Abstract
Influenza virus infections generate antibodies that cross-react with antigenically similar viruses. However, the breadth of cross-reactivity is unclear. Here we analysed 200,000 haemagglutination inhibition (HAI) titrations from ferrets singly infected with A(H3N2) or A(H1N1)pdm09. We identified consistent influenza A virus subtype-specific patterns where breadth of HAI antibody cross-reactivity was associated with isolation time between tested and immunizing viruses. This was independent of virus strains, passage history and genetic mutations. A 6-year interval between virus isolation resulted in minimal HAI titres for A(H3N2), while A(H1N1)pdm09 demonstrated broader cross-reactivity with moderate titre reductions over the same interval. Analysis of HA substitutions revealed more amino acid substitutions between viruses for A(H3N2) and a greater reduction in HAI titres per substitution compared with A(H1N1). Longitudinal analysis of human antisera across age groups suggests that repeat A(H3N2) exposure increased HAI responses within the cross-reactivity range, with greater increases for more recent viruses. These results provide a framework for antigenically evolving pathogens such as influenza viruses.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All raw HAI data are publicly available from the original publications or reports. All raw sequence data are available in the original publications and in GISAID. The integrated datasets used in this study are accessible on GitHub at https://github.com/byyangyby/influenza_A_cross-reactivity (ref. 40). Source data are provided with this paper.
Code availability
Source code for the R scripts used in the analysis is available on GitHub40.
References
Iuliano, A. D. et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet 391, 1285–1300 (2018).
Yang, B. et al. Long term intrinsic cycling in human life course antibody responses to influenza A(H3N2): an observational and modeling study. Elife 11, e81457 (2022).
Yang, B. et al. Life course exposures continually shape antibody profiles and risk of seroconversion to influenza. PLoS Pathog. 16, e1008635 (2020).
Oidtman, R. J. et al. Influenza immune escape under heterogeneous host immune histories. Trends Microbiol. 29, 1072–1082 (2021).
Fonville, J. M. et al. Antibody landscapes after influenza virus infection or vaccination. Science 346, 996–1000 (2014).
Krammer, F. The human antibody response to influenza A virus infection and vaccination. Nat. Rev. Immunol. 19, 383–397 (2019).
Fisman, D. N. et al. Older age and a reduced likelihood of 2009 H1N1 virus infection. N. Engl. J. Med. 361, 2000–2001 (2009).
Auladell, M. et al. Influenza virus infection history shapes antibody responses to influenza vaccination. Nat. Med. 28, 363–372 (2022).
Kucharski, A. J., Lessler, J., Cummings, D. A. T. & Riley, S. Timescales of influenza A/H3N2 antibody dynamics. PLoS Biol. 16, e2004974 (2018).
Grenfell, B. T. et al. Unifying the epidemiological and evolutionary dynamics of pathogens. Science 303, 327–332 (2004).
Neher, R. A., Bedford, T., Daniels, R. S., Russell, C. A. & Shraiman, B. I. Prediction, dynamics, and visualization of antigenic phenotypes of seasonal influenza viruses. Proc. Natl Acad. Sci. USA 113, E1701–E1709 (2016).
Bedford, T. et al. Integrating influenza antigenic dynamics with molecular evolution. Elife 3, e01914 (2014).
Gupta, V., Earl, D. J. & Deem, M. W. Quantifying influenza vaccine efficacy and antigenic distance. Vaccine 24, 3881–3888 (2006).
Amanna, I. J., Carlson, N. E. & Slifka, M. K. Duration of humoral immunity to common viral and vaccine antigens. N. Engl. J. Med. 357, 1903–1915 (2007).
Hoa, L. N. M. et al. Influenza A(H1N1)pdm09 but not A(H3N2) virus infection induces durable seroprotection: results from the Ha Nam cohort. J. Infect. Dis. 226, 59–69 (2022).
Wraith, S. et al. Homotypic protection against influenza in a pediatric cohort in Managua, Nicaragua. Nat. Commun. 13, 1190 (2022).
Gouma, S. et al. Middle-aged individuals may be in a perpetual state of H3N2 influenza virus susceptibility. Nat. Commun. 11, 4566 (2020).
Ng, S. et al. Novel correlates of protection against pandemic H1N1 influenza A virus infection. Nat. Med. 25, 962–967 (2019).
Russell, C. A. et al. The global circulation of seasonal influenza A (H3N2) viruses. Science 320, 340–346 (2008).
Smith, D. J. et al. Mapping the antigenic and genetic evolution of influenza virus. Science 305, 371–376 (2004).
Fonville, J. M. et al. Antigenic maps of influenza A(H3N2) produced with human antisera obtained after primary infection. J. Infect. Dis. 213, 31–38 (2016).
Brouwer, A. F. et al. Birth cohort relative to an influenza A virus’s antigenic cluster introduction drives patterns of children’s antibody titers. PLoS Pathog. 18, e1010317 (2022).
Worldwide Influenza Centre. Annual and Interim Reports (The Francis Crick Institute, 2003–2022).
Hinojosa, M. et al. Impact of immune priming, vaccination, and infection on influenza A(H3N2) antibody landscapes in children. J. Infect. Dis. 224, 469–480 (2021).
Ertesvag, N. U. et al. Seasonal influenza vaccination expands hemagglutinin-specific antibody breadth to older and future A/H3N2 viruses. npj Vaccines 7, 67 (2022).
Lessler, J. et al. Evidence for antigenic seniority in influenza A (H3N2) antibody responses in southern China. PLoS Pathog. 8, e1002802 (2012).
Elbe, S. & Buckland-Merrett, G. Data, disease and diplomacy: GISAID’s innovative contribution to global health. Glob. Chall. 1, 33–46 (2017).
Koel, B. F. et al. Substitutions near the receptor binding site determine major antigenic change during influenza virus evolution. Science 342, 976–979 (2013).
Ushirogawa, H. et al. Re-emergence of H3N2 strains carrying potential neutralizing mutations at the N-linked glycosylation site at the hemagglutinin head, post the 2009 H1N1 pandemic. BMC Infect. Dis. 16, 380 (2016).
Perofsky, A. C. et al. Antigenic drift and subtype interference shape A(H3N2) epidemic dynamics in the United States. Elife 13, RP91849 (2024).
Yang, W., Lau, E. H. Y. & Cowling, B. J. Dynamic interactions of influenza viruses in Hong Kong during 1998–2018. PLoS Comput. Biol. 16, e1007989 (2020).
Kucharski, A. J. et al. Estimating the life course of influenza A(H3N2) antibody responses from cross-sectional data. PLoS Biol. 13, e1002082 (2015).
Rambaut, A. et al. The genomic and epidemiological dynamics of human influenza A virus. Nature 453, 615–619 (2008).
Wang, Y., Tang, C. Y. & Wan, X. F. Antigenic characterization of influenza and SARS-CoV-2 viruses. Anal. Bioanal. Chem. 414, 2841–2881 (2022).
Francis, T. On the Doctrine of Original Antigenic Sin. Proc. Am. Philos. Soc. 104, 572–578 (1960).
Einav, T. & Ma, R. Using interpretable machine learning to extend heterogeneous antibody–virus datasets. Cell Rep. Methods 3, 100540 (2023).
Niewiesk, S. Maternal antibodies: clinical significance, mechanism of interference with immune responses, and possible vaccination strategies. Front. Immunol. 5, 446 (2014).
Dugan, H. L. et al. Preexisting immunity shapes distinct antibody landscapes after influenza virus infection and vaccination in humans. Sci. Transl. Med. 12, eabd3601 (2020).
Nachbagauer, R. et al. Defining the antibody cross-reactome directed against the influenza virus surface glycoproteins. Nat. Immunol. 18, 464–473 (2017).
Yang, B. Cross-reactivity breadth for influenza A viruses. GitHub https://github.com/byyangyby/influenza_A_cross-reactivity (2024).
Acknowledgements
We thank the Francis Crick Institute for sharing antigenic data, especially N. Lewis and R. Harvey; A. Fox and A. Byrnes for helpful discussions; all data contributors and their submitting laboratories for generating the genetic sequence and metadata and sharing via the GISAID Initiative, on which part of this research is based. This project was supported by the Seed Fund for Basic Research for New Staff of The University of Hong Kong Project Number 2201100409 (B.Y.), Health Medical Research Funds Fellowship Scheme Project Number 7210167 (B.Y.), Theme-based Research Scheme Project Number T11-712/19-N (B.J.C.) of the Research Grants Council of the Hong Kong SAR Government and National Institutes of Health Project Number R01AI170116 (S.C. and B.J.C.). The funding bodies had no role in the design of the study or in the analysis and interpretation of data.
Author information
Authors and Affiliations
Contributions
B.Y. conceived the study, designed the analytic methodology, developed the software, performed visualization, wrote the first draft and secured funding. B.Y., R.Z., T.E. and L.P. curated the data. B.Y. and K.M.G. conducted formal analysis. B.Y., K.M.G., D.C.A., S.S.W., T.K.T., D.A.T.C., S.G.S., S.C. and B.J.C. contributed to the investigation. K.M.G., D.C.A., T.E., S.S.W., T.K.T., D.A.T.C., S.G.S., S.C. and B.J.C. critically reviewed and revised the paper. All authors approved the final draft.
Corresponding author
Ethics declarations
Competing interests
B.J.C. consults for AstraZeneca, Fosun Pharma, GSK, Haleon, Moderna, Novavax, Roche, Sanofi Pasteur, and Pfizer. S.G.S. reports consulting for AstraZeneca, GSK, Moderna, Novavax, Pfizer, Sanofi, CSL Seqirus and Evo Health. S.S.W. has previously received a speaker’s honorarium from Sanofi. D.A.T.C. reports research funding from Merck and Pfizer to his institution for research unrelated to this work. The other authors declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Steven Riley and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
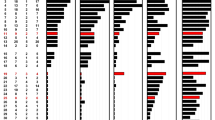
Extended Data Fig. 1 HAI antibody breadth for influenza A(H3N2) infections in ferrets, stratified by the year of isolation for the immunizing viruses.
Dots represent the raw data, and the lines indicate the expected values from the fitted LOESS function. Vertical dashed lines indicate the year of isolation of immunizing viruses. Horizontal dotted lines indicate the titer of 40. Data from the Crick’s reports, Smith et al. 2004, and Fonville et al., 2014 and Fonville et al. 2016 were used5,20,21,23. Numbers in the bracket indicate the number of titrations.
Extended Data Fig. 2 HAI antibody breadth for influenza A(H1N1) in ferrets, by the year of isolation of immunizing viruses.
Dots represent the raw data, and the lines indicate the expected values from the fitted LOESS function. Vertical dashed lines indicate the year of isolation of immunizing viruses. Horizontal dotted lines indicate the titer of 40. Data from the Crick’s reports were used.
Extended Data Fig. 3 Estimated HAI antibody breadth for influenza A(H3N2) viruses in ferrets using antigenic cluster defining virus.
Colored dots and bars indicate the expected values from the log-linear regressions fitted in subsets of each strain with antigenic drift. Grey lines and shades represent the expected values from the log-linear regressions fitted in the primary analysis. Vertical dashed lines indicate the year of isolation of immunizing viruses, while horizontal dashed lines represent a titer of 40.
Extended Data Fig. 4 GMT of HAI cross-reactivity at different years between isolations stratified by of AA substitutions in antigenic cluster transition sites.
Data from the Crick’s reports and GISAID were used. Dots, solid lines, and shaded areas represent the mean titer and 95% confidence intervals from the log-linear regression. Each panel represents one antigenic site, with colours indicating different AA combinations between immunizing and tested viruses at that site. For example, at site 135, ‘KN’ represents lysine for the immunizing virus and asparagine for the tested virus. (a) position 133. (b) position 135. (c) position 145. (d) position 155. (e) position 156. (f) position 158. (g) position 159. (h) position 189. (i) position 193.
Extended Data Fig. 5 GMT of HAI cross-reactivity at different years between isolations stratified by of AA substitutions potential N-linked glycosylation sites.
Data from the Crick’s reports and GISAID were used. Dots, solid lines, and shaded areas represent the mean titer and 95% confidence intervals from the log-linear regression. Each panel represents an antigenic site, with colours denoting distinct combinations of specific AA sequences that could potentially transform into glycosylation sites between the immunizing and tested viruses at that location. For instance, beginning at site 45, ‘NSS +/-‘ indicates the presence of asparagine-serine-serine in the immunizing virus but not in the tested virus. (a) position 45. (b) position 63. (c) position 122. (d) position 126. (e) position 133. (f) position 144. (g) position 158. (h) position 165. (i) position 246.
Extended Data Fig. 6 Longitudinal A(H3N2) antibody landscape changes after infections or vaccinations.
Panels a-c use data from Fonville et al.5, with 12 A(H3N2) PCR-positive individuals (aged 14-72 years). Panels d-f use secondary antisera data from Hinojosa et al.24, with children aged 7-17 years. The study includes 31 unvaccinated children receiving vaccines in the 2015/16 season and 41 children vaccinated in both 2014/15 (A/Texas/50/2012) and 2015/16 (A/Switzerland/9725193/2013) seasons. Panels g-i use secondary antisera data from Ertesvåg et al.25, with children aged 3–17 years. The study includes 42children receiving vaccines in 2012/13 or 2013/14 seasons, with vaccine strain of A/Victoria/261/2011 for both seasons. (a) Average landscapes before and after PCR-positive results, sorted by virus isolation year. Vertical dashed lines indicate PCR-positive result years (2008–2011). Fold changes were calculated using antisera from PCR-positive year and the previous year (same for panel d and g). (b) Aligned landscapes before and after PCR-positive results, sorted by years between virus isolation and PCR-positive results. Yellow shade (based on Fig. 4 estimates) represents expected time span of HAI titers at least 40 after a single infection (same for panel e and h). (c) Aligned landscapes before and after PCR-positive results, sorted by years between virus isolation and first virus encountered (assumed at age 4). (d) Average landscapes before and after vaccinations, sorted by virus isolation year and vaccine history. (e) Aligned landscapes before and after vaccinations, sorted by years between virus isolation and PCR-positive results, stratified by vaccine history. (f) Aligned landscapes before and after vaccinations, sorted by years between virus isolation and first virus encountered, stratified by vaccine history. (g) Average landscapes before and after vaccinations, sorted by virus isolation year. (h) Aligned landscapes before and after vaccinations, sorted by years between virus isolation and PCR-positive results. (i) Aligned landscapes before and after vaccinations, sorted by years between virus isolation and first virus encountered.
Extended Data Fig. 7 Fold change in A(H3N2) HAI titers with the difference in years between virus isolation and infection or vaccinated virus using longitudinal data.
Dots and error bars indicate the mean fold change and standard deviation at each difference in isolation time. Coloured lines and shades indicate the mean and 95% CI of fold change estimated from GAM. (a) Fold change in HAI titers with the difference in years between virus isolation and years with PCR confirmation of A(H3N2) infections. Fold changes were calculated for PCR individuals using antisera collected in and a year prior to the PCR positives (data from Fonville et al.5). (b) Fold change in HAI titers with the difference in years between virus isolation and vaccinations. Data from Ertesvåg et al.25 were used. (c) Fold change in HAI titers with the difference in years between virus isolation and vaccinations, stratified by vaccine history. Data from Hinojosa et al.24 were used.
Supplementary information
Supplementary Information
Supplementary Figs. 1–11 and Tables 1–4.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical Source Data
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, B., Gostic, K.M., Adam, D.C. et al. Breadth of influenza A antibody cross-reactivity varies by virus isolation interval and subtype. Nat Microbiol 10, 1711–1722 (2025). https://doi.org/10.1038/s41564-025-02033-4
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41564-025-02033-4