Abstract
Nivolumab monotherapy has been approved for the adjuvant treatment of adult patients with urothelial carcinoma who are at high risk of recurrence after undergoing radical resection of urothelial carcinoma based on results of the phase 3 CheckMate 274 trial, in which adjuvant nivolumab versus placebo demonstrated improvement in the primary endpoint of disease-free survival (DFS) in high-risk muscle-invasive urothelial carcinoma (MIUC). Identification of biomarkers associated with treatment outcomes can help refine patient selection, and inform on the immunobiology of disease. To assess the relevance of key biomarkers in the adjuvant MIUC setting, extensive exploratory analyses of tumor biomarkers, including associations with DFS, were performed. Differential gene expression and gene signature analysis found that immune-related genes and pathways, in particular a high interferon-γ signature, were predictive of improved DFS in nivolumab-treated patients. Positive predictive and prognostic associations, respectively, were found for CD4 gene expression and measures of CD8 T cell infiltration. A composite predictive model suggested that high tumor cell PD-L1 expression, high CD4 gene expression, high tumor mutational burden score, receipt of neoadjuvant cisplatin and low transforming growth factor-β gene signature score made the greatest contributions to predicting improved outcomes in nivolumab-treated patients. These results reinforce studies establishing the importance of tumor biomarkers of adaptive immunity in influencing response to PD-1–PD-L1 blockade, indicating the potential predictive rather than solely prognostic nature of such findings. ClinicalTrials.gov identifier: NCT02632409.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data for this study are available upon request. Genomic data are available at the European Genome-Phenome Archive (study, EGAS50000000560; datasets, EGAD50000000792 and EGAD50000000793) upon request, per Bristol Myers Squibb’s internal processes and requirements to comply with patient privacy and regulatory requirements. An independent review committee from Duke Clinical Research Institute will evaluate the proposal based on the scientific rationale and methodology, experience and relevant qualifications of the research team, presence of a robust statistical analysis plan, publication plan and no potential conflicts of interest. If conflicts of interest are present, there is a plan to address them. Before data being released, the researcher(s) will be expected to sign the Vivli Data Use Agreement. Upon execution of an agreement, the de-identified and/or anonymized datasets will be available in the Vivli Research environment: https://vivli.org/ourmember/bristol-myers-squibb/. The Bristol Myers Squibb policy on data-sharing and the data request form can be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html. Response time may vary depending upon the data request.
References
Bajorin, D. F. et al. Adjuvant nivolumab versus placebo in muscle-invasive urothelial carcinoma. N. Engl. J. Med. 384, 2102–2114 (2021).
Galsky, M.D. et al. Adjuvant nivolumab in high-risk muscle-invasive urothelial carcinoma: expanded efficacy from CheckMate 274. J Clin Oncol. 43, 15–21 (2025).
Ono Pharmaceutical Ltd. Ono receives supplemental approval of Opdivo® (nivolumab) for adjuvant treatment of urothelial carcinoma in Japan. Ono Pharma https://www.ono-pharma.com/en/news/20220328.html (2022).
Opdivo (nivolumab), package insert (Bristol Myers Squibb, 2023).
Opidivo (nivolumab), summary of product characteristics (Bristol Myers Squibb, 2023).
Wang, L. et al. EMT- and stroma-related gene expression and resistance to PD-1 blockade in urothelial cancer. Nat. Commun. 9, 3503 (2018).
Wang, L. et al. Myeloid cell-associated resistance to PD-1/PD-L1 blockade in urothelial cancer revealed through bulk and single-cell RNA sequencing. Clin. Cancer Res. 27, 4287–4300 (2021).
Mariathasan, S. et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554, 544–548 (2018).
Banchereau, R. et al. Molecular determinants of response to PD-L1 blockade across tumor types. Nat. Commun. 12, 3969 (2021).
Goswami, S. et al. ARID1A mutation plus CXCL13 expression act as combinatorial biomarkers to predict responses to immune checkpoint therapy in mUCC. Sci. Transl. Med. 12, eabc4220 (2020).
Powles, T. et al. Avelumab maintenance in advanced urothelial carcinoma: biomarker analysis of the phase 3 JAVELIN Bladder 100 trial. Nat. Med. 27, 2200–2211 (2021).
Sharma, P. et al. Nivolumab in metastatic urothelial carcinoma after platinum therapy (CheckMate 275): a multicentre, single-arm, phase 2 trial. Lancet Oncol. 18, 312–322 (2017).
Chakravarthy, A., Khan, L., Bensler, N. P., Bose, P. & De Carvalho, D. D. TGF-β-associated extracellular matrix genes link cancer-associated fibroblasts to immune evasion and immunotherapy failure. Nat. Commun. 9, 4692 (2018).
Galsky, M. D. et al. Nivolumab in patients with advanced platinum-resistant urothelial carcinoma: efficacy, safety, and biomarker analyses with extended follow-up from CheckMate 275. Clin. Cancer Res. 26, 5120–5128 (2020).
Gandara, D. R. et al. Tumor mutational burden (TMB) measurement from an FDA-approved assay and real-world overall survival (rwOS) on single-agent immune checkpoint inhibitors (ICI) in over 8,000 patients across 24 cancer types. J. Clin. Oncol. 41, 2503 (2023).
Morales-Barrera, R. et al. Association of TMB and PD-L1 with efficacy of first-line pembrolizumab (pembro) or pembro + chemotherapy (chemo) versus chemo in patients (pts) with advanced urothelial carcinoma (UC) from KEYNOTE-361. J. Clin. Oncol. 40, 540 (2022).
Doroshow, D. B. et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat. Rev. Clin. Oncol. 18, 345–362 (2021).
Galsky, M. D. et al. Disease-free survival analysis for patients with high-risk muscle-invasive urothelial carcinoma from the randomized CheckMate 274 trial by PD-L1 combined positive score and tumor cell score. Eur. Urol. 83, 432–440 (2023).
Gao, J. et al. Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma. Nat. Med. 26, 1845–1851 (2020).
Kamoun, A. et al. A consensus molecular classification of muscle-invasive bladder cancer. Eur. Urol. 77, 420–433 (2020).
Robertson, A. G. et al. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 171, 540–556 e525 (2017).
Petljak, M. et al. Characterizing mutational signatures in human cancer cell lines reveals episodic APOBEC mutagenesis. Cell 176, 1282–1294 e1220 (2019).
Prosz, A. et al. Mutational signature-based identification of DNA repair deficient gastroesophageal adenocarcinomas for therapeutic targeting. NPJ Precis. Oncol. 8, 87 (2024).
Sun, J. et al. Genomic signatures reveal DNA damage response deficiency in colorectal cancer brain metastases. Nat. Commun. 10, 3190 (2019).
Shi, R. et al. APOBEC-mediated mutagenesis is a favorable predictor of prognosis and immunotherapy for bladder cancer patients: evidence from pan-cancer analysis and multiple databases. Theranostics 12, 4181–4199 (2022).
Han, G. et al. 9p21 loss confers a cold tumor immune microenvironment and primary resistance to immune checkpoint therapy. Nat. Commun. 12, 5606 (2021).
Cristescu, R. et al. Pan-tumor genomic biomarkers for PD-1 checkpoint blockade-based immunotherapy. Science 362, eaar3593 (2018).
Breheny, P. & Huang, J. Group descent algorithms for nonconvex penalized linear and logistic regression models with grouped predictors. Stat. Comput. 25, 173–187 (2015).
Niglio, S. A. et al. Programmed death-1 or programmed death ligand-1 blockade in patients with platinum-resistant metastatic urothelial cancer: a systematic review and meta-analysis. Eur. Urol. 76, 782–789 (2019).
Huang, T.-B. et al. A novel 13-gene signature of TGF-beta pathway correlates with tumor stage and grade and predicts poor survival for bladder cancer patients. Int. J. Clin. Exp. Med. 10, 608–617 (2017).
Oh, D. Y. et al. Intratumoral CD4+ T cells mediate anti-tumor cytotoxicity in human bladder cancer. Cell 181, 1612–1625 e1613 (2020).
Ayers, M. et al. IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Invest. 127, 2930–2940 (2017).
Cohen, M. et al. The interaction of CD4+ helper T cells with dendritic cells shapes the tumor microenvironment and immune checkpoint blockade response. Nat. Cancer 3, 303–317 (2022).
Magen, A. et al. Intratumoral dendritic cell-CD4+ T helper cell niches enable CD8+ T cell differentiation following PD-1 blockade in hepatocellular carcinoma. Nat. Med. 29, 1389–1399 (2023).
Goubet, A. G. et al. Escherichia coli-specific CXCL13-producing TFH are associated with clinical efficacy of neoadjuvant PD-1 blockade against muscle-invasive bladder cancer. Cancer Discov. 12, 2280–2307 (2022).
Marcus, L. et al. FDA approval summary: pembrolizumab for the treatment of tumor mutational burden-high solid tumors. Clin. Cancer Res. 27, 4685–4689 (2021).
Nassar, A. H. et al. Ancestry-driven recalibration of tumor mutational burden and disparate clinical outcomes in response to immune checkpoint inhibitors. Cancer Cell 40, 1161–1172 e1165 (2022).
Valero, C. et al. Response rates to anti-PD-1 immunotherapy in microsatellite-stable solid tumors with 10 or more mutations per megabase. JAMA Oncol. 7, 739–743 (2021).
Spears, M. R., James, N. D. & Sydes, M. R. “Thursday’s child has far to go”-interpreting subgroups and the STAMPEDE trial. Ann. Oncol. 28, 2327–2330 (2017).
Szabados, B. et al. Final results of neoadjuvant atezolizumab in cisplatin-ineligible patients with muscle-invasive urothelial cancer of the bladder. Eur. Urol. 82, 212–222 (2022).
Powles, T. et al. ctDNA guiding adjuvant immunotherapy in urothelial carcinoma. Nature 595, 432–437 (2021).
Phillips, T. et al. Development of an automated PD-L1 immunohistochemistry (IHC) assay for non-small cell lung cancer. Appl. Immunohistochem. Mol. Morphol. 23, 541–549 (2015).
Motzer, R. J. et al. Biomarker analysis from CheckMate 214: nivolumab plus ipilimumab versus sunitinib in renal cell carcinoma. J. Immunother. Cancer 10, e004316 (2022).
Guramare, M. et al. 1282 Concordance analysis of AI-powered CD8 quantification and automated CD8 topology with manual histopathological assessment across seven solid tumor types. J. Immunother. Cancer 10, A1330 (2022).
Lee, G. et al. 387 The utility of AI-powered spatial classification of intratumoral CD8+ immune-cell distribution in predicting overall survival in patients with melanoma as part of the CheckMate 067 clinical trial. J. Immunother. Cancer 9, A420 (2021).
Weber, J., Aldana, R., Gallagher, B. & Edwards, J. Sentieon DNA pipeline for variant detection – software-only solution, over 20× faster than GATK 3.3 with identical results. Preprint at https://doi.org/10.7287/peerj.preprints.1672v1 (2016).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. Preprint at https://arxiv.org/abs/1303.3997 (2013).
Li, H. & Durbin, R. Fast and accurate long-read alignment with Burrows–Wheeler transform. Bioinformatics 26, 589–595 (2010).
Liu, Y. & Schmidt, B. Long read alignment based on maximal exact match seeds. Bioinformatics 28, i318–i324 (2012).
Hellmann, M. D. et al. Tumor mutational burden and efficacy of nivolumab monotherapy and in combination with ipilimumab in small-cell lung cancer. Cancer Cell 33, 853–861. e854 (2018).
Sherry, S. T. et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 29, 308–311 (2001).
Cibulskis, K. et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219 (2013).
Kim, S. et al. Strelka2: fast and accurate calling of germline and somatic variants. Nat. Methods 15, 591–594 (2018).
Cingolani, P. et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin) 6, 80–92 (2012).
Forbes, S. A. et al. COSMIC: somatic cancer genetics at high-resolution. Nucleic Acids Res. 45, D777–D783 (2017).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581, 434–443 (2020).
The 1000 Genomes Project Consortium. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Clark, M. J. et al. Performance comparison of exome DNA sequencing technologies. Nat. Biotechnol. 29, 908–914 (2011).
Chang, H. et al. Bioinformatic methods and bridging of assay results for reliable tumor mutational burden assessment in non-small-cell lung cancer. Mol. Diagn. Ther. 23, 507–520 (2019).
Bergstrom, E. N. et al. SigProfilerMatrixGenerator: a tool for visualizing and exploring patterns of small mutational events. BMC Genomics 20, 685 (2019).
Rosenthal, R., McGranahan, N., Herrero, J., Taylor, B. S. & Swanton, C. DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol. 17, 31 (2016).
Gelman, A. Scaling regression inputs by dividing by two standard deviations. Stat. Med. 27, 2865–2873 (2008).
Zhang, M. et al. Interaction analysis under misspecification of main effects: some common mistakes and simple solutions. Stat. Med. 39, 1675–1694 (2020).
Tian, L., Alizadeh, A. A., Gentles, A. J. & Tibshirani, R. A simple method for estimating interactions between a treatment and a large number of covariates. J. Am. Stat. Assoc. 109, 1517–1532 (2014).
Harrell, F. E. Jr, Lee, K. L. & Mark, D. B. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 15, 361–387 (1996).
Heagerty, P. J., Lumley, T. & Pepe, M. S. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 56, 337–344 (2000).
Acknowledgements
We thank the patients and families who made this study possible; the clinical study teams and the global trial manager; B. Dwivedi, S. Wang and K. H. Eng, who assisted with data analysis verification; A. Chhibber for additional data analysis; G. Lee and PathAI for CD8 topology data generation; M.-S. Chien for whole-exome sequencing pipeline and methodology development; and Dako, an Agilent Technologies, Inc. company, for collaborative development of the PD-L1 IHC 28-8 pharmDx assay (Santa Clara, CA, USA). This study was supported by Bristol Myers Squibb (Princeton, NJ, USA) in collaboration with Ono Pharmaceutical Company Ltd (Osaka, Japan). The sponsor collaborated with the academic authors for the conceptualization, data collection, data generation and interpretation of the analyses. Writing and editorial assistance were provided by N. Belletier, PhD, of Parexel, funded by Bristol Myers Squibb.
Author information
Authors and Affiliations
Contributions
All authors were involved in the conceptualization, data collection, generation or interpretation of the analysis. All authors were involved in the drafting, review and approval of the final draft.
Corresponding author
Ethics declarations
Competing interests
M.D.G. reports consulting roles with BioMotiv, Janssen, Dendreon, Merck, GlaxoSmithKline, Lilly, Astellas Pharma, Genentech, Bristol Myers Squibb (BMS), Novartis, Pfizer, EMD Serono, AstraZeneca, Seattle Genetics, Incyte, Aileron Therapeutics, Dracen, Inovio Pharmaceuticals, NuMab, Dragonfly Therapeutics, Basilea, UroGen Pharma, Infinity Pharmaceuticals, Gilead Sciences and Silverback Therapeutics; stock ownership with Rappta Therapeutics; and research funding with Janssen Oncology, Dendreon, Novartis, BMS, Merck, AstraZeneca and Genentech/Roche. D.F.B. reports consulting roles with Merck, Dragonfly Therapeutics, Fidia Farmaceutici S.p.A. and BMS Foundation; travel with Merck; and research funding to their institution with Novartis, Merck, BMS, AstraZeneca, Astellas Pharma and Seattle Genetics/Astellas. Y.T. reports consulting roles with Eisai, MSD and Ono Pharmaceutical; honoraria with Astellas Pharma, BMS Japan, Chugai Pharma, Novartis and Ono Pharmaceutical; and research funding to their institution with Astellas Pharma, AstraZeneca, Chugai Pharma, Eisai, MSD, Novartis, Ono Pharmaceutical, Pfizer and Takeda. D.Y. declares no conflicts of interest. M.A. declares no conflicts of interest. D.E. reports institution financial interests with Astellas for Bladder Cancer Preceptorship, Bayer for Ra223 advisory board and Janssen for Prostate Cancer UK Summit. A.P. reports being on advisory boards with Astellas, Bayer, BMS, Exelixis, Janssen, Medison Pharma, MSD, Takada and Teva; expert testimony with Roche; and an Institutional research grant from Sanofi (no financial interest). M.M. reports being an advisory board or invited speaker with Elsevier, Loxo/Lilly and Medscape; a co-editor-in-chief with Elsevier; having stocks and shares with Gilead Sciences, Merck and Pfizer; and institutional financial interests from Accuray, Acrivon Therapeutics, Alliance for Clinical Trials in Oncology, Alliance Foundation Trials, ALX Oncology, Amgen, Arvinas, Astellas Pharma, AstraZeneca/MedImmune, Bayer, BMS, Boehringer Ingelheim, Clovis Oncology, Constellation Pharmaceuticals, G1 Therapeutics, Hoosier Cancer Research Network, Incyte, Loxo, Merck, Mirati Therapeutics, Novartis, Prostate Cancer Clinical Trials Consortium, Roche/Genentech and Seagen. K.K. declares no conflicts of interest. M.O.-G. reports honoraria with AstraZeneca, MSD, Pfizer, Ipsen, Merck Serono, EUSA Pharma and Janssen Cilag; consulting roles with AstraZeneca, BMS, Ipsen, MSD, Pfizer, EUSA Pharma, Merck Serono, Takeda, Eisai, Bayer Vital and Janssen Cilag; research funding to their institution with BMS, Intuitive Surgical and Bayer Vital; and travel with BMS, Merck Serono, MSD, Janssen Cilag, Ipsen and AstraZeneca. F.S. reports institutional financial interests with BMS, Ipsen, MSD, Pfizer and Roche for advisory boards; institutional financial interests with BMS for being coordinating principal investigator; and no personal financial interests. J.M.D., J.L., S.D.C., F.N., A.A. and K.Ü.-K. report previous employment with and ownership of stock in BMS. A.N. reports consulting roles with Roche, Janssen, Bayer, Astellas, AstraZeneca, Merck, Clovis Oncology, Incyte and Pfizer; research grant to their institution from Merck, AstraZeneca, Ipsen, BMS and Gilead; and a nonfinancial leadership role with the Global Society of Rare Genitourinary Tumors.
Peer review
Peer review information
Nature Medicine thanks Michiel van der Heijden, Alexander Wyatt and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Ulrike Harjes, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
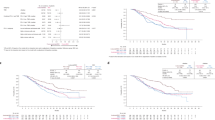
Extended Data Fig. 1 Overview of biomarker analyses and associations between DFS and treatment arm by patient population.
a. Overview of biomarker analyses completed. b. Associations between DFS and treatment arm in all treated patients, the CD8 digital IHC-evaluable population and the CD8 digital IHC non-evaluable population. Shaded areas indicate 95% CI. c. Associations between DFS and treatment arm in all treated patients, the RNA-seq–evaluable population and the RNA-seq non-evaluable population. Shaded areas indicate 95% CI. d. Associations between DFS and treatment arm in all treated patients, the WES-evaluable population and the WES non-evaluable population. Shaded areas indicate 95% CI.
Extended Data Fig. 2 Cox PH models with straight-line assumption to assess the association between biomarkers and DFS.
a. Cox PH model with straight-line assumption for CD8 digital IHC. Overall effect: P < 0.001. Interaction effect: P = 0.590. Shaded areas indicate 95% CI. b. Cox PH model with straight-line assumption for CD4 gene expression. Overall effect: P < 0.001. Interaction effect: P < 0.001. Shaded areas indicate 95% CI. c. Cox PH model with straight-line assumption for the 25-IFNγ GES. Overall effect: P < 0.001. Interaction effect: P = 0.002. Shaded areas indicate 95% CI. d. Cox PH model with straight-line assumption for TMB score. Overall effect: P = 0.001. Interaction effect: P = 0.061. Shaded areas indicate 95% CI. e. Cox PH model with straight-line assumption for the 19-FTBRS GES. Overall effect: P = 0.059. Interaction effect: P = 0.973. Shaded areas indicate 95% CI. f. Cox PH model with straight-line assumption for the 8-EMT/Stroma Core GES. Overall effect: P = 0.640. Interaction effect: P = 0.597. Shaded areas indicate 95% CI. g. Cox PH model with straight-line assumption for the 9-TGFβ Activation GES. Overall effect: P = 0.740. Interaction effect: P = 0.943. Shaded areas indicate 95% CI. h. Cox PH model with straight-line assumption for the 13-High risk TGFβ GES. Overall effect: P = 0.005. Interaction effect: P = 0.204. Shaded areas indicate 95% CI. i. Cox PH model with straight-line assumption for the 4-TLS gene signature. Overall effect: P = 0.006. Interaction effect: P = 0.025. Shaded areas indicate 95% CI.
Extended Data Fig. 3 CD8 topology and 19-FTBRS GES tertiles.
a. Frequency of CD8 topology categories by patient population. b. Distribution of CD8 digital IHC scores by CD8 topology category (n = 445). Curves show mirrored Gaussian kernel density estimates. Boxes extend from the first to third quartiles, middle lines show medians, and whiskers extend to the most extreme data point that is no more than 1.5 times the IQR from the box. c. Kaplan–Meier curves by treatment arm and CD8 topology category. Shaded areas indicate 95% CI. d. Distribution of 19-FTBRS GES scores by CD8 topology category (n = 222). Plot shows first quartile, median, and third quartile, with bars representing 1.5 × IQR. e. Kaplan–Meier curves by 19-FTBRS GES score tertile and treatment arm, for CD8 desert topology. f. Kaplan–Meier curves by 19-FTBRS GES score tertile and treatment arm, for CD8 excluded topology. g. Kaplan–Meier curves by 19-FTBRS GES score tertile and treatment arm, for CD8 inflamed topology.
Extended Data Fig. 4 Differential gene expression profiling.
a. Strength and direction of association between DFS and gene expression in the nivolumab arm versus that in the placebo arm. For each gene, the association in each arm is summarized by log2(HR), where the HR compares estimated hazards at the 75th and 25th percentiles of expression levels (percentiles defined for both arms combined). Positive values indicate that patients with higher expression levels tended to have greater hazard, ie, shorter DFS. Negative values indicate the opposite. Genes with interaction effect FDR ≤ 0.1 (from likelihood ratio tests) are labeled. Not all such gene symbols are shown due to overlap. FDR, false discovery rate. b. The 40 genes with most negative (left panel) or most positive (right panel) difference between log2(HR) for nivolumab (NIVO) and log2(HR) for placebo (PLB) (ie, treatment-gene interaction), among all genes with FDR ≤ 0.1 for a test of that difference. Here, HR is defined as in (a).
Extended Data Fig. 5 APOBEC signature association with DFS.
Plots show HR and 95% CI.
Extended Data Fig. 6 P value comparisons between single-biomarker models that did (y-axis) or did not (x-axis) allow for interactions between biomarkers, treatment, and a six-level factor that combined PD-L1 status, prior cisplatin therapy and tumor site.
The top two panels give results for Cox PH models with a straight-line assumption for biomarker effects. The bottom two panels give results for Cox PH models with restricted cubic splines for biomarker effects. Left panels show –log10(P values) for the test of overall biomarker effect. Right panels show –log10(P values) for the test of biomarker-treatment interaction.
Extended Data Fig. 7 Candidate biomarker correlations.
Correlation matrix depicting Pearson’s correlation coefficients (R) between assessed candidate tumor biomarkers. Values in blue show positive correlation, values in yellow show correlation coefficient estimates close to zero, and values in red show anticorrelation.
Extended Data Fig. 8 Composite model.
a. Median deviance versus log of penalty parameter from 50 repeated random iterations of five-fold cross validation. Error bars represent the median ± the standard deviation across the 50 repeats of cross-validation. b. Model performance by arm. Performance metrics were estimated from 50 repeated random iterations of an outer loop of 10-fold cross-validation. c. Partial-effect plots for continuous-valued predictors in composite model. The y-axis scale matches that for the partial-effect plots from the single-biomarker models to facilitate comparisons.
Supplementary information
Supplementary Information
Supplementary Table 1 and Figs. 1–4.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Galsky, M.D., Bajorin, D.F., Tomita, Y. et al. Adjuvant nivolumab in muscle-invasive urothelial carcinoma: exploratory biomarker analysis of the randomized phase 3 CheckMate 274 trial. Nat Med 31, 3062–3073 (2025). https://doi.org/10.1038/s41591-025-03802-8
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41591-025-03802-8