).
Mohammadi, S. et al. Brain-based sex differences in depression: a systematic review of neuroimaging studies. Brain Imaging Behav. 17, 541–569 (2023).
Biswal, B., Yetkin, F. Z., Haughton, V. M. & Hyde, J. S. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn. Reson. Med. 34, 537–541 (1995).
Mei, L. et al. Study of sex differences in unmedicated patients with major depressive disorder by using resting state brain functional magnetic resonance imaging. Front. Neurosci. 16, 814410 (2022).
Marcus, S. M. et al. Gender differences in depression: findings from the STAR*D study. J. Affect. Disord. 87, 141–150 (2005).
Teng, C. et al. Abnormal resting state activity of left middle occipital gyrus and its functional connectivity in female patients with major depressive disorder. BMC Psychiatry 18, 370 (2018).
Wang, X. et al. The sex differences in anhedonia in major depressive disorder: a resting-state fMRI study. J. Affect. Disord. 340, 555–566 (2023).
Yang, X. et al. Physical and social anhedonia in female adolescents: a factor analysis of self-report measures. Emotion 22, 1828–1840 (2022).
Li, G., Liu, P., Zhang, A., Andari, E. & Zhang, K.-R. A resting state fMRI study of major depressive disorder with and without anxiety. Psychiatry Res. 315, 114697 (2022).
Yao, Z. et al. Gender differences in brain activity and the relationship between brain activity and differences in prevalence rates between male and female major depressive disorder patients: a resting-state fMRI study. Clin. Neurophysiol. 125, 2232–2239 (2014).
Geng, J. et al. Altered regional homogeneity in patients with somatic depression: a resting-state fMRI study. J. Affect. Disord. 246, 498–505 (2019).
Sun, J. et al. A study of differential resting-state brain functional activity in males and females with recurrent depressive disorder. Brain Sci. 12, 1508 (2022).
Tian, X., Hu, N., Lu, L., Tan, L. & Li, P. Gender differences in major depressive disorder at different ages: a REST-meta-MDD project-based study. BMC Psychiatry 24, 575 (2024).
Wang, L., Hermens, D. F., Hickie, I. B. & Lagopoulos, J. A systematic review of resting-state functional-MRI studies in major depression. J. Affect. Disord. 142, 6–12 (2012).
Wei, S. et al. Amygdala functional connectivity in female patients with major depressive disorder with and without suicidal ideation. Ann. Gen. Psychiatry 17, 37 (2018).
Talishinsky, A. et al. Regional gene expression signatures are associated with sex-specific functional connectivity changes in depression. Nat. Commun. 13, 5692 (2022).
Yang, C. et al. Sex differences in aberrant functional connectivity of three core networks and subcortical networks in medication-free adolescent-onset major depressive disorder. Cereb. Cortex 34, bhae225 (2024).
Su, T. et al. Sex-specific habenular dysconnectivity in patients with late-life depression. Transl. Psychiatry 15, 121 (2025).
Dong, D. et al. Sex-specific resting state brain network dynamics in patients with major depressive disorder. Neuropsychopharmacology 49, 806–813 (2024).
Amiri, S., Arbabi, M., Kazemi, K., Parvaresh-Rizi, M. & Mirbagheri, M. M. Characterization of brain functional connectivity in treatment-resistant depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 111, 110346 (2021).
Stickel, S. et al. Neural correlates of depression in women across the reproductive lifespan—an fMRI review. J. Affect. Disord. 246, 556–570 (2019).
Weis, S., Hodgetts, S. & Hausmann, M. Sex differences and menstrual cycle effects in cognitive and sensory resting state networks. Brain Cogn. 131, 66–73 (2019).
Avila-Varela, D. S. et al. Whole-brain dynamics across the menstrual cycle: the role of hormonal fluctuations and age in healthy women. npj Women's Health 2, 8 (2024).
Hidalgo-Lopez, E. et al. Human menstrual cycle variation in subcortical functional brain connectivity: a multimodal analysis approach. Brain Struct. Funct. 225, 591–605 (2020).
Soares, C. N. & Zitek, B. Reproductive hormone sensitivity and risk for depression across the female life cycle: a continuum of vulnerability? J. Psychiatry Neurosci. 33, 331–343 (2008).
Apter-Levy, Y., Feldman, M., Vakart, A., Ebstein, R. P. & Feldman, R. Impact of maternal depression across the first 6 years of life on the child’s mental health, social engagement, and empathy: the moderating role of oxytocin. Am. J. Psychiatry 170, 1161–1168 (2013).
Nolan, L. N. & Hughes, L. Premenstrual exacerbation of mental health disorders: a systematic review of prospective studies. Arch. Women's Ment. Health 25, 831–852 (2022).
Bromberger, J. T. & Epperson, C. N. Depression during and after the perimenopause: impact of hormones, genetics, and environmental determinants of disease. Obstet. Gynecol. Clin. N. Am. 45, 663–678 (2018).
Owens, S. A. & Eisenlohr-Moul, T. Suicide risk and the menstrual cycle: a review of candidate RDoC mechanisms. Curr. Psychiatry Rep. 20, 106 (2018).
Admon, L. K. et al. Trends in suicidality 1 year before and after birth among commercially insured childbearing individuals in the United States, 2006–2017. JAMA Psychiatry 78, 171–176 (2021).
Nakanishi, M. et al. Association between menopause and suicidal ideation in mothers of adolescents: a longitudinal study using data from a population-based cohort. J. Affect. Disord. 340, 529–534 (2023).
Monteiro, D. C. et al. Functional and structural neuroimaging in premenstrual dysphoric disorder: a systematic review. J. Psychiatric Res. 175, 205–210 (2024).
Lu, W., Sun, Y., Gao, H. & Qiu, J. A review of multi-modal magnetic resonance imaging studies on perimenopausal brain: a hint towards neural heterogeneity. Eur. Radiol. 33, 5282–5297 (2023).
Tang, Y. et al. A systematic review of resting-state functional-MRI studies in the diagnosis, comorbidity and treatment of postpartum depression. J. Affect. Disord. 383, 153–166 (2025).
Petersen, N. et al. Resting-state functional connectivity in women with PMDD. Transl. Psychiatry 9, 339 (2019).
Seidman, S. N., Araujo, A. B., Roose, S. P. & McKinlay, J. B. Testosterone level, androgen receptor polymorphism, and depressive symptoms in middle-aged men. Biol. Psychiatry 50, 371–376 (2001).
Walther, A., Breidenstein, J. & Miller, R. Association of testosterone treatment with alleviation of depressive symptoms in men: a systematic review and meta-analysis. JAMA Psychiatry 76, 31–40 (2019).
Singh, P. Andropause: current concepts. Indian J. Endocrinol. Metab. 17, S621–S629 (2013).
Sramek, J. J., Murphy, M. F. & Cutler, N. R. Sex differences in the psychopharmacological treatment of depression. Dialogues Clin. Neurosci. 18, 447–457 (2016).
Ponton, E., Turecki, G. & Nagy, C. Sex differences in the behavioral, molecular, and structural effects of ketamine treatment in depression. Int. J. Neuropsychopharmacol. 25, 75–84 (2021).
Brus, O. et al. Subjective memory immediately following electroconvulsive therapy. J. ECT 33, 96–103 (2017).
Sackeim, H. A. et al. Clinical outcomes in a large registry of patients with major depressive disorder treated with Transcranial Magnetic Stimulation. J. Affect. Disord. 277, 65–74 (2020).
Hanlon, C. A. & McCalley, D. M. Sex/gender as a factor that influences transcranial magnetic stimulation treatment outcome: three potential biological explanations. Front. Psychiatry 13, 869070 (2022).
Woolley, C. S. Acute effects of estrogen on neuronal physiology. Annu. Rev. Pharmacol. Toxicol. 47, 657–680 (2007).
Chung, S. W. et al. The influence of endogenous estrogen on high-frequency prefrontal transcranial magnetic stimulation. Brain Stimul. 12, 1271–1279 (2019).
Huang, C.-C., Wei, I.-H., Chou, Y.-H. & Su, T.-P. Effect of age, gender, menopausal status, and ovarian hormonal level on rTMS in treatment-resistant depression. Psychoneuroendocrinology 33, 821–831 (2008).
Rivas-Grajales, A. M., Barbour, T., Camprodon, J. A. & Kritzer, M. D. The impact of sex hormones on transcranial magnetic stimulation measures of cortical excitability: a systematic review and considerations for clinical practice. Harv. Rev. Psychiatry 31, 114–123 (2023).
Kim, A. M., Tingen, C. M. & Woodruff, T. K. Sex bias in trials and treatment must end. Nature 465, 688–689 (2010).
Beery, A. K. & Zucker, I. Sex bias in neuroscience and biomedical research. Neurosci. Biobehav. Rev. 35, 565–572 (2011).
Wierenga, L. M. et al. Recommendations for a better understanding of sex and gender in the neuroscience of mental health. Biol. Psychiatry Glob. Open Sci. 4, 100283 (2024).
Sosinsky, A. Z. et al. Enrollment of female participants in United States drug and device phase 1–3 clinical trials between 2016 and 2019. Contemp. Clin. Trials 115, 106718 (2022).
Shapiro, J. R., Klein, S. L. & Morgan, R. Stop ‘controlling’ for sex and gender in global health research. BMJ Glob. Health 6, e005714 (2021).
Yan, C.-G. et al. Reduced default mode network functional connectivity in patients with recurrent major depressive disorder. Proc. Natl Acad. Sci. USA 116, 9078–9083 (2019).
Biswal, B. B. et al. Toward discovery science of human brain function. Proc. Natl Acad. Sci. USA 107, 4734–4739 (2010).
Williams, L. M. Defining biotypes for depression and anxiety based on large-scale circuit dysfunction: a theoretical review of the evidence and future directions for clinical translation. Depress. Anxiety 34, 9–24 (2017).
Drysdale, A. T. et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat. Med. 23, 28–38 (2017).
Cole, E. J. et al. Stanford Neuromodulation Therapy (SNT): a double-blind randomized controlled trial. Am. J. Psychiatry 179, 132–141 (2022).
Szadvári, I., Ostatníková, D. & Babková Durdiaková, J. Sex differences matter: males and females are equal but not the same. Physiol. Behav. 259, 114038 (2023).
Harrison, T. M. et al. Tau deposition is associated with functional isolation of the hippocampus in aging. Nat. Commun. 10, 4900 (2019).
Schaefer, A. et al. Local–global parcellation of the human cerebral cortex from intrinsic functional connectivity MRI. Cereb. Cortex 28, 3095–3114 (2018).
Author information
Authors and Affiliations
Contributions
M.S.: conceptualization; writing—original draft, literature review and editing; visualization. W.S.: writing—original draft, literature review and editing. N.D.J.: writing—original draft, literature review. M.T.: writing—original draft, literature review. C.E.R.: writing—critique and editing. I.H.K.: conceptualization; writing—critique and editing. N.R.W.: supervision; writing—critique and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sridhar, M., Struckmann, W., Johnson, N.D. et al. Functional neuroimaging highlights sex as a critical variable in depression research. Nat. Mental Health 3, 974–981 (2025). https://doi.org/10.1038/s44220-025-00477-5
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-025-00477-5