Abstract
This population-based longitudinal cohort study examines the association between ambient air pollution (PM2.5 and NO2) and Parkinson’s disease (PD) using a 28% representative sample of Northern Ireland’s population (2009–2016). We matched complete address records to annual average PM2.5 and NO2 concentrations at a 1 km grid level and tracked PD onset via first receipt of PD medication. After controlling for confounding factors at individual, household, and neighbourhood levels, we found no association between medium-term PM2.5 or NO2 exposure and PD onset in the overall cohort, over-50s, or sex-stratified samples. However, a positive association was observed between PM2.5 exposure and PD onset in those under 50 in 2011, with weaker evidence for NO2. We discuss potential etiological and non-etiological explanations for this age-related difference.
Similar content being viewed by others
Introduction
The Global Burden of Disease (GBD) study reported that 8.5 million people globally had Parkinson’s disease (PD) in 2019, with cases growing due to aging populations, showing a 145% increase between 1990 and 20161. In the United Kingdom (UK), PD prevalence for people over 20 in 2018 was 145,519, with a lifetime diagnosis risk of 2.7%. Incidence is expected to rise above 21,000 annually by 2025, alongside an 18% rise in prevalence2. In the United States (US) incidence rates for individuals aged 65+ range from 108 to 212 per 100,000, and from 47 to 77 per 100,000 for those aged 45+3. Understanding modifiable determinants of PD could help to mitigate this growing problem.
The etiology of PD remains unclear, with interactions between environmental and genetic factors implicated. Some emerging evidence links ambient air pollution, including particulate matter with a diameter of 2.5 micrometres or less (PM2.5) and nitrogen dioxide (NO2) to PD4. Ambient air pollution may contribute directly through neuro-inflammation and oxidative stress5 or indirectly through cardiovascular health6,7,8,9,10 or cerebrovascular disease11. Other risk factors include dairy products, pesticides, high body mass index, diabetes, cancer, and brain injury12.
The detrimental impact of air pollution on health in general has garnered significant attention in recent years13,14. Studies specifically on ambient air pollution and PD vary, examining pollutants such as PM2.5 and PM104,13,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31, as well as SO2, NO2, NOx, CO and Ozone4,19,21,32,33,34 and airborne metals such as lead, copper and manganese17,35,36.
Results are mixed, as evidenced by recent meta-analysis20,29,37, with some papers showing strong statistical associations4,23,32,35,36, while others have found weak or no associations16,19,21,31,34,38. This mixed picture is also reflected in the few studies that have estimated multipollutant models4,30,39. Variation in study context, exposure durations, and outcome measures likely contributes to these discrepancies27,29. For example, studies have restricted estimations to older age groups19,26 or younger4,16. Exposure over the short-term (<8 days)23, medium-term (≈1 year)40, and long-term (>2 years)22 has been analysed. Outcomes include self-reported PD cases, sometimes with verification from neurologists16,21,31,38; PD drug prescriptions19,33; cases from hospital or administrative databases4,21,22,23,24,26,30,32,37; and in one recent case, PD-related mortality collected from mortality registries30. But research findings have been mixed even within similar study types and contexts. Supplementary Table 1 in the Supplemental Content provides further details.
In this paper, we studied this question using new data from a large and nationally representative cohort tracked over an extended period. Specifically, we tracked a 28% representative sample of the Northern Ireland population between 2009 and 2016, with complete address records matched to annual average data on PM2.5 and NO2 concentrations at the 1 km grid-square level, with PD onset proxied by receipt of the first prescription for PD-related medication. Because studies suggest sex differences in PD pathophysiology (e.g., the role of oestrogen)41 and etiological differences in early versus late PD onset42, we also analysed associations by age and sex38,40. The study makes several distinctive contributions to the literature: it is the first to examine this association within Northern Ireland, a comparatively low-pollution context; our models account for delays in PD diagnoses, typically thought to range between 11 and 13 months43, but often overlooked in the existing literature; and it is one of very few studies to use prescription-based outcome measures or include subsample analyses by age and sex in the air pollution and PD literature.
Results
Our main analysis sample was composed of a total of 292,925 individuals, from which 3089 started receiving medication for PD during the analysis period for our preferred model, i.e., at some point between 2012 semester 1 and 2016 semester 2 inclusive, or until such time as they attrited from the sample through death or emigration.
There were clear differences in observed 2011 characteristics between those who did and did not subsequently receive PD medication (see Table 1). For example, compared to those not experiencing PD onset over this period, those experiencing PD onset were more likely to be older; female; born in Northern Ireland; without educational qualifications; to report poor general health in the 2011 Census; to be inactive or unemployed; to be divorced/separated/widowed or never married; to have no dependent children in the household; to have no cars in the household; and to live in more deprived neighbourhoods. In other words, there was a clear age/sex/disadvantage contrast between the two groups. When comparing exposure to pollutants over the analysis period, those experiencing PD onset were found to be exposed to broadly similar levels of PM2.5 and NO2 on average compared to those not experiencing PD onset, with only slightly higher (lower) percentages in the highest (lowest) quartiles of the relevant exposure distributions.
Table 2 presents our preferred Cox Proportional Hazard (CPH) model estimates for the effects of medium-term exposure to PM2.5 (Panel A) and NO2 (Panel B) on the onset of PD for the whole sample with 6-month exposures lagged 1 year. Model 1 estimates are unadjusted with no conditioning on measured characteristics, while Model 2 estimates are adjusted for measured individual, household and neighbourhood characteristics as listed in Table 1. Full results for Model 2 are presented in Supplementary Table 2.
Despite some evidence of an association between PD onset and lagged PM2.5 exposure in the unadjusted models (Table 2, Model 1, Panel A), there was no such evidence in the models adjusted for differences in measured individual, household and neighbourhood factors (Table 2, Model 2), nor for NO2 exposure in either unadjusted or adjusted models. In the linear adjusted model, the estimated hazard ratios were 0.99 for a 1 μg/m3 increase in PM2.5 and 0.99 for a 1 μg/m3 increase in NO2 (95% confidence intervals 0.96–1.02 for PM2.5 and 0.98–1.00 for NO2), or 0.99 (0.92–1.06) for PM2.5 and 0.94 (0.89–1.00) for NO2 per IQR. Estimated Model 2 hazard ratios for exposure quartiles were also everywhere close to 1 and statistically insignificant for both pollutants, with no suggestion of dose response.
Subsample analysis by sex and age
Tables 3 and 4 present equivalent estimates for the study population split by sex (Table 3), and age (Table 4), respectively. In each case, we present estimates for the linear and categorical exposure versions of the models in a single column to save space.
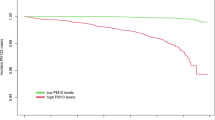
In line with Table 2, Table 3 shows no statistically significant associations between PM2.5 or NO2 exposure and PD onset for either men or women once estimates were adjusted for measured confounders, despite a statistically significant association between PM2.5 exposure and PD onset for females (but not males) in unadjusted models. Table 4 presents similar evidence for those aged 50+ years in 2011, with no statistically significant associations between pollution exposure and PD onset either in the adjusted or unadjusted models, bar a statistically significant hazard ratio marginally below 1 in the adjusted continuous model for NO2 exposure—statistically significant at the 95% level but not the 99% level—which likely reflected Type 1 error or residual confounding rather than a protective effect. In contrast, positive associations between the estimated hazard rate for PD onset and exposure to PM2.5 remained statistically significant at either the 95% or 99% level for the younger age group (under 50 years in 2011), after adjusting for measured confounders, in both the linear and categorical exposure models. The estimated hazard ratios were 1.05 (1.01–1.11) per 1 μg/m3 increase (1.13 (1.01–1.27) per IQR) in the adjusted linear exposure model and 1.26 (1.01–1.56), 1.23 (0.97–1.55) and 1.30 (1.01–1.67) for quartiles 2, 3 and 4 respectively, in the adjusted model with categorical exposures. There was also tentative evidence of a positive association with NO2 exposure, with the estimated hazard ratio for 3rd quartile exposure statistically significant at the 95% level (hazard ratio 1.24, confidence interval 1.00–1.54).
Sensitivity analysis
Our finding of no significant association between PM2.5 or NO2 exposure and PD onset in the overall sample, after adjusting for confounders, was robust to extensive sensitivity analysis. This included: dual-pollutant models (Supplementary Fig. 1); imputing partially missing exposure data using within-individual average exposure in adjacent periods (Supplementary Table 3); extending the at-risk period back to 2010 semester 2 (Supplementary Table 4); varying the exposure lag between 0 and 18 months with the first at-risk period fixed at 2012 semester 1 (Supplementary Tables 5–7); increasing the exposure lag to 18 and 24 months by varying the first at-risk period while keeping the first exposure period fixed at 2011 semester 1 (Supplementary Tables 8 and 9); replacing six-monthly exposures with 2-year moving averages (Supplementary Tables 10–12); adopting an alternative onset definition requiring prescriptions in at least two consecutive semesters (Supplementary Table 13); re-estimation as a stratified Cox model (by sex, age and education) to explore sensitivity to violations of the proportional hazards assumption suggested by Schoenfeld residual testing (Supplementary Table 14); and either dropping the covariates for general health and limiting long-term illness (Supplementary Table 15) or supplementing these with additional covariates for chronic illness as of 2011 semester 1 or prescription-based measures for diabetes and cardio-vascular disease as of 2011 semester 1 (Supplementary Table 16).
We also investigated age-related differences in associations by lag length, re-estimating age-specific models with no lag, a 6-month lag, and an 18-month lag in pollution exposure (Supplementary Tables 17–19). Even for the younger age group, most significant associations disappeared with shorter lags (Supplementary Tables 17 and 18), consistent with diagnosis delay per prior evidence43. Results were consistent with our primary model (Table 3) when extending the lag to 18 months (Supplementary Table 19), showing null associations for the older group and significant positive associations for younger individuals, with some evidence of dose-response for both pollutants. For older individuals, no positive association was found even with longer lags, suggesting age-related differences in delays in diagnosis or prescription do not explain the age-group contrast. In addition, robustness tests on age-group-specific models using 2-year moving averages with a 1-year lag (Supplementary Table 20) and extending the analysis window to earlier periods (Supplementary Table 21) yielded broadly consistent results. Estimated PM2.5 effects remained similar to those in Table 3, while NO2 effects were no longer statistically significant in these additional analyses. Finally, estimated pollution effects for the younger age group were no longer statistically significant at the 95% level when using the alternative two-consecutive-period-prescription onset measure, although key estimated HRs were similar in magnitude (e.g. an estimated hazard ratio of 1.06 (0.99–1.14) per 1 μg/m3 increase in PM2.5 (see Supplementary Table 22)).
Discussion
Our analysis aligns with prior studies that suggest a positive unadjusted association between medium-term PM2.5 exposures and PD onset23,24,25. However, pre-onset differences in characteristics such as age, sex and social disadvantage necessitated statistical adjustment, after which no positive associations with exposure to PM2.5 (nor NO2) were found, consistent with around half of the existing studies listed in Supplementary Table 115,16,21,31.
Comparing our own findings to those of other studies is complicated by variation in factors such as exposure levels and durations studied, the extent to which exposures are lagged, PD measures employed, population studied, and the extent of statistical adjustment for potentially confounding measurable factors. For example, our study took place in a relatively low pollution context compared to most existing studies reported in Supplementary Table 1. Exceptions to this include Salimi et al.21, which similarly found no statistically significant association between exposure to both NO2 and PM2.5 and self-reported PD in New South Wales, Australia; Rumrich et al.15 which similarly found no association between PM2.5 exposures and PD onsets in Finnish data; and Cole-Hunter et al.30 which found a positive and statistically significant association between PD mortality and PM2.5 exposure across six European countries, in contrast to our own finding. Note, however, that Salimi et al.21 and Rumrich et al.15 used diagnosis-based outcome measures (closer to our own prescriptions-based measure), whereas Cole-Hunter et al.30 used a measure of PD mortality.
Among the few studies in the overall pollution-PD literature that have used prescription-based outcome measures, conclusions appear similarly mixed. For example, Cerza et al.19 (who combine drug registry data with other outcome measures) found no statistically significant association between PD and PM2.5 exposure. In contrast, Lee at al.33 reported a statistically significant positive association, albeit for pollutants other than PM2.5 and NO2 (e.g., CO and NOx).
This study is one of few to have examined evidence for heterogeneity in the effect of exposure to pollution on PD onset. In line with our estimates for the overall cohort, we found no evidence of PM2.5 or NO2 effects on PD onset in subsamples by sex and for those aged 50+ years based on Census 2011. But we found some evidence suggesting a positive and statistically significant association between PM2.5 and PD onset among those aged under 50 years at that point, with a more tentative (and less robust) indication of an association with NO2 exposure. Again, existing evidence in these respects is mixed. By sex, Lee et al.40 report a significant association with PM2.5 exposure for males but not females, and Liu et al.38 report no significant association for either males or females (although they report a significant association with PM10 exposure for females but not males). These two studies took contrasting approaches in other respects, however, with the former paper using hospital admission records in cohort data and the latter using self-reported measures in case-control data, for example. Lee et al.40 also estimated associations by age group, reporting a significant association with PM2.5 exposure among study participants over-65 but not among those under-65. Though not directly comparable, the former finding appears at odds with our own finding of a significant association for under-50s but not for over-50s.
Our finding—unique in the literature to date—that exposure to pollution (particularly PM2.5 pollution) is associated, albeit tentatively, with the onset of PD among <50s but not with onset of PD among those aged 50+ years in the NILS-EPD cohort might reflect a genuine difference in the etiology of PD across age cohorts. There is some existing evidence for etiologic differences in early versus late onset of PD42. However, given that PD has several clinical subtypes, pathogenic genes and putative causative environmental agents44, reaching a fuller understanding of such differences remains a challenge for the wider literature.
There may also be one or more non-etiological explanations for this contrast. We conjecture here that one such potential explanation is differences in the delay between onset of symptoms and PD diagnosis and/or first prescription for PD medication, given existing evidence of higher diagnostic delays for PD at older ages. Such delays introduce uncertainty regarding the relevant lag structure for exposures within models of PD onset and, crucially, might also differentially attenuate estimated associations at a given lag length by age group. Most of the PD-pollution literature ignores this potential source of bias4,16,19,21,23,38, although it is acknowledged by some studies25,26. In the absence of data on the onset of symptoms, we have been unable to examine this issue explicitly here. Nevertheless, we have shown that our conclusions, and crucially the contrast between estimated pollution effects for under-50s and over-50s, are robust to extending the lag of exposures beyond 12 months, although less so to shortening the lag below 12 months. The suggestion is that diagnostic delays and/or gaps between diagnosis and first prescription are unlikely to fully explain the contrasting findings for the younger and older age groups, although we cannot rule out some role.
Another explanation for the age contrast suggested here is the possibility that our prescriptions-based measure disproportionately overestimates PD onsets among under-50s, as these drugs may be used for other health conditions with overlapping symptoms, e.g. RLS and Dystonia. These conditions share some aspects of etiology with PD, involving dopaminergic dysfunction, and thus their treatment can include enhancing dopamine activity in the brain, like the treatment of PD. Indeed, comparing our own estimate of PD incidence with the figures implied by statistics from the National Institute for Health and Care Excellence (NICE)45 suggests that we may overcount PD cases in our dataset, and by a factor of around 1.5 (NICE suggested an incidence rate of 144 per 100,000 person-years in 2016). Based on that rate, we should expect approximately 2160 incidences of PD across our sample over 5 years, which is lower than the 3089 incidences we identified.) Additionally, considering a recent meta-analysis of gender-specific PD incidence46, the overcounting of PD onsets may be more pronounced in our younger age group. Therefore, a more cautious interpretation of our research is that it suggests a tentative association between exposure to air pollution and the onset of conditions—including, but not limited to, Parkinson’s disease (PD)—for which these drugs are prescribed in younger age groups. In support of this more cautious interpretation, sensitivity analysis using a stricter two-consecutive-period-prescription measure of PD onset returned non-significant estimated hazard ratios for both age groups. Given the limitations of our dataset, a more detailed investigation is beyond the scope of this paper. However, this is an important avenue for further research.
In addition to the potential measurement errors stemming from our prescriptions-based proxy for PD onset, this study has other limitations, including the inability to assess indoor pollution effects, despite growing evidence of the importance of indoor air pollution in health outcomes47,48,49, and reliance on modelled annual outdoor pollution averages. Furthermore, we could not examine short-term pollution events or exposures longer than 2 years, leaving the most appropriate exposure duration for modelling PD onset unclear. Finally, characterising the nature of the pollutants involved would add value to the study, since some components of particulate matter may have different effects on health than others50,51. Unfortunately, suitable speciation data do not exist for Northern Ireland. Despite these limitations, our findings contribute to the growing PD-pollution literature, highlighting potential but tentative associations at younger ages even in low-pollution contexts like Northern Ireland.
It is crucial to emphasise that our overall null finding should not undermine the importance of reducing population exposures to PM2.5 or NO2. Reducing these exposures remains vital due to robust evidence linking pollution to various health outcomes and emerging evidence of its association with PD in specific contexts9,52,53,54,55,56,57,58,59. Our data also tentatively suggest there may be an association with PD, or perhaps a broader class of conditions for which PD-related drugs are sometimes prescribed, among under-50s.
In conclusion, this study examines the link between medium-term air pollution exposure and PD onset using a large, nationally representative cohort from Northern Ireland. It benefits from complete address records which enable linkage to pollutant concentrations at the local level over an extended time frame, detailed Census data for statistical adjustment, and primary care prescription data, reducing the scope for the kinds of measurement errors associated with self-reports or hospital-based outcome measures60,61,62. The study also explores potential differences by sex and age. Overall, no significant associations were found between PM2.5, NO2 exposure, and PD onset for this cohort, or in males, females, and those aged 50+ years. However, we found some evidence of a statistically significant association between air pollution exposure and PD onset, using our prescriptions-based proxy, among under-50s. In the absence of alternative measures of PD onset for this cohort, it remains unclear how to interpret this estimated association. But it clearly warrants further research.
Methods
Data
We used data from a new linkage between the Northern Ireland Longitudinal Study (NILS), pollution data at the 1 km grid-square level, and the Enhanced Prescribing Database (EPD). The NILS is a longitudinal study that follows a 28% representative sample of the Northern Ireland population drawn from the NI Health Card Registration System, which contains address histories updated biannually. The NILS is linked to several other administrative datasets including Census records for 2011, which provided rich information on socioeconomic and demographic characteristics and contexts for sample members63. The pollution data, matched at the residential property level to NILS participants, provided annual 1 km grid-square modelled pollution data from 2009–2016 for both PM2.5 and NO2. These data were produced by Ricardo Energy & Environment for the UK Government’s air quality assessments64. These data were then linked to the EPD, which contains detailed information relating to all primary care prescriptions dispensed in Northern Ireland since March 200865, made available to us at six-monthly frequency from January 2010 onwards. From this we extracted data on prescriptions in each 6-month period (January–June (hereafter semester 1) and July–December (hereafter semester 2)) of each year, from a defined list of items covering drugs that, according to the British National Formulary (BNF) classification system, were prescribed for PD at the time. (Note that, in the Northern Ireland health system the PD diagnostic process typically begins with a general practitioner (GP) conducting an initial assessment, followed by referral to a specialist—usually a neurologist or consultant with expertise in movement disorders—who is responsible for making the diagnosis.) All data were anonymized. Analysis was conducted in a trusted research environment under strict confidentiality and security protocols by ONS-accredited researchers. Researchers did not have access to addresses or other sensitive information.
Analysis sample
Our main analysis sample—used for our preferred models—included all NILS members present in the 2011 Census who were aged 28 years or older at the time, had full address records, and were not in receipt of PD medication prior to the semester January–June 2012, which we treated as the first at-risk period for the purposes of modelling PD onset. The first at-risk period and associated sample exclusion condition was varied in sensitivity analysis. Compared to the full NILS sample returned in the 2011 Census and aged 28+ years at that time (but similarly excluding those with PD prescriptions prior to 2012 semester 1), our analysis sample was slightly (around 3.5%) smaller, mainly due to missing information on exposure to pollution at some point during the analysis period due to incomplete address records. In terms of measured characteristics, however, the two samples were very similar (see Table 1).
Outcome variable
The outcome variable, drawn from the EPD, was set to 1 from the semester at which the individual had received any prescription for PD-related medication, including dopaminergic drugs, antimuscarinic drugs, and treatments for tremor, chorea, tics, and related disorders, and 0 otherwise (see Supplementary Table 23). Prescription data is commonly used in studies on air pollution and health66,67,68, but has rarely been used in the pollution and PD literature19,33.
Such prescription-based measures have advantages and disadvantages as proxies for the onset of PD. These measures are objective, requiring a prior PD diagnosis, but may undercount or overcount PD onsets. Undercounting is possible in cases where patients do not receive or delay receiving prescriptions, or where initial treatment occurs in hospitals rather than primary care. Such undercounting or delays could bias estimates if affected individuals were disproportionately exposed to higher or lower pollution levels. Sensitivity analysis varying exposure lag lengths was conducted to address these concerns, particularly relevant given evidence of longer diagnostic and prescription delays with increasing age of PD onset43. Alternatively, we may overcount PD onsets if prescriptions for drugs used to treat PD are sometimes issued to treat other conditions with overlapping symptoms, e.g. Restless Leg Syndrome (RLS) and Dystonia (For further information see NICE BNF online https://bnf.nice.org.uk/drug/ and https://bnfc.nice.org.uk/treatment-summaries/dystonias-and-related-disorders/#dopaminergic-drugs-used-in-dystonias, as well as, NHS website: https://www.nhs.uk/conditions/restless-legs-syndrome/treatment/). The direction of any resulting bias will depend on the extent to which these other conditions are themselves associated with air pollution exposure, which given a lack of existing evidence, remains unknown. Comparing the estimated incidence of PD using our prescriptions-based measure to that estimated by other methods suggested that overcounting was more likely an issue than undercounting, at least at younger ages. We assess this evidence and its implications for the interpretation of our estimates, particularly those where we split the sample by age group, in the discussion section.
Exposure variables
Our exposure variables were derived from annual average PM2.5 and NO2 concentrations modelled at the 1 km grid-square level across Northern Ireland produced by Ricardo Energy & Environment for the UK Government’s air quality assessments. These concentrations were themselves derived from the aggregation of values from a variety of large and small point sources, as well as area and distance sources, using various datasets, including the UK National Atmospheric Emissions Inventory64. Modelled concentrations were calibrated with data from the UK national monitoring network and evaluated using data from monitoring sites not used in the calibration process prior to their publication. These data have been used in several existing studies of the health effects of ambient air pollution exposure within the UK69,70, including specifically in Northern Ireland71. Similar modelled pollution data have also been used extensively in the international literature72,73,74,75, including in the specific literature on the association between ambient air pollution and PD16,32,34. The trade-off for the population coverage that such data offer is the potential for measurement error in pollution concentrations. For an analysis of potential implications for estimated health effects of exposure see Samoli et al.76.
PM2.5 and NO2 are the two pollutants which have attracted most interest in the air pollution-PD literature to date, and our focus on these pollutants reflected this. All individuals in the sample were assigned exposure values for PM2.5 and NO2, via their residential address, for every 6-month period from January–June 2009 (2009 semester 1) through to July–December 2016 (2016 semester 2), although in our preferred models we use exposure data only from 2011 semester 1 onwards. Addresses are updated every 6 months in the NILS, in April and October of each year. We used April addresses to determine exposures for semester 1 and October addresses to determine exposures for semester 2 of each year. In other words, six-monthly exposures were assigned according to address at approximately the mid-point of each semester. Note that although the underlying pollution data were annual frequency, there was within-year variation in exposure in our analysis sample where (and only where) individuals changed residential address between April and October in any given year.
These data are best suited for studying medium-term exposures, initially defined as exposure over a 6-month period. Exposures are lagged by 1-year, reflecting evidence on the average delay between symptom onset and PD diagnosis43. Medium-term exposure durations in the literature range from weeks to years77,78. Sensitivity analysis included 2-year moving averages and varied lags for both 6-month and 2-year moving average exposures from zero (contemporaneous exposures) to 6 and 18 months.
Covariates
The 2011 Census link allowed adjustment for a rich set of individual and household socio-economic and demographic covariates, each measured in March 2011. These variables are listed in Table 1, along with their (unweighted) sample means, both overall and separately for those in our analysis sample who did and did not experience PD onset. Approximately 0.1% of the sample had non-response (missing/edited) across multiple covariates, primarily from individuals in communal establishments during the 2011 Census, and were excluded from the sample. Table 1 also compares the analysis sample to the equivalent full sample of NILS members present in 2011 Census. We supplemented these covariates with neighbourhood deprivation indicators corresponding to 2011 Census residential address. These give the deprivation rank decile of the individual’s residential super output area (SOA) according to the 2010 multiple deprivation measure (MDM) index79. Note there are 890 SOAs in NI with an average population of 790 households.
Model
We used time-dependent CPH models, with calendar time as the underlying time scale, to examine the associations between pollution exposures and the onset of PD, as is typical in existing cohort studies of air pollution and PD4,19,30,34. We estimated hazard ratios for the association between medium-term exposure to ambient PM2.5 and NO2 and receiving a first prescription for PD. Following Jo et al.4 exposure to ambient air pollution was modelled both in continuous/linear form and in categorical form (as quartiles) to allow for non-linearity. We estimated unadjusted models as well as models adjusted for covariates at individual, household and neighbourhood level. Note that 7.1% of individuals are right censored at some point during the analysis period due to death or emigration.
In our preferred model specification, our analysis of PD onset starts in the period 2012 semester 1 with exposures measured from the corresponding semester 1 year previously (2011 semester 1). This ensured that measured exposures did not precede measurement of the covariates. In sensitivity analysis we relaxed this restriction, modelling PD onsets from the first available data point (2010 semester 2) with corresponding exposures prior to the 2011 Census date, in addition to examining sensitivity to the length and lag of the exposure period. Standard errors were clustered at the SOA level. Analysis was performed in the trusted research environment of the Northern Ireland Statistics and Research Agency (NISRA) using STATA 17.
Data availability
The datasets analysed in the current study are not publicly available per our data use agreement. The data, however, can be requested by accredited researchers from Northern Ireland Statistics and Research Agency (NISRA).
References
GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 459–480 (2019).
Parkinson’s UK. Incidence and Prevalence of Parkinson’s in the UK: Results from the Clinical Practice Research Datalink Summary Report (Parkinson’s UK, 2017).
Willis, A. W. et al. Incidence of Parkinson disease in North America. NPJ Parkinsons Dis. 8, 170 (2022).
Jo, S. et al. Association of NO2 and other air pollution exposures with the risk of Parkinson disease. JAMA Neurol. 78, 800–808 (2021).
Dias, V., Junn, E. & Mouradian, M. M. The role of oxidative stress in Parkinson’s disease. J. Parkinsons Dis. 3, 461–491 (2013).
Baumgart, M. et al. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: a population-based perspective. Alzheimers Dement 11, 718–726 (2015).
Grande, G., Ljungman, P. L. S., Eneroth, K., Bellander, T. & Rizzuto, D. Association between cardiovascular disease and long-term exposure to air pollution with the risk of dementia. JAMA Neurol. 77, 801–809 (2020).
Laden, F., Schwartz, J., Speizer, F. E. & Dockery, D. W. Reduction in fine particulate air pollution and mortality: extended follow-up of the Harvard Six Cities study. Am. J. Respir. Crit. Care Med. 173, 667–672 (2006).
Pope, C. A. & Dockery, D. W. Health effects of fine particulate air pollution: lines that connect. J. Air Waste Manag Assoc. 56, 709–742 (2006).
Wellenius, G. A. et al. Ambient air pollution and the risk of acute ischemic stroke. Arch. Intern. Med. 172, 229–234 (2012).
Yan, Y. et al. Ambient air pollution and cerebrovascular disease mortality: an ecological time-series study based on 7-year death records in central China. Environ. Sci. Pollut. Res. Int. 28, 27299–27307 (2021).
Ascherio, A. & Schwarzschild, M. A. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 15, 1257–1272 (2016).
Baranyi, G. et al. Higher air pollution exposure in early life is associated with worse health among older adults: a 72-year follow-up study from Scotland. Health Place 86, 103208 (2024).
Inoue, T., Nunokawa, N., Kurisu, D. & Ogasawara, K. Particulate air pollution, birth outcomes, and infant mortality: evidence from Japan’s automobile emission control law of 1992. SSM Popul. Health 11, 100590 (2020).
Rumrich, I. K. et al. Long-term exposure to low-level particulate air pollution and Parkinson’s disease diagnosis—a Finnish register-based study. Environ. Res. 229, 115944 (2023).
Palacios, N. et al. Particulate matter and risk of Parkinson disease in a large prospective study of women. Environ. Health 13, 80 (2014).
Palacios, N. et al. A prospective analysis of airborne metal exposures and risk of Parkinson disease in the Nurses’ Health Study cohort. Environ. Health Perspect. 122, 933–938 (2014).
Palacios, N. Air pollution and Parkinson’s disease—evidence and future directions. Rev. Environ. Health 32, 303–313 (2017).
Cerza, F. et al. Residential exposure to air pollution and incidence of Parkinson’s disease in a large metropolitan cohort. Environ. Epidemiol. 2, e023 (2018).
Kasdagli, M. I., Katsouyanni, K., Dimakopoulou, K. & Samoli, E. Air pollution and Parkinson’s disease: a systematic review and meta-analysis up to 2018. Int. J. Hyg. Environ. Health 222, 402–409 (2019).
Salimi, F. et al. Associations between long-term exposure to ambient air pollution and Parkinson’s disease prevalence: a cross-sectional study. Neurochem. Int. 133, 104615 (2020).
Han, C., Lu, Y., Cheng, H., Wang, C. & Chan, P. The impact of long-term exposure to ambient air pollution and second-hand smoke on the onset of Parkinson disease: a review and meta-analysis. Public Health 179, 100–110 (2020).
Lee, H. et al. Short-term air pollution exposure aggravates Parkinson’s disease in a population-based cohort. Sci. Rep. 7, 44741 (2017).
van Wijngaarden, E. et al. Neurodegenerative hospital admissions and long-term exposure to ambient fine particle air pollution. Ann. Epidemiol. 54, 79–86.e4 (2021).
Shin, S. et al. Effects of ambient air pollution on incident Parkinson’s disease in Ontario, 2001 to 2013: a population-based cohort study. Int. J. Epidemiol. 47, 2038–2048 (2018).
Shi, L. et al. Long-term effects of PM2·5 on neurological disorders in the American Medicare population: a longitudinal cohort study. Lancet Planet Health 4, e557–e565 (2020).
Cristaldi, A. et al. Possible association between PM2.5 and neurodegenerative diseases: a systematic review. Environ. Res. 208, 112581 (2022).
Rhew, S. H., Kravchenko, J. & Lyerly, H. K. Exposure to low-dose ambient fine particulate matter PM2.5 and Alzheimer’s disease, non-Alzheimer’s dementia, and Parkinson’s disease in North Carolina. PLoS ONE 16, e0253253 (2021).
Hu, C. Y. et al. Association between ambient air pollution and Parkinson’s disease: systematic review and meta-analysis. Environ. Res. 168, 448–459 (2019).
Cole-Hunter, T. et al. Long-term air pollution exposure and Parkinson’s disease mortality in a large pooled European cohort: an ELAPSE study. Environ. Int. 171, 107667 (2023).
Palacios, N. et al. Air pollution and risk of Parkinson’s disease in a large prospective study of men. Environ. Health Perspect. 125, 087011 (2017).
Ritz, B. et al. Traffic-related air pollution and Parkinson’s disease in Denmark: a case-control study. Environ. Health Perspect. 124, 351–356 (2016).
Lee, P. C. et al. Traffic-related air pollution increased the risk of Parkinson’s disease in Taiwan: a nationwide study. Environ. Int. 96, 75–81 (2016).
Chen, H. et al. Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: a population-based cohort study. Lancet 389, 718–726 (2017).
Finkelstein, M. M. & Jerrett, M. A study of the relationships between Parkinson’s disease and markers of traffic-derived and environmental manganese air pollution in two Canadian cities. Environ. Res. 104, 420–432 (2007).
Willis, A. W. et al. Metal emissions and urban incident Parkinson disease: a community health study of Medicare beneficiaries by using geographic information systems. Am. J. Epidemiol. 172, 1357–1363 (2010).
Dhiman, V., Trushna, T., Raj, D. & Tiwari, R. R. Is ambient air pollution a risk factor for Parkinson’s disease? A meta-analysis of epidemiological evidence. Int. J. Environ. Health Res. 33, 733–750 (2023).
Liu, R., Young, M. T., Chen, J. C., Kaufman, J. D. & Chen, H. Ambient air pollution exposures and risk of Parkinson disease. Environ. Health Perspect. 124, 1759–1765 (2016).
Nunez, Y. et al. Parkinson’s disease aggravation in association with fine particle components in New York State. Environ. Res. 201, 111554 (2021).
Lee, H., Kim, O. J., Jung, J., Myung, W. & Kim, S. Y. Long-term exposure to particulate air pollution and incidence of Parkinson’s disease: a nationwide population-based cohort study in South Korea. Environ. Res. 212, 113165 (2022).
Cerri, S., Mus, L. & Blandini, F. Parkinson’s disease in women and men: what’s the difference?. J. Parkinsons Dis. 9, 501–515 (2019).
Hirsch, E. C. & Hunot, S. Neuroinflammation in Parkinson’s disease: a target for neuroprotection?. Lancet Neurol. 8, 382–397 (2009).
Hähnel, T. et al. Predictive modeling to uncover Parkinson’s disease characteristics that delay diagnosis. medRxiv https://doi.org/10.1101/2024.03.12.24304165 (2024).
Jankovic, J. & Tan, E. K. Parkinson’s disease: etiopathogenesis and treatment. J. Neurol. Neurosurg. Psychiatry 91, 795–808 (2020).
National Institute for Health and Care Excellence. Parkinson’s disease: prevalence. NICE Clinical Knowledge Summaries. https://cks.nice.org.uk/topics/parkinsons-disease/background-information/prevalence/ (2025).
Hirsch, L., Jette, N., Frolkis, A., Steeves, T. & Pringsheim, T. The incidence of Parkinson’s disease: a systematic review and meta-analysis. Neuroepidemiology 46, 292–300 (2016).
Barn, P. et al. The effect of portable HEPA filter air cleaner use during pregnancy on fetal growth: the UGAAR randomized controlled trial. Environ. Int. 121, 981–989 (2018).
Cincinelli, A. & Martellini, T. Indoor air quality and health. Int. J. Environ. Res. Public Health 14, 1286 (2017).
Karottki, D. G. et al. An indoor air filtration study in homes of elderly: cardiovascular and respiratory effects of exposure to particulate matter. Environ. Health 12, 116 (2013).
Raaschou-Nielsen, O. et al. PM2.5 air pollution components and mortality in Denmark. Environ. Int. 171, 107685 (2023).
Committee on the Medical Effects of Air Pollutants. Statement on the differential toxicity of particulate matter according tosource or constituents: 2022. UK Government. https://www.gov.uk/government/publications/particulate-air-pollution-health-effects-of-exposure/statement-on-the-differential-toxicity-of-particulate-matter-according-to-source-or-constituents-2022 (2022).
Currie, J., Neidell, M. & Schmieder, J. F. Air pollution and infant health: lessons from New Jersey. J. Health Econ. 28, 688–703 (2009).
Brook, R. D. et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121, 2331–2378 (2010).
Paul, K. C., Haan, M., Mayeda, E. R. & Ritz, B. R. Ambient air pollution, noise, and late-life cognitive decline and dementia risk. Annu. Rev. Public Health 40, 203–220 (2019).
Peters, R. et al. Air pollution and dementia: a systematic review. J. Alzheimers Dis. 70, S145–S163 (2019).
Power, M. C., Adar, S. D., Yanosky, J. D. & Weuve, J. Exposure to air pollution as a potential contributor to cognitive function, cognitive decline, brain imaging, and dementia: a systematic review of epidemiologic research. Neurotoxicology 56, 235–253 (2016).
Delgado-Saborit, J. M. et al. A critical review of the epidemiological evidence of effects of air pollution on dementia, cognitive function and cognitive decline in adult population. Sci. Total Environ. 757, 143734 (2021).
Bowe, B. et al. The 2016 global and national burden of diabetes mellitus attributable to PM2·5 air pollution. Lancet Planet Health 2, e301–e312 (2018).
Yang, M. et al. Effects of long-term exposure to air pollution on the incidence of type 2 diabetes mellitus: a meta-analysis of cohort studies. Environ. Sci. Pollut. Res. Int. 27, 798–811 (2020).
Althubaiti, A. Information bias in health research: definition, pitfalls, and adjustment methods. J. Multidiscip. Health 9, 211–217 (2016).
Futoma, J., Simons, M., Panch, T., Doshi-Velez, F. & Celi, L. A. The myth of generalisability in clinical research and machine learning in health care. Lancet Digit Health 2, e489–e492 (2020).
Halonen, P., Jämsen, E., Enroth, L. & Jylhä, M. Agreement between self-reported information and health register data on chronic diseases in the oldest old. Clin. Epidemiol. 15, 785–794 (2023).
O’Reilly, D., Rosato, M., Catney, G., Johnston, F. & Brolly, M. Cohort description: the Northern Ireland Longitudinal Study (NILS). Int. J. Epidemiol. 41, 634–641 (2012).
Brookes, D. M. et al. Technical report on UK supplementary assessment under The Air Quality Directive (2008/50/EC), The Air Quality Framework Directive (96/62/EC) and Fourth Daughter Directive (2004/107/EC) for 2018. https://uk-air.defra.gov.uk/assets/documents/reports/cat09/2102111100_2019_PCM_technical_report.pdf (2018).
Maguire, A., Hughes, C., Cardwell, C. & O’Reilly, D. Psychotropic medications and the transition into care: a national data linkage study. J. Am. Geriatr. Soc. 61, 215–221 (2013).
Blangiardo, M., Finazzi, F. & Cameletti, M. Two-stage Bayesian model to evaluate the effect of air pollution on chronic respiratory diseases using drug prescriptions. Spat. Spatiotemporal Epidemiol. 18, 1–12 (2016).
Chimonas, M. A. & Gessner, B. D. Airborne particulate matter from primarily geologic, non-industrial sources at levels below National Ambient Air Quality Standards is associated with outpatient visits for asthma and quick-relief medication prescriptions among children less than 20 years old enrolled in Medicaid in Anchorage, Alaska. Environ. Res. 103, 397–404 (2007).
Conti, S. et al. The short-term effect of particulate matter on cardiorespiratory drug prescription, as a proxy of mild adverse events. Environ. Res. 157, 145–152 (2017).
Dibben, C. & Clemens, T. Place of work and residential exposure to ambient air pollution and birth outcomes in Scotland, using geographically fine pollution climate mapping estimates. Environ. Res. 140, 535–541 (2015).
Clemens, T., Turner, S. & Dibben, C. Maternal exposure to ambient air pollution and fetal growth in North-East Scotland: a population-based study using routine ultrasound scans. Environ. Int. 107, 216–226 (2017).
Jahanshahi, B. et al. Prenatal exposure to particulate matter and infant birth outcomes: evidence from a population-wide database. Health Econ. 33, 2182–2200 (2024).
Fuks, K. B. et al. Arterial blood pressure and long-term exposure to traffic-related air pollution: an analysis in the European Study of Cohorts for Air Pollution Effects (ESCAPE). Environ. Health Perspect. 122, 896–905 (2014).
Künzli, N. et al. Public-health impact of outdoor and traffic-related air pollution: a European assessment. Lancet 356, 795–801 (2000).
McGuinn, L. A. et al. Association of long-term PM2.5 exposure with traditional and novel lipid measures related to cardiovascular disease risk. Environ. Int. 122, 193–200 (2019).
Van den Hooven, E. H. et al. Air pollution exposure estimation using dispersion modelling and continuous monitoring data in a prospective birth cohort study in the Netherlands. Environ. Health 11, 9 (2012).
Samoli, E. et al. The impact of measurement error in modeled ambient particles exposures on health effect estimates in multilevel analysis: a simulation study. Environ. Epidemiol. 4, e094 (2020).
Alexeeff, S. E. et al. Medium-term exposure to traffic-related air pollution and markers of inflammation and endothelial function. Environ. Health Perspect. 119, 481–486 (2011).
de Prado-Bert, P. et al. Short- and medium-term air pollution exposure, plasmatic protein levels and blood pressure in children. Environ. Res. 211, 113109 (2022).
Northern Ireland Statistics and Research Agency (NISRA). Northern Ireland Multiple Deprivation Measure 2010 (NIMDM2010). https://www.nisra.gov.uk/statistics/deprivation/northern-ireland-multiple-deprivation-measure-2010-nimdm2010 (2010).
Acknowledgements
The help provided by the staff of the Northern Ireland Longitudinal Study (NILS) and the NILS Research Support Unit is acknowledged. The NILS is funded by the Health and Social Care Research and Development Division of the Public Health Agency (HSC R&D Division) and NISRA. The NILS-RSU is funded by the ESRC and the Northern Ireland Government. The authors alone are responsible for the interpretation of the data and any views or opinions presented are solely those of the authors and do not necessarily represent those of NISRA/NILS. Funding through Administrative Data Research Northern Ireland is also gratefully acknowledged, as is the help of the Administrative Data Research Centre Northern Ireland staff team. The BSO data have been supplied for sole purpose of this project. We also thank Karen Doherty, Jason Fleming, Mark McGovern and seminar participants at multiple conferences for helpful comments on earlier drafts.
Funding
This work was supported by Administrative Data Research Northern Ireland (ADR-NI), itself supported by the UK Economic & Social Research Council. (Grant Numbers ES/S00744X/1 and ES/ W010240/1). The funder had no role in the design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Babak Jahanshahi wrote the main manuscript text, prepared the data for analysis, and created the figure and tables. Duncan McVicar contributed to writing the manuscript, conceptualisation, and methodology. Neil Rowland contributed to data curation, methodology, and analysis. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jahanshahi, B., McVicar, D. & Rowland, N. Exposure to ambient air pollution and onset of Parkinson’s disease in a large cohort study. npj Parkinsons Dis. 11, 291 (2025). https://doi.org/10.1038/s41531-025-01156-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01156-z