Abstract
The present randomized controlled trial aimed to investigate the effects of home-based telemedicine with wearable devices and usual care on pain-related outcomes in patients with chronic musculoskeletal pain, compared to usual care alone. The patients with chronic musculoskeletal pain were randomly allocated to the usual care group or the telemedicine group, which participated in telemedicine with wearable devices, the objective data from which were recorded, in conjunction with usual care for six months. The primary outcome measure was the Numeric Rating Scale (NRS) for pain. The secondary outcome measures were the Pain Catastrophizing Scale (PCS), Hospital Anxiety and Depression Scale (HADS), Pain Disability Assessment Scale (PDAS), and EuroQol-five dimensions-three level (EQ-5D-3L). Seventy-one participants were analyzed. At 1 and 3 months, there were no significant differences in the NRS scores between the groups; however, the telemedicine group had a significantly superior effect on all of the outcome measures at 6 months compared to the usual care group. The number of steps and distance were significantly increased at 6 months compared to baseline in the telemedicine group. Home-based telemedicine with wearable devices and usual care has a modest effect on pain-related outcomes compared to usual care in patients with chronic musculoskeletal pain.
This study was registered (UMIN000052994 - 04/12/2023).
Similar content being viewed by others
Introduction
Chronic musculoskeletal pain is defined as persistent or recurrent pain that affects various bones, joints, muscles, and related soft tissues, or can be nonspecific1. Non-pharmacological self-management strategies, including education and exercise, are recommended for the treatment of patients with chronic pain2,3,4,5. Barriers to the use of non-pharmacological treatments for chronic pain, however, include high costs, transportation problems, low motivation, distress experienced from ongoing pain, and unsupportive relationships with clinicians6,7,8.
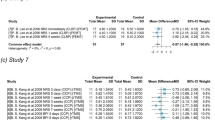
Telemedicine is the practice of medicine through electronic communication, information technology, or other means, allowing a physician in one location to treat a patient in another location9. Telemedicine has the potential to be an effective tool for delivering more frequent and timely healthcare to people with chronic conditions from a distance, and for improving overall access to health care10. Telemedicine for the treatment of pain, in particular, focuses on self-management, physical activity, and education, with a duration of 6 weeks to 6 months11,12,13. In patients with chronic pain, telemedicine reduces pain-related outcomes, although the additional effect on pain is limited, compared to usual care alone11,12,13.
Physical activity is assessed during telemedicine visits for patients with chronic pain; however, some patients may over- or under-report their self-monitored physical activity by as much as 50% of that documented by external monitoring14, or they may simply forget the activities they have performed. Commercial wearable devices accurately measure physical activity15,16, and physical activity-related variables have been investigated in previous studies using Fitbit (Fitbit, Inc., San Francisco, CA, USA), some of the commercially available wearable devices15,16. The objective measurements of physical activity obtained by these devices can educate and motivate individuals toward greater physical activity and better health17,18, although they have no significant effect on pain, functional tests, disability, quality of life, or fatigue in patients19. Physical activity should, however, be tailored to individual disabilities by clinicians19, although the benefits of home-based telemedicine with wearable devices have yet to be demonstrated in patients with chronic musculoskeletal pain.
The present randomized controlled clinical trial aimed, therefore, to evaluate the effects of home-based telemedicine with wearable devices and usual care on pain-related outcomes in patients with chronic musculoskeletal pain with a minimum duration of 6 months, as compared with usual care alone. The authors hypothesized that home-based telemedicine with a wearable device would have an additional effect on pain-related outcomes compared to usual care.
Methods
Study design and randomization
A randomized controlled trial design was established prior to the confirmatory study. The authors hypothesized that telemedicine and usual care would be superior to usual care alone in the treatment of patients with chronic musculoskeletal pain with an effect size of 0.7 for the primary outcome measure, based on previous findings11,12,13,19,20. Based on this assumption, the sample size for a power > 0.80 and a two-tailed α at a significance level of < 0.05 required a minimum of 68 subjects (34 subjects per group), as calculated using G*Power (v3.1.9.2; Franz Faul, Universität Kiel, Kiel, Germany). The protocol for the present study was registered (no. UMIN000052994), approved by the ethics committee at Hayaishi Hospital (R2-10–30), and all study participants provided written informed consent. The present study adhered to the CONSORT checklist for reporting clinical trials. All methods were performed in accordance with the relevant guidelines and regulations.
A flowchart of this process is shown in Fig. 1. Because we expected a dropout rate of 10% with low acceptance21,22, 76 consecutive patients with chronic musculoskeletal pain were randomly allocated, equally, into the usual care or telemedicine group. The allocation was performed using block randomization by an individual who was not involved in patient treatment. Allocation concealment was performed using the sealed envelope technique.
Participants
Participants were recruited consecutively at our tertiary center between August 2020 and September 2021. The inclusion criteria were as follows: (1) age > 20 years; (2) persistent primary musculoskeletal pain of a minimum duration of 6 months before entry into the study; and (3) a score ≥ 3 on a 10-point Numeric Rating Scale (NRS) for subjective pain intensity. The exclusion criteria were as follows: (1) not willing to participate; (2) tumor-related pain or neurological symptoms; (3) surgery within 3 months prior; and (4) taking medicine for the treatment of dementia. Patients were, however, allowed to take regular long-term medications. All inclusion and exclusion criteria were evaluated by the referring physicians.
Treatment
Throughout the present study, treatments were performed by orthopedic physicians and physical therapists. The patients were instructed that they could stop treatment if their symptoms improved or if any problems occurred during the study period.
All patients in both groups received usual care based on the recommendations from clinical practice guidelines2,3,4,5. In-person face-to-face treatments by orthopedists and physical therapists in the clinic were performed once a month for 6 months. The treatment included advising the patient to remain active and providing education and reassurance as first-line care. Physical therapy included exercise, active and passive mobilization, and electro physical modalities, as necessary. If patients needed second-line care, non-pharmacological treatment was attempted before pharmacological treatment. If pharmacological treatments were used, they were administered at the lowest effective dose and for the shortest possible period by orthopedists who were blinded to the randomization.
The telemedicine group received telemedicine using wearable devices and usual care. Telemedicine was conducted for 20 min per session, every week, for 6 months, by a referring physical therapist. The patients used a wrist-worn wearable device, the Fitbit Inspire HR (Fitbit, Inc., San Francisco, CA, USA)23, all day and night. Data from the wearable devices were used for each telemedicine session, after which the patients were directed to increase their physical activity by 10% the following week. If the participants did not increase their physical activity, they were encouraged to repeat their goals the following week. The telemedicine visits focused on supporting self-management and providing education11,12,13. Patients were provided with information on the neurophysiology of pain from a bio-psychosocial perspective and a rationale for treatment, as well as the importance of exercise.
Exploratory outcomes
The exploratory outcomes recorded by the wearable device were as follows: number of steps; distance; duration of light activity; duration of moderate and vigorous physical activity (MVPA); duration of sedentary time; consumption of calories per activity; and duration of total, rapid eye movement (REM), light, and deep sleep.
Outcome assessment
Outcome measures were evaluated at baseline and again at 1, 3, and 6 months after starting each treatment using the following assessments: pain-NRS24, Pain Catastrophizing Scale (PCS)25,26, Hospital Anxiety and Depression Scale (HADS)27,28, Pain Disability Assessment Scale (PDAS)29, and EuroQol-five dimensions-three level (EQ-5D-3L)30,31. The trial was single-blinded in that the patients were aware, but the assessors of the patient outcomes were not, of the group the patient was randomized to.
As a primary outcome measure, the pain-NRS was used to evaluate the severity of the patient’s pain at each assessment, where 0 = no pain and 10 = worst pain imaginable24. Secondary outcomes were assessed using the PCS, HADS, PDAS, and EQ-5D-3L. All questionnaires were translated into Japanese. The PCS consists of 13 items, with which participants rate how frequently they have experienced the specified cognition/emotions25,26. The total PCS score can range from 0–52, with higher scores indicating higher levels of catastrophizing. The HADS, consisting of 14 items separated into anxiety (HADS-A) and depression (HADS-D) subscales, each with 7 items, was designed to assess 2 separate dimensions, anxiety and depression27,28, using a 4-point response scale (ranging from 0 = absence of symptoms to 3 = maximum symptoms), with possible scores for each subscale ranging from 0–21. The PDAS, which included 20 items, assesses the degree to which chronic pain has interfered with various daily activities during the prior week based on the participant’s response to each question29. The total PDAS scores ranged from 0–60, with higher scores indicating higher levels of pain interference. The EQ-5D-3L score assesses the subjective health-related quality of life30,31 based on five dimensions: mobility; self-care; usual activities; pain/discomfort; and anxiety/depression. The EQ-5D-3L score ranges from -0.111–1.000 as follows: negative scores, worse health than death; 0, death; and 1.000, full health.
Statistical analysis
The Shapiro–Wilk normality test was initially used to determine whether the data for continuous variables were normally distributed. Continuous variables are presented as mean, standard deviation, and 95% confidence interval, while categorical variables are presented as the number and percentage of patients. The groups were compared for each outcome using the chi-squared test, two-way analysis of variance (ANOVA), and unpaired t-test between the usual care and telemedicine groups. Changes in values were compared using repeated-measures ANOVA or a paired t-test. Correlations between changes in pain-NRS or EQ-5D-3L scale scores and variables were analyzed using Pearson’s rank test. Cohen’s d, Cramer’s V, and correlation coefficients were used to evaluate the magnitude of effect size. Data were analyzed using SPSS (version 28.0 for Microsoft Windows; SPSS, Chicago, IL, USA), and statistical significance was set at P < 0.05.
Results
Patient characteristics
A flowchart of the participants’ dispositions is shown in Fig. 1. Initially, 77 potential participants were assessed for eligibility, 1 of whom declined to participate; therefore, 76 consecutive patients with chronic musculoskeletal pain were randomly allocated to 2 equal groups: usual care and telemedicine. Of the 76 participants, 5 (6.5%) fell out of contact and did not complete the follow-up assessments (usual care group, 4 vs. telemedicine group, 1). In total, therefore, 71 participants (93.4%) completed the study (usual care group, 34 vs. telemedicine group, 37).
Table 1 presents the participants’ characteristics. Of the 71 participants, 55 (77.5%) were female. The mean ages were 56.6 ± 14.3 years and 56.5 ± 14.7 years in the usual care and telemedicine groups, respectively. The mean pain-NRS scores at baseline were 6.0 ± 1.8 points in the usual care group and 6.4 ± 2.3 points in the telemedicine group (Table 2). The mean EQ-5D-3L scores at baseline were 0.57 ± 0.16 points in the usual care group and 0.60 ± 0.16 points in the telemedicine group. No variables showed significant differences between the groups at baseline. No patients had an opioid prescription in the present study.
Changes in values in the wearable devices in telemedicine group
The values from the wearable devices at baseline and six months are shown in Table 3. The sleep duration data were lacking for one participant at baseline and three participants at 6 months. Overall, participants showed a significant increase in the number of steps (baseline, 7,110 ± 4,164 vs. 6 months, 8,054 ± 4,168; P = 0.012*; d = 0.387) and distance (4.6 ± 2.6 km vs. 5.3 ± 2.7 km; P = 0.008*; d = 0.416) per day at 6 months, compared with baseline. There was no significant difference, however, in the duration of sedentary time, duration of light activity, duration of MVPA, consumption of calories by activity, or sleep duration.
Primary and secondary outcomes
The primary and secondary outcomes from baseline to each follow-up are shown in Table 2. The pain-NRS score decreased significantly at 6 months (-1.3 points; P = 0.015*; d = 0.420), in the telemedicine group compared with baseline although not at the 1- (-0.3 points; P = 0.568) and at 3-month (-0.8 points; P = 0.110) follow-ups. There were no significant difference in the usual care group (± 0.0 to + 0.4 points; P = 0.632) at 6 months, compared with baseline. The 1- and 3-month assessments showed no significant difference in the pain-NRS scores between the usual care and telemedicine groups (1 month, P = 0.279; 3 months, P = 0.220), while on the 6-month assessment the telemedicine group was significantly lower than the usual care group (usual care group, 6.3 ± 2.2 vs. telemedicine group, 5.1 ± 3.0; P = 0.039*; d = 0.424). The number of participants with a pain-NRS score improvement ≥ 2 points was 8 of 34 (23.5%) in the usual care group, compared to 16 of 37 (43.2%) in the telemedicine group (P = 0.079; d = 0.208). The group × time interaction was not statistically significant (P = 0.341).
The secondary outcomes were significantly improved for the PCS (-5.5 points; P = 0.001*; d = 0.568) and EQ-5D-3L (+ 0.04 points; P = 0.035*; d = 0.361) scores at 6 months in the telemedicine group compared with baseline, but not for the PDAS (-3.1 points; P = 0.072) or HADS (-2.4 points; P = 0.054) scores. There were no significant differences in the usual care group at 6 months, compared with baseline (PCS score, -0.1 points, P = 0.470; HADS score, ± 0.0 points, P = 0.061; PDAS score, + 1.0 points, P = 0.853; and EQ-5D-3L score, ± 0.0 points, P = 0.669). The secondary outcomes from the 1- and 3-month assessments showed that the PCS, HADS, PDAS, and EQ-5D-3L scores in the telemedicine group were superior to those in the usual care group (P < 0.05*), with the exception of the HADS score at 3 months (P = 0.075). The telemedicine group had a superior effect at 6 months compared with usual care group on the PCS (usual care group, 32.1 ± 12.4 vs. telemedicine group, 25.6 ± 13.6; P = 0.020*; d = 0.501), HADS (18.6 ± 9.2 vs. 13.9 ± 9.2; P = 0.028*; d = 0.461), PDAS (25.8 ± 12.1 vs. 20.6 ± 12.4; P = 0.044*; d = 0.411), and EQ-5D-3L (0.57 ± 0.19 vs. 0.64 ± 0.16; P = 0.049*; d = 0.398) scores. The group × time interactions were not significant (PCS, P = 0.506; HADS, P = 0.842; PDAS, P = 0.699; EQ-5D-3L, P = 0.775).
Associations with improvement of pain-NRS for 6 months and variables
There was no significant correlation between the improvement in pain-NRS score at six months and the PCS, HADS, PDAS, EQ-5D-3L scores, or the data from the wearable devices at baseline (Table 4). A higher pain-NRS score at baseline, however, was associated with a greater improvement in pain-NRS scores over 6 months (r = 0.404; P < 0.001*).
Discussion
The results of the present randomized controlled clinical trial showed that home-based telemedicine with wearable devices and usual care had a modest effect on pain-related outcomes compared to usual care alone in patients with chronic musculoskeletal pain. The telemedicine group had significantly increased physical activity for six months; however, the improvement in pain-NRS was not associated with the change in the variables recorded by the wearable devices.
Clinically important improvement in chronic pain is defined as a reduction from baseline of ≥ 2 points or 30% on the pain-NRS, specifically, “much improved” or better24,32,33. The pain-NRS showed a reduction of 1.3 points or 20% compared with baseline and a reduction of more than 2 points in less than half patients in the telemedicine group. Among the other outcome measures, clinically important differences in chronic pain are defined as follows: EQ-5D-3L, 0.08 points; PDAS, 6.71 points; and PCS, 6.48 points32,33. The present study, however, showed the following improvement compared to baseline: EQ-5D-3L, 0.04 points; PDAS, 3.1 points; and PCS, 5.5 points. Based on the aforementioned results, therefore, home-based telemedicine had a significantly superior effect on pain-related outcomes compared to usual care alone, but the effects were modest.
Telemedicine for the treatment of chronic pain provides support for self-management, physical activity, and education, leading to improvements of symptoms11,12,13. Improvement in the pain-NRS score, however, was not associated with an increase in physical activity for six months in the telemedicine group. Tailoring health communication leads to several intended effects: (1) personalization, which helps increase the perceived meaningfulness of the message by creating an impression; (2) feedback, which directs the attention of the individual to their own characteristics or behaviors; and (3) adaptation or content matching, which refers to creating content packages20,34. In some cases, telemedicine is combined with videoconferencing intervention35, cognitive behavioral therapy36, lectures, and workshops37. Previous studies on pain have performed telemedicine every, or every other week11,12,13, or even five days per week38. In the initial phase, the frequency of telemedicine is increased in some studies39,40,41. The best practices of telemedicine for chronic pain have not yet been defined11,12,13, although the present study showed a significant, albeit limited, effect of telemedicine with wearable devices on pain-related outcomes.
Telemedicine has the potential to be an effective tool for delivering frequent and timely health care10,42, and most patients expressed positive feelings toward telemedicine and wearable devices by the end of treatment21,22,43. Telemedicine with wearable devices provides better knowledge and concrete feedback on physical activity, motivates behavioral change, facilitates daily exercise at home, reinforces wellness group activities and goals, and reduces the distance between physicians and patients43,44,45. Limited evidence has shown the cost savings associated with the lack of travel in telemedicine10,46,47. Physicians who specialize in pain and have higher confidence in recommending online resources are more likely to recommend online health resources48. Electronic tools also help support physician time management, reduce the clinic load, and prioritize issues that may need further attention42; however, the utilization of health resources for seeking treatment are recommended by only half to three-quarters of healthcare physicians and patients (before the coronavirus disease 2019 pandemic)48,49.
Half of the patients presented with a wearable device initially expressed negative or neutral feelings towards the device43. Some patients report that wearable devices have barriers to purchase, such as cost and choice confusion, and feel they can have a poor fit, leading to discomfort; therefore, some patients are unsure and/or skeptical43. Furthermore, participants’ compliance and adherence to wearing the device, the limited battery life and need to recharge the device, participants’ disinterest in wearing the device, and being self-conscious around others should also be considered50. Physicians are concerned about safety issues related to the risk of misinterpreting online information, issues related to patients’ affordability to access the internet, the mismatch between the patient and healthcare providers, and the lack of developing a therapeutic relationship with clinicians48. Additionally, the use of wearable devices without education has shown no benefits for pain, function, disability, quality of life, or fatigue in patients with pain19.
Wait times for in-person chronic pain management services range from 10–575 days, with deterioration in health-related quality of life and psychological well-being continuing during the waiting period51,52. The management of chronic pain has increasingly relied on pharmacological treatments, while physical therapy referrals have not increased, despite numerous published national guidelines6. The results of the present study suggested the limited benefit of home-based telemedicine using wearable devices in patients with chronic musculoskeletal pain. A supportive system for patients with chronic pain influences self-discovery and empowers individuals to continue incorporating self-management strategies into maneuvering daily life with chronic pain8.
The present study had several limitations. First, the effects of home-based telemedicine and the wearable devices were not investigated separately, and the number of interventions was disproportionate between the groups because a placebo rehabilitation was not feasible. Second, the subjective and objective outcomes were not observed over the long term, nor was physical activity assessed in the usual care group. Third, the etiology in some patients was unknown. The data of a previous medication, treatment, or physical therapy were not collected. Finally, only a small number of heterogeneous patients from a single medical center were included in the present study; therefore, the findings should be interpreted with caution. Further studies addressing these limitations are needed to confirm the benefits of home-based telemedicine using wearable devices.
Conclusions
The results of the present randomized controlled clinical trial showed that home-based telemedicine with wearable devices and usual care has a superior effect on symptoms in patients with chronic musculoskeletal pain compared to usual care alone. Although this effect was limited, home-based telemedicine using wearable devices could have an additional therapeutic effect on the symptoms of patients with chronic musculoskeletal pain.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
References
Treede, R. D. et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain. 160, 19–27 (2019).
Geneen, L. J. et al. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 4, CD011279 (2017).
The Committee for Clinical Practice Guideline for Chronic Pain. Clinical Practice Guideline for Chronic Pain (Shinko Trading Co. Ltd., Tokyo, 2018).
Lin, I. et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: Systematic review. Br. J. Sports Med. 54, 79–86 (2020).
Foster, N. E. et al. Lancet Low Back Pain Series Working Group. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet. 391, 2368–2383 (2018).
Mafi, J. N., McCarthy, E. P., Davis, R. B. & Landon, B. E. Worsening trends in the management and treatment of back pain. JAMA Intern. Med. 173(1573), 1581 (2013) (Erratum. In: JAMA Intern Med. 2015 175 869).
Becker, W. C. et al. Barriers and facilitators to use of non-pharmacological treatments in chronic pain. BMC Fam. Pract. 18, 41 (2017).
Devan, H., Hale, L., Hempel, D., Saipe, B. & Perry, M. A. What works and does not work in a self-management intervention for people with chronic pain? Qualitative systematic review and meta-synthesis. Phys. Ther. 98, 381–397 (2018).
Centers for disease control and prevention. Telehealth and telemedicine: A research anthology of law and policy resources https://www.cdc.gov/phlp/publications/topic/anthologies/anthologies-telehealth.html (Accessed Jan 24, 2024).
Flodgren, G., Rachas, A., Farmer, A. J., Inzitari, M. & Shepperd, S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD002098.pub2 (2015).
Cottrell, M. A., Galea, O. A., O’Leary, S. P., Hill, A. J. & Russell, T. G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 31, 625–638 (2017).
O’Brien, K. M. et al. Effectiveness of telephone-based interventions for managing osteoarthritis and spinal pain: A systematic review and meta-analysis. PeerJ. 6, e5846 (2018).
Adamse, C., Dekker-Van Weering, M. G., van Etten-Jamaludin, F. S. & Stuiver, M. M. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: A systematic review. J. Telemed. Telecare. 24, 511–526 (2018).
Lichtman, S. W. et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N. Engl. J. Med. 327, 1893–1898 (1992).
Fuller, D. et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: Systematic review. JMIR Mhealth Uhealth 8, e18694 (2020).
Ringeval, M., Wagner, G., Denford, J., Paré, G. & Kitsiou, S. Fitbit-based interventions for healthy lifestyle outcomes: Systematic review and meta-analysis. J. Med. Internet Res. 22, e23954 (2020).
Patel, M. S., Asch, D. A. & Volpp, K. G. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 313, 459–460 (2015).
Mercer, K., Li, M., Giangregorio, L., Burns, C. & Grindrod, K. Behavior change techniques present in wearable activity trackers: A critical analysis. JMIR Mhealth Uhealth 4, e40 (2016).
Davergne, T., Pallot, A., Dechartres, A., Fautrel, B. & Gossec, L. Use of wearable activity trackers to improve physical activity behavior in patients with rheumatic and musculoskeletal diseases: A systematic review and meta-analysis. Arthr. Care Res. (Hoboken). 71, 758–767 (2019).
Martorella, G. et al. Tailored web-based interventions for pain: Systematic review and meta-analysis. J. Med. Internet Res. 19, e385 (2017).
Guilkey, R. E., Draucker, C. B., Wu, J., Yu, Z. & Kroenke, K. Acceptability of a telecare intervention for persistent musculoskeletal pain. J. Telemed. Telecare. 24, 44–50 (2018).
Janevic, M. R., Shute, V., Murphy, S. L. & Piette, J. D. Acceptability and effects of commercially available activity trackers for chronic pain management among older african american adults. Pain. Med. 21, e68–e78 (2020).
Fitbit. Fitbit Inspire & Inspire HR. https://www.fitbit.com/sg/inspire (Accessed Jan 24, 2024).
Farrar, J. T., Young, J. P. Jr., LaMoreaux, L., Werth, J. L. & Poole, M. R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 94, 149–158 (2001).
Sullivan, M. J. L., Bishop, S. R. & Pivik, J. The pain catastrophizing scale: development and validation. Psychol. Assess. 7, 524–532 (1995).
Matsuoka, H. & Sakano, Y. Assessment of cognitive aspect of pain: Development, reliability, and validation of Japanese version of pain catastrophizing scale. Jpn. J. Psychosom. Med. 47, 95–102 (2007).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370 (1983).
Kugaya, A., Akechi, T., Okuyama, T., Okamura, H. & Uchitomi, Y. Screening for psychological distress in Japanese cancer patients. Jpn. J. Clin. Oncol. 28, 333–338 (1998).
Yamashiro, K. et al. A multidimensional measure of pain interference: Reliability and validity of the pain disability assessment scale. Clin. J. Pain. 27, 338–343 (2011).
EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 16, 199–208 (1990).
Tsuchiya, A. et al. Estimating an EQ-5D population value set: The case of Japan. Health Econ. 11, 341–353 (2002).
Salaffi, F., Stancati, A., Silvestri, C. A., Ciapetti, A. & Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain. 8, 283–291 (2004).
Suzuki, H. et al. Clinically significant changes in pain along the pain intensity numerical rating scale in patients with chronic low back pain. PLoS One. 15, e0229228 (2020).
Hawkins, R. P., Kreuter, M., Resnicow, K., Fishbein, M. & Dijkstra, A. Understanding tailoring in communicating about health. Health Educ. Res. 23, 454–466 (2008).
Bennell, K. L. et al. Effectiveness of an internet-delivered exercise and pain-coping skills training intervention for persons with chronic knee pain: A randomized trial. Ann. Intern. Med. 166, 453–462 (2017).
Rutledge, T. et al. Randomized controlled trial of telephone-delivered cognitive behavioral therapy versus supportive care for chronic back pain. Clin. J. Pain. 34, 322–327 (2018).
de Rezende, M. U. et al. One-year results of an educational program on osteoarthritis: A prospective randomized controlled trial in Brazil. Geriatr. Orthop. Surg. Rehabil. 7, 86–94 (2016).
Kristjánsdóttir, O. B. et al. A smartphone-based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: randomized controlled trial. J. Med. Internet Res. 15, e5 (2013).
Hughes, S. L. et al. Fit and strong!: Bolstering maintenance of physical activity among older adults with lower-extremity osteoarthritis. Am. J. Health Behav. 34, 750–763 (2010).
Allen, K. D. et al. A combined patient and provider intervention for management of osteoarthritis in veterans: A randomized clinical trial. Ann. Intern. Med. 164, 73–83 (2016).
Allen, K. D. et al. Patient, provider, and combined interventions for managing osteoarthritis in primary care: A cluster randomized trial. Ann. Intern. Med. 166, 401–411 (2017).
Davergne, T., Rakotozafiarison, A., Servy, H. & Gossec, L. Wearable activity trackers in the management of rheumatic diseases: where are we in 2020?. Sensors (Basel). 20, 4797 (2020).
Gualtieri, L., Rosenbluth, S. & Phillips, J. Can a free wearable activity tracker change behavior? the impact of trackers on adults in a physician-led wellness group. JMIR Res. Protoc. 5, e237 (2016).
Eriksson, L., Lindström, B. & Ekenberg, L. Patients’ experiences of telerehabilitation at home after shoulder joint replacement. J. Telemed. Telecare. 17, 25–30 (2011).
Peacock, A. et al. Geographic variation in health service use and perceived access barriers for Australian adults with chronic non-cancer pain receiving opioid therapy. Pain. Med. 17, 2003–2016 (2016).
Eze, N. D., Mateus, C. & Cravo Oliveira Hashiguchi, T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS One. 15(8), e0237585 (2020).
Akiyama, M. & Yoo, B. K. A systematic review of the economic evaluation of telemedicine in Japan. J. Prev. Med. Pub. Health 49, 183–196 (2016).
Devan, H. et al. Current practices of health care providers in recommending online resources for chronic pain self-management. J. Pain Res. 12, 2457–2472 (2019).
Skrepnik, N. et al. Assessing the impact of a novel smartphone application compared with standard follow-up on mobility of patients with knee osteoarthritis following treatment with hylan g-f 20: A randomized controlled trial. JMIR Mhealth Uhealth 5, e64 (2017).
Maddison, R. et al. Usefulness of wearable cameras as a tool to enhance chronic disease self-management: Scoping review. JMIR Mhealth Uhealth 7, e10371 (2019).
Hogg, M. N., Gibson, S., Helou, A., DeGabriele, J. & Farrell, M. J. Waiting in pain: A systematic investigation into the provision of persistent pain services in Australia. Med. J. Aust. 196, 386–390 (2012).
Lynch, M. E. et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain. 136, 97–116 (2008).
Acknowledgements
The authors sincerely thank all of the patients, collaborating physicians and therapists (Motoshi Kaneko, Hidekazu Yuki, Yoshiaki Nishikawa, Keiichiro Kawamura, Yoshiro Yanagisawa, Taichi Takeda, Yuki Mae, Ryuji Katsuda, Shogo Yonemochi, Kunio Ogata), and other medical staff in Hayaishi hospital for their important contributions to this study.
Funding
This work was supported by the Japan Pain Foundation. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
KM led the design of the study design with KH, YS, TT, TT, MH, and MY. KH led the analysis and the interpretation of data and drafted the manuscript with KM, YS, TT, TT, MH, and MY. All authors were involved in the interpretation of the results, writing of the manuscript, and they all approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Hayaishi Hospital (R2-10-30).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hayashi, K., Miki, K., Shiro, Y. et al. Utilization of telemedicine in conjunction with wearable devices for patients with chronic musculoskeletal pain: a randomized controlled clinical trial. Sci Rep 15, 1396 (2025). https://doi.org/10.1038/s41598-024-85056-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-85056-x