Abstract
Erythroderma is a severe and heterogeneous inflammatory skin condition with little guidance on the approach to management in cases of unknown etiology. To guide therapeutic selection, we sought to create an immunophenotyping platform able to identify aberrant cell populations and cytokines in subtypes of erythroderma. We performed high-parameter flow cytometry on peripheral blood mononuclear cells (PBMCs) and whole blood of a patient with refractory idiopathic erythroderma, erythrodermic patients with Sézary syndrome and pityriasis rubra pilaris, and healthy controls. We found that the index patient had a novel form of erythroderma characterized by increased interleukin (IL)-13- and IL-17-producing γVδ2 T cells, basophils, and activated platelets. Whole-genome sequencing of PBMCs and immunofluorescence staining of skin biopsies revealed increased expression of Th2- (IL-13, IL-4Rα) and Th17-associated markers (IL-17, IL-17Rα) and non-functional mutations associated with Th2 and Th17 signaling, demonstrating that PBMCs can reflect cutaneous disease pathology. Targeted intervention via dual dupilumab and secukinumab therapy resulted in complete disease control and reduction of immunopathogenic cell populations and cytokines. This study highlights a novel form of erythroderma with concomitant Th2 and Th17 dysregulation and introduces a minimally invasive peripheral blood-based immunophenotyping platform that offers a personalized medicine approach to the management of systemic inflammatory diseases.
Similar content being viewed by others

Introduction
Erythroderma is a severe and potentially life-threatening skin disorder characterized by diffuse erythema and inflammation involving a majority of the skin surface area. The annual incidence of erythroderma in adults is estimated at 1–2 per 100,000 persons. It is a heterogeneous condition, with common etiologies including drug hypersensitivity reaction, psoriasis, contact dermatitis, and atopic dermatitis. Less common causes include pityriasis rubra pilaris (PRP) and Sézary syndrome (SS), a form of cutaneous T cell lymphoma (CTCL)1,2,3.
Although there are non-specific therapies such as methotrexate, cyclosporine, oral retinoids, and phototherapy that can be used in all types of erythroderma, effective management is often heavily reliant on identifying and treating the underlying cause, which often consists of targeting disease-specific immune signatures. For example, erythrodermic atopic dermatitis features a predominantly T-helper (Th)-2 signature and can benefit from agents such as dupilumab, an interleukin (IL)-4 receptor alpha antagonist that inhibits the signaling of the Th2-associated cytokines IL-4 and IL-134,5. Conversely, erythrodermic psoriasis is characterized by Th1 and Th17 activation and is therefore commonly treated with IL-17, IL-23, and tumor necrosis alpha (TNF-α) inhibitors6,7,8. Similarly to psoriasis, erythrodermic patients with PRP have pathogenic activation of the IL-23/IL-17 axis and elevated TNF- α, and can therefore also benefit from TNF-α, IL-23, and IL-17 targeted biologics9,10. Finally, in patients with erythrodermic SS, treatment can target the pathogenic clonal T cells via immunostimulatory therapies such as interferon which enhances Th1 responses, or via monoclonal antibodies such as mogamulizumab, brentuximab vedotin, and alemtuzumab which bind various cell surface markers associated with malignant T cells11. Unfortunately, the etiology of erythroderma remains unknown in up to 36% of cases, with no specific treatments for idiopathic erythroderma and a lack of diagnostic modalities to guide therapeutic choice12. These patients suffer because providers are unable to target the underlying pathophysiology.
We report the case of an otherwise healthy 68-year-old male who presented with recalcitrant idiopathic erythroderma involving 80% of his body surface area, associated with severe pruritus and burning pain. Extensive medical workup including complete blood count with differential, comprehensive metabolic panel, skin biopsy, clinical flow cytometry, T cell receptor sequencing, and discontinuation of medications associated with cutaneous hypersensitivity reactions revealed no clear etiology. Initial treatment with prednisone 60 mg daily and intramuscular triamcinolone provided little benefit. Subsequently, the patient failed to improve on two months of PUVA, adalimumab 40 mg weekly, and acitretin 20 mg daily, as well as oral methotrexate, exhausting many of the commonly utilized treatment options for idiopathic erythroderma12. We thus sought to create an immunophenotyping platform able to identify pathogenic, targetable immune cell populations and cytokine signatures in various subtypes of erythroderma in order to guide the selection of targeted therapeutics from the many available monoclonal antibodies and small molecule inhibitors approved for other therapeutic indications.
We utilized high-parameter flow cytometric analysis to identify immunopathogenic signatures in the index patient, and compared this immune signature to erythrodermic controls (PRP and SS) and healthy controls. The index patient’s unique peripheral blood immune signature included increased IL-13 and IL-17 produced primarily by γVδ2 T cells, increased basophils, and unique IgE- and MRGPRX2-expressing granulocytic populations. Our immunophenotyping platform also identified unique pathogenic features of the erythrodermic controls, differentiating the index patient from PRP and SS. In the index patient, dual therapy with dupilumab and secukinumab, biologic inhibitors of IL-13 and IL-17, respectively, resulted in disease clearance and reduction of immunopathogenic populations. These results highlight a non-invasive, peripheral blood-based systemic immunophenotyping platform with the capability to identify unique immunopathogenic cell populations and cytokine signatures. Utilization of a similar approach may aid clinicians by guiding the selection of targeted therapies in the management of idiopathic erythroderma and other systemic inflammatory diseases.
Results
To identify immune cell composition and immunopathogenic populations in the index patient, functional immunophenotyping via high-parameter flow cytometry was performed and compared with erythrodermic controls (PRP and SS) as well as healthy controls with no known history of inflammatory or pruritic dermatologic conditions (n = 3) (Fig. 1A). Flow cytometric analysis was performed on peripheral blood mononuclear cells (PBMCs) stimulated with a pan-T stimulation (phorbol 12-myristate 13-acetate [PMA]-ionomycin) to characterize T cell differentiation, and on PBMCs stained with antigen-presenting cell (APC)-focused markers to characterize macrophages, monocytes, and dendritic cells (DCs)13. To further examine the granulocytic population, flow cytometric analysis was performed on the patients’ whole blood. The schematic outline is shown in Fig. 1B.
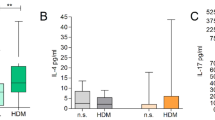
Flow cytometric analysis of Th immune profile reveals a unique immune cell phenotype in erythroderma of unknown etiology. (A) Clinical presentation of index patient and erythrodermic controls. PRP, pityriasis rubra pilaris; SS, Sézary syndrome. (B) PBMC and whole blood flow cytometry study design. (C) Representative flow plots of stimulated or unstimulated CD3 + T cells expressing Th cytokines (IL-4, IL-13, IL-17, and IFN-γ) (D) Representative flow plots of stimulated or unstimulated CD3 + T cells expressing TGF-β and IL-10 in the index patient and controls. (E) Bar plots showing percentages of patient immune cell populations, stratified by percentage of IL-13-producing or IL-17-producing T cells.
Functional analysis of T cells reveals combined Th2 and Th17 dysregulation in the index patient
We assessed the peripheral blood T cell immune profile by evaluating intracellular IL-4, IL-13, IL-17, and interferon (IFN)-γ in PMA-ionomycin stimulated and unstimulated CD3+ T cells of the index patient, erythrodermic controls, and healthy controls13. The gating strategy for flow cytometric analysis of the CD3+ T cell populations and their associated cytokines is depicted in Supplementary Figure S1. In the index patient, stimulated T cells expressed more IL-13 (15.11%) and IL-17 (6.21%) when compared to healthy controls (mean 3.17% and 1.70% for IL-13 and IL-17, respectively), PRP (4.48% and 2.55%), and SS (12.71% and 4.82%) (Fig. 1C). Unstimulated T cells in the index patient also showed greater activation of IL-10-producing CD3+ regulatory T cells (4.90%) compared to healthy controls (0.73%), PRP (2.58%), and SS (2.78%) (Fig. 1D), suggesting an activated immune response. To identify the cellular source of the index patient’s elevated IL-4 and IL-13, we examined IL-4- and IL-13-secreting cells. When stratified by type of CD3+ IL-13-secreting cell, the index patient had an elevated population of clonal γVδ2 T cells (3.13%) as compared to healthy (mean 0.13%) or erythrodermic controls (0.00% SS, 0.30% PRP). Additionally, among the stratified types of CD3+ IL-17-producing cells, the index patient had the highest level of clonal γVδ1 T cells (46.80%) and γVδ2 T cells (1.21%) compared to all other patient populations examined, and only the index patient and PRP patient demonstrated any clonal γVδ2 T cells (Fig. 1E). These findings suggest that γVδ T cells are a likely source of the pathogenic IL-13 and IL-17 in the index patient.
Cutaneous immune profiling and whole-genome sequencing reveal combined Th2 and Th17 dysregulation in the index patient
Immunofluorescence staining of skin biopsies revealed increased cutaneous expression of IL-17 and IL-17Rα, as well as IL-13 and IL-4Rα in the index patient compared to healthy controls (Fig. 2A-F). These findings suggest functional signaling of IL-13 and IL-17 in the skin. To evaluate the genetic composition of the index patient, we performed whole-genome sequencing of PBMCs. Analysis of all single-nucleotide polymorphisms, deletions, and insertions in the index patient revealed missense and intronic mutations related to IL-4, IL-13, and IL-17 cytokines, as well as their associated signaling pathways (Supplementary Tables S1-S2).
Immunofluorescent staining of skin biopsies reveals cutaneous dysregulation of the Th2 and Th17 immune axes in erythroderma of unknown etiology. (A) Immunofluorescence co-staining of IL-17 and IL-17Rα in the lesional skin of the index patient and healthy controls. (B) Representative immunofluorescence images showing individual and overlaid immunofluorescence staining for IL-17 and IL-17Rα in the index patient and healthy control; yellow staining in “Merge” demonstrates overlay of IL-17Rα and IL-17. (C) Immunofluorescence co-staining of IL-13 and IL-4Rα in the lesional skin of the index patient and healthy controls (n = 3). (D) Representative immunofluorescence images showing individual and overlaid immunofluorescence staining for IL-13 and IL-4Rα in the index patient and healthy control; yellow staining in “Merge” demonstrates overlay of IL-13 and IL-4Rα. (E) Hematoxylin and eosin staining of the index patient’s skin biopsy. (F) Bar graphs showing arbitrary units of fluorescence intensity of IL-17, IL-17Rα, IL-13, and IL-4Rα in the index patient and healthy control.
Functional immunophenotyping and single cell clustering analysis of PBMCs show distinct T cell profiles in patients with erythroderma
Dimensionality reduction algorithms, including Uniform manifold approximation and projection (UMAP) plots of T cell immune populations, were utilized to cluster subpopulations of CD3+ PBMCs (Fig. 3A)14. The individual markers in the panel used to identify these subpopulations are visualized in Fig. 3B. We identified differences in the T cell subpopulations between the index patient, erythrodermic controls, and healthy controls which can be visualized in Fig. 3C. The index patient had increased γδ T cells (22% vs. 9.11% in SS, 6.71% in PRP, and mean 6.7% in healthy controls) (Fig. 3D), including γVδ1 (16.76% vs. 8.07%, 4.5%, and mean 4.74%) and γVδ2 (2.8% vs. 0.25%, 0.5%, and mean 0.34%) clonal T cell subpopulations (Fig. 3E), compared to the healthy and erythrodermic controls.
High-parameter flow cytometric analysis of stimulated T cells reveals distinct immune profiles in various forms of erythroderma.
(A) Uniform manifold approximation and projection (UMAP) plot of T cell immune populations combined in the index patient, erythroderma controls, and healthy controls. (B) UMAP plot of the expression of each individual marker characterizing functional T cell immune populations. (C) UMAP plot of the differences in T cell immune populations between the index patient, erythrodermic controls, and healthy controls. (D) Bar plots showing percentages of subtypes of CD3 + T cells in the patients. (E) Subpopulations of the percentage of CD3 + T cell types shown in d: γVδ T cells are stratified by γVδ1TCR and γVδ2TCR cells. CD4 T cells are stratified by naive CD4 (CD3 + CD4 + CD45RA+) and memory CD4 (CD3 + CD4 + CD45RO+) T cells. CD8 T cells are stratified by naive CD8 (CD3 + CD8 + CD45RA+) and memory CD8 (CD3 + CD4 + CD45RO+) T cells. (F) FlowSOM metaclustering algorithm demonstrating similarities and differences in the T cell immune populations between each group. Each coded color represents an overlay of the immune cell populations and metaclusters. (G) Bar plots showing the abundance of the metaclusters between the groups.
To further compare the immune signatures in the index patient and other erythrodermic patients, FlowSOM meta-clustering was used to cluster CD3+ T cell immune populations in each group, yielding 10 meta-clusters (Fig. 3F-G)15. Both the PRP and SS controls demonstrated similarity to the index patient in some subpopulations of T cells. PRP shared Cluster 1 of naive and memory CD4+ T cells (Fig. 3F), and SS shared Cluster 10 of naive CD8+ T cells and Cluster 7 of CD4+ T- cells (Fig. 3F) with the index patient. However, there were also differences in the CD3 + T cell subpopulations between the index, PRP, and SS patients. This is demonstrated by clusters 4, 5, and 6, which consist of γδ T cells and NK T cells exhibiting exclusive expression in the index patient (Fig. 3F). These data suggest that functional immunophenotyping and single cell clustering analysis from PBMCs can identify distinct T cell profiles in patients with erythroderma.
Functional immunophenotyping and single cell clustering analysis of whole blood show distinct granulocytic and monocytic immune cell populations in patients with erythroderma
Immunophenotyping of granulocytic and monocytic immune cell populations was performed via high-parameter flow cytometry of whole blood from the index patient, erythrodermic controls, and healthy controls. Additional functional markers, specifically immunoglobulin E (IgE) and Mas-related G protein-coupled receptor member X2 (MRGPRX2), which are known mediators of itch, were examined to identify different immunopathogenic mediators of this patient’s presentation16. The gating strategy for whole blood flow cytometric analysis is depicted in Supplementary Figure S2.
Results revealed uniquely increased basophils in the index patient (17.4% of live singlets vs. 6.67% in SS, 2% in PRP, and mean 7% in healthy controls) (Fig. 4A). Additionally, activated platelets were elevated in the index patient (18.2%) and SS (14.2%), mast cells were elevated in PRP (46.9%) and SS (46.7%), and overall MRGPRX2 expression was increased in the index patient (25.1%) and SS (25.6%) (Fig. 4A-B).
High-parameter flow cytometric analysis of granulocytic and monocytic immune cell populations from whole blood reveals distinct immune profiles in various forms of erythroderma.
(A) Bar plots showing percentages of subtypes of granulocytic and monocytic cell populations in the index patient and controls; DC, dendritic cells. (B) Bar plots showing expression of MRGPRX2 and IgE in the index patient and controls; MRGPRX2, Mas-related G protein-coupled receptor member X2; Ig, immunoglobulin.
High-parameter flow cytometric analysis of APCs reveals active glycolysis with increased IL-6 and IL-12 cytokines in erythroderma patients
To investigate the immunophenotype of antigen-presenting cells (APCs), we performed high-parameter flow cytometric analysis with an APC-targeted panel on PBMCs from the index patient, erythrodermic controls, and healthy controls (Supplementary Figure S3A). The gating strategy for monocytes, macrophages, and DCs is shown in Supplementary Figure S4. The functional APC immune populations for all samples collectively were visualized by T-distributed stochastic neighbor embedding (tSNE) plot (Supplementary Figure S3B), and then stratified by those present in the index patient and controls (Supplementary Figure S3C). The percentages of macrophages, monocytes, DCs, and plasmacytoid dendritic cell (pDC) cells were not significantly different across erythrodermic patients and healthy controls (Supplementary Figure S3D). All patients with erythroderma had increased percentages of glycolytically active macrophages and pDCs (Supplementary Figure S3E-G), as well as a greater percentage of IL-6- and IL-12-producing macrophages, with the index patient demonstrating the greatest increase (Supplementary Figure S3H-I). Correlation of markers and their relative density of expression in the APCs is visualized by heatmap (Supplementary Figure S3J).
Dual inhibition of IL-4Rα and IL-17 results in clinical improvement of the index patient
Prior to this study, the index patient was treated with numerous systemic medications, including immunosuppressants and antimetabolites, with minimal response. Based on our immunophenotyping results, he was started on dupilumab, a monoclonal antibody which inhibits IL-4 and IL-13 signaling via IL-4 receptor alpha subunit (IL-4Rα) blockade, and secukinumab, a monoclonal antibody which selectively binds IL-17 A and prevents its interaction with the IL-17 receptor. Initial dosing was 300 mg of dupilumab every 2 weeks and 300 mg of secukinumab weekly. The frequency of secukinumab administration was tapered to once every 4 weeks, resulting in flares between dosing. At present, he remains disease-free on a regimen of dupilumab every two weeks and secukinumab every three weeks. Figure 5 A demonstrates the clinical course of the index patient through three time intervals. After 4 months of dual therapy (T2), erythema improved significantly and itch severity decreased from 10/10 to 0/10 on the Worst Itch Numeric Rating Scale17. Additionally, Dermatology Life Quality Index (DLQI) scores reflected an improvement from extremely large negative impact on quality of life to small impact (Supplementary Figure S5A-B)18.
Clinical improvement with dual inhibition of IL-4Rα and IL-17 A is accompanied by reduction of immunopathogenic T cell populations. (A) Clinical and treatment course of the index patient. (B) TriMAP of all stimulated T cell immune populations in the index patient for all timepoints before and after treatment initiation. (C) TriMAP showing changes in stimulated T cell immune populations before and after treatment, stratified by time point. Differences in immune populations before and after treatment are colored gray. (D) TriMAP plot of the expression of each individual marker in stimulated T cells in the index patient. (E) Bar plot showing percentages of subtypes of stimulated CD3 + T cells in the index patient at different treatment time points. (F) Subpopulations of the percentage of stimulated CD3 + T cell types shown in e: γVδ T cells are stratified by γVδ1TCR and γVδ2TCR cells. CD4 T cells are stratified by naive CD4 (CD3 + CD4 + CD45RA+) and memory CD4 (CD3 + CD4 + CD45RO+) T cells. CD8 T cells are stratified by naive CD8 (CD3 + CD8 + CD45RA+) and memory CD8 (CD3 + CD4 + CD45RO+) T cells. (G) T-distributed stochastic neighbor embedding (tSNE) plot of all unstimulated T cells in the index patient in the three timepoints. (H) tSNE plots showing changes in unstimulated T cell immune populations before and after treatment, stratified by time point. Differences in immune populations before and after treatment are colored gray. (I) tSNE plots of the expression of each individual marker in unstimulated T cells in the index patient. T0, before treatment, T1 and T2, after treatment.
Dual inhibition of IL-4Rα and IL-17 A results in reduction of immunopathogenic T cell populations in the index patient
To evaluate the molecular effects of the treatment regimen, PBMCs and whole blood were collected from the index patient for analysis at three time intervals. We followed changes in immune responses, including T cells, granulocytes, and APCs as outlined in Fig. 1B. All cell populations in stimulated (Fig. 5B) and unstimulated (Fig. 5G) PBMCs were stratified by three time intervals (Fig. 5C and H for stimulated and unstimulated PBMCs, respectively), and CD3+ cell populations were identified by cell-specific markers (Fig. 5D and I for stimulated and unstimulated PBMCs, respectively), revealing alterations in immune cell populations over the treatment course. There was a 3.5-fold decrease in the proportion of γδ T cells in stimulated CD3+ cells (from 22 to 6.14%), with virtual clearance of pathogenic γVδ2 T cells (decreased from 2.8 to 0.25%) (Fig. 5E-F). Single cell analysis and clustering of stimulated CD3+ T cell populations by time interval revealed reductions in IL-17+ γδ T cells and IL-13+/IL-4+ naive γδ T cells or memory T cells (Supplementary Figure S6A-B). Finally, there was a reduction in IL-13-producing immune cell populations, including NK T cells, γVδ1 T cells, and γVδ2 T cells, as well as a reduction in IL-4-producing CD4+ T cells and γδ T cells in unstimulated PBMCs, identified via single cell clustering analysis in unstimulated PBMCs by time intervals (Supplementary Figure S6C-D).
Dual inhibition of IL-4Rα and IL-17 a results in reduction of immunopathogenic granulocyte and APC populations
Reversal of immunopathogenic populations was also seen in the index patient’s whole blood and APCs. All immune populations from the index patient’s whole blood (Fig. 6A) were stratified by those present at each of the three time intervals (Fig. 6B), demonstrating immune populations that were cleared after treatment. By utilizing the differential expression of each immune marker (Fig. 6C), single cell cluster analysis revealed four unique clusters (Fig. 6D), which are highlighted in Fig. 6A. Analysis of the whole blood cell subtypes at each time interval revealed a decrease in the percentages of basophils (from 17.4 to 7.25%) and activated platelets (from 18.2 to 4.63%) in the index patient after treatment (Fig. 6E). Additionally, APC-focused high-parameter flow cytometry of the index patient’s PBMCs revealed clearance of Glut1 and IL-12p70+ macrophages, as well as a reduction in monocytes and DCs (Supplementary Figure S7A-B). A summary of changes in the index patient’s immunopathogenic populations over the treatment course are illustrated in Fig. 6F.
High-parameter flow cytometric analysis reveals modulation of immunopathogenic granulocytic and monocytic immune cell populations with dual inhibition of IL-4Rα and IL-17 A. (A) TriMAP plot of all immune populations in the index patient for all time points before and after treatment initiation. (B) TriMAP plot showing changes in immune cell types before and after treatment, stratified by time point. Differences in immune populations before and after treatment are colored gray. (C) TriMAP plot of the expression of each individual marker in the index patient. (D) Representative histograms show the identification of four immune population clusters with breakdown of markers in each cluster. (E) Bar plots showing percentages of subtypes of granulocytic and monocytic cell populations in the three timepoints before and after treatment; DC, dendritic cells. (F) Illustration showing immunopathogenic populations in the whole blood of the index patient that decreased with treatment. (G) Quantification of mean fluorescence intensity (MFI) and absolute numbers of MRGPRX2-producing cells between different timepoints. (H) Quantification of mean fluorescence intensity (MFI) and absolute numbers of IgE-producing cells between different timepoints. (I) Bar plots showing expression of MRGPRX2 and IgE at the three timepoints. T0, before treatment, T1 and T2, after treatment.
Regulation of MRGPRX2 by dual inhibition of IL-4Rα and IL-17 A
We found that the expression of MRGPRX2 was downregulated in immune cells with dual inhibition of IL-4Rα and IL-17 A. Quantification of mean fluorescence intensity (MFI) of MRGPRX2-expressing cells at each time interval revealed decreased MFI after treatment (Fig. 6G). This reduced expression of the receptor was independent of the immune cell numbers, as is evident in eosinophils, which demonstrated a drastic decrease in MRGPRX2 MFI accompanied by an increase in absolute cell count (Fig. 6G). Furthermore, quantification of IgE+ cells at each time interval did not reveal any definite pattern, as shown by the MFI and absolute cell counts (Fig. 6H). The percent of total cells expressing MRGPRX2 decreased from 25.1 to 3.99% with treatment, demonstrating a much greater reduction than the percent of total cells expressing IgE, which decreased from 8.81 to 3.34% (Fig. 6I). Summative analyses of all MRGPRX2-expressing cells suggest that the index patient’s unique form of erythroderma is characterized by increased MRGPRX2 expression in immune cells, which unlike IgE expression, was regulated by treatment with IL-13 and IL-17 inhibition.
Discussion
Here we demonstrate the powerful ability of peripheral blood immunophenotyping via high-parameter flow cytometry to identify underlying patient-specific disease pathophysiology and guide therapeutic selection. We identified dysregulated Th2 and Th17 signaling pathways with increased IL-13 and IL-17 as targetable immunopathogenic mechanisms in a patient with refractory idiopathic erythroderma, and we monitored the subsequent clearance of immunopathogenic populations after dual monoclonal antibody treatment. Notably, our methods were able to differentiate the index patient from healthy controls and erythrodermic patients with PRP and SS. These results also represent the discovery of a previously unrecognized form of erythroderma featuring Th2/Th17 immune polarization.
We build on previous landmark studies utilizing single cell cutaneous immunophenotyping to reveal targetable pathogenic cell populations in drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms (DiHS/DRESS), psoriasis, and acne19,20,21. While previous investigations employed single-cell RNA sequencing of tissue biopsies, our approach introduces a less invasive and resource-intensive method for functional immunophenotyping. We demonstrate that peripheral blood immune signatures can reflect cutaneous disease pathology, as confirmed by concordant findings on flow cytometry and immunofluorescence staining. Specifically, our flow cytometric analysis identified dysregulated Th2 and Th17 signaling in the blood, while IF staining revealed increased expression of Th2 and Th17 cytokines and receptors in the skin.
The machine learning single-cell clustering analysis of peripheral blood cell populations employed in this study identified γδ T cells as the source of aberrant IL-13 and IL-17, which decreased after treatment. IL-13- and IL-17-producing γδ2 T cells were unique to the index patient and not seen in healthy or erythrodermic controls. γVδ1 and γVδ2 T cells are the two significant subtypes of γδ T cells, the latter of which is predominant in the blood, while γVδ1 T cells are predominantly in the thymus and peripheral tissues22. In response to IL-23 and T cell receptor signaling, cord blood naive T cells can differentiate into cytotoxic IL-17+IFN-γ−Vγ9γVδ2 T cells. Notably, stimulation of Vγ9Vδ2 T cells in rheumatoid arthritis induces IFN-γ and IL-17 secretion23. In psoriasis, Vγ9Vδ2 cells redistribute from blood to skin, and release inflammatory cytokines also seen in this patient, including IFN-γ, TNF-α, and IL-17 A24. We identify a combined Th2 and Th17 profile with IL-13- and IL-17-producing γVδ1 and γVδ2 T cells as unique pathogenic cell populations in this patient. With targeted therapy utilizing dual dupilumab and secukinumab, these immunopathogenic populations decreased.
In the index patient’s whole blood we identified a unique elevation in basophils compared to erythrodermic and healthy controls, which are closely intertwined with the type 2 immune response and secrete itch mediators such as histamine when activated by upstream IL-4 and IL-13 signaling25. We also identify increased numbers of activated platelets in the index and SS patients as well as a reduction in activated platelets with treatment in the index patient, supporting the role of platelets as critical immune mediators that can release soluble chemokines, cytokines, and antimicrobial peptides to propagate inflammation26.
Furthermore, we identified aberrant elevation of MRGPRX2 expression in platelets, basophils, and eosinophils, which resolved upon treatment. MRGPRX2 is a G protein-coupled receptor with known roles in pain and itch modulation27,28. It is expressed on dorsal root ganglia and granulocytes such as mast cells, basophils, and eosinophils, but not neutrophils29. To our knowledge, this is the first study to identify the presence of MRGPRX2 on human platelets, opening a new area of inquiry. In granulocytic cells, signaling through MRGPRX2 induces calcium influx and subsequent degranulation29. Given that platelets also have granules containing chemokines, cytokines, and various enzymes, platelet MRGPRX2 activation could also potentially result in degranulation and inflammatory effects26. This receptor has been implicated in numerous conditions, including pseudoallergic drug hypersensitivity reactions and non-IgE-mediated anaphylaxis30. As MRGPRX2 is highly expressed on skin mast cells, it has also been implicated in pruritic dermatologic conditions such as chronic spontaneous urticaria and atopic dermatitis31. While the regulation of MRGPRX2 expression is still poorly understood, decrease in the expression of the MRGPRX2 after treatment suggests another functional pathogenic target in the index patient.
The single-cell immunophenotyping strategies utilized in this study have the potential for broad impact. There is currently an unprecedented translational revolution taking place within medicine, with the rapid development of dozens of targeted monoclonal antibodies and small molecule inhibitors. Unfortunately, approvals for these medications are largely limited to highly prevalent conditions such as atopic dermatitis, psoriasis, or rheumatoid arthritis. Thus, there is an urgent need for the development of immunophenotyping platforms to guide therapeutic selection for patients with less common conditions or unique disease presentations. The peripheral blood-based immunophenotyping platform described in this study offers a framework for guiding therapeutic selection in such cases.
There is a paucity of data on the safety of dual biologic therapy, but emerging observational data suggest promising safety profiles for various combinations of biologics in a number of chronic inflammatory conditions32. There have been reports of dupilumab and secukinumab used concomitantly without adverse effects for other indications, and the potential benefits of this regimen were felt to outweigh the risks in our patient with refractory idiopathic erythroderma33,34,35. Our patient experienced no adverse events. Until long-term safety data are available for specific regimens and patient populations, the decision to initiate dual biologic therapy should be considered carefully on a case-by-case basis. Immunophenotyping may provide invaluable information when weighing these decisions.
Limitations of this study include low sample size, and further verification is needed in a larger patient cohort. In summary, we suggest that a peripheral blood-based systemic immunophenotyping platform may provide a novel personalized medicine approach to the management of treatment-refractory, idiopathic systemic inflammatory diseases.
Materials and methods
Sampling human materials
Sample collection and patient care were performed in accordance with protocols approved by the Institutional Review Board at Johns Hopkins University. All individuals provided written informed consent for sample acquisition and all subsequent analyses, including gene expression studies. Two 4-mm punch biopsies of lesional skin were obtained from the index patient, two erythrodermic controls, and three healthy control patients after local anesthesia with lidocaine. PBMCs were obtained from fresh blood samples from the patient and controls. Plasma was also obtained from fresh blood samples from the patient and controls.
Cell isolation and processing
PBMCs 1 mL of whole blood was removed, 100 uL DMSO was added and cryopreserved using an isopropanol-based freezing container for slow freeze at -80 °C, and transferred to liquid nitrogen (LN2) vapor phase 24–72 h later. The remaining blood was used for ficoll gradient, spun at 630xg for 25 min. Additional ficoll spin may be performed to clean up severe hemolysis. PBMC layer was removed, washed using DPBS, and counted using Vi-Cell counter. Wash spin and post-count spin were centrifuged at 315xg for 5 min. PBMCs were frozen down at ~ 5e6 cells/vial using RPMI + 10% FBS + 10% DMSO freezing media. PBMCs were then placed in an isopropanol-based freezing container for slow freeze at -80 °C and transferred to LN2 vapor phase 24–72 h later.
Plasma We centrifuged at 1960xg for 10 min. We transferred plasma (avoiding buffy layer) to create up to four 1 mL aliquots. We then placed the plasma in an isopropanol-based freezing container for slow freeze at -80 °C and transferred to LN2 vapor phase 24–72 h later.
Whole Blood To freeze whole blood, we added DMSO to the sample (10% by volume) to inhibit ice crystal formation inside the cells and freeze the samples at a controlled rate of 1 °C per hour. The storage temperature for whole blood was − 180 °C.
Storage conditions Samples were frozen down − 1 °C/min in an isopropanol-based freezing container and then transferred to LN2 vapor phase after 24 h. All inventory was stored in LN2 vapor phase (-180 °C) until retrieved.
PBMC T cell flow cytometry
Viable cells (3-5 × 106) were stimulated in RPMI with eBioscience Cell Stimulation Cocktail. Cells were collected after stimulation, and single-cell suspensions were obtained after filtering through a 40-mm cell filter. The cells were then washed in RPMI. The single-cell suspension was incubated with TruStain fcX (BioLegend, San Diego, CA) to block Fc receptor binding and was resuspended to label with mAbs against extracellular cell surface markers. The cell surface markers were incubated with the cells in Hanks Balanced Salt Solution with 2% Calf Serum and 5 mM 4-(2- hydroxyethyl)-1-piperazineethanesulfonic acid along with Brilliant Stain Buffer (BD Biosciences, San Jose, CA). The stained cells were washed with PBS and stained for viability (Zombie Aqua Fixable Viability Kit, BioLegend). The surface-labeled cells were fixed in the BD Cytofix/ Cytoperm Buffer kit (BD Biosciences). The cells were further labeled for intracellular cytokine markers. The complete antibody panel with associated fluorophores is shown in Supplementary Table S3. The mAb-labeled cells were then washed in intracellular staining buffer and resuspended in Stabilizing Fixative (BD Biosciences). Cell acquisition was performed on the BD LSRFortessa flow cytometer (BD Biosciences), and data were analyzed using Cytobank software (Cytobank, Mountain View, CA) and FlowJo 10 and R Statistical program V4.0. Samples were normalized via R statistical program scripts with CytoNorm v.1.23 and DownSample v3. Data on a minimum of 50,000 events in the live singlets gate were collected and analyzed. Single cell analysis was performed with R statistical program scripts with Cluster algorithms including Phenograph v3, TriMap v0.2 and UMAP v3.2. The absolute number of the corresponding cell population was calculated as the total number of live cells % of the corresponding cell population/100. For immunophenotyping of the T-cell subsets, including CD4, CD8, γδ, and invariant NK T cells, the cells were first gated on live cells, singlets and CD3 + cells, CD4 + CD8‒ (T helper) cells, CD8 + CD4‒ (cytotoxic T) cells, CD4‒ CD8‒ γδTCRþ (γδ T) cells, and CD4‒ CD8‒ CD56+ (invariant NK T) cells. Graphs of cell percentages were made in GraphPad Prism.
Whole blood flow cytometry
Cryopreserved whole blood (1 ml) samples were thawed on ice with 1 ml ACK lysis buffer (Quality Biological) for 7 min. Samples were washed in PBS and transferred to a 96-well U-bottom plate for staining. Samples were stained with LIVE/DEAD Fixable Dead Cell Stain (Zombie-Aqua, Thermo Fisher, L34957) at room temperature for 20 min in PBS. Samples were washed and stained with antibodies (Supplementary Table S4) for 20 min on ice in FACS Staining Buffer along with Brilliant stain buffer 50 µl. Human Fc block was added to the surface stain master mix. The cells were then fixed with BD Cytofix. Flow cytometry was performed on BD Fortessa and data were analyzed using FlowJo 10 and R Statistical program V4.0. Samples were normalized with R statistical program scripts with CytoNorm v.1.23 and DownSample v3. Data on a minimum of 50,000 events in the live singlets gate were collected and analyzed. Single cell analysis was performed with R statistical program scripts with Cluster algorithms including Phenograph v3, TriMap v0.2 and UMAP v3.2. Graphs of cell percentages were made in GraphPad Prism.
PBMC antigen-presenting cell flow cytometry
Cryopreserved PBMC (1 ml) samples were thawed on ice with 1 ml ACK lysis buffer (Quality Biological) for 7 min, then washed in PBS and transferred to a 96-well U-bottom plate for staining. Samples were stained with LIVE/DEAD Fixable Dead Cell Stain (Zombie-Aqua, Thermo Fisher, L34957) at room temperature for 20 min in PBS, then washed and stained with antibodies (Supplementary Table S5) for 20 min on ice in FACS Staining Buffer along with Brilliant stain buffer 50 µl. Human Fc block was added to the surface stain master mix. The cells were then fixed with BD Cytofix. Flow cytometry was performed on the Cytek Aurora and data was analyzed using FlowJo 10 and R Statistical program V4.0. Samples were normalized with R statistical program scripts with CytoNorm v.1.23 and DownSample v3. Data on a minimum of 50,000 events in the live singlets gate were collected and analyzed. Single cell analysis was performed with R statistical program scripts with Cluster algorithms including Phenograph v3, TriMap v0.2 and UMAP v3.2. Graphs of cell percentages were made in GraphPad Prism.
Immunofluorescence staining
Skin punch biopsy specimens from each participant were fixed in neutral-buffered 10% formalin. The specimens were then embedded in paraffin and cut into 5-µm sections, which were placed on slides. Slides were submerged in pre-heated antigen retrieval solution (Cell Marque, 920P-06) and microwaved until boiling for 15 min, after which they were washed with PBS three times and samples were treated with blocking reagent (Dako, X0909) for 1 h at room temperature in a humidified, light-protected chamber. Samples were then stained with primary antibodies (IL-4R, 1:80, LifeSpan BioSciences, LS-C11209 and IL-13, 1:200, LifeSpan BioSciences, LS-B7417; IL-17 A, 1:100, Abcam, ab189377 and IL-17RA, 1:200, LifeSpan BioSciences, LS-B15779) and incubated at 4 °C overnight. The next day, samples were washed with PBST three times, stained with secondary antibodies (Alexa Fluor 488, 1:500, Abcam, ab150077 and Alexa Fluor 568, 1:500, Invitrogen, A-11031) for 1 h at room temperature, and washed again with PBST. Slides were counterstained with DAPI working solution for 30 min, rinsed with PBS, and mounted with ProLong Diamond (Invitrogen, P36970). All images were taken with a Leica SP8 confocal microscope and immunofluorescence was quantified using ImageJ (National Institutes of Health).
Whole-genome sequencing
Whole-genome analysis was conducted on PBMCs which were collected at the index patient’s middle time interval (T1). DNA from the sample was extracted using Qiagen’s DNeasy kit. The library preparation was performed using the Agilent SureSelectXT Library Prep Kit/SureSelectXT Target V5 kit and was enriched using the Enrichment System for Illumina Version B.2, and subsequently was sequenced using NovaSeq6000 S4 (150 bp PE). The bwa.v0.7.7 tool was used for running the read alignments against the hg38 genome, and Piccard-tools1.119 was used to add read groups and remove duplicate reads. GATK v3.6.0 base call recalibration steps were used to create a final alignment file. The bcftools v1.5 was used to call variants against the reference. MuTect2 v3.6.0 was used to call variants against a panel of normals, and snpEFF (v4.1) was used to annotate the passed variant calls. Subsequently, the passed variants were converted to Mutation Annotation Format (MAF) using vcf2maf 1.6.19. Somatic variants in the patient that intersected with major IL-4, IL-13, and IL-17 pathways were reported, and Integrative Genomics Viewer (IGV) was used to view individual variants.
Study approval
The index patient provided written consent to protocols that were approved by the Institutional Review Board of Johns Hopkins University (IRB00231694), which enabled de-identified research use of biospecimens, genetic testing results, clinical data, and standard of care. Written informed consent was also received for the use of the photographs and record of this informed consent has been retained. Patient care and research was conducted in compliance with the CAse REport guideline and the Declaration of Helsinki.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Inamadar, A. C. & Ragunatha, S. The rash that becomes an erythroderma. Clin. Dermatol. 37, 88–98. https://doi.org/10.1016/j.clindermatol.2018.12.002 (2019).
Akhyani, M., Ghodsi, Z. S., Toosi, S. & Dabbaghian, H. Erythroderma: a clinical study of 97 cases. BMC Dermatol. 5 https://doi.org/10.1186/1471-5945-5-5 (2005).
Mathew, R. & Sreedevan, V. Erythroderma: A clinicopathological study of 370 cases from a tertiary care center in Kerala. Indian J. Dermatol. Venereol. Leprol. 83, 625. https://doi.org/10.4103/0378-6323.198434 (2017).
Tsoi, L. C. et al. Atopic dermatitis is an IL-13-Dominant disease with greater molecular heterogeneity compared to psoriasis. J. Invest. Dermatol. 139, 1480–1489. https://doi.org/10.1016/j.jid.2018.12.018 (2019).
Brunner, P. M. et al. The atopic dermatitis blood signature is characterized by increases in inflammatory and cardiovascular risk proteins. Sci. Rep. 7, 8707. https://doi.org/10.1038/s41598-017-09207-z (2017).
Ghoreschi, K., Weigert, C. & Röcken, M. Immunopathogenesis and role of T cells in psoriasis. Clin. Dermatol. 25, 574–580. https://doi.org/10.1016/j.clindermatol.2007.08.012 (2007).
Carrasquillo, O. Y. et al. Treatment of erythrodermic psoriasis with biologics: A systematic review. J. Am. Acad. Dermatol. 83, 151–158. https://doi.org/10.1016/j.jaad.2020.03.073 (2020).
Avallone, G. et al. Interleukin-17 vs. Interleukin-23 inhibitors in pustular and erythrodermic psoriasis: A retrospective, multicentre cohort study. J. Clin. Med. 12 (4), 1662. https://doi.org/10.3390/jcm12041662 (2023). Published 2023 Feb 19.
Kromer, C., Sabat, R., Celis, D. & Mössner, R. Systemic therapies of pityriasis rubra pilaris: A systematic review. JDDG: J. Der Deutschen Dermatologischen Gesellschaft. 17, 243–259. https://doi.org/10.1111/ddg.13718 (2019).
Feldmeyer, L. et al. Interleukin 23-Helper T cell 17 Axis as a treatment target for Pityriasis Rubra Pilaris. JAMA Dermatol. 153, 304–308. https://doi.org/10.1001/jamadermatol.2016.5384 (2017).
Kamijo, H. & Miyagaki, T. Mycosis Fungoides and Sézary Syndrome: Updates and review of current therapy. Curr. Treat. Options Oncol. 22, https://doi.org/10.1007/s11864-020-00809-w (2021).
Cuellar-Barboza, A., Ocampo-Candiani, J. & Herz-Ruelas, M. E. Eritrodermia en el adulto: Un enfoque práctico para el diagnóstico y tratamiento. Actas Dermosifiliogr. 109, 777–790. https://doi.org/10.1016/j.ad.2018.05.011 (2018).
Belzberg, M. et al. Prurigo Nodularis is characterized by systemic and cutaneous T helper 22 Immune polarization. J. Invest. Dermatol. 141, 2208–2218e14. https://doi.org/10.1016/j.jid.2021.02.749 (2021).
Becht, E. et al. Dimensionality reduction for visualizing single-cell data using UMAP. Nat. Biotechnol. https://doi.org/10.1038/nbt.4314 (2018).
Quintelier, K. et al. Analyzing high-dimensional cytometry data using FlowSOM. Nat. Protoc. 16, 3775–3801. https://doi.org/10.1038/s41596-021-00550-0 (2021).
Yang, F. et al. Structure, function and pharmacology of human itch receptor complexes. Nature 600, 164–169. https://doi.org/10.1038/s41586-021-04077-y (2021).
Kimel, M., Zeidler, C., Kwon, P., Revicki, D. & Ständer, S. Validation of Psychometric properties of the itch numeric rating scale for Pruritus associated with Prurigo Nodularis: A secondary analysis of a randomized clinical trial. JAMA Dermatol. 156, 1354–1358. https://doi.org/10.1001/jamadermatol.2020.3071 (2020).
Finlay, A. Y. & Khan, G. K. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin. Exp. Dermatol. 19, 210–216. https://doi.org/10.1111/j.1365-2230.1994.tb01167.x (1994).
Kim, D. et al. Targeted therapy guided by single-cell transcriptomic analysis in drug-induced hypersensitivity syndrome: a case report. Nat. Med. 26, 236–243. https://doi.org/10.1038/s41591-019-0733-7 (2020).
Liu, J. et al. Single-cell RNA sequencing of psoriatic skin identifies pathogenic Tc17 cell subsets and reveals distinctions between CD8 + T cells in autoimmunity and cancer. J. Allergy Clin. Immunol. 147, 2370–2380. https://doi.org/10.1016/j.jaci.2020.11.028 (2021).
O’Neill, A. M. et al. Antimicrobial production by perifollicular dermal preadipocytes is essential to the pathophysiology of acne. Sci. Transl Med. 14, eabh1478. https://doi.org/10.1126/scitranslmed.abh1478 (2022).
Lawand, M., Déchanet-Merville, J. & Dieu-Nosjean, M. C. Key features of Gamma-Delta T-Cell subsets in Human diseases and their immunotherapeutic implications. Front. Immunol. 8, 761. https://doi.org/10.3389/fimmu.2017.00761 (2017).
Hu, C. et al. Antigen-presenting effects of effector memory Vγ9Vδ2 T cells in rheumatoid arthritis. Cell. Mol. Immunol. 9, 245–254. https://doi.org/10.1038/cmi.2011.50 (2012).
Qi, C., Wang, Y., Li, P. & Zhao, J. Gamma delta T cells and their pathogenic role in Psoriasis. Front. Immunol. 12, 627139. https://doi.org/10.3389/fimmu.2021.627139 (2021).
Jia, F., Zhao, Q., Shi, P., Liu, H. & Zhang, F. Dupilumab: Advances in the off-label usage of IL4/IL13 antagonist in dermatoses. Dermatol. Ther. 35, e15924. https://doi.org/10.1111/dth.15924 (2022).
Tamagawa-Mineoka, R. Important roles of platelets as immune cells in the skin. J. Dermatol. Sci. 77, 93–101. https://doi.org/10.1016/j.jdermsci.2014.10.003 (2015).
Lansu, K. et al. In silico design of novel probes for the atypical opioid receptor MRGPRX2. Nat. Chem. Biol. 13, 529–536. https://doi.org/10.1038/nchembio.2334 (2017).
Liu, Q. et al. Sensory neuron-specific GPCR mrgprs are itch receptors mediating chloroquine-induced pruritus. Cell 139, 1353–1365. https://doi.org/10.1016/j.cell.2009.11.034 (2009).
Wedi, B., Gehring, M. & Kapp, A. The pseudoallergen receptor MRGPRX2 on peripheral blood basophils and eosinophils: Expression and function. Allergy 75, 2229–2242. https://doi.org/10.1111/all.14213 (2020).
Porebski, G., Kwiecien, K., Pawica, M. & Kwitniewski, M. Mas-related G protein-coupled Receptor-X2 (MRGPRX2) in drug hypersensitivity reactions. Front. Immunol. 9, 3027. https://doi.org/10.3389/fimmu.2018.03027 (2018).
Kühn, H. et al. Mas-related G protein-coupled receptor X2 and its activators in dermatologic allergies. J. Allergy Clin. Immunol. 147, 456–469. https://doi.org/10.1016/j.jaci.2020.08.027 (2021).
Quiroga, L. C. & Sabourin, A. A. Review of dual biologics in specialty pharmacy practice. Ann. Pharmacother. 57 (9), 1094–1110. https://doi.org/10.1177/10600280221135177 (2023).
Gisondi, P., Maurelli, M., Costanzo, A., Esposito, M. & Girolomoni, G. The combination of Dupilumab with other monoclonal antibodies. Dermatol. Ther. (Heidelb). 13 (1), 7–12. https://doi.org/10.1007/s13555-022-00851-6 (2023).
Balestri, R., Magnano, M., Girardelli, C. R., Bortolotti, R. & Rech, G. Long-term safety of combined biological therapy in a patient affected by arthropathic psoriasis and atopic dermatitis. Dermatol. Ther. 33 (4), e13498. https://doi.org/10.1111/dth.13498 (2020).
Mahar, P. D., Zubrinich, C. M., Manuelpillai, N. & Foley, P. Combination treatment with monoclonal antibodies: Secukinumab, benralizumab and dupilumab for the combined management of psoriasis and severe asthma. Australas J. Dermatol. 62 (4), 506–508. https://doi.org/10.1111/ajd.13676 (2021).
Acknowledgements
Shawn G. Kwatra is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number K23AR077073-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the patients who agreed to participate in this study. We thank the Genetic Resources Core Facility Cell Center and Biorepository for their technical support in processing and storing PBMCs. We also thank Dr. Kornel Schuebel, Dr. Vasan Yegnasubramanian, and Dr. Sarah Wheelan of the Johns Hopkins Experimental and Computational Genomics Core for their support in whole-genome sequencing. We also thank Dr. Ronald Sweren, Dr. Robert Berger, Dr. Elizabeth Richard, and Dr. Shivani Patel for their contributions. Finally, we thank Dr. Nishadh Sutaria and Dr. Sophie Roh for their contributions.
Funding
National Institutes of Health Award Number K23AR077073 (SGK).
Author information
Authors and Affiliations
Contributions
Conceptualization: SGK; Methodology: MPA, MM, KKL, AD, MMK, SGK; Investigation: MPA, MM, SGK; Data curation: MPA, VP, JD, HC, AK, ALK, TP, MM, KKL, AD, SGK; Formal analysis: MPA, VP, JD, HC, AK, ALK, MM, KKL, AD, SGK; Visualization: MPA, VP, JD, HC, ALK, MM, KKL, AD, SGK; Funding acquisition: SGK; Project administration: SGK; Supervision: MPA, MMK, SGK; Writing – original draft: HC, VP, JD, AK, AD, SGK; Writing – review & editing: MPA, HC, AK, ALK, JD, TP, MM, KKL, AD, JHB, JPM, KP, JM, EM, VP, MMK, WJH, SGK.
Corresponding author
Ethics declarations
Competing interests
Dr. Shawn Kwatra is an advisory board member/consultant for Abbvie, Amgen, Arcutis Biotherapeutics, Aslan Pharmaceuticals, Bristol Myers Squibb, Cara Therapeutics, Castle Biosciences, Celldex Therapeutics, Galderma, Genzada Pharmaceuticals, Incyte Corporation, Johnson & Johnson, Leo Pharma, Novartis Pharmaceuticals Corporation, Pfizer, Regeneron Pharmaceuticals, and Sanofi and has served as an investigator for Galderma, Incyte, Pfizer, and Sanofi. He is also on the Executive Board of the Skin of Color Society. All other authors have no conflicts of interest to report. A provisional patent application (patent no. is 63/422,061) was filed for the workflow used in the creation of this manuscript on November 3, 2022.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cornman, H.L., Alphonse, M.P., Dykema, A. et al. Targeted dual biologic therapy for erythroderma of unknown etiology guided by high-parameter peripheral blood immunophenotyping. Sci Rep 15, 1298 (2025). https://doi.org/10.1038/s41598-024-81060-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81060-3