Abstract
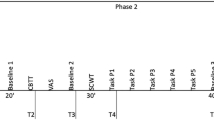
Depression is a major mental health concern among adolescents, and adverse childhood experiences (ACEs) are known risk factors. However, how depression affects the recall of ACEs remains unclear. Using three waves of data from 6,260 Chinese adolescents in the Developmental & Emotional Pathways in Transition to Adulthood Study, we examine the bidirectional relationship between depression and ACE recall. Depression was assessed with the Beck Depression Inventory-II and ACEs with an adapted ACE scale, controlling for sociodemographic factors. Random intercept cross-lagged panel model analyses show that, within individuals, baseline depressive symptoms predict increased subsequent recall of ACEs, whereas ACE recall did not predict later depression. Cross-lagged panel network analysis identified punishment feelings, fatigue and emotional neglect as key nodes linking depression and ACE recall. These findings indicate that depression can reshape autobiographical memory of adversity, probably via negative emotional processing and memory bias. This highlights the need to account for depression-driven distortions when assessing trauma history, and suggests that alleviating depressive symptoms may reduce trauma-related distress.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data supporting the main findings of this study are available from the corresponding author upon reasonable request, subject to compliance with the laws of the People’s Republic of China and approval from the Human Research Ethics Committees of South China Normal University. The data are not publicly available owing to their sensitive nature and the potential for identification, which could compromise research participant privacy.
Code availability
The R code used for data processing and statistical analyses in this study has been deposited in Zenodo and is publicly available for replication purposes (https://doi.org/10.5281/zenodo.17649422)95. No custom algorithms were developed, and all analyses were conducted using standard functions from publicly available R packages.
Change history
21 January 2026
In the version of the article initially published, in the Acknowledgements section, the last digit was inadvertently omitted from the Research Center for Brain Cognition and Human Development, Guangdong, China grant no. 2024B0303390003 which has now been corrected in the HTML and PDF versions of the article.
References
Shorey, S., Ng, E. D. & Wong, C. H. J. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and meta-analysis. Br. J. Clin. Psychol. 61, 287–305 (2022).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 175, 1142–1150 (2021).
Hua, Z., Wang, S. & Yuan, X. Trends in age-standardized incidence rates of depression in adolescents aged 10–24 in 204 countries and regions from 1990 to 2019. J. Affect. Disord. 350, 831–837 (2024).
Akee, R., Copeland, W. & Simeonova, E. Child mental health, family circumstance, and long-term success: the effect of household income. J. Hum. Resour. 59, S77–S107 (2024).
Okońska, A. et al. Risk factors for depression in adolescents. Qual. Sport 39, 58314 (2025).
Zhou, X. & Zhen, R. How do physical and emotional abuse affect depression and problematic behaviors in adolescents? The roles of emotional regulation and anger. Child Abuse Negl. 129, 105641 (2022).
Li, S., Zhao, F. & Yu, G. Childhood emotional abuse and depression among adolescents: roles of deviant peer affiliation and gender. J. Interpers. Violence 37, NP830–NP850 (2022).
Kobrinsky, V. & Siedlecki, K. L. Mediators of the relationship between adverse childhood experiences (ACEs) and symptoms of anxiety, depression, and suicidality among adults. J. Child Adolesc. Trauma 16, 233–246 (2023).
Yang, J. Z. et al. Effect of adverse childhood experiences on hypothalamic-pituitary-adrenal (HPA) axis function and antidepressant efficacy in untreated first episode patients with major depressive disorder. Psychoneuroendocrinology 134, 105432 (2021).
Vyas, N. et al. Systematic review and meta-analysis of the effect of adverse childhood experiences (ACEs) on brain-derived neurotrophic factor (BDNF) levels. Psychoneuroendocrinology 151, 106071 (2023).
Snyder, K. S., Luchner, A. F. & Tantleff-Dunn, S. Adverse childhood experiences and insecure attachment: the indirect effects of dissociation and emotion regulation difficulties. Psychol. Trauma Theory Res. Pract. Policy 16, S20–S27 (2024).
Elrefaay, S. M. M. & Elyzal, A. S. Adverse childhood experiences and depression: the mediating role of resilience and emotional regulation. J. Psychosoc. Nurs. Ment. Health Serv. 62, 45–54 (2024).
Baldwin, J. R., Reuben, A., Newbury, J. B. & Danese, A. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry 76, 584–593 (2019).
Cohen, R. T. & Kahana, M. J. A memory-based theory of emotional disorders. Psychol. Rev. 129, 742–776 (2022).
Richards, J. M. & Gross, J. J. Emotion regulation and memory: the cognitive costs of keeping one’s cool. J. Pers. Soc. Psychol. 79, 410–424 (2000).
Vaish, A., Grossmann, T. & Woodward, A. Not all emotions are created equal: the negativity bias in social-emotional development. Psychol. Bull. 134, 383–403 (2008).
Dalgleish, T. & Hitchcock, C. Transdiagnostic distortions in autobiographical memory recollection. Nat. Rev. Psychol. 2, 166–182 (2023).
Danese, A. & Widom, C. S. Objective and subjective experiences of child maltreatment and their relationships with psychopathology. Nat. Hum. Behav. 4, 811–818 (2020).
Zhang, Z. et al. Frailty and depressive symptoms in relation to cardiovascular disease risk in middle-aged and older adults. Nat. Commun. 16, 6008 (2025).
Li, K. et al. The ripple effect: unveiling the bidirectional relationship between negative life events and depressive symptoms in medical cadets. Psychol. Res. Behav. Manag. 16, 3399–3412 (2023).
Núñez-Regueiro, F., Juhel, J., Bressoux, P. & Nurra, C. Identifying reciprocities in school motivation research: a review of issues and solutions associated with cross-lagged effects models. J. Educ. Psychol. 114, 945–965 (2022).
Marciano, L., Schulz, P. J. & Camerini, A.-L. How do depression, duration of internet use and social connection in adolescence influence each other over time? An extension of the RI-CLPM including contextual factors. Comput. Hum. Behav. 136, 107390 (2022).
Wu, T. C.-H., Lloyd, A., Viding, E. & Fearon, P. Examining longitudinal associations between interpersonal outcomes and general psychopathology factors across preadolescence using random intercept cross-lagged panel model. J. Child Psychol. Psychiatry 66, 932–945 (2025).
Ashbaugh, A. R., Marinos, J. & Bujaki, B. The impact of depression and PTSD symptom severity on trauma memory. Memory 26, 106–116 (2018).
Wheatley, J., Hackmann, A. & Brewin, C. in A Casebook of Cognitive Therapy for Traumatic Stress Reactions (ed. Grey, N.) 94–108 (Routledge, 2009).
Griffith, J. W. et al. Effects of childhood abuse on overgeneral autobiographical memory in current major depressive disorder. Cogn. Ther. Res. 40, 774–782 (2016).
LeMoult, J. & Gotlib, I. H. Depression: a cognitive perspective. Clin. Psychol. Rev. 69, 51–66 (2019).
Clark, H. Depression and Narrative: Telling the Dark (Univ. of New York Press, 2008).
Nesi, J. et al. Emotional responses to social media experiences among adolescents: longitudinal associations with depressive symptoms. J. Clin. Child Adolesc. Psychol. 51, 907–922 (2022).
Li, C. et al. The role of self-esteem and emotion regulation in the associations between childhood trauma and mental health in adulthood: a moderated mediation model. BMC Psychiatry 23, 241 (2023).
Giano, Z. et al. ACE domains and depression: investigating which specific domains are associated with depression in adulthood. Child Abuse Negl. 122, 105335 (2021).
Iob, E., Lacey, R., Giunchiglia, V. & Steptoe, A. Adverse childhood experiences and severity levels of inflammation and depression from childhood to young adulthood: a longitudinal cohort study. Mol. Psychiatry 27, 2255–2263 (2022).
Falkenström, F. Time-lagged panel models in psychotherapy process and mechanisms of change research: methodological challenges and advances. Clin. Psychol. Rev. 110, 102435 (2024).
Wickersham, A. et al. Systematic review and meta-analysis: the association between child and adolescent depression and later educational attainment. J. Am. Acad. Child Adolesc. Psychiatry 60, 105–118 (2021).
Gariépy, G., Honkaniemi, H. & Quesnel-Vallée, A. Social support and protection from depression: systematic review of current findings in western countries. Br. J. Psychiatry 209, 284–293 (2016).
Kraft, L., Ebner, C., Leo, K. & Lindenberg, K. Emotion regulation strategies and symptoms of depression, anxiety, aggression, and addiction in children and adolescents: a meta-analysis and systematic review. Clin. Psychol. Sci. Pract. 30, 485–502 (2023).
Ye, C., Ye, B. & Zhang, Z. The relationship between unpredictability in childhood and depression among college students: the mediating roles of coping style and resilience. BMC Psychol. 12, 333 (2024).
Madigan, S. et al. Adverse childhood experiences: a meta-analysis of prevalence and moderators among half a million adults in 206 studies. World Psychiatry 22, 463–471 (2023).
Malhi, G. S. & Mann, J. J. Depression. Lancet 392, 2299–2312 (2018).
Weissman, M. M. & Klerman, G. L. Gender and depression. Trends Neurosci. 8, 416–420 (1985).
Frost, D. M. & Meyer, I. H. Minority stress theory: application, critique and continued relevance. Curr. Opin. Psychol. 51, 101579 (2023).
Rivas-Koehl, M., Rivas-Koehl, D. & McNeil Smith, S. The temporal intersectional minority stress model: reimagining minority stress theory. J. Fam. Theory Rev. 15, 706–726 (2023).
Kundakovic, M. & Rocks, D. Sex hormone fluctuation and increased female risk for depression and anxiety disorders: from clinical evidence to molecular mechanisms. Front. Neuroendocrinol. 66, 101010 (2022).
Albert, P. R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 40, 219–221 (2015).
Kappel, R. H., Livingston, M. D., Patel, S. N., Villaveces, A. & Massetti, G. M. Prevalence of adverse childhood experiences (ACEs) and associated health risks and risk behaviors among young women and men in Honduras. Child Abuse Negl. 115, 104993 (2021).
Melo, S., Guedes, J. & Mendes, S. in Encyclopedia of Gerontology and Population Aging (eds Gu, D. & Dupre, M. E.) 1–8 (Springer, 2019).
Dannefer, D. Cumulative advantage/disadvantage and the life course: cross-fertilizing age and social science theory. J. Gerontol. B Psychol. Sci. Soc. Sci. 58, P327–P337 (2003).
Houtepen, L. C. et al. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: a prospective cohort study in the UK. PLoS Med. 17, e1003031 (2020).
Buckman, J. E. J. et al. Socioeconomic indicators of treatment prognosis for adults with depression: a systematic review and individual patient data meta-analysis. JAMA Psychiatry 79, 406–416 (2022).
Brinker, J. & Cheruvu, V. K. Social and emotional support as a protective factor against current depression among individuals with adverse childhood experiences. Prev. Med. Rep. 5, 127–133 (2017).
Gallo, L. C., Bogart, L. M., Vranceanu, A.-M. & Matthews, K. A. Socioeconomic status, resources, psychological experiences, and emotional responses: a test of the reserve capacity model. J. Pers. Soc. Psychol. 88, 386–399 (2005).
González, L. et al. Poverty, social exclusion, and mental health: the role of the family context in children aged 7–11 years INMA mother-and-child cohort study. Eur. Child Adolesc. Psychiatry 32, 235–248 (2023).
Stordal, E., Mykletun, A. & Dahl, A. A. The association between age and depression in the general population: a multivariate examination. Acta Psychiatr. Scand. 107, 132–141 (2003).
Zhang, Z. et al. Application of DASS-21 in Chinese students: invariance testing and network analysis. BMC Public Health 24, 2934 (2024).
Daescu, A.-M. C. et al. The paradox of sexual dysfunction observed during pregnancy. Healthcare (Basel) 11, 1914 (2023).
Beck, A. T., Steer, R. A. & Carbin, M. G. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin. Psychol. Rev. 8, 77–100 (1988).
Snoek, A., McGeer, V., Brandenburg, D. & Kennett, J. Managing shame and guilt in addiction: a pathway to recovery. Addict. Behav. 120, 106954 (2021).
Stuewig, J. & McCloskey, L. A. The relation of child maltreatment to shame and guilt among adolescents: psychological routes to depression and delinquency. Child Maltreat. 10, 324–336 (2005).
Sekowski, M. et al. The relations between childhood maltreatment, shame, guilt, depression and suicidal ideation in inpatient adolescents. J. Affect. Disord. 276, 667–677 (2020).
Pust, G. E. A. et al. Association of fatigue severity with maladaptive coping in multiple sclerosis: a data-driven psychodynamic perspective. Front. Neurol. 12, 652177 (2021).
Zhao, J., Sun, X. & Wang, Q. Emotional neglect and depressive symptoms of left-behind adolescents: the role of friendship quality and gender. J. Affect. Disord. 295, 377–383 (2021).
Hanson, J. L., Hariri, A. R. & Williamson, D. E. Blunted ventral striatum development in adolescence reflects emotional neglect and predicts depressive symptoms. Biol. Psychiatry 78, 598–605 (2015).
Sahle, B. W. et al. How much do adverse childhood experiences contribute to adolescent anxiety and depression symptoms? Evidence from the longitudinal study of Australian children. BMC Psychiatry 24, 289 (2024).
Munder, T. et al. Is psychotherapy effective? A re-analysis of treatments for depression. Epidemiol. Psychiatr. Sci. 28, 268–274 (2019).
Cuijpers, P. et al. Interpersonal psychotherapy for depression: a meta-analysis. Am. J. Psychiatry 168, 581–592 (2011).
Lane, R. D., Ryan, L., Nadel, L. & Greenberg, L. Memory reconsolidation, emotional arousal, and the process of change in psychotherapy: new insights from brain science. Behav. Brain Sci. 38, e1 (2015).
McNally, R. J., Bryant, R. A. & Ehlers, A. Does early psychological intervention promote recovery from posttraumatic stress? Psychol. Sci. Public Interest 4, 45–79 (2003).
Christian, C. et al. A pilot, time-series investigation of depression, anxiety and eating disorder symptoms in adults experiencing major depressive symptoms: the need for eating disorder assessment and research in depression. Behav. Ther. 54, 214–229 (2023).
Yu, S. Uncovering the hidden impacts of inequality on mental health: a global study. Transl. Psychiatry 8, 98 (2018).
Moss, N. E. Gender equity and socioeconomic inequality: a framework for the patterning of women’s health. Soc. Sci. Med. 54, 649–661 (2002).
Comacchio, C., Antolini, G., Ruggeri, M. & Colizzi, M. Gender-oriented mental health prevention: a reappraisal. Int. J. Environ. Res. Public Health 19, 1493 (2022).
Parbst, M. & Wheaton, B. The effect of welfare state policy spending on the equalization of socioeconomic status disparities in mental health. J. Health Soc. Behav. 64, 336–353 (2023).
Finkelhor, D., Shattuck, A., Turner, H. & Hamby, S. A revised inventory of adverse childhood experiences. Child Abuse Negl. 48, 13–21 (2015).
Purewal, S. K. et al. Screening for adverse childhood experiences (ACEs) in an integrated pediatric care model. Zero Three 37, 10–17 (2016).
Merrin, G. J. et al. Adverse childhood experiences and bullying during adolescence: a systematic literature review of two decades. Adolesc. Res. Rev. 9, 513–541 (2024).
Senaratne, D. N. S. et al. The impact of adverse childhood experiences on multimorbidity: a systematic review and meta-analysis. BMC Med. 22, 315 (2024).
Haczkewicz, K. M. et al. Adverse childhood experiences (ACEs), resilience, and outcomes in older adulthood: a scoping review. Child Abuse Negl 168, 106864 (2024).
Beck, A. T., Steer, R. A. & Brown, G. Beck Depression Inventory–II (Pearson, 2011).
Paykani, T., Zimet, G. D., Esmaeili, R., Khajedaluee, A. R. & Khajedaluee, M. Perceived social support and compliance with stay-at-home orders during the COVID-19 outbreak: evidence from Iran. BMC Public Health 20, 1650 (2020).
Zhang, Z. et al. Gender differences in the mental symptom network of high school students in Shanghai, China: a network analysis. BMC Public Health 24, 2719 (2024).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2024).
Hirschfeld, G. & von Brachel, R. Improving multiple-group confirmatory factor analysis in R – a tutorial in measurement invariance with continuous and ordinal indicators. Pract. Assess. Res. Eval. 19, 7 (2014).
Chen, F. F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. Multidiscip. J. 14, 464–504 (2007).
Mulder, J. D. & Hamaker, E. L. Three extensions of the random intercept cross-lagged panel model. Struct. Equ. Model. Multidiscip. J. 28, 638–648 (2021).
Rosseel, Y. lavaan: an R package for structural equation modeling. J. Stat. Softw. 48, 1–36 (2012).
Hamaker, E. L., Kuiper, R. M. & Grasman, R. P. P. P. A critique of the cross-lagged panel model. Psychol. Methods 20, 102–116 (2015).
Savalei, V. & Rosseel, Y. Computational options for standard errors and test statistics with incomplete normal and nonnormal data in SEM. Struct. Equ. Model. Multidiscip. J. 29, 163–181 (2022).
Yuan, K.-H. & Bentler, P. M. 5. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociol. Methodol. 30, 165–200 (2000).
Hu, L. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 6, 1–55 (1999).
Burnham, K. P. & Anderson, D. R. Multimodel inference: understanding AIC and BIC in model selection. Sociol. Methods Res. 33, 261–304 (2004).
Epskamp, S., Cramer, A. O. J., Waldorp, L. J., Schmittmann, V. D. & Borsboom, D. qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 48, 1–18 (2012).
Friedman, J., Hastie, T. & Tibshirani, R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 33, 1–22 (2010).
Ren, L. et al. Network structure of depression and anxiety symptoms in Chinese female nursing students. BMC Psychiatry 21, 279 (2021).
Epskamp, S. & Fried, E. I. A tutorial on regularized partial correlation networks. Psychol. Methods 23, 617–634 (2018).
Zhang, Z. & Zhou, C. R scripts for CLPN and RI-CLPM analyses. Zenodo https://doi.org/10.5281/zenodo.17649422 (2025).
Acknowledgements
All funding sources have been acknowledged. This research was supported by the National Natural Science Foundation of China (grants 82201708 and 32571271 to Y.W.; grant 32371098 to Q.M.), Guangdong Basic and Applied Basic Research Foundation (grant 2025A1515011554 to Y.W.; grant 2024A1515011429 to Q.M.), Guangdong Philosophy and Social Science Foundation (grant GD25YXL09 to Y.W.), Guangzhou Philosophy and Social Sciences Planning Project (grant 2025GZYB21 to Y.W.), the Research Center for Brain Cognition and Human Development, Guangdong, China (grant 2024B0303390003 to Y.W.), and the Striving for the First-Class, Improving Weak Links and Highlighting Features (SIH) Key Discipline for Psychology at South China Normal University. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Z.Z. and C.Z. contributed to conceptualization, methodology, formal analysis, visualization, writing of the original draft, and review and editing. R.Z. contributed to validation, and review and editing. Y.T. contributed to visualization, and review and editing. Y.Z. contributed to data curation and resources. P.Q. provided supervision and contributed to the methodology. B.S. provided supervision and resources. Y.W. contributed to conceptualization, supervision, funding acquisition and resources.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Farah Harb, Sofia Orellana, Dajung Sung and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–7 and Figs. 1–5
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Zhou, C., Zhang, R. et al. Depression shapes the recall of adverse childhood experiences: evidence from a three-wave longitudinal study of 6,260 Chinese adolescents. Nat. Mental Health (2026). https://doi.org/10.1038/s44220-025-00580-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44220-025-00580-7