Abstract
The association between serum free hemoglobin (sfHb) level and white matter hyperintensity (WMH) volume is controversial. This study is to examine this association considering nonlinearity, sex dimorphism, and WMH type. We enrolled 704 older adults among the participants of the Korean Longitudinal Study on Cognitive Aging and Dementia and visitors to the Dementia Clinic of Seoul National University Bundang Hospital. We measured sfHb level in the venous blood and WMH volume (VWMH) using fluid-attenuated inversion recovery magnetic resonance images. The association between sfHb level and periventricular VWMH was linear in men (linear regression; β = − 0.18, p = 0.006) and U-shaped in women (restricted cubic spline; F = 6.82, p < 0.001). sfHb level was not associated with deep VWMH in either sex. These findings were also observed in participants without anemia. To conclude, sfHb level is associated with periventricular VWMH in older adults of both sexes. Maintaining an optimal sfHb level may contribute to the prevention of WMH.
Similar content being viewed by others
Introduction
White matter hyperintensity (WMH) is prevalent in older adults1,2; associated with various adverse outcomes such as stroke, dementia, cognitive decline, and mortality3; and attributed to hypoxia and arteriosclerosis4,5. The levels of hemoglobin, a key oxygen-transport protein, steadily decrease with advancing age6. Thus, a low hemoglobin level may contribute to the development of WMH in older adults by inducing hypoxia and arteriosclerosis7,8.
Although the World Health Organization (WHO) proposed ≥ 13.0 g/dL and ≥ 12.0 g/dL as normal serum free hemoglobin (sfHb) levels in men and women respectively9, the optimal sfHb levels for health-related outcomes were different from the normal sfHb levels proposed by the WHO in older adults. For example, the optimal sfHb levels for increasing survival were ≥ 13.7 g/dL in men and sfHb ≥ 12.6 g/dL in women10, and those for reducing hospitalization and mortality were 14.0–17.0 g/dL in men and 13.0–15.0 g/dL in women11.
Although sfHb may also influence the risk and severity of cerebral WMH, its effect was not consistent in previous studies. To our knowledge, optimal sfHb levels for preventing or reducing cerebral WMH have never been investigated. Three cross-sectional studies investigated the association of sfHb level with the volume of cerebral WMH (VWMH) but their results were not consistent along with the studies. sfHb level showed a U-shaped association with VWMH in one study12 while did not show a linear or non-linear association with VWMH in other two studies13,14. One cross-sectional study found no association between sfHb level and the severity of cerebral WMH measured by a semi-quantitative visual rating scale15. One prospective study found that sfHb level did not influence the change in the severity of cerebral WMH measured by a semi-quantitative visual rating scale over 5-year follow-up period in older adults16. These inconsistencies among the previous studies might be attributable to the differences in the characteristics of participants, such as the age and sfHb level. In addition, several methodological issues should be considered. First, none of the previous studies considered the type of cerebral WMH (periventricular WMH [PVWMH] versus deep WMH [DWMH]) in their analyses despite that PVWMH is more affected by cerebral hypoperfusion than DWMH4,17. Second, three previous studies did not consider the effect of sex on the association between sfHb level and the severity or volume of WMH12,13,14, despite that normal sfHb level and prevalence of anemia are different between men and women6. Third, two studies examined the linear relationship between sfHb level and VWMH only15,16 despite that the relationship between them may be non-linear12. Fourth, two studies measured the severity of cerebral WMH using semi-quantitative visual ratings instead of VWMH15,16. Despite of its clinical usefulness, the visual ratings on the severity of cerebral WMH are less sensitive to subtle differences in VWMH compared to the fully quantitative volumetric measures18.
This study investigated whether the association of sfHb with VWMH are different by the type of cerebral WMH and the sex of the participants under following hypotheses: (a) lower sfHb level is associated with higher VWMH; (b) the association between sfHb level and VWMH may differ between men and women; and (c) the association of sfHb level with the volume of PVWMH (VPVWMH) may be different from that with the volume of DWMH (VDVWMH).
Methods
Study design, setting, and participants
This cross-sectional study included 358 participants from the Korean Longitudinal Study on Cognitive Aging and Dementia (KLOSCAD) and 346 visitors to the Dementia Clinic at Seoul National University Bundang Hospital (SNUBH) from 2010 to 2020. The KLOSCAD is an ongoing prospective cohort study that randomly samples 6818 community-dwelling Korean older adults. The baseline assessment of the KLOSCAD was conducted from 2010 to 2012 and four consecutive 2-year follow-up assessments had been completed in 2013–202119. The participants of KLOSCAD took one or more brain scan at the baseline or follow-up assessments. The first brain scan of each participant was collected for the current study when the participant took two or more brain scans. Data were collected from the follow-up assessments as well as the baseline assessment of the KLOSCAD because some participants took their first brain scan in the baseline assessment while others took their brain scan at one of follow-up assessments. All participants were aged 55 years or older. The participants with a history of hematological (e.g., myelodysplastic syndrome, multiple myeloma, and polycythemia vera) and other malignancies, gastrointestinal tract resection, traumatic brain injury, multiple sclerosis, brain tumor, intellectual disability, and any dementing illnesses were excluded. Compared to the participants from the KLOSCAD, those from the SNUBH Dementia Clinic were older and showed higher prevalence of mild cognitive impairment, systolic blood pressure, VWMH and VPVWMH but lower burden of comorbidities and better estimated glomerular filtration rate (Supplementary Table S1).
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-0912-089-010). All participants were fully informed about the study protocol and provided written informed consent.
Clinical assessments
Geriatric psychiatrists conducted face-to-face standardized diagnostic interviews, physical and neurologic examinations, and routine laboratory tests to all participants using the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet Clinical Assessment Battery20. A consensus panel of geriatric psychiatrists determined the diagnoses of dementia according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria. Trained research nurses assessed the prior and current history of medical illnesses and the burden of comorbidities using the Cumulative Illness Rating Scale (CIRS)21. The trained research nurses also measured the mean systolic and diastolic blood pressure and body mass index (BMI). The estimated glomerular filtration rate was calculated from the serum creatinine level, age, and sex22.
Assessment of sfHb level and anemia
After overnight fasting, trained research nurses collected venous blood samples from the participants for routine laboratory tests, including those for complete blood cell counts, total and high-density lipoprotein cholesterol levels, chemistry panel, thyroid function, and serum folate and vitamin B12 levels and serological tests for syphilis screening. The sfHb concentration in the venous blood was measured by using an ADVIA 2120i system (Siemens, Germany) for the KLOSCAD samples and an XN-9000 Hematology Analyzer (Sysmex, Japan) for the Clinic samples. The anemia was defined as the sfHb level of < 13 g/dL in men and < 12 g/dL in women according to the World Health Organization criteria9.
Magnetic resonance imaging scan acquisition and processing
We obtained brain magnetic resonance imaging (MRI) scans using a 3.0 Tesla scanner (GE SIGNA by GE Healthcare, Milwaukee, WI, USA). Images were acquired using a T1-weighted sequence (echo time = 3.68 ms, repetition time = 25.0 ms, sagittal slice thickness = 1.0 mm) and fluid-attenuated inversion recovery (FLAIR) (echo time = 160 ms, repetition time = 9900 ms, axial slice thickness = 3.0 mm). We measured the intracranial volume using Freesurfer software version 5.3.0.0 (http://surfer.nmr.mgh.harvard.edu).
To segment the WMH, first, we obtained FLAIR images of all participants and we applied a bias correction on the images to correct non-uniformities caused by the bias field owing to different tissue properties and physics of MRI, using the “Segment” tool from Statistical Parametric Mapping software version 8 (SPM8, Wellcome Trust Centre for Neuroimaging, London, UK). We then segmented WMH from bias-corrected FLAIR images by using a fully automated in-house code run on MATLAB 2014a (MATLAB and statistics Toolbox Release 2014a, MathWorks, Inc., Natick, MA) which has been previously shown to work on different protocols from different scanners without any parameter adjustment23. The algorithm started with the brain extraction from FLAIR images and computed the surrogate for the VWMH. The algorithm calculated the optimal threshold intensity for classifying WMH with intensities of normal distribution that corresponded to normal tissues and WMH by applying Bayesian decision rule. It then removed false positive WMH which was located at gray matter or non-cerebral region. We calculated the total VWMH. Meanwhile, we segmented lateral ventricle of every participant from T1-weighted MR images and measured intracranial volume using Freesurfer software version 5.3.0 (http://surfer.nmr.mgh.harvard.edu) which enables fully-automated surface-based cortical segmentation. The lateral ventricle was co-registered and the WMH images were segmented to estimate PVWMH and DWMH volume according to the distance rule24. We classified PVWMH as WMH within 13 mm from lateral ventricle, else was classified as DWMH.
Statistical analysis
We compared the continuous variables and categorical variables between groups using Student’s t-tests and Pearson’s chi-square tests, respectively. We examined the association between sfHb level and cerebral VWMH using linear regression and restricted cubic spline analyses. In both analyses, we adjusted for age, hypertension, diabetes, stroke, CIRS score, drinking status, smoking status, systolic blood pressure, BMI, total cholesterol level, high-density lipoprotein cholesterol level, glomerular filtration rate, and cohort as covariates. In these regression analyses, VWMH was normalized to individuals’ intracranial volumes and log-transformed. As sensitivity analysis, we performed the same linear regression analysis and restricted cubic spline analysis in the following two subgroups of participants as in the total participants: (1) subgroup 1 without anemia or iron supplementation (N = 612) and (2) subgroup 2 without a history of stroke (N = 680). The knots for restricted cubic spline analyses were set at the 5th, 35th, 65th, and 95th percentiles25, and the sfHb levels at the knots were provided in Supplementary Table S2. We performed all statistical analyses using STATA 12.1 (StataCorp LP; College Station, Texas).
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of Seoul National University Bundang Hospital (B-0912-089-010).
Consent to participate
All participants were fully informed about the study protocol and provided written informed consent.
Results
As summarized in Table 1, female participants had a lower sfHb level than male participants. However, the frequency of anemia was comparable between sexes. Female participants showed smaller intracranial volume and VWMH than male participants. However, after adjusting for intracranial volume, the VWMH was comparable between them (p = 0.201 for total WMH; p = 0.208 for PVWMH; p = 0.770 for DWMH).
In male participants, the linear regression models demonstrated that sfHb level was negatively associated with the log-transformed VWMH and VPVWMH. However, this association was not observed for the log-transformed VDWMH (Table 2). Similar findings were observed for the restricted cubic spline models adjusted for the same covariates as those used in the linear regression models (Table 3).
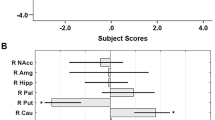
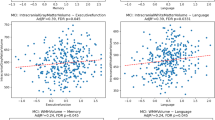
In female participants, the associations between sfHb level and the log-transformed VWMH, VPVWMH, and VDWMH were not significant in the regression models. However, the associations between sfHb level and the log-transformed VWMH and VPVWMH were significant in the restricted cubic spline models adjusted for the same covariates as those used in the linear regression models, indicating that the association may be nonlinear (Table 3). As demonstrated in Fig. 1, which shows the fitted regression with 95% confidence intervals estimated from the restricted cubic spline models, the associations between sfHb level and the log-transformed VWMH and VPVWMH were linear in male participants and U-shaped in female participants.
Serum free hemoglobin level and volumes of white matter hyperintensities. ICV intracranial volume VWMH volume of total white matter hyperintensity, VPVWMH volume of periventricular white matter hyperintensity, VDWMH volume of deep white matter hyperintensity. Restricted cubic spline analyses for the association of serum free hemoglobin level with volumes of white matter hyperintensities. Volumes of total (A), periventricular (B), and deep (C) white matter hyperintensities and serum free hemoglobin level in male older adults, and volumes of total (D), periventricular (E), and deep (F) white matter hyperintensities and serum free hemoglobin level in female older adults. All the volumes were normalized to individuals’ intracranial volumes and log-transformed.
These results did not change when we analyzed subgroups 1 and 2 separately (Tables 2, 3).
Discussion
The results of this study in older adults showed that the association between sfHb level and VWMH was sexually dimorphic and confined to PVWMH. The sfHb level showed a negative linear association with VPVWMH in men and a U-shaped association in women. Furthermore, these associations remained significant when participants without anemia were analyzed separately.
To our knowledge, this is the first study to identify that the association between sfHb level and VWMH differed by the type of WMH. Our findings demonstrated that a lower sfHb level was associated with increasing VPVWMH only in both sexes. This result is in line with a previous study on stroke patients. In stroke patients, sfHb level was associated with VPVWMH, but not with VDWMH26. When the sfHb level decreases, cerebral blood flow increases to compensate for cerebral deoxygenation7,27. As the microvasculature in white matter is scarcer and its’ connection to the pial capillary plexus is longer, more indirect and tortuous than those in gray matter28,29, the compensatory increase of cerebral blood flow against deoxygenation associated with low sfHb level in white matter is far lower than that in cerebral gray matter30. Within cerebral white matter, periventricular white matter is more vulnerable to focal or systemic cerebral hypoperfusion than deep white matter because periventricular white matter has less collateral blood supplies for ventriculofugal vessels than deep white matter31. PVWMH was associated with decreased cortical blood flow but DWMH was not17. The current study suggests that dynamic autoregulation of cerebral blood flow against altered sfHb levels may be more decompensated in periventricular white matter than in deep white matter. The impaired dynamic autoregulation of cerebral blood flow is closely associated with the cerebrovascular risk factors known to increase dementia risk32, and that could partially explain why the PVWMH is more strongly associated with the risk of dementia than DWMH5. Maintaining optimal sfHb level may be beneficial to reduce the risk of PVWMH and cognitive decline associated with PVWMH in older adults.
This study also found the sexually dimorphic association between sfHb level and VPVWMH. Our finding is in line with a previous study reported a sexually dimorphic association between the risk of stroke and sfHb level. In that study, a U-shaped association between the risk of stroke and sfHb level was found in women only33. Regardless of sex, the increase in sfHb level may reduce cerebral blood flow by elevating blood viscosity and activating platelets34. In women, reduced blood estrogen levels by increasing age may weaken the ability to compensate for the reduced cerebral microcirculation associated with a high sfHb level, because estrogen is known to facilitate cerebral microvasculature dilatation and regulates the coagulation pathway35,36. In men, however, serum androgen which constricts brain microvasculature decreases with increasing age. Therefore, older men may have better ability to compensate for the reduced cerebral blood flow induced by high sfHb level than older women36.
The inconsistent results on the sfHb–WMH association in previous studies12,13,14,15,16 may be, at least in part, attributable to the dimorphisms in the sfHb–WMH association by sex and the type of WMH demonstrated in the current study. The sfHb–WMH association with increasing age might have been prominent specifically in this study because of the participants with higher age and lower sfHb level compared to the most previous studies12,13,14,15. In men with the sfHb level below the normal range and women with the sfHb level below or above the normal range, the risk of PVWMH and associated cognitive impairments needs to be evaluated and their abnormal sfHb should be quickly managed. In addition, optimal sfHb levels for men and women should be investigated in future research because the dimorphic sfHb–WMH association was observed in the older adults without anemia.
This study has several limitations. First, this is a cross-sectional design, which limits the interpretation of the causal relationship between sfHb level and VWMH. Second, this study analyzed data from two separate cohorts with different participants and measured sfHb levels using different automated systems. However, our analytic models included cohort as a covariate and still showed significant associations between hemoglobin with WMH. Third, the chronicity and the etiology of low or high sfHb levels were not identified. Finally, this study was limited to the Asian population. As the normal range of hemoglobin and the prevalence of red cell disorders are differentially distributed by ethnicities, our findings should be replicated in various populations.
Summary
Our study provides evidence that sfHb level differentially affects VWMH according to sex and lesion type. Older adults with abnormal sfHb levels may be at high risk of periventricular white matter lesions; thus, modifiable factors should be screened to prevent adverse outcomes related to WMH.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Breteler, M. M. et al. Cerebral white matter lesions, vascular risk factors, and cognitive function in a population-based study: The Rotterdam Study. Neurology 44, 1246–1252. https://doi.org/10.1212/wnl.44.7.1246 (1994).
Longstreth, W. T. et al. Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people. The Cardiovascular Health Study. Stroke 27, 1274–1282. https://doi.org/10.1161/01.str.27.8.1274 (1996).
Debette, S. & Markus, H. S. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ 341, c3666. https://doi.org/10.1136/bmj.c3666 (2010).
Kim, K. W., MacFall, J. R. & Payne, M. E. Classification of white matter lesions on magnetic resonance imaging in elderly persons. Biol. Psychiatry 64, 273–280. https://doi.org/10.1016/j.biopsych.2008.03.024 (2008).
Prins, N. D. & Scheltens, P. White matter hyperintensities, cognitive impairment and dementia: An update. Nat. Rev. Neurol. 11, 157–165. https://doi.org/10.1038/nrneurol.2015.10 (2015).
Patel, K. V. Epidemiology of anemia in older adults. Semin. Hematol. 45, 210–217. https://doi.org/10.1053/j.seminhematol.2008.06.006 (2008).
Hino, A., Ueda, S., Mizukawa, N., Imahori, Y. & Tenjin, H. Effect of hemodilution on cerebral hemodynamics and oxygen metabolism. Stroke 23, 423–426. https://doi.org/10.1161/01.str.23.3.423 (1992).
Sarnak, M. J. et al. Anemia as a risk factor for cardiovascular disease in The Atherosclerosis Risk in Communities (ARIC) study. J. Am. Coll. Cardiol. 40, 27–33. https://doi.org/10.1016/s0735-1097(02)01938-1 (2002).
WHO. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Vitamin and Mineral Nutrition Information System (World Health Organization, 2011).
Zakai, N. A. et al. A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort: The Cardiovascular Health Study. Arch. Intern. Med. 165, 2214–2220. https://doi.org/10.1001/archinte.165.19.2214 (2005).
Culleton, B. F. et al. Impact of anemia on hospitalization and mortality in older adults. Blood 107, 3841–3846. https://doi.org/10.1182/blood-2005-10-4308 (2006).
Wolters, F. J. et al. Hemoglobin and anemia in relation to dementia risk and accompanying changes on brain MRI. Neurology 93, e917–e926. https://doi.org/10.1212/WNL.0000000000008003 (2019).
Kim, J. W. et al. Blood hemoglobin, in-vivo Alzheimer pathologies, and cognitive impairment: A cross-sectional study. Front. Aging Neurosci. 13, 625511. https://doi.org/10.3389/fnagi.2021.625511 (2021).
Tan, B. et al. Haemoglobin, magnetic resonance imaging markers and cognition: A subsample of population-based study. Alzheimers Res. Ther. 10, 114. https://doi.org/10.1186/s13195-018-0440-5 (2018).
Park, S. E. et al. Decreased hemoglobin levels, cerebral small-vessel disease, and cortical atrophy: Among cognitively normal elderly women and men. Int. Psychogeriatr. 28, 147–156. https://doi.org/10.1017/S1041610215000733 (2016).
Inzitari, M. et al. Anemia is associated with the progression of white matter disease in older adults with high blood pressure: The cardiovascular health study. J. Am. Geriatr. Soc. 56, 1867–1872. https://doi.org/10.1111/j.1532-5415.2008.01950.x (2008).
Bahrani, A. A. et al. White matter hyperintensity associations with cerebral blood flow in elderly subjects stratified by cerebrovascular risk. J. Stroke Cerebrovasc. Dis. 26, 779–786. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.10.017 (2017).
van Straaten, E. C. et al. Impact of white matter hyperintensities scoring method on correlations with clinical data: The LADIS study. Stroke 37, 836–840. https://doi.org/10.1161/01.STR.0000202585.26325.74 (2006).
Han, J. W. et al. Overview of the Korean longitudinal study on cognitive aging and dementia. Psychiatry Investig. 15, 767–774. https://doi.org/10.30773/pi.2018.06.02 (2018).
Lee, J. H. et al. Development of the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K): Clinical and neuropsychological assessment batteries. J. Gerontol. B Psychol. Sci. Soc. Sci. 57, 47–53. https://doi.org/10.1093/geronb/57.1.p47 (2002).
Miller, M. D. et al. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the cumulative illness rating scale. Psychiatry Res. 41, 237–248 (1992).
Levey, A. S. et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of diet in Renal Disease Study Group. Ann. Intern. Med. 130, 461–470 (1999).
Yoo, B. I. et al. Application of variable threshold intensity to segmentation for white matter hyperintensities in fluid attenuated inversion recovery magnetic resonance images. Neuroradiology 56, 265–281. https://doi.org/10.1007/s00234-014-1322-6 (2014).
Griffanti, L. et al. Classification and characterization of periventricular and deep white matter hyperintensities on MRI: A study in older adults. Neuroimage 170, 174–181. https://doi.org/10.1016/j.neuroimage.2017.03.024 (2018).
Harrell, F. E. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis 23–24 (Springer, 2001).
Pan, J., Yin, B., Xu, Z. Q., Lou, H. Y. & Liang, H. Hemoglobin is associated with periventricular but not deep white matter hyperintensities in lacunar ischemic stroke. CNS Neurosci. Ther. 19, 632–634. https://doi.org/10.1111/cns.12110 (2013).
Borzage, M. T. et al. Predictors of cerebral blood flow in patients with and without anemia. J. Appl. Physiol. 120, 976–981. https://doi.org/10.1152/japplphysiol.00994.2015 (2016).
Nagata, K. et al. Cerebral circulation in aging. Ageing Res. Rev. 30, 49–60. https://doi.org/10.1016/j.arr.2016.06.001 (2016).
Marin-Padilla, M. The human brain intracerebral microvascular system: Development and structure. Front. Neuroanat. 6, 38. https://doi.org/10.3389/fnana.2012.00038 (2012).
Chai, Y. et al. White matter has impaired resting oxygen delivery in sickle cell patients. Am. J. Hematol. 94, 467–474. https://doi.org/10.1002/ajh.25423 (2019).
Pantoni, L. & Garcia, J. H. Pathogenesis of leukoaraiosis: A review. Stroke 28, 652–659. https://doi.org/10.1161/01.str.28.3.652 (1997).
Bahrani, A. A. et al. Diffuse optical assessment of cerebral-autoregulation in older adults stratified by cerebrovascular risk. J. Biophotonics 13, e202000073. https://doi.org/10.1002/jbio.202000073 (2020).
Panwar, B. et al. Hemoglobin concentration and risk of incident stroke in community-living adults. Stroke 47, 2017–2024. https://doi.org/10.1161/STROKEAHA.116.013077 (2016).
van der Veen, P. H. et al. Hemoglobin, hematocrit, and changes in cerebral blood flow: The second manifestations of ARTerial disease-magnetic resonance study. Neurobiol. Aging 36, 1417–1423. https://doi.org/10.1016/j.neurobiolaging.2014.12.019 (2015).
Frohlich, M. et al. Effects of hormone replacement therapies on fibrinogen and plasma viscosity in postmenopausal women. Br. J. Haematol. 100, 577–581. https://doi.org/10.1046/j.1365-2141.1998.00594.x (1998).
Murphy, W. G. The sex difference in haemoglobin levels in adults—Mechanisms, causes, and consequences. Blood Rev. 28, 41–47. https://doi.org/10.1016/j.blre.2013.12.003 (2014).
Funding
This research was supported by a Grant from the Korean Health Technology R&D Project, Ministry of Health, Welfare, Republic of Korea (Grant No. A092077) and the National Institute of Health research project (project No. 2019-ER6201-01).
Author information
Authors and Affiliations
Contributions
D.J.O., J.S.K., and K.W.K. conceptualized and designed this work. All authors acquired and analyzed the data. D.J.O. and K.W.K. drafted manuscript. All authors have read and approved the final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oh, D.J., Kim, J.S., Lee, S. et al. Association between serum free hemoglobin level and cerebral white matter hyperintensity volume in older adults. Sci Rep 12, 3296 (2022). https://doi.org/10.1038/s41598-022-07325-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-07325-x
This article is cited by
-
Association between hemoglobin levels and cerebral white matter volume in a general older Japanese population: the Iki-Iki study
Neuroradiology (2024)
-
Association between Serum Amyloid A Level and White Matter Hyperintensity Burden: a Cross-Sectional Analysis in Patients with Acute Ischemic Stroke
Neurology and Therapy (2023)