Abstract
Cardiac development is a complex and intricate process involving numerous molecular signals and pathways. Researchers have explored cardiac development through a long journey, starting with early studies observing morphological changes and progressing to the exploration of molecular mechanisms using various molecular biology methods. Currently, advancements in stem cell technology and sequencing technology, such as the generation of human pluripotent stem cells and cardiac organoids, multi-omics sequencing, and artificial intelligence (AI) technology, have enabled researchers to understand the molecular mechanisms of cardiac development better. Many molecular signals regulate cardiac development, including various growth and transcription factors and signaling pathways, such as WNT signaling, retinoic acid signaling, and Notch signaling pathways. In addition, cilia, the extracellular matrix, epigenetic modifications, and hypoxia conditions also play important roles in cardiac development. These factors play crucial roles at one or even multiple stages of cardiac development. Recent studies have also identified roles for autophagy, metabolic transition, and macrophages in cardiac development. Deficiencies or abnormal expression of these factors can lead to various types of cardiac development abnormalities. Nowadays, congenital heart disease (CHD) management requires lifelong care, primarily involving surgical and pharmacological treatments. Advances in surgical techniques and the development of clinical genetic testing have enabled earlier diagnosis and treatment of CHD. However, these technologies still have significant limitations. The development of new technologies, such as sequencing and AI technologies, will help us better understand the molecular mechanisms of cardiac development and promote earlier prevention and treatment of CHD in the future.
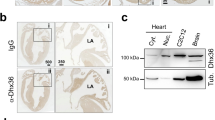
Similar content being viewed by others
Introduction
The heart, as the first functional organ in the fetus, undergoes a complex developmental process starting from the differentiation of mesodermal cells during gastrulation. This process involves three main regions with cardiac precursor cells, namely, the cardiogenic mesoderm, the proepicardium, and the cardiac neural crest. Through the coordinated regulation of various signaling pathways, heart development begins with the migration of mesodermal cells from the primitive streak, moving to the both sides of the embryonic midline formatting two heart-forming regions (HFRs), each consisting of the first heart field (FHF) on the anterior lateral side and the secondary heart field (SHF) on the anterior medial side. The HFRs then merge to form the cardiac crescent, from which cells of the FHF eventually fold to form the primitive heart tube, initiating subsequent pulsation. Subsequently, the heart tube undergoes rapid growth through the recruitment of cells from the SHF and cell proliferation. Simultaneously, it bends to the right and initiates looping, ultimately leading to the formation of the right and left ventricles and atria, accompanied by the development of myocardial trabeculae, growth of the epicardium, development of the coronary vascular system, and subsequent formation of cardiac septa and valves.1,2,3
Based on previous studies exploring cardiac development, numerous signaling pathways, particularly those involving various transcription factors (TFs) and growth factors (GFs), have been found to play pivotal roles in different phases of heart development.4,5,6 For instance, the transcription factor NK2 homeobox 5 (NKX2-5) is a marker of cardiac precursor cells that regulates the proliferation and differentiation of these cells in the early phases of cardiac development.7 Another important transcription factor for cardiac development, GATA binding protein 4 (GATA4), has been found to interact with NKX2-5 through its zinc finger structure and specific residues in the C-terminal extension,8 while bone morphogenetic protein (BMP) 4, one of the GFs essential for embryonic heart development, has been suggested to regulate NKX2-5 expression via GATA4.9 Therefore, the molecular mechanisms of cardiac development are complex and intricate, involving numerous molecules and pathways in different cells that interact to form a finely tuned-regulatory network, thereby promoting normal cardiac development. Over the last few decades, advancements in genetics, molecular biology, and cell biology have deepened our understanding of the mechanisms of cardiac development. The development of stem cell and organoid technology allows us to mimic the process of animal or human cardiac development in vitro, although this technology still faces many challenges, such as the immaturity of differentiated cells and differences from the in vivo environment. Nevertheless, these studies provide a possible in vitro model for further understanding and validating the molecular mechanisms of cardiac development.
Multi-omics analysis, stemming from the development of bioinformatics, also provides technical support for understanding the process of cardiac development at different levels. A study by Hu et al. identified novel core TFs [Kruppel-like factor 11 (KLF11) and E2F transcription factor 6 (E2F6)] and dynamic changes in enriched key pathways through multi-omics analysis.10 Another study delineated cellular niches within eight regions of the human heart, revealing the characteristics of cells in the cardiac conduction system and their multicellular niches.11 These new technologies enable us to understand the molecular mechanisms of cardiac development at different cellular and regulatory levels, comprehensively improving our knowledge of cardiac development.
Disruption of the molecular regulatory network of cardiac development by genetic or nongenetic factors can lead to various types of cardiac malformations, which are characteristic of congenital heart defects (CHDs), with ventricular septal defects (VSDs) being the most common. CHDs encompass various types, and depending on the location of the cardiac malformation, they can be classified as septal defects, conotruncal defects, valve defects, among others. Several critical CHDs, including hypoplastic left heart syndrome (HLHS), transposition of the great arteries, and pulmonary atresia, can result in severe consequences if not treated promptly. Moreover, certain developmental diseases affecting multiple organ systems are often associated with a high incidence of CHD, such as DiGeorge syndrome, commonly linked with Tetralogy of Fallot (ToF),12 and Noonan syndrome, often associated with pulmonary valve stenosis (PVS).13 These different types of CHDs have distinct pathogenic mechanisms. For instance, mutations in TBX5 frequently lead to septal defects, while abnormalities in Notch and TGFβ signaling are often associated with defective valve development. However, the pathogenesis of CHD remains unclear, with only 15% of cases attributed to genetic inheritance and 30% associated with environmental risk factors, including fever, infections, maternal smoking, alcohol consumption, diabetes, and hypertension.14 These factors can affect any aspect of the cardiac developmental regulatory network, leading to abnormalities in the differentiation and proliferation of cardiomyocytes, endocardial cells, and smooth muscle cells and ultimately resulting in congenital heart defects.14,15 Although surgical procedures and palliative care are the main treatments for CHD, advancements in understanding cardiac development offer promising avenues for innovative therapeutic approaches, particularly in the early prevention and treatment of CHD. Advances in genetic technologies, bioinformatics, and big data analytics may enable the precise identification of genetic or nongenetic factors contributing to CHD, facilitating the development of precision and individualized disease prediction models and more effective prevention strategies, ultimately reducing the occurrence of CHD and the necessity for surgical interventions in the future.
This review aims to summarize the processes and molecular mechanisms involved in cardiac development, as well as the latest applied technologies and discoveries in this field, which will significantly enhance our understanding of cardiac development. Furthermore, we explore diseases associated with abnormal cardiac development and offer insights into future directions for managing CHD.
The history of cardiac development research
The exploration of cardiac development has a long and intricate journey (Fig. 1). With the advent of microscopy at the end of the 17th century, embryology experienced rapid development. This progress was significantly influenced by William Harvey (1578–1667) through his observations of deer and chick embryos, Caspar Friedrich Wolff (1733-1794) with his theory of epigenesis, and Karl Ernst von Baer (1792–1876) with his formulation of von Baer’s laws. These foundational works paved the way for Robert Remak’s (1815–1865) theory of the three germ layers in embryonic development.16,17 In 1927, Davis conducted the first morphological study of human heart embryos using postmortem material. He proposed that the heart consists of different segments, each giving rise to a definitive cardiac cavity, which he termed “primitive cardiac cavities”—including the aortic bulb, bulbus cordis, left ventricle, and atria (right and left). Davis also described a V-shaped plate called the cardiogenic plate within the splanchnopleure and the appearance of the sinus venosus.18,19
Timeline of milestone events in cardiac development research history. Each significant breakthrough in cardiac development research has been accompanied by advancements in related disciplines and technologies. The research of cardiac development starting with early studies observing morphological changes to exploration of molecular mechanisms using various molecular biology methods. Nowadays, advancements in stem cell technology and sequencing technology, such as the generation of cardiac organoids and multi-omics sequencing, have enabled researchers to understand the molecular mechanisms of cardiac development better. AV atrioventricular; AVC atrioventricular canal, CHD congenital heart disease, GATA4 GATA binding protein 4, hPSCs human pluripotent stem cells, Isl1 islet 1, MERFISH multiplexed error-robust fluorescence in situ hybridization, Mesp1 mesoderm posterior 1, Nkx2-5 NK2 homeobox 5, OFT outflow tract, PE proepicardium, RA retinoic acid, SHF second heart field, Tbx18 T-box transcription factor 18. This figure was created using Microsoft Powerpoint
In 1943, Rawles defined the cardiogenic mesoderm of the chick embryo as the region within the HH5 (Hamburger and Hamilton stage 5) lateral plate mesoderm with myocardial potential.20 With the advancement of molecular biology techniques, scientists have further explored cardiac development through lineage tracing and in vivo labeling. DeHaan’s group meticulously studied the morphological changes and fate map of the precardiac mesoderm in chicks. By transplanting radiolabeled donor embryos into stage HH5 chick embryos and comparing the initial and final positions of each transplant, they found that the morphogenesis of the heart likely occurs in a highly coordinated manner. This study identified the precise locations of precursors for different regions of the heart within these areas.21,22,23 Based on in vivo labeling and deletion experiments, researchers such as Castro-Quezada et al. 24 and de la Cruz and associates25,26,27 mapped the fate of the heart tube in chick embryos, indicating that primitive cardiac cavities do not directly form future definitive cardiac structures. Instead, new segments (primitive cardiac segments) appear during development from the heart tube to the early looping period, each contributing only to specific regions of the mature heart, differing from Davis’s conclusions. During this period, the complex regulatory mechanisms of cardiac development began to be understood. Researchers discovered that through the processes of torsion and looping of the cardiac tube, various primitive cardiac segments change their spatial positions and establish new relationships with each other, ultimately facilitating the normal septation of the heart.28,29
Moreover, significant findings have been made regarding the formation of the cardiac septum, valves, conduction system, and blood vessels.18 Endocardial cushions of the atrioventricular canal were found to play a crucial role in the formation of the cardiac septum and leaflets.28,30,31,32 Transplantation experiments suggested that embryonic blood vessels originate from multiple sources, forming and growing through vasculogenesis, angiogenesis, and the incorporation of local and wandering angioblasts.33,34,35,36,37 The roles of various molecules and signals in heart development have become increasingly recognized, including retinoic acid (RA);38,39,40 TFs such as NKX2-5,41 GATAs,42,43 and myocyte enhancer factor 2 (MEF2);44 and GFs such as fibroblast growth factor (FGF),45 transforming growth factor (TGF)-β,46 BMP-2.47 Other important factors involved in heart looping include flectin,48,49 heart and neural crest derivatives expressed (HAND)1, and HAND2.50 These discoveries have deepened our understanding of cardiac development, highlighting the complex, organized regulatory networks involved.
In 1977, de la Cruz and colleagues discovered that the outflow tract (OFT) is affected after heart tube formation, but the origins of these secondarily added cells remain uncertain.28 In 2001, several groups found that the OFT in chick hearts (HH18-22) is formed by mesodermal cells outside the classical heart-forming region, and in mice (from E8.25 to E10.5), the right ventricle (RV) and OFT myocardium are added from the pharyngeal arch core and splanchnic mesoderm, termed the SHF.51,52,53 Subsequent research has focused on SHF markers, functions, and regulation, with SHF now thought to reside in the pharyngeal mesoderm, contributing differently to the arterial and venous poles of the heart. Precursor cells from the anterior SHF contribute to the myocardium of the RV and OFT, as do smooth muscle cells associated with the great arteries. Cells added to the venous pole contribute to the myocardium of the atria and atrial septum.54,55,56,57,58 Islet 1 (ISL1),59 FGF8,60 and sine oculis homeobox homolog 2 (SIX2) have been identified as SHF markers,57 although some of these markers are nonspecifically expressed in other embryonic regions, including the FHF region.61,62 With the progress of technology and our deepened understanding of heart development, more detailed molecular regulatory mechanisms, such as the roles of epigenetic regulation and cilia in cardiac development, are being studied. These issues will be elaborated upon in the next chapter.
Recent developments in stem cell and bioinformatics techniques, especially the advent of human pluripotent stem cell (hPSC) technology and multi-omics analysis, have ushered our understanding of heart development in a new phase (Fig. 2). Through single-cell RNA sequencing analysis of mesoderm posterior 1 (Mesp1+) cardiac progenitors in mouse embryos at E6.75 and E7.25, Lescroart et al. identified distinct populations of Mesp1+ progenitors committed to different cell lineages and regions of the heart, including endothelial cells, cardiomyocytes (CMs), and anterior and posterior SHF populations, suggesting that Mesp1+ cardiac progenitor cells rapidly segregate from the outer layer of the embryo into distinct cardiovascular lineages.63 Single-cell sequencing technology has also enabled precise observation of gene expression and cell fate in FHF and SHF cells. A recent study revealed that primitive streak cells contributing to the ventricles exhibit a distinct molecular signature compared to those forming the OFT and atrium.64 Xiong et al. conducted single-cell transcriptomic analysis of Nkx2-5 and Isl1 lineages in mouse embryos from E7.75 to E9.25 and revealed that FHF cells differentiate rapidly into CMs, whereas SHF cells undergo gradual transitions to achieve their final cell fate, underscoring finely tuned regulation across multiple stages. Additionally, SHFs are attracted to the FHF-populated heart tube region through chemotactic interlineage communications mediated by macrophage migration inhibitory factor (MIF)—C-X-C motif chemokine receptor 2 (CXCR2).65 Another study replicated the development of FHF, anterior SHF, and posterior SHF in hPSCs using different differentiation protocols and identified the genetic characteristics of these cardiac lineages through single-cell sequencing, highlighting the pivotal roles of varying levels of Activin/Nodal and BMP signals in inducing mesoderm differentiation in FHF and SHF.66 Table 1 summarizes recent technological advancements in the field of cardiac development.
The molecular mechanisms of cardiac development were explored using pluripotent stem cell technology and multi-omics analysis. Pluripotent stem cells are generated by reprogramming adult somatic cells from CHD patients or animal models into a pluripotent state. These cells can differentiate into various cardiac cells, such as cardiomyocytes, smooth muscle cells, endothelial cells, and epicardial cells, through different differentiation protocols. Pluripotent stem cells can also form cardiac organoids through self-organization and specific differentiation methods, thereby creating an in vitro model of cardiac development. Multiomics analysis encompasses genomics, transcriptomics, proteomics, epigenomics, and metabolomics. By analyzing heart tissues obtained from CHD patients or animal models or cells derived from pluripotent stem cells, multi-omics analysis can be used to investigate the molecular mechanisms involved in the regulation of cardiac development at multiple levels. CHD congenital heart disease. This figure was created using Adobe Illustrator
The molecular mechanisms of cardiac development
To better understand the molecular mechanisms underlying cardiac development, it is essential to investigate the process of heart development. Various animals, such as chicks, mice, and human embryos, have been utilized in studies of cardiac development. Despite species differences, there are similarities in the processes and regulatory signals involved. Here, we primarily focused on human heart development to illustrate the developmental process (Fig. 3). In general, heart formation encompasses several stages, including pre-cardiac and cardiac mesoderm induction, formation of the cardiac crescent, heart tube formation, cardiac looping, and the formation of the four-chambered fetal heart. After birth, further maturation of cardiomyocytes involves cell cytoskeletal structure, metabolism, and a decrease in proliferation with occasional incomplete cell cycles. During the first week after birth, most cardiomyocytes complete their final cell division. Subsequently, the increase in heart size is largely achieved through the hypertrophy of cardiomyocytes. Recent reviews have extensively discussed cardiac development during this stage.67,68,69 This review focuses primarily on prenatal development. Cardiac development initiates when cardiac mesoderm progenitors migrate away from the primitive streak and coalesce in an anterior lateral region relative to the streak, known as the heart-forming region (HFR). These mesodermal cells acquire the ability to differentiate into cardiac lineages during migration, characterized by the expression of the MESP1 gene, which subsequently gives rise to both FHF and SHF progenitors.70,71 This process is regulated by various signaling pathways and molecules, including Activin/Nodal, BMP, FGF, and WNT/β-catenin signaling.1,72,73,74 Concurrently, as cardiac mesoderm cells migrate and differentiate, some undergo epithelial-to-mesenchymal transition (EMT) to form endocardial cells between the primary cardiac mesoderm and endoderm. These endocardial cells organize into a small network of channels that merge into larger channels as development progresses.75
Human cardiac development and its regulatory mechanisms. Cardiac development involves five distinct stages. The first stage, mesoderm cardiac induction (15-17 days), begins with cardiac mesoderm progenitors migrating from the primitive streak to the heart-forming region, an anterior lateral area relative to the streak. During migration, these mesodermal cells acquire the ability to differentiate into the cardiac lineage and express markers such as Brachyury and MESP1. The key signaling pathways involved include the Nodal/Activin, BMP, and WNT signaling pathways. In the second stage (17–19 days), the cardiac crescent forms, and MESP1-derived cardiac mesodermal cells differentiate into FHF and SHF progenitors. Molecular signals, including WNT signaling, BMP signaling, and various TFs, are critical. FHF progenitor cells, positioned more anteriorly and laterally in the crescent, readily respond to molecular cues and begin differentiation. SHF progenitors remain proliferative and undifferentiated until they reach later stages when they contribute to the heart tube. The third to fifth stages include heart tube formation (19–22 days), cardiac looping (22–35 days), and the formation of the four-chambered fetal heart (35–60 days). During these stages, the cardiac crescent fuses at the midline and folds into a Y-shaped FHF-derived linear heart tube. SHF cells proliferate rapidly and contribute to the arterial and venous poles of the heart tube. Subsequently, the heart tube undergoes rapid growth and rightward looping, forming distinct chambers by approximately day 32 in humans that are fully septated and connected to the pulmonary trunk and aorta by week 7 of fetal development. Events such as the migration of CNCCs, myocardial trabeculation, and the development of endocardial cushions and the epicardium are crucial during these stages. Signaling pathways, including FGF signaling, Notch signaling, and Shh signaling, are involved in the migration of CNCCs, promoting the development of the aortic arch and outflow tract. FGF signaling, Notch signaling, BMP signaling, and others contribute to myocardial trabeculation. Furthermore, FGF signaling, Notch signaling, TBX5, HAND1/2, and related signals aid in the development of endocardial cushions, facilitating subsequent septum and valve development. Finally, FGF signaling, TBX18, WT1, Notch signaling, and others contribute to epicardial development, promoting coronary artery formation and subsequent proliferation of myocardial cells. BRY brachyury, BMP bone morphogenetic protein, CNCCs cardiac neural crest cells, FGF fibroblast growth factor, FHF first heart field, GATA GATA binding protein, HAND heart and neural crest derivatives expressed, HFR heart-forming region, ISL1 islet 1, MEF myocyte enhancer factor, MESP1 mesoderm posterior 1, NKX2-5 NK2 Homeobox 5, RA retinoic acid, Shh sonic hedgehog, SHF second heart field, TBX T-box transcription factor, TGF transforming growth factor, TFs transcription factors, WT1 Wilms tumor 1. This figure was created using Adobe Illustrator
At approximately week 2 of human gestation, these cardiac mesoderm cells in the HFR form the horseshoe-shaped cardiac crescent, with the commitment to a cardiac fate remaining flexible.70 During this phase, MESP1+ cells further differentiate into FHF and SHF progenitors. Due to their positioning in the crescent (more anterior and lateral relative to SHF progenitors), FHF progenitors are more susceptible to regulation by BMP and FGF families, as well as inhibitors of the WNT pathway, which initiates their differentiation.76,77 In contrast, at a later stage, SHF progenitors remain in a proliferative undifferentiated state until they ingress into the heart tube.78
At approximately week 3 of human gestation, the cardiac crescent undergoes rapid growth and rightward looping, forming a linear heart tube with two posterior inflow tracts (venous poles) and one anterior outflow tract (arterial pole or outflow tract). The heart tube consists of the outer layers of two to three layers of myocardial cells and the inner layers of endocardial cells separated by the extracellular matrix (ECM) called cardiac jelly. At this stage, the heart tube begins to display slow contractions originating from the venous poles, and a sinusoidal morphology can be observed in electrocardiograms.79 Subsequently, SHF precursor cells from the dorsal and caudal regions of the pericardial cavity continue to migrate to the venous and arterial poles of the heart tube. SHF cells proliferate at a high rate mediated by classical WNT/β-catenin signaling and contribute to the arterial and venous poles of the heart tube during differentiation.80,81 Simultaneously, cardiac neural crest cells (CNCCs) delaminate from the neural tube and migrate toward the heart via preestablished pathways mediated by the BMP, FGF, WNT/β-catenin, and RA signaling pathways.82
At approximately the end of week 3 of human gestation, the heart tube undergoes further growth and rightward looping, with well-defined chambers visible around day 32 of human development. By week 7, the fetal heart was fully septated and connected to the pulmonary trunk and aorta.1,83,84 During this phase, SHFs continue to migrate to the venous and arterial poles of the heart tube. Myocardial cells in the outer curvature of the heart tube and atrial myocardial cells undergo transcriptional programs associated with chamber formation and re-entry of the cell cycle and proliferation, leading to ventricular “ballooning”.85,86,87 Concurrently, the cardiac jelly between the endocardial and myocardial layers disappears, and myocardial trabeculae become evident on the endocardial side of the chamber. Ventricular chambers start forming trabeculae under the control of Notch, Neuregulin (NRG), Ephrin (EFN), and BMP10 signalings.88,89 Subsequently, the outer layer of the myocardium begins to compact, reducing proliferation in myocardial trabeculae. During this period, development progresses in the cardiac septum, valves, epicardium, and conduction system. Atrial septation begins during the fourth developmental period and is mediated by the proliferation of atrial cells. Simultaneously, as the right ventricle and left ventricle form, the ventricular septum also begins to form.86 The septation process starts with the expansion of the cardiac jelly between the endothelial cell layer and myocardial cell layer of the atrioventricular canal (AVC) and OFT, which primarily involves posterior and anterior atrioventricular cushions in the AVC and parietal and septal outflow cushions in the OFT. Initially filled by endocardium-derived mesenchymal cells, Notch, BMP, and TGF-β signalings regulate the endocardial-to-mesenchymal transition (EndMT) in cushions.90,91,92 In addition to contributions from cells in the cushions, semilunar valves in the aorta and pulmonary trunk receive extracardiac contributions from CNCCs.90,93 These cells migrate to the heart via specific pathways mediated by EFN, FGF, semaphorins, and connexin 43,94 contributing to the development of the aortic arch arteries and OFT. Ablation of CNCCs results in disrupted Ca2+ handling and depressed ejection fraction,95 an interrupted aortic arch,96 a shortened OFT,97 and abnormal OFT septation.98
During this phase, the sinus venosus and sinoatrial node precursor are formed from T-box transcription factor (TBX)-5+, TBX18+, and hyperpolarization-activated cyclic nucleotide-gated potassium channel 4 (HCN4+) SHF progenitor cells. The dominant pacemaking activity gradually moves to the final sinoatrial node area.99,100 Developing ventricular and atrial chamber muscles acquire rapid cell-to-cell conduction properties due to the expression of connexin 40, connexin 43, Nav1.5, and other ion-handling proteins.101 Parts of the trabecular myocardium of the ventricles remodel into the Purkinje fiber network. The electrocardiogram of the heart also begins to transition from a sinusoidal waveform to a waveform resembling that of a mature heart, characterized by P waves, PR intervals, and QRS complexes.
The proepicardium (PE) arises around day 21 of human pregnancy from the coelomic mesenchyme of the septum transversum near the venous pole of the linear heart tube. Its development is primarily mediated by FGF and BMP signaling.102 These cells specifically express TBX18 and Wilms tumor 1 (WT1)103 and are released from the PE precursor by PE cell vesicles, flattening and spreading upon contact with the exposed myocardium to form the epicardium. The formed epicardium contributes to the formation of cardiac fibroblasts, vascular smooth muscle cells, and valves through epicardial EMT and the formation of epicardium-derived cells (EPDCs), mediated by TGF-β, Notch, and RA signals.104,105,106,107 The epicardium also secretes GFs such as FGF9, insulin-like growth factor (IGF)-2, and RA, which regulate the proliferation of ventricular myocardium closely adjacent to the epicardium.67,104 Next, we will provide a detailed summary of each important molecular mechanism regulating cardiac development and its effects at different stages of development.
Growth factors
Numerous studies have shown that GFs can mediate embryonic heart growth, determination, and differentiation through intercellular signaling at various stages of cardiac development. Among the most critical are the FGF family and members of the TGF-β family, including TGF-β1, TGF-β2, TGF-β3, BMP, Nodal, and Activin (Table 2). The FGF family comprises 22 multifunctional proteins identified in humans and mice that significantly influence early mesoderm induction, FHF and SHF formation, cardiac neural crest, and epicardium development.108 Previous studies have shown that FGF1 and FGF2 can induce mesoderm from naive prospective ectodermal cells in Xenopus.109,110 Further research revealed that paraxial mesoderm induction requires FGF signaling, while axial mesoderm induction relies on FGF signaling primarily for maintenance.111 FGF2 is also expressed in the PE, stimulating its differentiation into the epicardial lineage. In the proepicardial base, coexpression of BMP2 and FGF2 inhibits myocardial and epicardial differentiation.102 FGF4 and FGF8, along with their receptor FGFR4, are crucial for proper patterning of the paraxial mesoderm in the gastrula and left-right organizer, and their dysfunction leads to the loss of key genes involved in symmetry breakage, resulting in CHD associated with heterotaxy.112 FGF4 and FGF8 signal primarily through Hedgehog (Hh) signaling in the mesoderm.113 During the heart tube formation and looping stages, FGF8 and FGF10 are detectable in SHF.53,114 Abnormal Fgf8 expression results in significant loss of the Nkx2-5-Cre lineage and severe outflow and RV truncations by E9.5 in mouse embryos, mediated by decreased cell proliferation and aberrant cell death in both the pharyngeal endoderm and splanchnic mesoderm, while the remaining heart chambers (left ventricle and atria) appear grossly normal.115 Another study revealed that mesodermal Fgf8 is required for the correct alignment of the OFT and ventricles, while Fgf8 from the pharyngeal endoderm regulates outflow tract septation.116 High levels of FGF8 expression in the pharyngeal endoderm and ectoderm exhibit a chemotactic effect on cardiac crest cells, mediated by FGFR1 and FGFR3 along with mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK) intracellular signaling.117 FGF8 and FGF10 are involved in SHF progenitor proliferation, influencing the OFT and RV.60 Mutations in the FGF10 receptor Fgfr2-IIIb also lead to an underdeveloped OFT and RV, along with VSD associated with an overriding aorta or double outlet right ventricle (DORV), and include thin myocardial walls, trabecular abnormalities, and muscular VSD. Fgf10 and Fgfr2-IIIb mutant embryos lack pulmonary arteries and veins.118 Analysis of Fgf10-/- hearts and primary cardiomyocyte cultures revealed that Fgf10 regulates myocardial cell proliferation in fetal heart regions via the Forkhead Box O3 (FOXO3)/p27(kip1) pathway.119 FGF15 is present in the pharyngeal endoderm. Deficiency of Fgf15 results in heart defects consistent with malalignment of the aorta and pulmonary trunk, which correlates with early morphological abnormalities in the outflow tract due to abnormal behavior of the cardiac neural crest.120
The FGF9 subfamily includes FGF9, -16, and -20, which control myocardial differentiation and proliferation. FGF9, FGF16, and FGF20 are expressed in the endocardium and epicardium and signal specifically to the myocardium via FGFR1c and FGFR2c. Fgf9 knockout hearts exhibit disproportionate tissue loss in the heart apex and interventricular groove, reduced myocardial proliferation around the interventricular groove, atrial enlargement, and biventricular dilation.121 Fgf16 deficiency in embryonic hearts results in different outcomes in various mouse models. In C57 embryonic mice, Fgf16 deficiency results in slight decreases in heart weight and myocardial cell number by 6 months of age.122 In Black Swiss mice, Fgf16 deficiency leads to in-utero death, with common (or primitive) ventricular dilation and compromised trabeculae.123 These differences may stem from the distinct genetic backgrounds of the different mouse models. In the C57 embryonic mice, cardiac development does not completely depend on FGF16 for growth and differentiation. Specific genetic factors in C57 embryonic mice may rescue the embryonic lethality caused by Fgf16 deficiency. For example, relatively high levels of FGF9 in the C57BL/6 strain and the heightened sensitivity of Black Swiss mice to reduced FGF8 levels may explain the rescue of the embryonic lethality phenotype.123 Recent research has shown that FGF16 and FGF9 bind to different FGF receptors on cardiac progenitor and fibroblasts, promoting their proliferation. FGF16 also enhances proliferation in naive cardiac progenitor cells isolated from mouse hearts and human cardiomyocytes derived from induced pluripotent cells.124 Notably, functional redundancy may exist among the same FGF subfamily members; FGF16 and FGF20 likely act redundantly with FGF9 during cardiac development, signaling through FGFR1c and FGFR2c in the myocardium, similar to FGF9.121 Additionally, FGFs, including FGF1, -2, -7, and -9, are involved in angiogenesis and coronary development.125,126
The TGFβ family can be broadly divided into the TGFβ cluster and the BMP cluster. TGFβ and Activin ligands bind to specific receptor combinations to inhibit decapentaplegic (SMAD) 2/3 phosphorylation, while BMPs bind to receptors, leading to SMAD1/5/8 phosphorylation. Phosphorylated SMADs form complexes with SMAD4 and translocate to the nucleus to induce gene transcription.127 TGF-β family members also play significant roles in mesoderm induction and patterning. One of the earliest roles of TGF-β signaling in vertebrate development is the specification of mesendodermal cell fates by Nodal signaling. Loss of Nodal signaling results in the failure to form mesodermal and endodermal tissues.128,129 Nodal signals through Activin type II receptors (ActRII or ActRIIB) and primarily act on type I receptors ActRIB/ActR-like kinase (ALK)-4 or ALK7. Activin acts through ActRII or ActRIIB in conjunction with Alk4 or ActRIA/ALK2.72 Nodal family members are involved in patterning the mesoderm.130 As coreceptors of Nodal, Cripto is crucial for gastrulation and mesoderm formation. Cripto deficiency leads to the loss of somite and heart tissue in embryos, as well as the absence of cardiac-specific markers such as myosin heavy chain (Myh)-6, Myh7, myosin light chain (Myl)-2, Myl7, and natriuretic peptide A (Nppa).131,132 The absence of Activin-related receptors also disrupts primitive streak and mesoderm formation.133,134,135,136
At least 20 structurally and functionally related BMPs, including BMP-2, BMP-4, and BMP-10, which play roles in cardiac development, have been identified. Three receptor types, including BMP receptors, Activin receptors (ActRII, ActR-IIB), and an even larger number of type I receptors termed ALKs, mediate BMP binding, such as BMP2 and BMP4 binding to ALK3 and ALK6.72 Deficiency of Bmp4 and the BMP receptor causes embryonic lethality at E9.5, highlighting their crucial role in gastrulation and primitive mesoderm formation.134,137,138,139 Conditional deletion of BmpR1a in the Mesp1-Cre lineage results in the absence of the cardiac crescent and later primitive ventricle, indicating the essential role of BMP receptor signaling in FHF formation.140 Similarly, another study using Mox2-Cre to delete BmpR1a in the epiblast conditionally led to the lack of a distinct cardiac crescent structure or subsequent cardiac tissues.141
TGFβ and BMP signaling also play crucial roles in the later stages of cardiac development. Bmp2 deficiency leads to abnormal heart development in the exocoelomic cavity.142 Bmp10-deficient mice exhibit significantly reduced myocardial cell proliferation and severely thinned ventricular walls, accompanied by downregulation of the cardiac TFs Nkx2-5 and Mef2c.143 Conditional deletion of Bmp4 in the Tnnt2 or Nkx2-5-Cre linages results in AVC defects, abnormal morphogenesis of branchial-arch arteries, and defective OFT septation.144,145 Additionally, the contribution of TGF-β/BMP signaling to cushion development underscores its role in valve and septa development. During development, endocardial cells in the AVC and OFT become hypertrophic and undergo EndMT, transforming into mesenchymal cells that migrate into the cardiac jelly, eventually forming cardiac cushions.146 As EndMT progresses and mesenchymal cells proliferate, cardiac cushions continue to grow and develop into valves and septa. In mice, Tgfb1 and Tgfb2 are expressed in the endocardium and endothelium during development, particularly in the AVC and OFT, with Tgfb3 expression beginning after the onset of EndMT.147,148,149 Although single Tgfb1 or Tgfb3 deletions do not cause cardiac malformations, embryos and mothers lacking Tgfb1 show severe cardiac abnormalities, including valve disarray and vascular defects, indicating that maternally derived TGF-β1 is sufficient to rescue the cardiac phenotype in these knockout mice.150,151,152 Tgfb2 gene inactivation leads to heart defects, including atrial septal defects (ASDs) and VSDs, as well as enlarged cushions and valves.153,154 TGF-β1, -2, and -3 bind to TGFβRII with high affinity, activating ALK5 and downstream signaling. Alk5 deficiency leads to reduced mesenchymal cell proliferation and EndMT.155,156 Although mice with myocardial-specific Alk5 deletion do not exhibit cardiac defects, mice with endocardial-specific Alk5 deletion exhibit severely underdeveloped AV cushions, leading to septal defects.157 Further studies indicated that Tgfb2 activation in the endocardium requires interaction with TGFbRIII, without which the endothelial cell-cell separation step is inhibited.158,159 BMP ligands BMP2, -4, -5, -6, and -7 are expressed in the myocardium, covering the AVC and OFT.160,161 Myocardial-specific Bmp2 knockout results in reduced cardiac jelly and acellular cushion formation in the AVC.162 Bmp4 deficiency reduces cushion growth due to impaired proliferation, leading to OFT septation defects.145 However, another study suggested that Bmp4 is not required for EndMT indicating that Bmp4 mainly participates in the expansion and remodeling of the OFT endocardial cushion, rather than its initial EndMT, which results in severe OFT and VSDs.163 Notably, Bmp4 deficiency results in the upregulation of Bmp7 in the OFT myocardium, and compound knockout mice lacking both Bmp4 and Bmp7 show severely underdeveloped OFT cushions, indicating potential redundancy among Bmp4 and Bmp7 ligands.145 Additionally, in human pluripotent stem cells, BMP4 plays a crucial role in pacemaker cell differentiation, promoting the appearance of sinoatrial node CMs in conjunction with RA and Wnt signaling.164
TGF-β family members are also critical for epicardial development. Tgfb2 is expressed in the PE as early as E9.5, and Tgfb3 is expressed throughout the epicardium from E11.5 onward.147,165 Conditional deletion of Alk5 in epicardial cells using Gata5-Cre disrupts interactions between the epicardium and myocardium, leading to myocardial thinning, defects in the smooth muscle cell layer surrounding coronary arteries, and abnormal capillary formation in the myocardium.157 Tgfbr3 knockout mice exhibit coronary vessel formation failure and die by E14.5,166 which may be mediated by the inhibitory effect of TGF-β2 and BMP2 on epicardial cell invasion.167 In vitro application of TGF-β stimulates monolayer epicardial cells, inducing EMT characterized by morphological changes and increased EMT markers.165,168,169 BMP signaling also participates in proepicardial lineage determination. Myocardial-specific Alk3 knockout in epicardial cells results in a markedly reduced AV groove and severely underdeveloped fibrous annulus, although epicardial and EPDC formation remain unaffected.170 Inhibiting BMP signaling can rescue epicardial maturation defects caused by Wt1 knockout, suggesting that BMP signaling must be absent at specific stages for normal epicardial maturation.171
Transcription factors
The normal development of the heart involves the participation of many TFs, including NKX2-5, GATA family proteins, MEF2 factors, T-box factors, and the Lim-homeodomain protein ISL1. These TFs interact with each other and, along with other signals, regulate heart development (Table 2). For instance, BMP4 regulates the expression of NKX2-5 through GATA4, and NKX2-5 can regulate JARID2 expression to control heart development.9,18,172,173,174
NKX2-5 is first expressed in embryonic heart progenitor cells and continues to be expressed during the embryonic, fetal, and adult stages, where it controls multiple aspects of heart development.7 NKX2-5 can act synergistically with other cardiac TFs to promote CM differentiation and chamber identity. For example, it collaborates with HAND2 and MEF2C to promote cardiac ventricle formation175,176 and with GATA4 to promote cardiomyocyte differentiation.177 Previous studies have shown that Nkx2-5+ cardiac progenitor cells (CPCs) are not only involved in the cardiomyocyte lineage but also contribute to cardiac endothelial cells and smooth muscle cells.62,178 Recent single-cell sequencing has shown that Nkx2-5-expressing progenitor cells rapidly differentiate into CMs, contributing only to the CM lineage, possibly because the single-cell analysis focused only on cells actively expressing Nkx2-5, excluding their derivatives that had already ceased Nkx2-5 expression. One hypothesis is that the expression of Nkx2-5 quickly ceases after these progenitor cells differentiate into stable endocardial or smooth muscle cells. At E8.5, Nkx2-5+ cells co-express multiple cardiomyocyte and smooth muscle cell markers, suggesting that this population has the potential to differentiate into both cardiomyocytes and smooth muscle cells. However, this may also reflect the known expression of smooth muscle genes in immature cardiomyocytes.65,179 Nkx2-5+ progenitor cells also participate in the formation of the pulmonary myocardium at the junction of the pulmonary veins and atria. Interestingly, atrial cells do not participate in this process, suggesting that the pulmonary myocardium may originate from pulmonary mesenchymal cells.180 Additionally, NKX2-5 is crucial for the differentiation of the cardiac Purkinje fiber network.181,182 Thus, defects in NKX2-5 manifest not only as various cardiac developmental abnormalities but also as cardiac conduction defects and arrhythmias.183
GATA4 also plays a crucial role in heart development. GATA4 deficiency leads to the failure of midline fusion of the heart primordia and extensive endoderm defects, resulting in embryonic death.184,185 A gradual reduction in GATA4 leads to abnormal heart development, including in the common AVC, DORV, and underdeveloped ventricular myocardium.186 Patients with deletions in the GATA4 locus exhibit various cardiac developmental defects, including septation defects, OFT alignment defects, dextrocardia, and pulmonary stenosis (PS).187,188 This may be related to the interaction of GATA4 with other transcription factors, including NKX2-5, HAND2,189,190 TBX5,191 and ISL1.192 Combined defects in Gata4 and Tbx5 lead to complete atrioventricular septal defects (AVSDs), single atrioventricular valves, and myocardial thinning, while genetic interactions between Gata6 and Tbx5 can lead to neonatal lethality with thin myocardium.191 Mutations in Gata4 disrupt the physical interaction between Gata4 and Tbx5, leading to cardiac septal defects.193 These studies suggest the synergistic role of GATA4 and TBX5 in cardiac septum formation.
ISL1 is a LIM domain protein and a transcription factor that is transiently expressed during the appearance and expansion of SHFs and is downregulated as differentiation progresses.194 During development, ISL1 is expressed in the myocardial lineages of the distal OFT, atrial septum, and sinoatrial and atrioventricular nodes. It also contributes to the development of endothelial and vascular smooth muscle lineages, including the smooth muscle of coronary vessels.195 Further studies have shown that homeobox (Hox) genes (Hoxa1, Hoxb1, and Hoxa3) are temporarily expressed in early Isl1 progenitor cells.179 These genes encode highly conserved homeodomain TFs that play roles in septation, CNCCs migration, and OFT development.196 Isl1-expressing progenitor cells undergo gradient changes in key gene modules to adopt their terminal cell fate, indicating multiple steps of fine-tuned orchestration, thereby promoting the development of the OFT and RV.65,179 Mice lacking Isl1 show a complete absence of the OFT, RV, and most of the atria.59 Patients with heterozygous ISL1 mutations exhibit DORV combined with VSD,197 highlighting the crucial role of ISL1 in cardiac development.
Paired-like homeodomain transcription factor 2 (PITX2) encodes a paired related homeodomain transcription factor essential for cardiac development. During cardiac development, PITX2 has two main functions: morphogenesis of the OFT and left-right specification of the atria. As a target of canonical Wnt signaling, PITX2 functions in both cardiac neural crest and mesoderm-derived SHF, regulating OFT myocardial proliferation and promoting OFT development in the SHF.198,199 In the left atrium, PITX2 determines left atrial morphology. Mutations in Pitx2 result in left atrial characteristics, including venous valves and trabeculated myocardium, resembling those of the right side.198 Pitx2 deficiency leads to AVC with prominent swelling and juxtaposition of the atrium, accompanied by undeveloped tricuspid and mitral valves and the formation of a common atrioventricular valve, indicating the role of Pitx2 in valve development as well.200 Single-cell sequencing revealed that Pitx2 deficiency disrupts the differentiation dynamics of both anterior and posterior SHF-derived progenitor cells, preventing the activation of Tgfb1 and Hand1 in the OFT.201 Additionally, Pitx2-deficient embryos exhibit bilateral or ectopic sinoatrial nodes and defects in the pulmonary myocardial sleeve, which may explain the susceptibility to atrial fibrillation observed in adult animals with reduced PITX2 expression.180,202,203
Nuclear transcription factor Y subunit a (NFYa) is involved in regulating cell proliferation and metabolism. A recent study revealed that NFYa is expressed in the embryonic heart. Spatial and single-cell transcriptome sequencing revealed that Nfya deficiency leads to reduced CM proliferation and impaired mitochondrial metabolism, accompanied by a decrease in the number of immature regenerative cells and an increase in the number of trabecular and mature CMs. These effects are likely due to NFYa’s interaction with its cofactor SP2, which activates metabolism- and proliferation-related genes at the transcriptional level.204 However, research on the role of NFYa in heart development is still limited, and further studies are needed to explore its functions in this context.
HAND proteins are basic helix-loop-helix (bHLH) proteins that can form homo or heterodimers with bHLH partners, regulating gene expression. During mouse heart development, HAND factors are expressed in various or overlapping regions of CNCCs, the epicardium, the myocardium, and the endocardium.205 Early studies showed that HAND1 is primarily expressed in the left ventricle and is also expressed in CNCCs and the OFT, while HAND2 is strongly expressed in the endocardium and is also expressed in CNCCs, the OFT, and the epicardium. Mice lacking Hand2 exhibit severe right ventricular hypoplasia, a thin myocardium, a dilated aortic sac, and VSD.50,206,207,208 Mice with a global knockout of Hand1 die at E9.5 due to defects in extraembryonic tissues and cardiac morphology.209 Cardiac-specific Hand1 deletion leads to defects in the left ventricle and endocardial cushions and dysregulation of ventricular gene expression, with embryos surviving to the perinatal stage but dying from various cardiac abnormalities.210
Further studies revealed that conditional loss of Hand1 and Hand2 in the left ventricle causes abnormal trabeculation and thickened compact myocardium by mediating abnormal proliferation and differentiation, highlighting the role of HAND factors in left ventricular development.211 Interestingly, transgenic embryos with Hand2 expression throughout the ventricles show expanded boundaries between the left and right ventricles, with complete septal absence, indicating the critical importance of Hand2 expression balance for ventricular morphology.212 Single-cell sequencing identified Hand2 as a specifier of OFT cells but not RV cells. Temporal single-cell transcriptome analysis revealed that Hand2 deletion results in an undifferentiated OFT myocardium, while the right ventricular myocardium, although differentiated, fails to migrate properly to the arterial pole or differentiate, accompanied by disrupted RA signaling and anterior-posterior patterning of cardiac progenitors.213 Using Mef2c-, Tie2-, or Nfatc1-Cre to delete Hand2 specifically, researchers found that endocardial HANDs act downstream of the Notch endocardium-to-myocardium signaling pathway to regulate NRG1, leading to tricuspid atresia, double inlet left ventricle, and reduced ventricular trabeculation, suggesting that HAND2 plays a role in endocardial development.208,214 During epicardial development, HAND2 is downstream of HAND1, and HAND2 deficiency impairs epicardial EMT, preventing the normal formation of cardiac fibroblasts and coronary vessels, further emphasizing the role of HAND2 in epicardial development.215
TBX5 mutations were first discovered in human Holt-Oram syndrome patients who had secondary atrial and ventricular septal defects and defects in the cardiac conduction system.216 Tbx5-deficient embryonic mice exhibit incomplete heart septation and conduction block, along with underdeveloped atria, while Tbx5 overexpression inhibits ventricular maturation.217 TBX5 can physically interact with MEF2C to activate the expression of MYH6 in cardiomyocytes, and dual knockdown of Tbx5 and Mef2c causes severe defects in heart tube looping.218 Previous research has highlighted the role of TBX5 in septation. TBX5-mediated Hh signaling is required in the SHF for atrial septation in mice.219 TBX5 expression at ventricular boundaries defines the location of muscular septum formation in avian hearts, with TBX5-misexpressing hearts showing ventricular septum formation issues, resulting in a single ventricle.220,221 Additionally, Tbx5 and Mef2c exhibit genetic interactions during ventricular septum formation, producing muscular septal defects, and Mef2c co-regulates Tbx5 target genes.222 Using Mef2c-anterior heart field (AHF)-Cre mice, researchers found that AHF Mef2c+ cells primarily contribute to the development of the OFT, RV, and septal endocardial and myocardial components.223 The entire murine left ventricle, including the left side of the septum, expresses Tbx5, and further analysis revealed a small group of cells in the intersectional lineage expressing both Mef2c and Tbx5.224 These results suggest that TBX5 and MEF2C play synergistic roles in cardiac development, particularly during septation.
Other T-box factors also play significant roles in heart development. TBX1 is expressed in a multilineage-primed population within the cardiopharyngeal mesoderm, regulating the progressive differentiation of these cells into anterior and posterior SHF cells in the posterior pharyngeal region.225 TBX1 also interacts with the [brahma-related gene 1 (BRG1)/brahma (BRM)-associated factor 60a] (Baf60a)/[switch (SWI)/sucrose non-fermentable (SNF)-related, matrix-associated, actin-dependent regulator of chromatin] (Smarc)-d1 subunit of a chromatin remodeling complex to regulate Wnt5a expression, influencing cardiac progenitor differentiation.226 Tbx1 deficiency leads to DiGeorge syndrome with various cardiac defects, including reduced proliferation in the SHF, aortic arch patterning defects, and OFT anomalies.227,228,229 Genetic tracking using Tbx2-Cre alleles showed that myocardial cells of the free wall and base of the left ventricle are gradually added from Tbx2-expressing cells in the AVC, which downregulates Tbx2 expression upon leaving the canal. TBX2 functionally suppresses the chamber program in the AVC.230 TBX2 and TBX3 coordinate with BMP2 to trigger cushion development and locally repress chamber differentiation during chamber differentiation, stimulating AVC myocardium and AV nodal phenotype development and coordinating heart development.231 TBX18, along with other TFs such as WT1 and transcription factor 21 (TCF21), is expressed in epicardial progenitor cells and contributes to epicardial development. These functions are crucial for epicardial EMT and the subsequent formation of coronary vessels and interstitial fibroblasts.232,233,234 Single-cell sequencing further confirmed the role of Tbx18+ cells in epicardial EMT and the development of fibroblasts and cardiomyocytes.235 The cardiogenic mesoderm contains an additional subset of Tbx18-expressing progenitors proposed to form the Tbx18+/Nkx2-5- sinus venosus and PE.236 TBX20, which acts upstream of TBX2 in heart development, causes heart formation defects when deficient, including AVC constriction, OFT and RV hypoplasia, and reduced expression of NKX2-5, HAND1 and -2, and MEF2C.237,238,239
WNT signaling
In addition to various GFs and TFs, multiple signaling pathways regulate heart development. Table 3 summarized the signaling pathways commonly involved in cardiac development. The WNT signaling pathway plays a crucial role in heart development, especially during the early stages.
WNT was first discovered in mice in 1982 and was identified as a homolog of the Drosophila wingless gene in 1987.240,241 WNT, a secreted signaling molecule, includes 19 ligands that function through Frizzled (Fz) receptors.242,243 Although three distinct WNT signaling pathways (the canonical WNT/β-catenin, the noncanonical WNT/planar cell polarity and WNT/calcium pathways) operate independently, they interact to form a complex signaling network influencing every stage of cardiac development.240 WNT1, -2, -3, -3a, -8, and -8b primarily act through the canonical pathway, while WNT4, -5a, -5b, -6, -7a, and -11 primarily act through noncanonical pathways.244 When WNT binds to a seven-transmembrane (7TM) heterodimeric receptor complex containing Fz receptor 2 (Fz-2) or the frizzled and protein low-density lipoprotein receptor-related protein (LRP)-5/6, the canonical WNT pathway is activated, leading to Disheveled (Dsh) hyperphosphorylation, which inhibits glycogen synthase kinase-3β (GSK-3β) in vertebrates, causing β-catenin accumulation and translocation to the nucleus, where it affects the expression of development-related genes.245 The WNT/planar cell polarity pathway activates the c-Jun N-terminal kinase (JNK) and [rat sarcoma homologous (Rho)-associated protein kinase] (ROCK) kinases through interactions between Dsh proteins and Rho family GTPases.246,247 The WNT/calcium pathway relies on phospholipase C, which triggers the release of calcium ions into the cytoplasm, activating protein kinase C, calcium/calmodulin-dependent protein kinase II, and calcineurin.248
The WNT/β-catenin pathway is essential for mesoderm induction and patterning.249,250,251 Previous studies suggested that WNT signaling is necessary for the patterning and expansion of SHF progenitors by activating a series of FGFs, such as FGF3, FGF10, FGF16, and FGF20, which in turn activate FGF signaling.252,253 Ablation of β-catenin in Isl1-expressing progenitors disrupts heart development in multiple ways, causing defects in the expression of essential cardiac genes such as Tbx2, Tbx3, and Pitx2. Conversely, activation of β-catenin signaling in Isl1+ progenitors inhibits differentiation and causes morphogenic defects in the OFT.254,255 Conditional knockout of β-catenin in Mesp1+ cells disrupts cardiac looping and right ventricle formation, accompanied by the expansion of ISL1- and BMP4-expressing cells and the absence of the heart tube.140 Deletion of Wnt2 and Wnt11 similarly results in a reduction in posterior SHF progenitors and defects in the cardiac OFT and ventricular wall, respectively.256,257,258 Another study revealed that deletion of Wnt5a and Wnt11 leads to a significant loss of SHF progenitors during heart development, accompanied by increased Wnt/β-catenin signaling.259 Overexpression of Wnt5a affects the deployment of SHFs, preventing them from entering the OFT and leading to OFT shortening. Wnt5a deletion results in a reduction in the inferior OFT myocardial wall and its derivative, subpulmonary myocardium, and fails to extend into the arterial and venous poles, causing both OFT and ASD.260,261,262 A recent study revealed that WNT11 restricts the WNT/β-catenin signaling pathway through caspase-mediated degradation, which is necessary for cardiomyocyte differentiation.263 Single-cell sequencing revealed a specific subset of proximal OFT progenitor cells expressing the WNT signal activator gene leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5) in the human heart, which may promote the expansion of a transitional cell population to achieve correct arterial pole alignment.264 These findings indicate that WNT signaling plays a crucial yet complex role in SHF development.
Precise activation and inhibition of WNT signaling are key to regulating normal heart development. Research has further suggested that WNT signaling has a biphasic role in cardiac development. While activation of the WNT/β-catenin pathway is essential for early specification of mesoderm and cardiac progenitor cells, its activation at later stages inhibits heart development.265,266 The endoderm-derived WNT inhibitor Dickkopf (Dkk) can suppress WNT signaling and induce heart-specific gene expression in the posterior lateral plate mesoderm.267 This finding was corroborated by in vitro stem cell studies. During the early differentiation of human embryonic stem cells (hESCs) into human cardiomyocytes, WNT3 and WNT8A activate the canonical signaling pathway through Fz-7, promoting mesoderm induction and Brachyury expression. Subsequently, WNT5A/5B activates the WNT/planar cell polarity pathway through receptor tyrosine kinase-like orphan receptor 2 (ROR2), promoting MESP1 expression and differentiation of the cardiogenic mesoderm. Finally, WNT2, WNT5A/5B, and WNT11 activate the WNT/calcium pathway through F Fz-4 and Fz-6, working in conjunction with inhibition of the canonical pathway to promote CM differentiation.268 In hPSCs, temporal regulation of WNT signaling is critical for generating functional cardiomyocytes and pacemaker cells.269,270,271,272,273
WNT signaling also plays an important role in the endocardial cushion, valve, and epicardial development. At E12.5, WNT2 is expressed in the cushion mesenchyme, while WNT4 and WNT9B are mainly expressed in overlying endothelial cells. By E17.5, WNT3A and WNT7B are expressed in the atrioventricular and semilunar valves.274 Deletion of β-catenin leads to underdeveloped endocardial cushions with reduced mesenchymal cell proliferation.275 Overexpression of the WNT inhibitor Dkk1 prevents cushion formation.276 Moreover, Tbx20 deficiency causes severe valve extension defects and impaired cardiac function in mice, which is potentially mediated by the WNT pathway.277 WNT5A and WNT9B are expressed in the epicardium.278,279 Epicardial-specific deletion of β-catenin results in lethality between E12.5 and birth, resulting in impaired coronary formation, subepicardial space expansion, weakened myocardial invasion, and severely thinned ventricular myocardium.280,281
Furthermore, in embryos lacking the epicardial transcription factor WT1, epicardial EMT is inhibited, which is mediated by weakened canonical and noncanonical WNT signaling.279 Deletion of β-catenin also disrupts adherens junctions and randomizes the mitotic spindle orientation of epicardial cells, thus impairing epicardial EMT.282 Overall, WNT signaling plays multiple roles in heart development, including the specification of cardiac mesoderm and subsequent differentiation and proliferation, serving as a critical regulatory mechanism throughout cardiac development.
Retinoic acid
RA is synthesized from retinaldehyde through oxidation by retinaldehyde dehydrogenases (RALDH 1-3), with RALDH2 being the primary source of RA during embryonic development. RA enters the nucleus by binding to cellular RA binding proteins (CRABP) to regulate gene expression and can exert its effects by binding to retinoic acid receptors (RARs) and retinoic acid X receptors (RXRs).283,284 The critical role of RA in heart development has been established since early studies.18 RA is now known to play essential roles, from the early formation of anterior-posterior boundaries of the cardiac mesoderm to the development of the epicardium and the subsequent formation of normal cardiac morphology. RALDH2 is expressed in the posterior lateral plate mesoderm in mice at E7.5-E8.0, suggesting that caudal cardiac precursors are primarily exposed to RA.285 Subsequently, from E9.5-E12.5, RALDH2 expression gradually extends to the developing atria and epicardium.64,286,287,288 Deficiency of Raldh2 in zebrafish leads to specific increases in cardiac precursor cells in the anterior lateral plate mesoderm, resulting in larger hearts with increased numbers of atrial and ventricular cardiomyocytes, indicating a crucial role for RA in restricting the cardiac precursor area in the anterior lateral plate mesoderm.289,290 Deletion of Raldh2 at E8.0-E9.0, although after cardiac crescent formation, leads to downregulation of SHF-related genes at the pharyngeal level of the anterior SHF and posterior expansion.291,292 The LIM domain protein Ajuba inhibits ISL1 expression in an RA-dependent manner, thereby restricting SHF expansion.293
Furthermore, TBX1 in the anterior SHF antagonizes RA signaling, while the induction of TBX5 in the posterior SHF depends on RA signaling.294 Therefore, RA signaling plays crucial roles in the generation and maintenance of cardiac precursor cells in the anterior SHF and in delineating the boundary between the anterior and posterior SHF. Embryos with RXRa deficiency exhibit complex cardiac developmental defects, including VSD, atrioventricular cushion defects, and conotruncal ridge defects, with DORV, an aorticopulmonary window, and persistent truncus arteriosus (PTA).295 Deficiency of Raldh2 results in incorrect heart looping, severe defects in atrial and sinus venosus development, impaired formation of ventricular trabeculae, and defects in OFT septation.296 Subsequent studies revealed that RA acts on ventricles through RXRa receptors in the epicardium.278 Similarly, a lack of RA signaling in zebrafish significantly increased differentiation of FHF cardiomyocytes, markedly decreased OFTs and disturbed pacemaker cell differentiation.297 Interestingly, excess RA also leads to cardiac developmental defects, particularly abnormal OFT development, indicating that proper regulation of RA signaling is crucial for normal OFT development.298,299,300
RALDH2 expression in the epicardium begins as early as in the anterior epicardium at E9.5. While RA signaling is not essential for the initial formation of the epicardium, it exerts a significant influence on its subsequent differentiation.301 Epicardial WT1 directly activates RA signaling to regulate the expression of platelet-derived growth factor receptor a (PDGFRa), thereby modulating epicardial EMT.302 RA induces the expression of TCF21 and FGF9 in the epicardium, promoting their differentiation into fibroblasts and participating in myocardial proliferation and ventricular expansion, respectively.121,233 Excess or reduced RA signaling disrupts epicardial EMT, resulting in reductions in ventricular coverage, coronary vessel density, altered vessel morphology, and impaired recruitment of epicardial-derived mural cells.303 Additionally, RA signaling in the epicardium is necessary for cytoskeletal rearrangements during epicardial EMT, thereby promoting the infiltration of EPDCs into the myocardium.304 Under physiological conditions, high levels of RA synergize with myocardial-derived vascular endothelial growth factor (VEGF) to inhibit EPDC differentiation into coronary smooth muscle cells, ensuring the establishment of an extensive endothelial network.305
In recent years, studies using stem cells as in vitro models have extensively investigated the role of RA in myocardial and epicardial differentiation. In mouse embryonic stem cells (mESCs), differentiation into atrial cardiomyocytes in vitro is observed with different concentrations of RA.306 In hESCs, RA treatment at the cardiac progenitor stage promotes differentiation into atrial cardiomyocytes.307 Furthermore, Devalla et al. reported that atrial differentiation depends on the stimulation of RA signaling shortly after the peak expression of MESP1 in the cardiac mesoderm stage, a process mediated by meis homeobox 2 (MEIS2) and antagonized by ISL1 to induce the expression of the atrial transcription factor nuclear receptor subfamily 2 group F member 1 (NR2F1).308,309 In the absence of RA or other late induction signals in vitro, default differentiation of MESP1+ cardiac mesodermal cells leads most cell lines generated with existing differentiation protocols toward the ventricular lineage. Inhibiting RA signaling during differentiation may direct cells toward a ventricular fate.307,310 In contrast to in vivo findings, in vitro studies have shown that RA treatment can guide hPSC differentiation into PE. RA treatment synergizes with BMP4, VEGF, and WNT to guide hPSC differentiation into pro-Epi-like and Epi-like cells.284,310,311
Notch signaling
Notch proteins, including Notch1-4, are single-pass transmembrane receptors found in mammals. Their ligands are transmembrane proteins on adjacent cell surfaces, including Delta–Serrate–Lag family ligands such as Delta-like protein (DLL)-1, -3, and -4, as well as Jagged family ligands such as Jagged (JAG)-1 and -2. Upon ligand binding, the receptor-bound ligand is modified by the E3 ubiquitin-protein ligase mindbomb (MIB)-1, activating Notch signaling. Subsequently, the γ-secretase complex and disintegrin and metalloproteinase (ADAM) proteins cleave and release the Notch intracellular domain (NICD), allowing it to translocate into the nucleus. Inside the nucleus, the NICD binds to the recombination signal binding protein for the immunoglobulin kappa J region (RBPJ) and recruits the coactivator mastermind-like protein 1 (MAML1), releasing corepressors (Co-Rs). The hairy and enhancer of split (HES) and [hairy/enhancer-of-split related to tyrosine-arginine-proline-tryptophan (YRPW) motif] (HEY) families of basic helix–loop–helix transcription repressors are well-known Notch targets.89,312,313,314 Newly activated transcription complexes driven by Notch target genes promote normal heart development. Mutations in Notch signaling molecules can lead to various forms of cardiac developmental defects, including BAV, VSD, overriding aorta, hypoplastic left heart, and incomplete right ventricular development.315,316,317,318,319,320,321,322 Notch signaling begins to function early in cardiac development. Activation of Notch signaling in the cardiac mesoderm reduces myocardial gene expression in Xenopus embryos, accompanied by increased expression of mesocardium and pericardial roof genes, whereas inhibition of Notch signaling promotes cardiac differentiation.323 Activation of Notch signaling in early embryonic stages reduces cardiac mesodermal transcript expression,324,325 and this phenomenon of Notch signaling inhibiting cardiac differentiation early in differentiation is also observed in mESCs.326,327,328 A recent study revealed that noncanonical Notch signaling, which does not depend on the transcription factor RBPJ, can inhibit cardiac development by inducing damage to the SHF.329 Abnormal expression of Notch1 driven by Mesp1-Cre leads to abnormal heart morphogenesis characterized by ventricular and AVC deformities.330 Defects in Rbpj and Notch1 driven by Mesp1-Cre and Isl1-Cre, respectively, lead to incomplete RV development. In Isl1+ cells, Notch1 promotes SHF differentiation by downregulating WNT/β-catenin signaling,331 while in Mesp1+ cells, Notch signaling similarly regulates SHF differentiation as an upstream signal of WNT and BMP.332 Defects in Jag1 in the SHF lead to abnormalities in the mouse aortic arch and heart, accompanied by decreased expression of Fgf8 and Bmp4, defective migration of CNCCs, and defects in EndMT within the OFT endocardium.333 These results indicate that Notch signaling plays a role early in cardiac development, coordinating the development of cardiac precursor cells in the cardiac mesoderm and interacting with signals such as FGF, BMP, and WNT to regulate SHF progenitor cell differentiation.
Notch signaling is crucial for valve system development. Notch is highly active in the AVC and OFT endocardial cushions, cooperating with TGF-β, BMP, and WNT signals to induce EndMT. Disruption of Notch signaling impairs EndMT, leading to valve malformations such as enlarged valve cusps, BAV, DORV, and septal defects.330,334,335,336,337,338,339,340 Furthermore, defects in Notch signaling lead to excessive interstitial cells and abnormal valve thickening, possibly mediated by apoptosis regulated by Notch-RBPJ signaling to modulate leaflet remodeling341 or by limiting interstitial cell proliferation mediated by the activation of heparin-binding EGF-like growth factor (HBEGF).336 Aberrant expression of Notch1 using Tie2-Cre increases EndMT in AVC and ventricular endocardial cells but also leads to midgestation lethality with defects in angiogenic remodeling of embryonic and yolk sac vasculature, cardiac development, smooth muscle cell investment in vessels, and hematopoietic differentiation.337,342 In zebrafish, overexpression of N1ICD in endothelial cells leads to hypertrophic cardiac valves.343 Interestingly, Notch signaling also affects the development of the conduction system. Activation of Notch signaling results in fully penetrant accessory pathways and ventricular preexcitation, similar to what occurs in human Wolff‒Parkinson‒White syndrome, while inhibition of Notch signaling leads to hypoplastic AV nodes, specific loss of slow conduction cells expressing connexin-30.2, and loss of physiological atrioventricular conduction delay.344
Notch signaling also plays an important role in ventricular development. During the trabeculation stage, NOTCH1 is expressed in ventricular endocardial cells at the base of forming trabeculae, while its ligands DLL4 and JAG1 are expressed at the base of forming trabeculae and in myocardial cells forming trabeculae, respectively.345,346 Defects in DLL4 in the endocardium lead to impaired trabeculation and reduced expression of markers, including G protein-coupled receptor (Gpr)-126, Bmp10, Efn-b2, and Nrg1, resulting in trabecular formation disorders.346 Similarly, mutations in Rbpj and Notch1 lead to reduced expression and signaling of EFNB2, NRG1, and BMP10, decreased myocardial proliferation, and embryonic lethality at E10.5.345 Thus, NOTCH1 plays an important upstream role in trabeculation by regulating the expression of EFNB2, NRG1, and BMP10.
Another study revealed that NOTCH1 signaling promotes ECM degradation, while NRG1 promotes myocardial ECM synthesis, with NRG1-mediated VRGFa regulation linking these two systems to promote trabecular remodeling and growth.88 Recent studies also suggest the importance of Notch in coronary development. Notch signaling is activated to varying degrees during the transition from the PE to the epicardium-coronary artery, and specific deletion of Notch1 using Wt1-Cre leads to coronary artery differentiation disorders, thin myocardial walls, decreased myocardial cell proliferation, and reduced Raldh2 expression.286 Defects in Rbpj in the epicardium lead to disturbances in EPDC differentiation into coronary smooth muscle cells, while conditionally activating Notch signaling leads to premature differentiation of epicardial cells into smooth muscle cells and prevents coronary artery vasculogenesis.347 Another study revealed that prior to primary coronary plexus formation, coronary arterial precursors are specified through Notch in venous sinuses, with subsequent arterial differentiation depending on the DLL4-JAG1-EFNB2 signaling cascade.348
Hedgehog signaling and cilia
The Hh signaling pathway was first discovered in Drosophila and later identified in mice and humans with three Hedgehog genes: Sonic Hedgehog (Shh), Desert Hedgehog (Dhh), and Indian Hedgehog (Ihh).349,350 Among them, Shh has been found to be most strongly associated with heart development. The classical Shh signaling cascade involves the binding of Shh to its receptor, Patched-1 (PTCH1), which is located on the primary cilium membrane of the cell. Upon Shh binding, PTCH1 inhibits the transmembrane receptor Smoothened (SMO), promoting its accumulation in the primary cilium. This activation leads to the regulation of gene expression through glioma-associated (GLI) transcription factors.351 Both overexpression and downregulation of Hh pathway components can lead to cardiac developmental defects. In zebrafish, reduced Hh signaling results in defects in cardiac muscle cells, while increased Hh signaling leads to an excess of cardiac muscle cells, ensuring the appropriate number of myocardial progenitor cells during early cardiac development.352 Early expression of Shh occurs in the floor plate of the murine notochord, dorsal to the cardiac region, followed by the formation of a Shh gradient in the pharyngeal endodermal region and the ventral aspect of the cardiac region in developing embryos. After the initial formation and extension of the primitive heart tube, the Shh ligand is produced and secreted from the pharyngeal endoderm of branchial arches 3, 4, and 6.353 Loss of Shh results in widespread failure of pharyngeal arch development, leading to defects in the arch artery and OFT patterning, as well as abnormal migration of CNCCs, causing cardiac defects.354
Further studies confirmed that the Shh ligand produced by the endoderm is essential for CNCCs survival and filling of OFT cushions while also mediating signals from AHF myocardial cells to complete septation after cushion formation.355 Subsequent experiments also revealed that Shh is necessary for dorsal mesenchymal protrusion (DMP) and the formation of atrioventricular septation.356,357 Conditional deletion of Smo in the SHF impairs the development of the cardiac venous pole, resulting in hypoplasia of the atrium/inflow tract and bradycardia, accompanied by decreased expression of critical developmental genes in the inflow tract sinus node, as well as failure of EndMT in the atrioventricular cushion, suggesting its potential role in the development of the conduction system and valves.358
Compared with that of the Hh signaling pathway, the influence of cilia on cardiac development has been studied more deeply. Cilia are divided into motile, nodal, or primary types, with a 9 + 0 or 9 + 2 ultrastructural arrangement of axonemal microtubules. Many highly complex and tightly coordinated developmental signaling pathways in embryonic heart development depend on primary cilia, which are prominent antennae-like structures present in almost all eukaryotic cell types.359,360 The primary cilium is characterized by its core comprising an axoneme of nine microtubule doublets arranged around a central space devoid of microtubules.361 Intraflagellar transport (IFT) uses the microtubule doublet central core to transport proteins bidirectionally into and out of the cilium. In mammals, IFT utilizes kinesin family member 3A (KIF3A) for anterograde transport, while cytoplasmic dynein enables retrograde transport.362 Primary cilia not only regulate Hh signaling but also have close connections with calcium signaling,363,364 WNT signaling,365 TGF-β,366 and Notch signaling.367 These primary cilia are present in the endocardium, myocardium, and epicardium of the embryonic heart.368,369 The initial stage of cardiac left-right development is initiated within a transient ciliated epithelium known as the left-right organizer, where motile and primary cilia play a crucial role in establishing the left-right asymmetry of the body axis and proper placement and patterning of internal organs, including the heart.370,371,372 Defects in ciliary signaling result in severe congenital heart defects, including heterotaxy syndrome, AVSD, and transposition of the great arteries (TGA).373,374,375
In a study by Slough et al., cilia were found in the embryonic mouse heart from E9.5 to E12.5, and after Kif3a knockout, abnormalities in endocardial cushions and compact myocardium development were detected.376 Defects in polycystin (PKD)-2 and -1 located on primary cilia are associated with defects in cardiac development, including disturbances in ventricular and atrial septum formation, disorganization and thinning of myocardial walls, and DORV.377,378 In a globally reduced cilia model in the developing mouse heart, severe developmental defects were observed, including the formation of a single OFT, AVSD, an enlarged pericardial sac, dilated atrial chambers, and decreased expression of the Hh signaling molecules GLI1 and PTCH1, resulting in embryonic mice dying around E13.5.379 Deficiency in Ift88 leads to ventricular dilation at E11.5 in mouse embryos, reduced myocardial trabeculation, and abnormal OFT development.380
Cilia plays a crucial role in valve development, and patients with ciliopathies often have cardiac valve defects.381 Multiple cilia genes have been found to be associated with AVSD. Furthermore, mutations in cilia motility-related genes lead to AVSD only in the presence of heterotaxy syndrome, whereas mutations in cilia signaling-related genes lead to AVSD regardless of whether there are left-right patterning defects, perhaps because AVSD caused by mutations in cilia-motility genes results from situs abnormalities and does not involve Hedgehog signaling in SHF. In contrast, mutations in cilia signaling-related genes disrupt Hedgehog signaling in SHF, leading to AVSDs with or without laterality defects.382 Nonciliated mouse embryonic endothelial cells with a mutation in Tg737/Ift88 were found to induce EndMT under shear stress through TGF-β signaling.383 In another study, the absence of primary cilia led to the enlargement of mitral valve leaflets, manifested as the expansion of the ECM and histological damage.369 The expression of Dhh in the endocardium is necessary for cilium-induced activation of the T-lymphoma invasion and metastasis-inducing protein (TIAM)-1-Ras-related C3 botulinum toxin substrate (RAC)-1 axis, which in turn stimulates the ECM remodeling required for proper valve remodeling.384 Primary cilia are also expressed on aortic valve interstitial cells and are lost as these cells differentiate into fibroblast-like cells. Loss of Ift88 results in primary cilium loss increased fibrotic ECM production, and the occurrence of BAV.385 In summary, these results highlight the importance of cilia in cardiac development, particularly in early left-right organizer and subsequent valve development, as well as their impact on the OFT and ventricle formation.
Cell proliferation and Hippo signaling
Cell proliferation refers to the process by which cells multiply and increase in number and involves a series of events known as the cell cycle, which consists of distinct phases, such as the gap0 (G0) phase, gap1 (G1) phase, synthesis (S) phase, gap2 (G2) phase, and mitosis (M) phase. During heart development, cell proliferation plays a crucial role in the growth and formation of the heart. It involves the multiplication of cells, contributing to the expansion of different cardiac tissues, such as the myocardium, endocardium, and valves. In the early phases of cardiac development, upon the formation of the heart tube, the proliferation of primitive cardiomyocytes ceases. The heart tube experiences growth with the highly proliferative activity of SHF cells facilitated by WNT signaling.80 Subsequent growth of the embryonic heart primarily occurs through cell division in the ventricles and atrial chambers. As mentioned above, within the ventricles, trabeculae develop from the endocardial lining through highly proliferative activity mediated by Notch signaling. FGF signaling, IGF, and WNT signaling also participate in the proliferative expansion of EPDCs in the subepicardial myocardium. However, the proliferation rate of cardiomyocytes exhibits local variations within the developing heart, with the highest rates observed in the ballooning ventricles and decreased rates in distal parts of the OFT. The flow tract and atria are formed by highly proliferating cardiomyocytes.386 The Hippo pathway has emerged as a major regulator of the proliferation of differentiated cardiomyocytes during cardiac development,387 yet the proliferation of cardiomyocytes gradually diminishes with cardiac development.
The Hippo signaling pathway controls cardiac development through the regulation of cell proliferation, apoptosis, and cell fate determination. Activation of the mammalian Hippo signaling pathway begins with a kinase cascade involving sterile 20-like protein kinases (MST1/2) interacting with the adapter protein salvador (SALV), leading to phosphorylation of SALV, large tumor suppressor kinase (LATS)-1/2, and [monopolar spindle (Mps) one binder kinase activator-like 1] (MOB1). This results in phosphorylation, cytoplasmic retention, and degradation of the transcriptional coactivator Yes-associated protein (YAP) and the transcriptional coactivator with PDZ-binding motif (TAZ). YAP shuttles between the cytoplasm and nucleus, where it stimulates gene transcription. Inactivation of upstream kinases allows YAP and TAZ to enter the nucleus, where they interact with various transcription factors, including [transcription enhancer factor (TEA) domain family member 1-4 (Tead1-4)] and proline-proline-X-tyrosine (PPXY)-containing transcription factors [including p73, runt-related transcription factor (RUNX), erythroblastic oncogene B-B2 receptor tyrosine kinase 4 (ERBB4) cytoplasmic domain, and SMADs].388,389 In hPSCs, peroxisome proliferator-activated receptor gamma coactivator 1 (PGC1)/peroxisome proliferator-activated receptor α (PPARα) signaling promotes cardiomyocyte hypertrophy and contractility development via YAP1.390 Mutations in various genes in the Hippo pathway lead to defects in heart development, particularly causing abnormal cell proliferation states, thin ventricular walls, and abnormal heart size.388,389,391 In hESCs, loss of YAP has been reported to regulate cardiac mesoderm by influencing primitive streak differentiation in response to Activin.392 Embryonic stem cells with a double knockout of MST1/MST2 can differentiate into mesodermal cells but are significantly affected by further differentiation into cardiac cells, likely due to the inhibition of ligands of noncanonical WNT signaling.393 In zebrafish, sphingosine-1-phosphate (S1P) signaling also regulates bilateral cardiac precursor cell migration toward the midline through YAP1-dependent endoderm survival, with disrupted migration of cardiac precursors resulting in cardiac bifida, highlighting the important role of the Hippo signaling pathway during early cardiac development.394,395 The Hippo pathway also determines the number of cardiac precursors from the SHF that form the venous pole of the heart tube, which further determines the size of the atria.396 During this process, increased epithelial tension during heart tube extension may promote YAP-mediated cell division and proliferation, thus facilitating heart tube extension.397 Because the most prominent phenotype of Hippo pathway dysfunction in Drosophila is changes in organ size,398 controlling heart size via the Hippo pathway has long been of interest to researchers. The application of Nkx2.5-Cre to Salv knockout mice resulted in excessive embryonic heart growth. Although the cardiomyocyte size was unaffected, there was increased cardiomyocyte proliferation, and the embryos died postmutation. Mst1/2 and Lats2 knockout embryos also exhibit similar phenotypes.399
Interestingly, researchers have also found that Hippo signaling negatively regulates WNT signaling and that β-catenin heterozygosity suppresses the Hippo cardiomyocyte overgrowth phenotype, indicating that an interaction between Hippo and WNT signaling limits CM proliferation and controls heart size.399 Furthermore, embryonic inactivation of Yap1 leads to lethal myocardial hypoplasia and reduced cardiomyocyte proliferation, whereas activation of Yap1 stimulates the proliferation of cardiomyocytes, particularly trabecular cardiomyocytes, accompanied by significant downregulation of the expression of the myocardial marker Nppa. The mechanism by which Yap1 activation stimulates proliferation may involve the activation of IGF signaling in cardiomyocytes, leading to increased β-catenin abundance and the activation of the WNT pathway.400,401 Subsequent studies also revealed that defects in Taz lead to a decrease in the number of trabeculae in the heart, along with a disorganized cortical actin structure and abnormal cell-cell junctions.402
Recent studies have also suggested that Hippo plays a role in the development of the endocardium and epicardium. Conditional deletion of Yap in endothelial cells disrupts TGF-β-SMAD signaling, inhibiting EndMT and reducing endocardial cell proliferation, resulting in defective endocardial cushion development and embryonic lethality.403 Another study revealed that defects in endocardial YAP/TAZ suppress NRG1, leading to impaired myocardial growth and decreased ventricular wall thickness.404 The increase in myocardial chamber volume during development also promotes the nuclear localization of YAP1 and thereby promotes endocardial proliferation.405 Inhibition of YAP/TAZ also leads to impaired EMT in the epicardium, reduced proliferation of epicardial cells, and decreased differentiation into coronary endothelial cells, with embryos dying around E11.5-E12.5 due to cardiovascular insufficiency.406 Subsequent studies of epicardial-specific knockout of Lats1/2 also revealed embryonic lethality at E15.5, accompanied by defects in coronary vessel remodeling, likely due to mutant cells persistently expressing epicardial markers and failing to activate fibroblast differentiation.407
Epigenetic regulation
The genetic and epigenetic basis of most CHDs remains largely unknown. Interestingly, previous studies have found mutations in coding sequences in only a few CHD patients, while a high proportion of mutations have been identified in epigenetic regulatory factors, highlighting the importance of epigenetic regulation in cardiac development.408,409 Major epigenetic modifications include DNA modifications, histone modifications, chromatin structure changes, and regulation by noncoding RNAs (ncRNAs). These key molecules and processes of epigenetic modification have been extensively reviewed in other studies.410,411 Here, we primarily summarize their roles in cardiac development (Table 4).
In developing heart DNA, there is a significant enrichment of differentially methylated genes related to muscle contraction and cardiomyopathies. Additionally, high methylation of the GATA4 gene has been detected in fetuses with Down syndrome with or without congenital heart defects and in fetuses with isolated cardiac malformations.412 In myocardial biopsies of patients with ToF and VSD, a highly methylated novel developmental Cytosine-phosphate-Guanine (CpG) island was found in the synthesis of the cytochrome c oxidase (SCO)-2 promoter, which may contain binding sites for transcription factors involved in early cardiac development.413 These results suggest that the DNA methylation status of cardiac genes may be associated with congenital heart disease (CHD). Another study using DNA methylome analysis of purified E14.5 and neonatal cardiomyocytes revealed a wave of demethylation through the gene bodies of embryonic cardiomyocyte genes, followed by de novo DNA methylation, which shapes the epigenome of maturing cardiomyocytes after birth.414 Subsequent studies revealed that myocardial cell development is characterized by active CpG methylation and histone marks interacting in cis-regulatory and genic regions, thereby forming the myocardial cell transcriptome.415 Condorelli and colleagues mapped the hydroxymethylome of the embryonic heart and found that DNA methylation at 5-cytosine (5-mC) occurs at highly expressed genes as well as at distal regulatory regions with enhanced activity, correlating with gene transcription.416 These findings preliminarily suggest a role for DNA methylation in cardiac development, but the specific regulatory mechanisms involved require further study.
The role of BRG1/BRM-associated factor (BAF), a chromatin remodeling factor, in cardiac development has been extensively studied. In embryonic stem cells, BRG1 is crucial for regulating active and repressive chromatin states, especially by activating developmental enhancers during mesoderm lineage commitment, and its absence leads to failed mesodermal induction and cardiomyocyte differentiation.417 BRG1 also regulates CM proliferation by acting on BMP10 and cooperatively regulates fetal heart differentiation via histone deacetylase (HDAC) and [poly (ADP ribose) polymerase] (PARP).418 Other studies also indicate that BRG1 plays a role in the valve, trabeculation, and epicardial development, largely through the regulation of ECM signaling.419,420,421 The BAF complex subunit BAF60C interacts with TBX5, NKX2-5, and GATA4 and with myocardin (MYOCD), promoting the expression of contraction genes. Defects in Baf60c lead to cardiac morphological defects with significant cardiac dysfunction, impairing the proliferation and differentiation of SHF progenitors and CMs.422,423 A recent study using immunopurification with mass spectrometry revealed that BAF60C and BAF170, together with BRG1, coregulate gene expression in cardiac precursors, and their loss compromises the expression of myocardial genes in cardiomyocytes.424 The polybromo-associated BAF complex (PBAF)-specific subunit BAF180 regulates the promoters of RA target genes, and its loss leads to severe ventricular developmental defects.425
Histone modifications also play a regulatory role in cardiac development. Ubiquitously transcribed tetratricopeptide repeat X chromosome (UTX), a histone H3 lysine 27 (H3K27) demethylase, can be recruited to cardiac-specific enhancers and promote the recruitment of BRG1. Its deficiency can lead to defects in embryonic stem cell differentiation into cardiac cells and in mouse heart development.426 Through a genome-wide chromatin-immunoprecipitation DNA-sequencing approach, it was found that in cardiomyocytes, H3 methyltransferase disruptor of telomeric silencing 1-like (DOT1L) mediates enrichment of H3 lysine 79 (H3K79), which is enriched in genes expressed during cardiac differentiation and regulates their expression.427 Polycomb complexes (PRC1 and PRC2) are essential regulators of epigenetic gene silencing. PRC1 ubiquitinates histone H2A lysine 119 (H2AK119) through the Ring1 protein, while PRC2 methylates H3K27 through enhancer of zeste homolog (EZH)-1 and EZH-2. The PRC2 subunit EZH2 has been found to interact with GATA4 and directly methylate it at Lys 299, thereby attenuating its transcriptional activity.428 Polycomb complexes can regulate the differentiation of embryonic stem cells into mesodermal and cardiac cells.429 In zebrafish, mutations in the PRC1 subunit Rnf2 lead to tubular heart morphology accompanied by the upregulation and ectopic expression of Tbx2/3, resulting in the downregulation of ventricular-specific genes such as Myh6 and Nppa.430 Inactivation of another PRC1 subunit, Rae28, leads to defects in heart tube looping and ventricular development during embryonic heart development, accompanied by impaired Nkx2-5 expression.431 Loss of Ezh1 and Ezh2 also results in severe cardiac developmental defects, including EndMT impairment, reduced myocardial proliferation, incomplete endocardial cushion development, VSD, and incomplete trabeculation of the ventricular cavity.432,433,434
Additionally, the loss of histone deacetylases (HDACs), particularly HDAC1, HDAC2, HDAC5, and HDAC9, also leads to defects in cardiac development. Loss of HDAC1 results in embryonic lethality at E9.5, while mice lacking HDAC2 can survive until birth but exhibit a range of cardiac defects, including right ventricular chamber obstruction, excessive proliferation and apoptosis of myocardial cells, and bradycardia.435 Compound mutations in Hdac5 and Hdac9 result in lethal VSD and thin-walled myocardium.436 The nucleosome remodeling and histone deacetylation (NuRD) complex couples ATP-dependent chromatin remodeling with histone deacetylation. ATP-dependent chromatin remodeling activity is mediated by chromodomain-helicase-DNA-binding protein 3 (CHD3) and CHD4, and mutations in Chd4 can lead to left ventricular dilation, thinning of compact myocardium, and reduced myocardial trabeculation.437 During heart development, NuRD also interacts with TFs, such as a friend of GATA (FOG)-2,438 TBX5,439 and TBX20.440 Disruption of the interaction with FOG2 leads to defects in septum development, thinning of the ventricular myocardium, and reduced myocardial cell proliferation.438
Various histone methyltransferases also play roles in cardiac development, including Su(var)3-9, Enhancer-of-zeste, Trithorax (SET) and Myeloid-Nervy-DEAF-1 (MYND) domain containing 1 (Smyd1),441 Wolf-Hirschhorn syndrome candidate 1 (WHSC1),442 and lysine (K)-specific methyltransferase 2D (KMT2D).443 Their loss also leads to defects in cardiac development. In summary, the deficiency of various histone modification-related molecules has been associated with cardiac developmental defects, primarily through their impact on the expression of cardiac developmental genes. However, the detailed mechanisms of these effects require further investigation in future studies.
Noncoding RNAs, including long noncoding RNAs (lncRNAs, >200 nucleotides), microRNAs (miRNAs, up to 22 nucleotides), and circular RNAs (circRNAs, formed by 1-5 exons), are extensively studied ncRNAs. They serve as epigenetic regulators or modulate gene expression at the transcriptional or posttranscriptional level, thereby participating in the regulation of cardiac development. miRNAs regulate gene expression posttranscriptionally by silencing protein-coding and noncoding genes.444 LncRNAs regulate gene expression through various mechanisms, including DNA looping, the recruitment of chromatin modifiers and transcription factors, the ability to act as miRNA sponges, and the ability to influence mRNA splicing, translation, or degradation.445 CircRNAs can act as miRNA sponges to counteract miRNA-mediated repression and participate in the regulation of RNA-binding proteins.446,447 However, research on the role of circRNAs in cardiac development is still limited. Previous studies have reported the expression of various circRNAs during human embryonic heart development and differentiation into CMs from hESCs, but their specific functions require further investigation.448,449
During the early stages of cardiac development, ncRNAs participate in the regulation of the expression of the TFs Brachyury and eomesodermin (EOMES) in the mesoderm. For example, linc1405 mediates the activation of Mesp1 in the specification of cardiac mesoderm.450 Several ncRNAs are coexpressed with cardiac precursor cells, and TFs, such as EOMES, ISL1, TBX5, and TBX2, but their specific roles require further investigation.451,452 Another lncRNA, Braveheart (Bvht), acts upstream of Mesp1 during mouse embryonic stem cell differentiation and interacts with the PRC2 component suppressor of zeste 12 homolog (SUZ12) to promote mesoderm-to-cardiac fate development.453 Similarly, the lncRNA cardiac mesoderm enhancer-associated noncoding RNA (CARMEN) interacts with the PRC2 components SUZ12 and EZH2 as upstream regulators of the cardiac mesoderm-specific gene regulatory network, promoting the specification and differentiation of cardiac precursor cells.454 LncRNA plasma long noncoding RNA 4 (Platr4) interacts with the Hippo signaling pathway molecules Yap and Tead4 to regulate cardiac mesodermal lineage differentiation.455 Belmonte and colleagues identified three new lncRNAs, namely, transcriptional endoplasmic reticulum retention regulating long noncoding RNA (TERMINATOR), abnormal limb identity enhancer noncoding RNA (ALIEN), and PUNISHER, in hPSCs. TERMINATOR specifically controls pluripotent stem cell properties, ALIEN impairs cardiovascular development, and PUNISHER compromises endothelial cell function.456 The lncRNA novel long noncoding RNA 6 (Novlnc6) has been found to regulate the expression of Nkx2.5 and Bmp10 during development.457 The lncRNA [myocardial skeletal and heart enhancer (SHE) enhancer] (Moshe), an upstream regulator of Gata6, participates in cardiac development. Its downregulation increases Nkx2-5 and SHF lineage gene expression, indicating its role in the complex network of cardiac development.458 During hESC cardiac differentiation, miR-335-3p/5p activates the expression of WNT and TGFβ signaling pathways, upregulating Gata4, Nkx2-5, and troponin T (Tnnt2).459 MiR-1 and miR-133 play opposing roles in pluripotent embryonic stem cell differentiation: miR-1 promotes cardiac progenitor cell exit from the cell cycle and differentiation into cardiomyocytes by targeting the Notch ligand Dll-1, whereas miR-133 inhibits differentiation toward a cardiac fate.460 MiR-1 also promotes the differentiation of hESCs into CMs by suppressing the WNT and FGF signaling pathways.461
During heart tube looping, miR-322/-503, an X-chromosome miRNA cluster, is enriched in Mesp1+ cells and may drive cardiac muscle differentiation by targeting the RNA-binding protein CUG-binding protein Elav-like family member 1 (Celf1).462 In subsequent differentiation of the heart tube, BMP drives the miRNA-17-92 complex to inhibit the expression of Isl1 and Tbx1 during cardiac development, promoting SHF myocardial differentiation.463 Mice deficient in miRNA-17‒92 die shortly after birth due to pulmonary hypoplasia and VSD.464 MiR-1 affects cardiac morphogenesis, myocardial sarcomere and conduction system development, and cell cycle control.465,466,467 Double mutations in miR-133a-1 and miR-133a-2 result in lethal VSD, ectopic expression of cardiac smooth muscle genes, and abnormal myocardial cell proliferation in embryonic mice.468 MYOCD positively regulates the miR-1/133a cluster. Knock-out of miR-1-1/133a-2 and miR-1-2/133a-1 releases the transcriptional coactivator MYOCD, keeping embryonic cardiomyocytes in an immature state.469 Subsequent studies revealed that miR-133a and RA regulate the expression of RhoA and cell division cycle (CDC)-42 through a negative feedback mechanism, thereby controlling myocardial cell proliferation and the early development of the posterior cardiac tube segment.470 MiR-499 exhibits specific expression during cardiac differentiation. In silico analysis revealed that the predicted targets of miR-499 overlap significantly with cardiac-specific miRNAs. The overexpression of miRNA-499 and miRNA-1 promotes the upregulation of MEF2C during differentiation, suggesting potential roles for these miRNAs in cardiac development.471 In vitro studies have shown that overexpression of miR-1 and miR-499 promotes the differentiation of cardiac progenitor cells into CMs.472 Several other miRNAs, including miR-143, miR-138, and miR-21, have been found to be associated with ventricular morphogenesis and valve development.473,474,475,476 In zebrafish, knockdown of miR-218 leads to impaired cardiac cell migration and heart tube formation.477 Subsequent studies revealed that miR-218 promotes the migration of mESCs during differentiation into CMs and inhibits CM differentiation.478 MiR-27b shows significant cardiac muscle expression during heart development, with the transcription factor gene Mef2c being a target of miR-27b.479 MiR-302-367 is crucial for the proliferation of developing cardiac muscle cells; knockout of miR-302-367 results in thinning of the ventricular wall, abnormal ventricular septum development, and reduced myocardial cell proliferation, while overexpression increases myocardial cell proliferation but also restricts cardiac ejection function.480 Defects in the miRNA-processing enzyme Dicer lead to DORV with concurrent VSD.481
In recent studies using hPSCs, researchers identified 96 miRNAs that promote the proliferation of hPSC-derived cardiomyocytes. Sixty-seven of these miRNAs likely act on different components of the Hippo pathway; for instance, miR-520d-3p targets LATS2 and TEAD1, and miR-590-3p targets YAP and TEAD, suggesting that these miRNAs converge redundantly on Hippo signaling to activate YAP and robustly sustain proliferation. Therefore, further studies are needed to confirm the roles of these miRNAs.482 Other studies have shown that miR-302d and miR-10b also promote the proliferation of hPSC-derived cardiomyocytes, but their significance in cardiac development requires further investigation.483,484
Several lncRNAs also play roles during cardiac development by regulating various cardiac development-specific molecules. The lncRNA upper-hand (Uph) plays a crucial role in regulating Hand2 expression, thereby regulating cardiac muscle cell proliferation and coordinating the balanced development of cardiac cell lineages.485,486 The lncRNA ultraconserved element (uc).457 is differentially expressed in the hearts of patients with VSD and regulates the proliferation and differentiation of myocardial cells by suppressing the expression of the histone cell cycle regulation defective homologs A (HIRA), NPPA, TNNT2, and MEF2C.487 Interestingly, during the differentiation of P19 cells into CMs, the overexpression of long noncoding RNA transcript upregulated in cancer 40 (TUC40), uc.245, uc.167, and uc.40 in lncRNAs in tumors upregulated cancer cells inhibited the proliferation and differentiation of CMs, promoting cell apoptosis.488,489,490,491 A recently identified lncRNA named CARdiomyocyte Maturation-Associated lncRNA (CARMA) increases the expression of miR-1-1 and miR-133-a2, inhibits Notch signaling by regulating the expression of the key effector RBPJ and thus regulates the differentiation and maturation of cardiomyocytes.492 Another lncRNA, [B-Raf proto-oncogene, serine/threonine kinase (BRAF)-activated noncoding RNA] (BANCR), is exclusively present in fetal chimpanzee cardiomyocytes and regulates CM migration through TEAD/YAP signaling. Deletion of BANCR in mouse models results in increased heart size, indicating its potential impact on cardiac development, which requires further investigation.493
Embryonic microenvironment
With a deeper understanding of heart development, researchers have recognized the critical role of the embryonic microenvironment in this process. This unique milieu provides the foundation for normal cardiac development and intercellular signaling. Here, we focus on the effects of changes in the ECM, hypoxia, and metabolic environment on heart development from a broader perspective.
Although initially viewed as a relatively inert scaffold providing structural support to cells in their environment, the ECM is now widely recognized for its dynamic and plastic role in facilitating cell signaling, proliferation, and differentiation within the body, particularly during embryogenesis.494,495 Spatially, the ECM is primarily divided into the basement membrane/pericellular matrix and the interstitial matrix. The former is composed of fibronectin, collagen IV, laminin, procollagens, hyaluronic acid (HA), and proteoglycans, which promote signal transduction through cell surface receptors. The latter consists mainly of collagens I and III, providing tissue with structural and mechanical support.496 Throughout various stages of heart development, the role of ECM macromolecules is evident. During early development, the primitive heart ECM comprises chondroitin sulfate, collagens I and IV, laminin, fibulin, fibrillin, and fibronectin, which contribute to the migration of cardiac precursors toward the embryo midline.18,495,497 Fibronectin deposition at the midline is essential for heart development;498 its inactivation results in severe defects in mesodermally derived tissues, including cardiac development and early embryo death.499,500 After the primitive heart tube is formed, the cardiac jelly separates the endocardium and myocardium and contains various ECM molecules. The subsequent accumulation of ECM at the AV junction is crucial for the local swelling of cardiac jelly, which is essential for AV cushion formation. In zebrafish, knocking down the ECM protein Nephronectin limits AVC differentiation and cardiac jelly expansion by suppressing BMP4-hyaluronan-synthase 2 (HAS2) signaling, thereby preventing leaflet formation and trabeculation.501 The cardiac cushion ECM is rich in HA, and its disruption by hyaluronidase treatment leads to abnormal formation of endocardial cushions, thinning of the ventricular myocardial wall, and changes in ventricular function.502 Defects in uridine 5’-diphosphate (UDP)-glucose dehydrogenase, which is required for HA production, similarly lead to malformed AV cushions and valve formation issues.503 Embryos with defects in Hyaluronan-synthase 2 display similar outcomes, including myocardial thinning and impaired atrioventricular cushion development, while endocardial ERBB2-ERBB3 receptors may mediate the role of HA in valve and septum development.504,505 Other signals, such as BMP2 and TGF-β3, regulate heart AV cushion and valve development through the versican/HA and periostin/collagen pathways, respectively.506,507 Studies using gene knockout mouse models also highlight the essential role of periostin in septal and valve development.508,509
Furthermore, precise temporal and spatial control of ECM synthesis and degradation is crucial for the formation of trabeculations in the heart. Mutations in Has2 and Versican can lead to defects in trabeculation.505,510 The expression of matrix metalloproteinase A disintegrin and metalloproteinase with thrombospondin motifs (ADAMTS)-1 prevents excessive trabeculation.419 Notch regulates ECM synthesis and degradation through ECM proteases and NRG1, promoting ECM remodeling during trabeculation development and thus facilitating normal trabeculation.88 The matrix metalloproteinase ADAMTS9 has also been found to participate in myocardial compaction. ADAMTS9 is expressed during development in the SHF, vascular smooth muscle cells in the arterial wall, mesenchymal cells of the valves, and non-myocardial cells of the ventricular myocardium. Loss of Adamts9 results in abnormal valve development and abnormal myocardial projections, as well as a ‘spongy’ myocardium consistent with noncompaction of the left ventricle.511 During embryonic development, cardiac fibroblasts secrete ECM components, including fibronectin, collagen, and hyaluronic acid, promoting myocardial cell proliferation.512 In recent research, mouse embryonic stem cell-derived embryoid bodies were shown to generate heart organoids through the action of laminin-entactin (LN/ET) complexes and FGF4, which contains cardiac muscle, conducting tissues, smooth muscle, and endothelial cells capable of myocardial contraction and action potentials,513 emphasizing the importance of the ECM in heart development.
Fetal development occurs under conditions of relative hypoxia compared to adult oxygen tension. A low-oxygen environment during cardiac development is crucial for normal heart formation and maturation. A previous study indicated an increase in hypoxia staining and the accumulation of hypoxia-inducible factor 1 (HIF-1) during the peak of cardiomyocyte apoptosis in the OFT, a process essential for OFT remodeling. This finding suggested that hypoxia plays a significant role in embryonic OFT remodeling.514,515 Hypoxia also contributes to coronary vessel formation through VEGF during heart development.234,516 HIF-1, which is composed of α and β subunits, plays a significant role in hypoxia-dependent signaling, providing new insights into the role of hypoxia in heart development. In mice, hypoxic regions in the fetal heart are observed throughout embryonic development, with HIF stabilization correlating with these areas.517 The absence of HIF-1α leads to cardia bifida, abnormal cardiac looping, and cephalic blood vessels caused by reduced expression of MEF2C and HAND1 and defective CNCCs migration.518 Deletion of HIF-1β also results in embryonic lethality with placental and heart defects.519 Moreover, tissue-specific conditional knockout technology has been utilized to explore the role of HIF genes in heart development. Conditional knockout of HIF-1α in the embryonic mesoderm results in heart abnormalities, including the overriding aorta, ectopia cordis, and incomplete septation.520,521
While low oxygen conditions during fetal development are essential for embryonic heart growth, pathophysiological hypoxia can adversely affect cardiogenesis. Insufficient oxygen in utero leads to myocardial thinning, ventricle dilation, epicardium detachment, and a decrease in fetal heart maturation in both chicken and mouse models.522,523 Another study utilizing proteomics and metabolomics demonstrated that antenatal hypoxia alters pathways related to energy metabolism, lipid metabolism, oxidative stress, and inflammation and leads to mitochondrial reprogramming.524 The prevalence of CHD has been reported to be ten times greater in individuals living at high altitudes and exposed to chronic hypoxia than in those living at sea level.525 However, the intricate mechanism through which hypoxia regulates heart development requires further exploration.
During heart development, the embryonic heart undergoes significant changes in its metabolic environment. Due to the low levels of circulating free fatty acids in the fetal bloodstream, glucose and lactate serve as the main sources of ATP during early heart development and play crucial roles in cell proliferation. A decrease in glycolysis and a concurrent increase in fatty acid β-oxidation occur during myocardial maturation.526 However, due to the hypoxic environment, the embryonic heart continues to rely primarily on glycolysis rather than oxidative phosphorylation (OXPHOS) for ATP generation (Fig. 4).527 Furthermore, cardiomyocytes continue to depend on glycolysis and lactate oxidation for ATP production after birth, with a significant increase in fatty acid β-oxidation efficiency in subsequent days.528 A recent proteomic study in mouse embryos highlighted the significant upregulation of metabolic pathway-related proteins, including proteins involved in glycolysis, fatty acid oxidation, and OXPHOS, during late embryonic heart development (E13.5-E16.5). The mevalonate pathway also plays a critical role in regulating CM proliferation during heart development.529 The precise regulation of these metabolic transitions and their roles in fetal growth are increasingly being studied.
The role of hypoxia and metabolic transition during cardiac development. Significant changes in metabolic pathways accompany the maturation of cardiac development. During embryonic cardiac development, glucose and lactate serve as the primary sources of ATP. Hypoxic conditions activate HIF-1α during embryonic development, coupled with mitochondrial immaturity, which promotes a reliance on glycolysis for ATP production in the fetal heart, leading to increased lactate production. As cardiac development progresses, there is a simultaneous decrease in glycolysis and an increase in fatty acid β-oxidation during myocardial maturation. After birth, cardiac metabolism primarily relies on fatty acid oxidation, facilitated by an oxygen-rich environment. In this environment, the HIF-1α subunit is hydroxylated and targeted for degradation by VHL, thereby inhibiting its promotion of glycolysis. α-KG α-ketoglutarate, ATP adenosine triphosphate, CoA coenzyme A, HIF-1α hypoxia-inducible factor 1-alpha, OH hydroxide, O2 oxygen, TCA tricarboxylic acid, VHL von Hippel Lindau. This figure was created using Adobe Illustrator
The Warburg effect refers to a metabolic state in which cells exhibit high glucose uptake and ferment glucose into lactate despite the presence of adequate oxygen and functional mitochondria. However, fetal cellular metabolism does not conform to the Warburg effect because lactate is actively consumed, and the intrauterine environment is relatively hypoxic. Transient exposure to lactate has been shown to induce significant and enduring transcriptional alterations in hPSC-derived cardiomyocytes, including the inhibition of WNT signaling, reduced proliferation, and elevated gene expression related to cardiac contractility and calcium signaling, suggesting that lactate may act not only as a metabolic waste product but also as a regulator of molecular signals during development.530 However, another study demonstrated that deleting Hif1α inhibited glycolytic activity but did not affect heart differentiation,531 possibly because metabolic products from other pathways during development compensate for the effects of glycolytic inhibition and because the impact of lactate on heart development may be dose-dependent. In 2019, Zhao et al. reported that lactate can lactylate histone lysine residues, a modification implicated in various physiological and pathological processes.532 Interestingly, lactylation has been linked to signaling pathways crucial for heart development, such as the WNT pathway,533 Hippo pathway,534 and Notch pathway,535 suggesting its potential importance in cardiac development. However, there is currently no research specifically addressing the role of lactylation in heart development, and further studies are needed to elucidate the effects of lactate in this context.
Diabetes is a risk factor for CHD. During normal embryonic development, glucose intake in the developing heart gradually decreases in late pregnancy. Disruption of glucose metabolism during diabetic pregnancies negatively affects the maturation of cardiomyocytes in the fetal heart. High glucose enhances nucleotide biosynthesis via the pentose phosphate pathway in hPSC-derived CMs.536 Mature cardiomyocytes adaptively rely on fatty acid β-oxidation (FAO) for ATP production. Recent studies in hPSC-derived cardiomyocytes suggest that fatty acids promote cardiomyocyte maturation by stimulating mitochondrial biogenesis, enhancing oxidative metabolism closer to adult ventricular tissue transcriptional characteristics, increasing muscle fiber density and arrangement, improving calcium handling, enhancing contractility, and enhancing physiological action potential dynamics.537,538,539,540,541 Activation of PPAR signaling pathways associated with fatty acid maturation processes similarly promotes hPSC-derived cardiomyocyte maturation.530,542,543 However, the current understanding of how metabolic environments influence heart development is limited primarily to pluripotent stem cell models, and in vitro differentiation protocols for pluripotent stem cells are still immature and rely on empirical evidence. Thus, insights gained from in vitro models regarding gene-environment interactions need validation in animal models.
Advancements in understanding the molecular mechanisms of cardiac development
Autophagy is an intracellular process that generates double-membrane-bound vesicles called autophagosomes in the cytoplasm, which transport substrates to lysosomes for degradation. Recent studies have suggested that autophagy is involved in cardiac development by promoting the differentiation of myocardial cells and that the loss of autophagy can lead to defects in heart development. Autophagy plays an important role in regulating the pluripotency of embryonic stem cells.544 The activation of autophagy on days 0–4 of hPSC-derived cardiomyocyte differentiation decreased the expression of CM-specific genes, whereas the activation of autophagy on days 4–6 achieved the greatest CM differentiation efficiency by inhibiting the WNT signaling pathway, indicating that autophagy regulates CM differentiation in a stage-dependent manner. One possible explanation is that autophagy directly degrades cytoplasmic β-catenin, leading to the suppression of WNT signaling in the early stages of cardiomyocyte differentiation, while WNT activation is essential for the early phase of differentiation.545 Knockdown of genes required for the autophagic process led to a small, string-like heart with pericardial edema in zebrafish, with defects during the heart jogging process followed by imperfect cardiac looping.546 Moreover, the knockdown of core autophagy genes, including Atg5, Atg7, and Becn1, also causes defects in morphogenesis and abnormal heart structure in zebrafish.547
The development of single-cell RNA sequencing and single-nucleus RNA sequencing has uncovered the complex cell-to-cell communication and interactions between cardiomyocytes and numerous non-cardiomyocytes, which are crucial for normal heart development. Non-cardiomyocytes account for approximately 40%-70% of the total cells in the human heart, with the exact proportion varying across different studies, possibly due to differences in detection methods and sample types.548 Single-cell analysis of mouse hearts from embryonic days E9.5 to E18.5 identified eight different cell types, including cardiomyocytes, myoblasts, endothelial cells, vascular smooth muscle cells and pericytes, fibroblasts and myofibroblasts, T cells, macrophages, monocytes, and dendritic cells. 549 Another study analyzing the developing human heart [between 9 and 16 post-conception weeks (PCW)] identified cell types such as various subpopulations of cardiomyocytes, mesenchymal cells (epicardial cells, fibroblast-like vascular smooth muscle cells, and pericytes), endothelial cells (blood endothelial cells, lymphatic endothelial cells, and endocardial cells), blood cells (macrophages, white blood cells, and platelet-red blood cells), and neuronal cells (Schwann cells and neural crest cells).550 Further analysis revealed that Semaphorin (SEMA)-3C, secreted by ventricular fibroblasts, may attract Plexin A (PLXNA2/4)+ trabecular ventricular cardiomyocytes to migrate into the compact layer. Additionally, SEMA6A and SEMA6B in endothelial cells may compete with SEMA3C to prevent the further migration of trabecular ventricular cardiomyocytes within the compact layer. This theory is supported by the observation that specific deletion of the Sema3c gene in mouse cardiac fibroblasts leads to non-compacted, hypertrabeculated cardiac ventricles.550 In another study, Hou et al. used single-cell sequencing to identify 11 cell types in the developing human heart (at 8, 10, 11, and 17 PCW). CellChat analysis of intercellular communication revealed that at 8 PCW, the interaction strength between cell types was relatively low, but it significantly increased from 10 to 17 PCW. Furthermore, the interaction strength of the oncostatin M (OSM) signaling pathway gradually decreased during this period (from 8 to 17 PCW), while signaling pathways such as macrophage migration inhibitory factor (MIF), Pleiotrophin (PTN), and Granulin (GRN) became more complex, with increased cell-to-cell communication at 10, 11, and 17 PCW.551 Our previous research also explored cell communication between epicardial cells and other cardiac cells during mouse heart development. We found that epicardial cells interact with various cell types via ligand-receptor interactions. For example, they interact with immune cells through tumor necrosis factor (TNF)-Fms-related tyrosine kinase 4 (FLT4) and cluster of differentiation (CD)-44-FGFR2, with cardiomyocytes through CD74-MIF, and with fibroblast-like cells through CD46-JAG1.552 Although new technologies have provided vast amounts of information on the communication and interactions between different cell types during cardiac development, further validation is still required to clarify the specific roles of these interactions within complex signal network.
In recent years, the role of cardiac macrophages has gradually gained increased attention. Although recent single-cell studies have identified macrophages in the developing heart,549,550,551 their role in cardiac development remains largely unknown. Cardiac macrophages generally originate from two distinct sources: self-sustaining and renewable macrophages established during the embryonic stage, and macrophages derived from monocytes that migrate into tissues. The former makes up the majority of immune cells in the heart and is primarily active in development and homeostasis, where it functions in clearing apoptotic cells, regulating cardiomyocyte proliferation and angiogenesis, removing damaged mitochondria, and promoting electrical conduction. The latter is primarily associated with pathological conditions.553,554 Currently, through the use of cell surface markers [e.g., chemokine receptor-2 (CCR2); lymphatic vessel endothelial hyaluronan receptor 1 (LYVE1); and T-cell immunoglobulin and mucin domain-containing 4 (TIMD4)], genetic fate mapping, transcriptomic analysis, and functional studies, various subtypes of tissue-resident cardiac macrophages have been successfully identified and classified.553 In the mouse heart, three transcriptionally distinct macrophage subpopulations have been identified: TLF+ macrophages [expressing TIMD4, LYVE1, and/or folate receptor beta 2 (FOLR2)] maintained through self-renewal, CCR2+ macrophages dependent on monocytes [CCR2+ (TIMD4−LYVE1−FOLR2−)], and partially monocyte-dependent major histocompatibility complex (MHC-II)hi macrophages (TIMD4−LYVE1−FOLR2−CCR2−).555 Recent studies have revealed that these macrophages play critical roles in various cardiac diseases, such as myocardial injury,556,557 atherosclerosis,558 and myocarditis,559 though these aspects are not elaborated on here. Macrophages first appear in the yolk sac between E6.5 and E8.5, and these yolk sac-derived macrophages colonize the heart and persist as TLF+ and MHC-IIhi macrophages into adulthood.560 Between E12.5 and E17.5, the heart primarily receives macrophages from the fetal liver, including TLF+, MHC-IIhi, and CCR2+ macrophages. This occurs as hematopoietic stem cells migrate from the aorta-gonad-mesonephros (AGM) to the fetal liver around E10.5, making the fetal liver the primary hematopoietic site for macrophage production. From E16.5 onwards, hematopoietic stem cells colonize the developing bone marrow, and mature monocytes migrating into tissues differentiate into macrophages to replenish multiple cardiac macrophage lineages, primarily generating CCR2+ macrophages and minimally contributing to other subsets.554,560Other classification systems for cardiac macrophages include LYVE1hiMHCIIlo and LYVE1loMHCIIhi macrophages,561 as well as yolk sac/AGM-derived macrophages [Chemokine (C-X3-C motif) receptor 1 (Cx3Cr1)+ Colony stimulating Factor 1 Receptor (Csf1r)+F4/80+), fetal liver monocytes (F4/80loCD11bhi), and monocyte-derived macrophages (CCR2+MHC-IIhi).562 Among these, LYVE1hiMHCIIlo macrophages, Cx3Cr1+Csf1r+F4/80+ macrophages, and F4/80loCD11bhi macrophages are similar to the TLF+ macrophages described earlier. The emergence of different classification methods reflects the complex spatiotemporal heterogeneity of cardiac macrophages, where different macrophage phenotypes may be expressed at various stages of heart development, or even macrophages with identical phenotypes may originate from different sources. Further research is needed to elucidate the ontogeny and functions of cardiac macrophages.
Currently, embryonic cardiac macrophages can be first observed near the OFT around E10, increasing up to E14.5, predominantly on the surface of the heart in the subepicardial space. These cells play crucial roles in vascular and lymphatic vessel formation, as well as valve development (Fig. 5).560,562,563,564 Yolk sac-derived CCR2− macrophages are essential for the remodeling of the primitive coronary plexus, and IGF signaling potentially mediates the proangiogenic properties of embryonic-derived macrophages.564 Two other studies also revealed substantial numbers of embryonic tissue macrophages (phenotypes CD68+, F4/80+, CD206+, Lyve-1+, and Cx3cr1+) adhering to vascular and lymphatic walls around E12.5, with macrophages interacting directly with lymphatic endothelial cells via hyaluronic acid. Subsequently, between E14 and E17, cardiac macrophages can be classified into three subgroups expressing genes associated with vascular and lymphatic vessel formation and ECM remodeling.565,566 Shigeta and colleagues further discovered macrophages originating from endocardial cushion-associated hemogenic endothelial precursors in the embryonic heart, suggesting that these cells play an important role in valve development through phagocytic activity.563 In vitro studies have shown that hPSC-derived primitive yolk sac-like macrophages (CCR2−, LYVE1+, CD45−, CD14+, CD64+, and CD68+) cocultured with a tri-culture of endothelial cells, dental pulp stem cells, and CMs also localize around blood vessels and promote higher vessel density, junction number, and length, while reducing mean lacunarity. In the Biowire heart-on-chip platform, macrophage coculture resulted in denser and more intact ECM, highly dense and striated CMs, higher contractile force, and a greater excitation threshold. These effects may be attributed to the increased secretion of pro-angiogenic cytokines, cardioprotective upregulated cytokines, adiponectin, and the upregulation of genes involved in cardiac maturation and angiogenesis in tissues with macrophages.567 Another in vitro study using immuno-engineered human cardiac microtissues and hPSC-derived primitive yolk sac-like macrophages found that macrophages promote cardiomyocyte sarcomeric protein maturation and increase contractile force and relaxation kinetics.568 These findings suggest the potential roles of cardiac macrophages in heart development. However, since these results are based solely on in vitro studies, differences with the in vivo developmental environment remain, and further research is needed to confirm these observations.
The role of macrophages during cardiac development. Macrophages first appear during mouse embryo development around E10 near the outflow tract, sinus node, and endocardial cushions. As the heart matures, they are distributed beneath the epicardium, within the myocardial layer, and in the endocardial layer throughout the entire heart. Various macrophage subpopulations have been identified at different times and locations, with significant research focused on subepicardial space subpopulations (CX3CR1+ CD68+ F4/80+ Lyve-1+/-; CX3CR1high CD64+ Lyve-1+ CCR2-). These macrophages originate from the yolk sac and migrate to the epicardium under the influence of the transcription factor WT1, subsequently entering the subepicardial space. In the subepicardial space, these macrophages adhere to the endothelial cells of blood vessels, promoting the normal development of coronary arteries. Simultaneously, they adhere to the endothelial cells of lymphatic vessels and facilitate normal lymphatic development through direct interactions involving hyaluronic acid. Macrophages within endocardial cushions (Nfatc1+ CD45+ CD68+ F4/80+ CD206+), derived from endothelial cells, likely contribute to valve development through phagocytic activities. CCR2 C-C chemokine receptor type 2, CX3CR1 chemokine (C-X3-C motif) receptor 1, Lyve-1 lymphatic vessel endothelial hyaluronan receptor 1, Nfatc nuclear factor of activated T cells, cytoplasmic, WT1 Wilms tumor 1. This figure was created using Adobe Illustrator
While these molecular mechanisms regulating heart development have recently garnered researchers’ attention, in-depth studies still need to be completed. It remains to be investigated whether these mechanisms play other significant roles in heart development or whether these novel mechanisms impact classical mechanisms, such as whether autophagy influences heart development via WNT signaling or whether macrophages affect Notch signaling during valve development. Future research is needed to address these questions.
Diseases related to defects in cardiac development
Tracing the precise etiology of CHD remains challenging. Initially, researchers proposed that the occurrence of CHD results from abnormal embryonic development of primitive cardiac segments, manifested anatomically through regional pathology. For instance, abnormal development of the AVC leads to anomalous connections between the atria and ventricles, while anomalies in the primitive outlet manifest as congenital malformations in subarterial ventricular components.18 Currently, with ongoing research into the roles of genes and signaling pathways in cardiac development, we can explore the pathogenesis of CHD from a deeper perspective. Each cell involved in cardiac development, starting from stem cell differentiation, requires a regulatory network blueprint to determine its location and function. Individual genes form proteins through transcription and translation processes, thereby fulfilling their predetermined tasks in heart development. Disruption of this process by any factor can lead to various types of heart development defects (Fig. 6). The clinical phenotype of CHD is relatively complex; most patients exhibit only a single type of defect, such as a single ASD or VSD. However, some patients carrying deleterious variants in specific genes, such as TBX5 or TBX1 variants, exhibit multiple congenital heart defects combined with developmental disorders in other systems,569,570,571 possibly because the gene mutations causing these complex conditions are upstream in the embryonic developmental regulatory network. For example, TBX5 and TBX1 have been confirmed to be expressed early in mesodermal and SHF development and their mutations lead to severe, multifaceted developmental defects.
Common congenital heart defects and pathogenic mechanisms. Ventricular septal defect is a defect in the ventricular septum involving the loss of functions of various TFs, GFs, Notch signaling, RA signaling, etc.; atrial septal defect is a defect in the atrial septum, involving the loss of functions of various TFs, GFs, WNT signaling, RA signaling, etc; bicuspid aortic valve is a pathological condition where the aortic valve has only two leaflets instead of the normal three, involving the loss of functions of TGF-β signaling, Notch signaling, various TFs, etc.; mitral valve prolapse is a pathological condition where the mitral valve does not close properly, involving the loss of functions of TGF-β signaling, ECM signaling, FBN1, etc.; patent ductus arteriosus is a pathological condition in which the ductus arteriosus fails to close after birth, allowing a portion of oxygenated blood from the left heart to flow back to the lungs through the aorta, involving the loss of functions of TFAP2B, prostaglandin signaling, Notch signaling, etc.; tetralogy of Fallot includes ventricular septal defects, overriding of the aorta, right ventricular outflow obstruction and right ventricular hypertrophy, involving the loss of functions of various TFs, Notch signaling, VEGF signaling, etc.; double-outlet right ventricle is the defect that both the pulmonary artery and the aorta arise from the right ventricle instead of their normal positions, involving the loss of functions of various TFs, RA signaling, Notch signaling, etc.; transposition of the great arteries is a pathological condition where the pulmonary artery and aorta are switched in position, causing oxygen-rich blood from the lungs is pumped back to the lungs instead of being circulated to the rest of the body, and oxygen-poor blood from the body is pumped back to the body instead of being sent to the lungs to pick up oxygen, involving the loss of functions of cilia, various TFs, Nodal signaling, etc.; persistent truncus arteriosus is a pathological condition characterized by single large vessel arising from the heart that supplies blood to both the systemic and pulmonary circulations, involving the loss of functions of various TFs, RA signaling, Nodal signaling, etc.; hypoplastic left heart syndrome presents with different degrees of stenosis or atresia of the aortic and mitral valve along with hypoplasia of the left ventricle and ascending aorta involving the loss of functions of various TFs, Notch signaling, ECM signaling, etc. ECM extracellular matrix, FBN1 fibrillin 1, FLNA filamin A, FOG2 friend of GATA 2, GATA GATA binding protein, GFs Growth factors, HAND1 heart and neural crest derivatives expressed 1, HOXA1 homeobox A1, ISL1 islet 1, NKX2-5 NK2 homeobox 5, PITX2 paired-like homeodomain transcription factor 2, RA retinoic acid, TBX T-box transcription factor, TFs transcription factors, TFAP2B transcription factor AP-2 beta, TGF-β transforming growth factor beta, VEGF vascular endothelial growth factor, ZIC3 Zic family member 3. This figure was created using Adobe Photoshop
In contrast, single types of congenital heart defects may occur when more downstream molecules are affected after specification in other areas, although the etiology of these defects in individuals is currently less understood. Currently, three main mechanisms disrupt normal heart development: inheritance of gene mutations from parents, acquisition of de novo somatic gene mutations during embryogenesis, and disruption by nongenetic factors such as infections, maternal exposure to alcohol or certain drugs, and metabolic disturbances.572 However, these mechanisms account for less than half of CHD patients, and further exploration is needed to elucidate the specific pathogenic mechanisms in the remaining CHD patients. Despite some understanding of the signaling pathways and multi-level regulatory mechanisms involved in heart development, our overall knowledge remains quite limited. This contributes to the fact that the etiology in over half of CHD patients is unknown, preventing personalized early prevention and treatment. The complexity of cardiac development is the major challenge. The developmental process is lengthy and involves dynamic changes in numerous molecules and signals at each developmental stage, making it difficult to study. Most studies focus on the role of single molecules or pathways in heart development, with only a small portion examining the cooperative roles of two or more molecules. Therefore, this falls short of explaining the complex developmental networks in both physiological and pathological states.
Advances in sequencing technologies now provide powerful tools for comprehensively understanding heart development and the causes of CHD. For example, metabolomics and epigenomics allow us to observe cardiac development from different perspectives. Single-cell sequencing enables us to study changes in cell phenotypes and signaling pathways at single-cell resolution. Additionally, it allows us to perform pseudo-time and cell communication analysis to observe temporal molecular changes and cell interactions, offering more information than traditional basic researches. As previously mentioned, numerous single-cell sequencing studies have enhanced our understanding of cardiac development at a higher resolution (Table 1). Matthew et al. employed single-nucleus RNA sequencing and imaging mass cytometry to observe cell states in CHD. They found that CHD patients exhibit deficient monocytic immune function and a perivascular microenvironment with spatial distribution characteristics consistent with an immunodeficient state. Additionally, cardiac fibroblasts in HLHS showed signs of activation. These findings provide a theoretical foundation for future personalized treatments for CHD.573 However, single-cell sequencing has limitations, such as loss of spatial information and the inability to directly provide functional information. In recent years, spatial transcriptomics has advanced, but its integration with single-cell sequencing is still being refined. While studies using novel sequencing technologies have yielded informative results, we are still far from fully understanding the complex regulatory networks of heart development and the causes of CHD. More research is needed to rigorously validate and explore the findings from sequencing studies. In this section, we will review common congenital heart defects and their cellular and molecular mechanisms.
Septal defects
Septal defects primarily include ASDs, VSDs, and AVSDs. A ventricular or atrial septal defect is a hole in the septum, the wall that divides the left and right ventricles or atria of the heart. Depending on the location of the defect, ventricular defects can be classified as membranous VSDs, muscular VSDs, inlet VSDs, or infundibular VSDs.574 ASD can be classified as a patent foramen ovale, an ostium primum defect, an ostium secundum defect, a sinus venosus defect, a coronary sinus defect, or a common atrium defect.575 AVSDs are characterized by a defect in the atrioventricular septum accompanied by malformation of the atrioventricular valves, with or without ventricular septal defects, caused by inadequate development of the endocardial cushion. As mentioned earlier, dysfunctions in BMP4, TGF-β, HAND2, ISL1, TBX5, RA, Notch signals, and other molecules are involved in the formation of septal defects. One of the critical mechanisms through which these molecules contribute to VSD or ASD involves their impact on the normal development of endocardial cushions and the EndMT process. Although multiple molecules and signals have been established as key regulatory factors in cardiac septation, their specific roles in causing different types of septal defects remain unclear. For instance, individuals with TBX5 mutations may develop ASD, VSD, or AVSD.576 The complexity of the regulatory network in cardiac development suggests that a single gene or molecular signal does not solely determine the phenotype of CHD. Development occurs in multiple stages over time, involving changes in cell types and numbers. Disease phenotypes are typically observed in the final stages of development, making it challenging to establish a direct link between abnormal gene mutations or molecular signals and the final disease phenotype. This complexity also implies that abnormal molecular signals may undergo further regulation or cause additional abnormalities in intermediate stages, thereby leading to different downstream disease phenotypes. Further in vitro and in vivo studies are needed to confirm these relationships and establish clearer connections between the discovered molecular abnormalities and specific congenital heart disease phenotypes.
Conotruncal defects
Conotruncal defects arise due to inadequate or misaligned development of the ventricular septum, OFT, and/or great arteries, resulting in conditions such as ToF, PTA, DORV, and TGA. PTA, which is associated with DiGeorge syndrome (chromosome 22q11.2 deletion syndrome) and TBX1 deficiency, is a rare congenital heart defect characterized by abnormal embryonic cardiac development, leading to the absence of normal separation between the aorta and pulmonary artery during fetal development. Instead of two separate arteries, there is a single large vessel arising from the heart that supplies blood to both the systemic and pulmonary circulations.577,578 DORV occurs when both the pulmonary artery and the aorta, the two main arteries that carry blood away from the heart, originate from the RV rather than from their usual positions. In Obler et al.‘s study, both chromosomal and nonchromosomal abnormalities were associated with this phenotype, with mutations in the Cryptic Family 1 (CFC1) and chicken skeletal muscle X-linked (CSX) genes identified in very few cases.579 ToF, the most common cyanotic CHD, consists of four abnormalities: a ventricular septal defect, overriding aorta, right ventricular outflow obstruction, and right ventricular hypertrophy. It typically occurs sporadically but is also observed in conjunction with other syndromes. The pathogenesis of conotruncal defects primarily involves molecular signaling dysfunction in two crucial pathways related to the development of SHF and CNCCs. Loss-of-function mutations affecting molecules and signaling, such as FGF8, FGF10, NKX2-5, ISL1, Shh, and Notch signals, are implicated in conotruncal defects. Specifically, disruptions in FGF signaling, ISL1, and Notch signaling during the migration and functional integration of CNCCs are considered major factors contributing to these diseases.580,581
Valve defects
Common congenital valve developmental abnormalities include BAV, mitral valve prolapse (MVP), mitral stenosis, tricuspid atresia, and PVS. Although these developmental malformations are collectively referred to as valve defects, the molecular mechanisms underlying their disease phenotypes may be entirely distinct. As discussed in the previous section, valve formation begins with the expansion of cardiac jelly and the differentiation of endocardium-derived mesenchymal cells, with varying cellular origins and regulatory mechanisms involved in different valve developments. For instance, the mitral and tricuspid valves derive from atrioventricular valve development, while OFT cushions form the aortic and pulmonary valves, requiring migration from the CNCCs. Therefore, disruptions in related molecular regulatory networks, such as Notch signaling and TGFβ signaling, may lead to valve defects, but a precise understanding of the pathogenesis of various valve defects is still lacking. BAV is a congenital defect characterized by the aortic valve having only two leaflets instead of the normal three leaflets. Animal models of BAV are primarily constructed using genes such as Notch1 and Gata5/6, and multiple genes, including TGFBR2, TGFBR1, NOTCH1, ACTA2, and KCNJ2, have been associated with BAV.582 MVP is a pathological condition in which the mitral valve fails to close properly due to myxomatous degeneration, primarily caused by dysregulated TGFβ signaling, leading to the differentiation of valve interstitial cells into myofibroblasts and subsequent production and deposition of extracellular matrix, resulting in structural changes in the mitral valve.583,584 Ebstein anomaly is a rare congenital heart defect characterized by abnormalities in the tricuspid valve, which is located between the right atrium and the right ventricle of the heart. In individuals with Ebstein anomaly, the tricuspid valve is positioned abnormally low in the right ventricle, resulting in decreased blood flow to the lungs and reduced oxygen levels in the body.585 The pathogenesis of Ebstein anomaly remains unclear, but previous studies have suggested that mutations in the MYH7 gene are associated with this condition.586,587
Hypoplastic left heart syndrome
HLHS presents with varying degrees of aortic and mitral valve stenosis or atresia, along with hypoplasia of the left ventricle and ascending aorta. Studies using hPSCs to investigate HLHS have indicated intrinsic myocardial cell defects as potential causes, characterized by decreased cardiac differentiation efficiency, sarcomere disarray, abnormal mitochondrial structure, and impaired Notch signaling.588,589,590 Single-cell sequencing of induced pluripotent stem cell-derived endothelial cells (iECs) revealed abnormal ECM deposition and EndoMT in endothelial cells, leading to reduced proliferation and maturation of cardiomyocytes.591 Various gene mutations, such as those in RNA binding fox-1 homolog (RBFOX)-2, myelin regulatory factor (MYRF), and HAND1, have also been implicated in the occurrence of HLHS.592 However, while these in vitro studies provide insights into disease onset, a precise explanation for HLHS pathogenesis, particularly how abnormal differentiation of myocardial and endothelial cells leads to valve developmental defects, requires further validation through in vivo studies.
Patent ductus arteriosus
PDA is a condition in which the ductus arteriosus fails to close after birth, allowing some oxygenated blood from the left heart to flow back to the lungs through the aorta. The ductus arteriosus is crucial for fetal survival in the uterus. After birth, as the partial pressure of oxygen increases and the levels of prostaglandins and other vasodilators decrease, the ductus arteriosus constricts and closes, eventually transforming into the ligamentum arteriosum.593 This process involves two main stages: initial “functional” closure through smooth muscle contraction, followed by “anatomical” closure characterized by neointimal thickening and a reduction in smooth muscle cells in the inner muscle layer.594 Thus, normal smooth muscle contraction and the accumulation of various ECM components in the subendothelial area are critical for the closure of the ductus arteriosus. Deficiencies in multiple ECM molecules can lead to the PDA phenotype.595,596,597 Clinically, the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to inhibit cyclooxygenase and induce ductus arteriosus closure highlights the critical role of prostaglandin signaling in this process.598 Gene knockout studies have shown that various molecules involved in prostaglandin signaling are essential for ductus arteriosus closure, but their absence often results in a PDA phenotype and neonatal lethality.599,600,601,602 Notably, recent research suggests that the occurrence of PDA may be due not only to postnatal dysfunction of smooth muscle cells, ECM, and endothelial cells but also to abnormal vascular smooth muscle differentiation during heart development. For example, a defect in the smooth muscle cell-related gene Myh11 can delay ductus arteriosus closure,603 and knocking out Myocd in neural crest-derived SMCs results in a PDA phenotype with a loss of SMC markers,604 underscoring the importance of normal vascular smooth muscle development for ductus arteriosus closure. Furthermore, in mice, defects in smooth muscle Notch signaling can lead to PDA. Conditional knockout of Jag1 in mouse smooth muscle cells causes defects in the PDA and OFT, with reduced expression of mature smooth muscle cell markers in the OFT; moreover, indomethacin can partially rescue the PDA in these mice.605 Subsequent studies on smooth muscle Rbpj deficiency revealed phenotypes similar to those of Jag1 deficiency, with only a few gene-deficient mice being rescued by indomethacin.606 Another study indicated that Notch2 and Notch3 play crucial roles in promoting vascular smooth muscle cell development and functional closure of the ductus arteriosus.607
Developmental diseases presenting with cardiac congenital defects
Numerous congenital conditions affect various parts of the body and are often accompanied by a high incidence of cardiac congenital defects, leading to a spectrum of distinctive features and potential health complications. Most of these diseases are caused by specific genetic defects, with some of the key signals involved in heart development also playing a role. We have summarized these conditions in Table 5.
Treatment for congenital heart defects
For a long time, many children born with CHD had limited treatment options, often receiving only palliative care during their early years. In the early to mid-20th century, physicians began attempting surgical treatments for children with CHD. Recently, more surgical techniques have been developed and applied to various types of CHD. Procedures such as Fontan surgery, atrial redirection, and arterial switch operations for treating complex CHD have since been established. Currently, surgery has become the primary treatment for CHD.608 While these new surgical techniques, along with interventional catheterizations, have reduced risks for less complex CHD cases, CHD remains a global health challenge due to the complexity of surgeries, high treatment costs, poor quality of life for patients, and challenges in managing complications.609 Compared to the development of surgical treatments for CHD, progress in pharmacological treatments has been slower. Most medications are used to improve and stabilize the preoperative condition of patients, manage postoperative complications, or provide palliative care. The use of NSAIDs for treating PDA has provided an alternative treatment method because of a deeper understanding of PDA pathogenesis. The scarcity of medical treatment options for CHD reflects our insufficient understanding of the mechanisms underlying congenital heart defects. In this section, we summarize the current strategies for treating CHD and discuss advancements in therapeutic approaches for this condition.
The current treatment strategies for CHD
Currently, CHD is considered a lifelong chronic condition. CHD patients often require one or more surgeries or interventional treatments during infancy and early childhood. After surgery, patients may experience complications such as heart failure, stroke, arrhythmias, reduced exercise tolerance, and increased risk of sudden death throughout their lives. Thus, early surgical treatment and lifelong management are equally important in treating CHD.610 Current treatment strategies for CHD encompass a range of approaches, including surgical interventions such as surgical closure for atrial/ventricular septal defects, PDA occlusion, the Mustard or Senning atrial switch procedure for transposition of the great arteries, and heart transplantation for end-stage heart failure. However, for some of the most lethal CHDs, such as HLHS, although surgical interventions have significantly improved survival rates, complex and severe complications may still develop, and most patients inevitably progress to heart failure.611 The staged palliative surgical approach for HLHS has been developed to simulate a physiological circulation and includes three stages: the first stage palliation, the second stage palliation, and the Fontan procedure.612 The first-stage treatments include the Norwood procedure with Blalock-Taussig shunt (BTS), Norwood with Sano modification, and the hybrid procedure. Long-term survival data for these methods remain limited. In high-volume centers, the postoperative mortality rate for Norwood surgery is approximately 22%, with common complications including respiratory insufficiency (21.6%), arrhythmias (19%), and cardiac arrest (12%).613 The other two surgical approaches do not show significant advantages in survival probability compared to the Norwood procedure.611 The second stage, typically performed 2 to 6 months after the Norwood surgery, is known as the bidirectional Glenn procedure. Several years later, the third stage, the Fontan procedure, is performed to direct blood flow from the superior and inferior vena cava directly to the pulmonary arteries, bypassing the right ventricle. However, up to 50% of patients with Fontan circulation may experience significant adverse events before adulthood, including late failure, reoperation, percutaneous interventions, pacemaker implantation, thromboembolic events, or supraventricular tachycardia.614
Although the Fontan procedure can temporarily improve cardiac function, over time, Fontan circulation can lead to increased central venous pressure, organ congestion, cardiac remodeling, and decreased cardiac output, resulting in cardiovascular and non-cardiovascular complications. Single ventricle patients after Fontan palliation, particularly those with heart failure, can exhibit significant metabolic changes, including altered substrate consumption, induced ketolysis, and abnormal glucose-lipid metabolism patterns, which may affect the function of other organs such as the liver, kidneys, nervous system, and lymphatics.615 Post-Fontan myocardial fibrosis and electrophysiological remodeling greatly increase the risk of heart failure.616 SGLT2 inhibitors can reduce edema and lower plasma brain natriuretic peptide levels in post-Fontan patients.617,618 Case series have reported that Angiotensin Receptor Neprilysin Inhibitors (ARNIs) can improve right ventricular systolic function, reduce hospitalization rates, and significantly improve protein-losing enteropathy symptoms, though NYHA functional class symptoms do not show significant changes.619 Post-Fontan surgical trauma, fibrosis, and cardiac remodeling may contribute to the development of electrophysiological remodeling and arrhythmias. Common arrhythmias include sick sinus syndrome, supraventricular tachycardias, atrial tachycardia, and atrial fibrillation.620 In canine models, post-Fontan surgery has been shown to cause electrophysiological changes and ionic remodeling, including shortened refractory periods, altered ion channel expression, and induced atrial tachycardia.621 For atrial arrhythmias such as intra-atrial re-entrant tachycardia (IART), nonautomatic focal atrial tachycardia (NAFAT), and atrial fibrillation, catheter ablation can reduce arrhythmia burden, but it is also associated with complications such as atrioventricular block and residual inducible arrhythmias, with a lower success rate compared to non-Fontan patients.622,623,624 Pacemaker implantation benefits hemodynamics and symptom relief, and recent guidelines recommend pacemaker implantation for treating Fontan circulation sinus node dysfunction.624 However, permanent ventricular pacing increases the risk of transplantation and late death in post-Fontan patients, potentially due to the wide QRS complex produced. Optimizing pacemaker therapy, including shortening QRS duration and maintaining atrioventricular synchrony through atrial pacing or adjusting the atrioventricular interval, may mitigate the adverse hemodynamic effects of pacemaker treatment.625,626,627 Thus, current treatment options for adverse outcomes due to Fontan surgery-related remodeling remain limited, and clinical evidence is still insufficient, posing challenges for managing post-Fontan patients. The risk of severe complications remains very high for post-Fontan patients, including ventricular systolic dysfunction, arrhythmias, Fontan-associated liver disease, renal dysfunction, protein-losing enteropathy, and plastic bronchitis.628 Therefore, while surgical interventions have significantly improved survival probabilities for patients with lethal CHDs, lifelong management remains a challenge.
Additionally, for treatment of CHD, interventional catheterizations can be performed either as standalone procedures or as part of hybrid procedures, avoiding the need for sternotomy/thoracotomy. Common interventional catheterizations include closure of shunt lesions or unusual collaterals, balloon dilation or stenting of narrowed great vessels, or transcatheter pulmonary valve implantation. Pharmacological treatments are also utilized to manage circulation issues. These include diuretics, beta-blockers, and angiotensin-converting enzyme inhibitors for heart failure; prostaglandin drugs and endothelin receptor antagonists for pulmonary hypertension;629,630 and anticoagulants, antithrombotics, antiarrhythmics, and antihypertensive medications for symptomatic treatment. Dedicated centers should provide specialized lifelong care for CHD patients with expertise in pediatric cardiology and cardiac surgery. These strategies aim to address the diverse spectrum of CHD severity and complexity, with advancements in surgical techniques and ongoing research contributing to improved outcomes and quality of life for patients. The interventional and randomized clinical trials for the treatment of CHD are provided in Table 6.
Advances in therapeutic strategies for CHD
Cell therapy has been explored for the treatment of several types of CHD, including the injection of autologous umbilical cord blood-derived cells in patients with HLHS,631,632 and the intracoronary delivery of autologous cardio-sphere-derived cells in patients with a single ventricle.633 These studies have shown improvements in cardiac function. However, such treatments currently serve only as adjuncts to surgical interventions for CHD patients. With an increased understanding of cardiac developmental mechanisms and technological advancements, it is hoped that future treatments will enable earlier diagnoses, early interventions, and preventive measures (Fig. 7). The advent of fetal cardiac intervention (FCI) represents a significant step toward modifying CHD before birth, potentially improving neonatal health outcomes. FCI is mainly used for conditions such as a restricted or intact atrial septum, severe aortic stenosis with evolving HLHS, severe mitral stenosis, and pulmonary atresia with an intact ventricular septum.634 The results are promising, with most children showing significant symptom improvement.635,636 However, due to the limited number of patients treated with FCI, the long-term effects of FCI on patients require further observation.
Current and future advanced treatment strategies for CHD. Currently, CHD is considered a lifelong condition and is primarily treated through early surgical interventions, multiple interventional catheterizations, and cell therapies. However, postsurgery CHD patients often face challenges such as decreased exercise tolerance, multiple cardiovascular and cerebrovascular complications, increased risk of sudden cardiac death, and decreased quality of life. Therefore, lifelong management, including long-term medication and care, is necessary for CHD patients. Advances in technology and a deeper understanding of cardiac development mechanisms aim to achieve earlier diagnosis and prevention of CHD, minimizing its impact and improving patient quality of life and longevity. Early intervention strategies, such as FCI in select CHD patients, are already underway, although further research into related drug therapies and gene treatments is needed. The development of cardiac imaging combined with AI technology enhances CHD diagnosis accuracy, while genetic testing aids in detecting pathogenic variants associated with CHD, facilitating early diagnosis. PGT offers the possibility for early prevention of CHD by identifying genetic defects or chromosomal abnormalities in embryos early in pregnancy; thus, selecting embryos most likely to result in successful pregnancies and healthy offspring is highly desirable. Utilizing AI to integrate multi-omics and clinical data for constructing risk prediction models will enable the identification of more precise genetic or environmental risk factors, further promoting early prevention strategies for CHD in the future. AI artificial intelligence, CHD congenital heart disease, FCI fetal cardiac intervention, PGT preimplantation genetic testing. This figure was created using Adobe Illustrator
Currently, there are no targeted drugs or gene therapies specific to different types of CHD. This limitation is due to an incomplete understanding of the mechanisms of heart development and the immature nature of the technology. Targeted therapies, which act on specific molecules or genetic pathways to block or interfere with disease progression, are primarily used in oncology and autoimmune diseases, such as EGFR or VEGFR-tyrosine kinase inhibitors for non-small cell lung cancer, benefiting from an in-depth understanding of these diseases. A recent study used targeted drugs (phosphodiesterase type 5 [PDE-5] inhibitors and prostacyclin analogs) therapy to reduce pulmonary artery pressure in 13 pregnant women with Eisenmenger syndrome, thereby increasing maternal survival rates.637 However, this approach is currently limited to the treatment of adult CHD patients. The complex regulatory mechanisms of cardiac development make it challenging to develop targeted drug therapy for the early treatment of CHD. However, as our understanding of cardiac development mechanisms improves, targeted therapies may become promising treatment methods for CHD, potentially avoiding surgical interventions. The emergence of clustered, regularly interspaced short palindromic repeats/CRISPR-associated protein 9 (CRISPR/Cas9) technology has made gene editing therapy possible, but it has raised significant ethical concerns, such as whether humans should modify their genes. Additionally, the technology still needs to be mature. For instance, off-target effects may unintentionally alter genes outside the target sequence, making its future application uncertain.
Clinical genetic and genomic testing for genetic defects causing CHD can aid in early diagnosis, including chromosome analysis, chromosomal microarray, targeted gene sequencing/genetic testing panels, genomic testing with exome sequencing, genomic testing with genome sequencing, and mitochondrial genome sequencing.638 For example, one study applied whole exome sequencing to analyze 69 known CHD genes and identified likely pathogenic mutations in up to 33% of familial CHD patients, demonstrating the successful use of a CHD candidate gene list for rapid and early identification of likely pathogenic variants from large datasets.639 However, due to insufficient knowledge of pathogenic variants in most CHDs, genetic and genomic testing can only identify a small proportion of fetuses carrying genetic defects, highlighting significant limitations in early diagnosis. A greater understanding of cardiac developmental mechanisms is needed to enhance the application of genetic testing in early CHD diagnosis.
Preventing CHD remains challenging. Preimplantation genetic testing (PGT) during in vitro fertilization (IVF) can screen embryos for genetic abnormalities before implantation, identifying those most likely to result in a successful pregnancy and healthy offspring. These methods include PGT-A (aneuploidy screening), PGT-M (monogenic/single-gene disorder screening), and PGT-SR (structural rearrangement screening).640 However, there are several limitations: our understanding of pathogenic variants in CHD is incomplete, making full prevention difficult; this method is only applicable to IVF; it raises psychological and ethical considerations, such as eugenics and sex selection. In addition to genetic defects, many environmental factors contribute to CHD.14 While factors such as infections during pregnancy, diabetes, smoking, and alcohol consumption are known to be closely related to CHD, the specific mechanisms by which these risk factors lead to clinical phenotypes of CHD are still unclear. Therefore, while preventing the occurrence of CHD can reduce the need for complex surgeries and lifelong medical management, significantly enhancing the overall quality of life for affected individuals, our limited understanding of cardiac development mechanisms and incomplete knowledge of risk factors for most CHD mean that we can currently only prevent the occurrence of a small number of CHD cases.
The application of AI for management of CHD
The development of AI technology is encouraging. AI has been applied in various aspects of CHD diagnosis, risk prediction and treatment, including analyzing cardiac imaging data to assist in diagnosing and monitoring CHD, assessing disease severity, and planning interventions.641,642,643 Advances in cardiac imaging and artificial intelligence (AI) technology have allowed us to understand fetal CHD development during pregnancy better.644,645 In prenatal diagnosis of CHD, AI has the potential to enhance detection rates by automatically extracting standard imaging planes from streams of ultrasound imaging data. One algorithm based on a deep learning framework evaluated its performance in automatically detecting and assessing the quality of cardiac four-chamber planes.646 A random forest algorithm was found to improve the sensitivity of prenatal CHD screening.647 Another study trained neural network models to differentiate between normal hearts and complex CHD, finding that the model’s sensitivity was comparable to that of clinicians and remained robust even with out-of-hospital or low-quality images.648 These algorithms can help clinicians detect CHD earlier, improve detection rates, and more accurately assess disease severity, thereby aiding in clinical decision-making. Future optimization of AI algorithms or development of learning algorithms specifically targeting fetal CHD could further enhance the detection of unique CHD.
The AI is also used to predict clinical outcomes by inputting clinical, imaging, and genomic data from CHD patients, particularly in the management of adult congenital heart disease (ACHD) patients.649 Today, 97% of children with CHD survive into adulthood, but the increased lifespan also brings a higher risk of acquired diseases, such as type 2 diabetes, hypertension, acquired cardiovascular diseases, and cancer. Managing the growing number of ACHD patients has become a challenge.609,650 Transferring ACHD patients to specialist ACHD centers is a reasonable approach. Staff at these centers typically include adult and pediatric cardiologists with ACHD certification, CHD surgeons, pulmonary vascular disease experts, clinical geneticists, and psychologists, who work together to develop the most appropriate management and follow-up plans for each patient.610 The development of AI technology also supports improving the quality of ACHD patient management. Risk stratification systems are central to managing ACHD patients. Traditional ACHD risk stratification systems are based on limited data from single or few institutions, while AI can facilitate the integration of larger or longitudinal datasets, better fitting the underlying data and thus improving predictive capabilities.651 Currently, several studies have applied deep learning algorithms based on natural language processing,652 cardiac magnetic resonance (CMR) data,653 and recurrent neural networks654 for risk stratification in ACHD patients, predicting outcomes such as heart failure, prognosis, and mortality. These studies suggest the feasibility of using AI models for risk stratification. AI-based algorithms are also helpful in predicting postoperative complications, disease progression, and treatment outcomes.655 For instance, in managing heart transplant patients, AI models can more accurately predict graft failure and mortality and promote positive behavioral changes to reduce future cardiovascular risks.656 AI-driven risk prediction models also assist in predicting individual mortality risks for CHD patients undergoing surgery and ICU length of stay, thereby improving care planning and resource management.657,658 In addition to enhancing early diagnosis of CHD, AI algorithms can analyze electrocardiograms (ECGs) and cardiac imaging data to precisely identify changes in characteristics, aiding in more accurate risk prediction. AI-based ECG evaluation can address the issue of limited data in certain CHD populations. For example, Mayourian and colleagues developed and validated an AI-ECG model for predicting biventricular dysfunction and dilation in ACHD patients, which reduces the frequency of echocardiograms and CMRs to lower costs and improve access to care.659 Another study significantly improved the accuracy of junctional ectopic tachycardia detection in CHD patients using deep neural networks, allowing for precise diagnosis and timely intervention for this life-threatening postoperative arrhythmia.660 Machine learning models based on cardiac CMR can also help predict deterioration in patients with repaired ToF.661
The combination of AI and imaging technology facilitates surgical treatment for CHD.645 For example, generative adversarial networks have been successfully used to predict the optimal size, shape, and position of transannular patches to improve cardiac CT outcomes for patients with ToF.662 A random forest model based on preoperative cardiac CT has been shown to predict which post-Glenn shunt patients are at low or high risk for a mean pulmonary arterial pressure (mPAP) > 15 mmHg, thereby reducing the need for right heart catheterization in these patients.663 Another study utilized a Cycle Generative Adversarial Network to align pre-procedural CTs with intra-procedural transesophageal echocardiographic images, improving surgical navigation for CHD patients.664 One significant advantage of AI is its ability to integrate and synthesize multi-layered medical data, including clinical information, imaging data, genetic information, and environmental factors, to provide personalized analysis and precision medicine. While congenital heart defects can be broadly classified as mild, moderate, or severe, more detailed classifications can exceed 30 types. This underscores the complexity of ACHD patients and importance of personalized treatment for them.610 Although AI technology in the field of CHD and healthcare is still in its early stages, it has already yielded many promising results. In the future, AI technology is expected to advance the development of personalized treatments and interventions for ACHD patients.
At the same time, applying AI algorithms to integrate multi-omics data and clinical information from CHD patients to identify genetic variations and environmental factors associated with CHD susceptibility and severity, and developing corresponding risk prediction models, could advance early prevention of CHD. A recent study combined metabolomics and a machine learning model to screen maternal serum metabolites, identifying a metabolomic fingerprint for CHD and providing a non-invasive screening method for early detection of the condition.665 Another study using AI and epigenomics found that DNA methylation could predict aortic coarctation in neonates.666 However, these studies have only applied single-omics and AI algorithms, and the full potential of AI technology has yet to be realized. In the future, AI technology, by integrating multi-layered big data, could identify more genetic and non-genetic risk factors for CHD, thereby advancing early prevention and diagnosis.
Conclusion and perspective
This review provides an overview of the fundamental processes and molecular mechanisms underlying heart development, along with insights into CHD and current treatment approaches. First, from a historical perspective, we review the progress of heart development research. Each significant breakthrough in cardiac development research has been accompanied by advancements in related disciplines and technologies. Early observational studies elucidated the origins and processes of heart development, while molecular biology techniques have enabled the study of molecular mechanisms across in vivo and in vitro models. Technological advances continue to provide us with more research tools, allowing for a multifaceted and multilevel understanding of heart development. Heart development is divided into five stages: pre-cardiac and cardiac mesoderm induction, cardiac crescent formation, heart tube formation, cardiac looping, and four-chambered fetal heart formation. Numerous molecular signals regulate each stage of heart development, including GFs, TFs, WNT signal, Shh signal, Hippo signal, Notch signal, ECM, and epigenetic modifications. These signals often play roles in multiple stages of heart development, sometimes exerting opposite effects. For instance, FGF and BMP signals are crucial from mesoderm cardiac induction to chamber formation. WNT signaling is essential for early mesoderm specification, and its subsequent inhibition is critical for myocardial cell differentiation, reflecting the complexity of the regulatory network involved in heart development. Additionally, additional molecular mechanisms, including metabolism, autophagy, and macrophages, have been shown to be involved in heart development regulation. Research into these mechanisms in heart development is still in its early stages, and their roles will undergo further investigation in the future.
Finally, we summarize diseases caused by abnormalities in heart development, including common CHDs such as septal defects, conotruncal defects, valve defects, PDA, HLHS, and various developmental diseases associated with a high incidence of CHD. Currently, CHD requires lifelong management, primarily through surgical and palliative care approaches. The limited treatment options available for CHD stem from our incomplete understanding of the mechanisms regulating heart development. As our understanding of cardiac development mechanisms deepens in the future, we can prevent the occurrence of most CHDs and diagnose and intervene early in those cases, thereby preventing abnormal cardiac development and restoring it to its normal trajectory. However, this goal remains distant for now, but the development of new technologies offers hope. Therefore, further understanding of the processes and mechanisms of heart development is essential for developing new and effective treatments for CHD.
With the advancement of new technologies, especially in recent years, with the development of stem cell and sequencing technologies, we are gradually shifting from a perspective focused on single molecules or signals to understanding heart development from the viewpoint of the entire regulatory network. This network encompasses not only the participation of many genes or proteins but also integrates changes across multiple levels, including DNA, RNA, proteins, epigenetic or posttranslational modifications, metabolism, and more, over time and space. The development of multi-omics technologies and advancements in AI facilitates this holistic approach to understand heart development. Stem cell technologies play a crucial supportive role in this process, providing new tools for studying heart development. hPSCs, derived from patients with genetic backgrounds associated with heart developmental defects, address the limitations of most heart development studies conducted on animal models. These cells can differentiate into various cardiac cell types, including cardiomyocytes,271 endothelial cells,667 epicardial cells,668 and smooth muscle cells,669 allowing the study of pathogenic mechanisms in different cardiac cells in vitro.
Furthermore, the application of novel technologies has expanded the potential utility of hPSC-derived CMs in heart development research. The integration of CRISPR/Cas9 technology with hPSCs enables the exploration of the effects of variants with unknown significance in cardiac development by introducing these variants into wild-type cell lines or correcting them in patient-specific cell lines.670 Additionally, unlike cardiac microtissues and engineered cardiac tissues, cardiac organoids are developed by applying tissue-specific differentiation factors and hydrogels to promote the self-organization of pluripotent stem cells into tissue patterns resembling the embryonic heart, exhibiting key features of cardiac development.671 Recent studies have demonstrated the creation of hPSC-derived complex, highly structured, three-dimensional heart-forming organoids, including myocardial layers surrounded by septum-transversum-like anlagen and endocardial-like cell layers.672 Another study utilized hPSCs to construct heart organoids with complex lumens and vascular systems capable of mimicking congenital heart defects induced by gestational diabetes.673 Another study generated cardioids from three different types of cardiac progenitors, including FHF progenitors differentiating into left ventricle-like cardioids, anterior SHF progenitors differentiating into right ventricle and OFT-like cardioids, and posterior SHF progenitors forming atrial and AVC cardioids. These parts were functionally connected to form a multi-chamber heart model with shared cavities. This study successfully used these cardioids to in vitro model cardiac defects, including the effects of ISL1-KO on the RV, atria, and OFT, and the impact of TBX5-KO on AVC and CM differentiation efficiency.674 With further development of stem cell and organoid technologies, constructing in vitro models of CHD through molecular signaling and gene editing may become feasible, offering a promising approach for exploring heart development mechanisms and drug screening.
Moreover, with the advancement of sequencing technologies, various sequencing techniques, including single-cell transcriptomics, spatial transcriptomics, metabolomics, and epigenomics, have been applied in the field of cardiac development, providing a comprehensive understanding of the mechanisms and processes of cardiac development. However, the accompanying large datasets make subsequent comprehensive analysis challenging, which can potentially be addressed by powerful AI technologies. The application of AI technologies such as machine learning or deep learning to process sequencing data related to cardiac development enables the integration of data from different sources, such as genomic data, epigenomic data, transcriptomic data, and clinical data. This approach helps identify gene variants and molecular features associated with CHD susceptibility, severity, and treatment response.675,676 Subsequent validation and research in in vitro and in vivo models will further advance our understanding of cardiac development processes and mechanisms, enabling early prevention and intervention for CHD. For instance, this approach could facilitate early screening of CHD in affected children by providing a more comprehensive CHD candidate genetic defect list or identifying risk factors and molecular signaling characteristics leading to CHD during pregnancy for early pharmacological treatment development, thereby avoiding the necessity for later surgical treatment. Nevertheless, this remains a distant goal requiring further research in the future.
References
Brade, T., Pane, L. S., Moretti, A., Chien, K. R. & Laugwitz, K. L. Embryonic heart progenitors and cardiogenesis. Cold Spring Harb. Perspect. Med. 3, a013847 (2013).
Meilhac, S. M. & Buckingham, M. E. The deployment of cell lineages that form the mammalian heart. Nat. Rev. Cardiol. 15, 705–724 (2018).
Buijtendijk, M. F. J., Barnett, P. & van den Hoff, M. J. B. Development of the human heart. Am. J. Med. Genet. C Semin. Med. Genet. 184, 7–22 (2020).
Moorman, A. F. & Christoffels, V. M. Cardiac chamber formation: development, genes, and evolution. Physiol. Rev. 83, 1223–1267 (2003).
Abu-Issa, R. & Kirby, M. L. Heart field: from mesoderm to heart tube. Annu. Rev. Cell Dev. Biol. 23, 45–68 (2007).
Miyamoto, M. & Kwon, C. Uncovering the origins and lineage markers of human heart fields. Cell Stem Cell 29, 1285–1287 (2022).
Cao, C. et al. Nkx2.5: a crucial regulator of cardiac development, regeneration and diseases. Front. Cardiovasc. Med. 10, 1270951 (2023).
Kinnunen, S. et al. Nuclear receptor-like structure and interaction of congenital heart disease-associated factors GATA4 and NKX2-5. PLoS One 10, e0144145 (2015).
Wu, L. et al. Bone morphogenetic protein 4 promotes the differentiation of Tbx18-positive epicardial progenitor cells to pacemaker-like cells. Exp. Ther. Med. 17, 2648–2656 (2019).
Gu, Y. et al. Multi-omics profiling visualizes dynamics of cardiac development and functions. Cell Rep. 41, 111891 (2022).
Kanemaru, K. et al. Spatially resolved multiomics of human cardiac niches. Nature 619, 801–810 (2023).
Biggs, S. E., Gilchrist, B. & May, K. R. Chromosome 22q11.2 deletion (DiGeorge Syndrome): immunologic features, diagnosis, and management. Curr. Allergy Asthma Rep. 23, 213–222 (2023).
Linglart, L. & Gelb, B. D. Congenital heart defects in Noonan syndrome: diagnosis, management, and treatment. Am. J. Med. Genet. C. Semin. Med. Genet. 184, 73–80 (2020).
Boyd, R., McMullen, H., Beqaj, H. & Kalfa, D. Environmental exposures and congenital heart disease. Pediatrics 149 (2022).
Morton, S. U., Quiat, D., Seidman, J. G. & Seidman, C. E. Genomic frontiers in congenital heart disease. Nat. Rev. Cardiol. 19, 26–42 (2022).
Needham, J. A History of Embryology (Cambridge Univ. Press, 1959).
Grzybowski, A. & Pietrzak, K. Robert Remak (1815-1865): discoverer of the fungal character of dermatophytoses. Clin. Dermatol 31, 802–805 (2013).
de la Cruz, M. V. & Markwald, R. R. Living Morphogenesis of the Heart (Birkhäuser, 1998).
Hill, M. A. Embryology Paper - Development of the human heart from its earliest appearance to the stage found in embryos of twenty paired somites (1927), <https://embryology.med.unsw.edu.au/embryology/index.php/Paper_-_Development_of_the_human_heart_from_its_earliest_appearance_to_the_stage_found_in_embryos_of_twenty_paired_somites_(1927)> (2024).
Rawles, M. E. The heart-forming areas of the early chick blastoderm. Physiol. Zool. 16, 22–43 (1943).
Stalsberg, H. & DeHaan, R. L. The precardiac areas and formation of the tubular heart in the chick embryo. Dev. Biol. 19, 128–159 (1969).
Stalsberg, H. & DeHaan, R. L. Endodermal movements during foregut formation in the chick embryo. Dev. Biol. 18, 198–215 (1968).
Yelon, D. Commentary on “The precardiac areas and formation of the tubular heart in the chick embryo” by Stalsberg and DeHaan, 1969. Dev. Biol. 456, 105–137 (2019).
Castro-Quezada, A., Nadal-Ginard, B. & De La Cruz, M. V. Experimental study of the formation of the bulboventricular loop in the chick. J. Embryol. Exp. Morphol. 27, 623–637 (1972).
de la Cruz, M. V., Sanchez Gomez, C., Arteaga, M. M. & Arguello, C. Experimental study of the development of the truncus and the conus in the chick embryo. J. Anat. 123, 661–686 (1977).
De La Cruz, M. V., Sanchez-Gomez, C. & Palomino, M. A. The primitive cardiac regions in the straight tube heart (Stage 9) and their anatomical expression in the mature heart: an experimental study in the chick embryo. J. Anat. 165, 121–131 (1989).
De la Cruz, M. V., Gomez, C. S. & Cayre, R. The developmental components of the ventricles: their significance in congenital cardiac malformations. Cardiol. Young-. 1, 123–128 (1991).
de la Cruz, M. V., Castillo, M. M., Villavicencio, L., Valencia, A. & Moreno-Rodriguez, R. A. Primitive interventricular septum, its primordium, and its contribution in the definitive interventricular septum: in vivo labelling study in the chick embryo heart. Anat. Rec. 247, 512–520 (1997).
Manner, J., Seidl, W. & Steding, G. Correlation between the embryonic head flexures and cardiac development. An experimental study in chick embryos. Anat. Embryol. 188, 269–285 (1993).
Van Mierop, L. H., Alley, R. D., Kausel, H. W. & Stranahan, A. The anatomy and embryology of endocardial cushion defects. J. Thorac. Cardiovasc. Surg. 43, 71–83 (1962).
De la Cruz, M. V., Gimenez-Ribotta, M., Saravalli, O. & Cayre, R. The contribution of the inferior endocardial cushion of the atrioventricular canal to cardiac septation and to the development of the atrioventricular valves: study in the chick embryo. Am. J. Anat. 166, 63–72 (1983).
Wenink, A. C. & Gittenberger-de Groot, A. C. The role of atrioventricular endocardial cushions in the septation of the heart. Int. J. Cardiol. 8, 25–44 (1985).
Noden, D. M. Origins and patterning of avian outflow tract endocardium. Development 111, 867–876 (1991).
Folkman, J. Toward an understanding of angiogenesis: search and discovery. Perspect. Biol. Med. 29, 10–36 (1985).
Pardanaud, L., Altmann, C., Kitos, P., Dieterlen-Lievre, F. & Buck, C. A. Vasculogenesis in the early quail blastodisc as studied with a monoclonal antibody recognizing endothelial cells. Development 100, 339–349 (1987).
Risau, W. & Lemmon, V. Changes in the vascular extracellular matrix during embryonic vasculogenesis and angiogenesis. Dev. Biol. 125, 441–450 (1988).
Coffin, J. D. & Poole, T. J. Embryonic vascular development: immunohistochemical identification of the origin and subsequent morphogenesis of the major vessel primordia in quail embryos. Development 102, 735–748 (1988).
Heine, U. I., Roberts, A. B., Munoz, E. F., Roche, N. S. & Sporn, M. B. Effects of retinoid deficiency on the development of the heart and vascular system of the quail embryo. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 50, 135–152 (1985).
Osmond, M. K., Butler, A. J., Voon, F. C. & Bellairs, R. The effects of retinoic acid on heart formation in the early chick embryo. Development 113, 1405–1417 (1991).
Yutzey, K. E., Rhee, J. T. & Bader, D. Expression of the atrial-specific myosin heavy chain AMHC1 and the establishment of anteroposterior polarity in the developing chicken heart. Development 120, 871–883 (1994).
Lints, T. J., Parsons, L. M., Hartley, L., Lyons, I. & Harvey, R. P. Nkx-2.5: a novel murine homeobox gene expressed in early heart progenitor cells and their myogenic descendants. Development 119, 419–431 (1993).
Kelley, C., Blumberg, H., Zon, L. I. & Evans, T. GATA-4 is a novel transcription factor expressed in endocardium of the developing heart. Development 118, 817–827 (1993).
Laverriere, A. C. et al. GATA-4/5/6, a subfamily of three transcription factors transcribed in developing heart and gut. J. Biol. Chem. 269, 23177–23184 (1994).
Edmondson, D. G., Lyons, G. E., Martin, J. F. & Olson, E. N. Mef2 gene expression marks the cardiac and skeletal muscle lineages during mouse embryogenesis. Development 120, 1251–1263 (1994).
Parlow, M. H., Bolender, D. L., Kokan-Moore, N. P. & Lough, J. Localization of bFGF-like proteins as punctate inclusions in the preseptation myocardium of the chicken embryo. Dev. Biol. 146, 139–147 (1991).
Choy, M., Armstrong, M. T. & Armstrong, P. B. Transforming growth factor-beta 1 localized within the heart of the chick embryo. Anat. Embryol. 183, 345–352 (1991).
Lough, J. et al. Combined BMP-2 and FGF-4, but neither factor alone, induces cardiogenesis in non-precardiac embryonic mesoderm. Dev. Biol. 178, 198–202 (1996).
Tsuda, T., Philp, N., Zile, M. H. & Linask, K. K. Left-right asymmetric localization of flectin in the extracellular matrix during heart looping. Dev. Biol. 173, 39–50 (1996).
Icardo, J. M. & Manasek, F. J. Fibronectin distribution during early chick embryo heart development. Dev. Biol. 95, 19–30 (1983).
Srivastava, D. et al. Regulation of cardiac mesodermal and neural crest development by the bHLH transcription factor, dHAND. Nat. Genet. 16, 154–160 (1997).
Mjaatvedt, C. H. et al. The outflow tract of the heart is recruited from a novel heart-forming field. Dev. Biol. 238, 97–109 (2001).
Waldo, K. L. et al. Conotruncal myocardium arises from a secondary heart field. Development 128, 3179–3188 (2001).
Kelly, R. G., Brown, N. A. & Buckingham, M. E. The arterial pole of the mouse heart forms from Fgf10-expressing cells in pharyngeal mesoderm. Dev. Cell 1, 435–440 (2001).
Shenje, L. T. et al. Precardiac deletion of Numb and Numblike reveals renewal of cardiac progenitors. Elife 3, e02164 (2014).
Lescroart, F., Mohun, T., Meilhac, S. M., Bennett, M. & Buckingham, M. Lineage tree for the venous pole of the heart: clonal analysis clarifies controversial genealogy based on genetic tracing. Circ. Res. 111, 1313–1322 (2012).
Dominguez, J. N., Meilhac, S. M., Bland, Y. S., Buckingham, M. E. & Brown, N. A. Asymmetric fate of the posterior part of the second heart field results in unexpected left/right contributions to both poles of the heart. Circ. Res. 111, 1323–1335 (2012).
Zhou, Z. et al. Temporally distinct Six2-positive second heart field progenitors regulate mammalian heart development and disease. Cell Rep. 18, 1019–1032 (2017).
Zhao, K. & Yang, Z. The second heart field: the first 20 years. Mamm. Genome 34, 216–228 (2023).
Cai, C. L. et al. Isl1 identifies a cardiac progenitor population that proliferates prior to differentiation and contributes a majority of cells to the heart. Dev. Cell 5, 877–889 (2003).
Watanabe, Y. et al. Role of mesodermal FGF8 and FGF10 overlaps in the development of the arterial pole of the heart and pharyngeal arch arteries. Circ. Res. 106, 495–503 (2010).
Engleka, K. A. et al. Islet1 derivatives in the heart are of both neural crest and second heart field origin. Circ. Res. 110, 922–926 (2012).
Ma, Q., Zhou, B. & Pu, W. T. Reassessment of Isl1 and Nkx2-5 cardiac fate maps using a Gata4-based reporter of Cre activity. Dev. Biol. 323, 98–104 (2008).
Lescroart, F. et al. Defining the earliest step of cardiovascular lineage segregation by single-cell RNA-seq. Science 359, 1177–1181 (2018).
Ivanovitch, K. et al. Ventricular, atrial, and outflow tract heart progenitors arise from spatially and molecularly distinct regions of the primitive streak. PLoS Biol. 19, e3001200 (2021).
Xiong, H. et al. Single-cell transcriptomics reveals chemotaxis-mediated intraorgan crosstalk during cardiogenesis. Circ. Res. 125, 398–410 (2019).
Yang, D. et al. Modeling human multi-lineage heart field development with pluripotent stem cells. Cell Stem Cell 29, 1382–1401 e1388 (2022).
Gunthel, M., Barnett, P. & Christoffels, V. M. Development, proliferation, and growth of the mammalian heart. Mol. Ther. 26, 1599–1609 (2018).
Ali, H., Braga, L. & Giacca, M. Cardiac regeneration and remodelling of the cardiomyocyte cytoarchitecture. FEBS J. 287, 417–438 (2020).
Gong, G. et al. Parkin-mediated mitophagy directs perinatal cardiac metabolic maturation in mice. Science 350, aad2459 (2015).
Buckingham, M., Meilhac, S. & Zaffran, S. Building the mammalian heart from two sources of myocardial cells. Nat. Rev. Genet. 6, 826–835 (2005).
Bondue, A. & Blanpain, C. Mesp1: a key regulator of cardiovascular lineage commitment. Circ. Res. 107, 1414–1427 (2010).
Noseda, M., Peterkin, T., Simoes, F. C., Patient, R. & Schneider, M. D. Cardiopoietic factors: extracellular signals for cardiac lineage commitment. Circ. Res. 108, 129–152 (2011).
Gessert, S. & Kuhl, M. The multiple phases and faces of wnt signaling during cardiac differentiation and development. Circ. Res. 107, 186–199 (2010).
Costello, I. et al. The T-box transcription factor Eomesodermin acts upstream of Mesp1 to specify cardiac mesoderm during mouse gastrulation. Nat. Cell Biol. 13, 1084–1091 (2011).
Harris, I. S. & Black, B. L. Development of the endocardium. Pediatr. Cardiol. 31, 391–399 (2010).
Kelly, R. G., Buckingham, M. E. & Moorman, A. F. Heart fields and cardiac morphogenesis. Cold Spring Harb. Perspect. Med. 4 (2014).
Waardenberg, A. J., Ramialison, M., Bouveret, R. & Harvey, R. P. Genetic networks governing heart development. Cold Spring Harb. Perspect. Med. 4, a013839 (2014).
Kelly, R. G. The second heart field. Curr. Top. Dev. Biol. 100, 33–65 (2012).
Christoffels, V. M., Smits, G. J., Kispert, A. & Moorman, A. F. Development of the pacemaker tissues of the heart. Circ. Res. 106, 240–254 (2010).
Kwon, C. et al. Canonical Wnt signaling is a positive regulator of mammalian cardiac progenitors. Proc. Natl Acad. Sci. USA 104, 10894–10899 (2007).
van den Berg, G. et al. A caudal proliferating growth center contributes to both poles of the forming heart tube. Circ. Res. 104, 179–188 (2009).
Scholl, A. M. & Kirby, M. L. Signals controlling neural crest contributions to the heart. Wiley Interdiscip. Rev. Syst. Biol. Med. 1, 220–227 (2009).
Development Timeline of Human Heart Embryology, <https://www.vhlab.umn.edu/atlas/congenital-defects-tutorial/normal-cardiac-development/development-timeline-of-human-heart-embryology.shtml> (2024).
Sylva, M., van den Hoff, M. J. & Moorman, A. F. Development of the human heart. Am. J. Med. Genet. A 164A, 1347–1371 (2014).
Christoffels, V. M. et al. Chamber formation and morphogenesis in the developing mammalian heart. Dev. Biol. 223, 266–278 (2000).
Sizarov, A. et al. Formation of the building plan of the human heart: morphogenesis, growth, and differentiation. Circulation 123, 1125–1135 (2011).
Soufan, A. T. et al. Regionalized sequence of myocardial cell growth and proliferation characterizes early chamber formation. Circ. Res. 99, 545–552 (2006).
Del Monte-Nieto, G. et al. Control of cardiac jelly dynamics by NOTCH1 and NRG1 defines the building plan for trabeculation. Nature 557, 439–445 (2018).
MacGrogan, D., Munch, J. & de la Pompa, J. L. Notch and interacting signalling pathways in cardiac development, disease, and regeneration. Nat. Rev. Cardiol. 15, 685–704 (2018).
de Lange, F. J. et al. Lineage and morphogenetic analysis of the cardiac valves. Circ. Res. 95, 645–654 (2004).
Garside, V. C., Chang, A. C., Karsan, A. & Hoodless, P. A. Co-ordinating Notch, BMP, and TGF-beta signaling during heart valve development. Cell Mol. Life Sci. 70, 2899–2917 (2013).
MacGrogan, D., Luna-Zurita, L. & de la Pompa, J. L. Notch signaling in cardiac valve development and disease. Birth Defects Res. A Clin. Mol. Teratol. 91, 449–459 (2011).
Jiang, X., Rowitch, D. H., Soriano, P., McMahon, A. P. & Sucov, H. M. Fate of the mammalian cardiac neural crest. Development 127, 1607–1616 (2000).
Kuriyama, S. & Mayor, R. Molecular analysis of neural crest migration. Philos. Trans. R. Soc. Lond. B Biol. Sci. 363, 1349–1362 (2008).
Hutson, M. R. et al. Cardiac arterial pole alignment is sensitive to FGF8 signaling in the pharynx. Dev. Biol. 295, 486–497 (2006).
Hutson, M. R. & Kirby, M. L. Model systems for the study of heart development and disease. Cardiac neural crest and conotruncal malformations. Semin. Cell Dev. Biol. 18, 101–110 (2007).
Waldo, K. L. et al. Secondary heart field contributes myocardium and smooth muscle to the arterial pole of the developing heart. Dev. Biol. 281, 78–90 (2005).
Keyte, A. & Hutson, M. R. The neural crest in cardiac congenital anomalies. Differentiation 84, 25–40 (2012).
van Eif, V. W. W., Devalla, H. D., Boink, G. J. J. & Christoffels, V. M. Transcriptional regulation of the cardiac conduction system. Nat. Rev. Cardiol. 15, 617–630 (2018).
Yi, T. et al. Electrophysiological mapping of embryonic mouse hearts: mechanisms for developmental pacemaker switch and internodal conduction pathway. J. Cardiovasc. Electrophysiol. 23, 309–318 (2012).
Gros, D. et al. Genetically modified mice: tools to decode the functions of connexins in the heart-new models for cardiovascular research. Cardiovasc. Res. 62, 299–308 (2004).
Kruithof, B. P. et al. BMP and FGF regulate the differentiation of multipotential pericardial mesoderm into the myocardial or epicardial lineage. Dev. Biol. 295, 507–522 (2006).
Zhou, B., von Gise, A., Ma, Q., Rivera-Feliciano, J. & Pu, W. T. Nkx2-5- and Isl1-expressing cardiac progenitors contribute to proepicardium. Biochem. Biophys. Res. Commun. 375, 450–453 (2008).
Sucov, H. M., Gu, Y., Thomas, S., Li, P. & Pashmforoush, M. Epicardial control of myocardial proliferation and morphogenesis. Pediatr. Cardiol. 30, 617–625 (2009).
Lie-Venema, H. et al. Origin, fate, and function of epicardium-derived cells (EPDCs) in normal and abnormal cardiac development. Sci. World J. 7, 1777–1798 (2007).
Wessels, A. et al. Epicardially derived fibroblasts preferentially contribute to the parietal leaflets of the atrioventricular valves in the murine heart. Dev. Biol. 366, 111–124 (2012).
Aanhaanen, W. T. et al. Developmental origin, growth, and three-dimensional architecture of the atrioventricular conduction axis of the mouse heart. Circ. Res. 107, 728–736 (2010).
Khosravi, F., Ahmadvand, N., Bellusci, S. & Sauer, H. The multifunctional contribution of FGF signaling to cardiac development, homeostasis, disease and repair. Front. Cell Dev. Biol. 9, 672935 (2021).
Kimelman, D. & Kirschner, M. Synergistic induction of mesoderm by FGF and TGF-beta and the identification of an mRNA coding for FGF in the early Xenopus embryo. Cell 51, 869–877 (1987).
Slack, J. M., Darlington, B. G., Heath, J. K. & Godsave, S. F. Mesoderm induction in early Xenopus embryos by heparin-binding growth factors. Nature 326, 197–200 (1987).
Fletcher, R. B. & Harland, R. M. The role of FGF signaling in the establishment and maintenance of mesodermal gene expression in Xenopus. Dev. Dyn. 237, 1243–1254 (2008).
Sempou, E., Lakhani, O. A., Amalraj, S. & Khokha, M. K. Candidate heterotaxy gene FGFR4 is essential for patterning of the left-right organizer in xenopus. Front. Physiol. 9, 1705 (2018).
Guzzetta, A. et al. Hedgehog-FGF signaling axis patterns anterior mesoderm during gastrulation. Proc. Natl. Acad. Sci. USA 117, 15712–15723 (2020).
Mesbah, K. et al. Identification of a Tbx1/Tbx2/Tbx3 genetic pathway governing pharyngeal and arterial pole morphogenesis. Hum. Mol. Genet. 21, 1217–1229 (2012).
Ilagan, R. et al. Fgf8 is required for anterior heart field development. Development 133, 2435–2445 (2006).
Park, E. J. et al. Required, tissue-specific roles for Fgf8 in outflow tract formation and remodeling. Development 133, 2419–2433 (2006).
Sato, A. et al. FGF8 signaling is chemotactic for cardiac neural crest cells. Dev. Biol. 354, 18–30 (2011).
Marguerie, A. et al. Congenital heart defects in Fgfr2-IIIb and Fgf10 mutant mice. Cardiovasc. Res. 71, 50–60 (2006).
Rochais, F. et al. FGF10 promotes regional foetal cardiomyocyte proliferation and adult cardiomyocyte cell-cycle re-entry. Cardiovasc. Res. 104, 432–442 (2014).
Vincentz, J. W., McWhirter, J. R., Murre, C., Baldini, A. & Furuta, Y. Fgf15 is required for proper morphogenesis of the mouse cardiac outflow tract. Genesis 41, 192–201 (2005).
Lavine, K. J. et al. Endocardial and epicardial-derived FGF signals regulate myocardial proliferation and differentiation in vivo. Dev. Cell 8, 85–95 (2005).
Hotta, Y. et al. Fgf16 is required for cardiomyocyte proliferation in the mouse embryonic heart. Dev. Dyn. 237, 2947–2954 (2008).
Lu, S. Y. et al. Embryonic survival and severity of cardiac and craniofacial defects are affected by genetic background in fibroblast growth factor-16 null mice. DNA Cell Biol. 29, 407–415 (2010).
Jennbacken, K. et al. Phenotypic screen with the human secretome identifies FGF16 as inducing proliferation of iPSC-derived cardiac progenitor cells. Int. J. Mol. Sci. 20 (2019).
Lavine, K. J. et al. Fibroblast growth factor signals regulate a wave of Hedgehog activation that is essential for coronary vascular development. Genes Dev. 20, 1651–1666 (2006).
Morabito, C. J., Dettman, R. W., Kattan, J., Collier, J. M. & Bristow, J. Positive and negative regulation of epicardial-mesenchymal transformation during avian heart development. Dev. Biol. 234, 204–215 (2001).
Dronkers, E., Wauters, M. M. M., Goumans, M. J. & Smits, A. M. Epicardial TGFbeta and BMP signaling in cardiac regeneration: what lesson can we learn from the developing heart? Biomolecules 10 (2020).
Jones, C. M., Kuehn, M. R., Hogan, B. L., Smith, J. C. & Wright, C. V. Nodal-related signals induce axial mesoderm and dorsalize mesoderm during gastrulation. Development 121, 3651–3662 (1995).
Zhou, X., Sasaki, H., Lowe, L., Hogan, B. L. & Kuehn, M. R. Nodal is a novel TGF-beta-like gene expressed in the mouse node during gastrulation. Nature 361, 543–547 (1993).
Gritsman, K., Talbot, W. S. & Schier, A. F. Nodal signaling patterns the organizer. Development 127, 921–932 (2000).
Liguori, G. L. et al. Cripto-independent Nodal signaling promotes positioning of the A-P axis in the early mouse embryo. Dev. Biol. 315, 280–289 (2008).
Ding, J. et al. Cripto is required for correct orientation of the anterior-posterior axis in the mouse embryo. Nature 395, 702–707 (1998).
Gu, Z. et al. The type I serine/threonine kinase receptor ActRIA (ALK2) is required for gastrulation of the mouse embryo. Development 126, 2551–2561 (1999).
Mishina, Y., Crombie, R., Bradley, A. & Behringer, R. R. Multiple roles for activin-like kinase-2 signaling during mouse embryogenesis. Dev. Biol. 213, 314–326 (1999).
Song, J. et al. The type II activin receptors are essential for egg cylinder growth, gastrulation, and rostral head development in mice. Dev. Biol. 213, 157–169 (1999).
Gu, Z. et al. The type I activin receptor ActRIB is required for egg cylinder organization and gastrulation in the mouse. Genes Dev. 12, 844–857 (1998).
Winnier, G., Blessing, M., Labosky, P. A. & Hogan, B. L. Bone morphogenetic protein-4 is required for mesoderm formation and patterning in the mouse. Genes Dev. 9, 2105–2116 (1995).
Beppu, H. et al. BMP type II receptor is required for gastrulation and early development of mouse embryos. Dev. Biol. 221, 249–258 (2000).
Mishina, Y., Suzuki, A., Ueno, N. & Behringer, R. R. Bmpr encodes a type I bone morphogenetic protein receptor that is essential for gastrulation during mouse embryogenesis. Genes Dev. 9, 3027–3037 (1995).
Klaus, A., Saga, Y., Taketo, M. M., Tzahor, E. & Birchmeier, W. Distinct roles of Wnt/beta-catenin and Bmp signaling during early cardiogenesis. Proc. Natl. Acad. Sci. USA 104, 18531–18536 (2007).
Miura, S., Davis, S., Klingensmith, J. & Mishina, Y. BMP signaling in the epiblast is required for proper recruitment of the prospective paraxial mesoderm and development of the somites. Development 133, 3767–3775 (2006).
Zhang, H. & Bradley, A. Mice deficient for BMP2 are nonviable and have defects in amnion/chorion and cardiac development. Development 122, 2977–2986 (1996).
Chen, H. et al. BMP10 is essential for maintaining cardiac growth during murine cardiogenesis. Development 131, 2219–2231 (2004).
Jiao, K. et al. An essential role of Bmp4 in the atrioventricular septation of the mouse heart. Genes Dev. 17, 2362–2367 (2003).
Liu, W. et al. Bmp4 signaling is required for outflow-tract septation and branchial-arch artery remodeling. Proc. Natl Acad. Sci. USA 101, 4489–4494 (2004).
Kruithof, B. P., Duim, S. N., Moerkamp, A. T. & Goumans, M. J. TGFbeta and BMP signaling in cardiac cushion formation: lessons from mice and chicken. Differentiation 84, 89–102 (2012).
Molin, D. G. et al. Expression patterns of Tgfbeta1-3 associate with myocardialisation of the outflow tract and the development of the epicardium and the fibrous heart skeleton. Dev. Dyn. 227, 431–444 (2003).
Akhurst, R. J., Lehnert, S. A., Faissner, A. & Duffie, E. TGF beta in murine morphogenetic processes: the early embryo and cardiogenesis. Development 108, 645–656 (1990).
Azhar, M. et al. Transforming growth factor beta in cardiovascular development and function. Cytokine Growth Factor Rev. 14, 391–407 (2003).
Dickson, M. C. et al. Defective haematopoiesis and vasculogenesis in transforming growth factor-beta 1 knock out mice. Development 121, 1845–1854 (1995).
Letterio, J. J. et al. Maternal rescue of transforming growth factor-beta 1 null mice. Science 264, 1936–1938 (1994).
Kaartinen, V. et al. Abnormal lung development and cleft palate in mice lacking TGF-beta 3 indicates defects of epithelial-mesenchymal interaction. Nat. Genet. 11, 415–421 (1995).
Bartram, U. et al. Double-outlet right ventricle and overriding tricuspid valve reflect disturbances of looping, myocardialization, endocardial cushion differentiation, and apoptosis in TGF-beta(2)-knockout mice. Circulation 103, 2745–2752 (2001).
Sanford, L. P. et al. TGFbeta2 knockout mice have multiple developmental defects that are non-overlapping with other TGFbeta knockout phenotypes. Development 124, 2659–2670 (1997).
Mercado-Pimentel, M. E., Hubbard, A. D. & Runyan, R. B. Endoglin and Alk5 regulate epithelial-mesenchymal transformation during cardiac valve formation. Dev. Biol. 304, 420–432 (2007).
Townsend, T. A., Wrana, J. L., Davis, G. E. & Barnett, J. V. Transforming growth factor-beta-stimulated endocardial cell transformation is dependent on Par6c regulation of RhoA. J. Biol. Chem. 283, 13834–13841 (2008).
Sridurongrit, S., Larsson, J., Schwartz, R., Ruiz-Lozano, P. & Kaartinen, V. Signaling via the Tgf-beta type I receptor Alk5 in heart development. Dev. Biol. 322, 208–218 (2008).
Boyer, A. S. & Runyan, R. B. TGFbeta Type III and TGFbeta Type II receptors have distinct activities during epithelial-mesenchymal cell transformation in the embryonic heart. Dev. Dyn. 221, 454–459 (2001).
Brown, C. B., Boyer, A. S., Runyan, R. B. & Barnett, J. V. Requirement of type III TGF-beta receptor for endocardial cell transformation in the heart. Science 283, 2080–2082 (1999).
Kim, R. Y., Robertson, E. J. & Solloway, M. J. Bmp6 and Bmp7 are required for cushion formation and septation in the developing mouse heart. Dev. Biol. 235, 449–466 (2001).
Somi, S., Buffing, A. A., Moorman, A. F. & Van Den Hoff, M. J. Dynamic patterns of expression of BMP isoforms 2, 4, 5, 6, and 7 during chicken heart development. Anat. Rec. A Discov. Mol. Cell Evol. Biol. 279, 636–651 (2004).
Ma, L., Lu, M. F., Schwartz, R. J. & Martin, J. F. Bmp2 is essential for cardiac cushion epithelial-mesenchymal transition and myocardial patterning. Development 132, 5601–5611 (2005).
McCulley, D. J., Kang, J. O., Martin, J. F. & Black, B. L. BMP4 is required in the anterior heart field and its derivatives for endocardial cushion remodeling, outflow tract septation, and semilunar valve development. Dev. Dyn. 237, 3200–3209 (2008).
Protze, S. I. et al. Sinoatrial node cardiomyocytes derived from human pluripotent cells function as a biological pacemaker. Nat. Biotechnol. 35, 56–68 (2017).
Compton, L. A., Potash, D. A., Mundell, N. A. & Barnett, J. V. Transforming growth factor-beta induces loss of epithelial character and smooth muscle cell differentiation in epicardial cells. Dev. Dyn. 235, 82–93 (2006).
Compton, L. A., Potash, D. A., Brown, C. B. & Barnett, J. V. Coronary vessel development is dependent on the type III transforming growth factor beta receptor. Circ. Res. 101, 784–791 (2007).
Sanchez, N. S. & Barnett, J. V. TGFbeta and BMP-2 regulate epicardial cell invasion via TGFbetaR3 activation of the Par6/Smurf1/RhoA pathway. Cell Signal 24, 539–548 (2012).
Austin, A. F., Compton, L. A., Love, J. D., Brown, C. B. & Barnett, J. V. Primary and immortalized mouse epicardial cells undergo differentiation in response to TGFbeta. Dev. Dyn. 237, 366–376 (2008).
Moerkamp, A. T. et al. Human fetal and adult epicardial-derived cells: a novel model to study their activation. Stem Cell Res. Ther. 7, 174 (2016).
Lockhart, M. M. et al. Alk3-mediated Bmp signaling controls the contribution of epicardially derived cells to the tissues of the atrioventricular junction. Dev. Biol. 396, 8–18 (2014).
Velecela, V. et al. Epicardial cell shape and maturation are regulated by Wt1 via transcriptional control of Bmp4. Development 146 (2019).
McCulley, D. J. & Black, B. L. Transcription factor pathways and congenital heart disease. Curr. Top. Dev. Biol. 100, 253–277 (2012).
Kelly, R. G. The heart field transcriptional landscape at single-cell resolution. Dev. Cell 58, 257–266 (2023).
Barth, J. L. et al. Jarid2 is among a set of genes differentially regulated by Nkx2.5 during outflow tract morphogenesis. Dev. Dyn. 239, 2024–2033 (2010).
Yamagishi, H. et al. The combinatorial activities of Nkx2.5 and dHAND are essential for cardiac ventricle formation. Dev. Biol. 239, 190–203 (2001).
Vincentz, J. W., Barnes, R. M., Firulli, B. A., Conway, S. J. & Firulli, A. B. Cooperative interaction of Nkx2.5 and Mef2c transcription factors during heart development. Dev. Dyn. 237, 3809–3819 (2008).
Sepulveda, J. L., Vlahopoulos, S., Iyer, D., Belaguli, N. & Schwartz, R. J. Combinatorial expression of GATA4, Nkx2-5, and serum response factor directs early cardiac gene activity. J. Biol. Chem. 277, 25775–25782 (2002).
Saba, R. et al. Endocardium differentiation through Sox17 expression in endocardium precursor cells regulates heart development in mice. Sci. Rep. 9, 11953 (2019).
Jia, G. et al. Single-cell RNA-seq and ATAC-seq analysis of cardiac progenitor cell transition states and lineage settlement. Nat. Commun. 9, 4877 (2018).
Mommersteeg, M. T. et al. Pitx2c and Nkx2-5 are required for the formation and identity of the pulmonary myocardium. Circ. Res. 101, 902–909 (2007).
Choquet, C., Kelly, R. G. & Miquerol, L. Nkx2-5 defines distinct scaffold and recruitment phases during formation of the murine cardiac Purkinje fiber network. Nat. Commun. 11, 5300 (2020).
Moskowitz, I. P. et al. A molecular pathway including Id2, Tbx5, and Nkx2-5 required for cardiac conduction system development. Cell 129, 1365–1376 (2007).
Benson, D. W. Genetic origins of pediatric heart disease. Pediatr. Cardiol. 31, 422–429 (2010).
Molkentin, J. D., Lin, Q., Duncan, S. A. & Olson, E. N. Requirement of the transcription factor GATA4 for heart tube formation and ventral morphogenesis. Genes Dev. 11, 1061–1072 (1997).
Kuo, C. T. et al. GATA4 transcription factor is required for ventral morphogenesis and heart tube formation. Genes Dev. 11, 1048–1060 (1997).
Pu, W. T., Ishiwata, T., Juraszek, A. L., Ma, Q. & Izumo, S. GATA4 is a dosage-sensitive regulator of cardiac morphogenesis. Dev. Biol. 275, 235–244 (2004).
Okubo, A. et al. A novel GATA4 mutation completely segregated with atrial septal defect in a large Japanese family. J. Med. Genet. 41, e97 (2004).
Sarkozy, A. et al. Spectrum of atrial septal defects associated with mutations of NKX2.5 and GATA4 transcription factors. J. Med. Genet. 42, e16 (2005).
McFadden, D. G. et al. A GATA-dependent right ventricular enhancer controls dHAND transcription in the developing heart. Development 127, 5331–5341 (2000).
Zeisberg, E. M. et al. Morphogenesis of the right ventricle requires myocardial expression of Gata4. J. Clin. Investig. 115, 1522–1531 (2005).
Maitra, M. et al. Interaction of Gata4 and Gata6 with Tbx5 is critical for normal cardiac development. Dev. Biol. 326, 368–377 (2009).
Dodou, E., Verzi, M. P., Anderson, J. P., Xu, S. M. & Black, B. L. Mef2c is a direct transcriptional target of ISL1 and GATA factors in the anterior heart field during mouse embryonic development. Development 131, 3931–3942 (2004).
Garg, V. et al. GATA4 mutations cause human congenital heart defects and reveal an interaction with TBX5. Nature 424, 443–447 (2003).
Black, B. L. Transcriptional pathways in second heart field development. Semin. Cell Dev. Biol. 18, 67–76 (2007).
Sun, Y. et al. Islet 1 is expressed in distinct cardiovascular lineages, including pacemaker and coronary vascular cells. Dev. Biol. 304, 286–296 (2007).
Roux, M. & Zaffran, S. Hox genes in cardiovascular development and diseases. J. Dev. Biol. 4, 14 (2016).
Wang, Z. et al. A new ISL1 loss-of-function mutation predisposes to congenital double outlet right ventricle. Int. Heart J. 60, 1113–1122 (2019).
Liu, C., Liu, W., Lu, M. F., Brown, N. A. & Martin, J. F. Regulation of left-right asymmetry by thresholds of Pitx2c activity. Development 128, 2039–2048 (2001).
Ai, D. et al. Pitx2 regulates cardiac left-right asymmetry by patterning second cardiac lineage-derived myocardium. Dev. Biol. 296, 437–449 (2006).
Kitamura, K. et al. Mouse Pitx2 deficiency leads to anomalies of the ventral body wall, heart, extra- and periocular mesoderm and right pulmonary isomerism. Development 126, 5749–5758 (1999).
Hill, M. C. et al. A cellular atlas of Pitx2-dependent cardiac development. Development 146, dev180398 (2019).
Ammirabile, G. et al. Pitx2 confers left morphological, molecular, and functional identity to the sinus venosus myocardium. Cardiovasc. Res. 93, 291–301 (2012).
Wang, J. et al. Pitx2 prevents susceptibility to atrial arrhythmias by inhibiting left-sided pacemaker specification. Proc. Natl. Acad. Sci. USA 107, 9753–9758 (2010).
Cui, M. et al. Transcription factor NFYa controls cardiomyocyte metabolism and proliferation during mouse fetal heart development. Dev. Cell 58, 2867–2880 e2867 (2023).
Barnes, R. M. & Firulli, A. B. A twist of insight - the role of Twist-family bHLH factors in development. Int. J. Dev. Biol. 53, 909–924 (2009).
Barnes, R. M., Firulli, B. A., Conway, S. J., Vincentz, J. W. & Firulli, A. B. Analysis of the Hand1 cell lineage reveals novel contributions to cardiovascular, neural crest, extra-embryonic, and lateral mesoderm derivatives. Dev. Dyn. 239, 3086–3097 (2010).
VanDusen, N. J. et al. Loss of Hand2 in a population of Periostin lineage cells results in pronounced bradycardia and neonatal death. Dev. Biol. 388, 149–158 (2014).
Tsuchihashi, T. et al. Hand2 function in second heart field progenitors is essential for cardiogenesis. Dev. Biol. 351, 62–69 (2011).
Firulli, A. B., McFadden, D. G., Lin, Q., Srivastava, D. & Olson, E. N. Heart and extra-embryonic mesodermal defects in mouse embryos lacking the bHLH transcription factor Hand1. Nat. Genet. 18, 266–270 (1998).
McFadden, D. G. et al. The Hand1 and Hand2 transcription factors regulate expansion of the embryonic cardiac ventricles in a gene dosage-dependent manner. Development 132, 189–201 (2005).
Vincentz, J. W., Toolan, K. P., Zhang, W. & Firulli, A. B. Hand factor ablation causes defective left ventricular chamber development and compromised adult cardiac function. PLoS Genet. 13, e1006922 (2017).
Togi, K. et al. Essential role of Hand2 in interventricular septum formation and trabeculation during cardiac development. Biochem. Biophys. Res. Commun. 343, 144–151 (2006).
de Soysa, T. Y. et al. Single-cell analysis of cardiogenesis reveals basis for organ-level developmental defects. Nature 572, 120–124 (2019).
VanDusen, N. J. et al. Hand2 is an essential regulator for two Notch-dependent functions within the embryonic endocardium. Cell Rep. 9, 2071–2083 (2014).
Barnes, R. M. et al. Hand2 loss-of-function in Hand1-expressing cells reveals distinct roles in epicardial and coronary vessel development. Circ. Res. 108, 940–949 (2011).
Basson, C. T. et al. The clinical and genetic spectrum of the Holt-Oram syndrome (heart-hand syndrome). N. Engl. J. Med. 330, 885–891 (1994).
Bruneau, B. G. et al. A murine model of Holt-Oram syndrome defines roles of the T-box transcription factor Tbx5 in cardiogenesis and disease. Cell 106, 709–721 (2001).
Ghosh, T. K. et al. Physical interaction between TBX5 and MEF2C is required for early heart development. Mol. Cell Biol. 29, 2205–2218 (2009).
Xie, L. et al. Tbx5-hedgehog molecular networks are essential in the second heart field for atrial septation. Dev. Cell 23, 280–291 (2012).
Takeuchi, J. K. et al. Tbx5 specifies the left/right ventricles and ventricular septum position during cardiogenesis. Development 130, 5953–5964 (2003).
Koshiba-Takeuchi, K. et al. Reptilian heart development and the molecular basis of cardiac chamber evolution. Nature 461, 95–98 (2009).
Kathiriya, I. S. et al. Modeling human TBX5 haploinsufficiency predicts regulatory networks for congenital heart disease. Dev. Cell 56, 292–309 e299 (2021).
Verzi, M. P., McCulley, D. J., De Val, S., Dodou, E. & Black, B. L. The right ventricle, outflow tract, and ventricular septum comprise a restricted expression domain within the secondary/anterior heart field. Dev. Biol. 287, 134–145 (2005).
Devine, W. P., Wythe, J. D., George, M., Koshiba-Takeuchi, K. & Bruneau, B. G. Early patterning and specification of cardiac progenitors in gastrulating mesoderm. Elife 3, e03848 (2014).
Nomaru, H. et al. Single cell multi-omic analysis identifies a Tbx1-dependent multilineage primed population in murine cardiopharyngeal mesoderm. Nat. Commun. 12, 6645 (2021).
Chen, L. et al. Transcriptional control in cardiac progenitors: Tbx1 interacts with the BAF chromatin remodeling complex and regulates Wnt5a. PLoS Genet. 8, e1002571 (2012).
Scambler, P. J. 22q11 deletion syndrome: a role for TBX1 in pharyngeal and cardiovascular development. Pediatr. Cardiol. 31, 378–390 (2010).
Xu, H. et al. Tbx1 has a dual role in the morphogenesis of the cardiac outflow tract. Development 131, 3217–3227 (2004).
Francou, A., Saint-Michel, E., Mesbah, K. & Kelly, R. G. TBX1 regulates epithelial polarity and dynamic basal filopodia in the second heart field. Development 141, 4320–4331 (2014).
Aanhaanen, W. T. et al. The Tbx2+ primary myocardium of the atrioventricular canal forms the atrioventricular node and the base of the left ventricle. Circ. Res. 104, 1267–1274 (2009).
Singh, R. et al. Tbx2 and Tbx3 induce atrioventricular myocardial development and endocardial cushion formation. Cell Mol. Life Sci. 69, 1377–1389 (2012).
Duim, S. N., Goumans, M. J. & Kruithof, B. P. T. In Wilms Tumor (ed van den Heuvel-Eibrink, M. M.) (2016).
Acharya, A. et al. The bHLH transcription factor Tcf21 is required for lineage-specific EMT of cardiac fibroblast progenitors. Development 139, 2139–2149 (2012).
Jing, X. et al. Hypoxia induced the differentiation of Tbx18-positive epicardial cells to CoSMCs. Sci. Rep. 6, 30468 (2016).
Long, X., Wei, J., Fang, Q., Yuan, X. & Du, J. Single-cell RNA sequencing reveals the transcriptional heterogeneity of Tbx18-positive cardiac cells during heart development. Funct. Integr. Genom. 24, 18 (2024).
Mommersteeg, M. T. et al. The sinus venosus progenitors separate and diversify from the first and second heart fields early in development. Cardiovasc. Res. 87, 92–101 (2010).
Takeuchi, J. K. et al. Tbx20 dose-dependently regulates transcription factor networks required for mouse heart and motoneuron development. Development 132, 2463–2474 (2005).
Stennard, F. A. et al. Murine T-box transcription factor Tbx20 acts as a repressor during heart development, and is essential for adult heart integrity, function and adaptation. Development 132, 2451–2462 (2005).
Cai, X. et al. Myocardial Tbx20 regulates early atrioventricular canal formation and endocardial epithelial-mesenchymal transition via Bmp2. Dev. Biol. 360, 381–390 (2011).
van Amerongen, R. & Nusse, R. Towards an integrated view of Wnt signaling in development. Development 136, 3205–3214 (2009).
Nusse, R. et al. A new nomenclature for int-1 and related genes: the Wnt gene family. Cell 64, 231 (1991).
Wang, J., Sinha, T. & Wynshaw-Boris, A. Wnt signaling in mammalian development: lessons from mouse genetics. Cold Spring Harb. Perspect. Biol. 4 (2012).
Gordon, M. D. & Nusse, R. Wnt signaling: multiple pathways, multiple receptors, and multiple transcription factors. J. Biol. Chem. 281, 22429–22433 (2006).
Huelsken, J. & Behrens, J. The Wnt signalling pathway. J. Cell Sci. 115, 3977–3978 (2002).
Meganathan, K., Sotiriadou, I., Natarajan, K., Hescheler, J. & Sachinidis, A. Signaling molecules, transcription growth factors and other regulators revealed from in-vivo and in-vitro models for the regulation of cardiac development. Int. J. Cardiol. 183, 117–128 (2015).
Yamanaka, H. et al. JNK functions in the non-canonical Wnt pathway to regulate convergent extension movements in vertebrates. EMBO Rep. 3, 69–75 (2002).
Habas, R., Dawid, I. B. & He, X. Coactivation of Rac and Rho by Wnt/Frizzled signaling is required for vertebrate gastrulation. Genes Dev. 17, 295–309 (2003).
Slusarski, D. C. & Pelegri, F. Calcium signaling in vertebrate embryonic patterning and morphogenesis. Dev. Biol. 307, 1–13 (2007).
Kelly, G. M., Greenstein, P., Erezyilmaz, D. F. & Moon, R. T. Zebrafish wnt8 and wnt8b share a common activity but are involved in distinct developmental pathways. Development 121, 1787–1799 (1995).
Szeto, D. P. & Kimelman, D. Combinatorial gene regulation by Bmp and Wnt in zebrafish posterior mesoderm formation. Development 131, 3751–3760 (2004).
Yue, Q., Wagstaff, L., Yang, X., Weijer, C. & Munsterberg, A. Wnt3a-mediated chemorepulsion controls movement patterns of cardiac progenitors and requires RhoA function. Development 135, 1029–1037 (2008).
Ai, D. et al. Canonical Wnt signaling functions in second heart field to promote right ventricular growth. Proc. Natl. Acad. Sci. USA 104, 9319–9324 (2007).
Cohen, E. D. et al. Wnt/beta-catenin signaling promotes expansion of Isl-1-positive cardiac progenitor cells through regulation of FGF signaling. J. Clin. Investig. 117, 1794–1804 (2007).
Lin, L. et al. Beta-catenin directly regulates Islet1 expression in cardiovascular progenitors and is required for multiple aspects of cardiogenesis. Proc. Natl. Acad. Sci. USA 104, 9313–9318 (2007).
Qyang, Y. et al. The renewal and differentiation of Isl1+ cardiovascular progenitors are controlled by a Wnt/beta-catenin pathway. Cell Stem Cell 1, 165–179 (2007).
Tian, Y. et al. Characterization and in vivo pharmacological rescue of a Wnt2-Gata6 pathway required for cardiac inflow tract development. Dev. Cell 18, 275–287 (2010).
Zhou, W. et al. Modulation of morphogenesis by noncanonical Wnt signaling requires ATF/CREB family-mediated transcriptional activation of TGFbeta2. Nat. Genet. 39, 1225–1234 (2007).
Nagy, I. I. et al. Wnt-11 signalling controls ventricular myocardium development by patterning N-cadherin and beta-catenin expression. Cardiovasc. Res. 85, 100–109 (2010).
Cohen, E. D., Miller, M. F., Wang, Z., Moon, R. T. & Morrisey, E. E. Wnt5a and Wnt11 are essential for second heart field progenitor development. Development 139, 1931–1940 (2012).
Li, D. et al. Spatial regulation of cell cohesion by Wnt5a during second heart field progenitor deployment. Dev. Biol. 412, 18–31 (2016).
Sinha, T. et al. Loss of Wnt5a disrupts second heart field cell deployment and may contribute to OFT malformations in DiGeorge syndrome. Hum. Mol. Genet. 24, 1704–1716 (2015).
Li, D., Angermeier, A. & Wang, J. Planar cell polarity signaling regulates polarized second heart field morphogenesis to promote both arterial and venous pole septation. Development 146, dev181719 (2019).
Touma, M. et al. Wnt11 regulates cardiac chamber development and disease during perinatal maturation. JCI Insight 2, e94904 (2017).
Sahara, M. et al. Population and single-cell analysis of human cardiogenesis reveals unique LGR5 ventricular progenitors in embryonic outflow tract. Dev. Cell 48, 475–490.e477 (2019).
Naito, A. T. et al. Developmental stage-specific biphasic roles of Wnt/beta-catenin signaling in cardiomyogenesis and hematopoiesis. Proc. Natl. Acad. Sci. USA 103, 19812–19817 (2006).
Ueno, S. et al. Biphasic role for Wnt/beta-catenin signaling in cardiac specification in zebrafish and embryonic stem cells. Proc. Natl. Acad. Sci. USA 104, 9685–9690 (2007).
Marvin, M. J., Di Rocco, G., Gardiner, A., Bush, S. M. & Lassar, A. B. Inhibition of Wnt activity induces heart formation from posterior mesoderm. Genes Dev. 15, 316–327 (2001).
Mazzotta, S. et al. Distinctive roles of canonical and noncanonical Wnt signaling in human embryonic cardiomyocyte development. Stem Cell Rep. 7, 764–776 (2016).
Lian, X. et al. Robust cardiomyocyte differentiation from human pluripotent stem cells via temporal modulation of canonical Wnt signaling. Proc. Natl. Acad. Sci. USA 109, E1848–E1857 (2012).
Fonoudi, H. et al. A universal and robust integrated platform for the scalable production of human cardiomyocytes from pluripotent stem cells. Stem Cells Transl. Med. 4, 1482–1494 (2015).
Zhang, J. et al. Functional cardiomyocytes derived from human induced pluripotent stem cells. Circ. Res. 104, e30–e41 (2009).
Rowton, M., Guzzetta, A., Rydeen, A. B. & Moskowitz, I. P. Control of cardiomyocyte differentiation timing by intercellular signaling pathways. Semin. Cell Dev. Biol. 118, 94–106 (2021).
Ren, J. et al. Canonical Wnt5b signaling directs outlying Nkx2.5+ mesoderm into pacemaker cardiomyocytes. Dev. Cell 50, 729–743.e725 (2019).
Alfieri, C. M., Cheek, J., Chakraborty, S. & Yutzey, K. E. Wnt signaling in heart valve development and osteogenic gene induction. Dev. Biol. 338, 127–135 (2010).
Wang, Y. et al. Myocardial beta-Catenin-BMP2 signaling promotes mesenchymal cell proliferation during endocardial cushion formation. J. Mol. Cell Cardiol. 123, 150–158 (2018).
Hurlstone, A. F. et al. The Wnt/beta-catenin pathway regulates cardiac valve formation. Nature 425, 633–637 (2003).
Cai, X. et al. Tbx20 acts upstream of Wnt signaling to regulate endocardial cushion formation and valve remodeling during mouse cardiogenesis. Development 140, 3176–3187 (2013).
Merki, E. et al. Epicardial retinoid X receptor alpha is required for myocardial growth and coronary artery formation. Proc. Natl. Acad. Sci. USA 102, 18455–18460 (2005).
von Gise, A. et al. WT1 regulates epicardial epithelial to mesenchymal transition through beta-catenin and retinoic acid signaling pathways. Dev. Biol. 356, 421–431 (2011).
Zamora, M., Manner, J. & Ruiz-Lozano, P. Epicardium-derived progenitor cells require beta-catenin for coronary artery formation. Proc. Natl. Acad. Sci. USA 104, 18109–18114 (2007).
Rudat, C., Norden, J., Taketo, M. M. & Kispert, A. Epicardial function of canonical Wnt-, Hedgehog-, Fgfr1/2-, and Pdgfra-signalling. Cardiovasc. Res. 100, 411–421 (2013).
Wu, M. et al. Epicardial spindle orientation controls cell entry into the myocardium. Dev. Cell 19, 114–125 (2010).
Niederreither, K. & Dolle, P. Retinoic acid in development: towards an integrated view. Nat. Rev. Genet. 9, 541–553 (2008).
Wiesinger, A., Boink, G. J. J., Christoffels, V. M. & Devalla, H. D. Retinoic acid signaling in heart development: application in the differentiation of cardiovascular lineages from human pluripotent stem cells. Stem Cell Rep. 16, 2589–2606 (2021).
Hochgreb, T. et al. A caudorostral wave of RALDH2 conveys anteroposterior information to the cardiac field. Development 130, 5363–5374 (2003).
del Monte, G. et al. Differential Notch signaling in the epicardium is required for cardiac inflow development and coronary vessel morphogenesis. Circ. Res. 108, 824–836 (2011).
Brade, T. et al. Retinoic acid stimulates myocardial expansion by induction of hepatic erythropoietin which activates epicardial Igf2. Development 138, 139–148 (2011).
Moss, J. B. et al. Dynamic patterns of retinoic acid synthesis and response in the developing mammalian heart. Dev. Biol. 199, 55–71 (1998).
Waxman, J. S., Keegan, B. R., Roberts, R. W., Poss, K. D. & Yelon, D. Hoxb5b acts downstream of retinoic acid signaling in the forelimb field to restrict heart field potential in zebrafish. Dev. Cell 15, 923–934 (2008).
Keegan, B. R., Feldman, J. L., Begemann, G., Ingham, P. W. & Yelon, D. Retinoic acid signaling restricts the cardiac progenitor pool. Science 307, 247–249 (2005).
Ryckebusch, L. et al. Retinoic acid deficiency alters second heart field formation. Proc. Natl. Acad. Sci. USA 105, 2913–2918 (2008).
Sirbu, I. O., Zhao, X. & Duester, G. Retinoic acid controls heart anteroposterior patterning by down-regulating Isl1 through the Fgf8 pathway. Dev. Dyn. 237, 1627–1635 (2008).
Witzel, H. R. et al. The LIM protein Ajuba restricts the second heart field progenitor pool by regulating Isl1 activity. Dev. Cell 23, 58–70 (2012).
De Bono, C. et al. T-box genes and retinoic acid signaling regulate the segregation of arterial and venous pole progenitor cells in the murine second heart field. Hum. Mol. Genet. 27, 3747–3760 (2018).
Gruber, P. J. et al. RXR alpha deficiency confers genetic susceptibility for aortic sac, conotruncal, atrioventricular cushion, and ventricular muscle defects in mice. J. Clin. Investig. 98, 1332–1343 (1996).
Niederreither, K. et al. Embryonic retinoic acid synthesis is essential for heart morphogenesis in the mouse. Development 128, 1019–1031 (2001).
Duong, T. B., Holowiecki, A. & Waxman, J. S. Retinoic acid signaling restricts the size of the first heart field within the anterior lateral plate mesoderm. Dev. Biol. 473, 119–129 (2021).
Taylor, I. M., Wiley, M. J. & Agur, A. Retinoic acid-induced heart malformations in the hamster. Teratology 21, 193–197 (1980).
Rydeen, A. B. & Waxman, J. S. Cyp26 enzymes facilitate second heart field progenitor addition and maintenance of ventricular integrity. PLoS Biol. 14, e2000504 (2016).
Sakabe, M., Kokubo, H., Nakajima, Y. & Saga, Y. Ectopic retinoic acid signaling affects outflow tract cushion development through suppression of the myocardial Tbx2-Tgfbeta2 pathway. Development 139, 385–395 (2012).
Lin, S. C. et al. Endogenous retinoic acid regulates cardiac progenitor differentiation. Proc. Natl. Acad. Sci. USA 107, 9234–9239 (2010).
Guadix, J. A. et al. Wt1 controls retinoic acid signalling in embryonic epicardium through transcriptional activation of Raldh2. Development 138, 1093–1097 (2011).
Wang, S. et al. Alterations in retinoic acid signaling affect the development of the mouse coronary vasculature. Dev. Dyn. 247, 976–991 (2018).
Wang, S. et al. Retinoic acid signaling promotes the cytoskeletal rearrangement of embryonic epicardial cells. FASEB J. 32, 3765–3781 (2018).
Azambuja, A. P. et al. Retinoic acid and VEGF delay smooth muscle relative to endothelial differentiation to coordinate inner and outer coronary vessel wall morphogenesis. Circ. Res. 107, 204–216 (2010).
Wobus, A. M. et al. Retinoic acid accelerates embryonic stem cell-derived cardiac differentiation and enhances development of ventricular cardiomyocytes. J. Mol. Cell Cardiol. 29, 1525–1539 (1997).
Zhang, Q. et al. Direct differentiation of atrial and ventricular myocytes from human embryonic stem cells by alternating retinoid signals. Cell Res. 21, 579–587 (2011).
Devalla, H. D. et al. Atrial-like cardiomyocytes from human pluripotent stem cells are a robust preclinical model for assessing atrial-selective pharmacology. EMBO Mol. Med. 7, 394–410 (2015).
Quaranta, R. et al. Revised roles of ISL1 in a hES cell-based model of human heart chamber specification. Elife 7, e31706 (2018).
Tan, J. J. et al. Human iPS-derived pre-epicardial cells direct cardiomyocyte aggregation expansion and organization in vitro. Nat. Commun. 12, 4997 (2021).
Guadix, J. A. et al. Human pluripotent stem cell differentiation into functional epicardial progenitor cells. Stem Cell Rep. 9, 1754–1764 (2017).
Bray, S. J. Notch signalling: a simple pathway becomes complex. Nat. Rev. Mol. Cell Biol. 7, 678–689 (2006).
Itoh, M. et al. Mind bomb is a ubiquitin ligase that is essential for efficient activation of Notch signaling by Delta. Dev. Cell 4, 67–82 (2003).
Fischer, A. & Gessler, M. Delta-Notch-and then? Protein interactions and proposed modes of repression by Hes and Hey bHLH factors. Nucleic Acids Res. 35, 4583–4596 (2007).
McDaniell, R. et al. NOTCH2 mutations cause Alagille syndrome, a heterogeneous disorder of the notch signaling pathway. Am. J. Hum. Genet. 79, 169–173 (2006).
McElhinney, D. B. et al. Analysis of cardiovascular phenotype and genotype-phenotype correlation in individuals with a JAG1 mutation and/or Alagille syndrome. Circulation 106, 2567–2574 (2002).
Eldadah, Z. A. et al. Familial Tetralogy of Fallot caused by mutation in the jagged1 gene. Hum. Mol. Genet. 10, 163–169 (2001).
Nakajima, M., Moriizumi, E., Koseki, H. & Shirasawa, T. Presenilin 1 is essential for cardiac morphogenesis. Dev. Dyn. 230, 795–799 (2004).
McCright, B., Lozier, J. & Gridley, T. A mouse model of Alagille syndrome: Notch2 as a genetic modifier of Jag1 haploinsufficiency. Development 129, 1075–1082 (2002).
Foffa, I. et al. Sequencing of NOTCH1, GATA5, TGFBR1 and TGFBR2 genes in familial cases of bicuspid aortic valve. BMC Med. Genet. 14, 44 (2013).
McBride, K. L. et al. NOTCH1 mutations in individuals with left ventricular outflow tract malformations reduce ligand-induced signaling. Hum. Mol. Genet. 17, 2886–2893 (2008).
Kerstjens-Frederikse, W. S. et al. Cardiovascular malformations caused by NOTCH1 mutations do not keep left: data on 428 probands with left-sided CHD and their families. Genet Med. 18, 914–923 (2016).
Rones, M. S., McLaughlin, K. A., Raffin, M. & Mercola, M. Serrate and Notch specify cell fates in the heart field by suppressing cardiomyogenesis. Development 127, 3865–3876 (2000).
Contakos, S. P., Gaydos, C. M., Pfeil, E. C. & McLaughlin, K. A. Subdividing the embryo: a role for Notch signaling during germ layer patterning in Xenopus laevis. Dev. Biol. 288, 294–307 (2005).
Miazga, C. M. & McLaughlin, K. A. Coordinating the timing of cardiac precursor development during gastrulation: a new role for Notch signaling. Dev. Biol. 333, 285–296 (2009).
Nemir, M., Croquelois, A., Pedrazzini, T. & Radtke, F. Induction of cardiogenesis in embryonic stem cells via downregulation of Notch1 signaling. Circ. Res. 98, 1471–1478 (2006).
Schroeder, T. et al. Activated Notch1 alters differentiation of embryonic stem cells into mesodermal cell lineages at multiple stages of development. Mech. Dev. 123, 570–579 (2006).
Lowell, S., Benchoua, A., Heavey, B. & Smith, A. G. Notch promotes neural lineage entry by pluripotent embryonic stem cells. PLoS Biol. 4, e121 (2006).
Miyamoto, M. et al. Noncanonical Notch signals have opposing roles during cardiac development. Biochem. Biophys. Res. Commun. 577, 12–16 (2021).
Watanabe, Y. et al. Activation of Notch1 signaling in cardiogenic mesoderm induces abnormal heart morphogenesis in mouse. Development 133, 1625–1634 (2006).
Kwon, C. et al. A regulatory pathway involving Notch1/beta-catenin/Isl1 determines cardiac progenitor cell fate. Nat. Cell Biol. 11, 951–957 (2009).
Klaus, A. et al. Wnt/beta-catenin and Bmp signals control distinct sets of transcription factors in cardiac progenitor cells. Proc. Natl. Acad. Sci. USA 109, 10921–10926 (2012).
High, F. A. et al. Murine Jagged1/Notch signaling in the second heart field orchestrates Fgf8 expression and tissue-tissue interactions during outflow tract development. J. Clin. Investig. 119, 1986–1996 (2009).
Timmerman, L. A. et al. Notch promotes epithelial-mesenchymal transition during cardiac development and oncogenic transformation. Genes Dev. 18, 99–115 (2004).
Del Monte, G., Grego-Bessa, J., Gonzalez-Rajal, A., Bolos, V. & De La Pompa, J. L. Monitoring Notch1 activity in development: evidence for a feedback regulatory loop. Dev. Dyn. 236, 2594–2614 (2007).
MacGrogan, D. et al. Sequential ligand-dependent notch signaling activation regulates valve primordium formation and morphogenesis. Circ. Res. 118, 1480–1497 (2016).
Luna-Zurita, L. et al. Integration of a Notch-dependent mesenchymal gene program and Bmp2-driven cell invasiveness regulates murine cardiac valve formation. J. Clin. Investig. 120, 3493–3507 (2010).
Kokubo, H., Tomita-Miyagawa, S., Hamada, Y. & Saga, Y. Hesr1 and Hesr2 regulate atrioventricular boundary formation in the developing heart through the repression of Tbx2. Development 134, 747–755 (2007).
Wang, Y. et al. Endocardial to myocardial notch-wnt-bmp axis regulates early heart valve development. PLoS One 8, e60244 (2013).
Garg, V. et al. Mutations in NOTCH1 cause aortic valve disease. Nature 437, 270–274 (2005).
Wang, Y. et al. Notch-Tnf signalling is required for development and homeostasis of arterial valves. Eur. Heart J. 38, 675–686 (2017).
Venkatesh, D. A. et al. Cardiovascular and hematopoietic defects associated with Notch1 activation in embryonic Tie2-expressing populations. Circ. Res. 103, 423–431 (2008).
Beis, D. et al. Genetic and cellular analyses of zebrafish atrioventricular cushion and valve development. Development 132, 4193–4204 (2005).
Rentschler, S. et al. Notch signaling regulates murine atrioventricular conduction and the formation of accessory pathways. J. Clin. Investig. 121, 525–533 (2011).
Grego-Bessa, J. et al. Notch signaling is essential for ventricular chamber development. Dev. Cell 12, 415–429 (2007).
D’Amato, G. et al. Sequential Notch activation regulates ventricular chamber development. Nat. Cell Biol. 18, 7–20 (2016).
Grieskamp, T., Rudat, C., Ludtke, T. H., Norden, J. & Kispert, A. Notch signaling regulates smooth muscle differentiation of epicardium-derived cells. Circ. Res. 108, 813–823 (2011).
Travisano, S. I. et al. Coronary arterial development is regulated by a Dll4-Jag1-EphrinB2 signaling cascade. Elife 8, e49977 (2019).
Pathi, S. et al. Comparative biological responses to human Sonic, Indian, and Desert hedgehog. Mech. Dev. 106, 107–117 (2001).
Nusslein-Volhard, C. & Wieschaus, E. Mutations affecting segment number and polarity in Drosophila. Nature 287, 795–801 (1980).
Wilson, C. W. & Chuang, P. T. Mechanism and evolution of cytosolic Hedgehog signal transduction. Development 137, 2079–2094 (2010).
Thomas, N. A., Koudijs, M., van Eeden, F. J., Joyner, A. L. & Yelon, D. Hedgehog signaling plays a cell-autonomous role in maximizing cardiac developmental potential. Development 135, 3789–3799 (2008).
Marti, E., Takada, R., Bumcrot, D. A., Sasaki, H. & McMahon, A. P. Distribution of Sonic hedgehog peptides in the developing chick and mouse embryo. Development 121, 2537–2547 (1995).
Washington Smoak, I. et al. Sonic hedgehog is required for cardiac outflow tract and neural crest cell development. Dev. Biol. 283, 357–372 (2005).
Goddeeris, M. M., Schwartz, R., Klingensmith, J. & Meyers, E. N. Independent requirements for Hedgehog signaling by both the anterior heart field and neural crest cells for outflow tract development. Development 134, 1593–1604 (2007).
Briggs, L. E. et al. Wnt/beta-catenin and sonic hedgehog pathways interact in the regulation of the development of the dorsal mesenchymal protrusion. Dev. Dyn. 245, 103–113 (2016).
Goddeeris, M. M. et al. Intracardiac septation requires hedgehog-dependent cellular contributions from outside the heart. Development 135, 1887–1895 (2008).
Zhang, C. et al. Hedgehog signalling controls sinoatrial node development and atrioventricular cushion formation. Open Biol. 11, 210020 (2021).
Rash, J. E., Shay, J. W. & Biesele, J. J. Cilia in cardiac differentiation. J. Ultrastruct. Res. 29, 470–484 (1969).
Djenoune, L., Berg, K., Brueckner, M. & Yuan, S. A change of heart: new roles for cilia in cardiac development and disease. Nat. Rev. Cardiol. 19, 211–227 (2022).
Sun, S., Fisher, R. L., Bowser, S. S., Pentecost, B. T. & Sui, H. Three-dimensional architecture of epithelial primary cilia. Proc. Natl. Acad. Sci. USA 116, 9370–9379 (2019).
Fitzsimons, L. A., Brewer, V. L. & Tucker, K. L. Hedgehog morphogens act as growth factors critical to pre- and postnatal cardiac development and maturation: how primary cilia mediate their signal transduction. Cells 11, 1879 (2022).
Delling, M., DeCaen, P. G., Doerner, J. F., Febvay, S. & Clapham, D. E. Primary cilia are specialized calcium signalling organelles. Nature 504, 311–314 (2013).
DeCaen, P. G., Delling, M., Vien, T. N. & Clapham, D. E. Direct recording and molecular identification of the calcium channel of primary cilia. Nature 504, 315–318 (2013).
Lienkamp, S., Ganner, A. & Walz, G. Inversin, Wnt signaling and primary cilia. Differentiation 83, S49–S55 (2012).
Clement, C. A. et al. TGF-beta signaling is associated with endocytosis at the pocket region of the primary cilium. Cell Rep. 3, 1806–1814 (2013).
Ezratty, E. J. et al. A role for the primary cilium in Notch signaling and epidermal differentiation during skin development. Cell 145, 1129–1141 (2011).
Diguet, N., Le Garrec, J. F., Lucchesi, T. & Meilhac, S. M. Imaging and analyzing primary cilia in cardiac cells. Methods Cell Biol. 127, 55–73 (2015).
Toomer, K. A. et al. Primary cilia defects causing mitral valve prolapse. Sci Transl Med 11, eaax0290 (2019).
Norris, D. P. Cilia, calcium and the basis of left-right asymmetry. BMC Biol. 10, 102 (2012).
McGrath, J., Somlo, S., Makova, S., Tian, X. & Brueckner, M. Two populations of node monocilia initiate left-right asymmetry in the mouse. Cell 114, 61–73 (2003).
Nonaka, S. et al. Randomization of left-right asymmetry due to loss of nodal cilia generating leftward flow of extraembryonic fluid in mice lacking KIF3B motor protein. Cell 95, 829–837 (1998).
Kennedy, M. P. et al. Congenital heart disease and other heterotaxic defects in a large cohort of patients with primary ciliary dyskinesia. Circulation 115, 2814–2821 (2007).
Lin, A. E. et al. Laterality defects in the national birth defects prevention study (1998-2007): birth prevalence and descriptive epidemiology. Am. J. Med. Genet A 164A, 2581–2591 (2014).
Nakhleh, N. et al. High prevalence of respiratory ciliary dysfunction in congenital heart disease patients with heterotaxy. Circulation 125, 2232–2242 (2012).
Slough, J., Cooney, L. & Brueckner, M. Monocilia in the embryonic mouse heart suggest a direct role for cilia in cardiac morphogenesis. Dev. Dyn. 237, 2304–2314 (2008).
Wu, G. et al. Cardiac defects and renal failure in mice with targeted mutations in Pkd2. Nat. Genet. 24, 75–78 (2000).
Boulter, C. et al. Cardiovascular, skeletal, and renal defects in mice with a targeted disruption of the Pkd1 gene. Proc. Natl. Acad. Sci. USA 98, 12174–12179 (2001).
Willaredt, M. A., Gorgas, K., Gardner, H. A. & Tucker, K. L. Multiple essential roles for primary cilia in heart development. Cilia 1, 23 (2012).
Clement, C. A. et al. The primary cilium coordinates early cardiogenesis and hedgehog signaling in cardiomyocyte differentiation. J. Cell Sci. 122, 3070–3082 (2009).
Klena, N. T., Gibbs, B. C. & Lo, C. W. Cilia and Ciliopathies in congenital heart disease. Cold Spring Harb. Perspect. Biol. 9 (2017).
Burnicka-Turek, O. et al. Cilia gene mutations cause atrioventricular septal defects by multiple mechanisms. Hum. Mol. Genet. 25, 3011–3028 (2016).
Egorova, A. D. et al. Lack of primary cilia primes shear-induced endothelial-to-mesenchymal transition. Circ. Res. 108, 1093–1101 (2011).
Fulmer, D. et al. Desert hedgehog-primary cilia cross talk shapes mitral valve tissue by organizing smooth muscle actin. Dev. Biol. 463, 26–38 (2020).
Toomer, K. A. et al. A role for primary cilia in aortic valve development and disease. Dev. Dyn. 246, 625–634 (2017).
de Boer, B. A., van den Berg, G., de Boer, P. A., Moorman, A. F. & Ruijter, J. M. Growth of the developing mouse heart: an interactive qualitative and quantitative 3D atlas. Dev. Biol. 368, 203–213 (2012).
Dong, J. et al. Elucidation of a universal size-control mechanism in Drosophila and mammals. Cell 130, 1120–1133 (2007).
Zhou, Q., Li, L., Zhao, B. & Guan, K. L. The hippo pathway in heart development, regeneration, and diseases. Circ. Res. 116, 1431–1447 (2015).
Mia, M. M. & Singh, M. K. The Hippo signaling pathway in cardiac development and diseases. Front. Cell Dev. Biol. 7, 211 (2019).
Murphy, S. A. et al. PGC1/PPAR drive cardiomyocyte maturation at single cell level via YAP1 and SF3B2. Nat. Commun. 12, 1648 (2021).
He, L. et al. Zebrafish Foxc1a controls ventricular chamber maturation by directly regulating wwtr1 and nkx2.5 expression. J. Genet. Genom. 49, 559–568 (2022).
Hsu, H. T., Estaras, C., Huang, L. & Jones, K. A. Specifying the anterior primitive streak by modulating YAP1 levels in human pluripotent stem cells. Stem Cell Rep. 11, 1357–1364 (2018).
Li, P. et al. Functional role of Mst1/Mst2 in embryonic stem cell differentiation. PLoS One 8, e79867 (2013).
Fukui, H. et al. S1P-Yap1 signaling regulates endoderm formation required for cardiac precursor cell migration in zebrafish. Dev. Cell 31, 128–136 (2014).
Miesfeld, J. B. & Link, B. A. Establishment of transgenic lines to monitor and manipulate Yap/Taz-Tead activity in zebrafish reveals both evolutionarily conserved and divergent functions of the Hippo pathway. Mech. Dev. 133, 177–188 (2014).
Fukui, H. et al. Hippo signaling determines the number of venous pole cells that originate from the anterior lateral plate mesoderm in zebrafish. Elife 7, e29106 (2018).
Francou, A., De Bono, C. & Kelly, R. G. Epithelial tension in the second heart field promotes mouse heart tube elongation. Nat. Commun. 8, 14770 (2017).
Pan, D. The hippo signaling pathway in development and cancer. Dev. Cell 19, 491–505 (2010).
Heallen, T. et al. Hippo pathway inhibits Wnt signaling to restrain cardiomyocyte proliferation and heart size. Science 332, 458–461 (2011).
von Gise, A. et al. YAP1, the nuclear target of Hippo signaling, stimulates heart growth through cardiomyocyte proliferation but not hypertrophy. Proc. Natl. Acad. Sci. USA 109, 2394–2399 (2012).
Xin, M. et al. Regulation of insulin-like growth factor signaling by Yap governs cardiomyocyte proliferation and embryonic heart size. Sci. Signal 4, ra70 (2011).
Lai, J. K. H. et al. The Hippo pathway effector Wwtr1 regulates cardiac wall maturation in zebrafish. Development 145, dev159210 (2018).
Zhang, H. et al. Yap1 is required for endothelial to mesenchymal transition of the atrioventricular cushion. J. Biol. Chem. 289, 18681–18692 (2014).
Artap, S. et al. Endocardial Hippo signaling regulates myocardial growth and cardiogenesis. Dev. Biol. 440, 22–30 (2018).
Bornhorst, D. et al. Biomechanical signaling within the developing zebrafish heart attunes endocardial growth to myocardial chamber dimensions. Nat. Commun. 10, 4113 (2019).
Singh, A. et al. Hippo signaling mediators Yap and Taz are required in the epicardium for coronary vasculature development. Cell Rep. 15, 1384–1393 (2016).
Xiao, Y. et al. Hippo signaling plays an essential role in cell state transitions during cardiac fibroblast development. Dev. Cell 45, 153–169 e156 (2018).
Sifrim, A. et al. Distinct genetic architectures for syndromic and nonsyndromic congenital heart defects identified by exome sequencing. Nat. Genet. 48, 1060–1065 (2016).
Zaidi, S. et al. De novo mutations in histone-modifying genes in congenital heart disease. Nature 498, 220–223 (2013).
Moore-Morris, T., van Vliet, P. P., Andelfinger, G. & Puceat, M. Role of epigenetics in cardiac development and congenital diseases. Physiol. Rev. 98, 2453–2475 (2018).
Lozano-Velasco, E. et al. Post-transcriptional regulation of molecular determinants during cardiogenesis. Int. J. Mol. Sci. 23, 2839 (2022).
Serra-Juhe, C. et al. DNA methylation abnormalities in congenital heart disease. Epigenetics 10, 167–177 (2015).
Grunert, M. et al. Comparative DNA methylation and gene expression analysis identifies novel genes for structural congenital heart diseases. Cardiovasc. Res. 112, 464–477 (2016).
Gilsbach, R. et al. Dynamic DNA methylation orchestrates cardiomyocyte development, maturation and disease. Nat. Commun. 5, 5288 (2014).
Gilsbach, R. et al. Distinct epigenetic programs regulate cardiac myocyte development and disease in the human heart in vivo. Nat. Commun. 9, 391 (2018).
Greco, C. M. et al. DNA hydroxymethylation controls cardiomyocyte gene expression in development and hypertrophy. Nat. Commun. 7, 12418 (2016).
Alexander, J. M. et al. Brg1 modulates enhancer activation in mesoderm lineage commitment. Development 142, 1418–1430 (2015).
Hang, C. T. et al. Chromatin regulation by Brg1 underlies heart muscle development and disease. Nature 466, 62–67 (2010).
Stankunas, K. et al. Endocardial Brg1 represses ADAMTS1 to maintain the microenvironment for myocardial morphogenesis. Dev. Cell 14, 298–311 (2008).
Vieira, J. M. et al. BRG1-SWI/SNF-dependent regulation of the Wt1 transcriptional landscape mediates epicardial activity during heart development and disease. Nat. Commun. 8, 16034 (2017).
Akerberg, B. N., Sarangam, M. L. & Stankunas, K. Endocardial Brg1 disruption illustrates the developmental origins of semilunar valve disease. Dev. Biol. 407, 158–172 (2015).
Lickert, H. et al. Baf60c is essential for function of BAF chromatin remodelling complexes in heart development. Nature 432, 107–112 (2004).
Sun, X. et al. Cardiac-enriched BAF chromatin-remodeling complex subunit Baf60c regulates gene expression programs essential for heart development and function. Biol. Open 7 (2018).
Hota, S. K. et al. Dynamic BAF chromatin remodeling complex subunit inclusion promotes temporally distinct gene expression programs in cardiogenesis. Development 146 (2019).
Wang, Z. et al. Polybromo protein BAF180 functions in mammalian cardiac chamber maturation. Genes Dev. 18, 3106–3116 (2004).
Lee, S., Lee, J. W. & Lee, S. K. UTX, a histone H3-lysine 27 demethylase, acts as a critical switch to activate the cardiac developmental program. Dev. Cell 22, 25–37 (2012).
Cattaneo, P. et al. DOT1L-mediated H3K79me2 modification critically regulates gene expression during cardiomyocyte differentiation. Cell Death Differ. 23, 555–564 (2016).
He, A. et al. PRC2 directly methylates GATA4 and represses its transcriptional activity. Genes Dev. 26, 37–42 (2012).
Morey, L. et al. Polycomb regulates mesoderm cell fate-specification in embryonic stem cells through activation and repression mechanisms. Cell Stem Cell 17, 300–315 (2015).
Chrispijn, N. D. et al. Loss of the Polycomb group protein Rnf2 results in derepression of tbx-transcription factors and defects in embryonic and cardiac development. Sci. Rep. 9, 4327 (2019).
Shirai, M. et al. The Polycomb-group gene Rae28 sustains Nkx2.5/Csx expression and is essential for cardiac morphogenesis. J. Clin. Investig. 110, 177–184 (2002).
Chen, L. et al. Conditional ablation of Ezh2 in murine hearts reveals its essential roles in endocardial cushion formation, cardiomyocyte proliferation and survival. PLoS One 7, e31005 (2012).
He, A. et al. Polycomb repressive complex 2 regulates normal development of the mouse heart. Circ. Res. 110, 406–415 (2012).
Ai, S. et al. Divergent requirements for EZH1 in heart development versus regeneration. Circ. Res. 121, 106–112 (2017).
Montgomery, R. L. et al. Histone deacetylases 1 and 2 redundantly regulate cardiac morphogenesis, growth, and contractility. Genes Dev. 21, 1790–1802 (2007).
Chang, S. et al. Histone deacetylases 5 and 9 govern responsiveness of the heart to a subset of stress signals and play redundant roles in heart development. Mol. Cell Biol. 24, 8467–8476 (2004).
Wilczewski, C. M. et al. CHD4 and the NuRD complex directly control cardiac sarcomere formation. Proc. Natl. Acad. Sci. USA 115, 6727–6732 (2018).
Garnatz, A. S. et al. FOG-2-mediated recruitment of the NuRD complex regulates cardiomyocyte proliferation during heart development. Dev. Biol. 395, 50–61 (2014).
Waldron, L. et al. The cardiac TBX5 interactome reveals a chromatin remodeling network essential for cardiac septation. Dev. Cell 36, 262–275 (2016).
Kaltenbrun, E. et al. A Gro/TLE-NuRD corepressor complex facilitates Tbx20-dependent transcriptional repression. J. Proteome Res. 12, 5395–5409 (2013).
Park, C. Y. et al. skNAC, a Smyd1-interacting transcription factor, is involved in cardiac development and skeletal muscle growth and regeneration. Proc. Natl. Acad. Sci. USA 107, 20750–20755 (2010).
Nimura, K. et al. A histone H3 lysine 36 trimethyltransferase links Nkx2-5 to Wolf-Hirschhorn syndrome. Nature 460, 287–291 (2009).
Ang, S. Y. et al. KMT2D regulates specific programs in heart development via histone H3 lysine 4 di-methylation. Development 143, 810–821 (2016).
Rotini, A., Martinez-Sarra, E., Pozzo, E. & Sampaolesi, M. Interactions between microRNAs and long non-coding RNAs in cardiac development and repair. Pharm. Res. 127, 58–66 (2018).
Devaux, Y. et al. Long noncoding RNAs in cardiac development and ageing. Nat. Rev. Cardiol. 12, 415–425 (2015).
Memczak, S. et al. Circular RNAs are a large class of animal RNAs with regulatory potency. Nature 495, 333–338 (2013).
Pozzo, E., Chai, Y. C. & Sampaolesi, M. Comprehensive overview of non-coding RNAs in cardiac development. Adv. Exp. Med. Biol. 1229, 197–211 (2020).
Xu, T., Wu, J., Han, P., Zhao, Z. & Song, X. Circular RNA expression profiles and features in human tissues: a study using RNA-seq data. BMC Genom. 18, 680 (2017).
Tan, W. L. et al. A landscape of circular RNA expression in the human heart. Cardiovasc Res. 113, 298–309 (2017).
Guo, X. et al. A Linc1405/eomes complex promotes cardiac mesoderm specification and cardiogenesis. Cell Stem Cell 22, 893–908 e896 (2018).
Li, Y. et al. Dynamic organization of lncRNA and circular RNA regulators collectively controlled cardiac differentiation in humans. EBioMedicine 24, 137–146 (2017).
Grote, P. et al. The tissue-specific lncRNA Fendrr is an essential regulator of heart and body wall development in the mouse. Dev. Cell 24, 206–214 (2013).
Klattenhoff, C. A. et al. Braveheart, a long noncoding RNA required for cardiovascular lineage commitment. Cell 152, 570–583 (2013).
Ounzain, S. et al. CARMEN, a human super enhancer-associated long noncoding RNA controlling cardiac specification, differentiation and homeostasis. J. Mol. Cell Cardiol. 89, 98–112 (2015).
Hazra, R. et al. Platr4 is an early embryonic lncRNA that exerts its function downstream on cardiogenic mesodermal lineage commitment. Dev. Cell 57, 2450–2468.e2457 (2022).
Kurian, L. et al. Identification of novel long noncoding RNAs underlying vertebrate cardiovascular development. Circulation 131, 1278–1290 (2015).
Ounzain, S. et al. Genome-wide profiling of the cardiac transcriptome after myocardial infarction identifies novel heart-specific long non-coding RNAs. Eur. Heart J. 36, 353–368a (2015).
Kim, N. J. et al. Spatiotemporal expression of long noncoding RNA Moshe modulates heart cell lineage commitment. RNA Biol. 18, 640–654 (2021).
Kay, M., Soltani, B. M., Aghdaei, F. H., Ansari, H. & Baharvand, H. Hsa-miR-335 regulates cardiac mesoderm and progenitor cell differentiation. Stem Cell Res. Ther. 10, 191 (2019).
Ivey, K. N. et al. MicroRNA regulation of cell lineages in mouse and human embryonic stem cells. Cell Stem Cell 2, 219–229 (2008).
Lu, T. Y. et al. Overexpression of microRNA-1 promotes cardiomyocyte commitment from human cardiovascular progenitors via suppressing WNT and FGF signaling pathways. J. Mol. Cell Cardiol. 63, 146–154 (2013).
Shen, X. et al. miR-322/-503 cluster is expressed in the earliest cardiac progenitor cells and drives cardiomyocyte specification. Proc. Natl. Acad. Sci. USA 113, 9551–9556 (2016).
Wang, J. et al. Bmp signaling regulates myocardial differentiation from cardiac progenitors through a MicroRNA-mediated mechanism. Dev. Cell 19, 903–912 (2010).
Ventura, A. et al. Targeted deletion reveals essential and overlapping functions of the miR-17 through 92 family of miRNA clusters. Cell 132, 875–886 (2008).
Zhao, Y., Samal, E. & Srivastava, D. Serum response factor regulates a muscle-specific microRNA that targets Hand2 during cardiogenesis. Nature 436, 214–220 (2005).
Zhao, Y. et al. Dysregulation of cardiogenesis, cardiac conduction, and cell cycle in mice lacking miRNA-1-2. Cell 129, 303–317 (2007).
Heidersbach, A. et al. microRNA-1 regulates sarcomere formation and suppresses smooth muscle gene expression in the mammalian heart. Elife 2, e01323 (2013).
Liu, N. et al. microRNA-133a regulates cardiomyocyte proliferation and suppresses smooth muscle gene expression in the heart. Genes Dev. 22, 3242–3254 (2008).
Wystub, K., Besser, J., Bachmann, A., Boettger, T. & Braun, T. miR-1/133a clusters cooperatively specify the cardiomyogenic lineage by adjustment of myocardin levels during embryonic heart development. PLoS Genet. 9, e1003793 (2013).
Garcia-Padilla, C. et al. Inhibition of RhoA and Cdc42 by miR-133a modulates retinoic acid signalling during early development of posterior cardiac tube segment. Int. J. Mol. Sci. 23 (2022).
Wilson, K. D. et al. Dynamic microRNA expression programs during cardiac differentiation of human embryonic stem cells: role for miR-499. Circ. Cardiovasc. Genet. 3, 426–435 (2010).
Sluijter, J. P. et al. MicroRNA-1 and -499 regulate differentiation and proliferation in human-derived cardiomyocyte progenitor cells. Arterioscler. Thromb. Vasc. Biol. 30, 859–868 (2010).
Deacon, D. C. et al. The miR-143-adducin3 pathway is essential for cardiac chamber morphogenesis. Development 137, 1887–1896 (2010).
Miyasaka, K. Y. et al. Heartbeat regulates cardiogenesis by suppressing retinoic acid signaling via expression of miR-143. Mech. Dev. 128, 18–28 (2011).
Morton, S. U. et al. microRNA-138 modulates cardiac patterning during embryonic development. Proc. Natl. Acad. Sci. USA 105, 17830–17835 (2008).
Kolpa, H. J. et al. miR-21 represses Pdcd4 during cardiac valvulogenesis. Development 140, 2172–2180 (2013).
Fish, J. E. et al. A Slit/miR-218/Robo regulatory loop is required during heart tube formation in zebrafish. Development 138, 1409–1419 (2011).
Xu, T., Liu, N., Shao, Y., Huang, Y. & Zhu, D. MiR-218 regulated cardiomyocyte differentiation and migration in mouse embryonic stem cells by targeting PDGFRalpha. J. Cell Biochem. 120, 4355–4365 (2019).
Chinchilla, A. et al. MicroRNA profiling during mouse ventricular maturation: a role for miR-27 modulating Mef2c expression. Cardiovasc. Res. 89, 98–108 (2011).
Tian, Y. et al. A microRNA-Hippo pathway that promotes cardiomyocyte proliferation and cardiac regeneration in mice. Sci. Transl. Med. 7, 279ra238 (2015).
Saxena, A. & Tabin, C. J. miRNA-processing enzyme Dicer is necessary for cardiac outflow tract alignment and chamber septation. Proc. Natl. Acad. Sci. USA 107, 87–91 (2010).
Diez-Cunado, M. et al. miRNAs that induce human cardiomyocyte proliferation converge on the hippo pathway. Cell Rep. 23, 2168–2174 (2018).
Xie, Y. et al. MircroRNA-10b promotes human embryonic stem cell-derived cardiomyocyte proliferation via novel target gene LATS1. Mol. Ther. Nucleic Acids 19, 437–445 (2020).
Xu, F. et al. MicroRNA-302d promotes the proliferation of human pluripotent stem cell-derived cardiomyocytes by inhibiting LATS2 in the Hippo pathway. Clin. Sci. 133, 1387–1399 (2019).
Anderson, K. M. et al. Transcription of the non-coding RNA upperhand controls Hand2 expression and heart development. Nature 539, 433–436 (2016).
Han, X. et al. The lncRNA Hand2os1/Uph locus orchestrates heart development through regulation of precise expression of Hand2. Development 146 (2019).
Zhang, Q., Cheng, Z., Yu, Z., Zhu, C. & Qian, L. Role of lncRNA uc.457 in the differentiation and maturation of cardiomyocytes. Mol. Med. Rep. 19, 4927–4934 (2019).
Li, H. et al. The role of a novel long noncoding RNA TUC40- in cardiomyocyte induction and maturation in P19 cells. Am. J. Med. Sci. 354, 608–616 (2017).
Liu, H. et al. Effects of long non-coding RNA uc.245 on cardiomyocyte-like differentiation in P19 cells via FOG2. Gene 694, 83–92 (2019).
Song, G. et al. LncRNA-uc.167 influences cell proliferation, apoptosis and differentiation of P19 cells by regulating Mef2c. Gene 590, 97–108 (2016).
Wu, R., Xue, P., Wan, Y., Wang, S. & Gu, M. LncRNA-uc.40 silence promotes P19 embryonic cells differentiation to cardiomyocyte via the PBX1 gene. Vitr. Cell Dev. Biol. Anim. 54, 600–609 (2018).
Kay, M. et al. The conserved long non-coding RNA CARMA regulates cardiomyocyte differentiation. Cardiovasc. Res. 118, 2339–2353 (2022).
Wilson, K. D. et al. Endogenous retrovirus-derived lncRNA BANCR promotes cardiomyocyte migration in humans and non-human primates. Dev. Cell 54, 694–709.e699 (2020).
Bowers, S. L., Banerjee, I. & Baudino, T. A. The extracellular matrix: at the center of it all. J. Mol. Cell Cardiol. 48, 474–482 (2010).
Lockhart, M., Wirrig, E., Phelps, A. & Wessels, A. Extracellular matrix and heart development. Birth Defects Res. A Clin. Mol. Teratol. 91, 535–550 (2011).
Chang, C. W., Dalgliesh, A. J., Lopez, J. E. & Griffiths, L. G. Cardiac extracellular matrix proteomics: challenges, techniques, and clinical implications. Proteom. Clin. Appl. 10, 39–50 (2016).
Linask, K. K. & Lash, J. W. A role for fibronectin in the migration of avian precardiac cells. I. Dose-dependent effects of fibronectin antibody. Dev. Biol. 129, 315–323 (1988).
Trinh, L. A. & Stainier, D. Y. Fibronectin regulates epithelial organization during myocardial migration in zebrafish. Dev. Cell 6, 371–382 (2004).
George, E. L., Georges-Labouesse, E. N., Patel-King, R. S., Rayburn, H. & Hynes, R. O. Defects in mesoderm, neural tube and vascular development in mouse embryos lacking fibronectin. Development 119, 1079–1091 (1993).
Georges-Labouesse, E. N., George, E. L., Rayburn, H. & Hynes, R. O. Mesodermal development in mouse embryos mutant for fibronectin. Dev. Dyn. 207, 145–156 (1996).
Patra, C. et al. Nephronectin regulates atrioventricular canal differentiation via Bmp4-Has2 signaling in zebrafish. Development 138, 4499–4509 (2011).
Baldwin, H. S., Lloyd, T. R. & Solursh, M. Hyaluronate degradation affects ventricular function of the early postlooped embryonic rat heart in situ. Circ. Res. 74, 244–252 (1994).
Walsh, E. C. & Stainier, D. Y. UDP-glucose dehydrogenase required for cardiac valve formation in zebrafish. Science 293, 1670–1673 (2001).
Camenisch, T. D., Schroeder, J. A., Bradley, J., Klewer, S. E. & McDonald, J. A. Heart-valve mesenchyme formation is dependent on hyaluronan-augmented activation of ErbB2-ErbB3 receptors. Nat. Med. 8, 850–855 (2002).
Camenisch, T. D. et al. Disruption of hyaluronan synthase-2 abrogates normal cardiac morphogenesis and hyaluronan-mediated transformation of epithelium to mesenchyme. J. Clin. Investig. 106, 349–360 (2000).
Norris, R. A. et al. Periostin promotes a fibroblastic lineage pathway in atrioventricular valve progenitor cells. Dev. Dyn. 238, 1052–1063 (2009).
Inai, K., Burnside, J. L., Hoffman, S., Toole, B. P. & Sugi, Y. BMP-2 induces versican and hyaluronan that contribute to post-EMT AV cushion cell migration. PLoS One 8, e77593 (2013).
Snider, P. et al. Periostin is required for maturation and extracellular matrix stabilization of noncardiomyocyte lineages of the heart. Circ. Res. 102, 752–760 (2008).
Norris, R. A. et al. Periostin regulates atrioventricular valve maturation. Dev. Biol. 316, 200–213 (2008).
Hatano, S. et al. Versican/PG-M is essential for ventricular septal formation subsequent to cardiac atrioventricular cushion development. Glycobiology 22, 1268–1277 (2012).
Kern, C. B. et al. Reduced versican cleavage due to Adamts9 haploinsufficiency is associated with cardiac and aortic anomalies. Matrix Biol. 29, 304–316 (2010).
Ieda, M. et al. Cardiac fibroblasts regulate myocardial proliferation through beta1 integrin signaling. Dev. Cell 16, 233–244 (2009).
Lee, J. et al. In vitro generation of functional murine heart organoids via FGF4 and extracellular matrix. Nat. Commun. 11, 4283 (2020).
Barbosky, L. et al. Apoptosis in the developing mouse heart. Dev. Dyn. 235, 2592–2602 (2006).
Sugishita, Y., Leifer, D. W., Agani, F., Watanabe, M. & Fisher, S. A. Hypoxia-responsive signaling regulates the apoptosis-dependent remodeling of the embryonic avian cardiac outflow tract. Dev. Biol. 273, 285–296 (2004).
Yue, X. & Tomanek, R. J. Stimulation of coronary vasculogenesis/angiogenesis by hypoxia in cultured embryonic hearts. Dev. Dyn. 216, 28–36 (1999).
Lee, Y. M. et al. Determination of hypoxic region by hypoxia marker in developing mouse embryos in vivo: a possible signal for vessel development. Dev. Dyn. 220, 175–186 (2001).
Compernolle, V. et al. Cardia bifida, defective heart development and abnormal neural crest migration in embryos lacking hypoxia-inducible factor-1alpha. Cardiovasc. Res. 60, 569–579 (2003).
Maltepe, E., Schmidt, J. V., Baunoch, D., Bradfield, C. A. & Simon, M. C. Abnormal angiogenesis and responses to glucose and oxygen deprivation in mice lacking the protein ARNT. Nature 386, 403–407 (1997).
Guimaraes-Camboa, N. et al. HIF1alpha represses cell stress pathways to allow proliferation of hypoxic fetal cardiomyocytes. Dev. Cell 33, 507–521 (2015).
O’Reilly, V. C. et al. Gene-environment interaction demonstrates the vulnerability of the embryonic heart. Dev. Biol. 391, 99–110 (2014).
Ream, M., Ray, A. M., Chandra, R. & Chikaraishi, D. M. Early fetal hypoxia leads to growth restriction and myocardial thinning. Am. J. Physiol. Regul. Integr. Comp. Physiol. 295, R583–R595 (2008).
Sharma, S. K. et al. Impact of hypoxia on early chick embryo growth and cardiovascular function. Pediatr. Res. 59, 116–120 (2006).
Gao, Y. et al. Multi-omics integration reveals short and long-term effects of gestational hypoxia on the heart development. Cells 8, 1608 (2019).
Kalisch-Smith, J. I., Ved, N. & Sparrow, D. B. Environmental risk factors for congenital heart disease. Cold Spring Harb. Perspect. Biol. 12, a037234 (2020).
Morita, Y. & Tohyama, S. Metabolic regulation of cardiac differentiation and maturation in pluripotent stem cells: a lesson from heart development. JMA J. 3, 193–200 (2020).
Knutson, A. K., Williams, A. L., Boisvert, W. A. & Shohet, R. V. HIF in the heart: development, metabolism, ischemia, and atherosclerosis. J. Clin. Investig. 131 e137557 (2021).
Lopaschuk, G. D. & Jaswal, J. S. Energy metabolic phenotype of the cardiomyocyte during development, differentiation, and postnatal maturation. J. Cardiovasc. Pharm. 56, 130–140 (2010).
Edwards, W. et al. Quantitative proteomic profiling identifies global protein network dynamics in murine embryonic heart development. Dev. Cell 58, 1087–1105.e1084 (2023).
Wickramasinghe, N. M. et al. PPARdelta activation induces metabolic and contractile maturation of human pluripotent stem cell-derived cardiomyocytes. Cell Stem Cell 29, 559–576.e557 (2022).
Menendez-Montes, I. et al. Activation of amino acid metabolic program in cardiac HIF1-alpha-deficient mice. iScience 24, 102124 (2021).
Zhang, D. et al. Metabolic regulation of gene expression by histone lactylation. Nature 574, 575–580 (2019).
Miao, Z., Zhao, X. & Liu, X. Hypoxia induced beta-catenin lactylation promotes the cell proliferation and stemness of colorectal cancer through the wnt signaling pathway. Exp. Cell Res. 422, 113439 (2023).
Zhou, J. et al. GPR37 promotes colorectal cancer liver metastases by enhancing the glycolysis and histone lactylation via Hippo pathway. Oncogene 42, 3319–3330 (2023).
Lin, X. et al. Augmentation of scleral glycolysis promotes myopia through histone lactylation. Cell Metab. 36, 511–525.e517 (2024).
Nakano, H. et al. Glucose inhibits cardiac muscle maturation through nucleotide biosynthesis. Elife 6, e29330 (2017).
Correia, C. et al. Distinct carbon sources affect structural and functional maturation of cardiomyocytes derived from human pluripotent stem cells. Sci. Rep. 7, 8590 (2017).
Malandraki-Miller, S. et al. Metabolic flux analyses to assess the differentiation of adult cardiac progenitors after fatty acid supplementation. Stem Cell Res. 38, 101458 (2019).
Yang, X. et al. Fatty acids enhance the maturation of cardiomyocytes derived from human pluripotent stem cells. Stem Cell Rep. 13, 657–668 (2019).
Li, X. et al. Inhibition of fatty acid oxidation enables heart regeneration in adult mice. Nature 622, 619–626 (2023).
Ramachandra, C. J. A. et al. Fatty acid metabolism driven mitochondrial bioenergetics promotes advanced developmental phenotypes in human-induced pluripotent stem cell derived cardiomyocytes. Int. J. Cardiol. 272, 288–297 (2018).
Gentillon, C. et al. Targeting HIF-1alpha in combination with PPARalpha activation and postnatal factors promotes the metabolic maturation of human-induced pluripotent stem cell-derived cardiomyocytes. J. Mol. Cell Cardiol. 132, 120–135 (2019).
Chirico, N. et al. Small molecule-mediated rapid maturation of human induced pluripotent stem cell-derived cardiomyocytes. Stem Cell Res. Ther. 13, 531 (2022).
Zhou, J. et al. mTOR supports long-term self-renewal and suppresses mesoderm and endoderm activities of human embryonic stem cells. Proc. Natl. Acad. Sci. USA 106, 7840–7845 (2009).
Jiang, M. et al. Rapamycin promotes cardiomyocyte differentiation of human induced pluripotent stem cells in a stage-dependent manner. Stem Cells Dev. 29, 1229–1239 (2020).
Meneghetti, G. et al. Zebrafish ambra1a and ambra1b Silencing Affect Heart Development. Zebrafish (2020).
Lee, E. et al. Autophagy is essential for cardiac morphogenesis during vertebrate development. Autophagy 10, 572–587 (2014).
Ding, S. et al. Non-cardiomyocytes in the heart in embryo development, health, and disease, a single-cell perspective. Front. Cell Dev. Biol. 10, 873264 (2022).
Ramos, T. A. R. et al. Single-cell transcriptional landscape of long non-coding RNAs orchestrating mouse heart development. Cell Death Dis. 14, 841 (2023).
Farah, E. N. et al. Spatially organized cellular communities form the developing human heart. Nature 627, 854–864 (2024).
Hou, X. et al. Single-cell RNA sequencing reveals the gene expression profile and cellular communication in human fetal heart development. Dev. Biol. 514, 87–98 (2024).
Du, J. et al. Single-cell and spatial heterogeneity landscapes of mature epicardial cells. J. Pharm. Anal. 13, 894–907 (2023).
Jimenez, J. & Lavine, K. J. The dynamic role of cardiac macrophages in aging and disease. Curr. Cardiol. Rep. 24, 925–933 (2022).
Jin, J., Wang, Y., Liu, Y., Chakrabarti, S. & Su, Z. Cardiac resident macrophages: spatiotemporal distribution, development, physiological functions, and their translational potential on cardiac diseases. Acta Pharm. Sin. B 14, 1483–1493 (2024).
Dick, S. A. et al. Three tissue resident macrophage subsets coexist across organs with conserved origins and life cycles. Sci. Immunol. 7, eabf7777 (2022).
Thorp, E. B. et al. CCR2(+) monocytes promote white matter injury and cognitive dysfunction after myocardial infarction. Brain Behav. Immun. 119, 818–835 (2024).
Li, R. G. et al. YAP induces a neonatal-like pro-renewal niche in the adult heart. Nat. Cardiovasc. Res. 3, 283–300 (2024).
Zhang, X. et al. Development of a CD163-targeted PET radiotracer that images resident macrophages in atherosclerosis. J. Nucl. Med. 65, 775–780 (2024).
Ma, P. et al. Expansion of pathogenic cardiac macrophages in immune checkpoint inhibitor myocarditis. Circulation 149, 48–66 (2024).
Holt, M. et al. Dissecting and visualizing the functional diversity of cardiac macrophages. Circ. Res. 134, 1791–1807 (2024).
Chakarov, S. et al. Two distinct interstitial macrophage populations coexist across tissues in specific subtissular niches. Science 363, eaau0964 (2019).
Xu, N., Gonzalez, B. A. & Yutzey, K. E. Macrophage lineages in heart development and regeneration. Curr. Top. Dev. Biol. 156, 1–17 (2024).
Shigeta, A. et al. Endocardially derived macrophages are essential for valvular remodeling. Dev. Cell 48, 617–630.e613 (2019).
Leid, J. et al. Primitive embryonic macrophages are required for coronary development and maturation. Circ. Res. 118, 1498–1511 (2016).
Gula, G. et al. Potential functions of embryonic cardiac macrophages in angiogenesis, lymphangiogenesis and extracellular matrix remodeling. Histochem. Cell Biol. 155, 117–132 (2021).
Cahill, T. J. et al. Tissue-resident macrophages regulate lymphatic vessel growth and patterning in the developing heart. Development 148, dev194563 (2021).
Landau, S. et al. Primitive macrophages enable long-term vascularization of human heart-on-a-chip platforms. Cell Stem Cell 31, 1222–1238.e1210 (2024).
Hamidzada, H. et al. Primitive macrophages induce sarcomeric maturation and functional enhancement of developing human cardiac microtissues via efferocytic pathways. Nat. Cardiovasc. Res. 3, 567–593 (2024).
Vaughan, C. J. & Basson, C. T. Molecular determinants of atrial and ventricular septal defects and patent ductus arteriosus. Am. J. Med. Genet. 97, 304–309 (2000).
Rauch, A. et al. Assessment of association between variants and haplotypes of the remaining TBX1 gene and manifestations of congenital heart defects in 22q11.2 deletion patients. J. Med. Genet. 41, e40 (2004).
Al-Qattan, M. M. & Abou Al-Shaar, H. Molecular basis of the clinical features of Holt-Oram syndrome resulting from missense and extended protein mutations of the TBX5 gene as well as TBX5 intragenic duplications. Gene 560, 129–136 (2015).
Kloesel, B., DiNardo, J. A. & Body, S. C. Cardiac embryology and molecular mechanisms of congenital heart disease: a primer for anesthesiologists. Anesth. Analg. 123, 551–569 (2016).
Hill, M. C. et al. Integrated multi-omic characterization of congenital heart disease. Nature 608, 181–191 (2022).
Minette, M. S. & Sahn, D. J. Ventricular septal defects. Circulation 114, 2190–2197 (2006).
Geva, T., Martins, J. D. & Wald, R. M. Atrial septal defects. Lancet 383, 1921–1932 (2014).
Richards, A. A. & Garg, V. Genetics of congenital heart disease. Curr. Cardiol. Rev. 6, 91–97 (2010).
Khositseth, A., Tocharoentanaphol, C., Khowsathit, P. & Ruangdaraganon, N. Chromosome 22q11 deletions in patients with conotruncal heart defects. Pediatr. Cardiol. 26, 570–573 (2005).
Ziolkowska, L. et al. Chromosome 22q11.2 microdeletion in children with conotruncal heart defects: frequency, associated cardiovascular anomalies, and outcome following cardiac surgery. Eur. J. Pediatr. 167, 1135–1140 (2008).
Obler, D., Juraszek, A. L., Smoot, L. B. & Natowicz, M. R. Double outlet right ventricle: aetiologies and associations. J. Med. Genet. 45, 481–497 (2008).
Neeb, Z., Lajiness, J. D., Bolanis, E. & Conway, S. J. Cardiac outflow tract anomalies. Wiley Interdiscip. Rev. Dev. Biol. 2, 499–530 (2013).
Kirby, M. L. & Hutson, M. R. Factors controlling cardiac neural crest cell migration. Cell Adh. Migr. 4, 609–621 (2010).
Prakash, S. K. et al. A roadmap to investigate the genetic basis of bicuspid aortic valve and its complications: insights from the International BAVCon (Bicuspid Aortic Valve Consortium). J. Am. Coll. Cardiol. 64, 832–839 (2014).
Liu, A. C., Joag, V. R. & Gotlieb, A. I. The emerging role of valve interstitial cell phenotypes in regulating heart valve pathobiology. Am. J. Pathol. 171, 1407–1418 (2007).
Rizzo, S. et al. TGF-beta1 pathway activation and adherens junction molecular pattern in nonsyndromic mitral valve prolapse. Cardiovasc. Pathol. 24, 359–367 (2015).
Attenhofer Jost, C. H., Connolly, H. M., Dearani, J. A., Edwards, W. D. & Danielson, G. K. Ebstein’s anomaly. Circulation 115, 277–285 (2007).
Postma, A. V. et al. Mutations in the sarcomere gene MYH7 in Ebstein anomaly. Circ. Cardiovasc. Genet. 4, 43–50 (2011).
Bettinelli, A. L. et al. Familial Ebstein anomaly, left ventricular hypertrabeculation, and ventricular septal defect associated with a MYH7 mutation. Am. J. Med. Genet. A 161A, 3187–3190 (2013).
Hrstka, S. C., Li, X., Nelson, T. J. & Wanek Program Genetics Pipeline, Group NOTCH1-dependent nitric oxide signaling deficiency in hypoplastic left heart syndrome revealed through patient-specific phenotypes detected in bioengineered cardiogenesis. Stem Cells 35, 1106–1119 (2017).
Liu, X. et al. The complex genetics of hypoplastic left heart syndrome. Nat. Genet. 49, 1152–1159 (2017).
Yang, C. et al. Induced pluripotent stem cell modelling of HLHS underlines the contribution of dysfunctional NOTCH signalling to impaired cardiogenesis. Hum. Mol. Genet. 26, 3031–3045 (2017).
Miao, Y. et al. Intrinsic endocardial defects contribute to hypoplastic left heart syndrome. Cell Stem Cell 27, 574–589.e578 (2020).
Datta, S., Cao, W., Skillman, M. & Wu, M. Hypoplastic left heart syndrome: signaling & molecular perspectives, and the road ahead. Int. J. Mol. Sci. 24, 15249 (2023).
Yarboro, M. T., Gopal, S. H., Su, R. L., Morgan, T. M. & Reese, J. Mouse models of patent ductus arteriosus (PDA) and their relevance for human PDA. Dev. Dyn. 251, 424–443 (2022).
Clyman, R. I. Mechanisms regulating the ductus arteriosus. Biol. Neonate 89, 330–335 (2006).
Staiculescu, M. C., Kim, J., Mecham, R. P. & Wagenseil, J. E. Mechanical behavior and matrisome gene expression in the aneurysm-prone thoracic aorta of newborn lysyl oxidase knockout mice. Am. J. Physiol. Heart Circ. Physiol. 313, H446–H456 (2017).
van der Flier, A. et al. Endothelial alpha5 and alphav integrins cooperate in remodeling of the vasculature during development. Development 137, 2439–2449 (2010).
Ito, S. et al. Fibulin-1 integrates subendothelial extracellular matrices and contributes to anatomical closure of the ductus arteriosus. Arterioscler. Thromb. Vasc. Biol. 40, 2212–2226 (2020).
Shelton, E. L. & Reese, J. A historical perspective of investigations into the mechanisms and management of patent ductus arteriosus. Semin. Perinatol. 47, 151723 (2023).
Nguyen, M. et al. The prostaglandin receptor EP4 triggers remodelling of the cardiovascular system at birth. Nature 390, 78–81 (1997).
Reese, J. et al. Coordinated regulation of fetal and maternal prostaglandins directs successful birth and postnatal adaptation in the mouse. Proc. Natl. Acad. Sci. USA 97, 9759–9764 (2000).
Roizen, J. D., Asada, M., Tong, M., Tai, H. H. & Muglia, L. J. Preterm birth without progesterone withdrawal in 15-hydroxyprostaglandin dehydrogenase hypomorphic mice. Mol. Endocrinol. 22, 105–112 (2008).
Chang, H. Y., Locker, J., Lu, R. & Schuster, V. L. Failure of postnatal ductus arteriosus closure in prostaglandin transporter-deficient mice. Circulation 121, 529–536 (2010).
Morano, I. et al. Smooth-muscle contraction without smooth-muscle myosin. Nat. Cell Biol. 2, 371–375 (2000).
Huang, J. et al. Myocardin regulates expression of contractile genes in smooth muscle cells and is required for closure of the ductus arteriosus in mice. J. Clin. Investig. 118, 515–525 (2008).
Feng, X., Krebs, L. T. & Gridley, T. Patent ductus arteriosus in mice with smooth muscle-specific Jag1 deletion. Development 137, 4191–4199 (2010).
Krebs, L. T., Norton, C. R. & Gridley, T. Notch signal reception is required in vascular smooth muscle cells for ductus arteriosus closure. Genesis 54, 86–90 (2016).
Baeten, J. T., Jackson, A. R., McHugh, K. M. & Lilly, B. Loss of Notch2 and Notch3 in vascular smooth muscle causes patent ductus arteriosus. Genesis 53, 738–748 (2015).
Mavroudis, C., Ong, C. S., Vricella, L. A. & Cameron, D. E. Historical accounts of congenital heart surgery. World J. Pediatr. Congenit. Heart Surg. 14, 626–641 (2023).
Dellborg, M. Adult congenital heart disease. Circulation 149, 1397–1399 (2024).
Baumgartner, H. et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 42, 563–645 (2021).
Ramonfaur, D., Zhang, X., Garza, A. P., Garcia-Pons, J. F. & Britton-Robles, S. C. Hypoplastic left heart syndrome: a review. Cardiol. Rev. 31, 149–154 (2023).
Birla, A. K. et al. Current state of the art in hypoplastic left heart syndrome. Front. Cardiovasc. Med. 9, 878266 (2022).
Hornik, C. P. et al. Complications after the Norwood operation: an analysis of The Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann. Thorac. Surg. 92, 1734–1740 (2011).
Iyengar, A. J. et al. The extracardiac conduit Fontan procedure in Australia and New Zealand: hypoplastic left heart syndrome predicts worse early and late outcomes. Eur. J. Cardiothorac. Surg. 46, 465–473 (2014).
Renaud, D., Scholl-Burgi, S., Karall, D. & Michel, M. Comparative metabolomics in single ventricle patients after fontan palliation: a strong case for a targeted metabolic therapy. Metabolites 13 (2023).
Ma, J. et al. Complications and management of functional single ventricle patients with Fontan circulation: from surgeon’s point of view. Front. Cardiovasc. Med. 9, 917059 (2022).
Muneuchi, J. et al. Feasibility and safety of sodium glucose cotransporter-2 inhibitors in adults with heart failure after the Fontan procedure. Case Rep. Cardiol. 2022, 5243594 (2022).
Konduri, A. et al. Experience with SGLT2 inhibitors in patients with single ventricle congenital heart disease and Fontan circulatory failure. Pediatr. Cardiol. (2023).
Sanders, E., Knecht, K. & Zakaria, D. Protein-losing enteropathy in the failing Fontan: treatment with angiotensin receptor neprilysin inhibitor. JACC Case Rep. 29, 102395 (2024).
Okolska, M. et al. Prevalence of arrhythmia in adults after Fontan operation. J. Clin. Med. 11, 1968 (2022).
Wu, J. et al. Ionic mechanisms underlying atrial electrical remodeling after a fontan-style operation in a canine model. Heart Vessels 35, 731–741 (2020).
Moore, B. M. et al. Ablation of atrial arrhythmias after the atriopulmonary Fontan procedure: mechanism of arrhythmia and outcomes. JACC Clin. Electrophysiol. 4, 1338–1346 (2018).
Kamp, A. N., Nair, K., Fish, F. A. & Khairy, P. Catheter ablation of atrial arrhythmias in patients post-Fontan. Can. J. Cardiol. 38, 1036–1047 (2022).
Ohuchi, H. et al. JCS 2022 guideline on management and re-interventional therapy in patients with congenital heart disease long-term after initial repair. Circ. J. 86, 1591–1690 (2022).
Poh, C. L. et al. Pacemakers are associated with a higher risk of late death and transplantation in the Fontan population. Int. J. Cardiol. 282, 33–37 (2019).
Kochav, J. D. et al. Effect of ventricular pacing on morbidity in adults after Fontan repair. Am. J. Cardiol. 125, 1263–1269 (2020).
Miyazaki, A. Pacemaker therapy for the optimization of Fontan circulation. Circ. J. 88, 649–651 (2024).
Rychik, J. et al. Evaluation and management of the child and adult with Fontan circulation: a scientific statement from the American Heart Association. Circulation 140, e234–e284 (2019).
Galie, N. et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Heart J. 37, 67–119 (2016).
Skoro-Sajer, N. et al. Subcutaneous treprostinil in congenital heart disease-related pulmonary arterial hypertension. Heart 104, 1195–1199 (2018).
Burkhart, H. M. et al. Regenerative therapy for hypoplastic left heart syndrome: first report of intraoperative intramyocardial injection of autologous umbilical-cord blood-derived cells. J. Thorac. Cardiovasc. Surg. 149, e35–e37 (2015).
Burkhart, H. M. et al. Autologous stem cell therapy for hypoplastic left heart syndrome: Safety and feasibility of intraoperative intramyocardial injections. J. Thorac. Cardiovasc. Surg. 158, 1614–1623 (2019).
Ishigami, S. et al. Intracoronary cardiac progenitor cells in single ventricle physiology: the PERSEUS (Cardiac Progenitor Cell Infusion to Treat Univentricular Heart Disease) randomized phase 2 trial. Circ. Res. 120, 1162–1173 (2017).
Yuan, S. M. Fetal cardiac interventions. Pediatr. Neonatol. 56, 81–87 (2015).
Halder, V. et al. Fetal cardiac intervention and fetal cardiac surgery: where are we in 21st century? Am. J. Cardiovasc. Dis. 11, 642–646 (2021).
Guseh, S. & Tworetzky, W. Transforming congenital heart disease management: advances in fetal cardiac interventions. Prenat. Diagn. 44, 733–738 (2024).
Chen, W. et al. Successful Eisenmenger syndrome-targeted drug therapy in pregnant women: a case series and literature review. BJOG 130, 923–931 (2023).
Pidaparti, M., Geddes, G. C. & Durbin, M. D. Clinical genetic and genomic testing in congenital heart disease and cardiomyopathy. J. Clin. Med. 13 (2024).
LaHaye, S. et al. Utilization of whole exome sequencing to identify causative mutations in familial congenital heart disease. Circ. Cardiovasc. Genet. 9, 320–329 (2016).
Gudapati, S., Chaudhari, K., Shrivastava, D. & Yelne, S. Advancements and applications of preimplantation genetic testing in in vitro fertilization: a comprehensive review. Cureus 16, e57357 (2024).
Arafati, A. et al. Artificial intelligence in pediatric and adult congenital cardiac MRI: an unmet clinical need. Cardiovasc. Diagn. Ther. 9, S310–S325 (2019).
Pozza, A. et al. Utility of fetal cardiac resonance imaging in prenatal clinical practice: current state of the art. Diagnostics 13, 3523 (2023).
Chessa, M. et al. Three-dimensional printing, holograms, computational modelling, and artificial intelligence for adult congenital heart disease care: an exciting future. Eur. Heart J. 43, 2672–2684 (2022).
Sachdeva, R. et al. Novel techniques in imaging congenital heart disease: JACC scientific statement. J. Am. Coll. Cardiol. 83, 63–81 (2024).
Pozza, A., Zanella, L., Castaldi, B. & Di Salvo, G. How will artificial intelligence shape the future of decision-making in congenital heart disease? J. Clin. Med. 13 (2024).
Dong, J. et al. A generic quality control framework for fetal ultrasound cardiac four-chamber planes. IEEE J. Biomed. Health Inf. 24, 931–942 (2020).
Truong, V. T. et al. Application of machine learning in screening for congenital heart diseases using fetal echocardiography. Int. J. Cardiovasc. Imaging 38, 1007–1015 (2022).
Arnaout, R. et al. An ensemble of neural networks provides expert-level prenatal detection of complex congenital heart disease. Nat. Med. 27, 882–891 (2021).
Mathur, P., Srivastava, S., Xu, X. & Mehta, J. L. Artificial intelligence, machine learning, and cardiovascular disease. Clin. Med. Insights Cardiol. 14, 1179546820927404 (2020).
Dellborg, M. et al. Adults with congenital heart disease: trends in event-free survival past middle age. Circulation 147, 930–938 (2023).
Orwat, S., Arvanitaki, A. & Diller, G. P. A new approach to modelling in adult congenital heart disease: artificial intelligence.Rev. Esp. Cardiol. (Engl. Ed.) 74, 573–575 (2021).
Diller, G. P. et al. Machine learning algorithms estimating prognosis and guiding therapy in adult congenital heart disease: data from a single tertiary centre including 10 019 patients. Eur. Heart J. 40, 1069–1077 (2019).
Diller, G. P. et al. Prediction of prognosis in patients with tetralogy of Fallot based on deep learning imaging analysis. Heart 106, 1007–1014 (2020).
Lu, X. H. et al. Recurrent disease progression networks for modelling risk trajectory of heart failure. PLoS One 16, e0245177 (2021).
Jone, P. N. et al. Artificial Intelligence in congenital heart disease: current state and prospects. JACC Adv. 1, 100153 (2022).
Naruka, V. et al. Machine learning and artificial intelligence in cardiac transplantation: a systematic review. Artif. Organs 46, 1741–1753 (2022).
Chang Junior, J. et al. Predictors of in-ICU length of stay among congenital heart defect patients using artificial intelligence model: a pilot study. Heliyon 10, e25406 (2024).
Chang Junior, J. et al. Improving preoperative risk-of-death prediction in surgery congenital heart defects using artificial intelligence model: a pilot study. PLoS One 15, e0238199 (2020).
Mayourian, J. et al. Deep learning-based electrocardiogram analysis predicts biventricular dysfunction and dilation in congenital heart disease. J. Am. Coll. Cardiol. 84, 815–828 (2024).
Ju, Y. et al. A multimodal deep learning tool for detection of junctional ectopic tachycardia in children with congenital heart disease. Heart Rhythm O2 5, 452–459 (2024).
Samad, M. D. et al. Predicting deterioration of ventricular function in patients with repaired tetralogy of Fallot using machine learning. Eur. Heart J. Cardiovasc. Imaging 19, 730–738 (2018).
Zhang, G. et al. The optimal tetralogy of fallot repair using generative adversarial networks. Front. Physiol. 12, 613330 (2021).
Huang, L. et al. Prediction of pulmonary pressure after Glenn shunts by computed tomography-based machine learning models. Eur. Radiol. 30, 1369–1377 (2020).
Lu, Y. et al. CT-TEE image registration for surgical navigation of congenital heart disease based on a cycle adversarial network. Comput Math. Methods Med. 2020, 4942121 (2020).
Troisi, J. et al. Noninvasive screening for congenital heart defects using a serum metabolomics approach. Prenat. Diagn. 41, 743–753 (2021).
Bahado-Singh, R. O. et al. Precision cardiovascular medicine: artificial intelligence and epigenetics for the pathogenesis and prediction of coarctation in neonates. J. Matern. Fetal Neonatal Med. 35, 457–464 (2022).
Joachim, A., Ye, S. & Zhao, M. T. Generation of cardiomyocytes and endothelial cells from human iPSCs by chemical modulation of Wnt signaling. Methods Mol. Biol. 2549, 335–344 (2022).
Fernandes, I., Funakoshi, S., Hamidzada, H., Epelman, S. & Keller, G. Modeling cardiac fibroblast heterogeneity from human pluripotent stem cell-derived epicardial cells. Nat. Commun. 14, 8183 (2023).
Ayoubi, S., Sheikh, S. P. & Eskildsen, T. V. Human induced pluripotent stem cell-derived vascular smooth muscle cells: differentiation and therapeutic potential. Cardiovasc. Res. 113, 1282–1293 (2017).
Garg, P. et al. Genome editing of induced pluripotent stem cells to decipher cardiac channelopathy variant. J. Am. Coll. Cardiol. 72, 62–75 (2018).
Drakhlis, L. & Zweigerdt, R. Heart in a dish—choosing the right in vitro model. Dis. Model Mech. 16, dmm049961 (2023).
Drakhlis, L. et al. Human heart-forming organoids recapitulate early heart and foregut development. Nat. Biotechnol. 39, 737–746 (2021).
Lewis-Israeli, Y. R. et al. Self-assembling human heart organoids for the modeling of cardiac development and congenital heart disease. Nat. Commun. 12, 5142 (2021).
Schmidt, C. et al. Multi-chamber cardioids unravel human heart development and cardiac defects. Cell 186, 5587–5605.e5527 (2023).
Boskovski, M. T. et al. De novo damaging variants, clinical phenotypes, and post-operative outcomes in congenital heart disease. Circ. Genom. Precis. Med. 13, e002836 (2020).
Michel, M., Laser, K. T., Dubowy, K. O., Scholl-Burgi, S. & Michel, E. Metabolomics and random forests in patients with complex congenital heart disease. Front. Cardiovasc. Med. 9, 994068 (2022).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (82270281, 82400365), the Key Project of Technology Innovation and Application Development in Chongqing (CSTB2023TIAD-KPX0048), China Postdoctoral Science Foundation (2023MD744155), the Natural Science Foundation of Chongqing Science and Technology Commission (CSTB2023NSCQ-BHX0020), Construction of Graduate Tutor Team in Chongqing Medical University (cqmudstd202205), Chongqing Elite Teachers and Experts Project (QiangShe [2022]), Postdoctoral Project of Chongqing Natural Science Foundation (CSTB2022NSCQ-BHX0626), Senior Medical Talents Program of Chongqing for Young and Middle-aged (JianlinDu [2022]), Future Medicine Youth Innovation Team Development Support Program of Chongqing Medical University (W0133), and Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University.
Author information
Authors and Affiliations
Contributions
Conceptualization: Y.L., Q.S., J.D. Software: Y.L., J.D., B.L. Visualization: Y.L., J.D., S.D. Investigation: Y.L., S.D., Y.Y., Y.L., J.W. Supervision: Q.S., J.D., X.B. Writing—original draft: Y.L., J.D., S.D. Writing—review & editing: Q.S., J.D., S.D., B.L., Y.L., X.B. All authors have read and approved the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Du, J., Deng, S. et al. The molecular mechanisms of cardiac development and related diseases. Sig Transduct Target Ther 9, 368 (2024). https://doi.org/10.1038/s41392-024-02069-8
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41392-024-02069-8
This article is cited by
-
Identification of disease-associated gene expression signatures for mechanistic insights and drug prediction in dilated cardiomyopathy-induced heart failure
Molecular and Cellular Biochemistry (2026)
-
Clinical outcomes in neonates with congenital heart disease with concurrent congenital neurological anomalies
BMC Pediatrics (2025)
-
Causal links between congenital malformations, birth weight, and neuroblastoma: insights from Mendelian randomization
BMC Pediatrics (2025)
-
Genomic data-driven framework for drug target discovery in atrial fibrillation
Journal of Translational Medicine (2025)
-
Organoids in respiratory virus research: advances and perspectives
Molecular Biomedicine (2025)