Abstract
The American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) have recently issued updated guidelines on human epidermal growth factor receptor 2 (HER2) testing by fluorescence in situ hybridization (FISH) in invasive breast cancers. Cases with a HER2/chromosome enumeration probe 17 (CEP17) ratio of ≥2.0 but an average HER2 copy number of <4.0 signals per cell (ISH group 2) are no longer automatically classified as ISH positive. Herein, 30 cases in ISH group 2 were collected. Another 100 patients with a HER2/CEP17 ratio <2.0 and <4.0 HER2 signals per cell (ISH group 5) and 100 patients with a HER2/CEP17 ratio of ≥2.0 and an average HER2 copy number of ≥4.0 signals per cell (ISH group 1) were also recruited for comparison. According to the 2018 ASCO/CAP guidelines, all the cases in ISH group 2 were categorized as HER2 negative. The clinicopathological characteristics of the patients in ISH group 2 were intermediate between ISH group 1 and group 5. Survival analyses revealed that there was no significant disease-free survival (DFS) and overall survival (OS) difference between patients with or without targeted therapy in ISH group 2, as well as between patients with targeted therapy in ISH group 1 and patients in ISH group 2. Patients without targeted therapy in ISH group 2 had a significantly worse OS than patients with targeted therapy in ISH group 1 and patients in ISH group 5. In conclusion, patients in ISH group 2 represent a biologically heterogeneous subset, which are different from those in ISH group 1 and 5. A larger cohort of patients in ISH group 2 should be included for future researches to define the efficacy of HER2-targeted therapy.
Similar content being viewed by others
Introduction
Breast cancer is the most frequently diagnosed cancer and the leading cause of cancer death in females worldwide [1]. Overexpression of human epidermal growth factor receptor 2 (HER2) protein, mainly due to HER2 gene amplification, is reported in ~15–20% of breast cancers [2,3,4,5]. HER2 positivity is associated with poor prognosis [5,6,7]. Clinical trials have demonstrated that anti-HER2 targeted therapy can yield remarkable survival benefits in breast cancer patients with HER2-overexpression [8,9,10,11]. Therefore, it is of utmost importance to accurately assess HER2 status in breast cancer patients.
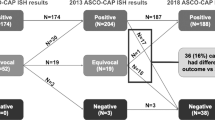
Two technologies, immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH), are routinely used to determine HER2 status. To ensure the accuracy, reproducibility, and precision of HER2 testing, the American Society of Clinical Oncology (ASCO) and College of American Pathologists (CAP) have periodically issued and updated the recommendations for conducting and interpreting HER2 testing [12,13,14]. In the latest version, five clinical questions have been addressed. Clinical question 3 focused on invasive breast cancers with a HER2/chromosome enumeration probe 17 (CEP17) ratio of ≥2.0 but an average HER2 copy number of <4.0 signals per cell (ISH group 2), which were considered ISH positive in 2013 recommendations [13, 14]. According to 2018 ASCO/CAP guidelines, a definitive diagnosis will be rendered based on additional workup. IHC testing for HER2 should be performed on sections from the same tissue samples used for FISH test. Cases with IHC 3+ and 1+/0 will be assigned as HER2 positive and negative respectively. Another observer, blinded to previous ISH results, should reevaluate the FISH slides in cases scored IHC 2+. If the results remain unchanged, diagnosis will be HER2 negative with a comment. Otherwise, the results should be adjudicated per internal procedures to define the final category [14].
Patients with this ISH pattern represent a less common subgroup of breast cancers. There are too few such cases to arrive at a definitive conclusion on the anti-HER2 targeted therapy efficacy. Owing to the limited data on the clinicopathological features, prognosis and outcome of this group of patients, we collected 30 breast cancer cases in ISH group 2 from January 2009 to February 2019 and compared with cases with a HER2/CEP17 ratio of ≥2.0 and an average HER2 copy number of ≥4.0 signals per cell (ISH group 1) and cases with a HER2/CEP17 ratio <2.0 and <4.0 HER2 signals per cell (ISH group 5) during the same period.
Materials and methods
Case cohort
Thirty breast cancer cases in ISH group 2 from January 2009 to February 2019 were recruited in the study. Meanwhile, 100 cases in ISH group 1 and 100 cases in ISH group 5 during the same period were also randomly collected. Clinicalpathological characteristics were retrieved from pathology reports. Follow-up data were obtained from telephone interview. The follow-up period ranged from 6 months to 10 years. This study was approved by the Ethics Committee of the First Affiliated Hospital, College of Medicine, Zhejiang University. The Committee waived the need for informed consents because the study was completed anonymously. All experiments were performed in accordance with relevant guidelines and regulations.
IHC
Automated IHC for HER2 (Rabbit, clone 4B5; Ventana Medical Systems, Tucson, AZ) was performed on 4-μm-thick tissue sections using an automated slide stainer, the Ventana Benchmark XT (Ventana Medical Systems). IHC staining for HER2 was categorized according to the 2018 guidelines.
FISH
Four-um-thick tissue sections were deparaffinized, rehydrated, and immersed in distilled water for 40 min at above 90 °C. The slides were incubated for 18 min in protease solution at 37 °C. After dehydration with alcohol, HER2/CEP17 mixture probe (Registration of national machinery 20153401702, Beijing Jinpujia Medical Technology Co., Ltd, China) was applied to the slides. The slides were then transferred to a hybridization oven (S500–24, Abbott molecular, USA). The procedure was as follows: denature at 83 °C for 5 min, and hybridization overnight at 42 °C. Next day, the slides were washed in preheated post-hybridization buffer, air dried, and then counterstained with DAPI. HER2 FISH signals were interpreted by one technologist (BW) and one pathologist (KS). Thirty nuclei from two nonoverlapping areas were counted. When there was a conflict between the scores, another pathologist (XLW) would review the slide and reach the final result. The 2018 guidelines were applied for the interpretation of FISH testing results.
Statistical analysis
Statistical analyses were performed using SPSS for Windows version 22.0. Comparisons of the clinicopathological features between the three groups were analyzed by χ2 test or Fisher’s exact test. Disease-free survival (DFS) was defined as the interval between pathological diagnosis to the date of relapse or metastasis. Overall survival (OS) was calculated from the date of pathological diagnosis to death by any cause or the date of the last follow-up. Survival analysis was estimated by the Kaplan–Meier method, and significance was determined by the log-rank test. P values <0.05 were considered to be statistically significant.
Results
Clinicopathological features of patients in ISH group 2
The age of patients ranged from 28 to 74 years, with the mean age of 51.4 years. Specimens came from surgical excisions (n = 26) and core needle biopsies (n = 4). There were 29 invasive ductal carcinomas (Fig. 1a) and 1 invasive micropapillary carcinoma (Fig. 1b). Tumor size could be recorded in 26 surgical excision samples, 53.3% (n = 16) of which was more than 2 cm. Twelve cases were WHO grade II and 14 were WHO grade III. The estrogen receptor (ER) and progesterone receptor (PR) positive rate was 66.7% (n = 20) and 53.3% (n = 16) respectively. Lymph node involvement was detected in 12 cases. The clinicopathological details of the patients in ISH group 2 were summarized in Table 1.
a HE staining of a sample with invasive ductal carcinoma in ISH group 2. The tumor showed invasive growth. The tumor cells were arranged in adenoid and nest-like clusters. The tumor cells were atypical, with increased nuclear-plasma ratio and thicker chromatin. Nucleoli and mitotic images were visible (200×). b HE staining of a sample with invasive micopapillary carcinoma in ISH group 2. The tumor cells were in cleft like retraction spaces. The tumor cells were arranged in micropapillary pattern, with abundant eosinophilic cytoplasm (200×). c A representative image of IHC staining in ISH group 2 after a repeated test using the same tissue section applied for FISH assay. More than 10% of the tumor cells showed weak to moderate complete membrane staining. According to the 2018 ASCO/CAP guidelines, this case was interpreted as IHC 2+(200×). d A representative image of FISH after a second FISH reading in a case with IHC 2+. The result showed no change, with a HER2/CEP17 ratio of 2.74 compared with a HER2/CEP17 ratio of 2.71 from original test. The average HER2 copy number per cell was 3.47, while it was 1.27 for CEP17 (Red: HER2; Green: CEP17) (1000×).
Reclassification of cases in ISH group 2
IHC staining for HER2 were performed using sections from the same tissue samples applied for FISH test. The number of cases scored as IHC 0, 1+, and 2+ was 8, 15, and 7 respectively (Table 2, Fig. 1c). After a second FISH reading in 7 cases with IHC 2+, the results showed no change (Table 2, Fig. 1d). Based on the 2018 guidelines, all the cases in this group were categorized as HER2 negative.
Comparison of the clinicopathological features between the three groups
The mean age of the patients in each group was 51 years old. Almost all the cases from the three groups were invasive ductal carcinoma. WHO grade III was predominant in ISH group 1 (59.0%) and group 2 (46.7%), while WHO grade II was more common in ISH group 5 (53.0%). Compared with patients in ISH group 5, patients in ISH group 1 and group 2 usually had larger tumor size (p < 0.05). Lymph node involvement was more common for cases in ISH group 1, followed by cases in ISH group 2 and group 5. The difference of ER expression between the three groups was significant, with the highest positive rate in ISH group 5. This was also the case for PR expression among the three groups (Table 1).
Survival analysis for the three groups
During the follow-up, of the 66 patients receiving HER2-targeted therapy in ISH group 1, eight developed local recurrence (n = 3), lymph node metastasis (n = 1), bone metastasis (n = 1) or lung metastasis (n = 3). Twelve patients died of breast cancer. For patients in ISH group 2, one of nine patients receiving HER2-targeted therapy had lymph node metastasis, and one of the other 21 patients without targeted therapy had local relapse. Four patients without targeted therapy died of breast cancer. With regard to the patients in ISH group 5, four developed local relapse and six had metastasis (lung metastasis n = 3; bone metastasis n = 2; multiple metastasis n = 1). Moreover, seven died of breast cancer. 34 cases in ISH group 1 and 36 cases in ISH group 5 were excluded from the following comparisons due to the missing data on the treatment or failure for follow-up.
Survival analyses revealed that there was no significant DFS and OS difference for patients with or without targeted therapy in ISH group 2 (Figs. 2 and 3).
Kaplan–Meier disease-free survival (DFS) curves showing no significant DFS difference between patients with targeted therapy and without targeted therapy in ISH group 2 (p = 0.719), as well as patients with targeted therapy in ISH group 1 vs patients with targeted therapy (p = 0.976) or without targeted therapy (p = 0.694) in ISH group 2, patients in ISH group 5 vs patients with targeted therapy (p = 0.742) or without targeted therapy (p = 0.586) in ISH group 2, patients with targeted therapy in ISH group 1 vs patients in ISH group 5 (p = 0.908).
Kaplan–Meier overall survival (OS) curves showing no significant OS difference between patients with or without targeted therapy in ISH group 2 (p = 0.154), as well as patients with targeted therapy in ISH group 2 vs patients with targeted therapy in ISH group 1 (p = 0.412) or patients in ISH group 5 (p = 0.315), patients with targeted therapy group 1 vs patients in ISH group 5 (p = 0.646). Patients without targeted therapy in ISH group 2 had a worse OS compared with patients with targeted therapy in ISH group 1 (p=0.017) or patients in ISH group 5 (p=0.058).
Compared with the 66 patients with targeted therapy in ISH group 1, there was no significant DFS and OS difference for patients with targeted therapy in ISH group 2 (Figs. 2 and 3), but patients without targeted therapy in ISH group 2 had a worse OS (Fig. 3).
This was also the case for the survival comparisons between patients in ISH group 2 and group 5 (Figs. 2 and 3).
There was also no significant DFS and OS difference between patients with targeted therapy in ISH group 1 and patients in ISH group 5 (Figs. 2 and 3).
Discussion
In China, if a new HER2/CEP17 probe is ready to be used in clinical tests for guiding HER2-targeted therapy, the manufacturers should take concordance testing by comparing with the Food and Drug Administration (FDA) approved PathVysion test kit. Only those passing the tests can get a certificate by the China Food and Drug Administration and then their products can be used in clinical practice. In the present study, the HER2/CEP17 probe is supplied by Beijing Jinpujia Medical Technology Co., Ltd. They have passed the concordance testing in 2007, with a concordance rate more than 95% compared with the FDA approved test kit. Since then, the HER2/CEP17 probe from Beijing Jinpujia Medical Technology Co., Ltd has become one of the most widely used probes in China. In the past 10 years, we have participated in the external proficiency testing programs for breast HER2 FISH organized by Pathology Quality Control Center for five times and United Kingdom National External Quality Assessment Service for one time. We have passed all the tests. Collectively, the HER/CEP17 probe used in the present study is reliable.
Breast cancers with a HER2/CEP17 ratio of ≥2.0 but an average HER2 copy number of <4.0 signals per cell are uncommon, with an incidence ranging from 0.4 to 3.7% [15,16,17,18,19]. Thirty such cases were collected in the present study, accounting for 0.6% of all breast cancer cases diagnosed in our department, which was consistent with the reported incidence. In the 2013 recommendations, cases with this ISH pattern were considered as ISH positive [13]. Given no significant benefit from trastuzumab therapy [14, 15], the 2018 guidelines has updated the HER2 testing algorithm for patients in this group [14]. The final HER2 status will be decided by reviewing the concomitant IHC test. A study conducted by Zare et al. revealed that 11 of the 18 cases in ISH group 2 were scored as IHC 0 or 1+, 7 were 2+, and none was 3+ [20]. Liu et al. found that eight cases in this group were reclassified as negative based on the 2018 recommendations due to the low IHC score [21]. In clinical trials BCIRG-005 and 006, 35 cases were featured with a HER2/CEP17 ratio of ≥2.0 but an average HER2 copy number of <4.0 signals per cell. After retested by IHC, only three were scored as IHC 2+ but none were IHC 3+ [15]. Similarly, our data also showed that all the cases in this ISH group were categorized as negative when applying the 2018 guidelines. To date, only one case in ISH group 2 was reclassified as positive with a HER2/CEP17 ratio of 3.0 and an average HER2 copy number of 6.1 signals per cell after targeted FISH was done [22].
The patterns of HER2 ISH testing using a dual-probe assay are divided into five groups: ISH group 1, ISH group 2, ISH group 3 (HER2/CEP17 ratio of <2.0 and an average HER2 copy number of ≥6.0 signals per cell), ISH group 4 (HER2/CEP17 ratio of <2.0 and an average HER2 copy number of ≥4.0 but <6.0 signals per cell), and ISH group 5. The clinicopathological features between each group have been reported to be significantly different. Yang et al. found that the cases in ISH group 1 had higher histological grade, more frequent occurrence of negative ER and PR status, and a higher Ki67 index than cases in ISH group 5 [23]. Compared with ISH group 5, patients in ISH group 4 presented with a higher histological grade and Ki67 index but a lower histological grade and Ki67 index than patients in ISH group 1 [23]. Gordian-Arroyo et al. reported that ISH group and HER2 copy number correlated with histologic grade [24]. The tumors from ISH group 1 had the highest mean grade, followed by tumors from ISH group 3, 4, and 5 [24]. Moreover, the rate of hormone receptors (HR) positivity was significantly different between the groups. The highest HR-positive rate was present in ISH group 5 [24]. In parallel with these findings, our results also showed that tumors in ISH group 1 and 2 usually had higher WHO grade and tumor size. Lymph node involvement was more common for cases in ISH group 1, followed by cases in ISH group 2 and group 5. In addition, the differences of ER and PR expression between ISH group 1, 2, and 5 were significant, with the highest positive rates in ISH group 5. However, another study by Zare et al. could not demonstrate statistically significant differences between ISH group 1 and 2 regarding the clinicopathological parameters [20].
HER2 amplification is considered as a predictor for HER2-targeted therapy [25, 26]. Clinical trials showed that patients in ISH group 1 had improved DFS and OS when treated with trastuzumab [15]. Our results also demonstrated that patients in ISH group 1 benefited from targeted therapy, with the comparable DFS and OS as the patients in ISH group 5. In the present study, nine patients in ISH group 2 received targeted therapy. Statistical analyses showed that there was no significant DFS and OS difference between these nine patients and patients in ISH group 5. Moreover, compared with patients with targeted therapy in ISH group 1 and patients in ISH group 5, the other 21 patients without targeted therapy in ISH group 2 had a comparable DFS but a significant worse OS. All these data suggest that patients in ISH group 2 may benefit from targeted therapy. However, clinical trials BCIRG-005 and 006 reported no apparent benefit from trastuzumab therapy for patients in ISH group 2 either in terms of DFS or OS [15]. The small number of cases receiving targeted therapy and the short period of follow-up for patients in ISH group 2 in the present study may be the underlying reasons for the difference in the outcome.
In conclusion, patients in ISH group 2 represent a biologically heterogeneous subset, which are different from those in ISH group 1 and 5. A larger cohort of patients in ISH group 2 should be included for future researches to define the efficacy of HER2-targeted therapy.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer Statistics. CA: Cancer J Clin. 2011; 61:69–90.
Ross JS, Slodkowska EA, Symmans WF, Pusztai L, Ravdin PM, Hortobagyi GN. The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist. 2009;14:320–68.
Dawood S, Broglio K, Buzdar AU, Hortobagyi GN, Giordano SH. Prognosis of women with metastatic breast cancer by HER2 status and trastuzumab treatment: an institutional-based review. J Clin Oncol. 2010;28:92–8.
Hanna WM, Ruschoff J, Bilous M, Coudry RA, Dowsett M, Osamura RY, et al. HER2 in situ hybridization in breast cancer: clinical implications of polysomy 17 and genetic heterogeneity. Mod Pathol. 2014;27:4–18.
Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, et al. Studies of the HER2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244:707–12.
Gabos Z, Sinha R, Hanson J, Chauhan N, Hugh J, Mackey JR, et al. Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol. 2006;24:5658–63.
Press MF, Bernstein L, Thomas PA, Meisner LF, Zhou JY, Ma Y, et al. HER-2/neu gene amplification characterized by fluorescence in situ hybridization: poor prognosis in node-negative breast carcinomas. J Clin Oncol. 1997;15:2894–904.
Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, et al. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002;20:719–26.
Marty M, Cognetti F, Maraninchi D, Snyder R, Mauriac L, Tubiana-Hulin M, et al. Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patients with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: the M77001 study group. J Clin Oncol. 2005;23:4265–74.
Smith I, Procter M, Gelber RD, Guillaume S, Feyereislova A, Dowsett M, et al. 2-Year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet. 2007;369:29–36.
Gianni L, Dafni U, Gelber RD, Azambuja E, Muehlbauer S, Goldhirsch A, et al. Treatment with trastuzumab for 1 year after adjuvant chemotherapy in patients with HER2-positive early breast cancer: a 4-year follow-up of a randomised controlled trial. Lancet Oncol. 2011;12:236–44.
Wolff AC, Hammond MEH, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45.
Wolff AC, Hammond MEH, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JM, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline focused update. J Clin Oncol. 2018;36:2105–22.
Press MF, Sauter G, Buyse M, Fourmanoir H, Quinaux E, Tsao-Wei DD, et al. HER2 gene amplification testing by fluorescent in situ hybridization (FISH): Comparison of the ASCO-College of American Pathologists guidelines with FISH scores used for enrollment in breast cancer international research group clinical trials. J Clin Oncol. 2016;34:3518–28.
Shah MV, Wiktor AE, Meyer RG, Tenner KS, Ballman KV, Green SJ, et al. Change in pattern of HER2 fluorescent in situ hybridization (FISH) results in breast cancers submitted for FISH testing: experience of a reference laboratory using US Food and Drug Administration criteria and American Society of Clinical Oncology and College of American Pathologists guidelines. J Clin Oncol. 2016;34:3502–10.
Press MF, Villalobos I, Santiago A, Guzman R, Cervantes M, Gasparyan A, et al. Assessing the new American Society of Clinical Oncology/College of American Pathologists guidelines for HER2 testing by fluorescence in situ hybridization: experience of an academic consultation practice. Arch Pathol Lab Med. 2016;140:1250–8.
Stoss OC, Scheel A, Nagelmeier I, Schildhaus HU, Henkel T, Viale G, et al. Impact of updated HER2 testing guidelines in breast cancer re-evaluation of HERA trial fluorescence in situ hybridization data. Mod Pathol. 2015;28:1528–34.
Ballard M, Jalikis F, Krings G, Schmidt RA, Chen YY, Rendi MH, et al. ‘Nonclassical’ HER2 FISH results in breast cancer: a multiinstitutional study. Mod Pathol. 2017;30:227–35.
Zare SY, Lin L, Alghamdi AG, Daehne S, Roma AA, Hasteh F, et al. Breast cancers with a HER2/CEP17 ratio of 2.0 or greater and an average HER2 copy number of less than 4.0 per cell: frequency, immunohistochemical correlation, and clinicopathological features. Hum Pathol. 2019;83:7–13.
Liu ZH, Wang K, Lin DY, Xu J, Chen J, Long XY, et al. Impact of the updated 2018 ASCO/CAP guidelines on HER2 FISH testing in invasive breast cancer: a retrospective study of HER2 fish results of 2233 cases. Breast Cancer Res Treat. 2019;175:51–57.
Lin L, Sirohi D, Coleman JF, Gulbahce HE. American Society of Clinical Oncology/College of American Pathologists 2018 focused update of breast cancer HER2 FISH testing guidelines. Am J Clin Pathol. 2019;152:479–85.
Yang LB, Chen M, Pu TJ, Wu S, Wei B, Yang JL, et al. The differences of clinicopathologic characteristics among subgroups of reclassified HER2 fluorescence in situ hybridization (FISH) according to the ASCO/CAP 2018 breast cancer HER2 testing guidelines. J Clin Pathol. 2019; https://doi.org/10.1136/jclinpath-2019-206222.
Gordian-Arroyo AM, Zynger DL, Tozbikian GH. Impact of the 2018 ASCO/CAP HER2 guideline focused update. Am J Clin Pathol. 2019;152:17–26.
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005;353:1659–72.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365:1273–83.
Acknowledgements
We thank Jinlong Cui and Liming Xu for their contributions to immunohistochemistry staining. We also thank Mei Kong and Jun Li for their histology work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, X., Teng, X., Ding, W. et al. A clinicopathological study of 30 breast cancer cases with a HER2/CEP17 ratio of ≥2.0 but an average HER2 copy number of <4.0 signals per cell. Mod Pathol 33, 1557–1562 (2020). https://doi.org/10.1038/s41379-020-0519-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41379-020-0519-y
This article is cited by
-
A clinicopathological study and survival analysis of 99 breast cancers with HER2/CEP17 ratio ≥ 2.0 and an average HER2 copy number < 4.0 per cell in China
BMC Cancer (2023)
-
HER2 in situ hybridization test in breast cancer: quantifying margins of error and genetic heterogeneity
Modern Pathology (2021)
-
Retrospective observational study of HER2 immunohistochemistry in borderline breast cancer patients undergoing neoadjuvant therapy, with an emphasis on Group 2 (HER2/CEP17 ratio ≥2.0, HER2 copy number <4.0 signals/cell) cases
British Journal of Cancer (2021)