Abstract
Pharmacological modulation of glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) through dual GIP/GLP-1 receptor agonists, commonly used for diabetes and obesity, shows promise in reducing alcohol consumption. We applied drug-target Mendelian randomization (MR) using genetic variation at these loci to assess their long-term effects on problematic alcohol use (PAU), binge drinking, alcohol misuse classifications, liver health, and other substance use behaviors. Genetic proxies for lowered BMI, modeling the appetite-suppressing and weight-reducing effects of variants in both the GIPR and GLP1R loci (“GIPR/GLP1R”), were linked with reduced binge drinking in the primary (β = −0.44, 95% CI [−0.72, −0.15], P = 2.42 × 10−3) and replication data (β = −0.13, [−0.22, −0.04], P = 0.0058). HbA1c lowering via GIPR/GLP1R variants was associated with reduced risk of heavy drinking with psychiatric comorbidities versus low-risk drinking (odds ratio [OR] = 0.62, [0.45, 0.85], P = 0.0031), with replication in independent HbA1c data (OR = 0.71, [0.60, 0.84], P = 5.22 × 10−5) and directional consistency with reduced PAU. Analysis of individual loci indicated that both GIPR and GLP1R were protective against heavy drinking, underscoring the importance of both targets. While estimates for other substance use disorders (tobacco, cannabis, opioid) were consistently null, food preference analyses revealed that BMI lowering via GIPR/GLP1R reduced fatty food liking (β = −1.58, [−2.01, −1.14], P = 1.62 × 10−12) and increased vegetarian food liking (β = 2.08, [1.17, 2.99], P = 8.22 × 10−6), implicating metabolic and appetite regulation pathways for the alcohol consumption findings. For liver health, HbA1c lowering via GIPR/GLP1R was associated with reduced NAFLD (β = −0.34, [−0.50, −0.18], P = 2.74 × 10−5) and lower ALT levels (β = −0.26, [−0.38, −0.15], P = 8.39 × 10−6), with replication supporting these findings. Consistency across multiple MR methods and colocalization analyses strengthened causal inference. Mediation analysis suggested reductions in hazardous alcohol consumption partially explain the cardioprotective effects of these agonists. Multi-ancestry analyses supported directionally aligned relationships in non-European cohorts. These findings support further clinical exploration of GLP1R, GIPR, and dual agonists in addiction medicine.
Similar content being viewed by others
Introduction
The therapeutic potential of glucagon-like peptide-1 receptor agonists (GLP1RAs), such as semaglutide, and dual GIP receptor (GIPR)/GLP1RAs, like tirzepatide, extends beyond metabolic diseases like diabetes and obesity [1, 2]. Semaglutide has demonstrated significant benefits in reducing body weight and improving glycemic control, while tirzepatide shows enhanced cardiometabolic outcomes due to its dual mechanism of action [1, 2]. Emerging evidence suggests these therapies may also address alcohol use disorder (AUD) and other substance use disorders (SUDs), presenting an opportunity to repurpose these agents for addiction treatment [3].
There are three FDA-approved treatments for AUD [4], yet only 2.1% of individuals with a past-year AUD in the United States received medication-assisted treatment [5], underscoring a critical unmet need [6]. GLP1RAs have shown promise in reducing alcohol and drug intake through preclinical and clinical studies [7, 8]. Rodent models demonstrate GLP1RAs can diminish the rewarding effects of alcohol, nicotine, and cocaine [9,10,11], clinical trials report reduced alcohol consumption and attenuated fMRI reward-related brain activity with agents like dulaglutide and exenatide [8, 12, 13], and a recent large-scale observational study found that individuals using GLP1RAs had a lower risk of alcohol-related hospitalizations, supporting a potential role for these medications in reducing alcohol consumption and related harms [8]. The role of GIPR agonism in SUDs, while less established, is gaining attention. Preclinical evidence suggests GIPR agonism influences glucose metabolism and weight regulation [14], and tirzepatide studies indicate that GIPR agonism independently enhances insulin sensitivity and glucose disposal [15]. Furthermore, GIPR mutations have been linked to alcohol dependence [16], suggesting its relevance in addiction biology. Importantly, dual GIPR/GLP1R agonists like tirzepatide demonstrate superior metabolic efficacy compared to GLP1RAs alone [17], highlighting the potential synergistic effects of targeting both pathways.
Addiction outcomes, including AUD, share overlapping neurobiological mechanisms with food overconsumption, such as reward deficiency and craving [18]. GLP1R and GIPR agonists inhibit food intake and modulate diet preferences [19, 20], which motivates their investigation for addiction-related behaviors. This dual impact on metabolic and neurobehavioral pathways suggests these therapies may address both the calorie-sensing (i.e., nutrient reward) and substance-craving dimensions of addiction. Given the novelty of GLP1R and GIPR as drug targets and the lack of well-powered randomized controlled trials (RCTs) to assess causal relationships with AUD and other alcohol use behaviors, drug-target Mendelian randomization (MR) provides an important approach for early evidence generation [21, 22]. MR leverages genetic variants associated with drug targets as instrumental variables, offering a robust approach to infer causal relationships between target activation and clinical outcomes [23, 24]. By simulating the physiological effects of pharmacological interventions, MR can provide valuable insights into the therapeutic potential of these targets before extensive RCT data is available, accelerating the evidence base for clinical translation (Fig. 1) [21, 22].
The design for a a hypothetical RCT that investigates the impact of GIPR/GLP1R agonists on alcohol consumption behaviors, liver health, and food preferences is compared to b a drug-target MR analysis assessing the impact of genetically proxied associations of GIPR/GLP1R activity. In b, Single nucleotide polymorphisms (SNPs) located within or near the genomic loci and associated with the downstream physiological impact emulate GIPR/GLP1R therapeutics (reduced glycated hemoglobin [HbA1c] or lowered body mass index [BMI]).
We use drug-target MR [21, 22] to assess whether genetically proxied agonism of GLP1R and GIPR influences AUD and problematic alcohol use behaviors, such as binge drinking. We validate the genetically mimicked GLP1R and GIPR agonism using positive controls, extend the alcohol-related analyses by exploring associations with other SUDs and food liking behaviors, and examine markers of liver health to provide a comprehensive understanding of the clinical implications of GLP1R and GIPR agonism in alcohol-related behaviors and their consequences. Given the potential role of alcohol reduction in cardiovascular protection, we perform a mediation analysis of these pathways and coronary artery disease (CAD) risk to assess whether reductions in harmful alcohol consumption mediate the cardioprotective effects of GIPR/GLP1R agonism. Finally, we conduct exploratory analyses in non-European cohorts, which together will advance equity in precision medicine and clarify the therapeutic potential of GLP1R, GIPR, and dual GIPR/GLP1R agonists for AUD and SUDs.
Methods
Study overview
Figure 1 provides conceptual comparison between drug-target MR and RCT designs, and a study overview is presented in Fig. 2. This study is reported in accordance with the MR Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplementary Checklist) [25]. Table 1 presents the included genome-wide associate study (GWAS) data.
This study used summary-level GWAS data relating to glycated hemoglobin (HbA1c) and body mass index (BMI) to construct genetic instruments modeling GLP1R and GIPR agonism. We constructed three instrument types: one proxying GLP1R agonism; one proxying GIPR agonism; and one combined instrument proxying dual GLP1R and GIPR agonism. Each instrument type included multiple exposure sources mimicking the expected physiological responses to pharmacological modulation of the targets (lowered glycated hemoglobin [HbA1c], reduced body mass index [BMI], and GLP1R or GIPR gene expression in the cortex). Instrument sets for each BMI and HbA1c exposure were constructed in two independent GWAS summary statistics (UK Biobank [plus GIANT for BMI] and the Million Veterans Program [MVP]). After instrumentation and validation with the primary clinical indications for GLP1R and GIPR agonism (type 2 diabetes and obesity), and assessing their impact on liver health, we obtained a selection of outcomes related to alcohol use disorder (AUD) and alcohol consumption behavior to assess the impact of GLP1R and GIPR agonism. We contextualized the alcohol-related analyses by analyzing other substance use disorders and investigating outcomes related to self-reported food liking. Because of the availability of large sample sizes and the most relevant endpoints, we used data from European ancestry as the main analysis set, but we also performed analyses using East Asian and African ancestry data sources. Finally, for all drug-target MR estimates demonstrating evidence of a relationship (main drug-target MR method P < 0.05), we performed colocalization analyses to assess evidence of shared causal variants between the biomarker exposures and outcomes in the GLP1R and GIPR genomic loci. MR Mendelian Randomization, GLP1R Glucagon-like peptide-1 receptor, GIPR glucose-dependent insulinotropic polypeptide receptor, NAFLD Non-alcoholic fatty liver disease, ALD Alcohol-related liver disease, SNP Single nucleotide polymorphism, BMI Body mass index.
Genetically modeling GLP1R and GIPR analogs
We instrument GLP1R and GIPR using glycated hemoglobin (HbA1c) levels (mmol/mol) and body mass index (BMI) data because these traits capture the core biological and clinical effects of their agonists: HbA1c reflects glucose-lowering effects, as GLP-1 and GIP regulate insulin secretion and glucagon suppression, improving glycemic control. Clinically, GLP1RAs (e.g., semaglutide) and dual GIPR/GLP1R agonists (e.g., tirzepatide) significantly reduce HbA1c [26], making it a useful proxy for their metabolic impact. Similarly, BMI serves as a proxy for appetite suppression and weight loss, two hallmark effects of GLP1R agonists and dual agonists [27]. GLP1R activation reduces food intake via central appetite regulation and delayed gastric emptying, while GIPR co-activation enhances fat metabolism and energy expenditure [27]. Given that these drugs are primarily used for diabetes and obesity, instrumenting the GLP1R and GIPR using HbA1c and BMI in MR allows us to approximate their long-term physiological effects in real-world settings.
Primary instrument construction
To construct our primary instruments for European ancestry analyses, we applied cis-instrumentation strategies, selecting genetic variants within the locus of each drug target [22]. For GLP1R agonism, we used independent (linkage disequilibrium R² < 0.1), genome-wide significant (P < 5 × 10−8) SNPs located ±500 kilobases of the GLP1R locus (chromosome 6:39,016,574–39,055,519 on GRCh37/hg19) and associated with HbA1c levels (mmol/mol) in UK Biobank European ancestry participants. GIPR and GLP1R instruments were also separately constructed using BMI GWAS data, capturing their impact on appetite suppression and weight loss. For Europeans, we used a meta-analysis of GIANT and UK Biobank summary statistics [28]. Since no genome-wide significant BMI-associated variants were found within the GLP1R locus, we applied a relaxed P-threshold of 5 × 10−6, a strategy commonly used in cis-instrument MR studies when conventional genome-wide significant variants are absent [29, 30]. To model the effects of dual GLP1R and GIPR agonists (e.g., tirzepatide [31]), we combined the primary HbA1c and BMI instruments for GLP1R and GIPR into single instruments capturing both loci. The genetic models concatenating the glucose-lowering effects from both GLP1R and GIPR loci or BMI impact is denoted as “GIPR/GLP1R” for the remainder of the manuscript. To further validate the robustness of our findings, we used the Million Veterans Program (MVP) [32] GWAS summary statistics for BMI and HbA1c to perform replication analyses by instrumenting GLP1R, GIPR, and dual agonists in these biomarker data.
In addition to using two independent GWAS data sources per exposure to test robustness and consistency of the estimates, we also conducted sensitivity analyses using alternative instruments to evaluate potential pleiotropy, test for bias in instrument selection, and confirm that findings remain consistent across multiple instrument definitions [21, 22]. First, we constructed instruments for GLP1R, GIPR, and dual GIPR/GLP1R agonism by identifying SNPs that were associated with GLP1R and GIPR gene expression in the Genotype-Tissue Expression (GTEx) Project V8 eQTL dataset [33]. Lookups were performed separately for both GLP1R and GIPR, ensuring that selected variants were relevant for each receptor’s gene regulation. Second, we created additional GLP1R and GIPR instruments from the HbA1c and BMI GWAS data using missense SNPs (rs10305420 for GLP1R and rs1800437 for GIPR [rs1800437 was only extracted from BMI data because it was not present in the HbA1c data), identified using the VariantAnnotation R package (version 3.20) [34]. Finally, we constructed cis-instruments for GLP1R and GIPR reflecting gene expression changes in the brain cortex [35], evaluating potential effects on central nervous system regulation.
For the exploratory non-European ancestry analyses, we leveraged ancestry-specific datasets to construct GLP1R and GIPR genetic instruments. For East Asian ancestry, we used Biobank Japan (HbA1c N = 42,790; BMI N = 158,284) [36], identifying cis-acting variants within the GLP1R and GIPR loci to model the glycemic and metabolic effects of agonism. For African ancestry, we used data from the UK Biobank Pan-UKB release (HbA1c N = 5,901; BMI N = 6,458) constructed by the Neale Lab [27], applying similar cis-instrumentation strategies to approximate pharmacological modulation of these targets. All instruments used ancestry-specific 1000 Genomes panels [37].
Genetic instruments interpretation
Drug-target MR instruments aim to capture the lifelong expected physiological impact of the target of interest (here, GLP1R and GIPR agonism through genetic variants associated with BMI and HbA1c levels) [21, 22]. Importantly, the reported association findings are not confined to individuals with specific BMIs or Hba1c levels. Rather, they reflect the relationships of GLP1R and GIPR activity as inferred from the instruments genetically proxied effects on BMI and glycemic control. These instruments are constructed using variants that are associated with BMI and HbA1c within the GIPR and GLP1R loci, which serve as proxies for the therapeutic effects of drug targets that act through these pathways. Therefore, the findings are linked to changes in BMI or HbA1c due to the metabolic and appetite-regulating mechanisms of GLP1R and GIPR agonism. This approach allows for the assessment of drug target activity over the lifelong genetic exposure, rather than short-term clinical intervention, providing insights into the broader implications of GLP1R and GIPR modulation beyond metabolic regulation [21, 22].
Instrument validation
To validate the instruments, we assessed their associations with both type 2 diabetes (T2D) and obesity for each genetically proxied GLP1R, GIPR, and dual GIPR/GLP1R agonism exposure, ensuring they captured expected metabolic effects [31, 38, 39]. Our primary validation comparisons examined whether HbA1c-based instruments for GLP1R and GIPR agonism were associated with T2D risk and whether BMI-based instruments for GLP1R and GIPR agonism were associated with obesity risk, given these are the primary clinical effects of these pathways. However, we also tested all exposure-outcome pairs, including whether BMI-based instruments were associated with T2D and whether HbA1c-based instruments were associated with obesity, to fully characterize metabolic impacts. T2D effects were assessed using GWAS data from European, East Asian (88,109 cases/339,395 controls), and African (N = 50,251 cases/103,909 controls) populations [40]. Obesity associations were evaluated using European ancestry GWAS data from FinnGen release 11 [41], though comparable datasets were not available for East Asian or African populations. The expected associations confirm that these instruments appropriately capture the glycemic effects (via HbA1c) and weight-regulatory effects (via BMI) of GLP1R and GIPR agonism, supporting their validity for causal inference in alcohol-related and metabolic trait analyses.
Estimation of ancestry-specific activation allele prevalence
Because effect‐allele frequencies at GIPR and GLP1R vary across populations, estimating ancestry-specific carrier rates of activation alleles helps anticipate differential baseline receptor engagement and guide trial design [42, 43]. We estimated the proportion of individuals in each 1000 Genomes super-population (EUR, EAS, AFR) carrying at least one “activation” allele at our GIPR and GLP1R cis-instrument loci. Per-SNP carrier probabilities Pcarrier = 1 − (1−f)2 were combined across independent instruments to yield locus-level estimates (Plocus), then averaged to produce an overall ancestry-specific prevalence. Full computational details and formulae are provided in the Supplementary Methods.
Outcome data
Alcohol consumption
We curated a comprehensive set of alcohol-related outcomes to evaluate the therapeutic potential of GLP1R and GIPR agonism. The primary analysis focused on problematic alcohol use (PAU), defined by Zhou et al. through meta-analysis of AUD cases combined with Alcohol Use Disorders Identification Test (AUDIT) problem drinking scores (AUDIT-P, questions 7–10) from the UK Biobank [44]. Non-European ancestry analyses, restricted to AUD diagnoses, included East Asian (N = 7,364) and African (N = 122,024) populations. Additionally, we assessed distinct alcohol consumption behaviors to capture broader drinking patterns and misuse: weekly alcohol intake (grams/day; European N = 666,978; East Asian N = 90,852; African N = 8,078) [45], binge drinking frequency using AUDIT Question 3 (“How often do you have more than 6 drinks/occasion?”) [27], and weekly drinking [45]. Self-reported drinking behaviors were further stratified by drinking status (current, former, or lifetime abstainer), changes in drinking behavior over the past decade (increased, decreased, or stable), and typical drinking frequency (days per month) [46]. We also incorporated alcohol misuse classes identified via latent class analysis of 410,961 UK Biobank participants [46]. This classification model identified four groups: low risk, internalizing-light/non-drinkers, heavy alcohol use–low impairment, and broad high risk [46]. These classifications allowed for detailed exploration of how GLP1R and GIPR activity may differentially impact drinking behaviors associated with both low-risk and problematic use. Finally, we examined relationships with other substance use disorders (SUDs), including tobacco use disorder (TUD) [46], cannabis use disorder (CUD) [47], and opioid use disorder (OUD) [48], to explore broader addiction-relevant effects of GLP1R and GIPR modulation. See Table S1 and Supplementary Methods for more details.
Liver health
We analyzed six liver-related outcomes, including alcohol-related liver disease (ALD) from FinnGen (ICD10 code K70) [41], liver enzymes (alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase [ALP], and gamma-glutamyl transferase [GGT]) from the UK Biobank [27, 49, 50], and non-alcoholic fatty liver disease (NAFLD) from a recent meta-analysis [51]. NAFLD diagnoses were based on ICD-10 codes, excluding confounding conditions like ALD, liver transplantation, and hepatitis [51]. This GWAS included 8,464 NAFLD cases, with a prevalence of ~1%, below global estimates (~25%) [51, 52], likely reflecting underdiagnosis and some misclassification. To improve resolution, we integrated the NAFLD GWAS with liver fat percentage data (N = 33,235) [53] using Multi-Trait Analysis of GWAS (MTAG) [54], which jointly analyzed the traits. MTAG steps included filtering variants (MAF > 0.1%), merging datasets, calculating genetic covariance using LD Score regression (Supplementary Methods) [55], and annotating multi-trait GWAS results with Functional Mapping and Annotation (FUMA v1.5.2) [56] (Figures S1–S3). We refer to the combined multi-trait outcome as NAFLD throughout this manuscript.
Food liking
We used GWASs from the UK Biobank food liking questionnaire, which assessed responses to 139 food and drink items using a 9-point Hedonic scale (1 = “Extremely dislike” to 9 = “Extremely like”), with additional options for “Have never tried it” and “Prefer not to answer“ [57]. May-Wilson et al. conducted these GWASs and identified 45 multivariate food liking factors, capturing the genetic architecture of related traits (e.g., fatty food liking, vegetable liking, sweet food liking) that were used in our analyses (Table S1).
Statistical analysis
MR has 3 core assumptions: (1) the MR instruments are associated with the exposure (“relevance”); (2) there is no common cause between the genetic instruments and the outcome (“exchangeability”); and (3) the genetic instruments do not have a direct impact on the outcome (“exclusion restriction”) [21]. The first assumption was evaluated by calculating the proportion of variance explained and F-statistics for each instrument SNP [21, 58], which provides information regarding the potential for the results to be impacted by weak instrument bias (F-statistic >10 conventionally indicates minimal weak instrument bias), and also the additional instruments comprised of either SNPs with known biological function (missense SNPs), or have corresponding relationships with GLP1R or GIPR expression. Wald ratio [59] and inverse variance weighted (IVW) were used as the primary methods for analyses with 1 SNP instruments and 2 + SNP instruments, respectively [59]. Heterogeneity (Cochran’s Q) and MR Steiger directionality tests investigated evidence of pleiotropic SNPs and reverse causality [59]. For instruments with 3+ SNPs, complementary methods (MR-Egger, weighted median, weighted mode) were also used.
The exclusion restriction assumption was assessed with colocalization, which evaluates shared genetic architecture between the exposure-outcome pairs at the loci of interest [60]. Colocalization was performed for MR estimates with P < 0.05 to investigate shared causal variants between exposure and outcome traits at the GLP1R and GIPR loci. Complete methodological details are provided in the Supplementary Methods. Briefly, using the coloc R package (version 5.2.2) [61], we calculated posterior probabilities for five genetic association configurations, assuming a single causal variant per locus. Evidence for a shared causal variant was defined as a posterior probability for H4 (PP.H4) > 0.60, with default prior probabilities (p1 = p2 = 1 × 10−4; p12 = 1 × 10−5). For cases with weak outcome signals (low H3 and H4 but high H1), an alternate H4 ratio (H4/(H3 + H4)) was calculated, as applied in prior drug-target MR studies [60].
All MR and colocalization analyses were performed using the TwoSampleMR [62] (version 6.9) and coloc [62] R packages (version 5.2.1) in R version 4.2.2.
Interpretation of results
Estimates reflect a 1 SD decrease in HbA1c (mmol/L) or BMI (kg/m²), or increased GIPR/GLP1R expression. Binary and categorical outcomes (e.g., AUD, T2D, alcohol groups) are reported as ORs with 95% CIs, where ORs <1 indicate reduced odds and ORs >1 indicate increased odds. Continuous outcomes (e.g., PAU, binge drinking, liver enzymes, liver fat, food liking) are reported as β coefficients, reflecting changes per 1 SD decrease in BMI or HbA1c. For instance, a β = −0.34 for liver fat indicates a 0.34% reduction per 1 SD decrease in HbA1c, while an OR = 0.62 indicates a 38% lower likelihood of heavy drinking vs. light drinking from genetically proxied dual agonism.
Multiple testing and replication
We applied a Bonferroni-corrected threshold of 0.0025 (0.05/20) to account for testing across 20 alcohol, liver, and food liking outcomes. Given the use of independent exposure data for both BMI and HbA1c, we also highlight findings where there was evidence of at least P < 0.05 and consistent directional effects across both primary and replication analyses. While we caution against over-reliance on strict P-value thresholds [63], we use this correction as a heuristic to enable follow-up on a manageable number of findings. Our study leverages two biomarkers—BMI and HbA1c—to capture distinct physiological effects of GLP1R and GIPR agonism, with each biomarker instrumented using two separate GWAS summary statistic sources (primary and replication) of European ancestry (Table 1). By evaluating each receptor’s effects on BMI and HbA1c separately and replicating findings across these independent datasets for each exposure, we provide consistent, cross-validated evidence supporting their metabolic benefits. This dual-source approach strengthens the robustness of our findings and underscores the reproducibility of genetic estimates.
Mediation of the cardioprotective impact of GIPR/GLP1R agonism through alcohol consumption
Given the strong protective relationships observed with heavy drinking behavior and the well-documented links between these drinking behaviors and cardiovascular disease [64,65,66], we investigated whether reductions in alcohol consumption mediate the cardioprotective effects of GLP1R and GIPR agonism on coronary artery disease (CAD) risk using two-step MR [67] and the product of coefficients mediation method [67]. Given evidence that the cardioprotective effects of GLP1R agonism primarily operate through BMI reduction rather than glycemic modulation, we hypothesized that BMI-related instrument sets would show the strongest protective effects on CAD. We screened the main GLP1R and GIPR instruments for relationships with CAD risk and alcohol consumption traits, identifying lowered BMI via GIPR and combined GIPR/GLP1R as relevant instruments. Using the Aragam et al. CAD meta-analysis [68] and genome-wide independent SNPs for binge drinking frequency, we estimated causal relationships with CAD risk through inverse-variance weighted MR, MR-Egger, weighted median, and MR-LASSO to account for heterogeneity and pleiotropy. Mediation was quantified using the product of coefficients method, revealing that reductions in binge drinking explained a proportion of the protective effects of GIPR/GLP1R agonism on CAD risk. See the Supplementary Methods for full methodological details.
Results
Instrument validation
The F-statistics for SNPs used to proxy GLP1R and GIPR activity ranged from 19.07 to 436.91 (Table S2), confirming that weak instrument bias was unlikely to affect the findings [21, 58]. For GLP1R agonism, genetically proxied lower BMI by GLP1R variants was consistently associated with a reduced risk of obesity, with relationships observed for GLP1R agonism in the MVP BMI replication data and a directionally consistent, though less precise, estimate in the primary BMI GWAS data (Figure S4a-b, Table S3). Lower HbA1c via GLP1R was also linked to a lower T2D risk, with nearly identical effect sizes across the primary and replication datasets (Figure S4c). For GIPR agonism, genetically proxied lower BMI via GIPR showed a robust association with reduced obesity risk, with highly similar effect sizes across the two exposure datasets. Similarly, lower HbA1c by GIPR was protective against T2D, with effect estimates demonstrating excellent agreement between the two datasets. Colocalization analyses supported shared causal variants at the GIPR locus, particularly for T2D (PP.H4 = 0.98 for HbA1c levels in both the primary and replication exposure datasets) (Table S4), reinforcing the metabolic role of GIPR activation. Finally, for combined GIPR/GLP1R agonism, lower BMI through dual receptor activation resulted in a substantial reduction in obesity risk, with highly concordant estimates across datasets. Likewise, lower HbA1c via both GIPR and GLP1R loci was associated with a reduced T2D risk. Across all analyses, results were consistent across datasets and robust to sensitivity analyses, confirming that the associations observed were not driven by any single genetic approach.
Receptor-activating allele prevalence across ancestries
Across all populations, receptor‐activating alleles at both GIPR and GLP-1R loci are highly prevalent, but with modest ancestry‐specific variation (Table S5). In Europeans, per‐locus carrier probabilities (Plocus) for GIPR instruments ranged from 0.82 to 1.00 (average EAFs 0.42–0.56) and for GLP1R from 0.72 to 1.00 (average EAFs=0.38–0.70). In East Asians, the 10‐SNP GIPR–BMI instrument was universal, i.e., every individual is expected to carry at least one variant, (Plocus = 1.00; average EAF = 0.55), whereas single‐SNP HbA1c instruments were carried by 46% at GIPR (average EAF = 0.46; Plocus = 0.71) and 25% at GLP1R (average EAF = 0.25; Plocus = 0.44). Among Africans, multi‐SNP GLP-1R instruments for both BMI and HbA1c were universal (Plocus = 1.00; average EAFs ≈ 0.52–0.58), while the 3‐SNP GIPR–HbA1c set was carried by 79% (average EAF = 0.21). These subtle differences in baseline “agonist” allele carriage may inform dose–response expectations and safety monitoring in future multi‐ancestry trials.
Genetically proxied GLP1R and GIPR analogs impact binge drinking and alcohol misuse
Figures 3, 4, & S5 present the results of nine alcohol-related outcomes (full results in Table S6). We observed evidence for reduced binge drinking associated with BMI lowering via GIPR/GLP1R, with estimates in our primary instrument data surpassing the Bonferroni-corrected P-value threshold and replicating at P < 0.05 with BMI lowered via GIPR/GLP1R in the MVP cohort (Fig. 3b). Consistent reductions were also seen with BMI lowering by GIPR alone at P < 0.05, but not GLP1R, suggesting that GIPR modulation is responsible for the observed relationships. Colocalization analysis revealed high probabilities suggest shared causal variants between the BMI and binge drinking in the GIPR locus in the primary BMI (conditional PP.H461 = 0.74). In contrast to the relationships observed with binge drinking, the DPW analysis showed null findings across instruments and datasets (Fig. 3c).
This figure presents Mendelian Randomization (MR) estimates assessing the effects of GIPR, GLP1R, and dual GIPR/GLP1R agonism on Problematic Alcohol Use, self-reported binge drinking behavior, and drinks per week. Results are shown separately for genetically proxied reductions in BMI and HbA1c levels, two primary mechanisms through which these agonists exert their clinical effects. Beta values and 95% confidence intervals (CI) are displayed, with MR estimates derived from biomarker (BMI or HbA1c) data using the primary and replication data sources outlined in the Methods and Table 1. GIPR glucose-dependent insulinotropic polypeptide receptor, GLP1R Glucagon-like peptide-1 receptor, HbA1c glycated hemoglobin, BMI body mass index, CI confidence interval.
This figure presents MR estimates assessing the effects of GIPR, GLP1R, and combined GIPR/GLP1R agonism on high-risk drinking behaviors compared to other drinking patterns, including low risk drinking (4v1), Internalizing alcohol use (4v2), and heavy drinking (4v3). Results are displayed separately for genetically proxied reductions in BMI (left) and HbA1c levels (right), reflecting distinct physiological mechanisms of these agonists. Odds ratios (OR) and 95% confidence intervals (CI) are plotted for both primary and replication datasets. Independent replication data sources are described in the Methods and Table 1. GIPR glucose-dependent insulinotropic polypeptide receptor, GLP1R glucagon-like peptide-1 receptor, BMI body mass index, HbA1c glycated hemoglobin, CI confidence interval.
The associations with the alcohol misuse classifications were also consistent across our primary and replication analyses (Fig. 4a–c) and were strongest in the analyses of misuse classifications that included heavy drinking behaviors. Genetically lowered HbA1c by GIPR/GLP1R was associated with a 38% lower likelihood of broad heavy drinking with psychiatric comorbidities versus light drinking behavior (4v1) and was replicated with HbA1c lowered by GIPR/GLP1R in the MVP cohort. When each locus was analyzed individually, HbA1c lowering by GLP1R showed consistent evidence of protection across both primary and replication datasets (P < 0.05). Similarly, HbA1c lowering via GIPR exhibited consistent and directionally aligned estimates across both primary and replication analyses, indicating a protective effect in reducing broad heavy drinking with psychiatric comorbidities compared to light drinking behavior. Colocalization analysis further supported the GIPR findings, with the GIPR HbA1c signal demonstrating strong colocalization with broad heavy drinking with psychiatric comorbidities versus light drinking behavior (4v1) (conditional H4 = 0.89) (Table S4).
HbA1c lowering by GIPR/GLP1R also reduced heavy drinking with psychiatric comorbidities versus heavy drinking without comorbidities (4v3) with estimates surpassing correction for multiple comparisons in the primary and replication analyses. Moreover, these relationships aligned with the findings for reduced PAU (MR estimate P < 0.05) (Fig. 3a). The generally null results observed for the lighter drinking classifications (internalizing light/non-drinkers vs. low-risk drinking [2v1]) (Figure S5a–c) suggest that the overall DPW null findings are likely driven by null relationships with lighter drinking behaviors in the UK Biobank cohort. This pattern indicates that the protective effects observed are primarily related to heavier or more problematic drinking behaviors rather than general alcohol consumption across all drinkers.
Regarding sensitivity analyses, the estimates were directionally consistent across the complementary MR methods (Table S6) and the alternative instruments constructed using eQTLs, missense variants, and brain expression eQTLs (Figure S6). These sensitivity analyses produced estimates that aligned in magnitude and direction with the primary results, reinforcing the robustness of the associations observed across different analytical frameworks. Further, Steiger tests indicated correct causal orientation, with greater variance explained in the exposure across each instrument set. This consistency across datasets, complementary methods, and alternative instrument construction criteria further strengthens the evidence supporting a protective role of GIPR and GLP1R modulation in reducing alcohol-related risks.
Genetically proxied GLP1R and GIPR analogs are associated with healthier food preferences
Analyses of TUD, CUD, and OUD provided consistent null findings across primary and replication datasets (Figure S7a–c, Table S6). By contrast, robust associations were observed between genetically lowered BMI via GIPR and GLP1R modulation and food preferences, particularly for fatty and vegetarian foods (Figures S8a-c & S9a–b, Table S7). BMI lowering via GIPR/GLP1R was associated with reduced preference for fatty foods (β = −1.58, [−2.01, −1.14], P = 1.62 × 10−12), which replicated (β = −0.42, [−0.57, −0.27], P = 6.84 × 10−8). This relationship was primarily driven by BMI lowering via GIPR (Primary: β = −1.63, [−2.20, −1.06], P = 1.69 × 10−8; Replication: β = −0.59, [−0.79, −0.40], P = 4.42 × 10−9) as BMI lowering by GLP1R variants exhibited null relationships. Similarly, BMI lowering via GIPR/GLP1R was associated with increased preference for vegetarian foods (β = 2.08, [1.17, 2.99], P = 8.22 × 10−6), with replication also demonstrating a beneficial relationship (β = 0.82, [0.55, 1.10], P = 6.46 × 10−9). This finding was again primarily driven by BMI lowering via GIPR (Primary: β = 2.39, [1.71, 3.07], P = 7.11 × 10−12; Replication: β = 1.13, [0.76, 1.50], P = 2.18 × 10−9), while BMI lowering via GLP1R demonstrated null results (Figure S8). In contrast, analyses of coffee and alcohol liking produced consistently null results across all genetic models of GLP1R and GIPR agonism (Figure S8c, Table S7).
Overall, the observed relationships with food liking preferences were primarily driven by BMI lowering, with stronger and more robust associations than HbA1c lowering. While HbA1c lowering by GIPR/GLP1R showed some evidence of beneficial relationships with vegetarian food liking, this impact was generally weaker and less consistent. However, directionally consistent estimates were observed across both BMI and HbA1c exposures, particularly for GIPR-related modulation. Colocalization analysis further supported the associations between BMI lowering via GIPR and food liking traits, with high probabilities of shared causal variants for BMI and fatty food liking (PP.H4 = 0.977), vegetarian liking (PP.H4 = 0.992), and low caloric food liking (PP.H4 = 0.996) in the GIPR locus. Steiger directionality tests supporting the exposure-to-outcome directionality. The findings remained consistent across sensitivity analyses using missense variants, eQTLs, and brain expression eQTLs, indicating robustness. The replication across independent datasets and concordance across multiple instrument construction criteria strongly supports the role of GIPR modulation in shaping food preferences.
Genetically proxied GLP1R and GIPR analogs improve liver health
We next investigated the impact of GIPR and GLP1R modulation on liver disease and liver enzyme outcomes using GWAS summary statistics from European-ancestry cohorts (Table S8). HbA1c lowering by GIPR/GLP1R was associated with linked with lower NAFLD (β = −0.34, [−0.50, −0.18], P = 2.74 × 10−5), with consistent replication (β = −0.10, [−0.17, −0.04], P = 0.0028). This impact was primarily driven via GIPR variants, while the GLP1R locus demonstrated no relationship (Fig. 5a). These findings align with colocalization results demonstrating a high probability of shared genetic variants between HbA1c and NAFLD at the GIPR locus (PP.H4 = 0.96) and a more moderate overlap at the GLP1R locus (PP.H4 = 0.66) (Table S4). In contrast to the protective relationships with NAFLD, neither GIPR nor GLP1R were linked with ALD (Figure S9a, Table S8).
This figure presents MR estimates assessing the effects of GIPR, GLP1R, and dual GIPR/GLP1R agonism on the multi-trait NAFLD GWAS (see Methods), serum alanine aminotransferase levels, aspartate aminotransferase, and serum gamma-glutamyl transpeptidase levels. Results are shown separately for genetically proxied reductions in BMI and HbA1c levels, two primary mechanisms through which these agonists exert their clinical effects. Beta values and 95% confidence intervals (CI) are displayed, with MR estimates derived from biomarker (BMI or HbA1c) data using the primary and independent replication data sources (described in the Methods and Table 1). GIPR glucose-dependent insulinotropic polypeptide receptor, GLP1R Glucagon-like peptide-1 receptor, HbA1c glycated hemoglobin; BMI body mass index, CI confidence interval.
Analyses of liver enzymes levels further confirmed the role of HbA1c lowering via GIPR/GLP1R. Reductions in ALT levels were consistently observed across both primary and replication datasets and similar reductions were noted for GGT levels (Fig. 5b–d; Table S8). These associations were again primarily driven by GIPR, with BMI lowering via GIPR exhibiting consistent protective relationships in the primary and replication analyses. In contrast, GLP1R modulation showed weaker and less consistent relationships with liver enzymes, although some evidence of reductions in ALT was observed. Analyses of AST and ALP demonstrated no relationships, suggesting these liver enzymes are less influenced by GIPR and GLP1R modulation (Fig. 5c, Figure S9b, Table S8). Overall, the findings demonstrate that the observed effects on NAFLD and liver enzymes are primarily driven by HbA1c lowering via GIPR, with BMI lowering providing weaker and less consistent signals. The consistency of these findings across primary and replication datasets, as well as across multiple analytical frameworks, supports a robust and biologically plausible relationship between GIPR modulation and liver-related outcomes.
Reduced binge drinking mediates the cardioprotective relationships of genetic GLP1R and GIPR agonism
MR confirmed that BMI lowering via GIPR/GLP1R variants reduces CAD risk (OR = 0.36, [0.26, 0.51], P = 2.20 × 10−9) in addition to binge drinking frequency (Tables S9 & S10), suggesting a behavioral pathway contributing to cardiovascular benefits and aligning with previous MR work reporting this relationship [69]. Independent MR further confirmed that binge drinking increases CAD risk (OR = 0.75, [0.67, 0.84], P = 1.26 × 10−6), reinforcing the significance of alcohol reduction in cardiovascular protection and mediation analyses showed that 12.6% (P = 0.023) of the GIPR/GLP1R relationship (Figure S10) and 12.2% (P = 0.048) of the GIPR impact on CAD risk were mediated through reductions in binge drinking (Table S10). Results were consistent assessing lowered BMI via GIPR/GLP1R and GIPR in the MVP cohort, though mediation effects were attenuated, underscoring a novel behavioral mechanism through which GLP1R and GIPR agonists may reduce CAD risk.
Exploratory analyses
Exploratory analyses in East Asian and African ancestries, using smaller cohorts, assessed genetic relationships between drug targets and substance use outcomes. Limited by dataset availability, results offer preliminary insights into potential ancestry-specific effects.
East Asian ancestry
The SNP-based instruments targeting BMI and HbA1c lowering via GIPR, GLP1R, and their combined modulation were robustly powered with F-statistics ≥18 (Table S11). Notably, genetically reduced HbA1c via GIPR/GLP1R was associated with reduced T2D risk, with both loci demonstrating consistent, directionally aligned effects consistent with their intended therapeutic targeting of metabolic pathways (Table S12). Unexpectedly, BMI lowering via GIPR was associated with an increased risk of T2D (OR = 2.27, 95% CI [1.32, 3.91], P = 3.14 × 10−3). This result suggests that the GIPR instrument may inadequately capture GIPR activity in this population or may reflect confounding pathways unrelated to direct GIPR modulation. Colocalization analyses further supported these findings, with strong evidence of colocalization in the GIPR locus between BMI lowering and T2D (PP.H4 = 0.754) and for the GLP1R locus between HbA1c lowering and T2D (PP.H4 = 0.996) (Table S13). While the positive control outcomes aligned well with expected effects on T2D, there was little to no evidence of protective effects for alcohol-related outcomes, including AUD and drinks per week, with all estimates including the null (Table S12), suggesting divergence between metabolic-related and alcohol-related outcomes, particularly within this population.
African American/African Caribbean ancestry
Twelve SNPs were identified for analysis, including three for GIPR HbA1c, four for GLP1R BMI, and five for GLP1R HbA1c, all with F-statistics ≥10 (Table S14). HbA1c lowering via GIPR/GLP1R reduced T2D risk, consistent with the GLP1R HbA1c instrument but not GIPR (Table S15). No evidence was found for the three SUDs; however, HbA1c lowering by GIPR/GLP1R reduced DPW (β = −0.31, [−0.46, −0.15], P = 7.97 × 10−5), driven by GLP1R (Table S15). Colocalization signals were absent across all exposures (Table S16).
Discussion
This study used drug-target MR, large genetic datasets, and diverse alcohol use behaviors to assess GLP1R, GIPR, and dual agonism for AUD and drinking behaviors. While GLP1R agonism’s role in alcohol consumption is well-documented in preclinical models [9,10,11], the impact of GIPR is less explored. Our findings show genetic GIPR agonism significantly reduces high-risk and binge drinking behaviors, with distinct patterns between GIPR locus and the GLP1R locus, emphasizing the importance of distinguishing GLP1R and GIPR relationships for targeted treatments.
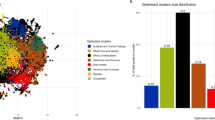
The divergence in the effects observed between GLP1R and GIPR instrumental analyses, particularly concerning their differential impact on BMI versus HbA1c (Fig. 6), suggests distinct mechanistic pathways. Specifically, BMI-lowering relationships via GLP1R and GIPR loci appear to be predominantly mediated through CNS-driven behavioral regulation, influencing binge drinking, food preferences, and obesity. This interpretation is supported by the expression of GLP1R and GIPR in brain regions critical for craving, impulsivity, and hedonic regulation [70, 71], which likely modulate reward and appetite circuits to reduce binge drinking and unhealthy food preferences. In contrast, the HbA1c-mediated effects on alcohol misuse behaviors and liver health suggest a role in hepatic metabolism, insulin sensitivity, and systemic inflammation, consistent with the established metabolic actions of these agonists [72]. Given that PAU is highly comorbid with cardiometabolic disorders [73, 74], the observed effects may contribute to the cardioprotective properties of GIPR/GLP1R agonism, further supported by MR evidence linking reduced binge drinking to lower CAD risk. These findings suggest that CNS-mediated aspects of GIPR/GLP1R agonism may be more relevant for targeting compulsive consumption behaviors, whereas glycemic and metabolic effects may have greater therapeutic potential in alcohol-related liver disease and cardiometabolic risk reduction. This distinction highlights the need for precision approaches in addiction and metabolic medicine, stratifying treatment strategies based on behavioral versus metabolic phenotypes. The mediation findings provide further support for this distinction, demonstrating that while HbA1c-lowering effects via GIPR/GLP1R primarily protect against heavy drinking and related cardiometabolic consequences, BMI-lowering effects exert additional protective effects on CAD that are partially mediated through reduced binge drinking. This suggests that GLP1R and GIPR agonists may act through complementary behavioral and cardiometabolic pathways, with glycemic control reducing disease risk through metabolic improvements and BMI reduction influencing disease pathways through changes in harmful drinking behaviors. The consistency of these findings across independent datasets highlights the therapeutic potential of dual agonists for integrated approaches addressing metabolic and addiction-related disease burdens.
This figure presents traits with consistent protective or beneficial associations across both primary and replication datasets for each receptor target (GIPR/GLP1R, GIPR, GLP1R), using either BMI (blue) or HbA1c (yellow) as the exposure biomarker. Arrows indicate direction of effect. Asterisks (*) denote associations that surpassed the Bonferroni-corrected significance threshold (P < 0.0025). Results with dashed borders surpassed testing for multiple comparisons in either the primary or replication exposure data but had P-value > 0.05 in the other. Traits shown include alcohol use behaviors (e.g., binge drinking, high-risk drinking), dietary preferences (e.g., fatty, fried, vegetarian, and low-calorie foods), and liver-related outcomes (e.g., NAFLD, ALT, AST, GGT). GIPR glucose-dependent insulinotropic polypeptide receptor, GLP1R Glucagon-like peptide-1 receptor, HbA1c glycated hemoglobin, BMI body mass index.
The combined GIPR/GLP1R relationships with NAFLD, liver enzymes (ALT, GGT), binge drinking, alcohol misuse, and food liking outcomes show consistent protective relationships across both loci, with estimates from the GIPR locus providing particularly robust evidence. While estimates for GLP1R alone were generally less precise, they were consistently directionally aligned with the protective effects observed for GIPR. This concordance underscores the therapeutic potential of dual agonists, such as tirzepatide [17], which target both GIPR and GLP1R pathways. The stronger and more consistent findings from GIPR suggest it may play a more central role in mediating these effects, but the overall pattern indicates that combined activation of both receptors offers the most comprehensive therapeutic benefit. The protective role of GIPR/GLP1R agonism aligns with the broader functions of the gut-brain axis, where GIP and GLP-1 peptides influence metabolic regulation and hedonic behaviors [70, 71].
Synergistic impacts on alcohol consumption and dietary outcomes support the hypothesis that these pathways interact to modulate reward and consumption behaviors [75]. The concurrent benefits observed in alcohol use reduction and liver function improvement have significant implications for managing alcohol-related liver disease, where integrated approaches targeting liver pathology and alcohol use behaviors are critical [76]. However, despite these positive associations, we did not observe evidence for a relationship between GIPR/GLP1R agonism and ALD. This null finding is potentially due to the lower statistical power of the available ALD GWAS compared to other liver traits, limiting the ability to detect smaller effects. Given the well-established role of alcohol in liver disease progression [77], larger and more refined ALD GWAS datasets are necessary to clarify whether GIPR and GLP1R agonism directly mitigates ALD risk. This evidence underscores the promise of GIPR agonism as a therapeutic avenue for addressing AUD and comorbid metabolic disorders, warranting further investigation in clinical settings.
No protective genetic links were found between GIPR or GLP1R activity and other SUDs, suggesting their effects on alcohol consumption, such as binge drinking behaviors, are likely driven by metabolic, appetite, and food-related pathways rather than classical dopaminergic reward pathways, although future studies should investigate these possibilities [78]. Differences between the genetics of alcohol consumption and AUD [44] underscore the need for distinct therapeutic strategies, such as harm reduction for alcohol use versus risk reduction for AUD [79]. Future RCTs are essential to validate these findings and clarify whether GLP1R and GIPR agonists can differentiate between various substance use behaviors and SUD diagnoses in clinical practice. Food liking analyses further support this hypothesis, showing that GLP1R and GIPR agonism reduces unhealthy food preferences, likely through mechanisms related to reward and metabolic regulation [78]. These results align with previous evidence of GLP1R and GIPR involvement in food intake and suggest that BMI-targeting therapies may influence alcohol consumption through changes in food behaviors [80, 81]. The observed associations between BMI modulation and reduced alcohol intake strengthen the hypothesis that metabolic states influence both dietary preferences and alcohol use. These findings highlight the therapeutic potential of GLP1R and GIPR agonists for addressing harmful alcohol consumption and unhealthy food behaviors through shared neurobiological pathways and rising comorbidities between AUD and obesity [82].
Study strengths include using a robust drug-target MR and colocalization framework to provide causal evidence of GLP1R and GIPR agonism effects on alcohol consumption and metabolic traits. The results were consistent across two independent datasets for each biomarker used to instrument the drug targets and multiple instrumentation strategies, including missense SNPs, eQTLs, and cortical gene expression. Leveraging large-scale GWAS datasets validates cardiometabolic impacts while contextualizing substance use and food liking traits, offering insights into metabolic regulation and reward pathways. Exploratory multi-ancestry analyses in East Asian and African cohorts address key gaps in genomic research diversity [83] and enhance the global relevance of these findings. However, limitations include the inability to model specific differences between drug classes or formulations [84] and the complexity of dual agonist mechanisms, which may not be fully captured by genetic instruments [85]. While cis-variant MR reduces pleiotropy risk, potential biases may remain [22]. Additionally, cultural factors significantly influence obesity, T2D, and substance use, and exploratory analyses in non-European populations were limited by smaller sample sizes and dataset availability [86,87,88]. Supplementary Discussion provides additional context and interpretation of the multi-ancestry findings. Replication in larger, diverse cohorts is essential for advancing addiction medicine, reducing health disparities, and enhancing precision healthcare [24, 83, 89]. An additional important consideration is the extent to which endogenous genetic “agonism” at these receptors may modify response to exogenous GIPR/GLP1R agonist therapy. The degree to which an individual’s innate genetic “agonism” of GLP1R and GIPR co-occurs with pharmacological treatment—and thereby modulates therapeutic response—has not yet been characterized. Our analyses show that a substantial proportion of the population carries receptor-activating alleles at these loci, making it probable that drug exposure and genetic predisposition overlap. This overlap could amplify signaling in some individuals or, conversely, lead to reduced efficacy or increased adverse effects in others. Unfortunately, pharmacogenomic data that directly test how these alleles interact with GIPR/GLP1R agonist therapy are not yet available and should be a priority for future clinical studies. Moreover, our ancestry-specific carrier estimates hint at meaningful differences in baseline allele frequencies across populations, but uneven sample sizes—particularly in non-European cohorts—mean that rarer but potentially important variants may be missed. Careful, ancestry-diverse pharmacogenetic investigation will therefore be critical to optimize dosing, maximize benefit, and minimize harm across all patient groups.
Conclusion
This study highlights the therapeutic potential of GLP1R and GIPR agonism, particularly dual GIPR/GLP1R targeting, in reducing problematic alcohol use behaviors and improving liver health. Our findings suggest that these effects are primarily driven by calorie-sensing and metabolic regulation pathways rather than addiction-specific mechanisms. The observed benefits on alcohol use behaviors, liver enzymes, and food preferences underscore the potential for these agents to address the dual burden of AUDs and metabolic comorbidities. These results provide a foundation for clinical trials exploring the repurposing of GLP1R and GIPR agonists to improve metabolic and psychiatric outcomes, offering a novel and integrated approach to harm reduction in addiction medicine.
Data availibility
This study used publicly available data. References and data links are available in Table S1.
Code availibility
Analyses were performed using publicly available analysis software. TwoSample MR is available at: https://github.com/MRCIEU/TwoSampleMR; coloc is available at: https://cran.r-project.org/web/packages/coloc/index.html. MTAG is available at https://github.com/JonJala/mtag.
References
Min T, Bain SC. The role of tirzepatide, dual GIP and GLP-1 receptor agonist, in the management of type 2 diabetes: the SURPASS clinical trials. Diabetes Ther. 2021;12:143–57. https://doi.org/10.1007/s13300-020-00981-0
Sinha R, Papamargaritis D, Sargeant JA, Davies MJ. Efficacy and safety of tirzepatide in type 2 diabetes and obesity management. J Obes Metab Syndr. 2023;32:25–45. https://doi.org/10.7570/jomes22067
Leggio L, Hendershot CS, Farokhnia M, Fink-Jensen A, Klausen MK, Schacht JP, et al. GLP-1 receptor agonists are promising but unproven treatments for alcohol and substance use disorders. Nat Med. 2023;29:2993–5. https://doi.org/10.1038/s41591-023-02634-8
Lohoff FW. Pharmacotherapies and personalized medicine for alcohol use disorder: a review. Pharmacogenomics. 2020;21:1117–38. https://doi.org/10.2217/pgs-2020-0079
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP23-07-01-006, NSDUH Series H-58). 2023. https://www.samhsa.gov/data/report/2022-nsduh-annual-national-report
Lohoff FW. Targeting unmet clinical needs in the treatment of alcohol use disorder. Front Psychiatry. 2022;13:767506 https://doi.org/10.3389/fpsyt.2022.767506
Klausen MK, Thomsen M, Wortwein G, Fink-Jensen A. The role of glucagon-like peptide 1 (GLP-1) in addictive disorders. Br J Pharmacol. 2022;179:625–41. https://doi.org/10.1111/bph.15677
Lähteenvuo M, Tiihonen J, Solismaa A, Tanskanen A, Mittendorfer-Rutz E, Taipale H. Repurposing semaglutide and liraglutide for alcohol use disorder. JAMA Psychiatry. 2025;82:94–98. https://doi.org/10.1001/jamapsychiatry.2024.3599
Chuong V, Farokhnia M, Khom S, Pince CL, Elvig SK, Vlkolinsky R, et al. The glucagon-like peptide-1 (GLP-1) analogue semaglutide reduces alcohol drinking and modulates central GABA neurotransmission. JCI Insight. 2023;8:e170671 https://doi.org/10.1172/jci.insight.170671
Aranäs C, Edvardsson CE, Shevchouk OT, Zhang Q, Witley S, Blid Sköldheden S, et al. Semaglutide reduces alcohol intake and relapse-like drinking in male and female rats. EBioMedicine. 2023;93:104642 https://doi.org/10.1016/j.ebiom.2023.104642
Shirazi RH, Dickson SL, Skibicka KP. Gut peptide GLP-1 and its analogue, Exendin-4, decrease alcohol intake and reward. PLoS One. 2013;8:e61965 https://doi.org/10.1371/journal.pone.0061965
Probst L, Monnerat S, Vogt DR, Lengsfeld S, Burkard T, Meienberg A, et al. Effects of dulaglutide on alcohol consumption during smoking cessation. JCI Insight. 2023;8:e170419 https://doi.org/10.1172/jci.insight.170419
Klausen MK, Jensen ME, Møller M, Le Dous N, Jensen A-MØ, Zeeman VA, et al. Exenatide once weekly for alcohol use disorder investigated in a randomized, placebo-controlled clinical trial. JCI Insight. 2022;7:e159863 https://doi.org/10.1172/jci.insight.159863
Holst JJ, Rosenkilde MM. Recent advances of GIP and future horizons. Peptides. 2020;125:170230 https://doi.org/10.1016/j.peptides.2019.170230
Samms RJ, Christe ME, Collins KAL, Pirro V, Droz BA, Holland AK, et al. GIPR agonism mediates weight-independent insulin sensitization by tirzepatide in obese mice. J Clin Invest. 2021;131:e146353 https://doi.org/10.1172/JCI146353
Tsermpini EE, Goričar K, Kores Plesničar B, Plemenitaš Ilješ A, Dolžan V. Genetic variability of incretin receptors and alcohol dependence: a Pilot study. Front Mol Neurosci. 2022;15:908948 https://doi.org/10.3389/fnmol.2022.908948
Gasbjerg LS, Rosenkilde MM, Meier JJ, Holst JJ, Knop FK. The importance of glucose-dependent insulinotropic polypeptide receptor activation for the effects of tirzepatide. Diabetes Obes Metab. 2023;25:3079–92. https://doi.org/10.1111/dom.15216
Rogers PJ. Food and drug addictions: similarities and differences. Pharmacol Biochem Behav. 2017;153:182–90. https://doi.org/10.1016/j.pbb.2017.01.001
Liskiewicz A, Khalil A, Liskiewicz D, Novikoff A, Grandl G, Maity-Kumar G, et al. Glucose-dependent insulinotropic polypeptide regulates body weight and food intake via GABAergic neurons in mice. Nature Metabolism. 2023;5:2075–85. https://doi.org/10.1038/s42255-023-00931-7
Brindisi MC, Brondel L, Meillon S, Barthet S, Grall S, Fenech C, et al. Proof of concept: Effect of GLP-1 agonist on food hedonic responses and taste sensitivity in poor controlled type 2 diabetic patients. Diabetes Metab Syndr. 2019;13:2489–94. https://doi.org/10.1016/j.dsx.2019.06.021
Sanderson E, Glymour MM, Holmes MV, Kang H, Morrison J, Munafò MR, et al. Mendelian randomization. Nat Rev Methods Primers. 2022;2:6 https://doi.org/10.1038/s43586-021-00092-5
Schmidt AF, Finan C, Gordillo-Marañón M, Asselbergs FW, Freitag DF, Patel RS, et al. Genetic drug target validation using Mendelian randomisation. Nat Commun. 2020;11:3255–3255. https://doi.org/10.1038/s41467-020-16969-0
Rosoff DB, Wagner J, Bell AS, Mavromatis LA, Jung J, Lohoff FW. A multi-omics Mendelian randomization study identifies new therapeutic targets for alcohol use disorder and problem drinking. Nat Human Behav. 2024. https://doi.org/10.1038/s41562-024-02040-1
Rosoff DB, Wagner J, Jung J, Pacher P, Christodoulides C, Smith GD, et al. Multi-omics Mendelian Randomization Study investigating the impact of PCSK9 and HMGCR inhibition on type 2 diabetes across five populations. Diabetes. 2024:db240451. https://doi.org/10.2337/db24-0451
Skrivankova VW, Richmond RC, Woolf BAR, Davies NM, Swanson SA, VanderWeele TJ, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ. 2021;375:n2233 https://doi.org/10.1136/bmj.n2233
Ussher JR, Drucker DJ. Glucagon-like peptide 1 receptor agonists: cardiovascular benefits and mechanisms of action. Nat Rev Cardiol. 2023;20:463–74. https://doi.org/10.1038/s41569-023-00849-3
Neale-Lab. UK Biobank GWAS. Accessed 2019. http://www.nealelab.is/uk-biobank/
Pulit SL, Stoneman C, Morris AP, Wood AR, Glastonbury CA, Tyrrell J, et al. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum Mol Genet. 2019;28:166–74. https://doi.org/10.1093/hmg/ddy327
Gordillo-Marañón M, Zwierzyna M, Charoen P, Drenos F, Chopade S, Shah T, et al. Validation of lipid-related therapeutic targets for coronary heart disease prevention using human genetics. Nat Commun. 2021;12:6120 https://doi.org/10.1038/s41467-021-25731-z
Henry A, Gordillo-Marañón M, Finan C, Schmidt AF, Ferreira JP, Karra R, et al. Therapeutic targets for heart failure identified using proteomics and mendelian randomization. Circulation. 2022;145:1205–17. https://doi.org/10.1161/circulationaha.121.056663
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. New Engl J Med. 2022;387:205–16. https://doi.org/10.1056/NEJMoa2206038
Verma A, Huffman JE, Rodriguez A, Conery M, Liu M, Ho Y-L, et al. Diversity and scale: genetic architecture of 2068 traits in the VA Million Veteran Program. Science. 2024;385:eadj1182 https://doi.org/10.1126/science.adj1182
Consortium GT. The Genotype-Tissue Expression (GTEx) project. Nat Genet. 2013;45:580–5. https://doi.org/10.1038/ng.2653
Obenchain V, Lawrence M, Carey V, Gogarten S, Shannon P, Morgan M. VariantAnnotation: a Bioconductor package for exploration and annotation of genetic variants. Bioinformatics. 2014;30:2076–8. https://doi.org/10.1093/bioinformatics/btu168
de Klein N, Tsai EA, Vochteloo M, Baird D, Huang Y, Chen C-Y, et al. Brain expression quantitative trait locus and network analyses reveal downstream effects and putative drivers for brain-related diseases. Nat Genet. 2023;55:377–88. https://doi.org/10.1038/s41588-023-01300-6
Kanai M, Akiyama M, Takahashi A, Matoba N, Momozawa Y, Ikeda M, et al. Genetic analysis of quantitative traits in the Japanese population links cell types to complex human diseases. Nat Genet. 2018;50:390–400. https://doi.org/10.1038/s41588-018-0047-6
Auton A, Abecasis GR, Altshuler DM, Durbin RM, Abecasis GR, Bentley DR, et al. A global reference for human genetic variation. Nature. 2015;526:68–74. https://doi.org/10.1038/nature15393
Tina V, Mikkel C, Anders EJ, Filip KK, Lise Lotte G. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ. 2012;344:d7771 https://doi.org/10.1136/bmj.d7771
Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8:728–42. https://doi.org/10.1038/nrendo.2012.140
Suzuki K, Hatzikotoulas K, Southam L, Taylor HJ, Yin X, Lorenz KM, et al. Genetic drivers of heterogeneity in type 2 diabetes pathophysiology. Nature. 2024;627:347–57. https://doi.org/10.1038/s41586-024-07019-6
Kurki MI, Karjalainen J, Palta P, Sipilä TP, Kristiansson K, Donner KM, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613:508–18. https://doi.org/10.1038/s41586-022-05473-8
Roden DM, Altman RB, Benowitz NL, Flockhart DA, Giacomini KM, Johnson JA, et al. Pharmacogenomics: challenges and opportunities. Ann Intern Med. 2006;145:749–57. https://doi.org/10.7326/0003-4819-145-10-200611210-00007
Hernandez S, Hindorff LA, Morales J, Ramos EM, Manolio TA. Patterns of pharmacogenetic variation in nine biogeographic groups. Clin Transl Sci. 2024;17:e70017 https://doi.org/10.1111/cts.70017
Zhou H, Kember RL, Deak JD, Xu H, Toikumo S, Yuan K, et al. Multi-ancestry study of the genetics of problematic alcohol use in over 1 million individuals. Nat Med. 2023;29:3184–92. https://doi.org/10.1038/s41591-023-02653-5
Saunders GRB, Wang X, Chen F, Jang S-K, Liu M, Wang C, et al. Genetic diversity fuels gene discovery for tobacco and alcohol use. Nature. 2022;612:720–4. https://doi.org/10.1038/s41586-022-05477-4
Toikumo S, Jennings MV, Pham BK, Lee H, Mallard TT, Bianchi SB, et al. Multi-ancestry meta-analysis of tobacco use disorder identifies 461 potential risk genes and reveals associations with multiple health outcomes. Nat Human Behav. 2024;8:1177–93. https://doi.org/10.1038/s41562-024-01851-6
Thijssen AB, Chartier K, Amstadter A, Dick DM, Lilley E, Gelzinis R, et al. Investigating genetically stratified subgroups to better understand the etiology of alcohol misuse. Mol Psychiatry. 2023;28:4225–33. https://doi.org/10.1038/s41380-023-02174-0
Deak JD, Zhou H, Galimberti M, Levey DF, Wendt FR, Sanchez-Roige S, et al. Genome-wide association study in individuals of European and African ancestry and multi-trait analysis of opioid use disorder identifies 19 independent genome-wide significant risk loci. Mol Psychiatry. 2022;27:3970–9. https://doi.org/10.1038/s41380-022-01709-1
Barton AR, Sherman MA, Mukamel RE, Loh PR. Whole-exome imputation within UK Biobank powers rare coding variant association and fine-mapping analyses. Nat Genet. 2021;53:1260–9. https://doi.org/10.1038/s41588-021-00892-1
Sakaue S, Kanai M, Tanigawa Y, Karjalainen J, Kurki M, Koshiba S, et al. A cross-population atlas of genetic associations for 220 human phenotypes. Nat Genet. 2021;53:1415–24. https://doi.org/10.1038/s41588-021-00931-x
Ghodsian N, Abner E, Emdin CA, Gobeil É, Taba N, Haas ME, et al. Electronic health record-based genome-wide meta-analysis provides insights on the genetic architecture of non-alcoholic fatty liver disease. Cell Rep Med. 2021;2:100437 https://doi.org/10.1016/j.xcrm.2021.100437
Sumida Y, Yoneda M. Current and future pharmacological therapies for NAFLD/NASH. J Gastroenterol. 2018;53:362–76. https://doi.org/10.1007/s00535-017-1415-1
van der Meer D, Gurholt TP, Sønderby IE, Shadrin AA, Hindley G, Rahman Z, et al. The link between liver fat and cardiometabolic diseases is highlighted by genome-wide association study of MRI-derived measures of body composition. Commun Bio. 2022;5:1271 https://doi.org/10.1038/s42003-022-04237-4
Turley P, Walters RK, Maghzian O, Okbay A, Lee JJ, Fontana MA, et al. Multi-trait analysis of genome-wide association summary statistics using MTAG. Nat Genet. 2018;50:229–37. https://doi.org/10.1038/s41588-017-0009-4
Bulik-Sullivan BK, Loh P-R, Finucane HK, Ripke S, Yang J, Patterson N, et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015;47:291–5. https://doi.org/10.1038/ng.3211
Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat Commun. 2017;8:1826 https://doi.org/10.1038/s41467-017-01261-5
May-Wilson S, Matoba N, Wade KH, Hottenga J-J, Concas MP, Mangino M, et al. Large-scale GWAS of food liking reveals genetic determinants and genetic correlations with distinct neurophysiological traits. Nat Commun. 2022;13:2743 https://doi.org/10.1038/s41467-022-30187-w
Hemani G, Tilling K, Davey Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLOS Genetics. 2017;13:e1007081 https://doi.org/10.1371/journal.pgen.1007081
Burgess S, Small DS, Thompson SG. A review of instrumental variable estimators for Mendelian randomization. Stat Methods Med Res. 2017;26:2333–55. https://doi.org/10.1177/0962280215597579
Zuber V, Grinberg NF, Gill D, Manipur I, Slob EAW, Patel A, et al. Combining evidence from Mendelian randomization and colocalization: review and comparison of approaches. Am J Hum Genet. 2022;109:767–82. https://doi.org/10.1016/j.ajhg.2022.04.001
Giambartolomei C, Vukcevic D, Schadt EE, Franke L, Hingorani AD, Wallace C, et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet. 2014;10:e1004383 https://doi.org/10.1371/journal.pgen.1004383
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7:e34408 https://doi.org/10.7554/eLife.34408
Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567:305–7. https://doi.org/10.1038/d41586-019-00857-9
Rosoff DB, Davey Smith G, Mehta N, Clarke T-K, Lohoff FW. Evaluating the relationship between alcohol consumption, tobacco use, and cardiovascular disease: a multivariable Mendelian randomization study. PLOS Medicine. 2020;17:e1003410 https://doi.org/10.1371/journal.pmed.1003410
Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. The Lancet. 2019;393:1831–42. https://doi.org/10.1016/S0140-6736(18)31772-0
Biddinger KJ, Emdin CA, Haas ME, Wang M, Hindy G, Ellinor PT, et al. Association of habitual alcohol intake with risk of cardiovascular disease. JAMA Network Open. 2022;5:e223849–e223849. https://doi.org/10.1001/jamanetworkopen.2022.3849
Relton CL, Davey Smith G. Two-step epigenetic Mendelian randomization: a strategy for establishing the causal role of epigenetic processes in pathways to disease. Int J Epidemiol. 2012;41:161–76. https://doi.org/10.1093/ije/dyr233
Aragam KG, Jiang T, Goel A, Kanoni S, Wolford BN, Atri DS, et al. Discovery and systematic characterization of risk variants and genes for coronary artery disease in over a million participants. Nat Genet. 2022;54:1803–15. https://doi.org/10.1038/s41588-022-01233-6
Patel A, Gill D, Shungin D, Mantzoros CS, Knudsen LB, Bowden J, et al. Robust use of phenotypic heterogeneity at drug target genes for mechanistic insights: application of cis-multivariable Mendelian randomization to GLP1R gene region. Genet Epidemiol. 2024;48:151–63. https://doi.org/10.1002/gepi.22551
Zhang Q, Delessa CT, Augustin R, Bakhti M, Colldén G, Drucker DJ, et al. The glucose-dependent insulinotropic polypeptide (GIP) regulates body weight and food intake via CNS-GIPR signaling. Cell Metabolism. 2021;33:833–844.e5. https://doi.org/10.1016/j.cmet.2021.01.015
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39. https://doi.org/10.1152/physrev.00034.2006
Campbell JE, Müller TD, Finan B, DiMarchi RD, Tschöp MH, D’Alessio DA. GIPR/GLP-1R dual agonist therapies for diabetes and weight loss—chemistry, physiology, and clinical applications. Cell Metabolism. 2023;35:1519–29. https://doi.org/10.1016/j.cmet.2023.07.010
Hoek AG, van Oort S, Mukamal KJ, Beulens JWJ. Alcohol consumption and cardiovascular disease risk: placing new data in context. Curr Atheroscler Rep. 2022;24:51–59. https://doi.org/10.1007/s11883-022-00992-1
Wang T, Farokhnia M, Leggio L. FGF21 regulates alcohol intake: new hopes on the rise for alcohol use disorder treatment? Cell Rep Med. 2022;3:100578 https://doi.org/10.1016/j.xcrm.2022.100578
Sobrino Crespo C, Perianes Cachero A, Puebla Jiménez L, Barrios V, Arilla Ferreiro E. Peptides and food intake. Front Endocrinol (Lausanne). 2014;5:58 https://doi.org/10.3389/fendo.2014.00058
Rosoff DB, Charlet K, Jung J, Lee J, Muench C, Luo A, et al. Association of high-intensity binge drinking with lipid and liver function enzyme levels. JAMA Network Open. 2019;2:e195844–e195844. https://doi.org/10.1001/jamanetworkopen.2019.5844
Osna NA, Donohue TM Jr, Kharbanda KK. Alcoholic liver disease: pathogenesis and current management. Alcohol Res. 2017;38:147–61.
Wang XF, Liu JJ, Xia J, Liu J, Mirabella V, Pang ZP. Endogenous glucagon-like peptide-1 suppresses high-fat food intake by reducing synaptic drive onto mesolimbic dopamine neurons. Cell Rep. 2015;12:726–33. https://doi.org/10.1016/j.celrep.2015.06.062
Charlet K, Heinz A. Harm reduction—a systematic review on effects of alcohol reduction on physical and mental symptoms. Addiction Biology. 2017;22:1119–59. https://doi.org/10.1111/adb.12414
Carreras-Torres R, Johansson M, Haycock PC, Relton CL, Davey Smith G, Brennan P, et al. Role of obesity in smoking behaviour: Mendelian randomisation study in UK Biobank. BMJ. 2018;361:k1767 https://doi.org/10.1136/bmj.k1767
Bjørklund O, Wichstrøm L, Llewellyn C, Steinsbekk S. The prospective relation between eating behaviors and BMI from middle childhood to adolescence: a 5-wave community study. Prev Med Rep. 2022;27:101795 https://doi.org/10.1016/j.pmedr.2022.101795
Tawa EA, Hall SD, Lohoff FW. Overview of the genetics of alcohol use disorder. Alcohol Alcohol. 2016;51:507–14. https://doi.org/10.1093/alcalc/agw046
Fatumo S, Chikowore T, Choudhury A, Ayub M, Martin AR, Kuchenbaecker K. A roadmap to increase diversity in genomic studies. Nature Medicine. 2022;28:243–50. https://doi.org/10.1038/s41591-021-01672-4
Anderson EL, Williams DM. Drug target Mendelian randomisation: are we really instrumenting drug use? Diabetologia. 2023;66:1156–8. https://doi.org/10.1007/s00125-023-05875-x
Chavda VP, Ajabiya J, Teli D, Bojarska J, Apostolopoulos V. Tirzepatide, a new era of dual-targeted treatment for diabetes and obesity: a mini-review. Molecules. 2022;27:4315 https://doi.org/10.3390/molecules27134315
Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217 https://doi.org/10.1016/j.metabol.2022.155217
Volkow ND, Blanco C. Substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatry. 2023;22:203–29. https://doi.org/10.1002/wps.21073
Ong KL, Stafford LK, McLaughlin SA, Boyko EJ, Vollset SE, Smith AE, et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. The Lancet. 2023;402:203–34. https://doi.org/10.1016/S0140-6736(23)01301-6
Rosoff DB, Bell AS, Wagner J, Mavromatis LA, Hamandi A, Park L, et al. Assessing the impact of PCSK9 and HMGCr inhibition on liver function: drug-target mendelian randomization analyses in four ancestries. Cell Mol Gastroenterol Hepatol. 2023. https://doi.org/10.1016/j.jcmgh.2023.09.001
Chauquet S, Zhu Z, O’Donovan MC, Walters JTR, Wray NR, Shah S. Association of antihypertensive drug target genes with psychiatric disorders: a Mendelian Randomization Study. JAMA Psychiatry. 2021;78:623–31. https://doi.org/10.1001/jamapsychiatry.2021.0005
Acknowledgements
We would like to acknowledge the participants and investigators of the many studies used in this research without whom this effort would not be possible, including publicly available GWAS data provided by the UK Biobank, Psychiatric Genomics Consortium, DIAMANTE, and FinnGen studies. We also want to acknowledge the Meta-Analyses of Glucose and Insulin-related traits Consortium, Neale Lab, Million Veterans Program, GTEx Project, and MetaBrain Consortium. Finally, we would like to acknowledge the Medical Research Council Integrative Epidemiology Unit (MRC-IEU, University of Bristol, England), especially the developers of the MRC-IEU UK Biobank Genome-Wide Association Study Pipeline. We acknowledge their contributing studies and the participants in those studies, without whom this effort would not be possible.
Funding
This work was supported by the National Institutes of Health intramural funding (ZIA-AA000242 to Dr. Lohoff) of the Division of Intramural Clinical and Biological Research of the National Institute on Alcohol Abuse and Alcoholism. The funding sources had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The contributions of the NIH author(s) are considered Works of the United States Government. The findings and conclusions presented in this paper are those of the author(s) and do not necessarily reflect the views of the NIH or the U.S. Department of Health and Human Services. Open access funding provided by the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
JR and DBR performed analyses, drafted the manuscript, and created figures. TP, AW, JJ, and JW critically revised the manuscript. BCR provided scientific insight. DBR and FWL designed the study. FWL oversaw the project. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics considerations
This study used publicly available, de-identified GWASs using participants of European, East Asian, and African ancestries (Table 1). These studies had existing ethical permissions from their respective internal review boards and ethics committees. They included participant informed consent with rigorous quality control for all subjects. No additional informed consent was required in this study. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Reitz, J., Rosoff, D.B., Perlstein, T. et al. Genetically modeled GLP1R and GIPR agonism reduce binge drinking and alcohol-associated phenotypes: a multi-ancestry drug-target Mendelian randomization study. Mol Psychiatry 30, 6119–6133 (2025). https://doi.org/10.1038/s41380-025-03199-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03199-3