Abstract
Recent interest in growth differentiation factor 15 (GDF15) has been further heightened by its association with rheumatic diseases. GDF15 has been extensively studied as a potential diagnostic and prognostic biomarker. However, no direct evidence currently links GDF15 to primary Sjögren’s syndrome (pSS). In this study, we measured serum GDF15 levels in 151 pSS patients and 61 healthy controls (HCs). GDF15 levels were significantly elevated in pSS patients compared to HCs. Receiver operating characteristic (ROC) curve analysis demonstrated that GDF15 effectively distinguished pSS patients from HCs. Notably, GDF15 levels were higher in pSS patients with extra-glandular manifestations and positively correlated with the number of such manifestations. Specifically, elevated GDF15 levels were observed in patients with pulmonary, hematological, renal, or nervous system involvement. Furthermore, GDF15 levels were significantly increased in patients with active disease compared to those in non-active stage, and ROC analysis confirmed its discriminative capacity for disease activity. Using advanced machine learning techniques, we developed an adaptive boosting model that combined GDF15 with albumin, red blood cell count, and C-reactive protein, which showed reliable predictive value for disease activity. These findings suggest that serum GDF15 may serve as a valuable biomarker for assessing disease severity and guiding treatment in pSS.
Similar content being viewed by others
Introduction
Primary Sjögren’s syndrome (pSS) is a chronic autoimmune disorder characterized by lymphocytic infiltration of exocrine glands, leading to xerostomia and keratoconjunctivitis sicca, which significantly impacts the quality of life for affected individuals1. The clinical presentation of pSS is highly heterogeneous, characterized by hallmark symptoms dry mouth and dry eyes, as well as a variety of extra-glandular manifestations (EGMs) that can affect multiple organs and systems, including the joints, skin, kidneys, lungs, and nervous system2. EGMs may range in severity and affect the prognosis of pSS patients3,4.
A key aspect of pSS management is the assessment of disease activity, which is crucial for monitoring disease progression, guiding treatment decisions, and evaluating therapeutic responses5. Disease activity in pSS is multifaceted, encompassing clinical symptoms, serological markers, and immunological parameters. The accurate measurement of disease activity is challenging due to the heterogeneous presentation of pSS and the lack of universally accepted activity indices. However, various tools, including the EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI), have been developed to standardize this assessment5. Recent researches have also highlighted the potential role of novel biomarkers, such as circular RNAs6 and specific cytokines7,8,9, in reflecting disease activity and providing insights into the underlying immunopathogenesis of pSS.
Growth differentiation factor 15 (GDF15), a cytokine belonging to the transforming growth factor-β (TGF-β) superfamily, has garnered significant attention for its potential as a biomarker in various pathological conditions10. Initially recognized for its role in cellular growth and differentiation, GDF15 has been found to be up-regulated under circumstances of cellular stress, inflammation, and tissue injury11. Recent studies have implicated GDF15 in a range of diseases, including cardiovascular disorders11, cancer12, and autoimmune diseases13,14,15,16, highlighting its potential as a diagnostic, prognostic, and therapeutic target. In the context of rheumatic diseases, GDF15 has been the subject of intensive study due to its potential as a diagnostic and prognostic biomarker13,14,15,17. Its elevated levels in serum and tissue have been correlated with disease severity and response to treatment in systemic lupus erythematosus15, stable multiple sclerosis13, dermatomyositis14, polymyositis14, and other idiopathic inflammatory myopathies18. The ability of GDF15 to reflect the underlying pathological processes, including inflammation19 and muscle damage14,20, positions it as a valuable tool in the rheumatologist’s arsenal. However, there is currently no direct evidence linking GDF15 to pSS. Hence, further research is needed to elucidate the specific role of GDF15 in pSS and its potential as a biomarker.
Methods
Human subjects
In this study, 151 pSS patients (145 females and 6 males) treated at the Xiangya Hospital between December 2022 and March 2024 were recruited. Diagnoses were based on the 2012 ACR criteria and the 2016 pSS classification criteria21,22. The exclusion criteria for pSS were as follows: 1. age below 18 years; 2. pregnancy; 3. complication with other systemic autoimmune diseases, or other major illnesses; 4. diagnosis of HIV, HCV and/or other virus infections; 5. cancer; 6. cases with incomplete clinical data. Disease activity was evaluated using the ESSDAI to judge the degree of disease activity of pSS patients. Patients with ESSDAI scores ≥ 5 were in the active stage of disease, while patients with ESSDAI scores < 5 were in the nonactive stage of disease5. In the same period, 61 age- and sex-matched healthy persons were recruited among adults who had undergone routine physical examinations and had no chronic medical problems or medications as the healthy controls (HCs). Informed written consent was obtained from all subjects, and the study was approved by the Ethics Committee of Xiangya Hospital, Central South University, where the study was performed. Research have been performed in accordance with the Declaration of Helsinki.
Data collection
Clinical data including age, sex, disease duration, clinical symptoms and treatment were collected. The data of clinical symptoms gathered encompassed dry eyes, dry mouth, and EGMs, including ongoing joint involvement, pulmonary involvement, interstitial lung disease (ILD), skin vasculitis, peripheral neurological involvement, central nervous involvement, haematopoietic system involvement and renal involvement characterized by persistent proteinuria, tubular acidosis, interstitial nephritis, or glomerulonephritis. The criteria for haematopoietic system involvement are the presence of neutropenia or anaemia or thrombocytopenia5.
The following laboratory parameters were analyzed: total protein, albumin, globulin, albumin/globulin, erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, complement fractions 3, complement fractions 4, immunoglobulins G, immunoglobulins A, immunoglobulins M, white blood cell count, red blood cell count, haemoglobin, neutrophil count and platelet count. These samples were analyzed within 24 h of enrolment using routine laboratory techniques. Anti-SSA and anti-SSB antibody were detected using immunoblotting and antinuclear antibody using indirect immunofluorescence. Demographic data of the patient groups are shown in Table 1.
Measurement of serum GDF15 levels
All serum samples were quickly frozen after centrifugation and stored at -20℃. Serum GDF15 levels were measured within 12 months after collection. Serum GDF15 levels were measured using a GDF15 chemiluminescent immunoassay kit (Maccura Biotechnology, Chengdu, China). The details of the experiment shown in the previously published article14.
Statistical analysis
Data were tested for normality using the Kolmogorov–Smirnov test. Differences between groups were assessed using the t-test or Mann–Whitney non-parametric test. Data are shown as the mean ± standard deviation or median with interquartile range, as appropriate. The correlations between variables were evaluated using the Spearman’s rank correlations. Receiver operating characteristic (ROC) curves were used to evaluate the discriminative role of the serum markers. In all comparisons and correlations, statistical significance was assumed if p < 0.05. Statistical analyses were performed using Prism software (version 5.0; GraphPad Software, Inc., San Diego, CA, USA) or the Deepwise and Beckman Coulter DxAI platforms (http://dxonline.deepwise.com).
Predictive model construction using machine learning
To develop a predictive model for evaluating disease activity, we employed the Deepwise and Beckman Coulter DxAI platforms for identifying key variables and constructing the model. The clinical features outlined in Table 3 served as the independent variables. The feature selection process was conducted in two phases. Initially, we assessed statistical differences using either the Student’s t-test or the Wilcoxon rank-sum test for continuous variables, based on their distribution characteristics. Subsequently, we determined the Spearman’s correlation coefficients among the features that showed significant differences. When a correlation coefficient between any two features surpassed 0.7, one feature was randomly eliminated to mitigate multicollinearity. Following feature selection, we utilized four machine learning algorithms to develop predictive models: logistic regression, adaptive boosting (Adaboost), decision tree, and random forest. To further optimize these models, we applied a refinement strategy based on the feature importance from the top-performing models, eliminating variables with minimal impact. The Delong test was utilized to assess whether there were statistical differences in the area under the curve (AUC) values between the refined model and full model. A five-fold cross-validation method was used to assess the performance of the machine learning algorithms. The entire dataset was divided into five folds, using four folds for the training set to build the model and the remaining fold was used as the internal validation set to score the model. This process was repeated five times. The optimal predictive model was selected on the basis of the performance of the internal validation set. Model performance was evaluated using AUC, accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and F1-score. Statistical significance was considered if the two-sided p value was below 0.05.
Results
Serum GDF15 levels in pSS patients and HCs
Serum GDF15 concentrations (median [interquartile range]) in pSS patients were significantly higher than that in HCs (1190 pg/mL [821–2176.7] vs 671.7 pg/mL [552.7–819.1], p < 0.001; Fig. 1A). To evaluate the value of serum GDF15 as a clinical marker of pSS, ROC curve analysis was performed on the relative expression levels of GDF15 in patients with pSS and HCs. The AUC value of GDF15 was 0.78 (95% CI: 0.73–0.86, P < 0.001, Fig. 1B), the sensitivity was 70.90%, and the specificity was 80.30%.
Serum levels of GDF15 in pSS patients. (A) Serum GDF15 levels in patients with primary Sjögren’s syndrome (pSS) and healthy controls (HCs). (B) Area under the receiver operating characteristic (ROC) curve was used to assess the ability of GDF15 level to distinguish between patients with pSS and HCs. The reference curve is also shown. (C) Serum GDF15 levels in anti-SSA negative pSS patients and HCs. (D) ROC curve analysis was used to assess the ability of GDF15 level to distinguish between anti-SSA negative pSS patients and HCs. (E) Serum GDF15 levels in pSS patients with disease duration ≥ 10 years group and disease duration < 10 years group. (F, G) The correlation of serum GDF15 levels with age in HCs (F) and pSS patients (G). Statistical significance is indicated by asterisks: *** p < 0.001.
Further, we compared the serum GDF15 levels in anti-SSA negative pSS patients and HCs. As shown in Fig. 1C, the serum GDF15 levels in anti-SSA negative pSS patients (1968.9 pg/mL [986.2–3007.3]) was significantly higher than in HCs (p < 0.001). ROC curve analysis was performed, and the AUC value was 0.84 (95% CI: 0.69–0.98, P < 0.001, Fig. 1D), the sensitivity was 84.60%, and the specificity was 77.0% to distinguish anti-SSA negative pSS patients and HCs.
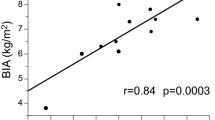
Patients with disease duration ≥ 10 years showed higher serum GDF15 levels (2,181 pg/mL [1527.4 − 2896.5], n = 23) than those disease duration < 10 years (1125.2 pg/mL [787.9 − 1,824.6], n = 128, p < 0.001, Fig. 1E). GDF15 levels in disease duration ≥ 10 years group and disease duration < 10 years group were both higher than those in HCs (p < 0.001 in both cases, Fig. 1E). Moreover, we found a positive correlation between GDF15 levels and age in HCs (r = 0.59, p < 0.001, Fig. 1F), which was also present in patients with pSS (r = 0.49, p < 0.001, Fig. 1G).
The serum GDF15 levels and clinical manifestations of pSS patients
To investigate the relationship between serum levels of GDF15 and clinical symptoms in pSS patients, participants were categorized into those with and without dry mouth or dry eyes. Results showed that there were no significant differences in serum GDF15 concentrations between the groups with and without the aforementioned symptoms (both p > 0.05, Fig. 2A, B). In addition to the classic symptoms, other clinical manifestations of pSS patients were diverse, featuring numerous EGMs. Related data about EGMs are listed in Table 1. To explore the correlation between serum GDF15 and EGMs, pSS patients were divided into two groups: those with EGM and those without EGM. The serum levels of GDF15 were higher in patients with EGM (1330 pg/mL [885.1 − 2620], n = 122) than in those without EGM (986.2 pg/mL [737 − 1274], n = 29, Fig. 2C). Further, ROC curve analysis was performed on GDF15 to distinguish pSS-EGM and pSS-non-EGM, and the AUC value was 0.68 (95% CI: 0.58–0.76, P < 0.01, Fig. 2D). Table 2 presents the characteristic of these two groups. Compared to pSS-non-EGM patients, pSS patients with EGM had higher levels of C-reactive protein, erythrocyte sedimentation rate, white blood cell count, and neutrophil count. In addition, the levels of total protein, albumin and haemoglobin were lower in pSS-EGM patients, when compared to pSS-non-EGM patients.
Association between clinical manifestations and serum levels of GDF15 in pSS patients. (A, B) Serum GDF15 levels in patients with or without (A) dry eye and (B) dry mouth were detected. (C) Serum GDF15 levels in pSS-EGM subgroups and pSS-non-EGM. (D) ROC curve analysis was used to assess the ability of GDF15 level to distinguish between pSS-EGM and pSS-non-EGM group. (E) A comparison of serum GDF15 concentrations among groups stratified by the number of EGMs present. (F) Patients were sorted into six subgroups based on their types of symptoms: arthritis involvement, cutaneous involvement, pulmonary involvement, hematological involvement, renal involvement, and nervous system involvement. Serum GDF15 levels in patients with above-mentioned symptoms and pSS-non-EGM. (G) Pulmonary-involved group were divided into two groups: interstitial lung disease (ILD) group and other pulmonary-involved group. Serum GDF15 levels in ILD group, other pulmonary-involved group and pSS-non-EGM. Statistical significance is indicated by asterisks: **p < 0.01, ***p < 0.001, n.s. p > 0.05.
In pSS-EGM patients, the number and types of affected systems were variated. The proportion of pSS patients with involvement of one, two, three, or four EGMs was 36.4%, 28.5%, 12.6%, and 3.3%, respectively. The serum GDF15 concentrations in two, three, or four EGMs involved groups were significantly higher than zero or one EGMs involved groups (all p < 0.01, Fig. 2E). In addition, we sorted the patients into six subgroups based on their types of symptoms. There was a notable rise in GDF15 levels in patients with pulmonary involvement (n = 73, p < 0.001), hematological involvement (n = 39, p < 0.001), renal involvement (n = 13, p < 0.01), and nervous system involvement (n = 18, p < 0.01), compared to pSS-non-EGM patients (n = 29), except for those with arthritis involvement and cutaneous involvement (both p > 0.05, Fig. 2F). To further distinguish the impact of ILD within the pulmonary-involved group, we categorized these patients into two groups: ILD group and other pulmonary-involved group. Results showed that the levels of GDF15 were much higher in the ILD group (n = 33) compared with other pulmonary-involved group (n = 40, Fig. 2G). GDF15 levels in both the ILD group and other pulmonary-involved group were higher than those pSS-non-EGM group (p < 0.001 and p < 0.01, Fig. 2G).
Correlation of GDF15 and laboratory parameters of pSS patients
Serum GDF15 levels showed significant correlations with several peripheral blood component parameters in pSS patients. Specifically, serum GDF15 level negatively correlated with haemoglobin (r = −0.45, p < 0.001, Fig. 3A), red blood cell count (r = −0.44, p < 0.001, Fig. 3B), and albumin (r = −0.54, p < 0.001, Fig. 3C). Conversely, serum GDF15 level positively correlated with C-reactive protein (r = 0.38, p < 0.001, Fig. 3D) and erythrocyte sedimentation rate (r = 0.46, p < 0.001, Fig. 3E).
Association of GDF15 with laboratory parameters of pSS patients. Correlation between serum GDF15 level and haemoglobin (A), red blood cell count (B), albumin (C), C-reactive protein (D), erythrocyte sedimentation rate (E) and ESSDAI (F). Statistical significance is indicated by asterisks: *** p < 0.001.
The serum GDF15 levels and disease activity in pSS patients
To investigate the role of GDF15 in disease activity, we initially investigated the correlation of serum GDF15 levels with ESSDAI score. As shown in Fig. 3F, serum GDF15 level positively correlated with ESSDAI score (r = 0.45, p < 0.001). Furthermore, according to the ESSDAI score, patients with ESSDAI scores ≥ 5 were categorized into the disease activity group, and those with ESSDAI scores < 5 were included in the non-disease activity group. One hundred and nineteen patients were included in the disease activity group, and an ESSDAI score was 13.0 ± 6.8. Thirty-two patients were included in the non-disease activity group, and an ESSDAI score was 2.3 ± 1.3. The serum GDF15 in the disease activity group was 1423 pg/mL (934–2674), which was higher than that in the non-disease activity group (821 pg/mL [632–1078]) (p < 0.001, Fig. 4A). Moreover, ROC analysis was performed to further assess the potential of using GDF15 level to discriminate between active or non-active stages. The corresponding AUC values were 0.78 (95% CI: 0.71–0.86, p < 0.001, Fig. 4B). Based on the ROC curve coordinates, the cut-off value for GDF15 concentrations were 1358.8 pg/mL, with a sensitivity of 52.1%, and a specificity of 100%.
The serum GDF15 levels and disease activity in pSS patients. (A) Expression of serum GDF15 levels in pSS patients with active stage and non-active stage. (B) ROC curve analysis was used to assess the ability of GDF15 level to distinguish between pSS patients with active stage and non-active stage. (C) ROC curves of four models to distinguish pSS patients in active stage or in non-active stage. Statistical significance is indicated by asterisks: ***p < 0.001.
Establishment and evaluation of a predictive model
To enhance the accuracy of serum GDF15 level in identifying pSS patients with active or non-active stages, we integrated GDF15 levels with other variables into machine learning models and assessed their predictive reliability. Firstly, 9 parameters that significantly differed between active and non-active stages were screened out (Table 3). Secondly, a correlation analysis was performed on the 9 variables, retaining only one variable when correlation coefficients exceeded 0.7, which let to the exclusion of haemoglobin and globulin. The screened variables were then processed for model training. Within the scope of this study, we utilized four machine learning algorithms to build our predictive model: logistic regression, Adaboost, decision tree, and random forest. The Adaboost model demonstrated the highest performance, with an AUC of 0.91. By examining the feature importance within the model, we identified the four most influential features including albumin, GDF15, red blood cell count, and C-reactive protein, and employed these to construct predictive models.
The optimal predictive model was selected based on the internal validation set performance. All four models achieved an AUC greater than 0.88 (Fig. 4C). Among them, the Adaboost model demonstrated the best performance regarding AUC, specificity, accuracy, and F1 score (Table 4). In the Adaboost model, the feature weights were distributed as follows: albumin had the highest weight, followed by GDF15, red blood cell count and C-reactive protein, with values of 1, 0.5169, 0.2503 and 0.191, respectively.
In this research, we created an online tool for pSS patients to predict whether they are in an active or inactive stage, which can be widely applied. The resulting probability and outcome can be found on the following website: https://dxonline.deepwise.com/prediction/index.html?baseUrl=%2Fapi%2F&id=49100&topicName=undefined&from=share&platformType=wisdom
Discussion
In this study, we showed that serum levels of GDF15 were significantly increased in patients with pSS, even in anti-SSA negative patients. PSS patients with EGMs exhibited elevated levels of GDF15, with the concentration tending to increase in tandem with a higher count of EGMs. Notably, the level of GDF15 strongly distinguished between patients with pSS in the active and non-active stages. This study is the first to focus on the GDF15 concentration in relation to pSS patients.
Recent studies have focused on GDF15 and rheumatic diseases, with elevated serum levels of GDF15 observed in patients with systemic lupus erythematosus15, stable multiple sclerosis13, rheumatoid arthritis16, and idiopathic inflammatory myopathies14,17. In this study, we found that serum GDF15 levels were significantly higher in patients with pSS, the elevated serum levels of GDF15 could serve as a diagnostic biomarker for pSS, assisting in the identification of the disease. Furthermore, our research showed that even in anti-SSA negative pSS patients, serum GDF15 levels were markedly higher than in HCs. Anti-SSA antibodies are prevalent among individuals with pSS and play a significant role in the diagnostic criteria for pSS22. Nonetheless, a considerable proportion, estimated between 30 and 40%, of pSS patients who meet the 2016 diagnostic criteria are negative for these antibodies2. This indicates that even in the absence of anti-SSA antibodies, we can distinguish pSS patients from HCs based on serum GDF15 levels. Furthermore, patients with a disease duration of 10 years or more showed higher circulating GDF15 levels than those with a disease duration of less than 10 years, suggesting that GDF15 levels are related to the severity and complexity of disease. In addition, we found a positive correlation between GDF15 and age, both in HCs and pSS patients, which is consistent with previous report17,23. The exploration of GDF15 in rheumatic diseases is particularly significant as it offers insights into the complex interplay between the immune system and the cytokine network.
PSS is a chronic, systemic autoimmune disease characterized by a diverse spectrum of clinical manifestations. While the hallmark symptoms are dry mouth and dry eyes, many patients with pSS also experience a range of EGMs that affect multiple organs and systems. As shown in this paper, approximately 80.8% of pSS patients had one or more EGMs, which was consistently with recently published studies8. Notably, patients with EGMs exhibit higher GDF15 level, which rose with the number increase of EGMs. Among the involved extra-glandular organs, lungs were the most commonly in this study, with ILD being the most common type. The levels of GDF15 were highest in ILD patients, lower in other pulmonary-involved group, and the lowest in non-pulmonary-involved group, which consistent with our previous reports in dermatomyositis and polymyositis14, suggesting the relation between GDF15 and pulmonary disease. Literature reports indicated that in idiopathic pulmonary fibrosis24, chronic obstructive pulmonary disease25, and pulmonary arterial hypertension25, GDF15 significantly increased and correlated with the decline of lung function and disease severity. Interestingly, GDF15 mitigated lung damage caused by sepsis, by inhibiting glycolysis and inflammatory responses in alveolar macrophages26, suggesting the immunoprotective role of GDF15 in pulmonary disease. Hence, we guess that the elevation of GDF15 in serum may be the protection mechanism initiated after body injure. Additionally, we also found that GDF15 is related to kidney, haematopoietic and nervous system damage. Regarding kidney damage, research has shown that GDF15 is closely associated with proteinuria, glomerulosclerosis, and renal function impairment27, and it is significantly elevated under renal disorders27. All of these findings indicate that the serum level of GDF15 in pSS patients may be correlated with disease severity.
The assessment of disease activity is crucial for informing treatment decisions in pSS. For patients with active disease, systemic treatments such as immunosuppressants and corticosteroids may be necessary to manage inflammation and immune responses. In contrast, patients with stable disease conditions might benefit more from symptom management, including the use of artificial tears and saliva substitutes to alleviate dryness symptoms28. Therefore, identifying novel biomarkers that can effectively assess disease activity is a significant research priority. Our findings suggest that the level of GDF15 could serve as a valuable biochemical indicator for monitoring disease activity. Firstly, we observed that GDF15 levels were notably elevated in individuals with pSS during active phases compared to non-active phases. Higher serum GDF15 levels may reflect the intensity of the immune response and the extent of glandular inflammation. Secondly, GDF15 level were higher in pSS patients with EGMs, and they rose with the increase of the number of EGMs. Thirdly, our analysis using the ROC curve validated these findings. By integrating GDF15 levels with albumin, red blood cell count, and C-reactive protein, we developed predictive models that could accurately determine disease activity in pSS patients with an AUC of 0.91. This underscores the significant prognostic value of GDF15 levels in evaluating disease activity in pSS. These advances offer hope for a more nuanced understanding of disease activity in pSS and may facilitate the development of personalized therapeutic strategies tailored to individual patients’ needs.
The TGF-β superfamily, comprising TGF-β, bone morphogenetic protein (BMPs), GDFs and activins, plays a pivotal role in immune regulation29. Despite its immunological significance, research on TGF-β superfamily members in pSS remains limited. As a prototypical member, TGF-β1 has emerged as a reliable diagnostic biomarker for pSS. Its serum levels demonstrate positive correlations with both disease activity and labial gland histopathological severity in pSS patients30, a finding corroborated by our study. Mechanistically, TGF-β exhibits anti-inflammatory properties through TNF-α suppression in pSS pathogenesis31. Intriguingly, another superfamily member BMP6 shows elevated expression in pSS patients, where it exacerbates autoimmunity by modulating immunoregulatory functions of salivary gland-derived mesenchymal stem cells32. Our study provides novel evidence linking GDF15 to pSS disease activity, though its precise mechanistic contributions require further elucidation. GDF15 is a multifunctional protein that can play a protective role in tissue damage and chronic inflammation by inhibiting excessive inflammatory responses and activating the immunosuppressive network33. Given that pSS pathogenesis involves chronic immune dysregulation leading to exocrine gland and systemic tissue inflammation, we postulate that GDF15 may stimulate immune responses either non-specifically via TGF-β superfamily receptors or specifically through the GFRAL/HPA/glucocorticoid pathway. These pathways collectively enhance the functional capacity of immunosuppressive cell populations—including myeloid-derived suppressor cells (MDSCs), regulatory T cells (Tregs), and M2 macrophages. Mechanistically, these activated cells not only suppress pathogenic autoimmune responses but also secrete anti-inflammatory cytokines (e.g., IL-10 and TGF-β), thereby attenuating chronic inflammatory injury characteristic of pSS.
While the results of the study are pertinent and timely for clinical practice, several limitations are noteworthy. A significant constraint of this research is the absence of future-oriented data. The long-term data to assess the variability of GDF15 levels over time in relation to changes in disease activity is insufficient, further research with paired specimens and multiple cohorts is required to validate these findings. Moreover, our examination of GDF15 was limited to the expression level; further investigation is essential to understand the mechanisms by which GDF15 influences the development and progression of pSS.
Conclusion
This study is the first to show that serum GDF15 level is elevated in pSS patients and significantly correlated with EGMs and disease activity. Serum GDF15 may serve as a useful biomarker for monitoring disease progression and guiding treatment in pSS.
Data availability statement
All data generated or analyzed in this study are available from the corresponding author upon reasonable request.
References
Fox, R. I. Sjogren’s syndrome. Lancet 366(9482), 321–331. https://doi.org/10.1016/S0140-6736(05)66990-5 (2005).
Brito-Zeron, P. et al. Sjogren syndrome. Nat Rev Dis Primers. 2, 16047. https://doi.org/10.1038/nrdp.2016.47 (2016).
Ter Borg, E. J. & Kelder, J. C. Development of new extra-glandular manifestations or associated auto-immune diseases after establishing the diagnosis of primary Sjogren’s syndrome : a long-term study of the antonius Nieuwegein sjogren (ANS) cohort. Rheumatol Int. 37(7), 1153–1158. https://doi.org/10.1007/s00296-017-3715-4 (2017).
Ramos-Casals, M. et al. Systemic involvement in primary Sjogren’s syndrome evaluated by the EULAR-SS disease activity index: analysis of 921 Spanish patients (GEAS-SS Registry). Rheumatology (Oxford) 53(2), 321–331. https://doi.org/10.1093/rheumatology/ket349 (2014).
Seror, R. et al. EULAR Sjogren’s syndrome disease activity index (ESSDAI): a user guide. RMD Open 1(1), e000022. https://doi.org/10.1136/rmdopen-2014-000022 (2015).
Ji, J. et al. Hsa_circ_0008301 as a potential biomarker of disease activity for primary Sjogren’s syndrome: Increased expression in peripheral blood of patients with primary Sjogren’s syndrome. Int Immunopharmacol. 112, 109231. https://doi.org/10.1016/j.intimp.2022.109231 (2022).
Yu, X. et al. Serum CCL28 as a biomarker for diagnosis and evaluation of Sjogren’s syndrome. Scand J Rheumatol. 52(2), 200–207. https://doi.org/10.1080/03009742.2021.2001930 (2023).
Hong, J. et al. CXCL9 may serve as a potential biomarker for primary Sjogren’s syndrome with extra-glandular manifestations. Arthritis Res Ther. 26(1), 26. https://doi.org/10.1186/s13075-023-03229-x (2024).
Caraba, A., Iurciuc, S., Nicolin, M. & Iurciuc, M. Endothelial dysfunction in primary Sjogren’s syndrome: Correlation with serum biomarkers of disease activity. Int J Mol Sci. https://doi.org/10.3390/ijms241813918 (2023).
Johann, K., Kleinert, M. & Klaus, S. The role of GDF15 as a myomitokine. Cells https://doi.org/10.3390/cells10112990 (2021).
Wollert, K. C., Kempf, T. & Wallentin, L. Growth differentiation factor 15 as a biomarker in cardiovascular disease. Clin Chem. 63(1), 140–151. https://doi.org/10.1373/clinchem.2016.255174 (2017).
Siddiqui, J. A. et al. Pathophysiological role of growth differentiation factor 15 (GDF15) in obesity, cancer, and cachexia. Cytokine Growth Factor Rev. 64, 71–83. https://doi.org/10.1016/j.cytogfr.2021.11.002 (2022).
Amstad, A. et al. Growth differentiation factor 15 is increased in stable MS. Neurol Neuroimmunol Neuroinflamm. https://doi.org/10.1212/NXI.0000000000000675 (2020).
Wu, Q. et al. Activity prediction modeling based on a combination of growth differentiation factor 15 and serum biomarker levels in dermatomyositis and polymyositis. Arch Med Res. 55(7), 103058. https://doi.org/10.1016/j.arcmed.2024.103058 (2024).
Xu, W. D., Huang, Q., Yang, C., Li, R. & Huang, A. F. GDF-15: A potential biomarker and therapeutic target in systemic lupus erythematosus. Front Immunol. 13, 926373. https://doi.org/10.3389/fimmu.2022.926373 (2022).
He, Y. W. & He, C. S. Association of growth and differentiation factor 15 in rheumatoid arthritis. J Inflamm Res. 15, 1173–1181. https://doi.org/10.2147/JIR.S350281 (2022).
De Paepe, B. Growth differentiation factor-15 as an emerging biomarker for identifying myositis. Expert Rev Clin Immunol. 18(2), 115–123. https://doi.org/10.1080/1744666X.2022.2021879 (2022).
De Paepe, B., Verhamme, F. & De Bleecker, J. L. The myokine GDF-15 is a potential biomarker for myositis and associates with the protein aggregates of sporadic inclusion body myositis. Cytokine 127, 154966. https://doi.org/10.1016/j.cyto.2019.154966 (2020).
Nyarady, B. B. et al. Growth and differentiation factor-15: A link between inflammaging and cardiovascular disease. Biomed Pharmacother. 174, 116475. https://doi.org/10.1016/j.biopha.2024.116475 (2024).
Chiariello, A. et al. Different roles of circulating and intramuscular GDF15 as markers of skeletal muscle health. Front Endocrinol (Lausanne). 15, 1404047. https://doi.org/10.3389/fendo.2024.1404047 (2024).
Shiboski, S. C. et al. American College of Rheumatology classification criteria for Sjogren’s syndrome: a data-driven, expert consensus approach in the Sjogren’s International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken). 64(4), 475–487. https://doi.org/10.1002/acr.21591 (2012).
Shiboski, C. H. et al. 2016 American College of Rheumatology/European league against rheumatism classification criteria for primary sjogren’s syndrome: A consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 69(1), 35–45. https://doi.org/10.1002/art.39859 (2017).
Conte, M. et al. Human aging and longevity are characterized by high levels of mitokines. J Gerontol A Biol Sci Med Sci. 74(5), 600–607. https://doi.org/10.1093/gerona/gly153 (2019).
Zhang, Y. et al. GDF15 is an epithelial-derived biomarker of idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol. 317(4), L510–L521. https://doi.org/10.1152/ajplung.00062.2019 (2019).
Wan, Y. & Fu, J. GDF15 as a key disease target and biomarker: Linking chronic lung diseases and ageing. Mol Cell Biochem. 479(3), 453–466. https://doi.org/10.1007/s11010-023-04743-x (2024).
Lu, S. et al. GDF15 ameliorates sepsis-induced lung injury via AMPK-mediated inhibition of glycolysis in alveolar macrophage. Respir Res. 25(1), 201. https://doi.org/10.1186/s12931-024-02824-z (2024).
Delrue, C., Speeckaert, R., Delanghe, J. R. & Speeckaert, M. M. Growth differentiation factor 15 (GDF-15) in kidney diseases. Adv Clin Chem. 114, 1–46. https://doi.org/10.1016/bs.acc.2023.02.003 (2023).
Ramos-Casals, M. et al. EULAR recommendations for the management of Sjogren’s syndrome with topical and systemic therapies. Ann Rheum Dis. 79(1), 3–18. https://doi.org/10.1136/annrheumdis-2019-216114 (2020).
Chen, W. & Ten Dijke, P. Immunoregulation by members of the TGFbeta superfamily. Nat Rev Immunol. 16(12), 723–740. https://doi.org/10.1038/nri.2016.112 (2016).
He, J. et al. Clinical significance of the expression levels of serum transforming growth factor-beta and CXC type chemokine ligand 13 in primary Sjogren’s syndrome patients. Clin Rheumatol. 42(12), 3283–3288. https://doi.org/10.1007/s10067-023-06783-6 (2023).
Maslinska, M., Paradowska-Gorycka, A., Manczak, M., Kostyra-Grabczak, K. & Kwiatkowska, B. The level of TGF-beta in sera of patients with primary Sjogren’s syndrome. Reumatologia 57(6), 309–314. https://doi.org/10.5114/reum.2019.91276 (2019).
Xu, J. et al. Effect of bone morphogenetic protein 6 on immunomodulatory functions of salivary gland-derived mesenchymal stem cells in sjogren’s syndrome. Stem Cells Dev. 27(22), 1540–1548. https://doi.org/10.1089/scd.2017.0161 (2018).
Salminen, A. GDF15/MIC-1: A stress-induced immunosuppressive factor which promotes the aging process. Biogerontology 26(1), 19. https://doi.org/10.1007/s10522-024-10164-0 (2024).
Acknowledgements
We thank Mr. Yuming Cheng and Miss Xialin Wang from Beckman Coulter Commercial Enterprise Co. Ltd. (Shanghai, China) for technical support in predictive model construction.
Author information
Authors and Affiliations
Contributions
WSY designed the experiments; FJF and PWC performed the experiments; FJF, WQ, ZYL and WW collected the serum samples; WSY analysed the data and wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Xiangya Hospital, Central South University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fu, J., Peng, W., Wu, Q. et al. Serum growth differentiation factor 15 associates with extra-glandular manifestations and disease activity of primary Sjögren’s syndrome. Sci Rep 15, 20007 (2025). https://doi.org/10.1038/s41598-025-03698-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03698-x
Keywords
This article is cited by
-
Growth differentiation factor 15: from stress response to clinical utility in chronic liver diseases
Journal of Gastroenterology (2025)