Abstract
Studies investigating the association between type 2 diabetes mellitus and central adiposity are lacking. Therefore, this study aimed to investigate trends in type 2 diabetes mellitus stratified by central adiposity using waist-to-height ratio (WHtR). Trends in type 2 diabetes mellitus were examined by central adiposity, using WHtR, with data from the Korea National Health and Nutrition Examination Survey (2005–2022). Individuals aged 30 years and over who participated in the survey were selected. Type 2 diabetes mellitus was identified based on serum glucose or HbA1c levels, the use of diabetes medications, or a prior diagnosis by a physician. Weighted β-coefficients or odd ratios (ORs) with 95% confidence intervals (CIs) were calculated to assess changes in disease prevalence. A total of 79,368 participants were included in the database (female: 45,163 [56.9%]). from 2005 to 2022, the prevalence of type 2 diabetes mellitus increased from 3.3 to 5.8% in the healthy central adiposity group, from 11.2 to 17.1% in the increased central adiposity group, and from 18.0 to 26.7% in the high central adiposity group. Males, older population, lower education level, lower household income, and smoking are associated with a higher risk of type 2 diabetes. In the high central adiposity group, overweight and obese individuals had higher susceptibility than underweight or normal-weight individuals, with ORs of 5.85 (95% CI, 2.54–13.47) and 8.24 (3.79–17.94), respectively. The prevalence of type 2 diabetes mellitus has increased in all central adiposity groups in the past decade. This underscores the need for tailored interventions to address disparities and improve diabetes management in at-risk populations.
Similar content being viewed by others
Introduction
Central adiposity, defined as the excessive accumulation of fat in the abdominal region, has exhibited a close association with various metabolic disorders, including type 2 diabetes mellitus1,2. High central adiposity is a crucial risk factor for the development of insulin resistance and other metabolic abnormalities that can lead to chronic health conditions; therefore, the increase in its prevalence is alarming3,4. The global prevalence of diabetes has increased steadily5. A similar trend has been observed in South Korea, with the prevalence of diabetes among adults aged ≥ 30 years increasing from 8.6% in 2001 to 16.7% in 20206. This global burden highlights the urgent need to identify factors contributing to high central adiposity and develop effective strategies for preventing and managing the increasing prevalence of type 2 diabetes mellitus.
The waist-to-height ratio (WHtR), a straightforward and effective measure that can predict cardiovascular diseases accurately (including diabetes), is a key indicator used to assess central adiposity7. Some studies suggest that WHtR is a more accurate indicator of health risks than the widely used body mass index (BMI)8. The applicability of WHtR across various age groups and sexes enhances its clinical relevance and practicality9.
We aimed to analyze the prevalence of type 2 diabetes mellitus in Korea from 2005 to 2022 by categorizing individuals by their central adiposity levels as divided by the WHtR. The central adiposity groups were stratified into the healthy, increased, and high central adiposity groups10. The findings of this study will (1) provide detailed insights into the effect of elevated levels of central adiposity on the risk of developing type 2 diabetes mellitus, (2) underscore the importance of managing high central adiposity in the prevention and management of type 2 diabetes mellitus, (3) contribute to the formulation of effective public health strategies, (4) and validate the clinical utility of WHtR in health management guidelines in Korea.
Methods
Patient selection and data collection
Data from the Korea National Health and Nutrition Examination Survey (KNHANES), conducted by the Korea Disease Control and Prevention Agency (KDCA) from 2005 to 2022, was examined in this study11. Individuals aged 30 years and over who participated in the survey were selected based on the criteria used in previous studies12,13. Data regarding sex, age, region of residence, central adiposity group, BMI group, education level, household income, and smoking status were collected for each participant14. A nationally representative sample of 79,368 participants was selected, and the prevalence of type 2 diabetes mellitus was evaluated and stratified by the central adiposity group. The survey, conducted over the span of 18 years, included the following participant counts by year group: 6,960 in 2005–2007, 16,812 in 2008–2010, 14,269 in 2011–2013, 13,408 in 2014–2016, 13,408 in 2017–2019, 4,444 in 2020, 4,421 in 2021, and 4,127 in 2022.
The research protocol was approved by the Institutional Review Boards of the KDCA (2007-02CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, 2013-12EXP-03-5C, 2018-01-03-P-A, 2018-01-03-C-A, 2018-01-03-2C-A, 2018-01-03-5C-A, and 2018-01-03-4C-A) and the local law of the Act (Article 2, Paragraph 1), and Enforcement Regulation (Article 2, Paragraph 2, Item 1) of the Bioethics and Safety Act, Government of Korea. Written informed consent was obtained from all participants before commencing the study. The study protocol adhered to the ethical guidelines established by the relevant national and Institutional Review Boards for human research, as well as the 1975 Helsinki Declaration as amended in 2008. Furthermore, the KNHANES provides public access to its data; therefore, the data can be used for diverse epidemiological investigations.
Definition of type 2 diabetes mellitus
We aimed to examine the annual variations in the prevalence of type 2 diabetes mellitus among individuals aged 30 years and over by three central adiposity groups from 2005 to 2022. Diabetes mellitus was defined as a diagnosis confirmed by a physician within the past year (self-reported), the utilization of oral hypoglycemic agents or the administration of insulin injections (self-reported), a glycated hemoglobin (HbA1c) level of 6.5% or higher (direct measurement), or fasting blood glucose levels of 126 mg/dL or higher (direct measurement). Fasting blood glucose and HbA1c levels were measured through blood tests conducted by KDCA, while information regarding medical diagnoses of diabetes and the use of glucose-lowering medications or insulin injections was collected through self-reported surveys15,16.
To identify patients with type 2 diabetes among those who meet the above criteria, an age criterion has been established. According to the Korean Diabetes Association, the prevalence of diabetes in Korea significantly increases in individuals aged 30 years and older6. Given that approximately 90–95% of diabetes patients worldwide are diagnosed with type 2 diabetes within this age group, this age criterion has been utilized17,18. Individuals who meet the aforementioned diabetes criteria but are under the age of 30 are classified as having type 1 diabetes.
Covariates
The covariates in this study were selected based on relevance to the development of type 2 diabetes mellitus. Sex, age (30–39, 40–49, 50–59, and ≥ 60 years), region of residence (urban and rural), central adiposity groups (underweight, increased adiposity, and high central adiposity), BMI groups (underweight, normal weight, overweight, and obese), education level (based on the highest level of education attained: elementary school or lower, middle school, high school, and college or higher education), household income (lowest, second, third, and highest quartiles)19, and smoking status (current, ex-, and nonsmokers) were the covariates used in this study. Information on sex, age, region of residence, education level, household income, and smoking status was collected through self-reported data obtained from the health and examination surveys, while physical measurements, including height, weight, and waist circumference, were obtained through direct measurement. The participants were categorized as underweight (< 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obese (25.0–34.9 kg/m2) based on their BMI values according to Asia-Pacific guidelines20. WHtR, calculated by dividing the waist circumference by height, was used to categorize the participants into healthy central adiposity (WHtR 0.40–0.49), increased central adiposity (WHtR 0.50–0.59), and high central obesity (WHtR ≥ 0.60) groups according to the guidance from the National Institute for Health and Care Excellence10. These classifications applied to individuals with a BMI of under 35.0 kg/m2 regardless of sex, ethnicity, or muscle mass. Therefore, participants with a BMI above 35.0 kg/m2 were excluded.
Statistical analyses
This study utilized quantitative data from the Korea National Health and Nutrition Examination Survey (KNHANES), categorizing the data into crude with percentage and group-weighted analyses with 95% confidence intervals (CIs) to identify trends in the prevalence of diabetes mellitus by the levels of central adiposity in South Korea. Additionally, a weighted odds ratio (wOR) was calculated for each period to confirm these trends. A weighted linear regression model was applied to compute the β-coefficients for the comparison of periods before and during the COVID–19 pandemic, thus assessing the pandemic’s impact21,22,23.
A stratified analysis was conducted for the following covariates, which were categorized into three groups based on central adiposity classifications: sex, age, region of residence, BMI groups, education level, household income, and smoking status. This analysis facilitated the identification of vulnerable variables associated with central obesity among patients with diabetes mellitus and allowed for an evaluation of the pandemic’s effects. A weighted logistic regression was employed, and the wORs were used to assess the impact of the pandemic. A two-sided p-value of less than 0.05 was considered statistically significant, and all statistical analyses were performed using SAS software (version 9.4; SAS Institute, Cary, NC, USA).
Results
A total of 160,591 participants were surveyed and included in the KHNANES database between 2005 and 2022. However, individuals aged < 30 years were excluded from the dataset in this study according to the age criteria used in previous studies. In addition, 65,642 participants were excluded owing to data regarding age groups, household income, and weight values being missing. Furthermore, 15,581 participants who were under 30 years old were also excluded. Therefore, the final sample comprised 79,368 individuals (Figure S1).
Table 1 indicates the baseline characteristics of the participants over the 18-year period: sex (34,205 [43.10%] males and 45,163 [56.90%] females), age (30–39 years, 14,830 [18.69%]; 40–49 years, 16,833 [21.21%]; 50–59 years, 17,064 [21.50%]; and ≥ 60 years, 30,641 [38.61%]) and central adiposity groups (healthy central adiposity group, 33,207 [41.84%]; increased central adiposity group, 39,807 [50.16%]; and high central adiposity group, 6,354 [8.01%]).
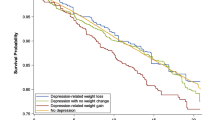
Table 2; Fig. 1 present the prevalence of type 2 diabetes mellitus in the central adiposity groups, comparing data for the periods before and during the COVID-19 pandemic from 2005 to 2022. The prevalence of type 2 diabetes mellitus in the healthy, increased, and high central adiposity group increased from 3.32% (95% CI, 2.57 to 4.07) in 2005–2007 to 5.80% (95% CI, 4.67 to 6.93) in 2022, 11.22% (95% CI, 9.91 to 12.53) to 17.07% (95% CI, 15.36 to 18.78), and 18.00% (95% CI, 13.82 to 22.19) to 26.70% (95% CI, 21.96 to 31.44), respectively. Therefore, an increased prevalence of type 2 diabetes mellitus was observed during the study period (Table S1). A specific sub-analysis, comparing the periods of 2017–2019 and 2020–2022 separately, also observed similar trends (Table S2).
Table 3 shows the factors associated with an increased risk of type 2 diabetes mellitus in each central adiposity group. Advanced age, lower educational attainment, lower household income, and current or former smoking status were identified as statistically significant risk factors for an increased likelihood of type 2 diabetes mellitus across all three groups. Furthermore, the risk of type 2 diabetes mellitus was higher in males than females in all groups. Compared with individuals in their 30s, individuals aged ≥ 60 years (ratio of ORs 17.72 [95% CI, 13.63 to 23.05]) exhibited a significantly higher risk of type 2 diabetes mellitus in the healthy central adiposity group. Furthermore, residing in rural areas and being overweight increased the risk of type 2 diabetes mellitus in the increased central adiposity group. Compared with those who were underweight or normal weight, individuals who were overweight (ratio of ORs 5.85 [95% CI, 2.54 to 13.47]) or obese (ratio of ORs 8.24 [95% CI, 3.79 to 17.94]) exhibited a significantly higher risk of type 2 diabetes mellitus in the high central adiposity group. However, when comparing the β values by dividing the entire year into pre-pandemic and pandemic periods, significant differences were observed among the three central groups. Otherwise, when analyzing the wOR for each period, the significant intervals varied, and no common significant period was identified (Table S3). The risk of type 2 diabetes mellitus tended to increase across all assessed variables; however, the individuals in the increased and high central adiposity groups were more susceptible to type 2 diabetes than the healthy central adiposity group (Table S4).
Discussion
Key findings
This study used KNHANES data for an 18-year period spanning from 2005 to 2022 to analyze the trend of type 2 diabetes mellitus by stratifying central adiposity into the healthy, increased, and high central adiposity group (n = 79,368). The prevalence of type 2 diabetes mellitus increased from 3.32 to 5.80%, 11.22–17.07%, and 18.00–26.70% in the healthy, increased, and high central adiposity group, respectively. The risk of developing type 2 diabetes mellitus was consistently associated with the following socio-demographic factors: older population (≥ 60 years), middle school or lower education level, lower household income, and smoking. In the healthy central adiposity group, susceptibility to developing type 2 diabetes mellitus increased significantly with age. Therefore, various factors, particularly aging, increase the risk of developing type 2 diabetes mellitus, even in the healthy central obesity groups. In addition, the risk of developing type 2 diabetes mellitus was higher in males than in females. Furthermore, only in individuals with high central adiposity was an increased risk of developing type 2 diabetes mellitus with higher BMI observed; this association was inconsistent in other groups.
Comparison with previous studies
Compared to previous studies, our findings corroborate existing research that indicates an increasing prevalence of type 2 diabetes mellitus across various socio-demographic groups and levels of central adiposity. The role of reduced physical activity, unhealthy dietary habits, and socioeconomic factors in exacerbating the risk of developing type 2 diabetes has been consistently emphasized in previous studies24,25. These factors contribute to the development of insulin resistance and metabolic dysfunction, which are central to the development of diabetes.
Several recent studies have highlighted significant sex differences in the risk of developing diabetes. For instance, research has consistently shown that males exhibit higher rates of abdominal obesity and associated insulin resistance compared to females26,27. This aligns with our findings, which reveal that males are more susceptible to developing type 2 diabetes mellitus across all levels of central obesity. Furthermore, the literature underscores a progressive increase in diabetes risk with aging28,29,30,31. Our study corroborates these findings and emphasizes the heightened vulnerability of older adults, including those who initially have healthy central adiposity. The findings of the present study confirm these trends and emphasize the significant vulnerability of older adults, even those with initially healthy central adiposity.
In the context of obesity and diabetes mellitus risk, obesity is closely linked to a high prevalence of type 2 diabetes and its complications32. Various anthropometric methods and surrogate adipose indices are used to assess the risk of diabetes and insulin resistance33. BMI is one of the most commonly used clinical measures for determining obesity. However, previous studies have found that the WHtR correlates significantly better with body fat than BMI34,35.
Our study supports existing findings regarding the WHtR. When evaluating and analyzing central fat using WHtR, a significant increase in the risk of type 2 diabetes was observed only in patients with high central obesity across all BMI categories. While both BMI and WHtR can be utilized to assess diabetes prevalence based on levels of obesity, our results suggest that WHtR is more sensitive in evaluating obesity and more effectively captures diabetes prevalence. This underscores the importance of using both WHtR and BMI together to understand the impact of central obesity on the prevalence of type 2 diabetes.
Similar patterns have emerged internationally. In Japan, the rising prevalence of type 2 diabetes has been accompanied by an increase in central obesity, despite BMI levels remaining relatively stable, reinforcing the stronger association between abdominal obesity and diabetes risk36. In China, WHtR has proven more effective than BMI and waist-to-hip ratio (WHR) in predicting cardiovascular risk in patients with diabetes37. Furthermore, research from the UK indicates that WHtR is not only a more effective indicator than BMI for diabetes risk but also a simpler and more reliable metric for identifying a range of other health conditions38.
Additionally, we compared the trends of type 2 diabetes in Korea with other countries. Globally, the prevalence of type 2 diabetes has been increasing due to factors such as rising rates of overweight individuals and shifts in dietary habits6,39,40. Countries such as the UK, Ireland, and Luxembourg had reported a more than 1.2 fold increase in diabetes prevalence by 2019 compared to 199041. Similarly, in the U.S., the prevalence of type 2 diabetes increased from 9.8% during 1999–2000 to 14.3% by 2017–2018, primarily attributed to a substantial rise in obesity rates and widening socioeconomic disparities42,43. Likewise, our study showed an increase in the prevalence of type 2 diabetes in South Korea, from 8.74% in 2005–2007 to 15.19% in 2022.
Plausible underlying mechanisms
In our study, we observed an increasing trend in the prevalence of type 2 diabetes mellitus was observed in all central adiposity groups with significantly higher prevalence observed in 2022 compared to 2005. This increase could be attributed to lifestyle changes over the past decades, including increased consumption of high-calorie, processed foods, which contributed to weight gain and central adiposity44,45. Additionally, the aging population and prolonged exposure to risk factors such as sedentary behavior and unhealthy dietary habits likely played a significant role in the rising prevalence of type 2 diabetes mellitus46.
This study showed that several socio-demographic increased susceptibility to type 2 diabetes across all central adiposity groups. Individuals with lower education levels and household incomes may possess limited health knowledge and access to healthcare, further exacerbating their risk of developing type 2 diabetes mellitus47. These groups may have encounter barriers in obtaining the information and resources necessary for the prevention and management of the disease, hindering early detection and appropriate treatment of type 2 diabetes mellitus. Nicotine, a major physiologically active component of tobacco, may disrupt glucose homeostasis and lead to abnormalities in glucose metabolism48,49. Moreover, males exhibit a higher vulnerability of developing type 2 diabetes mellitus compared to females across all levels of central adiposity. Females are more likely to accumulate adipose tissue in the hips and thighs, while males tend to accumulate fat in the abdominal region. Abdominal obesity is associated with insulin resistance, which is generally higher in males than in females50.
We found that the risk of developing type 2 diabetes mellitus increased with age in all adiposity groups. Specifically, in our study, the healthy central adiposity group showed a significant risk of type 2 diabetes among the older population (≥ 60 years) compared to those in their 30s. This finding suggests that the risk of developing type 2 diabetes mellitus increases significantly in the 60s due to aging, even in individuals with healthy central obesity51. Furthermore, the findings of this study suggest that the individuals in the increased central adiposity group are likely to develop diabetes at an earlier age than those in the healthy central adiposity group but still later than those with high central adiposity. Individuals with high central adiposity may develop diabetes much earlier. This progression indicates that the onset of type 2 diabetes mellitus occurs earlier as the central adiposity levels increase52. Factors such as the decline in metabolic functions, increased insulin resistance, decreased physical activity, hormonal changes, and chronic inflammation collectively heighten the risk of developing type 2 diabetes in aging individuals. Therefore, individuals with high central adiposity are significantly more susceptible to developing early-onset diabetes than those with increased or healthy central adiposity.
Interestingly, this study found that an increased risk of developing type 2 diabetes mellitus associated with higher BMI was only observed in the high central adiposity group. While BMI is commonly used to measure overall body fat, it may have limitations in accurately reflecting central adiposity, as it does not account for the distribution of fat53. This is particularly relevant, given that central adiposity—defined as fat accumulation in the abdominal area— has been associated with an increased risk of metabolic disorders, such as type 2 diabetes and cardiovascular disease. In contrast, WHtR offers an additional assessment of central adiposity by considering waist circumference in relation to height. Research indicates that WHtR may be a more effective predictor of health risks associated with obesity, especially those linked to abdominal fat accumulation34,54. Therefore, this study suggests that using both BMI and WHtR in combination could improve the identification of individuals at higher risk for metabolic complications, thereby supporting more targeted prevention and management strategies.
Clinical and policy implications
The present study highlights the need for increased screening and monitoring of type 2 diabetes mellitus among individuals with high central adiposity. Healthcare professionals should use WHtR alongside BMI for a more precise risk assessment. Regular monitoring and targeted screening may facilitate early detection and intervention. Personalized lifestyle modifications are crucial for the older population (≥ 60 years) with high central adiposity. Enhancing health education and support systems is vital for effective diabetes risk management. Public health campaigns that promote physical activity and healthy eating habits, particularly among low-income populations, are essential for disease prevention. Furthermore, policy measures should aim to improve access to healthcare and incorporate WHtR into clinical guidelines to enhance health outcomes.
Strength and limitations
This study has several limitations. First, as a cross-sectional study, it does not allow for tracking changes within the same individuals, which limits our ability to understand how factors such as aging, lifestyle changes, or urbanization may influence the development or progression of diabetes over time. For example, although we analyzed prevalence trends before and after the COVID-19 pandemic, we were unable to assess how individual risk factors evolved or contributed to changes in diabetes prevalence55,56,57. To better understand these dynamic relationships, future studies employing longitudinal data would be necessary to elucidate the temporal effects of urbanization and other evolving factors on type 2 diabetes mellitus risk58, stratified by WHtR. Second, the study focused on individuals aged 30 and above, aligning with the standard age range for adult type 2 diabetes mellitus in many existing studies. Consequently, the 0–29 years age group was excluded, which omitted information regarding changes in the prevalence of type 2 diabetes mellitus among younger individuals and related prevention strategies. While the KNHANES dataset does not distinguish between diabetes types, analyzing individuals aged 30 and older aligns with prior studies for targeting type 2 diabetes59,60. However, this focus facilitated a more precise analysis of adults with type 2 diabetes mellitus. Third, type 2 diabetes mellitus is influenced by various lifestyle and environmental factors. Due to a lack of data, we were unable to account for all relevant factors; however, this analysis included other lifestyle-related factors such as BMI and smoking. Additionally, the dataset utilized in the study is unable to classify the specific types of diabetes mellitus. This presents a potential limitation in the approach, as individuals with other forms of diabetes mellitus may be misclassified as having type 2 diabetes. Although this issue may only affect a small subset of cases, it nonetheless restricts the accuracy of the classification of type 2 diabetes cases. Lastly, the use of self-reported data introduces potential recall and social desirability biases. Recall bias may lead to inaccuracies, while social desirability bias may compel respondents to provide answers they perceive as more acceptable to others rather than reflecting their true thoughts or behaviors56.
Despite these limitations, the strength of this study lies in the use of nationwide representative data spanning 18 years to monitor the prevalence trends of type 2 diabetes mellitus, stratified by level of central adiposity. We present representative trends for South Korea based on comprehensive nationwide data collected over an extended period. Furthermore, we examined the sociodemographic factors and their association with central obesity in patients with type 2 diabetes mellitus, identifying older age, low education level, low household income, and smoking status as significant risk factors. Finally, this study emphasizes the importance of identifying and managing risk factors related to central obesity in patients with type 2 diabetes mellitus.
Conclusion
This study identified an increasing prevalence of type 2 diabetes mellitus in all central adiposity groups from 2005 to 2022, including during the COVID-19 pandemic. Specifically, the prevalence of type 2 diabetes mellitus rose from 3.32 to 5.80% in the healthy central adiposity group, from 11.22 to 17.07% in the increased central adiposity group, and from 18.00 to 26.70% in the high central adiposity group over this period. Our study found that socio-demographic factors such as older age (≥ 60 years), lower education levels, lower household income, and smoking universally increase the risk of developing type 2 diabetes mellitus, with males being more susceptible than females, regardless of central adiposity levels. This study contributes to developing more effective diabetes screening and management strategies by emphasizing the importance of using WHtR alongside BMI for risk assessment and advocating for targeted interventions and policy measures to improve health outcomes among individuals with high central adiposity.
Data availability
The data are available upon request. Study protocol and statistical codes: Available from DKY (yonkkang@gmail.com). Dataset: Available from the Korea Disease Control and Prevention Agency through a data use agreement. Korea National Health and Nutrition Examination Survey is public available as followed link: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do.
References
Wan, H. et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc. Diabetol. 19, 118. https://doi.org/10.1186/s12933-020-01095-4 (2020).
Oh, J. et al. National and regional trends in the prevalence of type 2 diabetes and associated risk factors among Korean adults, 2009–2021. Sci. Rep. 13, 16727. https://doi.org/10.1038/s41598-023-43353-x (2023).
Lechner, K., Lechner, B., Crispin, A., Schwarz, P. E. H. & von Bibra, H. Waist-to-height ratio and metabolic phenotype compared to the Matsuda index for the prediction of insulin resistance. Sci. Rep. 11, 8224. https://doi.org/10.1038/s41598-021-87266-z (2021).
Jang, W. et al. Awareness, treatment, and control of type 2 diabetes in South Korea (1998 to 2022): Nationwide cross-sectional study. JMIR Public. Health Surveill. 10, e59571. https://doi.org/10.2196/59571 (2024). Prevalence.
Williams, J. & Loeffler, M. Global trends in type 2 diabetes, 2007–2017. JAMA. 322, 1542–1542. https://doi.org/10.1001/jama.2019.16074 (2019).
Bae, J. H. et al. Diabetes fact sheet in Korea 2021. Diabetes Metab. J. 46, 417–426. https://doi.org/10.4093/dmj.2022.0106 (2022).
Kim, K. K. et al. Evaluation and treatment of obesity and its comorbidities: 2022 Update of clinical practice guidelines for obesity by the Korean Society for the study of obesity. J. Obes. Metab. Syndr. 32, 1–24. https://doi.org/10.7570/jomes23016 (2023).
Zhang, F. L. et al. Strong association of waist circumference (WC), body mass index (BMI), waist-to-height ratio (WHtR), and waist-to-hip ratio (WHR) with diabetes: A population-based cross-sectional study in Jilin Province, China. J Diabetes Res 8812431 (2021). https://doi.org/10.1155/2021/8812431
Zong, X. et al. Establishing international optimal cut-offs of waist-to-height ratio for predicting cardiometabolic risk in children and adolescents aged 6–18 years. BMC Med. 21, 442. https://doi.org/10.1186/s12916-023-03169-y (2023).
Gibson, S. & Ashwell, M. A simple cut-off for waist-to-height ratio (0·5) can act as an indicator for cardiometabolic risk: Recent data from adults in the Health Survey for England. Br. J. Nutr. 123, 681–690. https://doi.org/10.1017/s0007114519003301 (2020).
Kang, J. et al. National trends and Prevalence of atopic dermatitis and pandemic-related factors among Korean adults, 2007–2021. Int. Arch. Allergy Immunol. 185, 320–333. https://doi.org/10.1159/000535666 (2024).
Lawler, T. et al. Type 2 diabetes and colorectal cancer risk. JAMA Netw. Open 6, e2343333–e2343333. https://doi.org/10.1001/jamanetworkopen.2023.43333 (2023).
Kaptoge, S. et al. Life expectancy associated with different ages at diagnosis of type 2 diabetes in high-income countries: 23 Million person-years of observation. Lancet Diabetes Endocrinol. 11, 731–742. https://doi.org/10.1016/S2213-8587(23)00223-1 (2023).
Park, S. et al. National trends in physical activity among adults in South Korea before and during the COVID-19 pandemic, 2009–2021. JAMA Netw. Open 6, e2316930. https://doi.org/10.1001/jamanetworkopen.2023.16930 (2023).
Ko, S. H. et al. Diabetes mellitus in the elderly adults in Korea: Based on data from the Korea National Health and Nutrition Examination Survey 2019 to 2020. Diabetes Metab. J. 47, 643–652. https://doi.org/10.4093/dmj.2023.0041 (2023).
Hwang, J. & Shon, C. Relationship between socioeconomic status and type 2 diabetes: Results from Korea National Health and Nutrition Examination Survey (KNHANES) 2010–2012. BMJ Open. 4, e005710. https://doi.org/10.1136/bmjopen-2014-005710 (2014).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98. https://doi.org/10.1038/nrendo.2017.151 (2018).
Bragg, F. et al. Blood pressure and cardiovascular diseases in Chinese adults with type 2 diabetes: A prospective cohort study. Lancet Reg. Health West. Pac. 7, 100085. https://doi.org/10.1016/j.lanwpc.2020.100085 (2021).
Yun, S. & Oh, K. The Korea National Health and Nutrition Examination Survey data linked cause of death data. Epidemiol. Health. 44, e2022021. https://doi.org/10.4178/epih.e2022021 (2022).
Eum, S. & Rhee, S. Y. Age, ethnic, and sex disparity in body mass index and waist circumference: a bi-national large-scale study in South Korea and the United States. Life Cycle. 3, e4. https://doi.org/10.54724/lc.2023.e4 (2023).
Lee, S. W. Methods for testing statistical differences between groups in medical research: Statistical standard and guideline of life cycle committee. Life Cycle. 2, e1. https://doi.org/10.54724/lc.2022.e1 (2022).
Lee, S. W. Regression analysis for continuous independent variables in medical research: Statistical standard and guideline of life cycle committee. Life Cycle. 2, e3. https://doi.org/10.54724/lc.2022.e3 (2022).
Hong, S. et al. National prevalence of smoking among adolescents at tobacco tax increase and COVID-19 pandemic in South Korea, 2005–2022. Sci. Rep. 14, 7823. https://doi.org/10.1038/s41598-024-58446-4 (2024).
Forouhi, N. G., Misra, A., Mohan, V., Taylor, R. & Yancy, W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ. 361, k2234. https://doi.org/10.1136/bmj.k2234 (2018).
Gallardo-Gómez, D. et al. Optimal dose and type of physical activity to improve glycemic control in people diagnosed with type 2 diabetes: A systematic review and Meta-analysis. Diabetes Care. 47, 295–303. https://doi.org/10.2337/dc23-0800 (2024).
Tramunt, B. et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 63, 453–461. https://doi.org/10.1007/s00125-019-05040-3 (2020).
Meisinger, C. et al. Sex differences in risk factors for incident type 2 diabetes mellitus: The MONICA Augsburg cohort study. Arch. Intern. Med. 162, 82–89. https://doi.org/10.1001/archinte.162.1.82 (2002).
Palmer, A. K. & Jensen, M. D. Metabolic changes in aging humans: Current evidence and therapeutic strategies. J. Clin. Investig. 132, https://doi.org/10.1172/jci158451 (2022).
Bellary, S., Kyrou, I., Brown, J. E. & Bailey, C. J. Type 2 diabetes mellitus in older adults: Clinical considerations and management. Nat. Rev. Endocrinol. 17, 534–548. https://doi.org/10.1038/s41574-021-00512-2 (2021).
Sun, H. et al. IDF Diabetes atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119. https://doi.org/10.1016/j.diabres.2021.109119 (2022).
Kim, T. H. et al. Association between glucagon-like peptide-1 receptor agonists and risk of suicidality: A comprehensive analysis of the global pharmacovigilance database. Diabetes Obes. Metab.https://doi.org/10.1111/dom.15864 (2024).
Ong, K. L. et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the global burden of disease study 2021. Lancet. 402, 203–234. https://doi.org/10.1016/S0140-6736(23)01301-6 (2023).
Cornier, M. A. et al. Assess adiposity. Circulation 124, 1996–2019. https://doi.org/10.1161/CIR.0b013e318233bc6a (2011).
Sun, K. et al. Assessment of adiposity distribution and its association with diabetes and insulin resistance: A population-based study. Diabetol. Metab. Syndr. 11, 51. https://doi.org/10.1186/s13098-019-0450-x (2019).
Sang, H. et al. Prediction model for cardiovascular disease in patients with diabetes using machine learning derived and validated in two independent Korean cohorts. Sci. Rep. 14, 14966. https://doi.org/10.1038/s41598-024-63798-y (2024).
Hara, K. et al. Trends of HbA1c and BMI in people with type 2 diabetes: A Japanese claims-based study. Diabetes Ther. 15, 801–817. https://doi.org/10.1007/s13300-024-01543-4 (2024).
Ma, Y. L. et al. Waist-to-height ratio is a simple and practical alternative to waist circumference to diagnose metabolic syndrome in type 2 diabetes. Front. Nutr. 9, 986090. https://doi.org/10.3389/fnut.2022.986090 (2022).
Ashwell, M. & Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 6, e010159. https://doi.org/10.1136/bmjopen-2015-010159 (2016).
Veit, M., van Asten, R., Olie, A. & Prinz, P. The role of dietary sugars, overweight, and obesity in type 2 diabetes mellitus: A narrative review. Eur. J. Clin. Nutr. 76, 1497–1501. https://doi.org/10.1038/s41430-022-01114-5 (2022).
Abarca-Gómez, L., Abdeen, Z. A., Hamid, Z. A., Abu-Rmeileh, N. M., Acosta-Cazares, B., Acuin, C,. Adams, R. J., Aekplakorn, W. , Afsana, K., Aguilar-Salinas, C. A. & Agyemang, C. Worldwide trends in body-mass index, underweight, overweight, and obesity from. to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 390, 2627–2642. https://doi.org/10.1016/s0140-6736(17)32129-3(2017) (1975).
Goodall, R. et al. Trends in type 2 diabetes mellitus disease burden in European Union countries between 1990 and 2019. Sci. Rep. 11, 15356. https://doi.org/10.1038/s41598-021-94807-z (2021).
Wang, L. et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999–2018. JAMA. 326, 1–13. https://doi.org/10.1001/jama.2021.9883 (2021).
Hill-Briggs, F. et al. Social determinants of health and diabetes: A scientific review. Diabetes Care. 44, 258–279. https://doi.org/10.2337/dci20-0053 (2020).
Santos, L. The impact of nutrition and lifestyle modification on health. Eur. J. Intern. Med. 97, 18–25. https://doi.org/10.1016/j.ejim.2021.09.020 (2022).
Konieczna, J. et al. Longitudinal association of changes in diet with changes in body weight and waist circumference in subjects at high cardiovascular risk: The PREDIMED trial. Int. J. Behav. Nutr. Phys. Act. 16, 139. https://doi.org/10.1186/s12966-019-0893-3 (2019).
O’Hearn, M. et al. Incident type 2 diabetes attributable to suboptimal diet in 184 countries. Nat. Med. 29, 982–995. https://doi.org/10.1038/s41591-023-02278-8 (2023).
Yao, R. et al. Inequities in health care services caused by the adoption of digital health technologies: Scoping review. J. Med. Internet Res. 24, e34144. https://doi.org/10.2196/34144 (2022).
Yuan, S. & Larsson, S. C. A causal relationship between cigarette smoking and type 2 diabetes mellitus: A mendelian randomization study. Sci. Rep. 9, 19342. https://doi.org/10.1038/s41598-019-56014-9 (2019).
Maddatu, J., Anderson-Baucum, E. & Evans-Molina, C. Smoking and the risk of type 2 diabetes. Transl Res. 184, 101–107. https://doi.org/10.1016/j.trsl.2017.02.004 (2017).
Ahmed, B., Sultana, R. & Greene, M. W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 137, 111315. https://doi.org/10.1016/j.biopha.2021.111315 (2021).
Zhong, P. et al. Normal-weight central obesity and risk of cardiovascular and microvascular events in adults with prediabetes or diabetes: Chinese and British cohorts. Diabetes Metab. Res. Rev. 39, e3707. https://doi.org/10.1002/dmrr.3707 (2023).
Cao, C. et al. Association between central obesity and incident diabetes mellitus among Japanese: A retrospective cohort study using propensity score matching. Sci. Rep. 12, 13445. https://doi.org/10.1038/s41598-022-17837-1 (2022).
Jiang, J. et al. Relationship of obesity to adipose tissue insulin resistance. BMJ Open. Diabetes Res. Care. 8, https://doi.org/10.1136/bmjdrc-2019-000741 (2020).
Hou, Z. H. et al. Is waist-to-height ratio better than body mass index as a predictive indicator of coronary atherosclerosis disease? A cohort study. J. Cardiovasc. Comput. Tomogr. 13, 188–189. https://doi.org/10.1016/j.jcct.2019.06.009 (2019).
Oh, J. et al. Hand and oral hygiene practices of South Korean adolescents before and during the COVID-19 pandemic. JAMA Netw. Open. 6, e2349249. https://doi.org/10.1001/jamanetworkopen.2023.49249 (2023).
Yon, D. K. et al. Indoor exposure and sensitization to Formaldehyde among Inner-City children with increased risk for asthma and rhinitis. Am. J. Respir Crit. Care Med. 200, 388–393. https://doi.org/10.1164/rccm.201810-1980LE (2019).
Lee, J. H. et al. National trends in sexual intercourse and usage of contraception among Korean adolescents. World J. Pediatr. https://doi.org/10.1007/s12519-024-00810-5 (2024).
Woo, H. G. et al. National trends in sadness, suicidality, and COVID-19 pandemic-related risk factors among South Korean adolescents from 2005 to 2021. JAMA Netw. Open. 6, e2314838. https://doi.org/10.1001/jamanetworkopen.2023.14838 (2023).
Fan, T., Koro, C. E., Fedder, D. O. & Bowlin, S. J. Ethnic disparities and trends in glycemic control among adults with type 2 diabetes in the U.S. from 1988 to 2002. Diabetes Care. 29, 1924–1925. https://doi.org/10.2337/dc05-2238 (2006).
Yang, J. J. et al. Association of Diabetes with all-cause and cause-specific mortality in Asia: A pooled analysis of more than 1 million participants. JAMA Netw. Open 2, e192696. https://doi.org/10.1001/jamanetworkopen.2019.2696 (2019).
Acknowledgements
None.
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT; RS-2023-00248157) and the MSIT (Ministry of Science and ICT), Korea, under the ITRC (Information Technology Research Center) support program (IITP-2024-RS-2024-00438239) supervised by the IITP (Institute for Information & Communications Technology Planning & Evaluation). The funders played no role in the study design, data collection, data analysis, data interpretation, or manuscript writing.
Author information
Authors and Affiliations
Contributions
Dr. Dong Keon Yon had complete access to all study data and bore responsibility for the integrity and accuracy of the data analysis. The final version of the manuscript was approved by all authors before submission. Study concept and design: HK, SP, JH, and DKY; Acquisition, analysis, or interpretation of data: HK, SP, JH, and DKY; Drafting of the manuscript: HK, SP, JH, and DKY; Critical revision of the manuscript for important intellectual content: all authors; Statistical analysis: HK, SP, JH, and DKY; Study supervision: HK, SP, JH, and DKY. DKY supervised the study and serves as the guarantor. Hyunjee Kim and Seoyoung Park contributed equally as first authors. Jiyoung Hwang, Lee Smith and Dong Keon Yon contributed equally as corresponding authors. Lee Smith is the senior author. The corresponding authors affirms that all listed authors meet the authorship criteria, and no other authors meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
The research protocol was approved by the Institutional Review Boards of the KDCA (2007-02CON-04-P, 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C, 2013-07CON-03-4C, 2013-12EXP-03-5C, 2018-01-03-P-A, 2018-01-03-C-A, 2018-01-03-2C-A, 2018-01-03-5C-A, and 2018-01-03-4C-A) and by, local law of the Act (Article 2, Paragraph 1), and Enforcement Regulations (Article 2, Paragraph 2, item 1) of the Bioethics and Safety Act, from Korean government. Written informed consent was obtained from all participants prior to their participation. Furthermore, KNHANES provides public access to its data, which can be used as a valuable resource for diverse epidemiological investigations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H., Park, S., Park, J. et al. National trends in type 2 diabetes mellitus stratified by central adiposity using waist-to-height ratio in South Korea, 2005–2022. Sci Rep 14, 24273 (2024). https://doi.org/10.1038/s41598-024-75002-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-75002-2
Keywords
This article is cited by
-
Family history of non-communicable diseases and the risk of cardiovascular-kidney-metabolic syndrome
Scientific Reports (2025)