Abstract
The endocannabinoid (eCB) system has risen as a critical modulator linking the environmental challenges to behavioral maladaptation, such as trait anxiety and reward learning impairment. However, the association between trait anxiety and reward learning and how they share molecular mechanism in eCB system is still unknown. Here, we utilized a series of behavioral tests to screen the correlation among the behavioral patterns, especially between trait anxiety and reward learning. The elevated platform stress and open field test (OFT) were employed to classify the mice into the different level of trait anxiety, and ethanol-induced conditioned place preference (CPP) was used to assess the ability of reward learning. Our results indicated that high trait anxiety (HTA) mice exhibited increased reward learning. Intracranial administration of the cannabinoid CB1 receptor (CB1R) antagonist AM-251 or agonist WIN55,212-2 in nucleus accumbens (NAc) showed the different effect on anxiety-like behavior and reward learning. Similarly, CB1R knockout in VTA dopaminergic (VTADA) neurons resulted in anxiety-like behavior and reward learning impairment. Thus, we reveal insight into the role of CB1R in dopaminergic circuit from VTA to NAc, and present the evidence for a shared molecular mechanism between anxiety and reward learning.
Similar content being viewed by others
Introduction
Anxiety, a complex and multifaceted emotion, occupies a significant position in the human emotional experiences, transcending age and cultural boundaries [1, 2]. Its prevalence and impact on mental health have garnered increasing attention in recent years [3, 4]. Anxiety is also associated with depression, post-traumatic stress disorder (PTSD), and reward learning deficits [5,6,7,8]. As the diverse symptoms of anxiety, it can be categorized into trait anxiety and state anxiety [9]. Trait anxiety denotes the propensity of individuals to display diverse behavioral responses to similar or identical stressors, thereby revealing variations in their inherent anxiety predispositions [10]. It involves individual differences in the experience and management of anxiety across various situations [11]. Typically, anxiety-like behavior diminishes once individuals are removed from the stressful situations and stimuli. In contrast, state anxiety represents a transient reaction of such behaviors that is generally recoverable [12]. Accordingly, prolonged and persistent state anxiety may culminate in irreversible anxiety disorders [13]. Despite numerous studies affirming the distinction between trait and state anxiety [9, 14], the mechanism underlying how these two types of anxiety influence other behavioral outputs remains unclear.
Reward learning serves as a fundamental mechanism through which animals adapt to their environments and pursue positive outcomes [15, 16]. Also, reward learning is a one of the three subtypes of reward processing that are impaired in anhedonia, a prevalent symptom associated with major depressive disorder [17]. The process of reward learning involves specific neural circuits in the brain, particularly the classical dopaminergic pathway that extends from the ventral tegmental area (VTA) to the nucleus accumbens (NAc) [18, 19]. Within this circuit, dopamine release plays a key role in modulating reward learning [20, 21]. The dopamine release is typically governed by dopamine receptors, dopamine transporters, and endocannabinoid (eCB) system [22,23,24,25]. Previous study has elucidated the significant role of eCB system in modulating anxiety-like behaviors [26] and reward learning [27, 28]. The ligands of eCB system include anandamide (AEA) and 2-arachidonoylglycerol (2-AG), which are synthesized from arachidonic acid present in the human body [29]. These ligands interact with a family of G-protein-coupled receptors known as cannabinoid receptors type 1 (CB1R) and cannabinoid receptors type 2 (CB2R) [30]. CB1R is predominantly located in the terminals of both central and peripheral neurons, particularly within glutamatergic and GABAergic neuron populations. Additionally, CB1R is present in multiple brain regions, including the VTA and NAc [31]. In the nervous system, eCB bind to CB1R at the axon terminal, thereby activating Gi/o protein-mediated intracellular signaling pathways [26]. This process ultimately leads to the inhibition of neurotransmitter release from synaptic vesicles. Another study has demonstrated that CB1R are highly expressed in the mesolimbic dopamine system of the midbrain [32]. When mice are administered the natural cannabinoid Δ9-tetrahydrocannabinol (Δ9-THC), there is a significant reduction in dopamine levels within the NAc [33]. A neuropharmacological experiment has demonstrated that the injection of CB1R antagonist AM251 in the NAc shell and VTA significantly reduces cocaine intake when exposed to stress-induced conditions [31]. Furthermore, genetic variation in eCB system-related genes is a contributing factor for increased susceptibility to cannabis dependence in adolescents [34]. However, the role of CB1R in anxiety-related reward learning is still unknown.
In this study, we initially assessed the correlation between trait anxiety and reward learning by analyzing multidimensional behavioral performances in mice. Subsequently, we employed the elevated platform stress paradigm to stratify mice into high trait anxiety (HTA) and low trait anxiety (LTA) groups, thereby evaluating the impact of trait anxiety on reward learning through the ethanol-induced conditional place preference (CPP) test. Furthermore, the CB1R antagonist AM-251 or agonist WIN-55,212-2 was intracerebrally administrated in NAc to clarify the role of CB1R in anxiety-related reward learning. Finally, we utilized genetic technique to verify the influence of CB1R knockout within the VTA dopaminergic (VTADA) neurons on anxiety-like behavior and reward learning in mice. Thus, our study reveals that the CB1R of eCB pathway in VTADA-NAc circuit links trait anxiety with reward learning, and can provide a potential target for mood disorders.
Materials and methods
Animals
Male C57BL/6J mice, aged six to eight weeks, were purchased from Mouse Noble (Wuhan) Technology Co., Ltd. Adult male CB1R-flox mice were kindly provided by Prof. Man Li from the Department of Neurobiology, Huazhong University of Science and Technology [35]. All mice are housed at stable temperature (22–25 °C) and consistent humidity (50 ± 5%) on a 12-h light/dark cycle. Mice were housed in groups (3–4 mice per cage) for 1 week prior to the experiment and were acclimatized to the behavioral testing chamber at least 1 h prior to the behavioral tests. The sample size of each group was determined in accordance with prior experience and published studies. Age-matched mice under the same condition were randomly allocated to treatment and control groups. All animal experiments were approved by the Animal Care and Use Committee of Huazhong University of Science and Technology.
Viral vectors
All of the AAVs were provided by BrainVTA Co., Ltd. (Wuhan, China). AAVs were stored at −80 °C until use. The AAV9-TH-Cre-mCherry was used for stereotaxic injection at 5 × 1012 genome copies/ml.
Stereotaxic virus injection and cannula injection
For stereotactic virus injection, all mice were anesthetized via inhalation of isoflurane at a concentration of 3–5% for induction and 1–2% for maintenance. The stereotaxic apparatus (68030, RWD, China) and a microinjection pump (53311, Stoelting Co.) equipped with a glass needle were utilized to precisely inject the virus into the VTA (AP:−3.15 mm; ML:±0.6 mm; DV:−4.50 mm). For cannula implantation, mice were anesthetized and implanted in the NAc (AP: +1.42 mm; ML: ±0.75 mm; DV: −4.7 mm) with an outer diameter of 0.48 mm and an inner diameter of 0.34 mm. AM251 (CAS No:183232-66-8, Sigma-Aldrich) and WIN55,212-2 (CAS No:131543-23-2, Shanghai Yuanye Biotechnology Co., Ltd) was dissolved in DMSO and subsequently diluted with 0.9% saline to achieve a working solution concentration of 0.6 and 0.7 mg/ml respectively. For intracerebral injection, we employed previously implanted microinjection pumps and cannulas for localized administration into the NAc. Based on pre-established criteria, if the implantation site was incorrect upon anatomical validation, the mouse data were excluded.
Trait anxiety classification
We employed the elevated platform, a circular platform with a height of 1.3 meters and a diameter of 8 centimeters, to assess the trait anxiety in mice. The mice were promptly subjected to the open field test after a duration of 15 min on the surface. The classification of mice is based on the time spent in the central zone. Subsequently, these mice were divided into high trait anxiety (HTA) group (bottom one-third population) and low trait anxiety (LTA) group (top one-third population).
Open field test (OFT)
The mice were placed in an open square arena with 50 × 50 cm, allowing them to explore freely the environment. The whole arena was divided into a central zone and an outer zone. The spontaneous locomotion of the mice were recorded using a video tracking system (SuperMaze+, Xinruan, Shanghai). The movement trajectories were monitored and analyzed statistically over a duration of 5 min.
Elevated plus maze (EPM)
The EPM comprises a central platform, flanked by two arms enclosed by light grey walls and two open arms. Each arm is 350 mm in length and the maze was positioned 100 mm above ground level. Mice were placed on the central platform of EPM, and their behavior was monitored using commercial behavioral software (SuperMaze+, Xinruan, Shanghai). Also, the behavioral data were statistically analyzed over a duration of 5 min.
New object recognition (NOR)
The experiment is divided into three stages: habituation, familiarization, and testing. Each stage lasts for 10 min, totaling 30 min. During the habituation stage, mice are free to explore an open space for 10 min. In the familiarization phase, each mouse is given two identical objects, which are placed on the same side for 10 min. They have 10 min to explore and familiarize themselves with the objects (A1 and A2), which are recorded for subsequent analysis (SuperMaze, Xinruan, Shanghai). In the testing phase, at least one hour after the familiarization period, the A1 object is substituted with a novel object. The mice are positioned in the same way, and the behavioral data is collected.
Three-chamber sociability and social novelty test (SNT)
According to our earlier study [29], the three-chamber (3C) sociability and social novelty test was utilized to evaluate the social ability and social novelty in mice. The 3C apparatus is a white acrylic container measuring 40 cm in width, 60 cm in length, and 20 cm in height. The length of the box is partitioned into three sections: the left chamber, the middle chamber, and the right chamber, which are divided by semi-transparent acrylic dividers (0.5 cm in width, 20 cm in length, and 20 cm in height). A rectangular gate, 10 cm wide, is located in the center of two dividers, enabling animals to move in and out easily. The mouse was first positioned in the center chamber to explore freely for 10 min, with no other mice present on either chamber. For the social ability test session, the experimental mouse was taken out and returned to its home cage, while an unfamiliar homogeneous mouse was randomly placed in left or right chamber. Then the mouse was reintroduced to the middle chamber for another 10 min of exploration. For the social novelty test session, another unfamiliar homogeneous mouse was placed in the opposite chamber, and the test mouse was again placed in the middle to explore. The behavioral software (SuperMaze, Xinruan, Shanghai) with a top camera was used to monitor the movement trajectory. The amount of the time spent in each chamber was recorded to evaluate the social ability and social novelty.
Tail suspension test (TST)
Attach tape 1 cm from the end of the tail of mouse, Then hang it about 30 cm above the table so that the mouse cannot reach the surface. Position a plastic tube on the tail to stop the mouse from climbing up. Observe the mouse by the behavior software(SuperMaze, Xinruan, Shanghai)and document its immobility ratio for a duration of 5 min.
Sucrose preference test (SPT)
Prior to the official experiment, the mice will experience a 24-hour period to adapt to sucrose. Each mouse will be singly housed and given two bottles containing different solutions (water and a 1% sucrose). The positions of the water and sucrose bottles will be alternated every 8 h to prevent the mice from developing a preference for one position. During the testing phase, the mice will again receive water and sucrose using the same method, without needing to switch the bottle positions. After 12 h, the amount of sucrose and water consumed will be recorded. The preference for sucrose will be calculated as a percentage using the formula (amount of sucrose consumed × 100) / (amount of sucrose consumed + amount of water consumed).
Ethanol-induced conditioned place preference (CPP)
The ethanol-induced conditioned place preference (CPP) experiment was conducted in a three-chamber apparatus (Xinruan, Shanghai). Each chamber had a unique design, with one being a white room with a circular patterned floor and the other a black room with a rectangular patterned floor, separated by a central narrow black compartment. The ethanol-induced CPP procedure was divided into three stages: pre-training (day 1), training (days 2–9), and testing (day 10).
During the pre-training phase, mice were placed in the center of the box and allowed 20 min to explore freely. Software (SuperMaze, Xinruan, Shanghai) was used to monitor the time spent on each side. The side with more mouse preference was paired with saline, and the less preferred side with ethanol.
The training phase spanned 8 days, with four trials conducted over this period, each trial lasting two days. On the first day of each trial, mice received an intraperitoneal injection of 0.25 mL of a 20% ethanol solution in saline, followed by saline on the second day. Mice were then placed in the designated side for 5 min.
For the testing phase, mice were again allowed to explore the box freely for 20 min, with software tracking the time spent in each chamber.
Clustering analysis
In our study, we employed the pheatmap package in R to perform hierarchical clustering to classify the animals into distinct groups based on their behavioral performance across multiple tests. Before conducting the clustering analysis, we normalized all the data. For the hierarchical clustering, we applied the centroid linkage method. This method calculates the distance between two clusters as the distance between their centroids, which helps to minimize the variance within each cluster. The clustering process starts by treating each sample as a separate cluster and then iteratively merges the closest clusters until all samples are grouped into a single cluster. The resulting dendrogram was cut at a height that yielded two distinct clusters.
Western blotting
The VTA tissues (approximately 0.5 mg) obtained from mice were lysed in RIPA buffer supplemented with a protease inhibitor cocktail. After lysis, the lysates were centrifuged at 12,000 × g for 15 min at 4 °C, and the resulting supernatants were utilized for immunoblotting on 10% gels. Subsequently, the proteins were transferred onto a polyvinylidene fluoride (PVDF) membrane. Following the blocking step with 5% nonfat dry milk in TBST for 3 h at room temperature, the blots were then incubated overnight at 4 °C with primary antibodies. The next day, the membranes were washed with TBST and incubated with horseradish peroxidase-conjugated secondary antibodies at room temperature for 1 h. After three washes with TBST, the antibody-reactive bands were visualized using enhanced chemiluminescence (ECL) detection reagents (1:1, GE Healthcare) and a gel imaging system (Tanon, Shanghai, China). The primary antibodies used in assays were: CB1R (1:1000, CST, Cat#17978-1-AP) and GAPDH (1:3000, Proteintech, 10494-1-AP). Quantification was performed using the ImageJ software.
Immunofluorescence staining
In this research, mice underwent intracardial perfusion with a 4% paraformaldehyde solution after being anesthetized, followed by an overnight fixation of their brains at 4°C. Coronal sections of 35μm were then prepared using a Leica cryostat microtome after the brains were dehydrated in 20 and 30% sucrose solutions. The brain slices were washed with PBST (1 × PBS with 0.05% Tween 20), permeabilized with 0.3% Triton X-100, and blocked with a solution containing 0.1% bovine serum albumin (BSA) and 3% goat serum in 1 × PBS for 1 hour at 37 °C. The slices were incubated separately with primary antibodies, including tyrosine hydroxylase (TH, 1:1000, Proteintech, Cat#25859-1-AP), cannabinoid receptor 1 (1:1000, CST, Cat#17978-1-AP), at 4 °C for 16 hours. After three washes with PBST for 5 min each, the brain slices were incubated with secondary antibodies for 90 min at 37 °C in the dark. The secondary antibodies used were goat anti-rabbit antibodies conjugated with CoraLite 488 (Proteintech, 1:200, green stain, Cat# SA00013-2). Following nuclear counterstaining with DAPI, the sections were mounted in fluorescent medium and stored at 4 °C until analysis. Images were captured using an Olympus VS120 microscope and a Zeiss LSM780, and automated counting of fluorescent protein-positive neurons was conducted using ImageJ Fiji plugins.
Statistical analysis
Utilize a range of statistical tests to analyze the data. Begin with the Shapiro-Wilk test to evaluate the normality of all datasets. For datasets that are normally distributed, perform a two-tailed Student’s t-test for comparisons between two groups, and follow up with post-hoc Dunnett or Tukey multiple comparison tests after conducting one-way ANOVA for experiments involving more than two groups with a single factor. In cases where the data does not conform to a normal distribution, employ suitable non-parametric tests. Use Wilcoxon tests and Mann-Whitney tests for two-group comparisons, and apply the Kruskal-Wallis test along with Dunn’s multiple comparison test for experiments with more than two groups with a single factor. For analyses involving multiple comparisons within the same experimental group, we applied the Benjamini-Hochberg procedure to adjust p-values, thereby reducing the risk of Type I errors. Present all results as mean ± SEM, with significance levels marked as *P < 0.05, **P < 0.01, ***P < 0.001. P-values are computed using GraphPad Prism 8 (Graph Pad Software, Inc.). Same investigators analyzed the data, and all statistical details are provided in Data S1.
Results
Trait anxiety is positively associated with reward learning
To explore the relationship among multifaceted behavior performance in mice, we subjected all mice to a serious of behavioral tests, including the open field test (OFT) and elevated plus maze (EPM) for trait anxiety, new object recognition (NOR) and social novelty test (SNT) for cognition, tail suspension test (TST) and sucrose preference test (SPT) for trait depression, and ethanol-induced conditioned place preference (CPP) for reward learning (Fig. 1A). Subsequently, we conducted Pearson correlation analysis on all indicators and found a strong correlation not only between OFT and CPP, but also between EPM and CPP (Fig. 1B). Analyzing the preference scores and trait anxiety showed that mice with higher CPP preference scores corresponded to those exhibiting reduced time spent and distance travelled in central zone (Fig. 1C, D), and decreased time spent in open arms and entries into open arms (Fig. 1E, F). These pairwise correlation results indicate that trait anxiety is positively correlated with reward learning.
A. Experimental paradigm for a serious of behavioral tests. B. An analysis of correlation regarding the magnitude of behavioral associations among the mice; the lower left quadrant presents the correlation magnitudes, while the upper right quadrant displays the corresponding P-values. n = 34. C-F. Correlation analysis conducted among OFT, EPM, and CPP. G. Clustering analysis based on the indices from OFT, EPM, and CPP. Cluster1 (n = 18), Cluster2 (n = 16). H-M. Statistics of mice in the Cluster1 and Cluster 2 in OFT, EPM and CPP. Data are presented as the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, and ns for no significance.
To further investigate the relationship between trait anxiety and reward learning, we performed cluster analysis based on the behavioral indicators from OFT, EPM, and CPP. The results indicated that all mice could be divided into two distinct clusters (Fig. 1G). To evaluate the efficiency of the cluster analysis, we assessed the behavioral indicators of OFT, EPM, and CPP in different clusters. The results showed that the Cluster 1 group spent more time and travelled more distance in central zone for OFT compared with Cluster 2 group (Fig. 1H, I). Similarly, the time spent in open arms and entries into open arms of Cluster 2 mice also exhibited remarkably decrease (Fig. 1J, K). In the CPP, Cluster 1 group spent more time in conditional side (CS) and displayed higher preference score than Cluster 2 group (Fig. 1L, M). These results demonstrate that trait anxiety is positively correlated with reward learning.
HTA mice manifest enhanced reward learning compared to LTA mice
To further investigate the relationship between trait anxiety and reward learning, we exposed 42 mice to elevated platform stress for 15 min to induce a brief bout of anxiety. After the elevated platform stress, the OFT was conducted to assess the distinct trait anxiety level (Fig. 2A). According to the time spent in the central zone of OFT, mice were classified into high trait anxiety (HTA) mice (bottom one-third population) and low trait anxiety (LTA) mice (top one-third population) on Day 1. HTA mice displayed decreased exploration time, distance travelled in the central zone, and entries into the central zone compared with LTA mice (Fig. 2B–E). Meanwhile, total distance traveled in OFT did not differ between HTA and LTA mice (Fig. 2F). To determine if these differences prolonged without prior stress, the mice were subjected to the second OFT 24 hours after the first OFT (Fig. 2A). On day 3, there was no significant difference between HTA and LTA mice in central exploration time, central distance traveled, or entries into central zone (Fig. 2G–K), indicating that the elevated platform stress-provoked anxiety-like behavior was reversible.
A. Behavior paradigm of anxiety trait classification and ethanol-induced conditioned place preference. n = 42. B-F. Representative traces and statistics in OFT on day 1. high trait anxiety (HTA) group, n = 14; low trait anxiety (LTA) group, n = 14. G-K. Traces and statistics representing mice performance in OFT on day 3. L. Representative traces of mice in the HTA and LTA groups in CPP. M-N. Mean time spent in the conditioned side and preference score during the post-training test for both HTA and LTA groups. Data are presented as the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, and ns for no significance.
Then, we employed the CPP paradigm to investigate the ability of reward learning in different trait anxiety mice. Initially, we administered 2 g/kg ethanol via intraperitoneal injection and confined the mice to the conditioned side of the three-chamber CPP apparatus. In alternating sessions, the unconditional side (US) was paired with saline. Thereafter, mice were allowed freely access to either chamber (Fig. 2A). The two indicators of average time spent in the CS (paired with ethanol) and preference score were utilized to evaluate ethanol-induced CPP. The results showed that both the HTA group and LTA group exhibited a significant preference for ethanol after training (Fig. 2L–N). Meanwhile, the HTA mice spent a significantly increased time in the CS and showed the higher preference scores compared to LTA mice (Fig. 2L–N). Thus, these findings indicate that the mice with different trait anxiety manifest distinct ability of reward learning. Specifically, HTA mice exhibit enhanced reward learning compared to LTA mice.
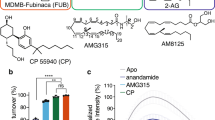
Bidirectional modulation of CB1R activity in NAc has the opposite effect on anxiety
Next, we aim to clarify whether the CB1R in the NAc involves in anxiety-like behavior in mice. The cannulas were implanted bilaterally in the NAc, and the CB1R antagonist AM251 or agonist WIN55,212-2 were administrated via intracerebral injection. The control mice received the equal volume of vehicle (Vehicle group). Thirty minutes later, the OFT and EPM were conducted to assess anxiety-like behaviors in mice (Fig. 3A). The implantation sites of cannulas in the NAc were confirmed by morphological analysis (Fig. 3B). The behavioral results of the OFT showed that the AM251 group spent less time and travelled shorter distance in the central zone compared to the Vehicle group, whereas the WIN55,212-2 group showed the more time spent and longer distance (Fig. 3C–E). Moreover, there was no significant difference of the entries into the central zone and the total distance travelled in the AM251 group and WIN55,212-2 group when comparing with Vehicle group (Fig. 3F–G). Similarly, in the EPM, the time spent and distance travelled in open arms, and the entries into open arms were significantly changed in AM251 group and WIN55,212-2 group (Fig. 3H–K). Moreover, the distance travelled in EPM was no significant changed among three groups (Fig. 3L). On Day 3, the mice were subjected to the second OFT and EPM. The results demonstrated no significant differences across groups in central exploration time, central distance traveled, or entries into the central zone, indicating that the behavioral alterations induced by CB1 receptor antagonist or agonist administration were reversible (Fig. S1). Moreover, we verified the expression of CB1R in the VTA of HTA and LTA mice. The results showed that CB1R expression in the VTA of HTA mice is significantly lower than that in LTA mice (Fig. S2). Then, when we injected the CB1R agonist WIN55,212-2 into HTA mice, they showed anxiolytic effects. In contrast, when we injected the CB1R antagonist AM251 into LTA mice, it caused state anxiety (Figs. S3–4). Furthermore, CB1R inhibition via AM251 administration in the NAc directly triggers state anxiety, whereas CB1R activation via WIN55,212-2 injection induces an anxiolytic effect. Collectively, these results indicate that modulating CB1R activity in the NAc has opposing effects on anxiety behavior.
A. Schematic diagram of cannula implantation and experimental scheme of anxiety tests. n = 8 mice for each group. B. Representative image of NAc-implantation sites and the placements of bilateral optic fiber tips. Scale bar, 100 μm. C-G. Representative traces and statistics in OFT. H-L. Traces and statistics representing mice performance in EPM. Data are presented as the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, and ns for no significance.
Blocking CB1R in NAc leads to reward learning deficit
Afterward, we utilized the same approach to explore the influence of CB1R on the ability of reward learning in mice. The cannulas were implanted bilaterally in the NAc to modulate the synaptic terminals of CB1R in the NAc. The ethanol-induced CPP paradigm was to assess the performance of reward learning (Fig. 4A). The results showed that both the Vehicle and WIN55,212-2 groups exhibited a stronger preference for ethanol, whereas the AM251 group did not displayed significant changes in the mean time spent in CS chamber and preference score (Fig. 4B). Furthermore, compared to the Vehicle mice, the AM251 mice showed a marked decrease in the average time spent in CS chamber and preference score, while the WIN55,212-2 mice exhibited no significant difference (Fig. 4C, D). Similarly, in HTA mice, we bilaterally implanted cannulas in the NAc and administered WIN55,212-2. In LTA mice, we injected AM251 into the NAc. Results indicated that HTA mice treated with WIN55,212-2 exhibited enhanced reward learning. Conversely, LTA mice administered AM251 showed significantly impaired reward learning (Figs. S5–6). Collectively, these findings indicate that the CB1R blockade in NAc results in reward learning dysfunction.
A. The timeline of experimental scheme and diagram for cannula implantation and ethanol-mediated CPP. Vehicle group (n = 7), AM-251 group (n = 8), WIN55,212-2 group (n = 8). B. Representative traces and behavioral performance result of pre/post-training test. C-D. Mean time spent in the conditioned side and preference score during the post-training test. Data are presented as the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, and ns for no significance.
CB1R knockout in VTADA neurons triggers state anxiety
To further study the effect of CB1R deletion in VTADA neurons on the anxiety and reward learning, we bilaterally injected the tyrosine hydroxylase (TH) promoter-containing adeno-associated virus (AAV9-TH-Cre-mCherry) into the VTA region of CB1R-flox transgenic mice to selectively express Cre recombinase in VTADA neurons. The wild-type (WT) mice were injected by AAV9-TH-Cre-mCherry as control. After three weeks of viral expression, the OFT and EPM were conducted to assess the anxiety-like behavior in all mice (Fig. 5A). The viral expression was confirmed by immunofluorescence staining with anti-TH in VTA (Fig. 5B). Meanwhile, the percentage of mCherry+TH+ cells reached 97.1% in mCherry+ cells and 81.7% in TH+ cells, indicating that the specificity and efficiency of viral-mediated expression was acceptable (Fig. 5C). The schematic diagram of mouse brain suggested that the all injections were restricted to the VTA region (Fig. 5D). To verify the efficiency of CB1R deletion in VTADA neurons, the double immunofluorescence staining was conducted. The results showed that the CB1R expression was remarkably reduced in the VTA area of CB1R−/− mice compared with WT mice (Fig. 5E). For the OFT, the CB1R−/− mice showed decreased time spent and distance travelled in the central zone, and reduced entries into the central zone compared with WT mice (Fig. 5F–I). There was no significant difference between the two groups in total distance travelled (Fig. 5J). The behavioral results of the EPM displayed that the CB1R−/− mice spent less time and travelled shorter distance in the open arms than WT mice (Fig. 5K–N). Moreover, no significant difference of the total distance travelled was observed between CB1R−/− mice and WT mice (Fig. 5J, O). Therefore, these findings demonstrate that CB1R deletion in VTADA neurons directly provokes prolonged state anxiety in mice.
A. Schematic shows the timeline of virus injection and behavior tests. B. Representative image of VTA-injection sites. Scale bar, 100 μm. n = 7 mice for each group. C. The quantitative analysis of the Venn diagram reveals the extent of co-expression between mCherry and TH in the VTA. D. Locations of the viral injection for all animals analyzed in WT and CB1R−/− groups. E. Co-localization and quantification of mCherry and CB1R in the VTA. F-J. Representative traces and statistical results of mice in OFT. K-O. Representative trajectories and statistical results of WT and CB1R−/− mice in EPM. Data are presented as the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, and ns for no significance.
CB1R knockout in VTADA neurons reduces the reward learning ability
Then, we examine the impact of CB1R knockout in VTADA neurons on the ability of reward learning. The virus of AAV9-TH-Cre-mCherry was bilaterally injected into the VTA area of CB1R-flox mice. Three weeks later, all mice were subjected to the pre-training CPP test on Day 1, the ethanol-induced CPP paradigm from Day 2 to Day 9, and the post-training CPP test on Day 10 (Fig. 6A). Similarly, the specificity and efficiency of viral-mediated expression, and the injection sites were confirmed through morphological analysis (Fig. 6B–D). Relative to the pre-training CPP test, WT mice showed markedly increased average time and high preference score in the CS chamber (Fig. 6E). For the CB1R−/− group, there was no significant difference between pre-training and post-training test (Fig. 6F–G). Furthermore, comparing with the WT mice, the average time spent in the ethanol-paired chamber and preference score was considerably reduced in CB1R−/− mice (Fig. 6F–G). In summary, these results indicate that CB1R knockout in VTADA neurons substantially diminishes the ability of reward learning.
A. Schematic of viral injection and ethanol-mediated CPP paradigm. WT group (n = 9), CB1R−/− group (n = 6). B. Immunofluorescent analysis of viral expression in VTA. Red channel showed the mCherry expression. Green channel exhibited the staining of anti-TH. Scale bar, 100 μm. C. The quantitative analysis of Venn diagram shows the co-expression level of mCherry with TH in SNc. D. Locations of the viral injection for all animals analyzed in WT and CB1R−/− groups. E. Representative traces and behavioral performance result of pre/post-training test. F-G. Mean time spent in the conditioned side and preference score during the post-training test. Data are presented as the mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, and ns for no significance.
Discussion
Despite numerous studies highlighting significant differences between trait anxiety and state anxiety, the relationship between trait anxiety and reward learning remains largely unexplored [36]. Here, we assessed the correlation between trait anxiety and reward learning by analyzing various behavioral performances in mice. Additionally, using the elevated platform stress paradigm, we successfully classified mice into distinct levels of trait anxiety based on their performance in the OFT. Notably, the anxiety-like behavior can be self-relieved 24 hours after the elevated platform treatment. Subsequently, we observed that HTA mice exhibited a heightened preference in ethanol-induced CPP paradigm. To elucidate the role of CB1R in anxiety and reward learning, we manipulated CB1R activity through pharmacological intervention and genetically modified mice to detect the behavioral changes in anxiety and reward learning. Our findings indicate that when CB1R activity is inhibited, mice display irreversible anxiety-like behavior and reduced ability of reward learning. In summary, these results showed that the trait anxiety is positively associated with reward learning, and CB1R within the VTADA-NAc circuit may share a common molecular mechanism for anxiety and reward learning.
Anxiety is the most prevalent neuropsychiatric disorder in humans, with a global prevalence ranging from 0.9 to 28.3% [37]. It not only leads to significant impairments in daily functioning but also frequently coexists with major depressive disorder and reward learning deficits [38, 39]. At present, the relationship between trait anxiety and reward learning deficits has attracted much attention. The ethanol-induced CPP was employed to evaluate reward learning due to its direct relevance to alcohol addiction. Alcohol use disorder is a major global public health problem, and it often coexists with anxiety disorders. This makes the study of their comorbidity crucial. Reward learning is a key part of addiction, and ethanol-induced CPP directly models this process. CPP has several advantages over other reward learning assays. Unlike self-administration, which can be influenced by motor activity differences, or sucrose preference tests, which measure general reward responsiveness, CPP specifically assesses cue-reward associations. This specificity is vital for studying the motivational aspects of addiction and the impact of anxiety on alcohol-related behaviors. In this study, we utilized the CPP paradigm, which links rewards to environmental cues and reflects motivated behavior associated with reward dependence, to investigate the impact of anxiety on reward learning in male mice [40, 41]. The results indicated that mice with high-level trait anxiety demonstrated more pronounced reward-seeking behavior. This is consistent with prior study that individuals who are more easily influenced by the external environment have stronger abilities in reward learning [42]. Moreover, mild stress stimulation-provoked acute anxiety can significantly enhance the reward-seeking behavior of mice [43]. Therefore, we adopted elevated platform stress paradigm to further classify the trait anxiety in mice. Based on the percentage of time spent in the central zone of OFT, we designated the group of mice with relatively higher exploration time in the central zone as LTA mice, while the lower group as HTA mice. On the second day following their removal from the elevated platform stress, the anxiety-like behaviors exhibited by all groups of mice restored. This observation indicates that our screening behavioral results reflect trait anxiety rather than state anxiety in the subjects. Furthermore, post-training CPP test revealed that the HTA mice demonstrated a significant preference for ethanol.
Previous studies have suggested that the VTADA neurons activity leads to an increase of dopamine concentration in the NAc, thereby modulating anxiety and reward learning [44, 45]. Meanwhile, the CB1R is abundantly expressed in the VTA and NAc, playing a pivotal role in modulating dopamine release [46, 47]. Thus, we administered the CB1R antagonist AM-251 and the agonist WIN55,212-2 into the NAc to assess their effects on anxiety-like behavior and reward learning in mice. These results indicate that when CB1R is blocked by AM-251 injection, mice exhibit significant anxiety-like behavior. Conversely, the agonist WIN55,212-2 injection elicited a marked anxiolytic effect, consistent with previous research [48, 49]. Interestingly, mice exhibited a marked impairment in reward learning following the CB1R antagonist AM-251 treatment. This is similar to a human study previously reported, where individuals with high anxiety levels showed reward learning deficits [50]. Moreover, the activation of VTADA-NAc circuit can significantly reduce ethanol consumption in mice [51]. These findings demonstrate that the loss of CB1R function may lead to overactivation of the VTADA-NAc circuit, resulting in state anxiety and reward learning deficits in mice. Overall, our experiments show that there’s a difference in CB1R expression between HTA and LTA mice. Manipulating CB1R in these mice has a significant impact on their reward learning. One possible reason is CB1R regulation can disrupt the dopamine balance in the VTADA-NAc circuit. As previous studies showed, CB1R play a key role in regulating dopamine release [52]. Normally, activated CB1R inhibit the activity of dopaminergic neurons, reducing dopamine release [53]. When CB1R are blocked, this may lead to overactivation of the VTA-NAc circuit. It may interfere with reward learning processes and reduce the brain’s sensitivity to reward signals, thus impairing reward learning [54]. To further validate the effect of CB1R on anxiety and reward learning, we administered the AAV9-TH-Cre-mCherry virus into the VTA region of CB1R-Flox mice. This approach allowed us to specifically knock out CB1R in both the VTADA neurons and these NAc-projected terminals. Then, the effect of CB1R knockout in VTADA neurons on anxiety and reward learning. These behavioral manifestations are consistent with the results of NAc injection of CB1R inhibitor. The above evidence indicates that when CB1R is knocked out in the VTA-NAc circuit, mice develop irreversible state anxiety and reward learning deficits.
As we delve deeper into the reasons behind these experimental differences, we speculate that these differences may be attributed to the distinct activities of the mesolimbic dopaminergic system between trait anxiety and state anxiety. Trait anxiety, which is relatively stable and personality-based, has been shown to correlate with structural and functional differences in brain networks such as the default mode network and salience network. In contrast, state anxiety, which is more transient and context-dependent, is associated with functional connectivity changes in these networks during specific tasks or stressors [9]. Additionally, the mesolimbic dopamine system, which includes the VTA and NAc, plays a significant role in both reward processing and anxiety disorders [55]. This system activity can vary depending on the type of anxiety and the specific neural pathways involved, potentially explaining the observed differences. Furthermore, the expression, trafficking and membrane localization of CB1R in the VTA-NAc circuit is crucial for anxiety and reward learning [47, 56, 57]. Our data show that CB1R expression in the VTA of HTA mice is significantly lower than that in LTA mice. Despite the reduced CB1R expression, HTA mice exhibit enhanced ethanol-induced CPP, which may be related to compensatory mechanisms that heighten the sensitivity of the mesolimbic dopaminergic system to reward-related stimuli, thereby amplifying the rewarding effects of ethanol in similar with the previous study [51]. The knockout of CB1R in the VTA-NAc circuit impairs the compensatory mechanism of the mesolimbic dopaminergic system, thereby leading to the state anxiety and impaired reward learning.
Certainly, this study has several limitations. We mainly explored the influences of CB1R in the VTADA-NAc circuit on anxiety and reward-related learning in the present study. Although the main downstream of VTADA neurons is the NAc, the projection of VTADA neurons to other brain regions would also be affected when the AAV9-TH-Cre-mCherry was injected into the VTA. Thus, at least some of the effects of CB1R knockout could be occurring in other downstream areas from VTADA neurons. Moreover, directly injecting CB1R agonists or antagonists into the NAc can also significantly affect the activity of glutamate and GABA neurons in the NAc. These changes can directly impact the coordination of neuronal activity and may lead to impaired reward learning.
In conclusion, our study indicates that mice exhibiting high level of trait anxiety exhibit enhanced ability in reward learning. Also, bidirectional modulation of CB1R within the VTADA-NAc circuit results in the distinct manifestations of anxiety-like behavior and reward learning ability. Therefore, this study illustrates that pharmacological targeting of CB1R represents a promising intervention for individuals experiencing mood disorders and their accompanying symptoms.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Global Burden of Disease Study C. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602.
Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. 2020;370:eaay0214.
Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–50.
Tiller JW. Depression and anxiety. Med J Aus. 2013;199:S28–31.
van Dis EAM, van Veen SC, Hagenaars MA, Batelaan NM, Bockting CLH, van den Heuvel RM, et al. Long-term outcomes of cognitive behavioral therapy for anxiety-related disorders: a systematic review and meta-analysis. JAMA Psychiatr. 2020;77:265–73.
Craske MG, Dunn BD, Meuret AE, Rizvi SJ, Taylor CT. Positive affect and reward processing in the treatment of depression, anxiety and trauma. Nat Rev Psychol. 2024;3:665–85.
Pike AC, Robinson OJ. Reinforcement learning in patients with mood and anxiety disorders vs control individuals a systematic review and meta-analysis. JAMA Psychiatr. 2022;79:313–22.
Saviola F, Pappaianni E, Monti A, Grecucci A, Jovicich J, De Pisapia N. Trait and state anxiety are mapped differently in the human brain. Sci Rep.-Uk. 2020;10:11112.
Endler NS, Kocovski NL. State and trait anxiety revisited. J Anxiety Disord. 2001;15:231–45.
Knowles KA, Olatunji BO. Specificity of trait anxiety in anxiety and depression: meta-analysis of the State-Trait Anxiety Inventory. Clin Psychol Rev. 2020;82:101928.
Hieu TH, Dibas M, Surya Dila KA, Sherif NA, Hashmi MU, Mahmoud M, et al. Therapeutic efficacy and safety of chamomile for state anxiety, generalized anxiety disorder, insomnia, and sleep quality: a systematic review and meta-analysis of randomized trials and quasi-randomized trials. Phytother Res. 2019;33:1604–15.
Liu WZ, Huang SH, Wang Y, Wang CY, Pan HQ, Zhao K, et al. Medial prefrontal cortex input to basolateral amygdala controls acute stress-induced short-term anxiety-like behavior in mice. Neuropsychopharmacology. 2023;48:734–44.
Steiner LM, Zaske S, Durand S, Molloy M, Arteta R. Spiritual factors predict state and trait anxiety. J Relig Health. 2017;56:1937–55.
Rajagopalan AE, Darshan R, Hibbard KL, Fitzgerald JE, Turner GC. Reward expectations direct learning and drive operant matching in. Proc Natl Acad Sci USA. 2023;120:e2221415120.
Schultz W. Multiple reward signals in the brain. Nat Rev Neurosci. 2000;1:199–207.
Borsini A, Wallis ASJ, Zunszain P, Pariante CM, Kempton MJ. Characterizing anhedonia: a systematic review of neuroimaging across the subtypes of reward processing deficits in depression. Cogn Affect Behav Neurosci. 2020;20:816–41.
Cohen JY, Haesler S, Vong L, Lowell BB, Uchida N. Neuron-type-specific signals for reward and punishment in the ventral tegmental area. Nature. 2012;482:85–U109.
Eshel N, Bukwich M, Rao V, Hemmelder V, Tian J, Uchida N. Arithmetic and local circuitry underlying dopamine prediction errors. Neuropsychopharmacology. 2015;40:S611–S.
Sharpe MJ, Chang CY, Liu MA, Batchelor HM, Mueller LE, Jones JL, et al. Dopamine transients are sufficient and necessary for acquisition of model-based associations (vol 20, pg 735, 2017). Nat Neurosci. 2018;21:1493.
Berke JD. What does dopamine mean?. Nat Neurosci. 2018;21:787–93.
Liu C, Kaeser PS. Mechanisms and regulation of dopamine release. Curr Opin Neurobiol. 2019;57:46–53.
Beaulieu JM, Gainetdinov RR. The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63:182–217.
Miller GW, Gainetdinov RR, Levey AI, Caron MG. Dopamine transporters and neuronal injury. Trends Pharm Sci. 1999;20:424–9.
Oleson EB, Hamilton LR, Gomez DM. Cannabinoid modulation of dopamine release during motivation, periodic reinforcement, exploratory behavior, habit formation, and attention. Front Synaptic Neurosci. 2021;13:660218.
Lutz B, Marsicano G, Maldonado R, Hillard CJ. The endocannabinoid system in guarding against fear, anxiety and stress. Nat Rev Neurosci. 2015;16:705–18.
Wenzel JM, Cheer JF. Endocannabinoid regulation of reward and reinforcement through interaction with dopamine and endogenous opioid signaling. Neuropsychopharmacology. 2018;43:103–15.
Parsons LH, Hurd YL. Endocannabinoid signalling in reward and addiction. Nat Rev Neurosci. 2015;16:579–94.
Li M, Lv XY, Li TX, Cui C, Yang XK, Peng X, et al. Basolateral amygdala cannabinoid CB1 receptor controls formation and elimination of social fear memory. ACS Chem Neurosci. 2023;14:3674–85.
Kondev V, Najeed M, Yasmin F, Morgan A, Loomba N, Johnson K, et al. Endocannabinoid release at ventral hippocampal-amygdala synapses regulates stress-induced behavioral adaptation. Cell Rep. 2023;42:113027.
McReynolds JR, Wolf CP, Starck DM, Mathy JC, Schaps R, Krause LA, et al. Role of mesolimbic cannabinoid receptor 1 in stress-driven increases in cocaine self-administration in male rats. Neuropsychopharmacology. 2023;48:1121–32.
Hernandez G, Oleson EB, Gentry RN, Abbas Z, Bernstein DL, Arvanitogiannis A, et al. Endocannabinoids promote cocaine-induced impulsivity and its rapid dopaminergic correlates. Biol Psychiat. 2014;75:487–98.
Bloomfield MA, Ashok AH, Volkow ND, Howes OD. The effects of Delta(9)-tetrahydrocannabinol on the dopamine system. Nature. 2016;539:369–77.
Burgdorf CE, Jing D, Yang R, Huang C, Hill MN, Mackie K, et al. Endocannabinoid genetic variation enhances vulnerability to THC reward in adolescent female mice. Sci Adv. 2020;6:eaay1502.
Zhu H, Xiang HC, Li HP, Lin LX, Hu XF, Zhang H, et al. Inhibition of GABAergic neurons and excitation of glutamatergic neurons in the ventrolateral periaqueductal gray participate in electroacupuncture analgesia mediated by cannabinoid receptor. Front Neurosci. 2019;13:484.
Leal PC, Goes TC, da Silva LCF, Teixeira-Silva F. Trait vs. state anxiety in different threatening situations. Trends Psychiatry Psychother. 2017;39:147–57.
Collaborators C-MD. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–12.
Cosci F, Fava GA. When anxiety and depression coexist: the role of differential diagnosis using clinimetric criteria. Psychother Psychosom. 2021;90:308–17.
Neumann SR, Glue P, Linscott RJ. Aberrant salience and reward processing: a comparison of measures in schizophrenia and anxiety. Psychol Med. 2021;51:1507–15.
Zhou Y, Zhu H, Liu Z, Chen X, Su X, Ma C, et al. A ventral CA1 to nucleus accumbens core engram circuit mediates conditioned place preference for cocaine. Nat Neurosci. 2019;22:1986–99.
Lei J, Zhang P, Li T, Cui C, Li M, Yang X, et al. Alternating bilateral sensory stimulation alleviates alcohol-induced conditioned place preference via a superior colliculus-VTA circuit. Cell Rep. 2024;43:114383.
Raio CM, Konova AB, Otto AR. Trait impulsivity and acute stress interact to influence choice and decision speed during multi-stage decision-making. Sci Rep. 2020;10:7754.
Klenowski PM, Zhao-Shea R, Freels TG, Molas S, Zinter M, M’Angale P, et al. A neuronal coping mechanism linking stress-induced anxiety to motivation for reward. Sci Adv. 2023;9:eadh9620.
Qi G, Zhang P, Li T, Li M, Zhang Q, He F, et al. NAc-VTA circuit underlies emotional stress-induced anxiety-like behavior in the three-chamber vicarious social defeat stress mouse model. Nat Commun. 2022;13:577.
Yagishita S. Cellular bases for reward-related dopamine actions. Neurosci Res. 2023;188:1–9.
Han X, Liang Y, Hempel B, Jordan CJ, Shen H, Bi GH, et al. Cannabinoid CB1 receptors are expressed in a subset of dopamine neurons and underlie cannabinoid-induced aversion, hypoactivity, and anxiolytic effects in mice. J Neurosci. 2023;43:373–85.
Bacharach SZ, Martin DA, Stapf CA, Sun F, Li Y, Cheer JF, et al. Decreased ventral tegmental area CB1R signaling reduces sign tracking and shifts cue-outcome dynamics in rat nucleus accumbens. J Neurosci. 2023;43:4684–96.
Sink KS, Segovia KN, Sink J, Randall PA, Collins LE, Correa M, et al. Potential anxiogenic effects of cannabinoid CB1 receptor antagonists/inverse agonists in rats: comparisons between AM4113, AM251, and the benzodiazepine inverse agonist FG-7142. Eur Neuropsychopharm. 2010;20:112–22.
Lisboa SF, Niraula A, Resstel LB, Guimaraes FS, Godbout JP, Sheridan JF. Repeated social defeat-induced neuroinflammation, anxiety-like behavior and resistance to fear extinction were attenuated by the cannabinoid receptor agonist WIN55,212-2. Neuropsychopharmacology. 2018;43:1924–33.
Guitart-Masip M, Walsh A, Dayan P, Olsson A. Anxiety associated with perceived uncontrollable stress enhances expectations of environmental volatility and impairs reward learning. Sci Rep. 2023;13:18451.
Juarez B, Morel C, Ku SM, Liu Y, Zhang H, Montgomery S, et al. Midbrain circuit regulation of individual alcohol drinking behaviors in mice. Nat Commun. 2017;8:2220.
Kucera R, Bouskila J, Elkrief L, Fink-Jensen A, Palmour R, Bouchard JF, et al. Expression and localization of CB1R, NAPE-PLD, and FAAH in the vervet monkey nucleus accumbens. Sci Rep. 2018;8:8689.
Freels TG, Lester DB, Cook MN. Arachidonoyl serotonin (AA-5-HT) modulates general fear-like behavior and inhibits mesolimbic dopamine release. Behav Brain Res. 2019;362:140–51.
Al-Hasani R, Gowrishankar R, Schmitz GP, Pedersen CE, Marcus DJ, Shirley SE, et al. Ventral tegmental area GABAergic inhibition of cholinergic interneurons in the ventral nucleus accumbens shell promotes reward reinforcement. Nat Neurosci. 2021;24:1414–28.
Lin ER, Veenker FN, Manza P, Yonga MV, Abey S, Wang GJ, et al. The limbic system in Co-occurring substance use and anxiety disorders: a narrative review using the RDoC framework. Brain Sci. 2024;14:1285.
Geisler CE, Hayes MR. Metabolic hormone action in the VTA: reward-directed behavior and mechanistic insights. Physiol Behav. 2023;268:114236.
Kibret BG, Canseco-Alba A, Onaivi ES, Engidawork E. Crosstalk between the endocannabinoid and mid-brain dopaminergic systems: implication in dopamine dysregulation. Front Behav Neurosci. 2023;17:1137957.
Acknowledgements
This work was supported financially by grants from National Natural Science Foundation of China (no. 31871073 and 32171023 to B.T. and no. 32271036 and 32471034 to P.Z.).
Author information
Authors and Affiliations
Contributions
Behavior experiments and immunofluorescence: CC, GGL, YYB, YLS. Data analyzing: CC, GGL, ML, JL, KR. Virus injection: CC. Mice breeding and reproduction: TXL, XP, XKY, JY, JSD, STC. Designing and writing: BT, PZ.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study involved only animal research. All experimental procedures involving animals were conducted with approved protocols from the Huazhong University of Science and Technology (No. S1871).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cui, C., Luo, G., Lei, J. et al. Cannabinoid CB1 receptor in dopaminergic circuit from ventral tegmental area to nucleus accumbens links trait anxiety with reward learning. Transl Psychiatry 15, 395 (2025). https://doi.org/10.1038/s41398-025-03644-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-025-03644-5