Abstract
Diabetes mellitus (DM) is a growing public health concern globally, particularly in Saudi Arabia, where increasing prevalence is associated with significant morbidity. This study aimed to assess the prevalence of diabetes-related complications among patients in Riyadh and examine the impact of sociodemographic factors, comorbidities, and lifestyle habits on these complications. A cross-sectional study was conducted with 980 diabetic patients attending health centers in Riyadh from March to April 2023. Data were collected via a validated bilingual questionnaire that captured sociodemographic information, diabetes-related variables, comorbid conditions, lifestyle habits, and complications. Statistical analyses, including descriptive statistics, chi-square tests, and binary regression, were performed via SPSS to identify significant associations. A p-value less than 0.05 was considered significant for all comparisons. Among the participants (980), 38% (378) reported diabetes-related complications, primarily neuropathy (30%), retinopathy (25%), and cardiovascular diseases (20%). Complications were significantly associated with older age (p < 0.001) and longer diabetes duration (more than 5 years; p < 0.001). Individuals with hypertension, hyperlipidemia, heart disease, kidney disease, and obesity had significantly higher complication rates than those without these conditions (p < 0.05). The most pronounced association was observed in participants with heart disease (85% vs. 15%; RR = 1.506), highlighting the need for better management of these comorbidities. Consuming fruits and vegetables, milk, and regular exercise were inversely associated with the risk of complications (p < 0.05). Conversely, sugary drinks, white bread, sheesha/vaping, and inadequate sleep were linked to increased risk (p < 0.05), highlighting the protective role of healthy dietary and lifestyle habits. This study highlights the impact of sociodemographic factors and lifestyle choices—such as age, education, family history, comorbidities, and poor diet—on diabetes complications. While early detection and lifestyle interventions are vital, a cautious approach is needed when applying these findings to other regions, given differences in socioeconomic circumstances.
Similar content being viewed by others
Background
Diabetes mellitus (DM) is a rapidly increasing global health concern. According to the latest International Diabetes Federation (IDF) Diabetes Atlas, the global prevalence of diabetes has reached 10.5%, with nearly half of adults (44.7%) remaining undiagnosed. IDF projections estimate that by 2045, 783 million adults will have diabetes, which equates to one in eight adults, marking a 46% increase—more than double the anticipated population growth of 20% during the same period1,2. Over the past two decades, the prevalence of diabetes has significantly increased in Gulf Cooperation Council (GCC) countries. Within the MENA (Middle Eastern and North African) region, Saudi Arabia ranks fourth in terms of the diabetic population (aged 20–79). The IDF predicts that by 2045, one-quarter of adults in Saudi Arabia will develop diabetes1.
Diabetes mellitus is a multifaceted condition caused by genetic predispositions and is often triggered by environmental factors3,4. Common lifestyle-related risk factors include diet, physical activity, smoking, and pancreatic infections5,6. Moreover, a region’s socioeconomic conditions significantly influence patients’ access to appropriate treatment7. Despite efforts by the Saudi Arabian government to curb the increasing prevalence of diabetes, controlling the disease remains a challenge because of unhealthy lifestyles, population growth, and the increasing number of elderly people.
Risk factors for diabetes can be divided into nonmodifiable and modifiable categories. Nonmodifiable factors include genetic or familial predispositions, where a strong family history of DM in first- or second-degree relatives significantly increases the risk of developing the condition. Additionally, age is another nonmodifiable factor, as studies show a greater susceptibility to diabetes in older populations. Al Nozha et al. reported a nearly 24% prevalence of DM in individuals over the age of 30 years, increasing to almost 50% for those over 50 years8. Babies born to mothers with gestational diabetes mellitus (GDM) are also at increased risk of developing diabetes later in life. Modifiable factors include obesity, a sedentary lifestyle, and poor nutritional habits. One report reported that the prevalence of obesity ranged from 14% in children under six years of age to 83% in adults9. A cross-sectional study of Saudi adolescents revealed that 84% of males and 91.2% of females spent more than two hours on screen daily, with nearly half of the males and three-quarters of the females not meeting daily physical activity guidelines.
Prevention or delay of type 2 diabetes in individuals with prediabetes involves screening, educational programs, lifestyle changes, nutritional interventions, pharmacologic treatments, and cardiovascular disease prevention10,11,12. Intensive lifestyle interventions, including a healthy diet, increased physical activity, and weight loss, have been shown to significantly reduce the incidence of type 2 diabetes10,13,14,15. Diet plays a crucial role in managing DM, and effective treatment is impossible without proper attention to nutrition16. Dietary interventions should promote weight control, ensure nutritional adequacy, allow for proper glycemic control, and address blood lipid abnormalities16,17,18,19. Achieving weight loss of more than 5% can benefit overweight or obese adults with type 2 diabetes or prediabetes, which can be achieved through caloric restriction and lifestyle modifications20. Recommended eating patterns for individuals with prediabetes include the Mediterranean diet (rich in vegetables, fruits, whole grains, beans, nuts, seeds, and olive oil), a low-calorie diet, and a low-fat diet, with an emphasis on healthy, low-calorie eating10,21,22,23,24.
Despite extensive research on diabetes mellitus (DM), there are significant gaps in understanding the complex interplay between sociodemographic factors, lifestyle choices, comorbidities, and the development of diabetic complications. Many studies have explored individual risk factors, but few have comprehensively assessed how these factors collectively influence complication rates, especially within specific populations such as those in Saudi Arabia. Additionally, while global data on diabetes incidence are well documented, there is limited region-specific evidence that addresses the unique lifestyles, dietary habits, and health challenges faced by Saudi diabetic patients. This gap in the literature hampers the ability to develop targeted interventions tailored to the cultural and environmental contexts of this region. By focusing on the correlations between hypertension, hyperlipidemia, heart disease, kidney disease, obesity, and lifestyle factors such as diet and exercise, this study aims to provide actionable insights into managing and preventing diabetic complications. The goal of this study was to assess the impact of sociodemographic factors, comorbidities, and lifestyle habits on the development of diabetic complications in Saudi Arabian patients.
Methods
Study design and participants
This observational cross-sectional study was conducted between March and April 2023 and targeted individuals diagnosed with type 2 diabetes in health centers across Riyadh, Saudi Arabia. All participants were confirmed type 2 diabetic patients referred by medical teams across study sites. At enrollment, trained outpatient nursing staff classified glycemic control using standardized clinical criteria: Controlled (HbA1c < 7.0%, per ADA guidelines), Uncontrolled (HbA1c ≥ 7.0%), or Unknown (no documented HbA1c within the prior 6 months). While individual laboratory values were not collected, this classification reflects real-world clinical practice where treatment decisions are often based on provider assessments. We acknowledge this methodological approach in our limitations and emphasize that all classifications were made by diabetes-trained nursing staff to ensure consistency. The eligibility criteria included being over 18 years of age, understanding the study objectives, providing informed consent, and visiting outpatient departments at the selected sites. A validated, pretested questionnaire was self-administered by the enrolled participants. Participants were reached through various venues, such as hospitals, health clinics, and health camps. They were provided with links to online questionnaires hosted on Google Forms. Individuals had the option to complete the questionnaire independently or with the help of an attendant, who could input their responses into the form on their behalf. Interviewers were available to address any uncertainties or questions. At the start of the form, the study’s objectives were explained, and informed consent was provided, allowing participants to either agree or decline, ensuring voluntary participation. For those unable to read, the informed consent was verbally explained. Participants were recruited immediately after they consulted with clinicians, ensuring that the information provided was accurate and based on recent discussions with healthcare providers. Additionally, to enhance the reliability of the data, clinicians were consulted regarding key participant details, without accessing the entire contents of the questionnaire. This approach served to corroborate self-reported information and mitigate potential recall bias.
The research proposal received approval from AlMaarefa University’s Institutional Ethical Committee, with reference number IRB23-032. This study adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines to uphold best practices and ethical standards in conducting and reporting the research. All methods were carried out according to relevant guidelines and regulations.
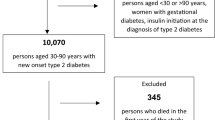
By utilizing a 5% margin of error and a 95% confidence level, the required sample size was determined to be 384 via the Raosoft sample size calculator (http://www.raosoft.com/samplesize.html). Ultimately, 1,242 participants were recruited, with 980 samples included in the final data analysis, as depicted in Fig. 1, which illustrates the enrollment and selection process of the study participants.
Ethical considerations
The Institutional Ethical Committee of AlMaarefa University approved the study (IRB23-032) before data collection. Informed consent was obtained from each participant, accompanied by a form outlining the study’s purpose, methodology, and potential outcomes, emphasizing the voluntary nature of participation. The participants were assured of the confidentiality of their responses and were informed that they could withdraw or refuse participation at any point without repercussions, particularly if they felt uncomfortable with any aspect of the questionnaire.
Questionnaire development and validation
The questionnaire was developed based on a comprehensive literature review and validated through a rigorous three-phase process:
Content validation
An 8-member multidisciplinary panel (endocrinologists, pharmacologists, statisticians, and medical educators) assessed item relevance, clarity, and comprehensiveness using a 4-point Likert scale. Items achieving a Content Validity Index (CVI) ≥ 0.80 were retained, while others underwent iterative refinements.
Pilot testing
The questionnaire was administered to a demographically representative sample (n = 30) to evaluate:
-
Item clarity: 92% of questions were understood without prompting (pre- vs. post-revision).
-
Reliability: Demonstrated strong internal consistency (Cronbach’s α = 0.769 for Arabic; 0.812 for English versions).
Cultural adaptation
Forward-backward translation by bilingual clinicians ensured linguistic accuracy, with semantic equivalence confirmed through cognitive interviews (5 participants per language).
The final instrument demonstrated robust content, construct, and criterion validity. It comprises four sections:
Questionnaire domains
-
1.
Demographics.
-
2.
Age, gender, nationality, education level, marital status, employment, and income.
-
3.
Comorbidity Profile.
-
4.
Self-reported presence of hypertension, hyperlipidemia, cardiovascular disease, chronic kidney/liver disease, thyroid disorders, and obesity.
-
5.
Diabetes Status and Management.
-
6.
Family history, duration since diagnosis, complications, medication adherence, classic symptoms (polyuria, polydipsia, polyphagia), and delayed wound healing.
-
7.
Lifestyle and Dietary Habits.
-
Diet: Frequency of vegetable intake, sugary drinks, refined carbohydrates (white bread, bakery items), full-fat dairy, and spreads.
-
Behaviors: Smoking/vaping status, physical activity levels, sleep duration, and subjective health perception.
Statistical analysis
The collected data were subjected to descriptive and inferential analyses. The risk estimates of factors influencing the development of DM complications were assessed via chi-square relative risk analysis and binary regression analysis. The collected data were subjected to binary regression analysis to identify the factors influencing the development of diabetes mellitus (DM) complications. This method was chosen for its ability to model the relationship between a binary dependent variable (presence or absence of complications) and one or more independent variables (sociodemographic factors, comorbidities, diabetes-related factors, and lifestyle choices). The analysis utilized a significance level of p < 0.05 to determine the statistical significance of each factor. The odds ratios (ORs) were calculated to estimate the likelihood of developing DM complications associated with various risk factors, providing insight into both protective and risk-enhancing characteristics. The 95% confidence intervals (CIs) for the odds ratios were also reported to assess the precision of the estimates. Statistical analysis was conducted via SPSS-IBM version 25.
Results
Association of DM complications with sociodemographic characteristics
The analysis presented in Table 1 examines the demographic characteristics of 980 participants and their associations with the incidence of diabetes-related complications. The findings revealed that participants aged 36 years and older had a significantly greater complication rate (47%, 316 out of 673) than those younger than 36 years (62 out of 307) (p = 0.001). The relative risk (RR) of 3.498 indicates that older participants are more than three times more likely to experience complications.
In terms of sex, complication rates were similar for both males and females at 39% (p = 0.986; RR = 1.002), suggesting that sex does not significantly influence the likelihood of complications. Nationality had a complication rate of 38% among Saudis (306 out of 815) versus 44% among non-Saudis (72 out of 165), although this difference was not statistically significant (p = 0.143; RR = 1.288). Educational attainment appears to impact complication risk, with those with a bachelor’s degree or higher having a lower complication rate of 29% (122 out of 422) than 46% (256 out of 558) among those with less education (p = 0.001; RR = 2.084). Additionally, married participants had a higher complication rate of 43% (277 out of 639) versus 30% (101 out of 341) among single individuals (p = 0.001; RR = 0.550), suggesting an increased risk for married individuals. Employment status also plays a role, as unemployed participants presented a higher complication rate of 45% (235 out of 517) than did employed participants (143 out of 463) (p = 0.001; RR = 1.865).
Moreover, individuals with a family income above 5000 SAR demonstrate a higher complication rate of 43% (177 out of 410) than those earning less (p = 0.012; RR = 1.395). Overall, the study highlights that age, educational level, marital status, employment, and income significantly influence the risk of diabetes complications, emphasizing the need for targeted healthcare interventions for those at greater risk. Sex and nationality, however, do not appear to significantly affect complication rates.
Association of DM complications with comorbidities
Table 2 outlines the relationships between various health conditions and the occurrence of complications among the 980 participants, categorized by their complication status. Individuals with hypertension had a complication rate of 72% (432 out of 547), which was significantly higher than the 28% (170 out of 433) rate in those without hypertension (p = 0.001; RR = 2.012). The participants with hyperlipidemia also had a high complication rate of 76% (455 out of 630), compared with 24% among those without hyperlipidemia (p = 0.001; RR = 1.720). The most striking association was observed in those with heart disease, where the complication rate was 85% (513 out of 777) versus 15% (89 out of 203) for those without heart disease (p = 0.001; RR = 1.506).
Additionally, individuals with kidney disease had an 89% complication rate (536 out of 851) compared with 11% (66 out of 129) of those without kidney disease (p = 0.010; RR = 1.231), and those with liver disease had a complication rate of 95% (571 out of 899) versus 5% (31 out of 81) without kidney disease (p = 0.001; RR = 1.660). The obese participants experienced complications at a rate of 76% (458 out of 666), whereas 24% (144 out of 314) of the nonobese individuals experienced complications (p = 0.001; RR = 1.50). Thyroid problems, however, had no significant effect (p = 0.066; RR = 1.129). These findings highlight the need for effective monitoring and management of hypertension, hyperlipidemia, heart disease, kidney disease, liver disease, and obesity to mitigate the risk of complications.
Association of DM complications with the status of diabetes patients and their controls
Table 3 shows the associations between diabetes-related characteristics and the incidence of complications among 980 participants, categorized by complication status. Participants with a family history of diabetes had a complication rate of 67% (178 out of 264), whereas those without a family history had a complication rate of 59% (424 out of 716). This association was statistically significant (p = 0.022; RR = 1.139), indicating that a family history of diabetes increases the risk of complications.
Individuals with diabetes for more than five years demonstrated a complication rate of 76% (282 out of 369), whereas 76% (291 out of 613) had diabetes for less than five years (p = 0.001; RR = 1.459), suggesting that a longer duration correlates with a greater likelihood of complications. Participants with polyuria had a significantly greater complication rate (74%, 292 out of 588) than those without polyuria (53%, 310 out of 392) (p = 0.001; RR = 1.413).
In terms of polydipsia, participants with this symptom had a complication rate of 72% (312 out of 433), whereas those without it had a complication rate of 53% (290 out of 547) (p = 0.001; RR = 1.359), indicating an elevated risk. Conversely, the presence of polyphagia had no significant effect on complications (p = 0.552; RR = 1.031). Finally, delayed wound healing was associated with a higher complication rate of 51% (197 out of 386) than 68% (405 out of 594) for those without this issue (p = 0.001; RR = 1.336).
Furthermore, adherence to diabetes medications was significantly associated with a reduction in the complication rate. Although the proportion of participants who were non-adherent to their medications was low (7%), they had a 1.534 times higher risk of developing complications compared to those who adhered to their medication regimen.
In summary, significant associations exist between a family history of diabetes, longer diabetes duration, polyuria, polydipsia, delayed wound healing, DM medication adherence, and increased complication risk. Conversely, polyphagia does not significantly affect complication rates, highlighting the need for comprehensive diabetes management to reduce complications effectively.
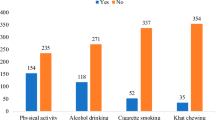
Association of DM complications with food and lifestyle habits
Table 4 explores the associations between various food and lifestyle habits and the incidence of complications among participants with diabetes mellitus. Among those who consumed fruits and vegetables, 61% reported complications, although the relationship was not statistically significant (p = 0.113; RR = 0.842). Conversely, participants who consumed processed foods had a statistically significant association for developing complications (63% Vs. 54%) (p = 0.034; RR = 1.167).
Eating white bread was also significantly associated, where 63% of the consumers experienced complications (p = 0.038; RR = 1.178). Full-fat spread consumption was associated with a greater complication rate (64%), but this difference was not statistically significant (p = 0.129; RR = 1.084). A protective association was identified for milk drinkers, with fewer complications (60% vs. 75% for non-consumers) and a significant p value (p = 0.014; RR = 0.804).
Cigarette smoking was not significantly associated with complications (p = 1.000), whereas smoking sheesha/vaping was significantly associated with a lower complication rate (60%) (p = 0.021; RR = 0.868). Regular exercise (typically involving at least one session per week, with walking being the most common activity) was associated with fewer complications (p = 0.001; RR = 0.799). Sleep duration did not significantly correlate with complications (p = 0.375; RR = 1.051), and those reporting satisfactory health status approached significance (p = 0.056; RR = 1.149).
Overall, the findings underscore the impact of food and lifestyle choices on complications in DM patients, highlighting exercise and milk consumption as protective factors, whereas bakery products and Sheesha/vaping pose greater risks.
Sociodemographic factors influencing the development of complications according to binary regression analysis
The binary regression analysis of sociodemographic factors influencing the development of DM complications revealed that age (< 36 years vs. ≤36 years) (OR = 0.322, 95% CI: 0.222–0.467, p < 0.001) and employment status (employed vs. unemployed) (OR = 0.576, 95% CI: 0.411–0.807, p = 0.001) were significantly associated with a lower likelihood of complications, indicating that younger and employed individuals are less likely to experience complications. Educational level approached significance (OR = 0.753, 95% CI: 0.555–1.020, p = 0.067), suggesting a potential protective effect of higher education. Other factors, including sex (OR = 1.255, 95% CI: 0.927–1.699, p = 0.142), nationality (OR = 0.798, 95% CI: 0.557–1.145, p = 0.220), marital status (OR = 1.282, 95% CI: 0.909–1.807, p = 0.156), and family income (OR = 0.782, 95% CI: 0.551–1.109, p = 0.168), were not statistically significant predictors of DM complications (Table 5).
Influence of comorbidities on the development of DM complications according to binary regression analysis
The binary regression analysis of comorbidities influencing the development of DM complications revealed that hypertension (OR = 1.238, 95% CI: 0.175–2.324, p < 0.001), hyperlipidemia (OR = 1.599, 95% CI: 0.430–3.035, p = 0.002), heart disease (OR = 1.696, 95% CI: 0.451–3.075, p = 0.002), kidney disease (OR = 1.453, 95% CI: 0.840–2.513, p = 0.001), and obesity (OR = 1.625, 95% CI: 0.439–2.890, p = 0.009) were significantly associated with a greater likelihood of developing DM complications. Chronic liver diseases (OR = 0.631, 95% CI: 0.352–1.130, p = 0.121) and thyroid problems (OR = 1.303, 95% CI: 0.862–1.970, p = 0.209) were not significant predictors (Table 6).
Influence of diabetes factors on the development of DM complications according to binary regression analysis
The binary regression analysis of diabetes-related factors influencing the development of DM complications revealed that polyuria (OR = 1.801, 95% CI: 1.262–3.569, p = 0.001), polydipsia (OR = 1.735, 95% CI: 0.515–3.050, p = 0.040), and polyphagia (OR = 1.026, 95% CI: 0.774–2.360, p = 0.035) were significantly associated with complications (Table 7). The duration of diabetes was a strong predictor (OR = 2.370, 95% CI: 1.275–3.498, p < 0.001), and a family history of type 2 DM was also significantly associated (OR = 1.836, 95% CI: 0.610–3.146, p = 0.026). Delayed wound healing presented a marginal association (OR = 0.689, 95% CI: 0.513–0.925, p = 0.073).
Influence of food and life on the development of DM complications according to binary regression analysis
The data analysis revealed significant correlations between diet and lifestyle factors and the development of diabetic complications (Table 8). Specifically, the consumption of fruits and vegetables (OR = 1.749, 95% CI: 0.897–3.411, p = 0.010), consumption of milk (OR = 2.119, 95% CI: 1.172–3.834, p = 0.013), regular exercise (OR = 1.888, 95% CI: 1.369–2.603, p < 0.001), and overall health status (OR = 1.730, 95% CI: 0.510–3.044, p = 0.035) are inversely correlated with the risk of complications, suggesting that these factors may help mitigate risk. In contrast, drinking sugary and sweet drinks (OR = 1.327, 95% CI: 0.919–1.914, p = 0.011), eating white bread (OR = 0.586, 95% CI: 0.386–0.892, p = 0.013), smoking sheesha/vaping (OR = 1.472, 95% CI: 1.012–2.142, p = 0.043), and duration of sleep per day (OR = 0.931, 95% CI: 0.703–1.232, p = 0.016) were directly associated with increased risk, whereas the consumption of bakery products, full-fat spread, and smoking cigarettes did not demonstrate significant correlations. Overall, these findings highlight the protective effects of healthy dietary choices and lifestyle practices against diabetic complications.
Discussion
Diabetes mellitus (DM) is a chronic metabolic disorder characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The global prevalence of diabetes is increasing at an alarming rate, leading to a concomitant rise in complications associated with the disease. This study aimed to explore the associations of DM complications with sociodemographic factors, comorbidities, diabetes status, and lifestyle habits among participants in Riyadh, Saudi Arabia. The findings highlight the complexity of factors contributing to DM complications, emphasizing the necessity for targeted interventions.
Sociodemographic factors
Sociodemographic characteristics play a significant role in the development of diabetes complications. In this study, age emerged as a crucial determinant, with older participants (aged 36 years and above) showing a higher complication rate (47%) than younger individuals (20%). This finding is consistent with international research indicating that age is a significant risk factor for diabetes-related complications. For example, a study conducted by Xu et al.25 in China reported that older age was positively correlated with increased rates of diabetic nephropathy and retinopathy, emphasizing the cumulative effects of chronic hyperglycemia and the natural aging process.
Furthermore, educational attainment influenced complication rates, with individuals with a bachelor’s degree or higher exhibiting lower rates (29%) than those with lower education levels (46%). This observation aligns with findings from a study by Sharif et al.26 in Pakistan, which revealed that higher health literacy positively impacts diabetes self-management, leading to better health outcomes and reduced complication risks. Conversely, those with lower educational levels often lack access to reliable health information, resulting in poor management of their diabetes.
In terms of marital status, married individuals had a higher complication rate, potentially due to shared lifestyle habits or increased stressors associated with family responsibilities. This finding is supported by a study conducted in Jordan by Alzubaidi et al.27, which highlighted that married individuals often face challenges in managing diabetes due to familial obligations, leading to poorer health outcomes. Conversely, unmarried individuals exhibited better health management practices, suggesting the importance of social support in managing chronic conditions.
Diabetes-related status
The association between diabetes-related status and complications was significant in this study. The participants with a family history of diabetes presented a complication rate of 67%, corroborating the findings of Alharbi et al.28 in Saudi Arabia, which emphasized the genetic predisposition to diabetes and its complications. Additionally, the duration of diabetes emerged as a critical factor; individuals diagnosed for more than five years experienced a complication rate of 76%. This finding aligns with international research29, which indicated that a longer diabetes duration is correlated with an increased risk for microvascular and macrovascular complications.
Moreover, the presence of diabetes symptoms such as polyuria and polydipsia, which are significantly associated with higher complication rates, reflects the findings of Sulaiman et al.30. Adherence to diabetes medications is crucial in managing blood glucose levels and preventing the development of diabetes-related complications. Consistent use of prescribed medications helps maintain better glycemic control, which in turn reduces the risk of complications such as cardiovascular disease, neuropathy, and kidney damage. Studies have shown that individuals who adhere to their diabetes medication regimen are less likely to experience these complications compared to those who are non-adherent. In our study, while the proportion of participants with poor medication adherence was low, they were found to have a 1.534 times higher risk of developing complications, highlighting the critical role of adherence in long-term diabetes management. This study highlighted the importance of early symptom recognition and management, as poorly controlled symptoms can lead to serious complications, emphasizing the need for ongoing monitoring and patient education.
Comorbidities
The relationship between comorbidities and diabetes complications is well documented in the literature. In this study, 72% of the participants with hypertension experienced a staggering complication rate. This finding is consistent with research by Khan et al.31, who reported that the prevalence of hypertension among diabetic patients significantly increased the risk of cardiovascular complications. Comorbid conditions, such as heart disease and hyperlipidemia, were also strongly associated with increased complication rates. A study by Aunapuu et al.32 in Estonia indicated that diabetes is often accompanied by cardiovascular diseases, significantly increasing the risk of mortality among patients.
Obesity emerged as a significant factor, with a complication rate of 76% among obese participants, corroborating findings from Elhassan et al.33, who identified obesity as a critical factor influencing diabetes-related complications. The interaction between obesity and diabetes exacerbates the risk of developing complications, reinforcing the need for lifestyle interventions that target weight management.
The impact of comorbidities is further illustrated by research from Faria et al.34, which demonstrated that patients with diabetes and multiple comorbid conditions face a relatively high incidence of complications, underscoring the need for comprehensive management approaches that address both diabetes and its associated comorbidities.
Lifestyle and diet
Lifestyle and dietary choices significantly impact the risk of developing diabetes complications. In this study, the consumption of processed foods and white bread was associated with a higher complication rate. This finding resonates with the research conducted by Al-Najjar et al.35, which emphasized that diets high in refined carbohydrates and sugars are associated with poor glycemic control and an increased risk of complications. The importance of promoting healthy dietary practices cannot be overstated, as evidenced by a study in Canada36, which highlighted the benefits of a Mediterranean diet in reducing diabetes complications.
Interestingly, regular exercise was associated with a lower complication rate (p = 0.001; RR = 0.799), supporting the literature on the benefits of physical activity in improving glycemic control. A systematic review by Colberg et al.37 underscored the role of physical activity in reducing the risk of cardiovascular disease and diabetes complications. This highlights the importance of incorporating regular exercise into diabetes management plans.
Moreover, milk consumption emerged as a protective factor, which aligns with findings from Kamel et al.38, suggesting that dairy products may play a role in metabolic health among diabetic patients. These findings emphasize the need for dietary recommendations that incorporate nutrient-dense foods to promote better health outcomes.
Impact on diabetes-related complications
Several studies across the Middle East and globally echo the findings of this research. In a comprehensive review by Malek et al.39, the associations between lifestyle factors and diabetes complications were explored, revealing that sedentary lifestyles and poor dietary habits significantly increase the risk of complications. Similarly, a meta-analysis by Chen et al.40 indicated that lifestyle interventions, including diet and exercise, effectively reduce the risk of complications among individuals with diabetes.
Moreover, regional studies, such as that by Qureshi et al.41 in the Gulf Cooperation Council (GCC) region, highlighted the role of sociodemographic factors in influencing diabetes management. Their findings indicated that cultural beliefs and socioeconomic status significantly affect diabetes self-management and the development of complications.
In Turkey, a study by Öztürk et al.42 emphasized the critical role of health literacy in diabetes management, supporting the findings of this study regarding the impact of educational attainment on complication rates. Their research highlighted the necessity for targeted educational programs to improve health outcomes among diabetic patients.
Internationally, the relationship between comorbidities and diabetes complications has been extensively documented. A systematic review by Sarwar et al.43 reported that comorbid conditions such as cardiovascular disease, kidney disease, and hypertension significantly increase the risk of complications in diabetic patients. This finding reinforces the findings of this study regarding the need for integrated management strategies addressing both diabetes and its comorbidities.
In summary, the findings of this study contribute to the growing body of literature on diabetes complications, underscoring the multifaceted nature of the disease. The interplay among sociodemographic factors, diabetes status, comorbidities, and lifestyle choices presents a complex landscape that requires comprehensive and individualized approaches to diabetes management. The need for health education, early intervention, and lifestyle modifications is paramount in mitigating the risks associated with diabetes complications.
Cultural beliefs and practices in Saudi Arabia
Cultural beliefs and practices in Saudi Arabia significantly influence the management of diabetes and the associated risk of complications. Traditional dietary practices, such as the consumption of high-calorie, carbohydrate-rich foods (e.g., kabsa and mutabbaq), can negatively affect blood glucose control. Additionally, the cultural practice of fasting during Ramadan can present challenges for individuals with diabetes, as changes in eating patterns may lead to unsafe fluctuations in blood sugar levels if not carefully managed44.
Physical activity levels are generally low in Saudi Arabia due to the hot climate and a sedentary lifestyle, especially in urban areas like Riyadh. Cultural norms, particularly for women, can further limit participation in exercise, impacting diabetes management45. Although walking is culturally acceptable, environmental and social barriers reduce opportunities for regular physical activity, which is essential for controlling diabetes.
Furthermore, while there is respect for medical professionals in Saudi Arabia, many individuals rely on traditional medicine, including herbal remedies and cupping, which may not always be effective in managing diabetes46. This reliance on alternative treatments can delay appropriate medical care and increase the risk of complications. Family dynamics also play a key role in diabetes management, with family support being both a positive influence and a potential barrier, especially when family gatherings encourage overeating.
Limitations
Despite the significant findings of this study, several limitations must be acknowledged to contextualize the results appropriately. The cross-sectional nature of the research restricts the ability to draw causal inferences regarding the relationships between sociodemographic factors and the development of diabetes complications. While the data provide valuable insights into associations, they do not establish direct cause‒and‒effect pathways. Additionally, reliance on self-reported information may introduce biases, as participants may inadvertently overestimate or underestimate their health status, lifestyle habits, or adherence to treatment regimens.
The study was conducted in Riyadh, and while it provides valuable insights, the generalizability of the findings may be limited due to cultural, social, and healthcare differences across other regions of Saudi Arabia and other countries. Riyadh, as a major urban center, shares many healthcare and socioeconomic characteristics with other large cities in Saudi Arabia, which may make the results more applicable to urban populations. However, regional variations in lifestyle, healthcare access, and cultural practices may affect the outcomes, limiting the relevance of the findings to rural areas or countries with different healthcare systems. Additionally, while the sample size is sufficient for statistical analysis, it may not fully represent the diversity of the Saudi population, which further limits the generalizability of the results. The study also focused on a limited range of sociodemographic variables, potentially overlooking the influence of other critical factors such as socioeconomic status and cultural differences. To improve the generalizability of the findings, future studies should include cross-country analyses that account for a wider array of sociodemographic variables.
Another limitation is regarding glycemic control assessment. First, while nursing staff classified participants using clinical HbA1c thresholds (controlled: <7.0%; uncontrolled: ≥7.0%), these classifications lacked laboratory verification, potentially introducing misclassification bias. Second, the absence of longitudinal HbA1c or other glycemic biomarkers limited our ability to evaluate long-term metabolic control. Nevertheless, our focus on sociodemographic, lifestyle, and comorbidity factors provides clinically relevant insights, as demonstrated by Kyrou et al.47 and Sharma et al.48, who established these variables as independent predictors of diabetes outcomes. Future studies should combine both biomarker data and psychosocial determinants for a more comprehensive assessment. Finally, the presence of unmeasured confounders, such as genetic predispositions and environmental influences, could further complicate the interpretation of the results. These limitations underscore the need for further research to validate these findings and explore the underlying mechanisms influencing diabetes complications in the Saudi Arabian context.
Recommendations
Future research should adopt longitudinal designs and incorporate objective measures, such as medical records, to increase data reliability. A broader range of socioeconomic variables should be considered. The implementation of health education initiatives aimed at promoting healthy lifestyles, especially among high-risk populations, is crucial. Additionally, policymakers should foster environments conducive to healthy living, while awareness campaigns can highlight the risks of diabetes complications, encouraging early detection and better management strategies.
Conclusion
This study underscores the multifaceted relationships among sociodemographic factors, diabetes-related status, comorbidities, and lifestyle choices in the development of diabetes complications among participants in Riyadh, Saudi Arabia. Among the 980 participants, 38% (378) reported diabetes-related complications, with the most common being neuropathy (30%), retinopathy (25%), and cardiovascular diseases (20%). The findings highlight that older age, lower educational attainment, a family history of diabetes, comorbidities such as hypertension and obesity, and poor dietary habits significantly contribute to increased complication rates. Addressing these interconnected factors through targeted health education, lifestyle interventions, and comprehensive management strategies is essential for improving health outcomes and reducing the burden of diabetes complications in the region. Continued research is necessary to inform effective public health initiatives.
Data availability
The authors confirm that the data supporting the findings of this study are as represented within the article and the framework can be made available on request to the corresponding author.
References
International Diabetes Federation. IDF Diabetes Atlas (7th ed). IDF news. (Accessed 28 Nov 2023) (2021).
Abdulaziz, A. M. et al. Diabetes mellitus in Saudi Arabia: a review of the recent literature. Curr. Diabetes. Rev. 12 (4), 359–368 (2016).
Hu, F. B. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids 38 (2), 103–108 (2003).
Hirschhorn, J. N. Genetic epidemiology of type 1 diabetes. Pediatr. Diabetes. 4 (2), 87–100. https://doi.org/10.1034/j.1399-5448.2001.00013.x (2003).
Alhyas, L., McKay, A. & Majeed, A. Prevalence of type 2 diabetes in the States of the co-operation Council for the Arab States of the Gulf: a systematic review. PLoS One. 7 (8). https://doi.org/10.1371/journal.pone.0040948 (2012).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 298 (22), 2654–2664. https://doi.org/10.1001/jama.298.22.2654 (2007).
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 27 (2004).
Al-Nozha, M. M. et al. Diabetes mellitus in Saudi Arabia. Saudi Med. J. 25, 1603–1610 (2004).
Madani, K. A. Obesity in Saudi Arabia: a review. Bahrain Med. Bull. 22 (3), 113–118 (2000).
Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J. Diabetes ;42(Suppl 1) (2018).
National Institute for Health and Care Excellence (NICE). NICE NG28 type 2 DM guideline 2010. (2017).
American Diabetes Association. Prevention or delay of type 2 diabetes: standards of medical care in diabetes—2020. Diabetes Care 43(Suppl 1) (2020).
Knowler, W. C. et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or Metformin. N. Engl. J. Med. 346, 393–403 (2002).
Lindström, J. et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish diabetes prevention study. Lancet 368, 1673–1679 (2006).
Li, G. et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing diabetes prevention study: a 23-year follow-up study. Lancet Diabetes Endocrinol. 2, 474–480 (2014).
Norris, S. L., Lau, J., Smith, S. J., Schmid, C. H. & Engelgau, M. M. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 25, 1159–1171 (2002).
Evert, A. B. et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 42, 731–754 (2019).
MacLeod, J. et al. Academy of nutrition and dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: nutrition intervention evidence reviews and recommendations. J. Acad. Nutr. Diet. 117, 1637–1658 (2017).
Sainsbury, E. et al. Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: a systematic review and meta-analysis. Diabetes Res. Clin. Pract. 139, 239–252 (2018).
Franz, M. J., Boucher, J. L., Rutten-Ramos, S. & VanWormer, J. J. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J. Acad. Nutr. Diet. 115, 1447–1463 (2015).
Salas-Salvadó, J. et al. Protective effects of the mediterranean diet on type 2 diabetes and metabolic syndrome. J. Nutr. 146, 920S–7S (2016).
Bloomfield, H. E. et al. Effects on health outcomes of a mediterranean diet with no restriction on fat intake: a systematic review and meta-analysis. Ann. Intern. Med. 165, 491–500 (2016).
Estruch, R. et al. PREDIMED study investigators. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extravirgin Olive oil or nuts. N. Engl. J. Med 378 (2018).
Schwingshackl, L., Bogensberger, B. & Hoffmann, G. Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet. 118, 74–100e11 (2018).
Xu, X. et al. Association of age and diabetes complications: a population-based study in China. Diabetol. Int. 11 (3), 207–215 (2020).
Sharif, N., Khattak, I. & Noorani, M. M. The impact of educational attainment on diabetes self-management: a study from Pakistan. Int. J. Diabetes Dev. Ctries. 41 (1), 122–130 (2021).
Alzubaidi, H., Rababa, M. & Hayajneh, F. Marital status and diabetes complications: the role of family dynamics in Jordan. J. Diabetes Res. 2020, 6057385 (2020).
Alharbi, M. et al. Family history and diabetes complications: a genetic predisposition study in Saudi Arabia. Saudi Med. J. 42 (5), 504–510 (2021).
Zafar, A., Ahmed, T., Qureshi, S. & Ali, M. The impact of diabetes duration on complications: a multicenter study in Pakistan. Pak J. Med. Sci. 36 (2), 201–206 (2020).
Sulaiman, N., Al-Habib, A. & Hussain, F. Early symptoms and diabetes complications in Saudi Arabia: a retrospective cohort study. Diabetes Metab. Syndr 17(1). (2023).
Khan, M., Gupta, N. & Hassan, I. Prevalence of hypertension among diabetic patients: a study from India. J. Clin. Hypertens. 21 (6), 798–804 (2019).
Aunapuu, M., Pirn, I. & Loit, H. M. Cardiovascular complications in diabetic patients: a population-based study in Estonia. BMC Cardiovasc. Disord. 22 (1), 102 (2022).
Elhassan, A., Alsulaiman, N. & Abdelgadir, N. Obesity and its effect on diabetes complications in Saudi Arabia. J. Diabetes Obes. 9 (1), 24–31 (2022).
Faria, C., Sousa, R. & Santos, A. C. Comorbidities and diabetes complications: a Portuguese perspective. Eur J. Public Health 30 (2020). (Suppl 5).
Al-Najjar, N., Al-Qazwini, F. & Ali, A. Dietary patterns and glycemic control: a study in Kuwait. Kuwait Med. J. 51 (2), 123–129 (2019).
Campbell, T., Smith, M. & Baker, R. The mediterranean diet and diabetes management: a Canadian study. J. Nutr. Health Aging. 25 (3), 456–463 (2021).
Colberg, S. R. et al. Physical activity/exercise and diabetes: a systematic review. Diabetes Care. 39 (11), 2065–2079 (2016).
Kamel, R., Gomaa, A. & Al-Mansouri, A. The role of dairy in managing diabetes: a systematic review from Saudi Arabia. Saudi J. Biol. Sci. 29 (3), 1448–1453 (2022).
Malek, A., Hariri, N. & Saadeh, N. Sedentary lifestyles and diabetes complications: A review of studies in the middle East. Diabetes Metab. Res. Rev 38(5) (2022).
Chen, L., Pei, J., Kuang, J., Chen, H. & Chen, Z. Lifestyle interventions and diabetes complications: A meta-analysis. Diabetes Res. Clin. Pract 161 (2020).
Qureshi, N., Ahmed, T. & Rehman, T. Sociodemographic factors and diabetes management in the GCC region: A review. Gulf Med. J. 10 (1), 57–63 (2021).
Öztürk, H., Kiliç, M. & Demirbas, H. Health literacy and diabetes management in Turkey: the role of education in improving outcomes. Turk. J. Endocrinol. Metab. 24 (2), 93–101 (2020).
Sarwar, N. et al. Diabetes, comorbidities, and the risk of major complications: A systematic review. Lancet 376 (9739), 2076–2084 (2020).
Al-Shaer, I. A. et al. The impact of ramadan fasting on diabetes control and management in Saudi Arabia. J. Diabetes Res. 2020, 1–9 (2020).
Alqurashi, K. A., Aljabri, K. S. & Alzahrani, A. S. Physical activity and health in Saudi Arabia. Saudi Med. J. 32 (8), 777–783 (2011).
Al-Daghri, N. M., Al-Attas, O., Alokail, M. S., Abd-Alrahman, S. H. & Alokail, M. S. Traditional medicine use in the management of diabetes in Saudi Arabia. J. Ethnopharmacol. 136 (3), 503–507 (2011).
Kyrou, I. et al. Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: a narrative review with emphasis on data from Europe. BMC Endocr. Disord. 20 (Suppl 1), 134. https://doi.org/10.1186/s12902-019-0463-3 (2020).
Sharma, K. et al. Depression and anxiety among patients with type II diabetes mellitus in Chitwan medical college teaching hospital, Nepal. Nurs. Res. Pract. 2021, 8846915. https://doi.org/10.1155/2021/8846915 (2021). PMID: 33520315; PMCID: PMC7817292.
Acknowledgements
The authors would like to acknowledge the Researchers Supporting Project number (RSP2025R115), King Saud University, Riyadh, Saudi Arabia, for extending financial support to do this research project. The Authors would like to thank the Deanship of Scientific Research at Shaqra University for supporting this work.
Funding
The authors would like to express gratitude to King Saud University, Riyadh, Saudi Arabia, for extending financial support to do this research project through the Researchers Supporting Project number (RSP2025R115). The authors are also thankful to AlMaarefa University, Riyadh, Saudi Arabia for supporting this research through the Researchers Supporting Project number (MHIRSP2024002).
Author information
Authors and Affiliations
Contributions
OA, NFA, FRNA, WRA, LKA, FNA, MA (Mansour Almuqbil), SMBA, and HAO: Study conception and design. WFA, ASA, MA (Majid Alhomrani), and AMA: Acquisition of data. NFA, FRNA, WRA, LKA, FNA, and MA (Mansour Almuqbil): Analysis and interpretation of data. WFA, ASA, MA (Majid Alhomrani), and AMA: Drafting of the manuscript. OA and SMBA: Critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The ethical approval for this study was obtained from the institutional review board of AlMaarefa University, Riyadh, Saudi Arabia via approval number IRB23-032. Informed consent was obtained from all participants before their involvement in the study. The purpose, procedures, potential risks, and benefits were thoroughly explained to the participants, ensuring their understanding. They were informed that their participation was voluntary and that they could withdraw from the study at any time without any consequences. Participants who were unable to read or comprehend the consent form were provided with a detailed verbal explanation. Consent was obtained either through written or verbal agreement before the study commenced.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
AlOmeir, O., Almuqbil, M., Alotaibi, N.F. et al. Prevalence and impact of sociodemographic factors, comorbidities, and lifestyle on diabetes complications among patients with type 2 diabetes in Riyadh. Sci Rep 15, 17299 (2025). https://doi.org/10.1038/s41598-025-02559-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02559-x