Abstract
Antimicrobial resistance (AMR) is a global health challenge. The gut microbiome, a major reservoir for AMR, is influenced by dietary habits. However, the specific impact of dietary patterns on gut resistome remains poorly understood. This study aimed to assess the effects of high-fat/low-fiber and high-fiber/low-fat diets on the development of AMR in the gut microbiome. The shift from a normal diet to a high-fat/low-fiber or a high-fiber/low-fat diet in mice resulted in corresponding increases and decreases in the relative abundance of the resistome (0.14 to 0.25, p < 0.001 vs. 0.14 to 0.09 p < 0.05), virulence genes (VGs) (0.56 to 0.91, p < 0.001 vs. 0.58 to 0.50, p < 0.05), and mobile genetic elements (MGEs) (0.20 to 1.66, p < 0.001 vs. 0.22 to 0.13, p < 0.05), respectively. Network analyses identified bacteria such as Bacteroides, Parabacteroides, and Alistipes as hosts of ARGs and VGs, with changes in their abundance closely associated with shifts in ARG and VG levels. Mobile genetic elements such as Tn916, ISBf10, IS91, and intl1 were linked to these variations, including genes conferring resistance to vancomycin and capsule-related VGs. In humans, a similar trend was observed, with high-fat diets correlating with higher resistome levels, while high-fiber diets were associated with lower resistome levels compared to a normal diet group. ARGs were more prevalent in pathogenic genera such as Enterococcus spp., Klebsiella spp., Pseudomonas spp., and Staphylococcus spp. The high-fat/low-fiber diet increased the bacterial resistome and VG abundance compared to a high-fiber/low-fat diet. Therefore, adopting a high-fiber/low-fat diet may be an effective strategy to reduce the AMR burden in the human gut, providing a valuable insight for public health recommendations.
Similar content being viewed by others
Introduction
Our diet profoundly influences our health, and the gut microbiome plays a critical role in this dynamic relationship1. Numerous studies have shown that a Western diet, rich in fat and low in fiber, contributes to the development of obesity, type 2 diabetes, cardiovascular diseases, microbial pathogenesis, and chronic inflammation1,2,3,4,5. One proposed mechanism is that a high-fat diet promotes the expansion of pro-inflammatory bacterial taxa, such as Bilophila, while concurrently reducing beneficial commensal microbes5. This dysbiosis has been directly linked to enhanced inflammatory responses and even carcinogenic outcomes, as observed in colonic tumorigenesis models5. In contrast, although the health benefits of a high-fiber, low-fat diet remain under debate, dietary fiber has been associated with reductions in both inflammation and depressive symptoms6. For instance, microbiota-accessible carbohydrates (MACs), a key component of dietary fiber, have been shown to suppress Clostridium difficile infection in mice by enhancing short-chain fatty acid (SCFA) production and maintaining microbial niche stability through competitive exclusion3. These findings highlight the critical role of high-fat versus high-fiber diets in shaping gut microbial communities and indicate divergent ecological and physiological outcomes depending on diet composition. Therefore, the popular saying “you are what you eat” captures the complex interaction between diet, the microbiome, and host health7.
Antimicrobial resistance (AMR) poses an urgent global threat to human health. According to a recent estimate by the Antimicrobial Resistance Collaborators (2021), approximately 4.71 million deaths were associated with bacterial AMR, including 1.14 million deaths directly attributable to it8. While infectious diseases caused by resistant bacteria directly result in human and animal deaths, increasing attention has been focused on AMR encoded within the gut microbiome. This concern arises from three key factors: (1) the gut microbiome serves as a reservoir for antimicrobial resistance genes (ARGs) in both humans and animals9,10; (2) the gut microbiome acts as a hotspot for horizontal gene transfer (HGT), facilitating the spread of ARGs to opportunistic bacteria11,12; and (3) opportunistic bacteria within the gut microbiome can cause infectious diseases, including blood infections13,14. Consequently, a high abundance of total ARGs in the gut, collectively referred to as the resistome, indicates an elevated risk to human health and may be considered as an atypical intestinal disorder.
While antibiotic use remains the primary driver of ARG dissemination, emerging evidence suggests that diets also play an important role in shaping the gut resistome. For instance, one study demonstrated that high-sugar, high-fat, and high-protein diets independently promote the enrichment and horizontal transfer of ARGs in the mouse gut microbiota by expanding Proteobacteria that harbor mobile resistance elements15. In humans, dietary patterns, such as omnivorous, vegetarian, or vegan diets, have been associated with varying ARG burdens, with vegans and vegetarians showing significantly lower intestinal ARG levels than omnivores16. Moreover, a recent study reported that dietary fiber intake was inversely associated with ARG carriage in healthy U.S. adults, while higher intake of total and saturated fat was positively correlated with the abundance of multidrug resistance genes17. Collectively, these studies support the notion that diet influences the human gut resistome. However, most existing research has focused exclusively on either animal models or observational associations in human cohorts based on food frequency questionnaires. A comprehensive evaluation of the effects of defined dietary patterns on gut resistome—validated in both experimental models and human data—remains lacking.
Herein, we conducted a comprehensive study to investigate the specific effects of two dietary patterns on AMR in the gut microbiome of both mice and humans: high-fat/low-fiber (hereafter referred to as high-fat) and high-fiber/low-fat (hereafter referred to as high-fiber). Our findings strengthen the link between AMR and dietary patterns, suggesting that dietary habits, particularly the high-fat/low-fiber diet (also known as the Western diet), prevalent in high- and middle-income countries, may influence AMR in the human gut microbiota once AMR is acquired. Furthermore, our findings offer a possible solution for reducing or potentially eliminating the gut resistome through dietary interventions.
Results
Diet altered the gut microbial composition in mice
The study design are shown in Fig. 1. Prior to the transition from the basic maintenance (normal) diet, the dominant genera in the three groups of mice (normal, high-fat, and high-Fiber) were Alistipes, Mucispirillum, Lactobacillus, and Bacteroides, which together constituted 80% of the gut microbiota (Fig. 2A and Supplementary Data 1). After switching from the normal diet to either a high-fat or high-fiber diet, both groups exhibited significant changes in alpha diversity, as evaluated by the Shannon index, and in beta diversity, as determined by principal coordinate analysis (PCoA) (Fig. 3A and Supplementary Fig. 1A). In the high-fat group, the relative abundance of Alistipes decreased from 28.71% to 4.85% and Bacteroides from 7.81% to 2.88%. Conversely, Lactococcus, Enterococcus, Anaerotruncus, and Escherichia increased from 0% to 20.55%, 0% to 0.04%, 4.88% to 5.58%, and 0.07% to 0.25%, respectively (Fig. 2B and Supplementary Data 2). In the high-fiber group, Alistipes decreased from 22.74% to 0.8%, while Parabacteroides and Bacteroides increased from 3.07% to 40.37% and from 7.12% to 14.03%, respectively (Fig. 2B and Supplementary Data 3). Similar trends were observed when comparing the high-fat group to the normal diet group, and the high-fiber group to the normal diet group. Lactococcus, Enterococcus, Anaerotruncus, and Escherichia were identified as biomarkers in the high-fat group, while Parabacteroides and Bacteroides were identified as biomarkers in the high-fiber group (Supplementary Fig. 2). These findings underscored the ability of high-fat and high-fiber diets to alter the taxonomic composition of the gut microbiota.
The study was conducted in two stages. First, a mouse experiment was performed to investigate the effect of different diets on the microbial community, resistome, mobilome and virulome. In second stage, we retrieved a human dataset containing complete metagenomics data from healthy individuals, along with dietary and demographic information, to determine whether similar dietary effects on the gut resistome observed in mice could be confirmed in humans. The analysis based on dietary habits and BMI was noted as prat I and part II respectively. Due to the minimal number of 5 individuals with high-fat/low-fiber diet and 11 individuals with obese, we ultimately included 5 and 11 as a minimum sample size of corresponding group for part I and part II analysis, respectively. The remaining groups were matched by gender and age in a 1:2 ratio. If the number of available individuals for matching was less than twice that of the high-fiber or obesity groups, we opted for a 1:1 ratio for comparative analysis.
Microbiota (A, B), ARGs (C, D), VGs (E, F), and MGEs (G, H). Significant between-group differences were detected by LefSe analysis with an LDA threshold score of 2 and a significance level of 0.05. Data are presented as average in bar plots and median with IQR (interquartile range) in box plots; horizontal lines within the boxes represent the first quartile, median, and third quartile, respectively. Whiskers denote the range of values within the first quartile – 1.5× the interquartile range and the third quartile + 1.5× the interquartile range. The Kruskal-Wallis rank sum test was used to determine significance between groups, with *p < 0.05, **p < 0.01, ***p < 0.001, and NS no significance.
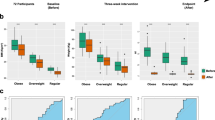
Alpha and beta diversity of the microbiota (A), ARGs (B), VGs (C), and MGEs (D) were accessed before and after switching from a normal diet to a high-fat or high-fiber diet. Data are presented as median with IQR in box plots; horizontal lines within the boxes represent the firstquartile, median, and third quartile, respectively. Whiskers represent the range of values within the first quartile—1.5× the interquartile range and the third quartile + 1.5× the interquartile range. The Wilcoxon rank sum test was used to detect significance in Shannon index differences, with *p < 0.05, **p < 0.01, ***p < 0.001, and NS no significance. Circles represent the 95% confidential interval for the corresponding group in beta diversity, with significant differences detected using PERMANOVA (permutations = 999).
High-fat diet increased the abundances of the resistome, virulome, and mobilome in mice
Prior to dietary transition, the gut resistome in mice mainly comprised genes encoding resistance to tetracycline, vancomycin, macrolide−lincosamide−streptogramin (MLS), bacitracin, and multidrug classes (Fig. 2C, Supplementary Data 4–6). Twenty-one days after switching to a high-fat diet, the total abundance of the resistome increased significantly from 0.14 to 0.25 (ARG/16S rRNA gene ratio; p < 0.001, Supplementary Data 5). In contrast, the high-fiber diet led to a decrease in resistome abundance from 0.14 to 0.09 (p < 0.05) (Fig. 2D and Supplementary Data 6). Distinct patterns in alpha and beta diversity were observed across the groups, indicating significant differences in resistome composition after the dietary change (Fig. 3B and Supplementary Fig. 1B). Notably, the relative abundance of vancomycin resistance genes (vanD, vanG, vanR, and vanS) in the high-fat group increased significantly from 0.019 to 0.071 ARG/16S rRNA gene ratio (p < 0.01, Fig. 2D, Supplementary Fig. 3A, and Supplementary Data 5). Conversely, the high-fiber diet resulted in significant decreases across most ARG categories, including resistance to bacitracin (bacA and bcrA), chloramphenicol (cat), MLS (lsa, vatB, and vatC), and vancomycin (vanD, vanG, vanR, and vanS) (Fig. 2D, Supplementary Fig. 3B, and Supplementary Data 6). These findings suggested that the high-fat diet promoted an increase in resistome abundance, whereas the high-fiber diet reduced it.
Similarly, the virulome—comprising 13 main categories of virulence genes—was significantly affected by diet. In the high-fat group (Supplementary Data 7–9), the virulome abundance increased from 0.56 to 0.91 VG/16S rRNA gene ratio (p < 0.001, Supplementary Data 8), whereas in the high-fiber group, it decreased from 0.58 to 0.50 (p < 0.05) (Fig. 2E, F, Supplementary Fig. 1C, and Supplementary Data 9). Alpha diversity increased significantly in the high-fat group but not in the high-fiber group (Fig. 3C). PCoA revealed distinct changes in beta diversity in the virulome induced by the high-fiber diet (Fig. 3C and Supplementary Fig. 3B). Functional category analysis showed increased abundances of genes associated with adherence, effector delivery system, motility, and immune modulation following the change to a high-fat diet (p < 0.01), along with the emergence of corresponding virulence systems (Fig. 2F, Supplementary Fig. 3C, and Supplementary Data 8). In contrast, the high-fiber diet was associated with decreases in genes related to adherence, biofilm, and stress survival, along with their corresponding virulence systems (Fig. 2F, Supplementary Fig. 3D, and Supplementary Data 9). Overall, these results suggested that the high-fat diet largely altered the virulome by increasing its abundance, while the high-fiber diet exerted a modest reductive effect.
The mobilome, which encompasses all MGEs including plasmids, transposons, and integrons in the microbiome, also showed large changes in response to diet (Fig. 2G, Supplementary Data 10–12). Following the switch from the normal diet, the total relative abundance of the mobilome increased 8-fold (from 0.20 to 1.66 ratio of MGE/16S rRNA gene ratio, Supplementary Data 11) on the high-fat diet, while it decreased from 0.22 to 0.13 on the high-fiber diet (Fig. 2H and Supplementary Data 12). Specifically, the high-fiber diet did not affect plasmid abundance, whereas the high-fat diet increased transposon abundance from 0.09 to 1.26 (MGE/16S rRNA ratio; p < 0.001, Fig. 2H). Further analyses revealed increases in the abundances of intl1, int2, Tn916-orf6, Xis-Tn916, and IS91 in the high-fat group, with corresponding decreases in the high-fiber group (Supplementary Fig. 3E, F, Supplementary Data 11 and 12). Although alpha diversity of the mobilome did not show significant differences after the diet change (Fig. 3D), PCoA of beta diversity indicated distinct gene clustering in the high-fat group compared to the high-fiber and normal groups (Fig. 3D and Supplementary Fig. 1D). Collectively, these findings highlighted the profound impact of a high-fat diet on the mobilome.
Changes in ARGs and VGs were closely related to changes in host bacteria in mice
We used assembled contigs to evaluate the host bacteria carrying specific ARGs and VGs. Prior to the diet change, Bacteroides and Alistipes were identified as hosts for both fosmidomycin resistance gene rosA and tetracycline resistance gene tet37. Anaerotruncus hosted vancomycin resistance genes, while Lactobacillus was the primary host for the multidrug resistance gene mdtG (Fig. 4A and Supplementary Data 13). Most host bacteria–ARG relationships remained unchanged following high-fat diet feeding, however, Lactobacillus, Lactococcus, and Parabacteroides emerged as new hosts for certain ARGs (Supplementary Fig. 4A and Supplementary Data 14). Notably, vanG and vanY were absent in Anaerotruncus after high-fiber diet feeding (Supplementary Fig. 4B and Supplementary Data 15), suggesting a potential elimination of these host bacteria under the high-fiber diet (Fig. 2A). Changes in both the relationship and abundance of host bacteria and ARGs were observed in the high-fat and high-fiber groups (Fig. 4B, C). Regarding VGs, Alistipes was associated with capsular polysaccharide, type III secretion system effectors, and type VI secretion system-related VGs, while Anaerotruncus was linked with capsule-related VGs, and Bacteroides was associated with capsular polysaccharide and capsule-related VGs prior to the diet change (Fig. 4D and Supplementary Data 16). Similar to ARGs, both increased and decreased abundances of VGs and their related host bacteria were observed following high-fat and high-fiber diet feeding, respectively (Fig. 4E, F, Supplementary Data 17 and 18). Additionally, the presence or absences of VGs in their corresponding host bacteria were also noted in both experimental diet groups (Supplementary Fig. 4C, D).
Bacterial taxonomy and ARGs (A–C), bacterial taxonomy and VGs (D–F), MGEs and ARGs (G–I), MGEs and VGs (J–L). Chord plots depict the distribution of ARGs/VGs linked with taxonomic genera or MGEs, with arch size representing the total number of linked items. In heatmap plot, the filled/empty box represents bacteria carrying/non-carrying corresponding ARGs; the top bar plot represents the relative abundance of MGEs or bacterial taxonomy, and the right bar plot represent the relative abundance of ARGs or VGs.
Increased MGEs were associated with increases in the corresponding ARGs and VGs in mice
Given the important role of HGT in enriching the resistome and virulome, we examined the networks between MGEs and ARGs/VGs. The ARGs were mainly associated with intl1, IS91, ISBf10, Tn916-orf6, tnpA-related transposon, and Xis-Tn916 (Fig. 4G and Supplementary Data 19). Most ARGs and their corresponding MGEs exhibited increased abundances following high-fat diet feeding but decreased after high-fiber diet feeding (Fig. 4H, I, Supplementary Fig. 5A,B, Supplementary Data 11, 12, 20 and 21). Notably, Tn916-orf6 was mainly associated with genes encoding resistance to vancomycin and tetracycline, and its abundance increased significantly after high-fat diet feeding (Fig. 4H, Supplementary Fig. 3C, Supplementary Data 5, 11, and 20). The abundance of tnpA-related transposons dramatically increased in the high-fat group, while the associated ARGs only slightly increased, indicating a potential but unclear association between tnpA and other enriched ARGs (Fig. 4H, Supplementary Data 5, 11, and 20). In the high-fiber group, both MGEs and their associated ARGs generally decreased in abundance, except for class A β-lactamase and its host vector ISBf10, which showed increased abundances (Fig. 4I, Supplementary Data 6, 12, and 21).
We also explored the relationship between MGEs and VGs before and after the dietary change (Fig. 4J, Supplementary Fig. 5C, D, Supplementary Data 22–24). Although the relationship between MGEs and VGs appeared more complex than those between MGEs and ARGs, similar trends were observed following the change to high-fat and high-fiber diet feeding (Fig. 4K, L, Supplementary Data 22–24). Notably, the abundances of capsule-related VGs increased after high-fiber diet feeding, while the abundances of their four associated host vectors (Xis-Tn916, tnpA, Tn916-orf6, and IS91) decreased, with the exception of an increase in ISBf10. These results suggested that ISBf10 may serve as the primary host vector for capsule-related VGs (Fig. 4L, Supplementary Data 9, 12 and 24).
Distinct energy source use by gut microbiota in high-fat and high-fiber groups in mice
We analyzed gene function within the microbiome to further explore the relationship between diet and microbial metabolic activity. Genes related to membrane transport, including phosphotransferase system and ABC transporters involved in carbohydrate uptake, were enriched in response to either the high-fat or high-fiber diet intervention (Supplementary Fig. 6). After high-fat diet feeding, the abundances of genes associated with fatty acid degradation and starch and sucrose metabolism significantly increased, likely due to the high lard and maltodextrin content in the high-fat diet (Supplementary Fig. 6A). In contrast, after high-fiber diet feeding, genes involved in glycan degradation and starch and sucrose metabolism became more abundant, likely reflecting the higher starch and cellulose content in the high-fiber diet (Supplementary Fig. 6B).
High-fat diet and obesity increase human gut resistome and mobilome
We investigated the resistome and mobilome in the human population from the perspectives of dietary habits and BMI (Fig. 1). In terms of resistome, genes encoding MLS, beta-lactam resistance and multidrug resistance were predominant in the human gut (Fig. 5A, E, Supplementary Data 25–30). Notably, the total abundance of the resistome in the high-fat population was significantly higher than in the high-fiber and normal diet populations (Supplementary Fig. 7A). Specifically, the relative abundances of genes conferring resistance to cephalosporin (blaTME-136, 7.31 × 10−6 vs 0.00, p < 0.05), MLS (lsa, 2.42 × 10−3 vs 9.56 × 10−4, p < 0.05) and aminoglycoside (aph(3”‘)-III, 7.19 × 10−3 vs 1.90 × 10−3, p < 0.05) were higher in individuals consuming a high-fat diet compared to those on a normal diet (Supplementary Data 31). A similar trend was observed in the obesity group (Supplementary Fig. 7B), where the relative abundance of genes associated with resistance to cephalosporin (blaTME-127, 3.25 × 10−6 vs 0.00, p < 0.05), phenicols-lincosamides-oxazolidinones-pleuromutilins-streptogramin A (cfr, 1.54 × 10−4 vs 1.80 × 10−5, p < 0.05), and tigecycline (tet(X), 2.68 × 10−3 vs 5.95 × 10−4, p < 0.05) were higher in individuals with obesity compared to those with a healthy BMI (Supplementary Data 32). Although Shannon diversity of ARGs showed no significant difference among the groups (Fig. 5B, F), the Bray-Curtis distance revealed distinct patterns based on dietary habits (Fig. 5C). Specifically, genes encoding resistance to tetracycline, vancomycin, and aminoglycoside resistance were enriched in the high-fat diet/obesity population (Fig. 5D, H). Regarding the mobilome, the total abundance of MGEs was higher in the high-fat/obesity population compared to the normal diet/healthy BMI population (Supplementary Fig. 8).
Dietary habits (A–D) and BMI (E–H). Data are presented as average in bar plots and median with IQR in box plots; horizontal lines within the boxes represent the first quartile, median, and third quartile, respectively. Whiskers denote the range of values within the first quartile—1.5× the interquartile range and the third quartile + 1.5× the interquartile range. The Wilcoxon rank sum test was used to detect significance between groups, with * p < 0.05, ** p < 0.01, *** p < 0.001, and NS no significance. Circles represent the 95% confidential interval for the corresponding group, and PERMANOVA (permutations = 999) was used to detect significant differences between groups.
ARG in dietary habits (A) and BMI categories (B), relationship in dietary habits (C) and BMI categories (D). The Bar plot at the top shows the relative abundance of ARG hosts at genus level. The bar plot on the right shows the relative abundance of ARGs. A correlation value of 1 indicates that the bacteria carry the corresponding ARGs, while a value of 0 indicates the absence of these ARGs.
We also detected the ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) in each group. The results showed that the total abundance of the genera Enterococcus, Staphylococcus, Klebsiella and Pseudomonas (ESKP) was higher in the high-fat and obesity group compared to the normal and healthy group (Supplementary Fig. 9). In terms of ARGs, the ESKP pathogens were the main host of ARGs, and the total abundance of ESKP-carrying ARG contigs in the high-fat population was significantly higher than in the high-fiber and normal diet populations, with an average abundance of 710.25, 89.37 and 133.48 TPM, respectively. Similarly, the total abundance of ESKP-carrying ARG contigs in the obesity population was higher than in the healthy population (1028.72 versus 158.96 TPM) (Fig. 6A, B). Notably, Klebsiella sp., which had the highest abundance among ESKP in different diet populations, mainly carried fosfomycin (fosA) and beta-lactam (blaSHV and penA) resistance genes (Fig. 6C, D, Supplementary Fig. 9, Supplementary Data 33 and 34). Staphylococcus sp. was associated with tetracycline resistance genes (tetM and tetL), while Enterococcus sp. was associated with tetracycline (tetM, tetL, and tetW), pleuromutilin–lincosamide–streptogramin A (lsa), and florfenicol (fexB) resistance genes. All these ARGs were more abundant in the high-fat diet/obesity population compared to the normal diet/healthy BMI population (Fig. 6C, D, Supplementary Fig. 9, Supplementary Data 33 and 34).
Discussion
The dissemination and persistence of resistome in the human gut microbiome are influenced by a variety of factors, such as lifestyle18,19, genetic background20 and antibiotic usage21,22,23. Among these, antimicrobial usage, the most well-explored driver, could shape the gut microbiome and resistome in both humans and animals22,23. Diet has emerged as another important determinant of gut microbial structure and function, with numerous studies demonstrating the role of the diet in gut microbial composition and its implications for human health7,24,25, including potential impacts on the composition of the gut resistome26. While contaminated vegetables and minimally processed foods have been suggested as potential contributors to the human gut resistome27, few reports have directly demonstrated the impact of diet on the abundance of gut resistome in human15,16. Our findings revealed that a high-fat/low-fiber diet in mice not only dramatically increased the abundance of the resistome but also enhanced the virulome and mobilome. In contrast, a high-fiber/low-fat diet may exert a modest opposing effect. Notably, metagenomic data from human stool samples confirmed the increased abundance of resistome in individuals with a high-fat diet or obesity. Based on comprehensive network analyses, we proposed two possible explanations for these changes: (1) the different nutrients provided by the two diets altered the microbial composition of the gut, leading to corresponding increases or decreases in ARGs, VGs, and MGEs located on bacterial chromosome; and (2) the high-fat diet enhanced the abundance of MGEs, thereby accelerating HGT within the microbiota, resulting in the increased abundances of ARGs and VGs carried by these MGEs. Although ARGs are mainly carried by commensal bacteria, which serve as HGT hotspots in the gut microbiome28,29,30 and do not directly cause human disease, their acquisition by pathogenic bacteria can reduce the efficacy of corresponding antibiotics and pose a threat to human health. In fact, the transfer of mobile ARGs between commensals and pathogens has been observed within individual gut microbiomes31,32.
Excessive fat consumption is recognized for its harmful effects on gut health, including dysbiosis, gut barrier dysfunction, and increased intestinal permeability, which may lead to low-grade systemic inflammation33. In our study, in addition to the growing resistome abundance, a significant increase in virulome abundance was observed following high-fat/low-fiber diet feeding in mice. Specifically, functional virulence categories related to adherence, effector delivery systems, motility, and immune modulation showed prominent increases. These specific virulence systems may support the survival of bacteria in the altered gut environment induced by the high-fat diet. For example, we observed an increased abundance of genes associated with capsular polysaccharide (CPS) production. CPS has been reported to enhance bacterial resilience by forming a protective barrier against hostile gut conditions, such as elevated bile acid levels that are commonly induced by high-fat diets34,35. This structural adaptation may confer a survival advantage to specific bacterial taxa, enabling them to persist and proliferate under dietary stress. As a result, bacteria harboring chromosomally encoded ARGs may be ecologically favored, leading to the co-selection of ARGs and virulence-associated traits. Although we did not directly assess inflammation-related factors, previous studies have demonstrated that a high-fat diet can induce gut inflammation36,37, which in turn has been shown to enhance HGT within the human gut microbiome15,38. These connections between diet-induced inflammation and increased HGT may help explain the dramatic increase in MGEs observed in our study following high-fat/low-fiber diet feeding.
The pathogens are typically associated with virulence genes, which help them colonize host intestine and causes diseases39. Our study revealed that the abundance of the ESKP genera, along with their harbored ARGs, was higher in individuals with a high-fat diet and obesity compared to those with normal diet and healthy BMI. This finding aligned with previous studies that reported a higher abundance of Klebsiella and Enterococcus in population consuming a high-fat diet or those with obesity40,41. The ESKAPE pathogens are the leading cause of nosocomial infections and pose the highest challenges in clinical practice worldwide. The findings of this study suggested that individuals with a high-fat diet or obesity may be at increased risk for infectious diseases caused by ESKP pathogens with higher abundance of ARGs.
Similar to high-fat diets, high-sugar and high-protein diets have also been linked to an increased abundance and transfer of ARGs among gut microbiota15. However, the impact of a high-fiber diet on ARGs is less well understood. Individuals consuming diet richer in dietary fiber were proved to have lower abundance of ARGs17. This is further supported by evidence showing a reduced abundance of ARGs in individuals following a vegan diet, which is rich in dietary fiber, compared to omnivores and vegetarians16. While our study aligned with these previous reports indicating that high-fiber diets are associated with lower ARG abundance, it extended the understanding by showing a concomitant decrease in virulome and mobilome, which has been less explored previously. This suggested a broader protective effect of a high-fiber diet against the emergence and spread of AMR, supporting the hypothesis that dietary fiber not only impacts gut microbiota composition but also reduces the overall genomic potential for virulence and resistance. This hypothesis is reinforced by our prior study, which showed that increased consumption of whole grains, a high-fiber diets, provided a protective effect against the colonization of mcr-1-positive E. coli, known for its resistance to colistin, a critical-important antibiotic in human medicine42. Dietary fiber is well-known for its health benefits, particularly in alleviating gut inflammation6. This protective effect is likely due to the fermentation of dietary fiber by gut microbiota, leading to the production of SCFAs that reduce gut pH and enhance gut barrier function, thereby reducing inflammation6. In our study, the observed reductions in the resistome and mobilome with a high-fiber diet, although not directly equivalent, may contribute to this protective effect by reducing inflammation and hindering HGT in the gut microbiome. Additionally, the observed reductions were relatively modest, and caution is warranted in interpreting them as definitive evidence of a suppressive effect of dietary fiber. Part of the decrease in ARGs, VGs, and MGEs may have resulted from general physiological stress associated with dietary shift, rather than from fiber-specific effects. Sudden dietary changes are known to transiently perturb gut microbial community and diversity, which can non-specifically influence functional gene profiles. Therefore, further studies are needed to elucidate the fiber or fiber-associated components affecting gut resistome.
We acknowledge several limitations in this study. First, although our study provided the overall changes in the gut microbiota, resistome, virulome, and mobilome associated with a high-fat/low-fiber and high-fiber/low-fat diet in a mouse model, the mouse gut resistome may not fully represent all clinically-relevant ARGs found in human populations. To address this limitation, we supplemented our findings with human stool samples, which confirmed similar patterns in the high-fat/high-fiber diet and healthy/obesity populations. Second, although we used assembly methods to determine the relationships between different genetic components, the exact genomic context of these components could not be fully elucidated due to the limitations of next-generation sequencing technologies, which produce relatively short reads. Future studies employing long-read sequencing technologies, such as PacBio Single Molecule Real-Time sequencing or Oxford Nanopore sequencing, may provide more comprehensive information on the genetic context of these components43.
In conclusion, our study demonstrated an increase in the abundance of the resistome in both high-fat diet-induced mice and humans with similar dietary habits. Our findings suggested that a high-fat/low-fiber diet, akin to a typical Western diet, may increase the risk of AMR development in the gut microbiome. Therefore, public health strategies should consider dietary interventions, particularly the reduction of high-fat/low-fiber diets, as a potential approach to mitigate the development and spread of AMR in humans. Further, promoting high-fiber diets could play a crucial role in reducing the burden of AMR, thereby enhancing the efficacy of antimicrobial treatments.
Methods
Animal study design
This study was conducted in two stages, as illustrated in Fig. 1. In the first stage, 21 mice (C57BL/6 J, Charles River, Beijing, China), aged 7 to 8 weeks, were used. All mice were bred under specific pathogen-free (SPF) conditions in individually ventilated cages at the Shenzhen Center for Disease Control and Prevention. Following a 14-day quarantine and acclimation period, the mice were randomly assigned to three dietary groups: a basic maintenance diet (D12450J, Research Diet Company, New Brunswick, USA, also called normal diet), a high-fat/low-fiber diet (D12492, Research Diet Company, New Brunswick, USA), and a high-fiber/low-fat diet (Diet SF11-029, Specialty Feed, Great Eastern Highway Glen Forrest, WA). Fecal samples were collected at two time points: immediately prior to dietary intervention (pre-change) and at the end of the 21-day feeding period (post-change). At the conclusion of the experiment, mice were euthanized by cervical dislocation. All animal experiments were reviewed and approved by the Committee on Animal Welfare and Experiment Ethics at China Agricultural University (Approval number: CAU20190326-2).
Human population study design
In the second stage, we retrieved metagenomics and questionnaires data from our previous project42 to assess the impact of dietary habits and body mass index (BMI) on the human gut resistome. A total of 199 entries were available, each with complete metagenomics sequencing data and corresponding questionnaires. We included data from participants with different dietary patterns (high-fat, high-fiber, and normal diet) and BMI categories based on previous study guidelines44,45. Initially, we retained 103 individuals after excluding those who had undergone surgery, used painkillers, antibiotics, and insulin, or had enterelcosis or missing BMI information. Based on dietary habits (noted as part I), we identified 54 individuals consuming a normal diet, 5 individuals consuming a high-fiber/low-fat diet, and 44 individuals consuming a high-fat/low-fiber diet. For BMI (noted as part II), 60 participants were classified as healthy, 32 as overweight, and 11 as obese. Given the small number of individuals in the high-fiber/low-fat diet (n = 5) and obese (n = 11) groups, we used these as the minimum sample sizes for comparison in Part I and Part II, respectively. The remaining groups were matched by gender and age in a 1:2 ratio. If the number of available individuals for matching was less than twice that of the high-fiber or obesity groups, we opted for a 1:1 ratio for comparative analysis (Fig. 1). Notably, in the second stage, part I and part II were undertaken separately, however, the cases included may have overlap between these two distinguished selection criteria, which does not affect the final results and conclusions. The metagenomics and questionnaire data from human were obtained from our previous project42, and the ethical approval (R2018021) was granted by the ethics committee of the Shenzhen CDC.
DNA extraction, metagenomic sequencing, and quality analysis
Mouse fecal samples were used for DNA extraction with the MoBio PowerFecal DNA Isolation Kit (MoBio Laboratories, Carlsbad, CA, USA), following the manufacturer’s protocol with a slight modification that the amount of input sample was reduced from the recommended 0.5 g to 0.1 g due to the limited quantity of feces collected from mouse. DNA libraries were constructed using the Illumina TruSeq® DNA Library Preparation Kit (Illumina, San Diego, CA, USA), and shotgun metagenomic sequencing was performed on the Illumina NovaSeq 6000 platform with 150 bp paired-end reads (BerryGenomics, Beijing, China). Raw metagenomic reads were processed using KneadData (https://github.com/biobakery/kneaddata, version 0.10.0), which integrates with trimmomatic and bowtie2 to remove Illumina adapters, trim low-quality reads, and filter out host-derived reads by aligning to mouse (C57BL) and human (GRCh38) reference genomes.
Bioinformatics analysis
The taxonomic composition of the metagenomes was profiled using HUMANN2 (version 0.11.1)46. Linear discriminant analysis effect size (Lefse, version 1.0.7) was employed to identify different taxa between pre-diet and post-diet samples47. The abundance of ARGs, VGs, and MGEs was calculated using ARGs-SOP (version 2.0) with default parameters and normalized to 16S rRNA gene copy number48. The ARG database was used the default database in ARGs-OAP with minor modifications, and the VGs and MGEs databases were constructed based on Virulence Factor Database (VFDB, http://www.mgc.ac.cn/VFs/) and Mobile Genetic Element Database (https://github.com/KatariinaParnanen/MobileGeneticElementDatabase). All above databases were created a public link to access (https://github.com/zzsunday/High-fat-and-low-fiber-diet-elevates-the-gut-resistome-a-comparative-metagenomic-study). The Shannon diversity indices for taxonomy, ARGs, VGs and MGEs were calculated using the diversity function in the R package vegan (version 3.6.1)49. Clean sequence data were assembled using metaSPAdes (version 3.9.0)50 with default parameters, and contigs longer than 5000 bp were retained for taxonomy annotation and further analysis. Taxonomic assignment of human- and mouse-derived microbial contigs was performed using Kraken2 (version 2.1.3) and MMseqs2 (version 14.5), based on default database and a self-constructed non-redundant database, respectively51,52. All labeled contigs were aligned to SARG 2.2 database or the VFDB to determine the relationship between host bacteria and ARGs/VGs. For MGEs, contigs were first aligned to the MGEs database, and then MGEs-containing contigs were aligned to the SARG 2.2 database or VFDB to elucidate the relationship between MGEs and ARGs/VGs. Alignments with an e-value < 1e − 6 were retained. The relative abundance of KEGG pathways was obtained using HUMANN2 (version 0.11.1), which maps UniRef90 gene families to KO46. The abundance of contigs carrying ARGs was quantified using Salmon (version 0.8.1) and presented as Transcripts Per Million (TPM)53.
Statistical analysis
The Wilcoxon rank-sum test, combined with the Benjamin-Hochberg method for multiple testing correction, was used to assess significant differences in the abundances of ARGs, VGs, and MGEs between pre-diet and post-diet samples. The non-parametric Kruskal-Wallis rank sum test was applied to detect significant differences in genus-level abundance across different groups. Significant differences are indicated in the figures as follows: * p < 0.05, ** p < 0.01, *** p < 0.001. Principal coordinates analysis (PCoA) was performed to evaluate the dissimilarities in the microbial community, resistome, virulome and mobilome. The significance of β-diversity between groups was determined using PERMANOVA, implemented in the vegan package within the Adonis function49. All figures were generated using the R statistical software package (version 3.6).
Data availability
The Raw sequenced data have been deposited in the National Center for Biotechnology Information (NCBI) under BioProject number PRJNA948687 and PRJNA1191677.
References
Dalvi, P. S. et al. High fat induces acute and chronic inflammation in the hypothalamus: Effect of high-fat diet, palmitate and tnf-alpha on appetite-regulating npy neurons. Int J. Obes. (Lond.). 41, 149–158 (2017).
Christ, A. et al. Western diet triggers nlrp3-dependent innate immune reprogramming. Cell 172, 162–175.e14 (2018).
Hryckowian, A. J. et al. Microbiota-accessible carbohydrates suppress Clostridium difficile infection in a murine model. Nat. Microbiol. 3, 662–669 (2018).
Li, J. et al. An obligatory role for neurotensin in high-fat-diet-induced obesity. Nature 533, 411–415 (2016).
Schulz, M. D. et al. High-fat-diet-mediated dysbiosis promotes intestinal carcinogenesis independently of obesity. Nature 514, 508–512 (2014).
Swann, O. G. et al. Dietary fiber and its associations with depression and inflammation. Nutr. Rev. 78, 394–411 (2020).
Zmora, N., Suez, J. & Elinav, E. You are what you eat: diet, health and the gut microbiota. Nat. Rev. Gastroenterol. Hepatol. 16, 35–56 (2019).
Collaborators GBDAR. Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet 404, 1199–1226 (2024).
Brinkac, L. et al. The threat of antimicrobial resistance on the human microbiome. Micro. Ecol. 74, 1001–1008 (2017).
Woolhouse, M. et al. Antimicrobial resistance in humans, livestock and the wider environment. Philos. Trans. R. Soc. Lond. B Biol. Sci. 370, 20140083 (2015).
McInnes, R. S. et al. Horizontal transfer of antibiotic resistance genes in the human gut microbiome. Curr. Opin. Microbiol. 53, 35–43 (2020).
Huddleston, J. R. Horizontal gene transfer in the human gastrointestinal tract: potential spread of antibiotic resistance genes. Infect. Drug Resist. 7, 167–176 (2014).
Wang, C., Li, Q. & Ren, J. Microbiota-immune interaction in the pathogenesis of gut-derived infection. Front Immunol. 10, 1873 (2019).
Tamburini, F. B. et al. Precision identification of diverse bloodstream pathogens in the gut microbiome. Nat. Med. 24, 1809–1814 (2018).
Tan, R. et al. High-sugar, high-fat, and high-protein diets promote antibiotic resistance gene spreading in the mouse intestinal microbiota. Gut Microbes 14, 2022442 (2022).
Losasso, C. et al. Assessing antimicrobial resistance gene load in vegan, vegetarian and omnivore human gut microbiota. Int. J. Antimicrob. Agents 52, 702–705 (2018).
Oliver, A. et al. Association of diet and antimicrobial resistance in healthy U.S. Adults. mBio 13, e0010122 (2022).
D’Souza, A. W. et al. Destination shapes antibiotic resistance gene acquisitions, abundance increases, and diversity changes in Dutch travelers. Genome Med. 13, 79 (2021).
Groussin, M. et al. Elevated rates of horizontal gene transfer in the industrialized human microbiome. Cell 184, 2053–67.e18 (2021).
Patangia, D. V. et al. Vertical transfer of antibiotics and antibiotic resistant strains across the mother/baby axis. Trends Microbiol. 30, 47–56 (2022).
Yip, A. Y. G. et al. Antibiotics promote intestinal growth of carbapenem-resistant enterobacteriaceae by enriching nutrients and depleting microbial metabolites. Nat. Commun. 14, 5094 (2023).
Mencia-Ares, O. et al. Antimicrobial use and production system shape the fecal, environmental, and slurry resistomes of pig farms. Microbiome 8, 164 (2020).
Reyman, M. et al. Effects of early-life antibiotics on the developing infant gut microbiome and resistome: a randomized trial. Nat. Commun. 13, 893 (2022).
Beam, A., Clinger, E. & Hao, L. Effect of diet and dietary components on the composition of the gut microbiota. Nutrients https://doi.org/10.3390/nu13082795 (2021).
Bibbo, S. et al. The role of diet on gut microbiota composition. Eur. Rev. Med. Pharm. Sci. 20, 4742–4749 (2016).
Baron, S. A., Diene, S. M. & Rolain, J.-M. Human microbiomes and antibiotic resistance. Hum. Microbiome J. 10, 43–52 (2018).
da Silva, S. F. et al. Influence of human eating habits on antimicrobial resistance phenomenon: aspects of clinical resistome of gut microbiota in omnivores, ovolactovegetarians, and strict vegetarians. Antibiotics (Basel) https://doi.org/10.3390/antibiotics10030276 (2021).
Carr, V. R. et al. Abundance and diversity of resistomes differ between healthy human oral cavities and gut. Nat. Commun. 11, 693 (2020).
Crits-Christoph, A. et al. Good microbes, bad genes? The dissemination of antimicrobial resistance in the human microbiome. Gut Microbes 14, 2055944 (2022).
Gill, S. R. et al. Metagenomic analysis of the human distal gut microbiome. Science 312, 1355–1359 (2006).
Forster, S. C. et al. Strain-level characterization of broad host range mobile genetic elements transferring antibiotic resistance from the human microbiome. Nat. Commun. 13, 1445 (2022).
Kent, A. G. et al. Widespread transfer of mobile antibiotic resistance genes within individual gut microbiomes revealed through bacterial hi-c. Nat. Commun. 11, 4379 (2020).
Malesza, I. J. et al. High-fat, western-style diet, systemic inflammation, and gut microbiota: a narrative review. Cells https://doi.org/10.3390/cells10113164 (2021).
Zhang, L. et al. Milk fat globule membrane protects Lactobacillus rhamnosus gg from bile stress by regulating exopolysaccharide production and biofilm formation. J. Agric Food Chem. 68, 6646–6655 (2020).
Yokota, A. et al. Is bile acid a determinant of the gut microbiota on a high-fat diet? Gut Microbes 3, 455–459 (2012).
Crawford, M. et al. Six-week high-fat diet alters the gut microbiome and promotes cecal inflammation, endotoxin production, and simple steatosis without obesity in male rats. Lipids 54, 119–131 (2019).
Kim, S. J. et al. Dietary fat intake and age modulate the composition of the gut microbiota and colonic inflammation in c57bl/6j mice. BMC Microbiol. 19, 193 (2019).
Stecher, B. et al. Gut inflammation can boost horizontal gene transfer between pathogenic and commensal enterobacteriaceae. Proc. Natl Acad. Sci. USA 109, 1269–1274 (2012).
Khater, F. et al. In silico analysis of usher encoding genes in klebsiella pneumoniae and characterization of their role in adhesion and colonization. PLoS ONE 10, e0116215 (2015).
Zhang, Z. et al. Lycium barbarum polysaccharide attenuates myocardial injury in high-fat diet-fed mice through manipulating the gut microbiome and fecal metabolome. Food Res. Int. 138, 109778 (2020).
Hou, Y. P. et al. Human gut microbiota associated with obesity in chinese children and adolescents. Biomed. Res. Int. 2017, 7585989 (2017).
Lv, Z. et al. Prevalence and risk factors of mcr-1-positive volunteers after colistin banning as animal growth promoter in China: a community-based case-control study. Clin. Microbiol. Infect.28, 267–272 (2022).
Tedersoo, L. et al. Perspectives and benefits of high-throughput long-read sequencing in microbial ecology. Appl. Environ. Microbiol. 87, e0062621 (2021).
Krisanits, B. et al. Pubertal mammary development as a “susceptibility window” for breast cancer disparity. Adv. Cancer Res. 146, 57–82 (2020).
Akbar, A. & Shreenath, A. P. High fiber diet. Statpearls, Treasure Island (FL) ineligible companies. Disclosure: Aparna Shreenath declares no relevant financial relationships with ineligible companies. Retreived from https://www.ncbi.nlm.nih.gov/pubmed/32644459.
Franzosa, E. A. et al. Species-level functional profiling of metagenomes and metatranscriptomes. Nat. Methods 15, 962–968 (2018).
Segata, N. et al. Metagenomic biomarker discovery and explanation. Genome Biol. 12, R60 (2011).
Yang, Y. et al. Args-oap: Online analysis pipeline for antibiotic resistance genes detection from metagenomic data using an integrated structured arg-database. Bioinformatics 32, 2346–2351 (2016).
Dixon, P. Vegan, a package of R functions for community ecology. J. Veg. Sci. 14, 927–930 (2003).
Bankevich, A. et al. Spades: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 19, 455–477 (2012).
Mirdita, M. et al. Fast and sensitive taxonomic assignment to metagenomic contigs. Bioinformatics 37, 3029–3031 (2021).
Wood, D. E. & Salzberg, S. L. Kraken: Ultrafast metagenomic sequence classification using exact alignments. Genome Biol. 15, R46 (2014).
Patro, R. et al. Salmon provides fast and bias-aware quantification of transcript expression. Nat. Methods 14, 417–419 (2017).
Acknowledgements
The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. This work was supported in part by grants from the National Key Research and Development Program of China (2022YFD1800400), the NSFC (32141002 and 81991535) and the 2115 Talent Development Program of China Agricultural University.
Author information
Authors and Affiliations
Contributions
Y.S., Z.L. and Y.W. designed the study. K.C., Z.L., J.J., D.Y.S., L.Y., C.S. and D.L. collected data. Y.S., D.S., Z.L., Y.W., Y.K., C.W., J.P., T.R.W. and J.S. analyzed and interpreted the data. Y.S., D.S. and Y.W. wrote the paper. All authors reviewed, revised and approved the final report.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shen, Y., Sun, D., Chen, K. et al. High-fat and low-fiber diet elevates the gut resistome: a comparative metagenomic study. npj Biofilms Microbiomes 11, 156 (2025). https://doi.org/10.1038/s41522-025-00799-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41522-025-00799-3