Abstract
Low-voltage areas (LVAs) in the left atrium may promote atrial fibrillation (AF), but the efficacy of LVA ablation for preventing arrhythmia has not been determined. In the present study, we carried out a multicenter, randomized controlled trial (SUPPRESS-AF) to investigate the efficacy of LVA ablation in patients with persistent AF who had left atrial LVAs. Patients with persistent AF and left atrial LVAs that covered ≥5 cm2 of the left atrial surface on a voltage map after pulmonary vein isolation (PVI) were randomized to undergo LVA ablation (PVI + LVA-ABL group) or not (PVI-alone group) in a 1:1 fashion. Recurrence of AF or atrial tachycardia (AT) was monitored using 24-h Holter electrocardiography (ECG) and twice-daily portable ECG recordings. The primary endpoint was freedom from AF or AT recurrence without antiarrhythmic drug use during 1 year of follow-up. Of 1,347 patients (1,003 males and 344 females) who underwent initial ablation for AF, patients with left atrial LVAs were assigned to the PVI + LVA-ABL (n = 170) or the PVI-alone group (n = 171). Although the PVI + LVA-ABL group demonstrated a numerically higher rate of freedom from AF or AT recurrence compared with the PVI-alone group (61% (95% confidence interval (CI) = 53–68%) versus 50% (95% CI = 42–57%)), this difference did not reach statistical significance (P for log(rank) test = 0.127). There was no difference in the procedure-related serious adverse events between the two groups (1.7% versus 1.8%, P < 0.0001). In conclusion, LVA ablation in addition to PVI did not significantly reduce 1-year AF or AT recurrence in patients with persistent AF with left atrial LVAs. Future studies are needed to identify patients who may receive greater benefit from LVA ablation.
Similar content being viewed by others
Main
Pulmonary vein isolation (PVI) is a standard procedure in ablation for persistent atrial fibrillation (AF), but its therapeutic effect is unsatisfactory1,2,3. Although several pre-specified anatomical ablations or local electrogram-guided ablations have been investigated, none has been determined to be effective3,4,5. Atrial myocardial degeneration such as fibrosis is reported to form extrapulmonary vein AF substrate6,7,8. As the degree of myocardial degeneration in each case varies from site to site9, individualized ablation techniques guided by myocardial degeneration may be effective. Magnetic resonance imaging has demonstrated regional consistency between low-voltage areas (LVAs) and areas with delayed gadolinium enhancement, representing increased extracellular volume such as fibrosis10,11,12. More recently, histological analysis has revealed that atrial myocardial degeneration is observed as an electrophysiological abnormality, including voltage reduction13. Based on these findings, ablation guided by LVAs may reduce AF substrates, leading to the suppression of AF recurrence. Several clinical trials have explored the efficacy of LVA ablation in addition to PVI in patients with persistent AF, but the results have been inconsistent14,15,16. A major criticism of these previous studies was their design, which assigned patients to treatment and nontreatment groups without knowledge of the presence of LVAs. Consequently, these studies may not have sufficiently examined the specific impact of LVA ablation.
To address this issue, we designed a study that specifically enrolled patients with identified LVAs. Randomization was conducted for patients with LVAs at the time of the procedure. The purpose of the present study was to explore the efficacy of LVA ablation in addition to PVI in patients with persistent AF and the presence of LVAs.
Results
A randomized controlled SUPPRESS-AF trial included patients undergoing initial ablation for persistent AF with left atrial LVAs on the voltage map after PVI. The patients were randomly assigned in a 1:1 ratio to undergo LVA ablation (PVI + LVA-ABL group) or not (PVI-alone group). Patients were followed for 12 months using v24-h Holter ECG at 6 and 12 months after ablation and twice-daily rhythm checks with portable ECG from 6 months to 12 months after ablation.
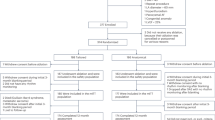
Patients and follow-up
Of 1,347 patients who underwent initial ablation for persistent AF between June 2019 and August 2022, left atrial LVAs were detected in 343 (25.5%) patients (Fig. 1). A total of 342 patients were randomly assigned to either the LVA-ABL group (170 patients) or the PVI-alone group (172 patients) and safety outcomes were assessed. Patient enrollment ended when the target sample size was reached. After excluding one patient who was found to have a history of thromboembolism after randomization and judged ineligible to participate in the study, the efficacy endpoint was assessed in 171 patients. During the 1-year follow-up period, 17 patients dropped out as a result of lack of daily ECG or loss to follow-up at the outpatient clinic. The follow-up protocol was completed in 324 (94.7%) patients. Twice-daily ECG recordings were done almost exactly as pre-specified with a recording rate of 96.0% (81.2%, 100.0%). Antiarrhythmic drugs used during the follow-up period are shown in Extended Data Table 1.
Of 1,347 patients who underwent initial ablation for persistent AF, left atrial LVAs were detected in 343 (25.5%) patients. A total of 342 patients were randomly assigned to either the PVI + LVA-ABL (170 patients) or the PVI-alone group (172 patients) and safety outcomes were assessed. After excluding 1 patient who was found to have a history of thromboembolism after randomization and judged ineligible to participate in the study, the efficacy endpoint was assessed in 170 patients in the LVA-ABL group and 171 patients in the PVI-alone group. During the 1-year follow-up period, 17 patients dropped out. The follow-up protocol was completed in 324 (94.7%) patients.
Baseline characteristics in the two groups were well balanced (Table 1). The mean age was about 74 years and nearly half of the patients were female. Most patients had an AF duration ≤1 year. The mean left atrial diameter was about 44 mm.
Procedural characteristics
Total procedure time, total radiofrequency application time and total applied energy were significantly greater in the PVI + LVA-ABL group than in the PVI-alone group (Table 2). First-pass left- and right-sided PVI rates were nearly 90% in both groups, with no difference between the groups. Mean LVA size was comparable between the two groups. Radiofrequency application time for LVA ablation was approximately 11 ± 5 min and complete LVA ablation was achieved in 78% of patients. Reasons for incomplete LVA ablation were concerns about damage to the esophagus and physiological conduction system, including the His bundle and anterior transverse conduction (Bachman’s bundle) in 29 patients, excessively extensive LVAs in 4 patients and inability to manipulate the ablation catheter to some LVAs in 4 patients. Ablation for regular AT was more frequently performed in the PVI + LVA-ABL group (details of AT origin are in Extended Data Table 2).
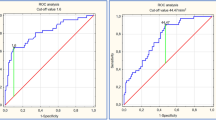
Efficacy endpoints
Kaplan–Meier curves, on the primary endpoint of freedom rate from AF or AT recurrence without antiarrhythmic drug use after a single ablation procedure, showed no statistical difference between groups (P for log(rank) test = 0.127; Fig. 2). At 1 year, the freedom rate from AF or AT recurrence was 61% (95% CI = 53–68%) in the PVI + LVA-ABL group and 50% (95% CI = 42–57%) in the PVI-alone group (Fig. 2a). The hazard ratio (HR) of the PVI + LVA-ABL group to the PVI-alone group was 0.781 (95% CI = 0.564–1.083). HRs adjusted for participating hospitals are listed in Extended Data Table 3.
a, Kaplan–Meier graph showing the primary endpoint of AF or AT recurrence-free rates after the initial ablation without antiarrhythmic drug use. b, Kaplan–Meier graph showing the secondary endpoint of AF or AT recurrence-free rates after multiple ablations without antiarrhythmic use. Comparison of the PVI + LVA-ABL group versus the PVI-alone group was performed using the two-sided, log(rank) test. The unadjusted HR and 95% CI of AF or AT recurrence in the PVI + LVA-ABL group, compared with the PVI-alone group, are also shown.
During a follow-up period of 1 year, 23 of 170 (13.5%) patients in the PVI + LVA-ABL group and 28 of 171 (16.4%) patients in the PVI-alone group underwent multiple ablation procedures: 2 procedures in 20 and 27 patients and 3 procedures in 3 and 1 patients, respectively. The secondary endpoint of freedom rate from AF or AT recurrence without antiarrhythmic drug use, after multiple ablation procedures at 1 year, was 68% (95% CI = 60–75%) in the PVI + LVA-ABL group and 57% (95% CI = 49%–65%) in the PVI-alone group (P for log(rank) test = 0.143; HR = 0.763 (95% CI = 0.526–1.106); Fig. 2b). Freedom rates from AF or AT recurrence with antiarrhythmic drug use after single or multiple ablation procedures did not differ between groups (Extended Data Fig. 1).
Post hoc analysis revealed that, among patients who developed the primary endpoint of AF or AT recurrence after single ablation, the proportion of AT on the first AF- or AT-detected ECG was higher in the PVI + LVA-ABL group (36% (95% CI = 24–49%)) than in the PVI-alone group (18% (95% CI = 10–30%), P = 0.029; Extended Data Fig. 2).
Subgroup analysis
Pre-specified subgroup analysis suggested that the efficacy of LVA ablation was demonstrated in patients aged ≥75 years and those with a CHA2DS2-VASc score ≥ 4, New York Heart Association (NYHA) functional class ≥II, left atrial diameter ≥45 mm, no diabetes mellitus and LVA size ≥20 cm2 (Fig. 3).
Forest plots displaying unadjusted HRs (center squares) and 95% CIs (error bands) of AF or AT recurrence in the PVI + LVA-ABL group compared with the PVI-alone group, as stratified according to pre-specified subgroups. P values for Wald’s test for interaction was also presented. Patients aged ≥75 years, with a CHA2DS2VASc score ≥4, NYHA functional class ≥II, left atrial diameter ≥45 mm, no diabetes mellitus and LVA size ≥20 cm2 had lower AF or AT recurrence rates in the PVI + LVA-ABL group than in the PVI-alone group.
Safety endpoints
There was no difference between the two groups in the safety endpoints of bleeding events, symptomatic stroke or death from any cause, except for periprocedural adverse events, which tended to be more often observed in the PVI + LVA-ABL group than in the PVI-alone group (Extended Data Table 4). Details of periprocedural adverse events are shown in Extended Data Table 5. All six heart failure cases recovered quickly with drug therapy and were discharged after an extended hospital stay of 2–9 d. There was no difference in procedure-related serious adverse events between the two groups. Case presentations of procedure-related serious adverse events are shown in Extended Data Table 6.
Discussion
Several randomized controlled trials have demonstrated inconsistent results on the efficacy of LVA ablation in patients with persistent AF. The STABLE-SR-II trial included 279 patients with persistent AF (133 (47.7%) patients had left atrial LVAs) and reported that LVA ablation in addition to PVI did not improve rhythm outcomes15. The ERASE-AF trial studied 324 patients with persistent AF, including 118 (36.4%) patients with atrial LVAs, and demonstrated fewer AF or AT recurrences in patients allocated to the PVI + LVA-ABL group than in those with PVI alone16. In contrast, the SUPPRESS-AF trial was uniquely designed such that patients with left atrial LVAs on the voltage map after PVI were randomized, allowing efficient validation of the effect of LVA ablation. Durable PVI was ensured by radiofrequency ablation guided by Visitag Surpoint and a resulting high first-pass PVI ratio17,18. In addition, to avoid underestimating AF or AT recurrence, twice-daily portable ECG monitoring, which is known to increase the AF detection rate after ablation19, was incorporated into follow-up ECG monitoring. The study was adequately powered to detect a pre-estimated difference in primary outcome between the two groups.
The LVA is an area of intense atrial tissue degeneration, which is thought to play a role in the development and persistence of AF6,10,11,12,13. The rationale for LVA ablation is that it can selectively modify diseased myocardium, which has individual differences in distribution. However, the SUPPRESS-AF trial failed to show statistical significance of the efficacy of adding LVA ablation to PVI, despite the numerical superiority of the PVI + LVA-ABL group. This suggests that the trial was underpowered to show the resulting efficacy of additional LVA ablation, which was less than initially estimated. Possible reasons why the efficacy of LVA ablation was lower than expected were as follows: first, the essential question of whether LVA ablation can reduce AF substrates has not been fully resolved. All LVAs may not play as an arrhythmogenic substrate and eliminating electrical activity by LVA ablation does not necessarily lead to suppression of the arrhythmic substrate. Second, the atrial arrhythmogenic substrate may not always be confined within LVAs. LVA ablation may therefore leave other substrates that can sustain AF, leading to failure to suppress AF in some cases. This idea is supported by the observation of not a few ATs arising from non-LVA sites such as the right atrium in the PVI + LVA-ABL group. In addition, several clinical studies reported the entire left atrial electrical remodeling (voltage reduction and electrical conduction velocity decrease) in patients with local voltage reduction or LVAs13,20,21. Third, extensive ablation, including LVA ablation, can increase iatrogenic ATs by generating re-entrant substrates such as electrical scars and slow conduction channels22,23,24,25. In the present study, patients in the PVI + LVA-ABL group underwent more AT ablations during the initial ablation and had a higher proportion of AT among AF or AT recurrences during 1 year of follow-up than those in the PVI-alone group. ATs after LVA ablation could have been reduced by using the methods in ERASE-AF16, including connecting nonconducting structures with linear ablation and achieving electrophysiological endpoints such as loss of local capture at a given lesion and bidirectional conduction block for linear ablation.
On the other hand, the efficacy of LVA ablation was demonstrated in subgroups of patients aged ≥75 years, with a CHA2DS2-VASc score ≥4, left atrial diameter ≥45 mm and LVA size ≥20 cm2. Some inferences about the possibility that LVA ablation suppressed AF can be made from the finding that efficacy was greater in patients with advanced atrial remodeling. The importance of LVA as an AF substrate may increase the more extensive it becomes, resulting in LVA ablation having a substantial impact. Alternatively, extensive left atrial ablation itself may effective for the modification of diffuse AF substrate. The opposite view is that maintenance of sinus rhythm cannot be expected even via LVA ablation in patients with extremely advanced atrial remodeling. However, such patients were a minority in the present study where patients had relatively less advanced atrial remodeling in terms of left atrial size and AF duration.
The present study also sheds light on the safety issue of LVA ablation. Procedure time was approximately half an hour longer in the PVI + LVA-ABL group than in the PVI-alone group. Serious, procedure-related, adverse event rates were not increased with the addition of LVA ablation. On the other hand, the incidence of all periprocedural adverse events tended to be higher in the PVI + LVA-ABL than in the PVI-alone group (11 (95% CI = 6.5%) versus 4 (95% CI = 2.3%) patients (odds ratio (OR) = 2.91 (95% CI = 0.91–9.31))) and a larger study may well have found a difference in safety endpoints. The tendency toward a difference between the two groups was mainly the result of minor complications, such as the incidence of heart failure, that were easily managed with medications and complications at the inguinal puncture site, which were probably caused by the longer procedure time and more extensive ablation.
Several limitations of the present study warrant mention. First, as the study was conducted at institutions in Japan, some limitations in generalizing the findings to other populations may be present. Second, several participants dropped out from follow-up visits or portable electrocardiogram recording, possibly because the study was conducted across the coronavirus disease (COVID)-19 pandemic period. Third, AF or AT recurrence was monitored by discontinuous ECG monitoring, giving rise to the possibility that asymptomatic episodes of AF or AT might have been missed. In addition, AF burden, which has recently been considered a meaningful efficacy outcome after ablation, could not be measured. Fourth, the divergence in the Kaplan–Meier curves suggests the possible efficacy of LVA ablation, but was statistically underpowered to detect a difference that was smaller than assumed when the protocol was created. When calculated from the recurrence rates of the LVA ablation and nonablation groups obtained in the present study, a sample size of 630 cases for each study arm would have demonstrated a significant difference. Fifth, LASSO NAV and PentaRay NAV have different electrode properties in terms of interelectrode spacing and arrangement and the recorded signals would not be identical. As a result, the arrhythmogenic implication of LVAs may differ between the two mapping catheters.
In conclusion, LVA ablation in addition to PVI did not significantly reduce 1-year AF or AT recurrence in patients with persistent AF who underwent initial ablation and had left atrial LVAs. Given that the efficacy of LVA ablation may depend on patient characteristics, future studies on improving patient selection for more effective LVA ablation are needed.
Methods
Trial design
A prospective, investigator-initiated, multicenter, randomized, open-label SUPPRESS-AF trial was conducted at eight centers in Japan. The trial protocol has been described previously26. Protocol creation, data monitoring and collection and primary data analysis were performed by the steering team of Osaka Cardiovascular Conference (Osaka University). Roles and responsibilities were agreed among collaborators ahead of the research. Local researchers and clinical research coordinators who were trained before and during the study were involved in the conduct of the study and data management at each site. Data collection was conducted using an electronic data capture system (DATATRAK ONE, Datatrack International). The Osaka University Ethics Committee conducted the central review and approval of the protocol (approval no. 18211) on behalf of other facilities, except for Osaka National Hospital, which conducted the ethics review and approved the protocol (approval no. 21056) independently. The study was sponsored by Biosense Webster through the Investigator Initiated Studies (IIS) program, which had no role in the conduct of the study except for review and approval of protocol creation. The present study complied with the Declaration of Helsinki. The trial protocol and statistical analysis plan are available in the Supplementary Information.
Trial participants
Patients undergoing initial ablation for persistent AF were considered for enrollment. Exclusion criteria were age <20 years, left atrial diameter ≥55 mm, history of cardiac surgery, valvular AF, hemodialysis, contraindication to ablation, contraindication to anticoagulant therapy, history of stroke or systemic embolism within the last 6 months, treatable cause of AF, pregnancy and physician’s judgment of unsuitability for enrollment.
Before the ablation procedure, provisional registration was made and an informed consent form was obtained. Patients with left atrial LVAs (defined as areas with a bipolar peak-to-peak voltage <0.50 mV) covering ≥5 cm2 of the left atrial surface on the voltage map after PVI were then fully enrolled in the study. They were randomly assigned in a 1:1 ratio to LVA ablation after PVI (PVI + LVA-ABL group) or PVI alone (PVI-alone group) immediately after voltage mapping. Randomization allocation was computer generated through a central concealed process and each site was informed online. A minimization method using participating hospitals as an adjustment factor was used so as not to cause large deviation within each hospital.
Interventions
Catheter ablation was performed under a carefully established procedural protocol to minimize variability among facilities and operators. An electroanatomical mapping system (CARTO 3, Biosense Webster) was used for catheter navigation, ablation guidance and mapping. Ipsilateral encircling PVI was performed in all patients using an open-irrigated ablation catheter with a contact force sensor (Thermocool Smarttouch SF, Biosense Webster). Radiofrequency energy application was guided using a Visitag Surpoint module (Biosense Webster). Target Visitag Surpoint was set at ≥425 for the anterior wall and ≥375 for the posterior wall with an interlesion distance of ≤4 mm27. Throughout the ablation procedure, the following VISITAG module setting was used: (1) catheter stability range of motion ≤2 mm, (2) catheter stability duration >5 s or (3) contact force ≥5 g (time ≥25%). After the waiting time of ≥20 min, both entrance and exit blocks were confirmed at each ipsilaterally isolated PV. Electrical cardioversion was performed in cases where AF persisted at the end of the PVI procedure.
After the PVI, left atrial voltage mapping was performed under 100 p.p.m. pacing from the high right atrium. Magnetic sensor-enabled, multielectrode mapping catheters with a 1-mm electrode size (LASSO NAV or PentaRay NAV, Biosense Webster) were used. Mapping points were automatically acquired using the Confidense Module (Biosense Webster) until all color gaps on the voltage map were filled in the following setting: cycle length filtering ±30 ms; local activation time stability 3 ms; position stability 2 mm; density 1 mm; tissue proximity indicator off; and fill and color interpolation threshold 10 mm. LVAs were defined as areas with a bipolar peak-to-peak voltage of <0.5 mV. The scar level was set at 0.05 mV. The area of the LVA was manually measured using the area measurement tool of the CARTO system and, when the total of the LVA area exceeded 5 cm2, it was judged that the left atrium LVA was present.
In the PVI + LVA-ABL group, homogenization ablation covering all LVAs was performed, except for scar areas where mapping points with voltage <0.05 mV concentrated. LVAs located at the posterior wall were allowed to be isolated with top (roof) and bottom lines. Each radiofrequency application was guided by a Visitag Surpoint of ≥350 with an interlesion distance of <6 mm. It was acceptable to omit ablation to sites where ablation could impair physiological electrical conduction system or damage collateral structures, including the esophagus.
After completion of these procedures, induction of AF or AT by atrial burst stimulation and intravenous administration of isoproterenol was performed. Induced AT and nonpulmonary-vein AF triggers could be ablated at the discretion of the attending operator. In addition, cavo-tricuspid isthmus ablation was permitted when tricuspid isthmus-dependent atrial flutter was clinically observed.
Follow-up
Patients were followed for 12 months and were required to visit a cardiology outpatient clinic at 6 and 12 months for medical assessment. A standard 12-lead electrocardiogram in the supine resting position and 24-h Holter ECG during the course of daily life was performed before each outpatient visit. Holter ECG was recorded using two leads: CM5 and NASA. In addition, twice-daily and symptom-driven ECG recordings for 30 s were performed with a portable electrocardiogram (HCG 901 or HCG 801; Omron) from 6 months to 12 months. Patients were instructed to place the electrodes in contact with the index finger and the anterior chest at a few centimeters below the nipple. The portable electrocardiogram recorder is approved by health authorities such as those in the European Union and Japan, and has been used in several clinical studies28,29.
AF or AT recurrence was defined as the occurrence of one of the following events: (1) AF or AT indicated on a scheduled or symptom-triggered electrocardiogram or (2) AF or AT of at least 30-s duration on Holter ECG monitoring. AF or AT episodes during the 3 months after the initial or repeat ablation were not included as recurrence events (blanking period). Antiarrhythmic drug use was not recommended for 3 months after the ablation procedure.
Repeat ablations were allowed for recurrent AF or AT. The procedure was required to be in accordance with the pre-specified protocol. In short, re-isolation of reconnected pulmonary veins followed by left atrial voltage mapping was performed. Ablation targeting residual LVAs was conducted in the PVI + LVA-ABL group, but not in the PVI-alone group. There were no protocol restrictions on other ablation procedures, which could be performed at the discretion of the operator.
Endpoints
The primary endpoint of the study was the recurrence of AF or AT without antiarrhythmic drug use during the 1-year follow-up period after the index ablation procedure. The secondary efficacy endpoint was recurrent AF or AT after repeat ablations. Safety endpoints included death from any cause, symptomatic cerebrovascular stroke or bleeding events during the 1-year follow-up period and any periprocedural adverse events. In addition, procedure-related serious adverse events, including cardiac tamponade, stroke or systemic thromboembolism, esophageal fistula, major bleeding and death, were also defined as safety endpoints. Bleeding events were defined as major bleeding in the ISTH bleeding criteria30 and bleeding requiring hospitalization. Serious adverse events were defined as events that led to death, threatened life or required hospitalization or an extended hospital stay period for treatment.
Statistical analysis
The time to event was compared with the assumption of 1-year AF or AT recurrence-free rates of 75% in the PVI + LVA-ABL group and 60% in the PVI-alone group (HR = 0.56). With a randomization ratio of 1:1, a sample size of 155 participants in each group was required to reject the null hypothesis with a power of 80% and a significance level of 5%. A total sample size of 340 patients was estimated to be required, allowing for some dropouts.
Continuous data are expressed as the mean ± s.d. or median (interquartile range). Categorical data are presented as absolute values and percentages. Analyses were based on the intention-to-treat principle. In primary and secondary efficacy endpoints, unadjusted survival curves were estimated using the Kaplan–Meier method and compared with the use of log(rank) tests. The 1-year AF or AT recurrence-free rate and its 95% CI after the initial or repeat ablation were calculated using Greenwood’s formula. Unadjusted HRs and 95% CIs derived from Cox’s proportional-hazards models were used in primary and secondary efficacy endpoints and subgroup analysis. HRs adjusted for the eight participating hospitals (classified into four groups: the top three hospitals with the highest number of enrolled cases and the remaining five hospitals) were also calculated. For each subgroup analysis, Wald’s test for interaction was performed. Safety endpoints were analyzed using Fisher’s exact test. All tests were conducted at a two-sided α level of 0.05. Procedural characteristics were compared using the unpaired Student’s t-test for continuous variables and the χ2 test or Fisher’s exact test for categorical variables. All analyses were performed using commercial software (SAS v.9.4, SAS Institute Inc.).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The datasets from the present study are not publicly available due to concerns about patient confidentiality and proprietary considerations. Deidentified individual patient-level clinical data will be available on request for academic use with appropriate consideration of patient confidentiality. Responses to enquiries will be made within 1 week. All requests for datasets should be directed to the corresponding author at masuda-masaharu@kansaih.johas.go.jp.
References
Joglar, J. A. et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 149, e1–e156 (2024).
Hindricks, G. et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 42, 373–498 (2021).
Verma, A. et al. Approaches to catheter ablation for persistent atrial fibrillation. N. Engl. J. Med. 372, 1812–1822 (2015).
Kistler, P. M. et al. Effect of catheter ablation using pulmonary vein isolation with vs without posterior left atrial wall isolation on atrial arrhythmia recurrence in patients with persistent atrial fibrillation: the CAPLA Randomized Clinical Trial. JAMA 329, 127–135 (2023).
Vogler, J. et al. Pulmonary vein isolation versus defragmentation: the CHASE-AF clinical trial. J. Am. Coll. Cardiol. 66, 2743–2752 (2015).
Nattel, S. Molecular and cellular mechanisms of atrial fibrosis in atrial fibrillation. JACC Clin. Electrophysiol. 3, 425–435 (2017).
Guichard, J. B. & Nattel, S. Atrial cardiomyopathy: a useful notion in cardiac disease management or a passing fad? J. Am. Coll. Cardiol. 70, 756–765 (2017).
Gorenek, B. et al. European Heart Rhythm Association (EHRA)/European Association of Cardiovascular Prevention and Rehabilitation (EACPR) position paper on how to prevent atrial fibrillation endorsed by the Heart Rhythm Society (HRS) and Asia Pacific Heart Rhythm Society (APHRS). Europace 19, 190–225 (2017).
Nairn, D. et al. Differences in atrial substrate localization using late gadolinium enhancement-magnetic resonance imaging, electrogram voltage, and conduction velocity: a cohort study using a consistent anatomical reference frame in patients with persistent atrial fibrillation. Europace 25, euad278 (2023).
Oakes, R. S. et al. Detection and quantification of left atrial structural remodeling with delayed-enhancement magnetic resonance imaging in patients with atrial fibrillation. Circulation 119, 1758–1767 (2009).
Mahnkopf, C. et al. Evaluation of the left atrial substrate in patients with lone atrial fibrillation using delayed-enhanced MRI: implications for disease progression and response to catheter ablation. Heart Rhythm 7, 1475–1481 (2010).
Zghaib, T. et al. Multimodal examination of atrial fibrillation substrate: correlation of left atrial bipolar voltage using multi-electrode fast automated mapping, point-by-point mapping, and magnetic resonance image intensity ratio. JACC Clin. Electrophysiol. 4, 59–68 (2018).
Takahashi, Y. et al. Histological validation of atrial structural remodeling in patients with atrial fibrillation. Eur. Heart J. 44, 3339–3353 (2023).
Kircher, S. et al. Individually tailored vs. standardized substrate modification during radiofrequency catheter ablation for atrial fibrillation: a randomized study. Europace 20, 1766–1775 (2018).
Yang, G. et al. Circumferential pulmonary vein isolation plus low-voltage area modification in persistent atrial fibrillation: the STABLE-SR-II trial. JACC Clin. Electrophysiol. 8, 882–891 (2022).
Huo, Y. et al. Low-voltage myocardium-guided ablation trial of persistent atrial fibrillation. NEJM Evid. 1, EVIDoa2200141 (2022).
Phlips, T. et al. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace 20, f419–f427 (2018).
Okamatsu, H. et al. Predictors of pulmonary vein non-reconnection in the second procedure after ablation index-guided pulmonary vein isolation for atrial fibrillation and its impact on the outcome. J. Cardiovasc. Electrophysiol. 34, 2452–2460 (2023).
Senoo, K. et al. The impact of home electrocardiograph measurement rate on the detection of atrial fibrillation recurrence after ablation: a prospective multicenter observational study. Int. J. Cardiol. Heart Vasc. 44, 101177 (2023).
Kurata, N. et al. Left atrial localized low-voltage areas indicate whole left atrial electrophysiological degeneration in atrial fibrillation patients. Circ. J. 86, 192–199 (2022).
Kurata, N. et al. Slow whole left atrial conduction velocity after pulmonary vein isolation predicts atrial fibrillation recurrence. J. Cardiovasc. Electrophysiol. 31, 1942–1949 (2020).
Rostock, T. et al. Characterization, mapping, and catheter ablation of recurrent atrial tachycardias after stepwise ablation of long-lasting persistent atrial fibrillation. Circ. Arrhythm. Electrophysiol. 3, 160–169. (2010).
Hung, Y., Chang, S. L., Lin, W. S., Lin, W. Y. & Chen, S. A. Atrial tachycardias after atrial fibrillation ablation: how to manage? Arrhythm. Electrophysiol. Rev. 9, 54–60 (2020).
Chugh, A. Mapping and ablation of post-AF atrial tachycardias. J. Cardiovasc. Electrophysiol. 32, 2830–2844 (2021).
Masuda, M. et al. Additional low-voltage-area ablation in patients with paroxysmal atrial fibrillation: results of the randomized controlled VOLCANO trial. J. Am. Heart Assoc. 9, e015927 (2020).
Sunaga, A. et al. The efficacy and safety of left atrial low-voltage area guided ablation for recurrence prevention compared to pulmonary vein isolation alone in patients with persistent atrial fibrillation trial: design and rationale. Clin. Cardiol. 44, 1249–1255 (2021).
Okumura, K. et al. Acute and mid-term outcomes of ablation for atrial fibrillation with VISITAG SURPOINT: the Japan MIYABI registry. Europace 25, euad221 (2023).
Hussein, A. et al. Use of ablation index-guided ablation results in high rates of durable pulmonary vein isolation and freedom from arrhythmia in persistent atrial fibrillation patients: the PRAISE study results. Circ. Arrhythm. Electrophysiol. 11, e006576 (2018).
Kotecha, D. et al. Integrating new approaches to atrial fibrillation management: the 6th AFNET/EHRA Consensus Conference. Europace 20, 395–407 (2018).
Schulman, S. & Kearon, C. Subcommittee on control of anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. J. Thromb. Haemost. 3, 692–694 (2005).
Acknowledgements
We thank K. Nishio, a statistics specialist, for his thorough support in statistical analysis, the clinical engineers, T. Sumigawa, N. Kurata, Y. Ikada, Y. Kikuchi, A. Shiono and H. Kobayashi, for their dedication in protocol creation and operation of ablation-related equipment according to the protocol, and the clinical research coordinators, N. Yoshioka, S. Kishimoto, K. Tatsumi and Y. Yoshida, for their excellent assistance in data collection, data management and secretarial administration. This work was supported by the Biosense Webster, Inc., through the IIS program 510.
Author information
Authors and Affiliations
Consortia
Contributions
M.M., T.W., H.M., Y.E., S.H., T.D., K.I. and Y. Sakata designed the study. M.M., A.S., S.H., T.D., K.I. and Y. Sotomi. organized and complied the study. M.M., A.S., N.T., T.W., H.M., Y.E., T.O., T.M., T.K., M.O., Y.M. and K.T. performed the clinical research at their respective institutions and contributed to data acquisition. M.M. wrote the paper with an input from all authors. T.Y. performed all statistical analyses. All authors contributed to the interpretation of the results and to paper development and approval of the paper.
Corresponding author
Ethics declarations
Competing interests
Unrelated to the research, M.M. received honoraria from Medtronic and Daiichi Sankyo. M.H. received honoraria from Medtronic and Abbott and technical guidance fees from Phillips and Cook Medical. I.K. received honoraria from Johnson and Johnson. S.Y received honoraria from Nippon Boehringer Ingelheim. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Nicholas Freemantle and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Michael Basson, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 AF/AT-recurrence-free rate with antiarrhythmic use.
a, Kaplan-Meier graph showing AF/AT-recurrence-free rates after the initial ablation with antiarrhythmic drug use. b, Kaplan-Meier graph showing AF/AT-recurrence-free rates after the multiple ablations with antiarrhythmic use. Comparison of the PVI+LVA-ABL group versus PVI-alone group was performed using the two-sided log-rank test. Unadjusted hazard ratios and two-sided 95% CIs of AF/AT recurrence in the PVI+LVA-ABL group compared with the PVI-alone group are also shown. AF/AT indicates atrial fibrillation or atrial tachycardia. AT indicates atrial tachycardia; AF, atrial fibrillation.
Extended Data Fig. 2 Type of recurred atrial tachyarrhythmias.
Proportion of AT on the first-AF/AT-detected ECG was higher in the PVI+LVA-ABL group (36% [24%–49%]) than in the PVI-alone group (18% [10%–30%], p = 0.029). AT indicates atrial tachycardia; AF, atrial fibrillation.
Supplementary information
Supplementary Information
Protocol and statistical analysis plan.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Masuda, M., Sunaga, A., Tanaka, N. et al. Low-voltage-area ablation for persistent atrial fibrillation: a randomized controlled trial. Nat Med 31, 1661–1667 (2025). https://doi.org/10.1038/s41591-025-03674-y
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41591-025-03674-y