Abstract
Opioid use disorder poses a complex challenge marked by high relapse rates, which stem from an intricate interplay between physical dependence and psychological vulnerabilities. Previous research has demonstrated that hyperbaric oxygen treatment (HBOT), exposure to 100% oxygen under elevated pressure, reduced physical withdrawal symptoms in morphine-dependent male mice. However, remaining unknown are the effects of HBOT in female mice, its impact on the rewarding and aversive behaviors associated with morphine exposure, and the underlying mechanisms that may be driving these effects. We confirmed the beneficial effects of HBOT in reducing physical withdrawal signs in male mice and, for the first time, demonstrated that HBOT also alleviates these symptoms in female mice. HBOT had no significant effect on morphine-conditioned place preference or conditioned place aversion, suggesting that our HBOT regimen does not influence motivated behaviors. Finally, we show that HBOT treatment reduces microglial soma volume in morphine-treated male and female mice in the paraventricular thalamus, suggesting a shift towards a “resting” state after HBOT. These findings collectively suggest that HBOT may offer a promising, non-pharmacological approach to mitigating opioid withdrawal symptoms across sexes, potentially through modulation of microglia.
Similar content being viewed by others
Introduction
Opioid use disorder (OUD) affects over 16 million people globally and 2.1 million in the United States annually1, with over 75% of drug overdose deaths being associated with opioids2. Current treatments for OUD face significant challenges, including high relapse rates and mortality3,4. When opioid use is discontinued, the resulting neuroadaptive changes often trigger severe somatic and affective withdrawal symptoms, increasing the risk for relapse4,5,6,7. Traditional medication maintenance therapies typically rely on less potent opioids that still carry abuse potential8,9,10 and often fail to prevent long-term relapse, as withdrawal symptoms can re-emerge when doses are tapered down11,12. These limitations underscore the need for more effective and safer treatment approaches for OUD.
Hyperbaric oxygen treatment (HBOT), which involves exposure to 100% oxygen at high pressure, offers a non-pharmacological strategy to treat OUD. HBOT has a long-standing record of safety in human use, with well-established clinical applications. Currently, the FDA approves the use of HBOT to treat thirteen inflammatory, ischemic, and hypoxic afflictions, such as diabetic wounds, radiation injury, severe anemia, and carbon monoxide poisoning13,14,15,16. However, it is not currently approved for treating OUD or its associated symptoms. Research in both humans and preclinical animal models has demonstrated the potential for HBOT to reduce the adverse withdrawal symptoms associated with OUD17,18,19,20,21. Patients with a range of substance use disorders that received HBOT reported “bio-energizing” effects and a decrease in their treatment duration21. Additionally, HBOT used in a small pilot sample of patients being treated with methadone maintenance therapy reduced their methadone dosage and recovered at a faster rate compared to those undergoing methadone treatment alone19. Another pilot study showed that HBOT in patients with OUD self-reported a decrease in withdrawal symptoms, pain, and drug cravings18. Finally, in preclinical models, HBOT reduced withdrawal symptoms in morphine-dependent male mice and rats17,20. Overall, these findings highlight HBOT as a promising adjunctive therapy for OUD, offering potential benefits in alleviating withdrawal symptoms and enhancing recovery outcomes.
Growing evidence underscores the neuroimmune system’s role in substance use disorders22,23,24,25,26. For instance, morphine exposure elicits a neuroinflammatory response by altering glial reactivity and stimulating proinflammatory cytokine release26,27,28,29,30,31. Notably, microglial depletion has been linked to reduced somatic morphine withdrawal symptoms30,32. Given HBOT’s demonstrated ability to attenuate microglial activation and proinflammatory cytokine release in models of traumatic brain injury and intracerebral hemorrhage33,34, we hypothesize that it may similarly reduce opioid-induced microglial changes in the paraventricular thalamus (PVT). The PVT was chosen due to its established role in mediating naloxone-precipitated aversion and somatic signs of withdrawal in morphine-dependent animals35,36,37,38. Consequently, HBOT’s anti-inflammatory and immune-modulating properties could contribute to the alleviation of opioid withdrawal-associated behaviors through microglia alterations in the PVT.
Building on prior work by us and others showing that HBOT reduced physical withdrawal signs in male rodents17,20, our study replicates and extends these findings to show that HBOT attenuates physical withdrawal signs in female mice. Preclinical studies have not addressed whether HBOT impacts OUD-associated motivated behaviors. Despite its effect on withdrawal, we show that HBOT did not significantly alter opioid reward and aversion properties, as measured by morphine-conditioned place preference (CPP) and conditioned place aversion (CPA), respectively. Importantly, our data shows for the first time that HBOT reduces microglial soma volume in the PVT of morphine-treated male and female mice, suggesting a shift towards a resting state and providing a mechanistic rationale for future studies.
The present study demonstrates that HBOT is an effective intervention for reducing somatic morphine withdrawal symptoms in both male and female mice. Furthermore, our findings show that HBOT modulates microglial activity in a morphine withdrawal model, consistent with an anti-inflammatory effect. This observation highlights neuroinflammation as a potential mechanism underlying HBOT’s therapeutic efficacy in managing opioid withdrawal symptoms.
Methods
Animals
A total of 132 C57BL/6J mice (67 males and 65 females), aged 8–12 weeks, were obtained from Jackson Laboratories (Bar Harbor, ME). The mice were acclimated for at least 1-week before experimentation began and were housed in 12:12 light: dark cycle. They were allowed ad libitum access to food and water throughout the experimental procedures. For physical withdrawal studies mice were housed in groups of 2–3. For morphine-induced CPP and CPA studies mice were housed alone to promote the acquisition of morphine CPP and naloxone-precipitated CPA39. All procedures were reviewed and approved by the Institutional Animal Care and Use Committee (IACUC) of Washington State University. All methods were carried out in compliance with relevant guidelines, including adherence to the ARRIVE guidelines for reporting animal research.
Drugs
Morphine sulfate salt pentahydrate was obtained from Sigma-Aldrich (St. Louis, MO) and dissolved in 0.9% sterile physiological saline. Naloxone hydrochloride was obtained from Somerset Therapeutics LLC (Hollywood, FL),
Hyperbaric oxygen treatment
Mice receiving HBOT (HBOT+) were placed in a research-grade hyperbaric chamber (Reimers Systems, Inc., Lorton, VA) as previously described17. The chamber was ventilated with 100% O2 at a flow rate of 4 L/min. The pressure within the cylindrical clear acrylic chamber (27.9 cm diameter x 55.9 cm L) was increased from 1.0 to 3.5 absolute atmosphere (ATA) over a period of 8–10 min. Once 3.5 ATA was reached, the mice remained in the chamber for 1 h. Before removing the mice from the chamber, the chamber was decompressed for 8–10 min. Control mice (HBOT−) were placed in the open hyperbaric chamber and breathed room air.
Morphine dependence and physical withdrawal assessment
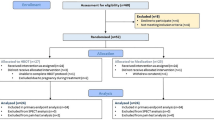
Animals received intraperitoneal (i.p.) injections of morphine or saline twice daily (Fig. 1A), with the morphine dose increasing incrementally each day (Day 1: 50 mg/kg, Day 2: 75 mg/kg, Day 3: 100 mg/kg, Day 4: 125 mg/kg), as previously described17. On Day 5, mice received HBOT, or control treatment as described above. An injection of naloxone (5.0 mg/kg, i.p.) was given after the treatment, which was also 24 h after the final injection of morphine or saline. Immediately following the naloxone injection, mice were placed in a Plexi-glass test chamber (40 cm x 20 cm x 25 cm) in groups of 2–3 and video recorded for 30 min. The number of physical withdrawal behaviors—jumping, forepaw tremors (FPT), wet dog shakes (WDS), rearing, and fecal boli were quantified manually for each mouse. Although the researcher could identify sex and drug treatment from the video recordings, HBOT treatment groups remained indistinguishable. The LabGym machine learning pipeline40,41 was used to measure horizontal activity from recorded videos. Horizontal activity is represented by the normalized distance traveled per 30 min. The software was unable to analyze 2 of the recorded videos, so horizontal activity data for 6 animals was excluded.
Conditioned place aversion
CPA was established as previously described42. Briefly, a three-chamber apparatus was used (Med Associates, Fairfax, VT). Each compartment of the box has distinct contextual characteristics: the center (neutral) compartment (7.2 cm × 12.7 cm × 12.7 cm) has gray walls and gray plastic floor, while the choice compartments (16.8 cm × 12.7 cm × 12.7 cm) each have either white walls and stainless-steel mesh floors or black walls and stainless-steel grid floor. All compartments were illuminated with dim light during use. The location of the mouse, locomotor activity, and time spent in each compartment was measured via automated data-collection software via infrared photo beam strips lining each compartment. A manual guillotine door separated each compartment, allowing for confinement of the mouse to one side of the apparatus. On day 1, mice were tested for 15 min to measure initial preferences followed by 4 days of twice daily morphine injections (10 mg/kg, 20 mg/kg, 30 mg/kg, 40 mg/kg, i.p.) with the doses increasing incrementally each day. On the CPA testing day, animals received another morphine injection (50 mg/kg, i.p.) in the morning. An hour later, the mice were injected with saline and confined to their non-preferred chamber, the chamber in which the mouse spent less time during the initial preference test. The 1-hour HBOT or control treatment was administered 4.5 h after saline-pairing. Immediately after exiting the HBOT chamber, the animals received a second injection of morphine (50 mg/kg, i.p.). One hour later, they were injected with naloxone (1 mg/kg, i.p.) and confined to the opposite (preferred) chamber for 20 min. The following day, mice underwent CPA testing in which they were allowed 15 min of free access to all compartments. The CPA score was calculated by subtracting the time spent in the naloxone-paired chamber post-test by the time spent in the naloxone-paired chamber pre-test.
Conditioned place preference
Mice were placed in the CPP apparatus, as described above, and received a 20-minute habituation session with the guillotine door open and were allowed free access to all compartments. The time spent within each compartment was recorded as described above. Following the initial preference testing, the animals underwent 5 days of conditioning that consisted of 30 min of saline and morphine (10 mg/kg, i.p.) pairing as previously described39. One day after conditioning, mice were exposed to HBOT (HBOT+) or control treatment (HBOT−) for 1 h. The CPP test was conducted 24 h after HBOT. The mice were allowed free access to all compartments for 20 min and tested for CPP. A morphine-primed test was conducted the following day, where animals were injected with a dose of morphine (10 mg/kg, i.p.) before undergoing the CPP test. The CPP score was calculated by subtracting the time spent in the morphine-paired chamber post-test by the amount of time spent in the morphine-paired chamber pre-test.
Tissue collection
Two and a half hours after the physical withdrawal assessment, mice were anesthetized with isoflurane and euthanized by transcardial perfusion, first with ice-cold phosphate-buffered saline (PBS) and then with 4% paraformaldehyde (PFA) in PBS. The brains were collected and stored in 4% PFA in PBS for 24 h (4⁰C). Brains were transferred to 20% sucrose in PBS for an additional 24–48 h (4⁰C). The brains were removed from the sucrose solution, frozen on dry ice, and stored at −80⁰C.
Immunohistochemistry (IHC) and microglia analysis
The collected brains were sliced coronally at 40 μm using a Leica 3050 cryostat (−20⁰C), targeting the paraventricular thalamus (PVT). Brain slices were incubated in blocking buffer consisting of PBS-Triton X-100 (0.3%; PBS-T) with 2% normal donkey serum (NDS) in PBST-Azide (Az) for 2 h at room temperature. Following blocking, the slices were incubated with a rabbit anti-Iba-1 primary antibody (1:1000, FUJIFILM Wako Pure Chemical Corporation Cat# 019-19741, RRID: AB 839504) for 48 h at room temperature. The slices were then rinsed in PBS-Az 3 times for 5 min, and incubated with anti-rabbit AlexaFlour 594 secondary antibody (1:500; Abcam Cat# ab150080, RRID: AB 2650602) and incubated for 3 h at room temperature. Slices were rinsed again with PBS-Az 3 times for 5 min and stored in PBS-Az at 4⁰C until mounting. Slices were mounted onto slides and coverslipped with Flouromount-G (Electron Microscopy Science, Hatfield, PA). Images were acquired with a Keyence BZ-X800 fluorescence microscope. Images were imported in IMARIS (Oxford Instruments) and the microglia soma were identified using the IMARIS surface function.
Data analysis
A repeated measures two-way analysis of variance (RM-ANOVA) was used to determine any effect of drug on body weight (Fig. 1B,C) and effect of HBOT on the amount of time spent in the appropriate chamber in the CPA and CPP experiments (Fig. 4C,F). A two-way ANOVA was used to detect main effects of HBOT and sex (Figs. 2 and 3) on physical withdrawal symptoms and a main effect of HBOT in CPP score (Fig. 4E). When appropriate, Bonferroni post-hoc analysis was used for multiple comparisons. The CPA study used an independent samples t-test to identify any significant difference between CPA scores of HBOT+ and HBOT− groups. The Kolmogorov-Smirnov test was used to analyze microglia soma volume (Fig. 5). An α value of 0.05 was used for all experiments.
Results
Physical withdrawal (body weight)
To establish morphine physical dependence, escalating doses of morphine injections (i.p.) were administered twice daily for 4 days (Fig. 1A). We found that morphine administration reduced body weight in both male mice (Fig. 1B: Mixed-effect analysis, Treatment x Day: F(4, 163) = 260.20, p < 0.0001) and female mice (Fig. 1C: 2-Way ANOVA, Treatment x Day: F(4, 156) = 147.20, p < 0.0001) compared to control mice exposed to saline. Šídák’s multiple comparisons test was conducted to evaluate differences. These results are consistent with previous literature showing that morphine withdrawal induces significant body weight loss43,44,45,46,47.
Physical withdrawal (morphine-naloxone)
Somatic measures of naloxone-precipitated withdrawal were scored following 4 days of morphine administration, followed by 1 h of control (HBOT−) or HBOT exposure (HBOT+), and then a naloxone injection to precipitate withdrawal (Fig. 2A). HBOT+ mice exhibited a significant main effect of HBOT treatment in the number of naloxone-precipitated WDS (Fig. 2B: 2-Way ANOVA, F(1, 30) = 6.48, p = 0.016), FPT (Fig. 2C: 2-Way ANOVA, F(1, 30) = 9.00, p = 0.005), and fecal boli (Fig. 2G: 2-Way ANOVA, F(1, 30) = 13.58, p < 0.001) in both male and female morphine-dependent mice. No main effect of HBOT was observed in jumps or rears. Independent of HBOT, morphine-dependent female mice exhibited a significant increase in jumping (Fig. 2D: 2-Way ANOVA, F(1, 30) = 6.46, p = 0.016) and rearing (Fig. 2E: 2-Way ANOVA, F(1, 30) = 5.80, p = 0.022), and a decrease in fecal boli (Fig. 2G: 2-Way ANOVA, F(1, 30) = 9.07, p = 0.005) compared to morphine-dependent male mice. No sex difference was observed in the WDS or FPT behaviors. A treatment x sex interaction was observed in horizontal activity of morphine-dependent mice (Fig. 2F: 2-Way ANOVA, F(1, 28) = 11.77, p = 0.002). Follow-up comparisons using Bonferroni’s multiple comparisons test indicated that HBOT− females exhibit significantly more horizontal activity than HBOT+ females. These data indicates that HBOT successfully reduced the occurrence of WDS, FPT, and fecal boli precipitated by naloxone in morphine-dependent male and female mice, whereas larger movement-based measures—jumps and rears, remained largely unaffected by HBOT, but did show differences across sexes.
Physical withdrawal (saline-naloxone)
To confirm our model accurately captured morphine-dependent withdrawal symptoms, a separate cohort of mice received saline injections instead of morphine and 1 h of control (HBOT−) or HBOT exposure (HBOT+), followed by naloxone administration (saline-naloxone; Fig. 3A). As expected, saline-naloxone treated mice displayed less somatic withdrawal symptoms than the morphine-naloxone treated mice (Fig. 3 vs. Figure 2), with the exception of activity-based measures (rears and horizontal activity) which are typically reduced during withdrawal48,49. Surprisingly, there was a significant main effect of HBOT on WDS (Fig. 3B: 2-Way ANOVA, F(1, 46) = 4.62, p = 0.04) and horizontal activity (Fig. 3F: F(1, 40) = 10.73, p = 0.002). In addition, there was a significant main effect of sex on jumps (Fig. 3D: 2-Way ANOVA, F(1, 46) = 7.71, p = 0.008) and horizontal activity (Fig. 3F: 2-Way ANOVA, F(1, 40) = 14.71, p < 0.001) and a significant treatment x sex interaction for fecal boli (Fig. 3G: 2-Way ANOVA, F(1, 46) = 12.92, p < 0.001). Therefore, our data suggests HBOT may impact the endogenous opioid system, and future studies will assess this speculation. A summary of the effects of HBOT on somatic withdrawal behaviors is shown in Table 1.
Conditioned place aversion (CPA)
To investigate whether HBOT attenuates naloxone-induced aversion in morphine-treated male mice, we employed a conditioned place aversion test (CPA; Fig. 4A). After a 4-day escalating morphine regimen, mice received morphine (50 mg/kg), followed 1 h later by saline paired with their preferred chamber. HBOT (or control; HBOT-) was administered 4.5 h later, immediately followed by a second morphine dose. Naloxone (1 mg/kg) was administered 1-hour post-HBOT to precipitate withdrawal and induce an aversive state. HBOT+ mice exhibited CPA comparable to control mice, as evidenced by a significant reduction in time spent in the naloxone-paired chamber on the test day compared to the habituation day (Fig. 4B: RM 2-Way ANOVA, F(1, 24) = 50.87, p < 0.0001). In addition, there was no significant difference in the CPA score (test-habituation) between HBOT+ and HBOT− male mice (Fig. 4C). This suggests that HBOT had no significant effect on the aversion toward naloxone-precipitated withdrawal in male mice.
Conditioned place preference (CPP)
To examine whether HBOT influences conditioned morphine seeking behavior in male mice, we employed a CPP model (Fig. 4D). There was a significant main effect of day indicating mice preferred the morphine-paired side (Fig. 4E: RM 2-Way ANOVA, F(1.61, 11.24) = 21.44, p = 0.0002). However, there was no effect of HBOT on morphine-induced preference. In addition, the CPP score significantly increased after a morphine-prime compared to the test day, as expected (Fig. 4E: RM 2-Way ANOVA, F(1, 7) = 16.09, p = 0.005). No significant effect of HBOT exposure on CPP score in male mice was observed. Overall, these data suggest that our HBOT regimen does not significantly influence the conditioned motivation effects associated with morphine, as it neither mitigates naloxone-induced aversion nor alters morphine-induced preference in male mice.
Microglia
To investigate a potential mechanism underlying the effect of HBOT on the expression of morphine withdrawal signs, we examined microglia morphological changes in the PVT of the mice that underwent the physical withdrawal protocol (Fig. 1A). Microglial changes were assessed by measuring soma volume, with larger soma size and reduced process complexity suggesting increased activation29,50,51. As expected, a Kolmogorov-Smirnov test revealed no difference in microglia soma volume distribution in saline-naloxone treated male (Fig. 5A) and female (Fig. 5C) mice regardless of whether they received HBOT. However, HBOT+ mice treated with morphine had more cells with decreased soma volume compared to HBOT− mice treated with morphine in both males (Fig. 5B: KS, D = 0.27, p = 0.0146) and females (Fig. 5D: KS, D = 0.4792, p < 0.0001). These findings suggest that HBOT may mitigate morphine withdrawal symptoms by reducing microglial activation in the PVT, indicating a potential neuroimmune mechanism underlying its therapeutic effect in male and female mice. A summary of the data for microglial soma volume is shown in Table 2.
Discussion
In this study, we investigated the efficacy of HBOT in attenuating morphine withdrawal signs in both male and female mice. Building upon Nicoara et al.‘s (2016) findings showing that HBOT suppresses withdrawal signs in morphine-dependent male mice17, our study extended this research by demonstrating that HBOT attenuates naloxone-precipitated physical withdrawal symptoms in both male and female mice. Notably, our study is the first to establish a correlation between HBOT’s suppression of physical withdrawal symptoms and reduced microglial soma volume in the PVT. We also show that HBOT did not impact conditioned morphine place preference (CPP) or conditioned withdrawal aversion (CPA) in male mice. Interestingly, HBOT reduced some withdrawal-like behaviors even in mice with no prior morphine history, suggesting a potential interaction with endogenous opioid systems, a mechanism warranting further investigation in future studies.
Expanding upon previous research, this study addresses the significant sex differences observed in opioid responses across both human and rodent models. Women with OUD typically exhibit a more severe clinical profile than men, including greater adverse effects52,53, more rapid escalation of use52, and higher prevalence of psychiatric comorbidities52. These patterns are mirrored in preclinical rodent models, where females show greater sensitivity to opioids’ reinforcing effects45,54,55,56 and reduced analgesic responsiveness55,57,58,59. However, the literature on sex differences in morphine withdrawal symptoms remains inconsistent, with studies reporting varied results likely due to differences in experimental parameters43,60,61,62,63,64,65. To address this research gap, we conducted a systematic assessment of physical withdrawal symptoms between sexes, aiming to clarify conflicting results and provide a more comprehensive understanding of sex differences in opioid withdrawal.
Consistent with existing literature on opioid dependence43,44,45,46,47, our study demonstrated that morphine administration resulted in significant weight loss in both male and female mice, contrasting the saline-treated control group that maintained stable body weights throughout the experiment as expected. Predictably, we observed a difference in the severity of naloxone-precipitated withdrawal symptoms between the two groups. Morphine-exposed mice exhibited pronounced withdrawal symptoms, whereas saline-exposed mice showed considerably fewer withdrawal signs following the naloxone injection. These observations strongly support the efficacy of our model in inducing physical dependence on morphine.
In this study, we show that HBOT reduced naloxone-precipitated WDS, FPT, and fecal boli in both male and female morphine-dependent mice. In addition, HBOT reduced naloxone-precipitated WDS and horizontal activity in both male and female mice with no history of morphine exposure. There were significant sex differences in activity metrics (jumps, rears, horizontal activity) with females in general exhibiting greater activity than males, which is consistent with previous findings showing that females generally exhibit increased activity and that male activity is more severely affected by morphine49,66. Finally, consistent with previous studies, males exhibited higher fecal boli counts, consistent with some studies showing males more severe diarrhea during morphine withdrawal compared to females43,67.
The measured behaviors of WDS, FPT, and defecation in rodents show strong translational relevance to core symptoms of opioid withdrawal in humans11,68,69. Clinical assessments including the Subjective Opiate Withdrawal Scale (SOWS) and Clinical Opiate Withdrawal Scale (COWS) identify shaking, cold flashes, tremors, and gastrointestinal distress as hallmark withdrawal manifestations11,68. In rodents, WDS, a thermoregulatory response to withdrawal-induced hypothermia, directly parallels the chills and piloerection observed during naloxone-precipitated withdrawal in humans69,70. Similarly, increased defecation reflects the diarrhea characteristic of human opioid withdrawal syndrome11,68. These behavioral parallels strengthen the translational validity of our model, particularly given that our observed reduction in withdrawal severity after HBOT aligns with preliminary clinical evidence showing HBOT’s efficacy in alleviating opioid withdrawal symptoms within 24 hours18.
Jumping behavior is considered the most reliable indicator of severe opioid withdrawal in C57BL/6 mice28,48,71. Our data support this, showing a significant increase in jumps among morphine-exposed mice compared to saline-treated controls. However, unlike WDS, FPT, and fecal boli, HBOT had no effect on jumping behavior in either sex. This contrasts with findings from Nicoara et al. (2016), who reported a significant reduction in jumping. The discrepancy may stem from differences in experimental conditions, as the previous study used male NIH Swiss mice and found reduced jumping only after a 1-hour HBOT session, but not a 30-minute session17. Given that mouse strain affects the presentation of morphine withdrawal symptoms and C57BL/6J mice jump more in response to naloxone-precipitated morphine withdrawal than NIH Swiss mice28,71,72,73, a longer HBOT session may be necessary to observe a significant reduction in jumping. Future studies will determine the impact of treatment duration and timing on withdrawal behaviors.
Sex differences in jumping behavior were evident in both saline and morphine-exposed mice, with females consistently displaying increased jumping. Although the literature on sex differences in withdrawal-induced jumping remains variable, a previous study demonstrated that gonadectomized male and female mice exhibit reduced jumping compared to intact mice74. These findings suggest that sex hormone levels may modulate activity and withdrawal-induced jumping, potentially explaining the observed sex differences and inconsistencies in existing research.
In alignment with established literature demonstrating increased activity in female rodents across environmental contexts49,66,75, our data shows sex differences in horizontal activity. Quantitative analysis with LabGym machine learning pipeline40,41 demonstrated that female mice maintained elevated activity levels compared to males across all experimental groups, including both saline-treated controls and morphine-exposed cohorts. In addition, the other metrics reflective of activity (jumps and rears) showed elevated counts in females relative to males. It is well-established that morphine withdrawal reduces activity48,49. In addition, previous research shows that while female rats naturally display higher levels of voluntary wheel running than males, morphine withdrawal attenuates activity in both sexes, with males experiencing more pronounced disruptions to their running patterns49. Our findings contradicted our hypothesis: rather than increasing horizontal activity in morphine-exposed mice receiving HBOT, we observed reduced activity in females and no effect in males. While we cannot entirely dismiss the possibility that HBOT generally reduced activity, it seems unlikely because not every behavior we scored was reduced. This evidence suggests that HBOT specifically decreases somatic withdrawal signs without causing a general reduction in activity levels. Notably, while HBOT has been shown to improve locomotor function in conditions such as Parkinson’s disease76 and traumatic brain injury77, our study indicates that its effects are targeted toward alleviating withdrawal-specific symptoms rather than broadly suppressing activity. However, we cannot rule out the possibility that HBOT may also exert anxiolytic effects, as previously demonstrated in rodent models78,79. This would also align with our observation of decreased fecal boli production following HBOT, a metric often associated with reduced anxiety levels80, in addition to withdrawal. Future studies are needed to determine whether the observed effects are opioid-specific or more broadly related to anxiety reduction.
While the negative somatic component of opioid withdrawal strongly motivate individuals to resume opioid use, they are not the only symptoms of OUD that contribute to relapse81,82,83,84. The affective and motivational elements underlying relapse are key components of the disorder that must be considered when evaluating potential OUD treatments. It has been shown that patients with OUD undergoing treatment can develop conditioned aversion to cues associated with the unpleasant outcomes induced by treatment itself81, such as healthcare personnel administering treatment, treatment facilities, and even individuals encouraging recovery. This conditioned aversion motivates relapse in attempt to avoid the physical and emotional discomfort associated with these cues that accompany treatment81. To assess the efficacy of HBOT on reducing this negative aversive state, we employed a naloxone-precipitated withdrawal CPA paradigm42. Indeed, environmental stimuli previously paired with withdrawal can independently elicit withdrawal-like states, heightening cravings and subsequent opioid seeking even after prolonged abstinence, thereby significantly contributing to relapse through conditioned negative reinforcement mechanisms in both humans and rodent models81,84. We did not observe any significant effect of HBOT on the CPA score, a measure of aversion toward a negative state of naloxone-precipitated withdrawal in male mice. This suggests that HBOT selectively attenuates somatic withdrawal-associated symptoms without affecting aversive conditioning to withdrawal-associated contexts. However, we cannot exclude the possibility that extended or additional HBOT sessions might influence aversive conditioning outcomes, and future studies will directly test this hypothesis.
Drug cravings triggered by exposure to drug cues represent another critical component of OUD that motivates relapse. Inverse to conditioned aversion, conditioned drug seeking is promoted by the exposure to cues associated with the positive effects of drug use, like drug paraphernalia and interactions with other drug users. These cues can acquire reinforcing properties, enhancing drug-seeking behavior and relapse potential and supporting the acquisition of new responses84. In our study, we investigated whether HBOT could reduce drug-seeking mediated by contextual cues using a CPP model. No significant effect of HBOT on CPP, a reflection of contextual drug seeking, was observed in male mice.
Additionally, administering multiple HBOT sessions (data not shown) still did not yield any significant effect during the CPP expression test. These findings suggest that while HBOT may attenuate somatic withdrawal symptoms, it does not appear to influence conditioned drug-seeking behaviors associated with environmental cues. While the CPP model is a valuable tool for assessing contextual drug-seeking behaviors, it has limitations in capturing the voluntary nature of drug-taking and the influence of drug-associated cues. This is because, in the CPP paradigm, animals are passively administered drugs, which may not fully reflect the active decision-making processes involved in human drug use. In contrast, drug self-administration models allow animals to actively engage in operant behaviors to obtain drugs, thereby more closely mirroring the voluntary aspects of human substance use disorders. These models are considered the “gold standard” for investigating the neurobiology of drug addiction in rodents85. Recognizing this limitation, future studies will employ self-administration paradigms to more accurately investigate the effects of HBOT on voluntary drug-taking behaviors and the impact of drug-associated cues on relapse to opioid seeking.
While human and preclinical studies suggest that HBOT may have promising effects in reducing withdrawal symptoms17,18,19,20,21, the underlying mechanisms by which HBOT exerts these benefits remain largely unexplored. We demonstrate for the first time that HBOT significantly reduces morphine-induced increases in microglial soma volume within the paraventricular thalamus (PVT). This structural normalization aligns with attenuated opioid withdrawal symptoms in both male and female mice86, suggesting a sex-independent anti-inflammatory mechanism.
The PVT plays a well-established role in modulating opioid-related somatic/affective states, with heightened activation observed during morphine withdrawal (spontaneous and naloxone-precipitated)35. Conversely, inhibition of PVT neurons induces conditioned morphine preference, a result that is mirrored by local morphine administration to the PVT87. Emerging evidence further implicates the PVT in mediating aversion35,37,88, reward87, and relapse behaviors88,89,90. Morphine administration induces distinct microglial remodeling in thalamic regions, including reduced complexity (lower fractal dimension), decreased cell area/perimeter, and increased density/soma volume31, morphological hallmarks of microglial activation29,50,51. Our work extends these observations by identifying HBOT as an effective intervention for altering morphine-associated microglial morphological changes.
HBOT’s anti-inflammatory effects may involve a biphasic response: initially, exposure to HBOT may trigger the generation of reactive oxygen species (ROS) and hypoxia-inducible factor upregulation, causing transient oxidative stress13,14,15. This is followed by a compensatory phase where antioxidants are recruited, stem progenitor cells are mobilized, growth factors are released, and perfusion is improved, collectively resolving inflammation13,14,15. This mechanism is supported by HBOT’s efficacy in reducing microglial soma volume (indicative of reduced activation) and proinflammatory cytokine release in intracranial ischemia33 and traumatic brain injury models34,77, consistent with our findings of decreased soma volume in PVT microglial cells. However, although HBOT reduced microglial soma volume in morphine-exposed mice, it is important to note that morphine did not appear to increase soma volume compared to saline controls in male mice, highlighting the need for future experiments to determine whether baseline levels are influencing the observed effects.
The strong correlation between HBOT-induced microglial normalization and reduced withdrawal severity highlights the potential of PVT microglia as therapeutic targets for OUD. It also underscores HBOT’s translational promise for mitigating neuroinflammatory components of addiction and provides a novel pathway for addressing sex-independent aspects of opioid withdrawal.
Our work further supports the use of HBOT as a therapeutic treatment for opioid withdrawal symptoms. Abnormal pain perception and aversive physical states are substantial comorbid conditions during withdrawal among individuals with OUD7,91,92, significantly increasing the risk of relapse7,91 and can persist for months after opioid use is terminated93. Therefore, alleviating somatic opioid withdrawal symptoms would be a critical first step in promoting recovery, as it would ease the process of detoxifying from the drug. The initial withdrawal symptoms that accompany recovery deter many individuals from abstinence and can cause others who have already begun recovery to relapse4,81. Hence, given that HBOT alleviated the somatic component of withdrawal, this treatment method would likely be most effective when used as an adjunct treatment to traditional therapies, especially ones that address the motivational factors of OUD, like cognitive behavioral therapy94,95.
Therefore, the best way to mitigate the effects of OUD would be employing preventative measures among high-risk groups. For instance, individuals receiving treatment for chronic pain could particularly benefit from HBOT, given that approximately 66.4% of patients with OUD have a history of chronic pain92, and the most common reason individuals with OUD report initiating opioid use is to relieve pain6,10. Exposure to HBOT has demonstrated antinociceptive effects, attenuating pain in rodent models96,97,98,99,100,101 and humans18,102. Alleviating initial withdrawal symptoms after stopping opioid pain medications could prevent the patient from abusing the drug. Furthermore, alleviating the underlying pain to begin with may prevent the need for opioids all together. Our study supports the potential for HBOT to be a safe, effective treatment for opioid withdrawal, as attenuating withdrawal-associated pain and discomfort will improve the prognosis of OUD, minimizing the detrimental effects of the disorder. These findings highlight the need for further research to fully establish HBOT’s efficacy in this context.
Morphine induces weight loss in mice. (A) Schematic representation of the experimental timeline. (B) Male mice treated with morphine (n = 17) lose more weight than control male mice (n = 26). (C) Female mice treated with morphine (n = 17) lose more weight than control female mice (n = 24). Data are represented as mean ± SEM. *p < 0.05. White Triangles: Saline-treated mice. Black circles: Morphine-treated mice.
HBOT attenuates somatic symptoms of morphine withdrawal in morphine-dependent male and female mice. (A) Schematic of experimental protocol. (B) Wet-dog shakes (WDS) are decreased following HBOT in male and female mice treated with morphine. (C) Forepaw tremors (FPT) are decreased following HBOT in both sexes. (D) Female mice jump more than male mice with no effect of HBOT. (E) Female mice rear more than male mice with no effect of HBOT. (F) Female mice exhibit more horizontal activity than male mice. HBOT decreases horizontal activity in female mice. (G) HBOT decreases fecal boli production in male and female mice and male mice produce more fecal boli than female mice. Data are represented as mean ± SEM. *p < 0.05. n = 8–9/group. White circles/white bars: Morphine-treated HBOT− mice. Purple circles/gray bars: Morphine-treated HBOT+ mice.
HBOT mitigates somatic symptoms in opioid-naïve mice administered naloxone. (A) Schematic of experimental protocol. (B) Wet-dog shakes (WDS) are decreased following HBOT in naloxone treated male and female mice without a history of morphine exposure. (C) Forepaw tremors (FPT) are not affected by HBOT. (D) Female mice jump more than male mice with no effect of HBOT. (E) Rears are not affected by HBOT. (F) HBOT decreases horizontal activity in both sexes and female mice exhibit more horizontal activity than male mice. (G) HBOT decreases fecal boli production in male mice. Data are represented as mean ± SEM. *p < 0.05. n = 8–9/group. White triangles/white bars: Saline-naloxone treated HBOT− mice. Purple triangles/gray bars: Saline-naloxone treated HBOT+ mice.
HBOT has no effect on conditioned aversion and contextual drug seeking behaviors. (A) Schematic for conditioned place aversion (CPA) experimental protocol. (B) CPA was successfully acquired, but there is no difference between HBOT+ (n = 14) and HBOT− (n = 12) groups on CPA score. (C) There is no difference between HBOT+ (n = 14) and HBOT− (n = 12) groups on the amount of time spent in the naloxone-paired chamber. (D) Schematic for conditioned place preference (CPP) experimental protocol. (E) CPP was successfully acquired, but there is no difference between HBOT+ (n = 5) and HBOT− (n = 4) groups on CPP score. (F) There is no difference between HBOT+ (n = 5) and HBOT− (n = 4) groups on the amount of time spent in the morphine-paired chamber. Data are represented as mean ± SEM. *p < 0.05. White circles/white bars: HBOT− male mice. Purple circles/gray bars: HBOT+ male mice.
HBOT is associated with decreased microglial soma volume in the PVT of morphine-naloxone but not saline-naloxone treated male and female mice. (A) HBOT had no significant effect on microglial soma volume in saline-naloxone treated male mice (HBOT–: n = 3 mice/43 cells; HBOT+: n = 4 mice/61 cells). (B) In contrast, HBOT significantly reduced microglial soma volume in morphine-naloxone treated male mice (HBOT–: n = 4 mice/90 cells; HBOT+: n = 4 mice/57 cells). (C) Similarly, no significant effect of HBOT was observed in saline-naloxone treated female mice (HBOT–: n = 4 mice/85 cells; HBOT+: n = 4 mice/58 cells). (D) However, HBOT significantly reduced microglial soma volume in morphine-naloxone treated female mice (HBOT–: n = 3 mice/41 cells; HBOT+: n = 4 mice/71 cells). Data are presented as relative frequency histograms. *p < 0.05. Symbols: White triangles, saline-naloxone treated HBOT– mice; purple triangles, saline-naloxone treated HBOT + mice; white circles, morphine-naloxone treated HBOT– mice; purple circles, morphine-naloxone treated HBOT + mice.
Conclusion
This study validates and expands upon previous research showing that HBOT reduces opioid withdrawal signs in male mice. Our key findings include: (1) HBOT attenuates somatic opioid withdrawal symptoms in both male and female mice; (2) HBOT reduces microglial soma volume in the PVT in both sexes; and (3) HBOT did not impact motivated behaviors. While further research is necessary to establish a definitive causal relationship between microglial changes and symptom alleviation, this study underscores neuroinflammation as a compelling mechanistic target for HBOT interventions. Future investigations should systematically evaluate whether varying HBOT parameters can specifically modulate motivation.
Data availability
The raw data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Dydyk, A. M., Jain, N. K. & Gupta, M. in StatPearls (2025).
Control, C. F. D. Understanding the opioid overdose epidemic. https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html (2024).
Hser, Y. I. et al. High mortality among patients with opioid use disorder in a large healthcare system. J. Addict. Med. 11, 315–319. https://doi.org/10.1097/ADM.0000000000000312 (2017).
Smyth, B. P., Barry, J., Keenan, E. & Ducray, K. Lapse and relapse following inpatient treatment of opiate dependence. Ir. Med. J. 103, 176–179 (2010).
Monroe, S. C. & Radke, A. K. Opioid withdrawal: role in addiction and neural mechanisms. Psychopharmacol. (Berl). 240, 1417–1433. https://doi.org/10.1007/s00213-023-06370-2 (2023).
Weiss, R. D. et al. Reasons for opioid use among patients with dependence on prescription opioids: the role of chronic pain. J. Subst. Abuse Treat. 47, 140–145. https://doi.org/10.1016/j.jsat.2014.03.004 (2014).
Liebmann, P. M. et al. Nervousness and pain sensitivity: II. Changed relation in ex-addicts as a predictor for early relapse. Psychiatry Res. 79, 55–58. https://doi.org/10.1016/s0165-1781(98)00024-9 (1998).
Dennison, S. J. Clonidine abuse among opiate addicts. Psychiatr Q. 72, 191–195. https://doi.org/10.1023/a:1010375727768 (2001).
Schuman-Olivier, Z. et al. Self-treatment: illicit buprenorphine use by opioid-dependent treatment seekers. J. Subst. Abuse Treat. 39, 41–50. https://doi.org/10.1016/j.jsat.2010.03.014 (2010).
McCabe, S. E., Cranford, J. A., Boyd, C. J. & Teter, C. J. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict. Behav. 32, 562–575. https://doi.org/10.1016/j.addbeh.2006.05.022 (2007).
Torres-Lockhart, K. E., Lu, T. Y., Weimer, M. B., Stein, M. R. & Cunningham, C. O. Clinical management of opioid withdrawal. Addiction 117, 2540–2550. https://doi.org/10.1111/add.15818 (2022).
Dunn, K. E., Sigmon, S. C., Strain, E. C., Heil, S. H. & Higgins, S. T. The association between outpatient buprenorphine detoxification duration and clinical treatment outcomes: a review. Drug Alcohol Depend. 119, 1–9. https://doi.org/10.1016/j.drugalcdep.2011.05.033 (2011).
Choudhury, R. Hypoxia and hyperbaric oxygen therapy: a review. Int. J. Gen. Med. 11, 431–442. https://doi.org/10.2147/IJGM.S172460 (2018).
Ortega, M. A. et al. A general overview on the hyperbaric oxygen therapy: applications, mechanisms and translational opportunities. Med. (Kaunas). 57. https://doi.org/10.3390/medicina57090864 (2021).
Thom, S. R. & 131S-141S. Hyperbaric oxygen: its mechanisms and efficacy. Plast. Reconstr. Surg. 127 (Suppl 1). https://doi.org/10.1097/PRS.0b013e3181fbe2bf (2011).
Weaver, L. K. Hyperbaric Oxygen Therapy Indications (Best Publishing Company, 2014).
Nicoara, D. et al. Hyperbaric oxygen treatment suppresses withdrawal signs in morphine-dependent mice. Brain Res. 1648, 434–437. https://doi.org/10.1016/j.brainres.2016.08.017 (2016).
Wilson, M., Bindler, R. J., Stanek, K., Layton, M. E. & Quock, R. M. Hyperbaric oxygen therapy for pain, opioid withdrawal, and related symptoms: A pilot randomized controlled trial. Pain Manag Nurs. 23, 616–624. https://doi.org/10.1016/j.pmn.2022.03.001 (2022).
Wilson, M. et al. Hyperbaric oxygen to assist adults with opioid use disorder in reducing methadone dose. J. Addict. Nurs. 33, 27–36. https://doi.org/10.1097/JAN.0000000000000447 (2022).
Chen, C. et al. Hyperbaric oxygen attenuates withdrawal symptoms by regulating monoaminergic neurotransmitters and NO signaling pathway at nucleus accumbens in Morphine-Dependent rats. Neurochem Res. 43, 531–539. https://doi.org/10.1007/s11064-017-2447-x (2018).
Yepifanova, N. M. Hyperbaric oxygenation in the treatment of patients with opioid addiction, substance addiction and alcoholism in the post-intoxication and abstinence periods. Anesthesiol. Resusit. Sci. (1995).
Hutchinson, M. R. et al. Possible involvement of toll-like receptor 4/myeloid differentiation factor-2 activity of opioid inactive isomers causes spinal proinflammation and related behavioral consequences. Neuroscience 167, 880–893. https://doi.org/10.1016/j.neuroscience.2010.02.011 (2010).
Hutchinson, M. R. et al. Opioid activation of toll-like receptor 4 contributes to drug reinforcement. J. Neurosci. 32, 11187–11200. https://doi.org/10.1523/JNEUROSCI.0684-12.2012 (2012).
Hutchinson, M. R. et al. Exploring the neuroimmunopharmacology of opioids: an integrative review of mechanisms of central immune signaling and their implications for opioid analgesia. Pharmacol. Rev. 63, 772–810. https://doi.org/10.1124/pr.110.004135 (2011).
Liu, J., Li, J. X., Wu, R. & Toll-Like Receptor 4: A novel target to tackle drug addiction?? Handb. Exp. Pharmacol. 276, 275–290. https://doi.org/10.1007/164_2022_586 (2022).
Watkins, L. R., Hutchinson, M. R., Rice, K. C. & Maier, S. F. The toll of opioid-induced glial activation: improving the clinical efficacy of opioids by targeting glia. Trends Pharmacol. Sci. 30, 581–591. https://doi.org/10.1016/j.tips.2009.08.002 (2009).
Schwarz, J. M. & Bilbo, S. D. Adolescent morphine exposure affects long-term microglial function and later-life relapse liability in a model of addiction. J. Neurosci. 33, 961–971. https://doi.org/10.1523/JNEUROSCI.2516-12.2013 (2013).
Liu, L., Coller, J. K., Watkins, L. R., Somogyi, A. A. & Hutchinson, M. R. Naloxone-precipitated morphine withdrawal behavior and brain IL-1beta expression: comparison of different mouse strains. Brain Behav. Immun. 25, 1223–1232. https://doi.org/10.1016/j.bbi.2011.03.016 (2011).
Zhang, X., Jin, T., Wang, H., Han, S. & Liang, Y. Microglia in morphine tolerance: cellular and molecular mechanisms and therapeutic potential. Front. Pharmacol. 15, 1499799. https://doi.org/10.3389/fphar.2024.1499799 (2024).
Kwok, C. H. T. et al. Pannexin-1 channel Inhibition alleviates opioid withdrawal in rodents by modulating locus coeruleus to spinal cord circuitry. Nat. Commun. 15, 6264. https://doi.org/10.1038/s41467-024-50657-7 (2024).
Liao, K. et al. Morphine-mediated release of miR-138 in astrocyte-derived extracellular vesicles promotes microglial activation. J. Extracell. Vesicles. 10, e12027. https://doi.org/10.1002/jev2.12027 (2020).
Hutchinson, M. R. et al. Reduction of opioid withdrawal and potentiation of acute opioid analgesia by systemic AV411 (ibudilast). Brain Behav. Immun. 23, 240–250. https://doi.org/10.1016/j.bbi.2008.09.012 (2009).
Yang, L. et al. Hyperbaric oxygen preconditioning attenuates neuroinflammation after intracerebral hemorrhage in rats by regulating microglia characteristics. Brain Res. 1627, 21–30. https://doi.org/10.1016/j.brainres.2015.08.011 (2015).
Lim, S. W. et al. Microglial activation induced by traumatic brain injury is suppressed by postinjury treatment with hyperbaric oxygen therapy. J. Surg. Res. 184, 1076–1084. https://doi.org/10.1016/j.jss.2013.04.070 (2013).
Zhu, Y., Wienecke, C. F., Nachtrab, G. & Chen, X. A thalamic input to the nucleus accumbens mediates opiate dependence. Nature 530, 219–222. https://doi.org/10.1038/nature16954 (2016).
Penzo, M. A. & Gao, C. The paraventricular nucleus of the thalamus: an integrative node underlying homeostatic behavior. Trends Neurosci. 44, 538–549. https://doi.org/10.1016/j.tins.2021.03.001 (2021).
Kirouac, G. J. Placing the paraventricular nucleus of the thalamus within the brain circuits that control behavior. Neurosci. Biobehav Rev. 56, 315–329. https://doi.org/10.1016/j.neubiorev.2015.08.005 (2015).
Hou, G. et al. Opioid receptors modulate firing and synaptic transmission in the paraventricular nucleus of the thalamus. J. Neurosci. 43, 2682–2695. https://doi.org/10.1523/JNEUROSCI.1766-22.2023 (2023).
McKendrick, G. et al. Ketamine blocks Morphine-Induced conditioned place preference and Anxiety-Like behaviors in mice. Front. Behav. Neurosci. 14, 75. https://doi.org/10.3389/fnbeh.2020.00075 (2020).
Goss, K. et al. Quantifying social roles in multi-animal videos using subject-aware deep-learning. BioRxiv https://doi.org/10.1101/2024.07.07.602350 (2024).
Hu, Y. et al. Quantification of user-defined animal behaviors using learning-based holistic assessment. Cell. Rep. Methods. 3, 100415. https://doi.org/10.1016/j.crmeth.2023.100415 (2023). LabGym.
Hikida, T., Kitabatake, Y., Pastan, I. & Nakanishi, S. Acetylcholine enhancement in the nucleus accumbens prevents addictive behaviors of cocaine and morphine. Proc. Natl. Acad. Sci. U S A. 100, 6169–6173. https://doi.org/10.1073/pnas.0631749100 (2003).
Papaleo, F. & Contarino, A. Gender- and morphine dose-linked expression of spontaneous somatic opiate withdrawal in mice. Behav. Brain Res. 170, 110–118. https://doi.org/10.1016/j.bbr.2006.02.009 (2006).
Garcia-Carmona, J. A., Baroja-Mazo, A., Milanes, M. V. & Laorden, M. L. Sex differences between CRF1 receptor deficient mice following naloxone-precipitated morphine withdrawal in a conditioned place aversion paradigm: implication of HPA axis. PLoS One. 10, e0121125. https://doi.org/10.1371/journal.pone.0121125 (2015).
Cicero, T. J., Nock, B. & Meyer, E. R. Gender-linked differences in the expression of physical dependence in the rat. Pharmacol. Biochem. Behav. 72, 691–697. https://doi.org/10.1016/s0091-3057(02)00740-2 (2002).
Kalamarides, D. J., Singh, A. & Dani, J. A. Protracted opioid withdrawal behaviors are reduced by nitric oxide Inhibition in mice. Addict. Neurosci. 12 https://doi.org/10.1016/j.addicn.2024.100167 (2024).
Kalamarides, D. J., Singh, A., Wolfman, S. L. & Dani, J. A. Sex differences in VTA GABA transmission and plasticity during opioid withdrawal. Sci. Rep. 13, 8460. https://doi.org/10.1038/s41598-023-35673-9 (2023).
Ozdemir, D., Meyer, J., Kieffer, B. L. & Darcq, E. Model of negative affect induced by withdrawal from acute and chronic morphine administration in male mice. Sci. Rep. 14, 9767. https://doi.org/10.1038/s41598-024-60759-3 (2024).
Morgan, M. M. & Nguyen, K. D. Diurnal sex differences in morphine withdrawal revealed by continuous assessment of voluntary home cage wheel running in the rat. Behav. Brain Res. 472, 115169. https://doi.org/10.1016/j.bbr.2024.115169 (2024).
Reddaway, J., Richardson, P. E., Bevan, R. J., Stoneman, J. & Palombo, M. Microglial morphometric analysis: so many options, so little consistency. Front. Neuroinform. 17, 1211188. https://doi.org/10.3389/fninf.2023.1211188 (2023).
Siemsen, B. M. et al. Chronic intermittent ethanol and lipopolysaccharide exposure differentially alter Iba1-derived microglia morphology in the prelimbic cortex and nucleus accumbens core of male Long-Evans rats. J. Neurosci. Res. 99, 1922–1939. https://doi.org/10.1002/jnr.24683 (2021).
Back, S. E. et al. Comparative profiles of men and women with opioid dependence: results from a National multisite effectiveness trial. Am. J. Drug Alcohol Abuse. 37, 313–323. https://doi.org/10.3109/00952990.2011.596982 (2011).
Muriel, J. et al. Long-term deprescription in chronic pain and opioid use disorder patients: Pharmacogenetic and sex differences. Acta Pharm. 73, 227–241. https://doi.org/10.2478/acph-2023-0018 (2023).
Cicero, T. J., Ennis, T., Ogden, J. & Meyer, E. R. Gender differences in the reinforcing properties of morphine. Pharmacol. Biochem. Behav. 65, 91–96. https://doi.org/10.1016/s0091-3057(99)00174-4 (2000).
Craft, R. M. Sex differences in analgesic, reinforcing, discriminative, and motoric effects of opioids. Exp. Clin. Psychopharmacol. 16, 376–385. https://doi.org/10.1037/a0012931 (2008).
Kimbrough, A. et al. Oxycodone self-administration and withdrawal behaviors in male and female Wistar rats. Psychopharmacol. (Berl). 237, 1545–1555. https://doi.org/10.1007/s00213-020-05479-y (2020).
Huhn, A. S., Tompkins, D. A., Campbell, C. M. & Dunn, K. E. Individuals with chronic pain who misuse prescription opioids report Sex-Based differences in pain and opioid withdrawal. Pain Med. 20, 1942–1947. https://doi.org/10.1093/pm/pny295 (2019).
Cicero, T. J., Nock, B. & Meyer, E. R. Sex-related differences in morphine’s antinociceptive activity: relationship to serum and brain morphine concentrations. J. Pharmacol. Exp. Ther. 282, 939–944 (1997).
Morgan, M. M. & Ataras, K. Sex differences in the impact of pain, morphine administration and morphine withdrawal on quality of life in rats. Pharmacol. Biochem. Behav. 219, 173451. https://doi.org/10.1016/j.pbb.2022.173451 (2022).
Brewer, A. L. et al. Modeling spontaneous opioid withdrawal in male and female outbred mice using traditional endpoints and hyperalgesia. Behav. Pharmacol. 34, 112–122. https://doi.org/10.1097/FBP.0000000000000714 (2023).
Blum, K., Eubanks, J. D., Wiggins, B. & Wallace, J. E. Morphine withdrawal reactions in male and female mice. Am. J. Drug Alcohol Abuse. 3, 363–368. https://doi.org/10.3109/00952997609077204 (1976).
Luster, B. R. et al. Inhibitory transmission in the bed nucleus of the stria terminalis in male and female mice following morphine withdrawal. Addict. Biol. 25, e12748. https://doi.org/10.1111/adb.12748 (2020).
el-Kadi, A. O. & Sharif, S. I. The influence of various experimental conditions on the expression of naloxone-induced withdrawal symptoms in mice. Gen. Pharmacol. 25, 1505–1510. https://doi.org/10.1016/0306-3623(94)90181-3 (1994).
Diaz, S. L., Kemmling, A. K., Rubio, M. C. & Balerio, G. N. Lack of sex-related differences in the prevention by Baclofen of the morphine withdrawal syndrome in mice. Behav. Pharmacol. 12, 75–79. https://doi.org/10.1097/00008877-200102000-00009 (2001).
Bobzean, S. A. M., Kokane, S. S., Butler, B. D. & Perrotti, L. I. Sex differences in the expression of morphine withdrawal symptoms and associated activity in the tail of the ventral tegmental area. Neurosci. Lett. 705, 124–130. https://doi.org/10.1016/j.neulet.2019.04.057 (2019).
Borbelyova, V., Janisova, K., Myslivecek, J. & Riljak, V. Sex-related differences in locomotion and climbing of C57Bl/6NTac mice in a novel environment. Physiol. Res. 68, S353–S359. https://doi.org/10.33549/physiolres.934348 (2019).
Diaz, S. L., Kemmling, A. K., Rubio, M. C. & Balerio, G. N. Morphine withdrawal syndrome: involvement of the dopaminergic system in prepubertal male and female mice. Pharmacol. Biochem. Behav. 82, 601–607. https://doi.org/10.1016/j.pbb.2005.10.012 (2005).
Dunn, K. E. et al. Operational definition of precipitated opioid withdrawal. Front. Psychiatry. 14, 1141980. https://doi.org/10.3389/fpsyt.2023.1141980 (2023).
Kanof, P. D. et al. Clinical characteristics of naloxone-precipitated withdrawal in human opioid-dependent subjects. J. Pharmacol. Exp. Ther. 260, 355–363 (1992).
Belknap, J. K. Components of the opioid withdrawal syndrome in mice are thermoregulatory responses. Pharmacol. Biochem. Behav. 34, 241–245. https://doi.org/10.1016/0091-3057(89)90306-7 (1989).
Thomas, J. H. L. et al. Toll-like receptors change morphine-induced antinociception, tolerance and dependence: studies using male and female TLR and signalling gene KO mice. Brain Behav. Immun. 102, 71–85. https://doi.org/10.1016/j.bbi.2022.02.001 (2022).
Navarro-Zaragoza, J. et al. Naloxone-induced conditioned place aversion score and extinction period are higher in C57BL/6J morphine-dependent mice than in swiss: role of HPA axis. Pharmacol. Biochem. Behav. 201, 173106. https://doi.org/10.1016/j.pbb.2021.173106 (2021).
Cobuzzi, J. L. & Riley, A. L. Spontaneous withdrawal in opiate-dependent Fischer 344, Lewis and Sprague-Dawley rats. Pharmacol. Biochem. Behav. 98, 28–34. https://doi.org/10.1016/j.pbb.2010.12.003 (2011).
Sadeghi, M. et al. Study of morphine-induced dependence in gonadectomized male and female mice. Pharmacol. Biochem. Behav. 91, 604–609. https://doi.org/10.1016/j.pbb.2008.09.015 (2009).
Broida, J. & Svare, B. Sex differences in the activity of mice: modulation by postnatal gonadal hormones. Horm. Behav. 18, 65–78. https://doi.org/10.1016/0018-506x(84)90051-5 (1984).
Hsu, H. T. et al. Hyperbaric oxygen therapy improves Parkinson’s disease by promoting mitochondrial biogenesis via the SIRT-1/PGC-1alpha pathway. Biomolecules. https://doi.org/10.3390/biom12050661 (2022).
Wee, H. Y. et al. Hyperbaric oxygen effects on neuronal apoptosis associations in a traumatic brain injury rat model. J. Surg. Res. 197, 382–389. https://doi.org/10.1016/j.jss.2015.04.052 (2015).
Carlile, E. L., Shirachi, D. Y. & Quock, R. M. An anxiolytic-like effect of hyperbaric oxygen in the mouse light/dark exploration test. Life Sci. 90, 267–271. https://doi.org/10.1016/j.lfs.2011.11.010 (2012).
Peng, Y. et al. Hyperbaric oxygen preconditioning ameliorates anxiety-like behavior and cognitive impairments via upregulation of thioredoxin reductases in stressed rats. Prog Neuropsychopharmacol. Biol. Psychiatry. 34, 1018–1025. https://doi.org/10.1016/j.pnpbp.2010.05.016 (2010).
Sturman, O., Germain, P. L. & Bohacek, J. Exploratory rearing: a context- and stress-sensitive behavior recorded in the open-field test. Stress 21, 443–452. https://doi.org/10.1080/10253890.2018.1438405 (2018).
Pantazis, C. B. et al. Cues conditioned to withdrawal and negative reinforcement: neglected but key motivational elements driving opioid addiction. Sci. Adv. 7 https://doi.org/10.1126/sciadv.abf0364 (2021).
Hutcheson, D. M., Everitt, B. J., Robbins, T. W. & Dickinson, A. The role of withdrawal in heroin addiction: enhances reward or promotes avoidance? Nat. Neurosci. 4, 943–947. https://doi.org/10.1038/nn0901-943 (2001).
Koob, G. F. Dynamics of neuronal circuits in addiction: reward, antireward, and emotional memory. Pharmacopsychiatry 42 (Suppl 1), 32–41. https://doi.org/10.1055/s-0029-1216356 (2009).
Vafaie, N. & Kober, H. Association of drug cues and craving with drug use and relapse: A systematic review and Meta-analysis. JAMA Psychiatry. 79, 641–650. https://doi.org/10.1001/jamapsychiatry.2022.1240 (2022).
Reiner, D. J. et al. Relapse to opioid seeking in rat models: Behavior, pharmacology and circuits. Neuropsychopharmacology https://doi.org/10.1038/s41386-018-0234-2 (2018).
Reiss, D., Maduna, T., Maurin, H., Audouard, E. & Gaveriaux-Ruff, C. Mu opioid receptor in microglia contributes to morphine analgesic tolerance, hyperalgesia, and withdrawal in mice. J. Neurosci. Res. 100, 203–219. https://doi.org/10.1002/jnr.24626 (2022).
McDevitt, D. S. et al. The paraventricular thalamic nucleus and its projections in regulating reward and context associations. eNeuro 11 (2024). https://doi.org/10.1523/ENEURO.0524-23.2024
Matzeu, A., Zamora-Martinez, E. R. & Martin-Fardon, R. The paraventricular nucleus of the thalamus is recruited by both natural rewards and drugs of abuse: recent evidence of a pivotal role for orexin/hypocretin signaling in this thalamic nucleus in drug-seeking behavior. Front. Behav. Neurosci. 8, 117. https://doi.org/10.3389/fnbeh.2014.00117 (2014).
Giannotti, G. et al. Extinction blunts paraventricular thalamic contributions to heroin relapse. Cell. Rep. 36, 109605. https://doi.org/10.1016/j.celrep.2021.109605 (2021).
Do-Monte, F. H., Minier-Toribio, A., Quinones-Laracuente, K., Medina-Colon, E. M. & Quirk, G. J. Thalamic Regulation of Sucrose Seeking during Unexpected Reward Omission. Neuron 94, 388–400 e384. https://doi.org/10.1016/j.neuron.2017.03.036 (2017).
Cragg, A. et al. Risk factors for misuse of prescribed opioids: A systematic review and Meta-Analysis. Ann. Emerg. Med. 74, 634–646. https://doi.org/10.1016/j.annemergmed.2019.04.019 (2019).
Hser, Y. I. et al. Chronic pain among patients with opioid use disorder: results from electronic health records data. J. Subst. Abuse Treat. 77, 26–30. https://doi.org/10.1016/j.jsat.2017.03.006 (2017).
Carcoba, L. M., Contreras, A. E., Cepeda-Benito, A. & Meagher, M. W. Negative affect heightens opiate withdrawal-induced hyperalgesia in heroin dependent individuals. J. Addict. Dis. 30, 258–270. https://doi.org/10.1080/10550887.2011.581985 (2011).
Moore, B. A. et al. Cognitive behavioral therapy improves treatment outcomes for prescription opioid users in primary care buprenorphine treatment. J. Subst. Abuse Treat. 71, 54–57. https://doi.org/10.1016/j.jsat.2016.08.016 (2016).
Abuse, N. I. D. Treatment and Recovery (2020). https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
Zylstra, C. C. et al. Role of nitric oxide (NO) in the hyperbaric oxygen (HBO2)-induced long‐lasting activation of endogenous opioid systems in mice. FASEB J. 22 https://doi.org/10.1096/fasebj.22.1_supplement.711.17 (2008).
Chung, E., Zelinski, L. M., Ohgami, Y., Shirachi, D. Y. & Quock, R. M. Hyperbaric oxygen treatment induces a 2-phase antinociceptive response of unusually long duration in mice. J. Pain. 11, 847–853. https://doi.org/10.1016/j.jpain.2009.12.004 (2010).
Brewer, A. L., Shirachi, D. Y. & Quock, R. M. Evaluation of hyperbaric oxygen (HBO2) as a treatment for hyperalgesia associated with naloxone-precipitated withdrawal in morphine‐dependent mice. FASEB J. 32 https://doi.org/10.1096/fasebj.2018.32.1_supplement.683.4 (2018).
Gibbons, C. R. et al. Involvement of brain opioid receptors in the anti-allodynic effect of hyperbaric oxygen in rats with sciatic nerve crush-induced neuropathic pain. Brain Res. 1537, 111–116. https://doi.org/10.1016/j.brainres.2013.08.050 (2013).
Quock, L. P. et al. The acute antinociceptive effect of HBO(2) is mediated by a NO-cyclic GMP-PKG-KATP channel pathway in mice. Brain Res. 1368, 102–107. https://doi.org/10.1016/j.brainres.2010.10.079 (2011).
Zelinski, L. M., Ohgami, Y., Chung, E., Shirachi, D. Y. & Quock, R. M. A prolonged nitric oxide-dependent, opioid-mediated antinociceptive effect of hyperbaric oxygen in mice. J. Pain. 10, 167–172. https://doi.org/10.1016/j.jpain.2008.08.003 (2009).
Kiralp, M. Z. et al. Effectiveness of hyperbaric oxygen therapy in the treatment of complex regional pain syndrome. J. Int. Med. Res. 32, 258–262. https://doi.org/10.1177/147323000403200304 (2004).
Acknowledgements
The authors would like to thank Yujia (Henry) Hu for LabGym tutorials and undergraduate students Charlotte Malcolm, Meghan Kerr, Amaya Sims, and Scott Briggs for assistance with behavioral experiments.
Funding
The authors declare no competing financial interests. This investigation was supported in part by the Washington State University Psychology Excellence Fund and funds provided for medical and biological research by the State of Washington Initiative Measure No. 171 (grant awarded to Meg Southard). In addition, WSU startup funds (Dr. Brown) and accrual funds (Dr. Quock).
Author information
Authors and Affiliations
Contributions
M.T.S., R.M.Q., and T.E.B designed the research. M.T.S. conducted all experiments. T.R.W. and L.G.B. made significant contributions to behavioral experiments. A.T. imaged microglia. G.G. and F.S. analyzed microglia data. M.T.S., T.E.B., and G.G. analyzed data. M.T.S., T.E.B, and G.G. wrote the manuscript. M.T.S., R.M.Q., T.E.B., G.G., and S.H. made significant intellectual contributions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Southard, M.T., Giannotti, G., Thakar, A. et al. Hyperbaric oxygen treatment attenuates naloxone-precipitated opioid withdrawal behaviors and alters microglial activity in male and female mice. Sci Rep 15, 23677 (2025). https://doi.org/10.1038/s41598-025-07937-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07937-z