Abstract
Haptic pulse reproduction technology enables physicians to conduct remote, contact-free pulse diagnosis by transcending temporal and spatial constraints in traditional medical practice. However, current systems face challenges in accurately reproducing realistic pulse haptic feedback, which impacts diagnostic reliability. Here, we developed an electroosmotic hydraulic-based pulse haptic reproduction interface (PHRI) system that can precisely reproduce realistic haptic information of the human pulse. This PHRI system demonstrates the rapid response and precise control of electroosmotic hydraulics, achieving a frequency response of 500 Hz and an output force of 100 mN at 160 V driving voltage. Besides, time-domain and frequency-domain analyses further confirm high accuracy, with a correlation coefficient of 0.99 between reproduced and actual pulses. When tested under varying pressures, the PHRI system shows a small root mean square error of <1 Pa in frequency spectra. This PHRI technology provides a robust platform for remote pulse diagnosis and advances the integration of traditional Chinese medicine with telemedicine systems.

Similar content being viewed by others
Introduction
As a historical medical system, traditional Chinese medicine (TCM) employs pulse diagnosis that plays a significant role in clinical practice. With the development of modern telemedicine technology, pulse detection and pulse haptic reproduction are two key technologies in TCM pulse diagnosis. Currently, many studies focus on pulse detection, and this area has developed relatively mature techniques1,2; however, research on pulse haptic reproduction remains scarce. Therefore, it is necessary to develop a pulse haptic reproduction interface (PHRI) system to realize the modernization and remote application of TCM pulse diagnosis3,4. Such technology aims to precisely reproduce patients’ pulse waveforms, allowing physicians to conduct remote diagnoses without physical contact. This pulse reproduction technology proves particularly valuable in remote healthcare settings, especially for patients with limited mobility.
In the past decade, many efforts have been made to develop haptic reproduction of pulse in TCM for remote diagnosis. Multiple PHRI systems have been reported recently. For example, a heart valve can be simulated by precisely controlling the opening and closing times of electromagnetic valves. Besides, pulses under different conditions can be replicated via regulating pressure and flow of fluid in pipelines5,6,7. Besides, voice coil motors have also been reported as actuators for pulse reproduction8,9. However, current PHRI actuators are rigid and show large dimensions, hindering their further applications in daily life10,11. Therefore, it is imperative to develop a compact PHRI based on new actuation methods, which could provide innovative support for remote pulse diagnosis.
Pulse haptic reproduction can be achieved through force-feedback interfaces that generate tactile sensations by applying controlled forces to skin, creating deformations that mimic natural pulse waveforms12. Recently, four types of force-based haptic interfaces have been reported, including (1) electromagnetic-, (2) piezoelectric-, (3) pneumatic-, and (4) hydraulic-based haptic interfaces13. (1) Electromagnetic haptic interfaces generate feedback of press and vibration via an electromagnetic actuation to produce deformation and displacement of surface14,15. An electromagnetic actuator is composed of a coil, a cavity-like support, a permanent magnet, and a handling layer16. When compared with other haptic interfaces, electromagnetic actuation exhibits better high-frequency vibrations, rapid response, larger force displacement, and stronger haptic feedback17. Nonetheless, such electromagnetic actuation shows structural rigidity and limited portability. (2) For piezoelectric-based haptic interfaces, electrical energy is converted into mechanical deformation or stress by using the inverse piezoelectric effect, which generates pressures on skin to achieve haptic feedback18,19. The commonly reported piezoelectric materials include lead zirconate titanate (PZT)20, polyvinylidene fluoride (PVDF)21, potassium niobate (KNbO3)22, and perovskite23. This haptic interface exhibits both compact dimensions and fast response time, demonstrating suitability for dynamic feedback applications24. However, this haptic interface exhibits limited displacement amplitude, typically below hundreds of micrometers even at resonance, leading to attenuated haptic feedback25. (3) Pneumatic haptic interfaces generate feedback through gas-pressure-induced deformations. However, integrating compressors and gas channels makes developing compact, lightweight wearable versions challenging26. Moreover, pneumatic haptic interfaces also suffer from slow response times, restricting their application to static, bump-like feedback through large displacements rather than dynamic scenarios27,28. (4) Hydraulic haptic interfaces utilize liquid as the transmission medium to convert pressure into mechanical force. By precisely regulating liquid volume and properties in microchannels, they deliver effective kinesthetic and tactile feedback29,30. Owing to the high density of liquid, hydraulic haptic interfaces can generate strong stretching forces, out-of-plane displacements, and pressure feedback31,32. However, these haptic interfaces require external components for liquid control and exhibit slow high-frequency response with attenuated peak-to-peak amplitudes. Safety issues also arise from the high voltages needed to activate dielectric/electrorheological fluids33,34,35. Consequently, existing force-based interfaces remain inadequate for TCM remote pulse diagnosis. To this end, it is necessary to design an efficient and effective haptic interface system for pulse, which could provide accurate haptic feedback of human pulse in a portable size.
Here, we developed an electroosmotic hydraulic-based PHRI system comprising multiple actuation units with integrated electroosmotic pumps for remote pulse diagnosis of TCM. The system accurately reproduces human pulse waveforms through electroosmotic principles. Through optimized structural design, we evaluated the actuation units’ performance using combined theoretical and experimental methods. The PHRI system achieves accurate haptic feedback reproduction by regulating driving voltage parameters. Both time-domain and frequency-domain analyses demonstrate the PHRI system’s capability for remote diagnostic applications. This work presents a prototype of the PHRI system for human pulse reproduction, which is promising for remote pulse diagnosis and facilitates the modernization of TCM.
Results and discussion
Design of electroosmotic hydraulic-based PHRI system
To sense patients’ pulse beyond spatial and temporal constraints, physicians require PHRI systems that are capable of precise pulse waveform reproduction (Fig. 1a). We developed a PHRI system based on electroosmotic hydraulic-driven elastomers, which generates hydraulic pressure via electroosmotic flow. Figure 1b illustrates the formation of an electrical double layer at solid–liquid interface when a solid material (e.g., glass fiber) contacts an ionic solution. This double layer comprises a fixed ion layer (i.e., Stern layer) and a mobile ion diffusion layer (i.e., Gouy–Chapman layer). The applied electric field drives Coulomb-force-mediated ion migration within the Gouy–Chapman layer. Through viscous coupling, this ion motion induces directional liquid movement, thus creating electroosmotic flow36.
a Concept of remote pulse diagnosis. b Principle of electroosmotic flow. c Structure and exploded view of PHRI. d Top view and output position of a PHRI. e An optical photograph of the electrode layer and via holes in the electrode layer of the electroosmotic hydraulic actuator. f Side view of electroosmotic hydraulic actuator prototype
According to electroosmosis theory, and building upon previous research32,37,38, we developed an electroosmotic hydraulic-based PHRI system. The detailed fabrication is shown in the “Methods” section. Figure 1c demonstrates the overall structure of the PHRI system. The elastic output layer deforms under hydraulic pressure generated by electroosmosis-driven upward liquid flow, which generates an actuation force and displacement. Besides, the PHRI system incorporates via-hole-embedded printed circuit boards (PCB) as upper/lower Au electrodes. Two PET layers of different thicknesses serve as rigid and spacer layers, forming a sealed cavity between the electrode and output layers. This cavity is filled with electroosmotic fluid, thus eliminates air gaps. The compact structural design of PHRI minimizes the deformation area while improving response speed. A glass fiber with a thickness of 0.2mm was used as a porous medium, which generates a large number of negative charges at the solid–liquid interface. Additionally, this glass fiber exhibits good chemical stability towards electroosmotic liquid. The bottom of PHRI is a liquid reservoir made of PET layers with different thicknesses, which is used to hold electroosmotic fluid.
In this work, we used propylene carbonate (PC, 99.7%) as an electroosmotic liquid because PC has a high dielectric constant, which enables strong polarization under an electric field and facilitates ion movement. Additionally, PC exhibits low viscosity, a wide liquid temperature range (from −48.8 to 242 °C), good chemical stability, and excellent electrical insulation. Although pure propylene carbonate itself contains no free ions, the PC liquid used in practice contains trace amounts of water or other electrolyte impurities. These trace impurities provide sufficient mobile ions to support the electroosmotic process39. The designed electroosmotic hydraulic-based PHRI is shown in Fig. 1d. The output shape is a rectangle with deformation position at the middle. The output shape can be designed in various shapes for different uses. Additionally, electrode layers of this PHRI show via holes for electroosmotic flow with a diameter of 250 μm (Fig. 1e). This PHRI shows a thickness of 3.5 mm (Fig. 1g), which shows promising application for portable devices.
To better understand the application of PHRI in remote pulse diagnosis, Fig. S1 provides a detailed illustration of signal flow and individual modules of PHRI, including Control & Drive, Electroosmotic Hydraulic Actuation, and Pulse Reproduction & Tactile Output. Regarding electrical safety, the driving voltage controller used in this work is equipped with overcurrent protection mechanisms. Additionally, when PHRI interacts with the user, there are insulating layers consisting of PET, Ecoflex, and PC liquid, all of which have breakdown voltages significantly higher than the operating drive voltage of PHRI. Detailed information on insulating materials and their dielectric properties can be found in Note S1 of Supplementary Information. These design features ensure the electrical safety of PHRI during operation.
Finite element analysis of electroosmotic flow in PHRI
The classical equation for controlling electroosmotic flow rate is Helmholtz–Smoluchowski equation36:
where \({v}_{{Eo}}\) is electroosmotic velocity; \({\varepsilon }_{0}\) and \({\varepsilon }_{f}\) are permittivities of vacuum and liquid, respectively; \({\mu }_{f}\) is viscosity of liquid; \(u\) is potential generated by surface charge density of double electric layer; and \(E\) is electric field strength. Figure 2a shows a schematic of an electroosmotic actuation unit based on the principle of electroosmotic flow, which is also the smallest actuation unit in Fig. 1c. To study the basic characteristics of this electroosmotic hydraulic actuation unit and the effects of different structural parameters on its performance, we simulated the unit using COMSOL software. Figure 2b shows the simulation structure schematic, where the layout and dimensions of the electrodes, porous membrane, and electroosmotic liquid (gray) match those in the red frame of Fig. 2a. Detailed simulation parameters are listed in Table S1 (Supplementary Information).
a An illustration of an electroosmotic actuation unit. b Simulation structure diagram. c Relationship between electric field, via hole diameter, and PCB thickness. d Electroosmotic flow rate at the central point P of the via hole at different voltages. e Electroosmotic flow rate at central point P of via hole with different diameters (r). f Volumetric flow rate of electroosmotic actuation unit with different diameters
According to Eq. 1, the electroosmotic flow rate is related to electric field strength. Therefore, the electric field distribution of electroosmotic hydraulic actuation was first simulated at different driving voltages (Fig. S2). The higher the voltage between two electrodes, the stronger the electric field strength at the central point P, which is generated by the superposition of fringe fields from horizontal and vertical electrodes. Moreover, the electric field strength at point P increases linearly with applied voltage (Fig. S3a, via hole diameter: 0.3 mm). However, at 200 V, the electric field strength decreases nonlinearly with increasing via hole diameter (Fig. S3b). Additionally, the electric field intensity at point P depends on both the via hole diameter (r) and electrode layer thickness (t). As shown in Fig. 2c, with increasing r, the field intensity rises with t. However, for smaller r values (<0.5 mm), the influence of t becomes gradually weaker at constant voltage. When r falls below 0.5 mm, t has a negligible effect on the field strength. Thus, for electroosmotic actuation units with r < 0.5 mm, the PCB thickness t can be ignored in electric field considerations.
The electroosmotic flow in the electroosmotic actuation unit was simulated by neglecting gravity, porous membrane resistance, and boundary effects. As shown in Fig. S4, the electroosmotic flow rate follows the electric field intensity pattern, with higher velocities between electrodes and lower velocities at the via hole. As shown in Fig. 2d (via hole diameter = 0.3 mm), the electroosmotic flow rate at point P exhibits a linear increase with applied voltage between electrodes. Furthermore, the electroosmotic flow rate at point P decreases with increasing via hole diameter (Fig. 2e, 200 V). Both Fig. 2d, e demonstrate consistent trends between electroosmotic flow rate and electric field intensity under varying voltages and via hole diameters, confirming their proportional relationships in Eq. 1.
The volumetric flow rate of the electroosmotic hydraulic actuation unit was further calculated from simulated velocities for different via hole diameters (Fig. 2f). A simplified 2D model was employed, yielding flow rate units of mm2 s−1 (differing from 3D conditions by a depth parameter). The results demonstrate that volumetric flow rate initially increases with via hole diameter before reaching equilibrium. This behavior occurs because larger diameters reduce the electric field intensity in the via hole, which further decreases the electroosmotic flow rate. Therefore, the volumetric flow rate, calculated by integrating electroosmotic flow velocity over the cross-section of the via hole, reaches an equilibrium state as the diameter increases.
Measurement of the output displacement of PHRI
To evaluate the practical use of the electroosmotic hydraulic-based PHRI system for TCM remote pulse diagnosis, we examined its output displacement under various operating conditions. In this work, the PHRI system featured a 6 × 6 mm output deformation area, with a 0.3 mm via hole diameter and 1.2 μm glass fiber filter paper pores. The output displacement of the PHRI actuator was measured using a laser ranging sensor (LGKG, HG-C1050-P), as shown in Fig. S5. Figure 3a shows that higher driving voltages generate greater output displacements with faster response rates, which is due to enhanced electric field strength and accelerated electroosmotic flow.
a Output displacement at various driving voltages. b PHRI with different output deformation sizes. c Output displacement of different output deformation sizes. d–h Output displacements at different frequency driving voltages with via hole diameters of d 0.4, e 0.6, f 0.8, g 1.0, and h 1.2 mm. i Comparison of peak-to-peak output displacement for different via hole diameters at different frequency driving voltages
We also measured the output displacement of PHRI with circular deformation areas (diameters: 4–6 mm) using 144 identical actuation units (Fig. 3b). Figure 3c shows the displacement response to square wave voltages. PHRI with a 4 mm deformation diameter exhibited the fastest deformation and recovery rates, as it drives the smallest area with the same number of actuation units. The PHRI with 4 mm deformation diameter was further driven by sinusoidal signals (160 V amplitude, 1–500 Hz frequency range) to evaluate its dynamic response. As shown in Fig. S6, the output displacement closely follows the driving voltage waveform without noticeable distortion at frequencies below 10 Hz. This result demonstrates the PHRI’s capability to track voltage waveforms within a certain frequency range.
Figure 3d–h presents the output displacement of PHRI with different via hole diameters at various frequency driving voltages. For a given via hole diameter, the displacement trend remains consistent across different driving frequencies. The output displacement amplitude shows minimal variation below 5 Hz but decreases at higher frequencies. Nevertheless, significant displacement output persists up to 20–30 Hz, with detectable response even at 500 Hz, demonstrating the PHRI’s capability for high-frequency pulse wave reproduction. Figure 3i shows the displacement amplitudes for different via hole diameters. At constant driving frequency, smaller diameters yield larger displacements, particularly at low frequencies.
Measurement of the output force of PHRI
Here, the force output capability of PHRI was studied, using a small force sensor (DAYSENSOR, DYZ 0–5 N, measurement accuracy: 0.5 mN) to measure the actuator’s output force (Fig. 4a). A 3D-printed base was used to fix the force sensor and a high-precision adjustable displacement stage for controlling the contact degree between the output layer and force sensor. The displacement stage was adjusted to achieve full contact between the unpowered PHRI’s output layer and the force sensor surface, maintaining a contact force below 1 mN. Due to the force sensor’s rigid surface, the PHRI’s output layer remains undeformed during both contact and operation. Consequently, the actuator’s complete output force is accurately measured by the force sensor.
a Output force measurement. b Output force at various driving voltages. c Output force with glass fiber filter paper with different pore sizes. d Output force with different via hole diameters. e Relationship between output force amplitude and via hole diameter. f Porosity of different via hole diameters
To investigate the effect of output deformation area size on the PHRI’s force output, a square wave with an amplitude of 160 V was used as driving voltage to measure the output force for different deformation areas (Fig. 4b). The results show that increasing the deformation area enhances the force output capacity, with a maximum measured force of 100 mN. This relationship arises because a larger deformation area (S) under constant electroosmotic hydraulic pressure (P) in cavity yields a greater output force (F), as described by Eq. 2
Generally, for the same volume, smaller pore sizes in the porous material create larger contact surfaces between the electroosmotic fluid and the material, resulting in more electric double layers and stronger electroosmotic actuation. However, smaller pores also increase resistance to electroosmotic flow. It is necessary to optimize the pore size to enhance the output performance of the PHRI. The output force of the PHRI based on glass fiber filter paper with pore sizes of 0.22, 0.8, 1.2, and 3 μm is shown in Fig. 4c. The experimental results indicate that maximum output force is with a pore size of 0.8 μm.
According to the simulation results, the via hole diameter in the electroosmotic actuation unit significantly impacts the output of the PHRI. Therefore, the output force of PHRI with different via hole diameters was measured, as shown in Fig. 4d, indicating that the smaller via hole diameter, the greater output force. The reason of this result is that smaller via hole diameters lead to a stronger electric field intensity at the center of the hole, as well as a higher number of electroosmotic actuation units within the PHRI. The PHRI can generate a maximum output force of 100 mN at low frequency with a driving voltage of 160 V, an output deformation of 6 mm, a glass fiber filter paper pore size of 0.8 μm, and a via hole diameter of 0.4 mm. As shown in Fig. 4e, the output force of PHRI decreases as the via hole diameter increases, consistent with the in Figs. 2e and 3i. Additionally, the small size of the box plot in Fig. 4e indicates that the PHRI’s output force remains stable at constant driving voltage. Moreover, different via hole diameters alter the overall porosity of the electrode when the electrode size and spacing between via holes are fixed. The porosity calculation method is given in Eq. S1. The porosity and number of via holes for different diameters are provided in Note S2 and Table S2. A higher porosity and smaller via hole diameter result in more via holes, which increases the number of electroosmotic actuation units and enhances actuation capability, as shown in Fig. 4f. Therefore, one effective strategy to optimize the output of PHRI is to reduce via hole diameter while increasing surface porosity.
Reproduction of pulse waveform based on PHRI
By combining simulations and experiments, we optimized and developed a PHRI system for TCM remote pulse diagnosis (Fig. 1d). The corresponding parameters are listed in Table S3. The PHRI’s diagnostic validity was assessed through reproduction experiments using nine randomly sampled pulse types from a public clinical pulse waveform database40. Each pulse signal was amplified to the same driving voltage for subsequent reproduction and analysis. The repeating frequency of all pulse waveforms was 1.5 Hz to simulate normal human pulse frequency. As shown in Fig. 5, the blue curve represents amplified driving voltage based on the actual pulse waveform, while the pink curve represents output displacement of PHRI. The output displacements closely match actual pulses. The PHRI can precisely capture and reproduce both normal and abnormal pulse waveforms, including characteristic morphological features (e.g., peaks/troughs), demonstrating good waveform reproduction capabilities.
To further evaluate the accuracy and effectiveness of PHRI, we analyzed four representative pulses (Pulses 1, 3, 5, and 9) using frequency spectrum analysis. Both the reproduced and original haptic feedback signals were processed via the one-sided Fourier transform (OSFT) method, as shown in Fig. S7. This method employs time-frequency conversion to analyze the signal’s spectral composition and energy distribution. The frequency-domain analysis demonstrates that reproduced pulses preserve the spectral characteristics of original pulses, confirming PHRI’s capability to accurately replicate fundamental frequency components of physiological pulse signals. The driving voltage and output displacement waveforms were not amplitude-compared due to signal normalization and unit differences.
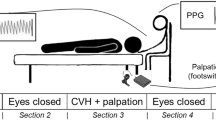
Reproduction of the actual pulse wave under different loading pressures
Physicians apply different levels of pressure with their fingers to perceive the patient’s pulse in TCM. To better reproduce the haptic feedback of pulse acting on the physicians’ fingers, the relationship between output pressure and driving voltage of PHRI needs to be established. As shown in Fig. 6a, the PHRI’s output pressure was measured using a pulse sensor (HUAKE, MB-R3) positioned between the device and a pressure loading system. A linear motor served as the loading device to apply controlled pressures on both a commercial pulse sensor and the PHRI. Since human pulse frequencies primarily are below 5 Hz, we calibrated the PHRI’s pressure-voltage relationship using 1–5 Hz sinusoidal driving voltages (Fig. 6b). The amplitude of output pressure remains relatively stable and changes with driving voltage. Figure 6c further demonstrates the linear dependence of pressure amplitude on driving voltage.
a Photo of the pressure calibration and reproduction measurement setup. b Output pressure of actuator at sinusoidal driving voltages of different frequencies. c Linear fitting of driving voltage and output pressure. d–f Haptic feedbacks of reproduced and actual pulse under static pressures of d 5040 Pa, e 9300 Pa, and f 14,420 Pa, respectively. g–i Analysis of consistency between frequency spectra of reproduced and original pulse haptic feedback under different loading pressures of g 5040 Pa, h 9300 Pa, and i 14,420 Pa, respectively
We further simulated pulse diagnosis by measuring multiple pulse signals from a healthy individual under varying applied pressures (Fig. S8). The pulse sensor simultaneously recorded applied static pressure and dynamic pulse signals as illustrated by red curves in Fig. 6d–f. The driving voltage (pink curves) for PHRI can be calculated through linear fitting from Fig. 6c based on pulse signals. The same pressure was applied to PHRI, simulating the force applied by a physician’s finger during pulse diagnosis. As shown in Fig. 6a, a commercial pulse sensor was used to detect haptic feedback of the reproduced pulse from PHRI. Figure 6d–f demonstrates the haptic feedback of reproduced pulse (blue curves) and original pulse under static pressures of 5040 Pa, 9300 Pa, and 14,420 Pa, respectively. The correlation coefficients between reproduced and original pulse haptic feedback are >0.99, indicating that the haptic feedback of reproduced pulse precisely matches the actual pulse.
To further validate consistency between reproduced and original pulse haptic feedback in the frequency domain, OSFT analysis was performed. As shown in Fig. 6g–I, the horizontal axis represents frequency components of pulses, while the vertical axis indicates corresponding pressure amplitude, which reflects the magnitude of each frequency component in pulses. Since we focus on pulses (dynamic variations), the static pressure (static component) is excluded. The reproduced and original pulse haptic feedbacks show a high consistency in their primary frequency components with correlation coefficients of >0.99 and a low root mean square (RMS) error of <1 Pa. Therefore, both time-domain and frequency-domain analyses demonstrate that the PHRI can precisely reproduce both dynamic characteristics and frequency components of original pulses, confirming its validity for remote pulse diagnosis.
Conclusion
In summary, we developed an electroosmotic hydraulic-actuated PHRI system to reproduce patients’ pulse waveforms for remote pulse diagnosis in TCM. By using finite element simulations, we first systematically analyzed the impact of various parameters on the output performance of electroosmotic hydraulic actuation. Additionally, the experimental results further validated simulation outcomes and provided an optimization strategy for this PHRI system. The PHRI prototype demonstrates a maximum response frequency up to 500 Hz without considering amplitude attenuation. The PHRI generates a maximum output force of 100 mN at 160 V in the low-frequency range. Moreover, we evaluated this PHRI’s performance by reproducing both reference pulses from an online library and actual pulses measured from a volunteer under varying pressure conditions. The PHRI system shows good waveform fidelity with a 0.99 time-domain correlation coefficient between reproduced and original pulses and <1 Pa spectral RMS error. These results confirm that the PHRI can precisely reproduce pulses and show good potential for remote pulse diagnosis. This work provides a promising tool for modernizing TCM pulse diagnosis and expanding remote healthcare services.
Methods
Materials and fabrication of PHRI
The PHRI uses an Ecoflex-30 (Smooth-On) elastic membrane as the output layer. The membrane has a thickness of 300 μm and is prepared by thoroughly mixing Ecoflex-30-A and Ecoflex-30-B in a weight ratio of 1:1, followed by spin coating. Printed circuit boards (PCBs) with via holes are used as upper/lower electrodes. A polyethylene terephthalate (PET) spacer is placed on PCB electrodes to form a cavity with the output layer, which also includes a PET board with via holes. This PET board is directly bonded to Ecoflex-30 membrane, reducing output deformation area and improving response speed. Laser-cut glass fiber filter paper is used as a porous medium, offering high porosity and chemical stability. PET spacer fills the gaps between the glass fiber filter paper and the PCB electrodes. The bottom part of the actuator is a liquid reservoir made of a thick PET board and a thin PET film, which holds electroosmotic liquid (i.e., propylene carbonate, PC) with a purity of 99.7%. All components are bonded together using 3 M double-sided tape, while the Ecoflex-30 elastic membrane is adhered to the PET board using silicone adhesive. All PET components are processed using the laser cutting method.
Experimental environmental conditions
All experiments in this work were conducted under typical room temperature and humidity conditions, which are representative of the environment in traditional Chinese pulse diagnosis. The experiments were performed at a stable ambient temperature of approximately 22–25 °C and relative humidity of 40–60%. These conditions were maintained throughout the study to ensure consistency and reliability in the performance of the PHRI system. Although fluctuations in environmental factors such as temperature and humidity may affect the performance of diagnostic systems, materials used in PHRI, including PET, Ecoflex, and electroosmotic fluid, exhibit strong stability under normal environmental conditions. Therefore, it is anticipated that the impact of such fluctuations on the system’s performance is minimal.
Power supply system
In this work, we conducted prototype testing using the power supply shown in Fig. S8. The controller (FeelTech, FY6300) provides control signals, which are amplified by a high-voltage amplifier (Credit, KDT3500) to drive the PHRI.
References
Chen, Y.-Y., Chang, R.-S., Jwo, K.-W., Hsu, C.-C. & Tsao, C.-P. A non-contact pulse automatic positioning measurement system for traditional Chinese medicine. Sensors 15, 9899–9914 (2015).
Chu, Y. et al. Human pulse diagnosis for medical assessments using a wearable piezoelectret sensing system. Adv. Funct. Mater. 28, 1803413 (2018).
Tang, A. C. Y. Review of traditional Chinese medicine pulse diagnosis quantification. Complement. Ther. Clin. Pract. 4, 61–80 (2012).
Dong, K. et al. Wearable photoelectric fingertip force sensing system based on blood volume changes without sensory interference. ACS Appl. Mater. Interfaces 15, 34578–34587 (2023).
Tang, W., Sun, H., Xu, J. & Li, B. Research on pulse simulation system of traditional Chinese medicine. Chin. J. Basic Med. Tradit. Chin. Med. 6, 105–106 (2000).
Wang, X., Wang, J., Chen, F., Shi, Q. & Li, Y. Research on teaching and testing machine for traditional Chinese medicine pulse-taking. Chin. Med. Equip. J. 28, 1–2 (2007).
Wang, X. et al. System of traditional chinese medicine pulse replay system based on multi-sensor technology. Chin. J. Sens. Actuators 26, 1604–1609 (2013).
Zhang, P., Master’s Thesis, Shanghai Jiao Tong University, China (2013).
Wang, Z., Master’s Thesis, University of Electronic Science and Technology of China, China (2019).
She, Y., Master’s Thesis, University of Electronic Science and Technology of China, China (2018).
Lv, H., Master’s Thesis, Tianjin University, China (2017).
Yu, X. et al. Skin-integrated wireless haptic interfaces for virtual and augmented reality. Nature 575, 473–479 (2019).
Huang, Y. et al. Recent advances in multi-mode haptic feedback technologies towards wearable interfaces. Mater. Today Phys. 22, 100602 (2022).
Ozioko, O., Karipoth, P., Hersh, M. & Dahiya, R. Wearable assistive tactile communication interface based on integrated touch sensors and actuators. IEEE Trans. Neural Syst. Rehabil. Eng. 28, 1344–1352 (2020).
Martínez, J., García, A., Oliver, M., Molina, J. P. & González, P. Identifying virtual 3D geometric shapes with a vibrotactile glove. IEEE Comput. Graph. Appl. 36, 42–51 (2016).
Zárate, J. J., Tosolini, G., Petroni, S., De Vittorio, M. & Shea, H. Optimization of the force and power consumption of a microfabricated magnetic actuator. Sens. Actuators A: Phys. 234, 57–64 (2015).
Zárate, J. J. & Shea, H. Using pot-magnets to enable stable and scalable electromagnetic tactile displays. IEEE Trans. Haptics 10, 106–112 (2017).
Sorgini, F. et al. Encapsulation of piezoelectric transducers for sensory augmentation and substitution with wearable haptic devices. Micromachines 8, 270 (2017).
Yeh, C.-H. et al. Application of piezoelectric actuator to simplified haptic feedback system. Sens. Actuators A: Phys. 303, 111820 (2020).
Kimura, M., Ando, A., Maurya, D. & Priya, S. Advanced Piezoelectric Materials. (Woodhead Publishing, Cambridge, UK, 2017).
Stadlober, B., Zirkl, M. & Irimia-Vladu, M. Route towards sustainable smart sensors: ferroelectric polyvinylidene fluoride-based materials and their integration in flexible electronics. Chem. Soc. Rev. 48, 1787–1825 (2019).
Maeder, M. D., Damjanovic, D. & Setter, N. Lead free piezoelectric materials. J. Electroceram. 13, 385–392 (2004).
Liao, W.-Q. et al. A molecular perovskite solid solution with piezoelectricity stronger than lead zirconate titanate. Science 363, 1206–1210 (2019).
Zhu, M. et al. Haptic-feedback smart glove as a creative human-machine interface (HMI) for virtual/augmented reality applications. Sci. Adv. 6, eaaz8693 (2020).
Seo, I.-T. et al. Multilayer piezoelectric haptic actuator with CuO-modified PZT-PZNN ceramics. Sens. Actuators A Phys. 238, 71–79 (2016).
Low, J. H. et al. Hybrid tele-manipulation system using a sensorized 3-D-printed soft robotic gripper and a soft fabric-based haptic glove. IEEE Robot. Autom. Lett. 2, 880–887 (2017).
Wu, X., Kim, S. H., Zhu, H., Ji, C. H. & Allen, M. G. A refreshable braille cell based on pneumatic microbubble actuators. J. Microelectromech. Syst. 21, 908–916 (2012).
Yao, L. et al. PneUI: pneumatically actuated soft composite materials for shape changing interfaces. The 26th annual ACM symposium on User interface software and technology 13–22 (2013).
Mazursky, A., Koo, J.-H. & Yang, T.-H. Design, modeling, and evaluation of a slim haptic actuator based on electrorheological fluid. J. Intell. Mater. Syst. Struct. 30, 2521–2533 (2019).
Acome, E. et al. Hydraulically amplified self-healing electrostatic actuators with muscle-like performance. Science 359, 61–65 (2018).
Leroy, E., Hinchet, R. & Shea, H. Multimode hydraulically amplified electrostatic actuators for wearable haptics. Adv. Mater. 32, 2002564 (2020).
Shultz, C. & Harrison, C. Flat panel haptics: embedded electroosmotic pumps for scalable shape displays. CHI Conference on Human Factors in Computing Systems 1–16 (2023).
Rumley, E. H. et al. Biodegradable electrohydraulic actuators for sustainable soft robots. Sci. Adv. 9, eadf5551 (2023).
Kim, H., Ma, J., Kim, M., Nam, J. & Kyung, K.-U. High-output force electrohydraulic actuator powered by induced interfacial charges. Adv. Intell. Syst. 3, 2100006 (2021).
Acome et al. Hydraulically amplified self-healing electrostatic actuators with muscle-like performance. Science 359, 61–65 (2018).
Kirby, B. J. in Micro- and Nanoscale Fluid Mechanics: Transport in Microfluidic Devices. (ed B. J. Kirby) (Cambridge University Press, Cambridge, UK, 2012), pp 131–152.
Rae-Grant, T., Harrison, C. & Shultz, C. DynaButtons: fast interactive soft buttons with analog control. 2024 IEEE Haptics Symposium (HAPTICS) pp 366–371 (2024).
Shen, V., Rae-Grant, T., Mullenbach, J., Harrison, C. & Shultz, C. Fluid reality: high-resolution, untethered haptic gloves using electroosmotic pump arrays. Proceedings of the 36th Annual ACM Symposium on User Interface Software and Technology Article 8 (2023).
Sritharan, D., Chen, A. S., Aluthgama, P., Naved, B. & Smela, E. Bubble-free electrokinetic flow with propylene carbonate. Electrophoresis 36, 2622–2629 (2015).
Charlton, P. H. et al. Modeling arterial pulse waves in healthy aging: a database for in silico evaluation of hemodynamics and pulse wave indexes. Am. J. Physiol.317, H1062–H1085 (2019).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant No. 21927808).
Author information
Authors and Affiliations
Contributions
K.D. and W.D. conceived the idea and designed the research. F.T. supervised this work. K.D., Y.L. and T.F. constructed the experimental platform. K.D., W.D. and X.T. performed the research and analyzed the data. K.D., X.Y., X.W., H.L. and F.T. discussed the data and prepared the paper. All authors discussed and reviewed the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dong, K., Deng, W., Liu, Y. et al. Electroosmotic hydraulic-based haptic reproduction of human pulse with high accuracy for remote diagnosis. Microsyst Nanoeng 11, 173 (2025). https://doi.org/10.1038/s41378-025-01042-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41378-025-01042-x