Abstract
IgA nephropathy (IgAN) is a common form of glomerulonephritis. According to the established multi-hit theory of IgAN pathogenesis, the final hit is the mesangial deposition of IgA1-containing immune complexes, leading to characteristic pathological features such as mesangial cell proliferation and expansion of extracellular matrix. We analyzed several public transcriptomic datasets, including microarray and bulk RNA-sequencing, to identify pathway alterations in IgAN patients and progressors. We also generated our own single-nucleus RNA-sequencing dataset from IgAN kidney biopsies with normal or reduced estimated glomerular filtration rate and integrated it with a publicly available healthy control dataset to comprehensively examine cell type-specific changes during IgAN progression. Pathways related to complement activation, focal adhesion, and collagen formation were significantly enhanced in IgAN compared to healthy controls. Our snRNA-seq data identified two mesenchymal stromal cell (MSC) clusters with higher scores in these pathways than other cell types, which were progressively perturbed as eGFR declined. We observed a potential transition from mesangial cells to myofibroblasts within MSCs, accompanied by increased expression of genes involved in complement activation, humoral immunity, collagen organization, and extracellular matrix assembly. This transition could be partially reversed through in silico knockdown of certain transcription factors, such as PRRX1.
Similar content being viewed by others
Introduction
IgA nephropathy is a clinically relevant form of glomerulonephritis worldwide, with rates of end-stage renal disease (ESRD) reaching 27% at 10 years1,2. This disease has placed a significant burden on healthcare resources and financial support systems.
Zheng et al. pioneered the use of single-cell RNA sequencing (scRNA-seq) in IgA nephropathy, providing a comprehensive view of the disease at single-cell resolution and emphasizing the important role of mesangial cells in the disease process3. However, the relatively small number of cells they captured may have limited the accurate identification of mesangial cells.
To overcome the challenge of limited and difficult-to-obtain glomerular cells, Chung et al. applied scRNA-seq to multiple mouse models of glomerular injury, collecting 5 448 high-quality glomerular cells, including podocytes, endothelial cells, mesangial cells, and smooth muscle cells4. They argued that precise genetic signatures for mesangial cells are important, as they may represent a specialized type of pericyte, and persistent mesangial reaction could contribute to the loss of kidney function in many diseases.
Kramann’s team has applied scRNA-seq to study the pathology of fibrosis in the kidney and heart. They stressed that dual-positive PDGFRα+/PDGFRβ + mesenchymal cells were the major contributors to the fibrosis process, with myofibroblasts, which differentiate from pericytes and various fibroblasts, playing a core role5. However, their work focused more on tubulointerstitial fibrosis rather than glomerulosclerosis.
Sanjay Jain et al. integrated more than 400,000 nuclei or cells from the kidney to provide a more accurate annotation reference for rare and previously undiscovered cell types, including mesangial cells, vascular smooth muscle cells, and myofibroblasts6.
Preserving kidney function is crucial for the management of IgA nephropathy, and the unique mechanisms underlying the progression of IgAN to chronic kidney disease need to be clarified. To investigate the progression, we collected and grouped our kidney biopsy samples according to eGFR. This study identifies the potential transformation of mesangial cells into myofibroblast-like cells during the progression of IgAN to chronic kidney disease, along with the transcription factors driving this transition, providing new insights for the prevention and management of IgAN progression to chronic kidney disease.
Result
Bulk RNA-seq and microarray reveal enhanced basement membrane regulation and complementary activation in IgA nephropathy compared to healthy individuals
We re-analyzed bulk RNA sequencing data from our previous study (GSE243078), which included samples from 5 IgAN patients and 4 healthy controls. Gene set enrichment analysis revealed significant activation of pathways such as miRNA targets in ECM and membrane receptors, basement membrane, and collagen trimer complexes in the kidneys of IgAN patients (Fig. 1A,B, Supplementary Data S1). These findings were validated using two independent microarray datasets (GSE37460 and GSE104948), confirming upregulation of these pathways in the glomeruli of IgAN patients. Additionally, we observed significant enrichment of type II interferon signaling, complement activation, and focal adhesion pathways in IgAN patients (Fig. 1C–F, Supplementary Data S1). In contrast, these pathways were not significantly activated in hypertensive nephropathy patients (GSE37460) but were enriched in patients with ANCA-associated vasculitis and lupus nephritis (GSE104948). Another bulk RNA-seq data set from six IgAN progressors and five non-progressors showed enriched pro-inflammatory and pro-fibrotic and intermediate filament cytoskeleton pathways in IgAN progressors (Supplementary Data S1).
Gene set enrichment analysis of IgA nephropathy using WikiPathway and gene ontology cellular component terms. Pathways significantly enriched in IgA nephropathy (IgAN) patients, compared to healthy controls, were analyzed using gene sets from WikiPathway (A, C, E) and the cellular component terms of Gene Ontology (B, D, F). (A, B) Enrichment analysis results from a bulk RNA-seq dataset (GSE243078). (C, D) Results from a microarray dataset (GSE37460). (E, F) Results from another microarray dataset (GSE104948).
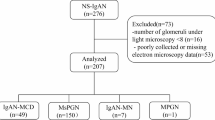
Transcriptomic alterations and pathway enrichment across eGFR groups and cell types in IgAN
We collected renal biopsy samples from 20 IgAN patients and pooled them into 3 normal eGFR and 3 low eGFR IgAN groups for snRNA-seq analysis. The patients’ clinical information is presented in Table 1. After integrating our IgAN snRNA-seq data with 5 healthy control snRNA-seq data set (GSE151302)7, we obtained a total of 61,515 cell nuclei and identified almost all the major cell types present in the kidney, including podocytes, parietal epithelial cells (PECs), and two clusters of mesenchymal stromal cells (Fig. 2A,B).
Two blurred boundary mesenchymal stromal cell subsets revealed by snRNA-seq analysis. (A) Uniform Manifold Approximation and Projection (UMAP) plot of all cells that passed quality control, with basic cell type annotations. (B) Dot plot showing canonical marker genes used for cell identity annotation. Darker dot colors indicated higher mean expression, and larger dot sizes represented a greater fraction of cells within clusters expressing the marker genes. (C) The plot showed the top 5 most specific regulons for the MSC1 cell identity, as well as the expression distribution of the FOXC2(+) regulon. Cells with FOXC2(+) regulon expression above the mean plus two standard deviations were highlighted in green. (D) The plot showed the top 5 most specific regulons for the MSC2 cell identity, as well as the expression distribution of the PRRX1(+) regulon. Cells with PRRX1(+) regulon expression above the mean plus two standard deviations were highlighted in green. (E, F) The dot plots show the top 5 enriched WikiPathway terms (E) and Gene Ontology (GO) cellular component terms (F), based on increasing q-value, from the enrichment analysis of the top 500 marker genes for MSC1 and MSC2, respectively, compared to all other cell types. Redder dot colors indicate lower q-values, and larger dot sizes represent more enriched marker genes in the term. (G) The plot presented the results of the perturbation analysis. The x-axis represented the Augur score 1, which indicated the perturbation when comparing the normal eGFR IgAN group to the normal control group. The y-axis represented the Augur score 2, which indicated the perturbation when comparing the low eGFR IgAN group to the normal control group. Cell types with an Augur score 2 higher than Augur score 1 are considered to have experienced continuous perturbation as IgAN occurred and progressed.
We conducted GSEA across all cell types in the different groups. Compared to the normal control group, the normal eGFR IgAN group showed significant enrichment of pathways related to oxidative phosphorylation and the electron transport chain (OXPHOS) across a broad range of cell types. In contrast, pathways associated with Type I interferon induction and signaling were significantly enriched only in B cells, dendritic cells, endothelial cells of the afferent and efferent arterioles, and endothelial cells of the glomerular capillaries. Complement-related pathways were notably enhanced only in connecting tubule cells, principal cells, intercalated cell type A, and intercalated cell type B. Inflammatory pathways were significantly increased in T cells, dendritic cells, principal cells, intercalated cell type B, and podocytes (Supplementary Data S2). When comparing the low eGFR IgAN group with the normal eGFR IgAN group, apoptosis-related pathways were significantly enriched in B cells, proximal tubular cells, and PECs. Additionally, complement and interferon-related pathways were significantly enriched across a broad range of cell types (Supplementary Data S2).
Identification of two mesenchymal stromal cell clusters
As shown in the UMAP visualization, the two MSC clusters were distributed in proximity, indicating they shared a more similar expression profile compared to other cell types. The canonical marker genes used to annotate them were displayed in dot plot (Fig. 2B). MSC1 and MSC2 both highly expressed genes like PDGFRB, ACTA2, COL1A1 and COL1A2.
Gene regulatory network (GRN) had found specific regulons for each cell types (Supplementary Data S3). Regulons FOXC2 and PRRX1 were the most specific for MSC1 and MSC2, with FOXC2 also being the third most specific regulon for MSC2. Both were highly expressed in both MSC clusters (Fig. 2C,D). Enrichment analysis of two MSC clusters was down. On the one hand, defined by WikiPathway enrichment, they both enriched in terms like Focal adhesion, miRNA targets in ECM and membrane receptors and Focal adhesion PI3K Akt mTOR signaling (Fig. 2E). On the other hand, defined by biological processes of Gene Ontology enrichment showed that MSC1 exhibited tendency towards muscle system, contraction ability and cell-matrix adhesion while MSC2 focused on the extracellular matrix organization, cell-matrix adhesion and collagen fibril organization (Fig. 2F). Then, we scored every cell using the gene sets we used in previous analysis; the results showed that two MSC clusters exhibited significantly higher scores in complement activation, focal adhesion, miRNA targets in ECM and membrane receptors, basement membrane, cell substrate junction and collagen trimer pathway than other cell types (Supplementary Table S1).
Augur’s perturbation analysis showed that although the perturbation of podocytes and endothelial cells was intense when IgAN occurred, the reactions of MSC1 and MSC2 to IgAN were continuously enhanced as the eGFR declined (Fig. 2G). This phenomenon was also observed in Chung et al.‘s single cell experiments.
We used our snRNA-seq data to estimate the cell proportions in two bulk RNA-seq data. Although the average estimated proportion of MSC2 of GSE243078 was higher in IgAN patients than healthy donors, it was not significantly (Supplementary Fig. S1). These could be resulted from the small number of samples, or the variance of glomerulus captured when doing kidney biopsy. In GSE210098, the estimated proportion of MSC2 in progressors of IgAN was significantly higher than non-progressors which indicated the important role of MSC whether in IgAN occurrence or in progression.
Altogether, the two major clusters of mesenchymal stromal cells shared close cell identities with only subtle differences. Their perturbations were consistently enhanced as IgAN progressed. Furthermore, the estimated proportions of MSC2 were increased when IgAN occurred or in the progressors of IgAN. Therefore, we believe that the mesenchymal stromal cells play essential roles in the development of IgAN.
Re-clustering and annotation of MSC subpopulations reveal distinct functional signatures
We pulled out cells from MSC1 and MSC2, and re-clustered and annotated them. The original annotation of MSC1 and MSC2 were overlapped in the new UMAP (Fig. 3A), and according to the marker genes provided by Sanjay Jain, we have annotated Mesangial cells (GATA3, PDGFRB, PIEZO2 and POSTN)4,6,8,9 with a total of 234 cells, smooth muscle cells (RGS6, RGS5, MCAM, MYH11 and ACTA2)8 with a total of 669 cells, and myofibroblasts (COL1A1, COL1A2, LAMA2 and ACTA2)8,8 (Fig. 3B,C) with a total of 438 cells.
Refined annotation of mesenchymal stromal cell subsets. (A) The UMAP plot showed the original annotation of the MSC1 and MSC2 subsets on the newly generated UMAP after re-clustering the cells from these two populations. (B) The UMAP plot displayed the more refined and precise cell type annotations on the same embedding following the re-clustering and re-annotation process. (C) The violin plot presented the expression of canonical marker genes used for precise mesenchymal stromal cell identity annotation. (D) The plot showed the top 5 highly expressed regulons in Mes (mesangial cells), Mes-Fib, SMC1 (smooth muscle cells), and MyoFib2 (myofibroblasts), with darker colors indicating higher mean expression levels. (E) The violin plot presents the expression levels of the PRRX1(+) regulon across the mesenchymal stromal cell subsets, revealing significantly higher expression in the MyoFib2 population compared to all other cell types.
The marker genes of Mes were enriched in axonogenesis, kidney development, and positive regulation of monoatomic ion transport. The marker genes of SMC1 were enriched in muscle system, regulation of blood circulation, and calcium ion transmembrane transport. The maker genes of MyoFib2 were enriched in extracellular matrix organization, ossification, and regulation of macrophage differentiation (Supplementary Data S4).
Pathways scoring analysis showed that, mesangial cell (Mes) exhibited high scores in cell differentiation involved in kidney development; vascular smooth muscle cells 1 (SMC1) exhibited high scores in smooth muscle contraction and myofibroblasts 2 (MyoFib2) exhibited high scores in collagen fibril organization and extracellular matrix assembly; and MyoFib2 also exhibited high scores in pathways like complement activation, focal adhesion, miRNA targets in ECM, membrane receptors, basement membrane, cell substrate junction and collagen trimer (Supplementary Table S2).
The regulon PRRX1 was significantly more highly expressed in MyoFib2 than in all other cell types, and its expression levels progressively increased from Mes to MyoFib2, through the intermediate cell states like Mes-Fib, Fib1 and Fib2 (Fig. 3D,E). PRRX1 was also the most specific regulon for MSC2, the larger cell-type category from which MyoFib2 originates. A team led by Kim in South Korea has proven the critical role of PRRX1 in defining a specific subpopulation of cancer-associated fibroblasts (CAFs) with a myofibroblast-like phenotype, which plays a crucial role in driving tumor development, metastasis, and cancer relapse10.
The potential transaction from mesangial cells to myofibroblasts
The percentage of mesangial cells (Mes) in the mesenchymal stromal cell population gradually decreased as the eGFR declined, while the percentage of Mes-Fib and myofibroblasts (MyoFib2) increased (Fig. 4A). We then applied the VIA algorithm to speculate on the potential cellular identity transitions and found that mesangial cells had the potential to transition into myofibroblasts (Fig. 4B).
Mesangial-to-myofibroblast transition during IgAN progression. (A) The bar plot presented the percentage of each mesenchymal stromal cell subset in the control group, normal eGFR IgAN group, and low eGFR IgAN group. The proportion of Mes (mesangial cells) decreased rapidly as IgAN occurred, while the percentages of Mes-Fib and MyoFib2 (myofibroblasts) increased stepwise as the disease progressed. (B) The stream plot showed the potential transition from Mes to MyoFib2 through Mes-Fib and Fib2 as intermediate states, as inferred by the VIA algorithm. (C) A new UMAP embedding was generated after pooling Mes, Mes-Fib, Fib2, and MyoFib2 cells. (D) Pseudotime analysis conducted on the new UMAP using Monocle3 revealed a trajectory from mesangial cells to myofibroblasts, with the pseudotime value increasing from dark to yellow. (E, F) In silico knockout of the transcription factor PRRX1, using information from snATAC-seq data (E) or CellOracle (F), could potentially reverse the mesangial-to-myofibroblast transition identified in the previous analyses. The deeper the red shading, the stronger the predicted reversal effect on the trajectory. Conversely, the deeper the green shading, the more the perturbation is predicted to promote the trajectory.
The pseudotime analysis using Monocle 3 focused on mesangial cells (Mes), mesangial-fibroblast transitory state (Mes-Fib), fibroblast (Fib2), and myofibroblast (MyoFib2) revealed a trajectory, with Mes at the start, Mes-Fib and Fib2 in the middle, and MyoFib2 at the terminal position (Fig. 4C,D). Along this trajectory, the canonical marker genes and regulons which highly expressed in mesangial cells gradually and smoothly decreased (Supplementary Fig. S2), while those of myofibroblasts increased. This was accompanied by the progressive upregulation of pathways related to complement activation, focal adhesion PI3K-AKT-mTOR signaling, basement membrane, collagen, and immune response. Importantly, immunohistochemistry confirmed the downregulation of mesangial cell markers GATA3 and PIEZO2, alongside the upregulation of myofibroblast markers PRRX1, COL1A1, and COL4A4, although the overall trend for PRRX1 was not as pronounced. These findings support the hypothesis of a mesangial-to-myofibroblast transition occurring during the progression of IgA nephropathy (IgAN) (Supplementary Fig. S3).
Using CellOracle, we simulated transcription factor knockouts and found that the mesangial to myofibroblast-like transition was largely reversed when PRRX1 was knocked out (Fig. 4E,F), in addition to knockouts of ESR2, BHLBE40, and JUN. The detailed perturbation scores for all transcription factor knockouts are provided in Supplementary Data S5, where higher scores indicate a more severe blockade of the differentiation process.
Parietal epithelial cell’s pro-fibrotic potential was enhanced during the IgA nephropathy progression
We re-clustered and dimensionally reduced the PECs without removing batch effects and observed that the distribution of PECs in the new UMAP was hierarchical to the estimated glomerular filtration rate (eGFR). The PECs from healthy donors were mainly distributed on the left, the low eGFR group on the right, and the normal eGFR IgAN group bridged them, which we annotated numerically (Fig. 5A,B). Some genes playing important roles in the complement system and fibrosis were also expressed in a hierarchical manner (Fig. 5C).
Pseudotime analysis of parietal epithelial cells. (A) A new UMAP embedding was generated after pooling parietal epithelial cells (PECs) without batch effect correction. The PEC subsets were numerically annotated. (B) The distribution of PECs from the control, normal eGFR IgAN, and low eGFR IgAN groups on the UMAP embedding revealed a hierarchical pattern, with control PECs primarily on the left side, low eGFR IgAN PECs on the right, and normal eGFR IgAN PECs bridging the two. (C) The expression of genes such as SPP1, ITGB3, and COL1A1 also displayed a hierarchical pattern across the PEC subsets, with higher expression in PECs from the low eGFR IgAN group compared to the other groups. (D) Pseudotime analysis performed on the PEC UMAP embedding using Monocle3 revealed a trajectory from PEC1 to PEC6, with the pseudotime value increasing from dark to yellow. (E, F) In silico knockout of the transcription factor MECOM, using information from snATAC-seq data (E) or CellOracle (F), has the potential to reverse the PEC1-to-PEC6 transition identified in the previous analyses.
We then applied trajectory analysis to the PECs, selecting PEC1 as the starting point. PEC6 was positioned at the end of the trajectory (Fig. 5D). Complement activation, type II interferon signaling, miRNA targets in ECM and membrane receptors, immunoglobulin complex, collagen trimer and fibrillar collagen trimer were all enhanced smoothly along this trajectory (Supplementary Fig. S2). Simulated knockouts using this trajectory showed that the depletion of MECOM, ESR2, and EBF1 could reverse the transition (Fig. 5E,F). The knockouts of ESR2, EBF1, and MECOM would reverse the fibrotic transition in PECs as well as the transition of mesangial cells to a myofibroblast-like state, suggesting their potential as therapeutic targets in glomerulosclerosis (Supplementary Data S6).
Pathologic cell-to-cell interactions between myofibroblasts and parietal epithelial cells were enhanced as the IgA nephropathy progress
The cell-cell interaction analysis by CellChat revealed a stepwise enhancement in the inferred interaction strength as IgAN progressed (Supplementary Fig. S4). The pathways involving Collagen, Laminin, MHC-I, SPP1, and Complement were progressively upregulated when comparing normal eGFR IgAN patients to healthy controls, and low eGFR IgAN patients to normal eGFR IgAN patients, mirroring the fibrotic and inflammatory processes.
As IgAN progressed, the MyoFib2 subtype emerged as the dominant signal sender and receiver (Fig. 6A, B, F and G). During both the onset and progression of IgAN, the enhanced signaling from the MyoFib2 subpopulation was primarily enriched in the Collagen, Laminin, and SPP1 pathways (Supplementary Fig. S4), which may significantly impact the development of fibrosis and the abnormal immune response. In normal eGFR IgAN patients, the outgoing signals from MyoFib2 were enhanced toward almost all cell types, particularly stronger within the MyoFib2 subpopulation itself, as well as mesangial cells, other MSCs, and endothelial cells (Fig. 6D). CellphoneDB analysis further showed that MyoFib2 sent more interactions to other MSCs, PECs, and endothelial cells, while receiving more signals from mesangial cells, endothelial cells, and other MSCs (Fig. 6G), supporting the notion that this MyoFib2 subtype is predominantly localized within the glomerulus. Furthermore, the CellChat analysis of the TGF-β signaling pathway revealed a shift during IgAN progression. Initially, the TGF-β signaling was mainly between endothelial cells, PECs, and immune cells. However, as the disease progressed, the TGF-β signaling became predominantly between myofibroblasts and endothelial cells, further supporting the abnormal fibrotic ability of myofibroblasts observed in our cell type annotations (Supplementary Fig. S5).
Pathological cell-cell interactions in IgAN progression. (A–C) These scatter plots illustrated the dominant sender (source) and receiver (target) cell populations in the (A) control, (B) normal eGFR IgAN, and (C) low eGFR IgAN groups, respectively. The x-axis represented the total outgoing communication probability, while the y-axis indicated the total incoming communication probability associated with each cell type. The dot size was proportional to the number of inferred communication links (both outgoing and incoming) for each cell population. The dot colors distinguished the different cell types. (D–E) These heatmaps provided a detailed view of the differential interaction strengths. The colored bar plots on the top represented the sum of values in each column (incoming signaling), while the bar plots at right side showed the sum of values in each row (outgoing signaling). The color scale indicated changes in signaling strength: red represented increased signaling in (D) the normal eGFR IgAN group compared to the control group, and (E) the low eGFR IgAN group compared to the normal eGFR IgAN group. Blue indicated decreased signaling. The rows and columns corresponded to the sender (source) and receiver (target) cell types, respectively. (F–H) These heatmaps displayed the total number of interactions inferred by CellphoneDB in the (F) control, (G) normal eGFR IgAN, and (H) low eGFR IgAN groups. The rows represented the sender (source) cell types, while the columns denoted the receiver (target) cell types. The color scale indicated the number of interactions, with red representing a higher number and blue indicating fewer interactions. Collectively, these analyses revealed the dynamic changes in the intercellular communication landscape during the progression of IgAN, as captured by the CellChat and CellphoneDB computational approaches.
Moreover, as eGFR declined in advanced IgAN, PECs showed increased incoming and outgoing signals enriched in the Collagen, Laminin, and SPP1 pathways (Supplementary Fig. S4), while the signaling from MyoFib2 to other cell types was further enhanced, primarily between MyoFib2 and PECs (Fig. 6C, E). CellphoneDB results also demonstrated that in low eGFR IgAN patients, the interactions from MyoFib2 were predominantly directed toward MyoFib2 itself, PECs, and other MSCs, while the incoming signals to MyoFib2 were mainly from MyoFib2 itself, mesangial cells, other MSCs, and PECs (Fig. 6H). Collectively, these findings suggest that the cell-cell interactions between myofibroblasts and injured PECs drive the fibrotic process in progressed IgAN.
A deeper examination of the ligand-receptor interactions within the COLLAGEN pathway revealed that the COL4A4 - (ITGAV + ITGB8) interaction from MyoFib2 to PECs, podocytes, and proximal tubular cells was progressively reinforced as IgAN occurred and progressed. Additionally, the COL4A4 - (ITGA1 + ITGB1) interaction from MyoFib2 to itself was also enhanced during IgAN progression (Supplementary Fig. S6). Furthermore, signals from MyoFib2 to dendritic cells, B cells, and T cells, such as COL4A4 - CD44, COL1A2 - (ITGA2 + ITGB1), and LAMA2 - (ITGA2 + ITGB1), were increased as IgAN developed and worsened. This suggests that reactive myofibroblasts may be able to recruit immune cells into the injured kidney and induce further immune processes.
Discussion
Our comprehensive analysis of microarray, bulk RNA-seq, and single-nucleus RNA-seq data underscores the critical involvement of pathways such as focal adhesion, miRNA targets in ECM and membrane receptors, basement membrane, collagen trimer, and complement activation in IgA nephropathy (IgAN). In the snRNA-seq analysis, we observed that the normal eGFR IgAN group exhibited significant enrichment in pathways related to oxidative phosphorylation and the electron transport chain (OXPHOS system) across various cell types, compared to the normal control group. This enhancement may reflect a protective response to cellular damage. In contrast, the low eGFR IgAN group demonstrated significant upregulation of the complement system and interferon signaling pathways in multiple cell types, suggesting that persistent immune activation.
, including the involvement of the complement and interferon systems, drives kidney damage and progression of dysfunction. Notably, mesenchymal stromal cells showed higher pathway activity in focal adhesion, collagen trimer, and complement activation compared to other cell types. Additionally, mesenchymal stromal cells exhibited progressive perturbations from the onset of IgAN, correlating with disease severity, which highlights their potential as therapeutic targets.
Within the mesenchymal stromal cell compartment, we made precise cell type annotations, including mesangial cells, smooth muscle cells, fibroblasts, and myofibroblasts. We discovered a potential transition from mesangial cells to myofibroblasts through, driven by transcriptional regulators like PRRX1. This transition was accompanied by the gradual enhancement of pathways like complement activation, focal adhesion PI3K AKT mTOR signaling, and miRNA targets in ECM and membrane receptors. The cell-to-cell interactions between myofibroblasts and other cell types, particularly PECs, were gradually enhanced as IgAN progressed, primarily through the Collagen, Laminin, and SPP1 pathways. As the disease advanced, myofibroblasts may have recruited immune cells to promote local immune processes through ligand-receptor pairs such as COL4A4-CD44. The prominent interaction between myofibroblasts and PECs may have driven the glomerulosclerosis process. CellOracle’s in silico analysis predicted that the fibrotic trajectory could be reversed by knocking down specific transcription factors, including PRRX1, ESR2, KLF3, and EBF1. However, these predictions require careful interpretation, as the role of these factors and their downstream targets may be either causative or compensatory in the pro-fibrotic and pro-inflammatory processes. PRRX1 is a well-established master regulator of the myofibroblastic program10,11, controlling extracellular matrix remodeling and wound healing-related factor secretion. It’s essential role in TGF-β-mediated myofibroblast transformation aligns with our finding that its predicted knockout could reverse the mesangial-to-myofibroblast-like transition in IgAN. The role of estrogen receptors in renal fibrosis is complex12,13,14,15. While studies have shown protective effects of tamoxifen through ERα-dependent TGF-β1/Smad signaling16,17, ERβ’s role remains controversial. It has become clear that the classic genomic mechanisms only partially explain the complexity of estrogen signaling. Our in silico knockout experiments primarily focused on the direct genomic signaling of the estrogen receptors. Therefore, whether the knockout of ESR2 (encoding ERβ) could effectively ameliorate the mesangial-to-myofibroblast transition remains to be validated through further laboratory experiments. Recent studies have demonstrated KLF3’s involvement in diabetic kidney disease through the KLF3/STAT3 pathway18, supporting our computational prediction of its role in the mesangial-to-myofibroblast transition. Similarly, EBF1’s known function in regulating glomerular maturation and NFAT signaling in the stromal-progenitor lineage suggests its potential importance in mesangial cell function19,20, though its role in mature mesangial cells requires further investigation. Additionally, our analysis revealed that the pro-fibrotic and pro-immune transformation of parietal epithelial cells in IgAN progression could potentially be reversed by downregulating MECOM, ESR1, ESR2, and WT1. This study has several limitations: First, our cell-cell interaction analysis, trajectory analysis, and transcription factor knockout simulations lack robust experimental validation and support. Second, the sample size for our sequencing is still relatively small, and future studies will require expanding the sample size to obtain more reliable data. Then, it remains unclear whether the findings are specific to IgA nephropathy or if similar results could be observed in other forms of glomerulonephritis or chronic kidney disease caused by non-IgA nephropathy factors. Further exploration in future work is needed to address this question. Lastly, our study primarily focused on mesenchymal stromal cells and parietal epithelial cells, which may have overlooked the potential contributions of other cell types to disease progression. Our study identifies several promising directions for future research and clinical applications. By providing insights into the molecular mechanisms underlying IgA nephropathy and renal fibrosis, our bioinformatics analysis highlights the potential regulatory roles of PRRX1, ESR2, and KLF3 in mesangial cells. From a translational perspective, our findings suggest potential therapeutic strategies targeting mesangial cell function. Selective inhibition, downregulation, or knockout of PRRX1, ESR2, and KLF3 may represent novel approaches for treating IgA nephropathy and chronic kidney disease. Furthermore, evaluating PRRX1 and ESR2 expression in mesangial cells from renal biopsy specimens could serve as a valuable biomarker-based approach for prognosis assessment, risk stratification, and personalized treatment in IgA nephropathy. Further experimental validation and clinical studies are required to assess the therapeutic feasibility and translational potential of these findings. In conclusion, this study identified a potential transition from mesangial cells to myofibroblasts, regulated by PRRX1 and other transcription factors, as a crucial event in the pathogenesis of glomerulosclerosis in IgAN.
Methods
Sample collection
We recruited patients aged 16–70 years who provided informed consent for both renal biopsy and tissue donation. Individuals with diabetes mellitus or prior corticosteroid/immunosuppressant use were excluded. Renal biopsy samples were collected under strict time constraints, with excision-to-snap-freezing duration kept within 2 min. Samples were stored in liquid nitrogen for no more than 20 min before transfer to a − 80 °C freezer, pending pathological evaluation. Following pathological review, IgA nephropathy cases with alternative primary glomerulonephritis diagnoses or significant tubulointerstitial injury were excluded. Within three months of storage, samples were stratified by estimated glomerular filtration rate and sent to CapitalBio Corporation (Beijing, China) for processing, including tissue dissociation, nuclear isolation, and sequencing on the 10x Genomics platform.
Nuclear isolation and quality control
Nuclear suspensions were prepared using the Nuclei Isolation Kit (CapitalBio, XS0100101) following the manufacturer’s protocol. Briefly, frozen tissues were mechanically dissociated in ice-cold Lysis Buffer supplemented with 1 mM DTT and 1 U/µL RNase inhibitor (Thermo Fisher Scientific) using a Dounce homogenizer. After 5-min incubation on ice, homogenates were filtered through a 40-µm nylon mesh, centrifuged at 500 ×g for 5 min at 4 °C, and resuspended in Lysis Buffer and RB Buffer. Intact nuclei were isolated via density gradient centrifugation, washed, and quantified using the CountStar Rigel S2 automated cell counter. Quality control criteria included nuclear viability (≤ 10%), aggregation rate (≤ 15%), and purity (≥ 50%). Samples passing QC were pooled based on eGFR to ensure sufficient nuclei for sequencing.
snRNA-seq library construction and sequencing
Single-nucleus suspensions were processed using the 10x Genomics Chromium Controller, where individual nuclei were encapsulated in Gel Bead-In-EMulsions (GEMs) containing 10x Barcodes and reagents for reverse transcription. Following cDNA synthesis, emulsions were disrupted, and cDNA was amplified by PCR. Fragment size and yield were assessed before purification. cDNA quality was verified using a Qubit 3.0 Fluorometer and Agilent 2100 Bioanalyzer, ensuring concentrations ≥ 1 ng/µL and fragment sizes within 200–9000 bp (peak: 1000–2000 bp). Sequencing libraries were constructed by enzymatically fragmenting cDNA into 200–300 bp segments, incorporating sequencing adapters through PCR. Purified libraries were pooled and sequenced on the NovaSeq 6000 platform (Illumina) using paired-end 150 bp reads (PE150) with a target depth of 50,000 reads per nucleus and 150 GB per sample.
Basic data processing
Base calling and raw data generation (FASTQ format) were performed using Illumina’s onboard software. Quality control was conducted using FastQC (v0.11.2, available at https://www.bioinformatics.babraham.ac.uk/projects/download.html#fastqc). Reads were aligned to the GRCh38 human reference genome (GRCh38-2020-A) using CellRanger (v7.0.0, available at https://www.10xgenomics.com/support/software/cell-ranger/downloads/previous-versions/) to generate filtered feature-barcode matrices for downstream analysis.
Micro array
We downloaded the microarray datasets GSE3746021, GSE9933922 and GSE10494823 from the GEO database; as GSE99339 is lack of normal control sample for comparisons, it was discarded, and the rest were imported into RStudio using the Affy package (v1.80.0, available at https://bioconductor.org/packages/affy/)24. We merged the expression matrices and reduced batch effects using the SVA package (v3.50.0, available at https://bioconductor.org/packages/sva/)25, and evaluated the quality control results with the arrayQualityMetrics (v3.62.0, available at https://bioconductor.org/packages/arrayQualityMetrics/) R package (Supplementary Data S7). Next, we performed differential gene expression analysis using the Limma package (v3.58.1, available at https://bioinf.wehi.edu.au/limma/)26.
Bulk RNA-seq
We used the two bulk RNA-sequencing datasets GSE21009827, which had been previously uploaded to the GEO database, and GSE24307828, which was downloaded from the GEO database. We analyzed these datasets separately, performing differential gene expression analysis using the DESeq2 package (v1.42.1, available at https://github.com/thelovelab/DESeq2/)29.
Basic single nucleus RNA-seq workflow
We processed the single-nucleus RNA-seq data using the Seurat package (v5.1.0)30. We retained cells with read counts between 450 and 8 000, and gene counts between 400 and 5 000. We then removed low-quality clusters and filtered the data to keep genes and reads within the 5th to 95th percentiles of the overall distribution, while also excluding cells with mitochondrial gene expression higher than 90% of the total. Next, we merged the Seurat objects and used the harmony package (v1.2.0, available at https://github.com/immunogenomics/harmony/)31 to reduce batch effects. For dimensional reduction, we employed the uniform manifold approximation and projection (UMAP) method. Finally, we annotated cell types based on canonical marker genes. Differential gene expression analysis was performed using the FindMarkers function in Seurat, with the “logfc.threshold” parameter set to 0 and all other parameters set to their default values.When combined with the bulk RNA-seq data, we used the MuSiC package (v1.0.0, available at https://github.com/xuranw/MuSiC/)32 to estimate the cell type composition in the bulk RNA-seq data.
Enrichment analysis
We performed enrichment analysis using the ClusterProfiler package (v4.12.0, available at https://yulab-smu.top/contribution-knowledge-mining/)33. For the significantly differentially expressed genes, we used the enrichWP and enrichGO functions. For the gene set enrichment analysis (GSEA), we ordered the genes by their average log fold change values in descending order as input. We then conducted the GSEA analysis using the WikiPathway (v2023.2.Hs.symbols) and Gene Ontology cellular component gene sets (v2023.2.Hs.symbols) gene set collections provided by the Molecular Signatures Database (MSigDB)34,35 as references, separately.
Gene regulatory network analysis
We first applied the pySCENIC (Single-cell rEgulatory Network Inference, v0.12.1, available at https://scenic.aertslab.org/) package36 to infer the gene regulatory network (GRN) from our single-nucleus RNA-seq data. To enhance the scalability and robustness of SCENIC, we modified its implementation by creating metacells from the single-nucleus RNA-seq data37. To quantify cell-type specificity, we adopted the regulon specificity score (RSS) developed by Shengbao S., which is an entropy-based approach using Jensen-Shannon Divergence (JSD)38. For in silico gene perturbation with GRNs, we followed the detailed tutorial provided by the morris lab. We utilized the CellOracle package (v0.18.0, available at https://morris-lab.github.io/CellOracle.documentation/)39, using transcriptional information from two sources: the hg38 transcription information provided by CellOracle team and the snATAC-seq data from GSE18594840.
Perturbation analysis
We utilized the Augur package (v1.0.3, available at https://github.com/neurorestore/Augur/)41 to estimate the perturbation of cell types between the control group and the normal eGFR IgAN group, as well as between the control group and the low eGFR IgAN group. By comparing the perturbation scores across these two scenarios, we aimed to identify the cell types that were continuously perturbed as IgAN progressed and kidney function declined.
Pathway scoring
To score pathways in each cell, we utilized the AUCell package (v1.24.0, available at http://scenic.aertslab.org/)36 and the WikiPathway (v2023.2.Hs.symbols), Gene Ontology biology process gene sets (v2023.2.Hs.symbols) and Gene Ontology cellular component gene sets (v2023.2.Hs.symbols) gene set collections from MSigDB. By combining this pathway scoring approach with the previous GSEA analysis, we aimed to identify the cell types that play a critical role in the occurrence and progression of IgAN, using consistent reference gene set collections.
Trajectory analysis
We focused our trajectory analysis on two key cell populations: mesenchymal stromal cells (MSCs) and parietal epithelial cells (PECs). For the MSC trajectory, we first applied the vector field integration approach (VIA) packaged42 in the Omicverse tool (v1.5.9, available at https://starlitnightly.github.io/omicverse/Installation_guild/)43 to ascertain the potential cell type transitions within the MSC compartment. This method can automatically identify the root cells, which discovered the potential transition from mesangial cells to myofibroblasts. For mesangial-to-myofibroblast pseudotime analysis and PEC pseudotime analysis, Monocle3 package (v1.4.11, available at https://cole-trapnell-lab.github.io/monocle3/docs/installation/)44,45 was employed. To speculate on in silico gene perturbations that could potentially reverse the observed trajectories, we utilized the CellOracle package (v0.18.0, available at https://morris-lab.github.io/CellOracle.documentation/)39.
Cell to cell interaction analysis
To investigate cell-cell interactions in the kidney, we utilized two complementary packages: CellChat (v2.1.2, available at https://github.com/jinworks/CellChat/)46 and CellphoneDB (v5.0.0, available at https://github.com/ventolab/CellphoneDB/)47. For the CellChat analysis, we first used the smoothData function to project the gene expression values onto an experimentally validated protein-protein interaction network. We then employed the “triMean” method to compute the average gene expression per cell group. In the CellphoneDB analysis, we adopted the version 5.0.0 database for the calculations.
Immunohistochemistry
Renal tissue samples were fixed in 4% paraformaldehyde, paraffin-embedded, and sectioned. The paraffin sections were deparaffinized and subjected to antigen retrieval using citrate buffer (G1201, Servicebio). Endogenous peroxidase activity was blocked with 3% H2O2, and non-specific binding sites were blocked with 3% bovine serum albumin (GC305010, Servicebio). The sections were then incubated with primary antibodies overnight at 4 °C. The primary antibodies used were rabbit anti-PROX1 (14963, Cell Signaling Technology), rabbit anti-Collagen I (ab138492, Abcam), rabbit anti-Collagen IV (ab6586, Abcam), rabbit anti-GATA3 (ab199428, Abcam), and rabbit anti-PIEZO2 (NBP1-78624, Novus Biologicals). After washing, the sections were incubated with HRP-conjugated goat anti-rabbit IgG secondary antibody (GB23303, Servicebio) at room temperature for 50 min. Immunoreactivity was visualized using DAB (G1212, Servicebio), and the sections were examined and scanned under a microscope.
Data availability
The snRNA-seq datasets generated and analyzed during the current study are available in the Gene Expression Omnibus repository, GSE286911. The public datasets used an analyzed during this study are also available from the GEO repository under the following accession numbers: GSE37460, GSE99339, GSE104948, GSE210098 and GSE243078.
Abbreviations
- IgAN:
-
IgA nephropathy
- eGFR:
-
estimated glomerular filtration rate
- snRNA-seq:
-
Single nucleus ribonucleic acid sequencing
- scRNA-seq:
-
Single cell ribonucleic acid sequencing
- MSCs:
-
Mesenchymal stromal cells
- UMAP:
-
Uniform manifold approximation and projection
- GRN:
-
Gene regulatory network
- PECs:
-
Parietal epithelial cells
- TFs:
-
Transcription factors
- ECM:
-
Extracellular matrix
- CAFs:
-
Cancer-associated fibroblasts
References
Barbour, S. J. et al. The MEST score provides earlier risk prediction in LgA nephropathy. Kidney Int. 89, 167–175 (2016).
Rodrigues, J. C., Haas, M. & Reich, H. N. IgA nephropathy. Clin. J. Am. Soc. Nephrol. 12, 677–686 (2017).
Zheng, Y. et al. Single-cell transcriptomics reveal immune mechanisms of the onset and progression of IgA nephropathy. Cell. Rep. 33, 108525 (2020).
Chung, J. J. et al. Single-Cell transcriptome profiling of the kidney glomerulus identifies key cell types and reactions to injury. J. Am. Soc. Nephrol. 31, 2341–2354 (2020).
Kuppe, C. et al. Decoding myofibroblast origins in human kidney fibrosis. Nature 589, 281–286 (2021).
Lake, B. B. et al. An atlas of healthy and injured cell states and niches in the human kidney. Nature 619, 585–594 (2023).
Muto, Y. et al. Single cell transcriptional and chromatin accessibility profiling redefine cellular heterogeneity in the adult human kidney. Nat. Commun. 12, 2190 (2021).
Abedini, A. et al. Single-cell multi-omic and spatial profiling of human kidneys implicates the fibrotic microenvironment in kidney disease progression. Nat. Genet. 56, 1712–1724 (2024).
Avraham, S., Korin, B., Chung, J. J., Oxburgh, L. & Shaw, A. S. The mesangial cell—The glomerular stromal cell. Nat. Rev. Nephrol. 17, 855–864 (2021).
Lee, K. W. et al. PRRX1 is a master transcription factor of stromal fibroblasts for myofibroblastic lineage progression. Nat. Commun. 13, 2793 (2022).
Jiang, W. D. et al. PRRX1 + MSCs enhance mandibular regeneration during distraction osteogenesis. J. Dent. Res. 102, 1058–1068 (2023).
Libby, A. E., Jones, B., Lopez-Santiago, I., Rowland, E., & Levi, M. Nuclear receptors in the kidney during health and disease. Mol. Aspects Med. 78, 100935 (2021).
Gui, Y. et al. Calponin 2 harnesses metabolic reprogramming to determine kidney fibrosis. Mol. Metab. 71, 101712 (2023).
Gui, Y. et al. Calponin 2 regulates ketogenesis to mitigate acute kidney injury. JCI Insight 8, e170521 (2023).
Ito, I. et al. Estrogen inhibits transforming growth factor beta signaling by promoting Smad2/3 degradation. J. Biol. Chem. 285, 14747–14755 (2010).
Kim, D. et al. Tamoxifen ameliorates renal tubulointerstitial fibrosis by modulation of estrogen receptor α-mediated transforming growth factor-β1/Smad signaling pathway. Nephrol. Dial Transpl. 29, 2043–2053 (2014).
Tingskov, S. J. et al. Tamoxifen attenuates renal fibrosis in human kidney slices and rats subjected to unilateral ureteral obstruction. Biomed. Pharmacother. 133, 111003 (2021).
Li, Q. et al. Small extracellular vesicles-shuttled miR-23a-3p from mesenchymal stem cells alleviate renal fibrosis and inflammation by inhibiting KLF3/STAT3 axis in diabetic kidney disease. Int. Immunopharmacol. 139, 112667 (2024).
Nelson, T., Velazquez, H., Troiano, N., Fretz, J. A. & Early, B. Cell factor 1 (EBF1) regulates glomerular development by controlling mesangial maturation and consequently COX-2 expression. J. Am. Soc. Nephrol. 30, 1559–1572 (2019).
Fretz, J. A. et al. Early B-cell factor 1 is an essential transcription factor for postnatal glomerular maturation. Kidney Int. 85, 1091–1102 (2014).
Berthier, C. C. et al. Cross-species transcriptional network analysis defines shared inflammatory responses in murine and human lupus nephritis. J. Immunol. 189, 988–1001 (2012).
Shved, N. et al. Transcriptome-based network analysis reveals renal cell type-specific dysregulation of hypoxia-associated transcripts. Sci. Rep. 7, 8576 (2017).
Grayson, P. C. et al. Metabolic pathways and immunometabolism in rare kidney diseases. Ann. Rheum. Dis. 77, 1226–1233 (2018).
Gautier, L., Cope, L., Bolstad, B. M. & Irizarry, R. A. Affy-analysis of affymetrix genechip data at the probe level. Bioinformatics 20, 307–315 (2004).
Leek, J. T., Johnson, W. E., Parker, H. S., Jaffe, A. E. & Storey, J. D. The Sva package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics 28, 882–883 (2012).
Ritchie, M. E. et al. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Rivedal, M. et al. Glomerular transcriptomics predicts long term outcome and identifies therapeutic strategies for patients with assumed benign IgA nephropathy. Kidney Int. 105, 717–730 (2024).
Zhai, Y., Tian, H., Zhang, W., Sun, S. & Zhao, Z. Genome-wide analysis of long noncoding RNAs as cis-acting regulators of transcription factor-encoding genes in IgA nephropathy. PLoS One 19, e0304301 (2024).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Hao, Y. et al. Dictionary learning for integrative, multimodal and scalable single-cell analysis. Nat. Biotechnol. 42, 293–304 (2024).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with harmony. Nat. Methods 16, 1289–1296 (2019).
Wang, X., Park, J., Susztak, K., Zhang, N. R. & Li, M. Bulk tissue cell type deconvolution with multi-subject single-cell expression reference. Nat. Commun. 10, 380 (2019).
Xu, S. et al. Using clusterprofiler to characterize multiomics data. Nat. Protoc. 19, 3292–3320 (2024).
Subramanian, A. et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. U S A 102, 15545–15550 (2005).
Liberzon, A. et al. Molecular signatures database (MSigDB) 3.0. Bioinformatics 27, 1739–1740 (2011).
Aibar, S. et al. SCENIC: Single-cell regulatory network inference and clustering. Nat. Methods 14, 1083–1086 (2017).
Baran, Y. et al. MetaCell: Analysis of single-cell RNA-seq data using K-nn graph partitions. Genome Biol. 20, 206 (2019).
Suo, S. et al. Revealing the critical regulators of cell identity in the mouse cell atlas. Cell. Rep. 25, 1436–1445e3 (2018).
Kamimoto, K. et al. Dissecting cell identity via network inference and in Silico gene perturbation. Nature 614, 742–751 (2023).
Muto, Y. et al. Defining cellular complexity in human autosomal dominant polycystic kidney disease by multimodal single cell analysis. Nat. Commun. 13, 6497 (2022).
Skinnider, M. A. et al. Cell type prioritization in single-cell data. Nat. Biotechnol. 39, 30–34 (2021).
Stassen, S. V., Yip, G. G. K., Wong, K. K. Y., Ho, J. W. K. & Tsia, K. K. Generalized and scalable trajectory inference in single-cell omics data with VIA. Nat. Commun. 12, 5528 (2021).
Zeng, Z. et al. OmicVerse: A framework for bridging and deepening insights across bulk and single-cell sequencing. Nat. Commun. 15, 5983 (2024).
Qiu, X. et al. Reversed graph embedding resolves complex single-cell trajectories. Nat. Methods 14, 979–982 (2017).
Cao, J. et al. The single-cell transcriptional landscape of mammalian organogenesis. Nature 566, 496–502 (2019).
Jin, S., Plikus, M. V. & Nie, Q. CellChat for systematic analysis of cell-cell communication from single-cell transcriptomics. Nat. Protoc. https://doi.org/10.1038/s41596-024-01045-4 (2024).
Garcia-Alonso, L. et al. Single-cell roadmap of human gonadal development. Nature 607, 540–547 (2022).
Acknowledgements
This work was supported by grants from the National Science Foundation of China [grant number 82470751, 82470752], Henan Provincial Department of Science and Technology under the Henan Key Research and Development Speical Project [grant number 241111310700, 251111313800], the Natural Science Foundation of Henan Province [grant number 242300421275]; the Henan Provincial Talent Training Program for Young and Middle-aged Health and Wellness Science and Technology Innovation [grant number YQRC2024010]; the Zhengzhou Huimin project [grant number 2022KJHM0021]; Zhengzhou Municipal Science and Technology Bureau Basic Research and Applied Basic Research [grant number 2024ZZJCYJ035]; the "Three Hundred Initiative" for the Cultivation of Clinical Medical Scientists in Henan Province [grant number S20240113]; the Henan Province High-Level Talent Internationalization Development Program [grant number GCC2025052]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We sincerely appreciate the patients who generously contributed their samples, enabling this research to take place. Our gratitude also extends to the proofreaders and editors for their invaluable support.
Author information
Authors and Affiliations
Contributions
Conceptualization and study design: Z.Z. and Y.Q.; kidney biopsy procedures: GY.C., X.Z., Z.W., J.Y., W.N., and Y.L.; data analysis: J.Y.; interpretation of findings: Z.Z., Y.Q., J.Y., and Y.Z.; immunohistochemistry: C.L. and H.H.; visualization: J.Y. and C.L.; all the authors contributed to writing the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Zhengzhou University First Hospital (Approval No. 2023-KY-0591). All methods were conducted in accordance with relevant guidelines and regulations, including the Declaration of Helsinki. Written informed consent was obtained from all participants and/or their legal guardians prior to their participation in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
You, JP., Cheng, GY., Zhang, XX. et al. Single nucleus RNA-seq reveals the process from onset to chronic kidney disease in IgA nephropathy. Sci Rep 15, 22780 (2025). https://doi.org/10.1038/s41598-025-04292-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04292-x