Abstract
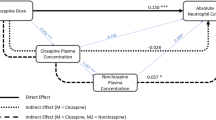
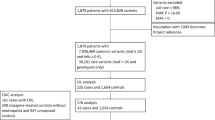
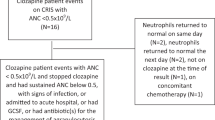
Clozapine is the most effective therapy for treatment-resistant schizophrenia, although it can cause neutropenia. In many countries, neutrophil count monitoring is mandatory for people taking clozapine, who must remain above a minimum threshold to start and continue treatment. Some people have low neutrophil counts without increased infection risk, caused by a homozygous variant in ACKR1 and termed ACKR1/DARC-associated neutropenia (ADAN). When ADAN is confirmed, reduced neutrophil count thresholds are applied to allow people to start and continue clozapine. However, ADAN diagnoses are often missed, resulting in reduced access to clozapine and unnecessary discontinuation. We review the evidence for ACKR1 genetic testing to rapidly identify ADAN in people taking clozapine. With multidisciplinary input, we recommend internationally relevant test eligibility criteria, comprising pre-emptive and reactive testing strategies, and we conduct a health economic analysis, estimating total cost savings between £42,732 and £727,990 for the UK healthcare system during the first year of testing. Finally, we propose how to integrate these criteria into clinical practice to enable equitable access to clozapine.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Code availability
Full calculations and formulas for the health economic analysis are shown in Supplementary Appendix 2.
References
Joint Formulary Committee. British National Formulary (online) (BMJ and Pharmaceutical Press, 2024).
National Institute for Health and Care Excellence. Quality Statement 4: Treatment with Clozapine [NICE QS80] (NICE, 2015).
Howes, O. D. et al. Treatment-resistant schizophrenia: Treatment Response and Resistance in Psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am. J. Psychiatry 174, 216–229 (2017).
Verdoux, H. et al. The time has come for revising the rules of clozapine blood monitoring in Europe. A joint expert statement from the European Clozapine Task Force. Eur. Psychiatry 68, e17 (2025).
Keepers, G. A. et al. The American Psychiatric Association practice guideline for the treatment of patients with schizophrenia. Am. J. Psychiatry 177, 868–872 (2020).
Government of Western Australia Guidelines for the Safe and Quality Use of Clozapine in the WA Health System Version 2.0 (Western Australian Department of Health, 2024).
Meltzer, H. Y. Treatment-resistant schizophrenia–the role of clozapine. Curr. Med. Res. Opin. 14, 1–20 (1997).
Kennedy, J. L., Altar, C. A., Taylor, D. L., Degtiar, I. & Hornberger, J. C. The social and economic burden of treatment-resistant schizophrenia: a systematic literature review. Int. Clin. Psychopharmacol. 29, 63–76 (2014).
Kane, J., Honigfeld, G., Singer, J. & Meltzer, H. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch. Gen. Psychiatry 45, 789–796 (1988).
Essali, A., Al-Haj Haasan, N., Li, C. & Rathbone, J. Clozapine versus typical neuroleptic medication for schizophrenia. Cochrane Database Syst. Rev. 2009, CD000059 (2009).
Leucht, S. et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 382, 951–962 (2013).
Wilson, W. H. & Claussen, A. M. 18-month outcome of clozapine treatment for 100 patients in a state psychiatric hospital. Psychiatr. Serv. 46, 386–389 (1995).
Gee, S. H., Shergill, S. S. & Taylor, D. M. Factors associated with changes in hospitalisation in patients prescribed clozapine. J. Psychopharmacol. 30, 819–825 (2016).
Vanasse, A. et al. Comparative effectiveness and safety of antipsychotic drugs in schizophrenia treatment: a real-world observational study. Acta Psychiatr. Scand. 134, 374–384 (2016).
Stroup, T. S., Gerhard, T., Crystal, S., Huang, C. & Olfson, M. Comparative effectiveness of clozapine and standard antipsychotic treatment in adults with schizophrenia. Am. J. Psychiatry 173, 166–173 (2016).
Taylor, D. M. Clozapine for treatment-resistant schizophrenia: still the gold standard?. CNS Drugs 31, 177–180 (2017).
Li, X. H. et al. The prevalence of agranulocytosis and related death in clozapine-treated patients: a comprehensive meta-analysis of observational studies. Psychol. Med. 50, 583–594 (2020).
Myles, N. et al. Meta-analysis examining the epidemiology of clozapine-associated neutropenia. Acta Psychiatr. Scand. 138, 101–109 (2018).
Bachmann, C. J. et al. International trends in clozapine use: a study in 17 countries. Acta Psychiatr. Scand. 136, 37–51 (2017).
Oloyede, E. et al. Clozapine haematological monitoring for neutropenia: a global perspective. Epidemiol. Psychiatr. Sci. 31, e83 (2022).
Oloyede, E. et al. Benign ethnic neutropenia: an analysis of prevalence, timing and identification accuracy in two large inner-city NHS hospitals. BMC Psychiatry 21, 502 (2021).
Oloyede, E. et al. There is life after the UK clozapine central non-rechallenge database. Schizophr. Bull. 47, 1088–1098 (2021).
Clozapine tablet, orally disintegrating. Daily Med https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=6fccf4f7-2e30-4272-9800-225aaef20584 (National Library of Medicine, 2023).
Kelly, D. L., Kane, J. M., Love, R. C. & Cotes, R. O. FDA eliminates the clozapine REMS—what comes next?. JAMA Psychiatry 82, 751–752 (2025).
Haddy, T. B., Rana, S. R. & Castro, O. Benign ethnic neutropenia: what is a normal absolute neutrophil count? J. Lab. Clin. Med. 133, 15–22 (1999).
Atallah-Yunes, S. A., Ready, A. & Newburger, P. E. Benign ethnic neutropenia. Blood Rev. 37, 100586 (2019).
Legge, S. E. et al. The Duffy-null genotype and risk of infection. Hum. Mol. Genet. 29, 3341–3349 (2020).
Duchene, J. et al. Atypical chemokine receptor 1 on nucleated erythroid cells regulates hematopoiesis. Nat. Immunol. 18, 753–761 (2017).
Hysong, M. R. et al. Characterization of the phenotypic consequences of the Duffy-null genotype. Blood Adv. 9, 1452–1462 (2025).
Fioredda, F. et al. The European guidelines on diagnosis and management of neutropenia in adults and children: a consensus between the European Hematology Association and the EuNet-INNOCHRON COST action. Hemasphere 7, e872 (2023).
Reich, D. et al. Reduced neutrophil count in people of African descent is due to a regulatory variant in the Duffy antigen receptor for chemokines gene. PLoS Genet. 5, e1000360 (2009).
Reiner, A. P. et al. Genome-wide association study of white blood cell count in 16,388 African Americans: the Continental Origins and Genetic Epidemiology Network (COGENT). PLoS Genet. 7, e1002108 (2011).
Charles, B. A. et al. Analyses of genome wide association data, cytokines, and gene expression in African-Americans with benign ethnic neutropenia. PLoS ONE 13, e0194400 (2018).
Legge, S. E. et al. A genome-wide association study in individuals of African ancestry reveals the importance of the Duffy-null genotype in the assessment of clozapine-related neutropenia. Mol. Psychiatry 24, 328–337 (2019).
Constantinescu, A. E. et al. A genome-wide association study of neutrophil count in individuals associated to an African continental ancestry group facilitates studies of malaria pathogenesis. Hum. Genomics 18, 26 (2024).
Cutbush, M. & Mollison, P. L. The Duffy blood group system. Heredity 4, 383–389 (1950).
Howes, R. E. et al. The global distribution of the Duffy blood group. Nat. Commun 2, 266 (2011).
Maheshwari, A. & Killeen, R. B. Duffy Blood Group System (StatPearls, 2024).
The All of Us Research Program Genomics Investigators. Genomic data in the All of Us Research Program. Nature 627, 340–346 (2024).
Whiskey, E., Olofinjana, O. & Taylor, D. The importance of the recognition of benign ethnic neutropenia in black patients during treatment with clozapine: case reports and database study. J. Psychopharmacol. 25, 842–845 (2011).
Oloyede, E. et al. Relaxation of the criteria for entry to the UK Clozapine Central Non-Rechallenge Database: a modelling study. Lancet Psychiatry 9, 636–644 (2022).
Aziri, H., Vallianatou, K., Balgobin, B. & Taylor, D. Genetic identification of undiagnosed benign ethnic neutropenia in patients receiving clozapine treatment. Br. J. Psychiatry 227, 533–537 (2025).
Wu, S. et al. Safety of BEN guidelines in clozapine treatment: a Canadian perspective. Schizophr. Res. 264, 451–456 (2024).
Miura, G. et al. Clinical outcomes after clozapine discontinuation in patients with schizophrenia: a systematic review. Pharmacopsychiatry 55, 181–192 (2022).
Masuda, T., Misawa, F., Takase, M., Kane, J. M. & Correll, C. U. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry 76, 1052–1062 (2019).
Masdrakis, V. G. & Baldwin, D. S. Prevention of suicide by clozapine in mental disorders: systematic review. Eur. Neuropsychopharmacol. 69, 4–23 (2023).
College Report CR237—The Role of Genetic Testing in Mental Health Settings (Royal College of Psychiatrists, 2023).
Taylor, D. M., Barnes, T. R. & Young, A. H. The Maudsley Prescribing Guidelines in Psychiatry 15th edn (Wiley, 2025).
Kelly, D. L. et al. Clozapine underutilization and discontinuation in African Americans due to leucopenia. Schizophr. Bull. 33, 1221–1224 (2007).
Munro, J. et al. Active monitoring of 12,760 clozapine recipients in the UK and Ireland. Beyond pharmacovigilance. Br. J. Psychiatry 175, 576–580 (1999).
Cho, J. et al. Clozapine and all-cause mortality in treatment-resistant schizophrenia: a historical cohort study. Acta Psychiatr. Scand. 139, 237–247 (2019).
Vermeulen, J. M. et al. Clozapine and long-term mortality risk in patients with schizophrenia: a systematic review and meta-analysis of studies lasting 1.1–12.5 years. Schizophr. Bull. 45, 315–329 (2019).
Land, R. et al. The impact of clozapine on hospital use: a systematic review and meta-analysis. Acta Psychiatr. Scand. 135, 296–309 (2017).
Blackman, G. & Oloyede, E. Clozapine discontinuation withdrawal symptoms in schizophrenia. Ther. Adv. Psychopharmacol. 11, 20451253211032053 (2021).
Moncrieff, J. Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse. Acta Psychiatr. Scand. 114, 3–13 (2006).
Borison, R. L., Diamond, B. I., Sinha, D., Gupta, R. P. & Ajiboye, P. A. Clozapine withdrawal rebound psychosis. Psychopharmacol. Bull. 24, 260–263 (1988).
Meltzer, H. Y., Lee, M. A., Ranjan, R., Mason, E. A. & Cola, P. A. Relapse following clozapine withdrawal: effect of neuroleptic drugs and cyproheptadine. Psychopharmacology 124, 176–187 (1996).
Blackman, G. et al. Reducing the risk of withdrawal symptoms and relapse following clozapine discontinuation—is it feasible to develop evidence-based guidelines?. Schizophr. Bull. 48, 176–189 (2022).
Oloyede, E. et al. The lived experience of clozapine discontinuation in patients and carers following suspected clozapine-induced neutropenia. BMC Psychiatry 23, 413 (2023).
Rappoport, N. et al. Correlation between ‘ACKR1/DARC null’ polymorphism and benign neutropenia in Yemenite Jews. Br. J. Haematol. 170, 892–895 (2015).
Jain, D. et al. Genome-wide association of white blood cell counts in Hispanic/Latino Americans: the Hispanic Community Health Study/Study of Latinos. Hum. Mol. Genet. 26, 1193–1204 (2017).
Dinardo, C. L. et al. Duffy null genotype or Fy(a-b-) phenotype are more accurate than self-declared race for diagnosing benign ethnic neutropenia in Brazilian population. Int. J. Lab. Hematol. 39, e144–e146 (2017).
Kelly, D. L. et al. Clozapine and neutrophil response in patients of African descent: a six-month, multinational, prospective, open-label clinical trial. Schizophr. Res. 268, 312–322 (2024).
Richardson, C. M. et al. Evaluation of the safety of clozapine use in patients with benign neutropenia. J. Clin. Psychiatry 77, e1454–e1459 (2016).
Meyer, J. M. & Stahl, S. M. The Clozapine Handbook: Stahl’s Handbooks (Cambridge Univ. Press, 2019).
Taylor, C., Marsh-Davies, A., Skelly, R., Archibald, N. & Jackson, S. Setting up a clozapine service for Parkinson’s psychosis. BJPsych Adv. 28, 90–98 (2022).
Friedman, J. H. Clozapine is severely underused in Parkinson’s disease patients. Mov. Disord. Clin. Pract. 9, 1021–1024 (2022).
Aitchison, K. J. & Kerwin, R. W. Cost-effectiveness of clozapine. A UK clinic-based study. Br. J. Psychiatry 171, 125–130 (1997).
Hayhurst, K. P., Brown, P. & Lewis, S. W. The cost-effectiveness of clozapine: a controlled, population-based, mirror-image study. J. Psychopharmacol. 16, 169–175 (2002).
Meltzer, H. Y. et al. Cost effectiveness of clozapine in neuroleptic-resistant schizophrenia. Am. J. Psychiatry 150, 1630–1638 (1993).
Jin, H., Tappenden, P., MacCabe, J. H., Robinson, S. & Byford, S. Evaluation of the cost-effectiveness of services for schizophrenia in the UK across the entire care pathway in a single whole-disease model. JAMA Netw. Open 3, e205888 (2020).
Butler, E. et al. Real-world clinical and cost-effectiveness of community clozapine initiation: mirror cohort study. Br. J. Psychiatry 221, 740–747 (2022).
Labour Force Survey: Population Aged 16-64: All: Thousands (Office for National Statistics, 2025).
Kirkbride, J. B. et al. Incidence of schizophrenia and other psychoses in England, 1950-2009: a systematic review and meta-analyses. PLoS ONE 7, e31660 (2012).
Census 2021. Ethnic Group, England and Wales: Census 2021 (Office for National Statistics, 2022).
Census 2021. Main Statistics Ethnicity Tables (Northern Ireland Statistics and Research Agency, 2022).
Scotland’s Census 2022. Ethnic Group, National Identity, Language and Religion (National Records of Scotland, 2022).
Shraga, R. et al. Evaluating genetic ancestry and self-reported ethnicity in the context of carrier screening. BMC Genet. 18, 99 (2017).
Mathieson, I. & Scally, A. What is ancestry? PLoS Genet. 16, e1008624 (2020).
Jin, H. et al. Cost and health impacts of adherence to the National Institute for Health and Care Excellence schizophrenia guideline recommendations. Br. J. Psychiatry 218, 224–229 (2021).
Rajagopal, S. Clozapine, agranulocytosis, and benign ethnic neutropenia. Postgrad. Med. J. 81, 545–546 (2005).
Inflation Calculator https://www.bankofengland.co.uk/monetary-policy/inflation/inflation-calculator (Bank of England, 2024).
Acknowledgements
Funding received by the authors has not influenced the content of this review. The below lists relevant funding for the authors. This study was funded by the following: the Medical Research Council (G1100583, MR/W020238/1, MR/Z504816/1), the National Institute for Health and Care Research (NIHR200756), Mental Health Research UK John Grace QC Scholarship 2018, an Economic Social Research Council’s co-funded doctoral award (ES/P000592/1), a British Medical Association Margaret Temple Fellowship, a Medical Research Council New Investigator and Centenary Award (G0901310) and the NIHR Biomedical Research Centre at University College London Hospitals NHS Foundation Trust and University College London (BRC1114/MH). A.R.-B. is funded by the Wellcome Trust through a PhD Fellowship in Mental Health Science (218497/Z/19/Z). This research was funded in whole or in part by the Wellcome Trust. For the purposes of open access, the authors have applied a CC BY public copyright licence to any author accepted manuscript (AAM) version arising from this submission. M.P. is supported by funding from the Economic and Social Research Council, the Medical Research Council, the NHS Genomics Unit, the NHS Race and Health Observatory, Health Data Research UK, the National Institute for Health and Care Research, the EU Innovative Medicines Initiative, Innovate UK and MC Diagnostics. N.B. is funded for one programmed activity per week by North Thames Genomic Medicine Service Alliance (Great Ormond Street Hospital) for a Mental Health Lead role. S.R. and R.J.H. are supported by the National Institute for Health and Care Research (NIHR) University College London Hospitals Biomedical Research Centre. Work in Cardiff University by J.T.R.W., A.F.P. and S.E.L. was supported by a Medical Research Council Program grant (MR/Y004094/1), and the Brain and Genomics Hub of the Mental Health Platform (MR/Z503745/1). We thank F. Smith and D. Rees from King’s College Hospital (London, UK) for kindly providing us with a cost estimate for a locally offered ACKR1 genetic test.
Author information
Authors and Affiliations
Contributions
S.M. contributed to conceptualization, formal analysis, methodology, project administration, visualization and writing (original draft). D.M. contributed to conceptualization, methodology, project administration, visualization and writing (original draft). N.S.K. contributed to conceptualization, methodology and writing (review and editing). M.C., L.V., A.R.-B., R.A., N.B., D.C., S.C., Y.D., J.d.V., F.E., S.E.L., A. Martin, A. McQuillin, D.P., A.F.P., M.R.-B., J.S., A.S., O.S., A.F.P., J.T.R.W., J.W., B.C. and S.G. contributed to conceptualization and writing (review and editing). R.J.H. and S.R. contributed to writing (review and editing). S.S.-S., M.P., H.J. and O.D. contributed to conceptualization, methodology and writing (review and editing). D.A.H. contributed to conceptualization, formal analysis, methodology and writing (review and editing). E.B. contributed to conceptualization, methodology, project administration, resources, supervision and writing (review and editing).
Corresponding authors
Ethics declarations
Competing interests
D.A.H. is Chair of the National Pharmacogenomics Group for NHS Wales and co-chair of the Pharmacogenomics Test Evaluation Group for NHS England. J.T.R.W. has received funding for research and consultancy work unrelated to this manuscript from Akrivia Health and funding for work unrelated to this manuscript from Takeda Pharmaceuticals. M.P. is Advisory Board Chair for Bosch Health Foundation (Stuttgart, Germany), Vice Chair for Qatar Precision Health Initiative, Chair for the Commission on Human Medicines, Medical Trustee for the British Heart Foundation, Council Member for the Medical Research Council and Chair for the Prix Galien Foundation UK. E.B. is a member of the Pharmacogenomics Test Evaluation Group for NHS England and a member of the NHS England National Genomics Education Programme GeNotes Mental Health Working Group. S.M. is a member of the NHS England National Genomics Education Programme GeNotes Mental Health Working Group. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Jose Rubio, Hiroyoshi Takeuchi and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Source Data
Source data file for Table 3
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Murtough, S., Mills, D., Khani, N.S. et al. ACKR1 genetic testing should be offered before starting clozapine treatment. Nat. Mental Health 4, 30–41 (2026). https://doi.org/10.1038/s44220-025-00554-9
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44220-025-00554-9