Abstract
Substance use disorders (SUDs) among adolescents and young adults aged 10–24 years represent a major global public health challenge, contributing to various medical conditions and significant disease burden. This study analyzed global, regional, and national estimates of the SUD burden within this demographic from 1990 to 2021. Using data from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2021, we analyzed incidence, prevalence, mortality, and disability-adjusted life-years (DALYs) of SUDs among population aged 10–24 years. SUDs in GBD 2021 encompass alcohol and drug use disorders. We calculated age-standardized rates (per 100,000 population) for incidence (ASIR), prevalence (ASPR), mortality (ASMR), and DALYs (ASDR). Health inequalities were assessed using the slope index of inequality (SII) and concentration index. Risk factors were also analyzed. Statistical analyses were performed in R (v4.4.1). In 2021, the global ASIR and ASPR of SUDs among population aged 10–24 years were 614.0 (95% CI 467.6–805.0) and 1557.0 (1234.1–1944.6) per 100,000 population. Substance-specific ASPRs in 2021 included alcohol (651.9, 95% CI 439.0–941.7), cannabis (536.8, 343.5–831.8), opioid use disorders (155.0, 120.0–199.7), etc. The global ASMR and ASDR for SUDs were 1.1 (1.0 to 1.2) and 228.9 (172.4–295.3). From 1990 to 2021, ASIR (average annual percent change [AAPC] − 0.70, 95% CI − 0.71 to − 0.69), ASPR (AAPC − 0.71, − 0.72 to − 0.70), and ASDR (AAPC − 0.60, − 0.63 to − 0.56) declined globally, while ASMR increased (AAPC 0.83, 0.52–1.23). During the COVID-19 pandemic (2019–2021), ASIR and ASPR decreased, ASDR remained stable, and ASMR rose. Substantial disparities were observed across regions and countries and territories. Males, older adolescents, and populations in higher socio-demographic index (SDI) regions exhibited disproportionately higher SUD burden. SUDs impose a significant health burden on adolescents and young adults aged 10–24 years, with distinct demographic and geographic inequities. Evidence-based interventions should prioritize male populations, older age groups, and the high-SDI regions. Lower-SDI regions require enhanced monitoring to address evolving epidemiological trends. Urgent implementation of targeted prevention and treatment strategies is critical to mitigate the impact of SUDs in this vulnerable population.
Similar content being viewed by others
Introduction
Substance use disorders (SUDs), defined as maladaptive patterns of psychoactive substance use that impair neurological function and overall health1, represent a critical public health challenge among adolescents and young adults (aged 10–24 years). Since the inception of the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) in the 1990s, SUDs have been increasingly recognized as a major contributor to global morbidity, with onset predominantly occurring during adolescence2,3,4. Early initiation of substance use progresses to chronic disorders characterized by high relapse rates and psychiatric comorbidities5, positioning SUDs among the leading preventable health risks for youth worldwide6,7. Affected individuals face elevated risks of physical and mental health comorbidities, neurocognitive impairment, and progression to severe addiction8,9. Acute consequences include injuries, violence, and high-risk sexual behaviors, while chronic outcomes involve disrupted educational attainment, reduced economic productivity, criminal justice involvement, and premature mortality10,11. These multidimensional impacts underscore the necessity of understanding age-specific SUD epidemiology to inform lifespan-oriented prevention and treatment strategies.
The etiology of SUDs involves multifactorial interactions across biological, psychological, and social domains. Adolescence and young adulthood encompass rapid neurodevelopmental and psychosocial transitions12,13,14, rendering this population uniquely vulnerable to SUD-related harm. Mental health conditions, particularly depression, anxiety, and post-traumatic stress disorder (PTSD), demonstrate bidirectional relationships with SUDs8,15,16. Familial factors, including intergenerational substance use, parental neglect, and high-conflict households, amplify susceptibility by fostering maladaptive coping mechanisms17,18. Environmental stressors such as socioeconomic deprivation, neighborhood substance availability, peer influence, and chronic adversity further exacerbate vulnerability by dysregulating stress responses and limiting healthcare access15,19. Gene-environment interactions modulate risk trajectories; for instance, genetic predispositions to impulsivity or reward sensitivity synergize with childhood adversity to accelerate SUD progression20,21,22.
The GBD framework provides unparalleled capacity to analyze SUD burden across developmental stages23,24. Despite calls for finer age stratification in youth health research12,13, few studies have utilized GBD 2021 data to examine SUD epidemiology across the 10–24-year age range. This study addresses this gap by analyzing incidence, prevalence, mortality, and disability-adjusted life years (DALYs) attributable to SUDs in three developmental subgroups: early adolescence (10–14 years), late adolescence (15–19 years), and young adulthood (20–24 years). Analysis based on these short developmental intervals could provide a detailed examination of this life phase13. By elucidating trends and disparities of SUD burden, as well as risk factors reported in GBD 2021, our findings aim to guide targeted policy interventions and healthcare resource allocation for this vulnerable population.
Methods
Data source
The GBD 2021 study estimated the prevalence, incidence, mortality, and DALYs for 371 diseases and injuries across 204 countries and territories using nationally representative data from vital registration systems, censuses, household surveys, disease registries, and health service encounters6. Detailed methodological protocols including modeling processes are described in the GBD 2021 publication6,25. Epidemiological estimates were processed and adjusted for reporting biases and missing data by the GBD collaborators using DisMod-MR 2.1, a Bayesian meta-regression tool that harmonizes data across sources6.
SUDs in GBD 2021 comprise two categories: alcohol use disorders and drug use disorders. The latter encompasses opioid, cocaine, amphetamine, cannabis, and other drug use disorders. Corresponding ICD-10 codes were provided in Table S1. We extracted age-stratified data (10–24 years) on case counts, rates (per 100,000 population), and corresponding 95% uncertainty intervals (UIs) for incidence, prevalence, mortality, and DALYs from 1990 to 2021. Risk factors contributing to SUD-associated DALYs were also analyzed. All estimates analyzed in this work were sourced from the Global Health Data Exchange (GHDx; http://ghdx.healthdata.org/gbd-results-tool) developed by the GBD collaborators. This study adheres to the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER)26. Ethical approval was waived by Guang’anmen Hospital, China Academy of Chinese Medical Sciences, as the study utilized deidentified, publicly available data.
Definition
This study analyzed four key measures6: incidence, prevalence, mortality, and DALYs, all reported as number and age-standardized rates (ASRs). Incidence refers to the annual new cases; prevalence represents the total number of existing cases; mortality refers to the number of deaths attributed to SUDs; DALYs quantify the total burden of disease by combining years of life lost due to premature mortality (YLLs) and years lived with disability (YLDs). Adolescence (10–19 years) and young adulthood (20–24 years) were analyzed as per WHO definitions27,28, with subgroups of early (10–14 years) and late adolescence (15–19 years)28,29.
All estimates were stratified by sex, age, and geographic location for the period 1990–2021. Analyses utilized the GBD 2021 framework, which classifies data across 21 regions and 204 countries and territories into quintiles of the Sociodemographic Index (SDI). The SDI, a composite measure developed by the GBD collaboration, reflects national socioeconomic development through three components: lag-distributed income per capita, educational attainment (average years of schooling for individuals ≥ 15 years), and fertility rates among females < 25 years6. Calculated as the geometric mean of normalized indices with 0 indicating theoretical minimum and 1 indicating theoretical maximum, SDI values for all GBD locations are publicly accessible via the Institute for Health Metrics and Evaluation (https://ghdx.healthdata.org/gbd-2021).
Statistical analysis
For the 10–24-year population, we computed ASRs per 100,000 population for incidence (ASIR), prevalence (ASPR), mortality (ASMR), and DALYs (ASDR) with 95% confidence intervals (CIs) using direct standardization with the GBD 2021 world standard population6. Age-specific rates were analyzed for three subgroups, i.e. 10–14, 15–19, and 20–24 years.
The first objective of this study was to evaluate global, regional, and national trends in SUD-related incidence, prevalence, mortality, and DALYs from 1990–2021. We computed ASRs and their average annual percentage changes (AAPCs) with 95% CIs via log-linear regression with rates as dependent variable and year as independent variable30. The AAPC, a weighted average of annual percentage changes (APCs), quantifies secular trends, where geometrically weighted APCs derived from regression coefficients describe yearly fluctuations31. For instance, an AAPC of 0.1 indicates a 0.1% annual increase. However, the AAPC may not capture non-linear short-term fluctuations occurring within a single segment. All AAPC values were reported to two decimal places to capture subtle temporal variations32.
The second objective was to identify inflection points in global trend trajectories using Joinpoint Regression analysis. This method iteratively fits segmented log-linear models using Monte Carlo permutation testing31. Final model selection combined expert adjudication and Weighted Bayesian Information Criterion optimization30.
The third objective was to examine sex-, age-, and SDI-specific disparities in SUD burden patterns. Health inequity metrics, slope index of inequality (SII) and concentration index, were calculated following the Handbook on Health Inequality Monitoring developed by the World Health Organization33. The SII is zero if there is no inequality, with greater absolute values indicating higher levels of inequality. SII values > 0 denote burden concentration in advantaged populations, while negative values indicate burden concentration in disadvantaged-group. The concentration index ranges from − 1 to 1, with larger absolute values signifying greater inequality. The sign of the index (positive or negative) indicates the direction of the disease burden distribution, consistent with the SII. All statistical analyses were performed using R software (v4.4.1)34, with P < 0.05 defining statistical significance.
Results
Global trends
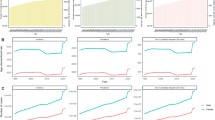
From 1990 to 2021, global estimates for SUD burden demonstrated declining trends in incidence, prevalence, and DALYs among adolescents and young adults aged 10–24 years. The number of incidence cases decreased insignificantly from 12.0 million (95% UI 9.1–15.8) in 1990 to 11.7 million (8.9–15.3) in 2021 (Fig. S1, Table S2). The ASIR declined from 764.6 (95% CI 577.0–1004.0) to 614.0 (467.6–805.0) per 100,000 population (AAPC − 0.70; 95% CI − 0.71 to − 0.69), with significant inflection points identified in 1993, 2003, 2006, 2009, and 2014 (Fig. 1A). Similarly, the prevalence of SUDs decreased from 30.5 million (95% UI 24.2–38.3) to 29.7 million (23.6–37.1) during this period (Table 1). The ASPR declined from 1937.1 (95% CI 1535.9–2430.4) to 1557.0 (1234.1–1944.6) per 100,000 population (AAPC − 0.71, − 0.72 to − 0.70) (Tables 1 and 2), marked by notable shifts in 1993, 2005, 2009, 2015, and 2019 (Fig. 1B).
Joinpoint regression analysis of global age-standardized rates for SUDs in adolescents and young adults aged 10–24 years, 1990–2021 (both sexes): (A) ASIR, (B) ASPR, (C) ASMR, and (D) ASDR. AAPC, average annual percentage change; APC, annual percentage change; ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life-years; SUDs, substance use disorders.
While mortality attributed to SUDs decreased numerically from 14,621.9 (95% UI 13,371.0–16,011.6) in 1990 to 13,659.2 (12,810.8–14,531.8) in 2021, the ASMR exhibited an upward trajectory (AAPC 0.83, 0.52–1.23), rising from 0.9 (95% CI 0.9–1.0) in 1990 to 1.1 (1.0–1.2) per 100,000 population in 2021 (Tables 1 and S3). Significant trend deviations occurred in 1994, 2006, 2012, and 2019 (Fig. 1C). DALYs remained stable at 4.4 million (95% UI 3.3–5.7 in 1990; 3.3–5.6 in 2021), though ASDR declined from 275.7 (95% CI 206.0–359.1) to 228.9 (172.4–295.3) per 100,000 population (AAPC − 0.60, − 0.63 to − 0.56) (Table 1 and S4), with inflection points in 1994, 2000, 2006, 2009, and 2013 (Fig. 1D).
During the COVID-19 pandemic (2019–2021), global ASMR surged (APC = 28.5), whereas ASIR and ASPR continued declining, and ASDR remained relatively stable (Fig. 1). The GBD 2021 data demonstrated significant reductions in both case numbers (− 0.02, 95% UI − 0.03 to − 0.01) and crude rates (− 0.03, 95% UI − 0.04 to − 0.02) of prevalence from 2019 to 2021. A comparable decline was observed in crude incidence rates (− 0.03, 95% UI − 0.04 to − 0.02). Details are presented in Tables S5 and S6. No statistically significant temporal changes were identified in mortality or DALYs during this period.
Subtype-specific analyses revealed diverging patterns. For alcohol use disorders, global ASIR and ASPR declined steadily since 1993, while ASMR decreased until 2018 before rising through 2021 (Fig. S2). The ASDR for alcohol use disorders has been decreasing since 2000 (Fig. S2). Drug use disorders displayed a triphasic trajectory: ASIR and ASPR decreased from 1990 to 2015, increased until 2019, then declined again (Fig. S3). ASMR and ASDR for drug use disorders rose consistently from 2011 and 2014 onward, respectively.
Regional trends
Comprehensive data on regional ASIR, ASPR, ASMR, and ASDR, along with their AAPCs, were detailed in Tables 1, S2–S4 and S7, and illustrated in Fig. 2 and 3. In 2021, high-income North America recorded the highest ASIR, ASPR, ASMR, and ASDR for SUDs among adolescents and young adults aged 10–24 years among the 21 GBD regions.
Age-standardized rates of SUDs in adolescents and young adults aged 10–24 years at the global level and across 21 GBD regions, 1990–2021 (both sexes): (A) ASIR, (B) ASPR, (C) ASMR, and (D) ASDR. ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life-years; SUDs, substance use disorders.
Sex-stratified AAPCs in age-standardized rates of SUDs in adolescents and young adults aged 10–24 years from 1990 to 2021, at the global level, across five SDI quintiles, and in 21 GBD regions: (A) ASIR, (B) ASPR, (C) ASMR, and (D) ASDR. Note: Dark red text denotes the global level and five SDI quintiles, while black text indicates 21 GBD regions. AAPCs, average annual percent changes; ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life-years; SDI, socio-demographic index; SUDs, substance use disorders.
Significant increases in ASIR were observed in North Africa and the Middle East, Oceania, and Southern Latin America based on AAPC estimates, while declining or statistically negligible trends were noted in other GBD regions (Fig. 3, Tables S2 and S7). Upward ASPR trends were evident in the Caribbean, high-income North America, North Africa and the Middle East, Oceania, Southeast Asia, and Southern Latin America. In contrast, Central Latin America, Eastern Sub-Saharan Africa, and Western Sub-Saharan Africa showed no significant changes, while other regions exhibited declines (Fig. 3, Tables 1 and S7).
Rising ASMR trajectories were identified in regions including the Caribbean, high-income North America, Southern Latin America, Tropical Latin America, and Western Sub-Saharan Africa. No significant change in ASMR was detected in Central Europe, Central Latin America, Central Sub-Saharan Africa, or Eastern Europe (Fig. 3, Tables S3 and S7). Notable ASDR increases occurred in regions such as Central Sub-Saharan Africa, high-income North America, North Africa and the Middle East, Oceania, and Tropical Latin America. Central Europe, Eastern Sub-Saharan Africa, and Southern Latin America displayed stable trends, whereas other regions experienced declines (Fig. 3, Tables S4 and S7).
National trends
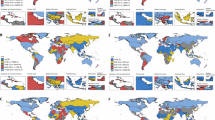
Detailed estimates for SUD burden metrics across 204 countries and territories in 2021 are presented in Tables S8–S11, with spatial distributions visualized in Fig. S4. AAPCs were visualized in Fig. 4.
Geospatial distribution of AAPCs in age-standardized rates of SUDs among adolescents and young adults aged 10–24 years, 1990–2021 (both sexes): (A) ASIR, (B) ASPR, (C) ASMR, and (D) ASDR. Note: Maps illustrate epidemiological transitions and disease burden patterns without implying political or territorial boundaries. The figure was generated using sf and ggplot2 packages in R software (v4.4.1) (https://www.r-project.org/). AAPCs, average annual percent changes; ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life years; SUDs, substance use disorders.
In 2021, the United States recorded the highest ASPR, ASMR, and ASDR, while Greenland exhibited the highest ASIR (Tables S8–S11). Among 66 countries and territories, ASIR for both sexes demonstrated upward trends, with Mongolia (AAPC 1.14, 95% CI 1.12–1.17) and Iran (AAPC 0.73, 0.71–0.74) showing the most pronounced increases. Conversely, Uzbekistan (AAPC − 1.24, − 1.26 to − 1.21) and India (AAPC − 1.22, − 1.28 to − 1.16) experienced the steepest declines; 16 countries and territories displayed statistically insignificant changes (Table S8). For ASPR, 73 countries exhibited increasing trends, led by Iran (AAPC 1.01, 0.98–1.04) and Mongolia (AAPC 1.00, 0.98–1.02). Australia (AAPC − 1.18, − 1.22 to − 1.15) and India (AAPC − 1.08, − 1.20 to − 0.99) demonstrated the most substantial reductions, with 7 countries and territories reporting non-significant shifts (Table S9).
ASMR increases were observed in 82 countries and territories, most notably in the United States (AAPC 6.76, 95% CI 6.58–6.91) and Canada (AAPC 5.92, 5.70–6.11). In contrast, Guam (AAPC − 6.76, − 7.52 to − 5.92) and Italy (AAPC − 5.92, − 6.16 to − 5.64) had the sharpest declines among 99 countries and territories, while 23 countries and territories displayed stable trends (Table S10). ASDR rose in 95 countries and territories, with the United States (AAPC 3.04, 3.00–3.07) and Sweden (AAPC 2.00, 1.94–2.04) at the forefront. Conversely, Switzerland (AAPC − 2.22, − 2.26 to − 2.18) and China (AAPC − 1.94, − 1.98 to − 1.89) led declines across 87 countries and territories; 22 countries and territories showed no significant changes (Table S11).
Global and SDI regional trends by sex and age subgroup
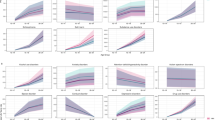
Globally and across all SDI regions, males consistently demonstrated higher ASRs than females for all four measures from 1990 to 2021 (Fig. 5). The global ASIR and ASPR increased more sharply in males compared to females. For ASMR diverged by sex, males exhibited an upward trend, while females showed a decline. Additionally, ASDR decreased faster in females than males (Table 2). Across all measures, ASRs escalated with age, peaking in the 20–24-year cohort, followed by 15–19-year and 10–14-year groups (Fig. 6).
Temporal trends in sex-stratified ASIR, ASPR, ASMR, and ASDR for SUDs in adolescents and young adults aged 10–24 years at the global level and by SDI quintile, 1990–2021, by sex. ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life-years; SDI, socio-demographic index; SUDs, substance use disorders.
SUD subtypes
Both alcohol and drug use disorders showed parallel reductions in ASIR, ASPR, ASMR, and ASDR (Tables 1–2 and S2–S4; Fig. S5). From 1990 to 2021, the global ASIR of alcohol use disorders declined from 493.3 (95% CI 328.3–734.0) to 375.7 (250.0–555.9), with an AAPC of − 0.87 (− 0.89 to − 0.85). Drug use disorders also decreased, with ASIR falling from 271.3 (205.6–353.1) to 238.3 (179.4–315.4; AAPC − 0.43, 95% CI − 0.46 to − 0.41). Cannabis use disorders dominated global and SDI-specific ASIR and ASPR across all drug subtypes (Fig. 7). Notably, opioid use disorders surged in ASIR, ASPR, ASMR, and ASDR within high-SDI regions. In 2021, incident cases comprised alcohol (61.3%), cannabis (20.6%), opioids (8.0%), amphetamines (5.4%), cocaine (1.5%), and other substances (3.2%) (Fig. 8). Notably, males exhibited higher ASRs than females across all substance types (Fig. S5–S6).
Age- and SDI-stratified trends in ASIR, ASPR, ASMR, and ASDR of specific drug use disorders (cannabis, opioids, amphetamines, cocaine, and others) in adolescents and young adults aged 10–24 years, 1990–2021 (both sexes). ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life-years; SDI, socio-demographic index.
Proportional contributions of specific SUD subtypes to numbers of global incidence, prevalence, mortality, and DALYs of SUDs among adolescents and young adults aged 10–24 years in 2021 (both sexes). ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized rate of DALYs; DALYs, disability-adjusted life-years; SUD, substance use disorder.
SDI correlation and health inequality
Regional and national disease burden estimates correlated strongly with SDI (Fig. 2 and Fig. S7). The SII and concentration index for ASDR across 204 countries and territories from 1990 to 2021 indicated disproportionate burden clustering in high-SDI settings (Fig. S8).
Risk factors attributions
Globally, adolescents and young adults with SUD faced three behavioral risk factors contributing to DALYs: drug use, high alcohol consumption, and childhood sexual abuse. Among these, drug use is the predominant risk factor, high alcohol consumption ranks second, and childhood sexual abuse accounted for a minor proportion of DALYs (Fig. S9).
Discussion
SUDs typically begin during adolescence and young adulthood, a neurodevelopmental period characterized by heightened vulnerability to substance reinforcement due to peer influence and incomplete maturation of prefrontal cortical circuits that regulate executive function and impulse control35. Longitudinal analysis of 11 cohorts from the Monitoring the Future study funded by U.S. National Institute on Drug Abuse revealed persistent trajectories: individuals with severe adolescent SUDs frequently retained ≥ 2 symptoms by midlife, with the highest adolescent severity predicting prescription drug misuse decades later36. The early-life onset and enduring consequences of SUDs underscore the necessity for updated epidemiological study, developmentally targeted prevention and early intervention strategies5,15.
This study delineates the global, regional, and national burdens of SUDs among adolescents and young adults aged 10–24 years from 1990 to 2021, capturing incidence, prevalence, mortality, and DALYs. Our findings align with prior evidence of a persistent, albeit declining, SUD burden in this population over the past three decades3,4,37,38,39. In 2021, aggregated estimates revealed approximately 11.7 million new SUD cases (6.0 per 1,000 population) and 29.7 million prevalent cases (15.6 per 1,000 population) among individuals aged 10–24 years globally. SUDs accounted for approximately 13,000 deaths and 4.4 million DALYs, ranking as the 20th leading contributor to DALYs among level 2 causes in the GBD classification in this age group. Alcohol use disorders contributed 1.4 million DALYs (level 3 causes rank: 48th), while drug use disorders accounted for 2.9 million DALYs (level 3 causes rank: 28th). Non-fatal disability burden was substantial. SUDs accounted for 3.4 million YLDs, ranking as the 12th leading contributor among Level 2 causes. This burden surpassed that of chronic respiratory diseases, enteric infections, and cardiovascular diseases. In addition, the GBD 2021 study identified three key risk factors for SUDs: drug use, high alcohol use, and childhood sexual abuse.
Early reports suggested increased substance use during the COVID-19 pandemic40, yet our analysis demonstrates declining ASIR and ASPR rates among 10–24-year-olds from 2019 to 2021, alongside stable ASDR trends. This parallels the U.S. Monitoring the Future survey, which documented unprecedented reductions in youth substance use in 202139. Moreover, the lowered levels of drug use after the pandemic were lasting through 202439. Sustained declines suggest pandemic-related disruptions, such as delayed substance initiation, reduced peer-group recruitment, and altered social dynamics, may yield long-term protective effects39. These shifts underscore the need to elucidate mechanisms driving both initial declines and their persistence, informing policies to disrupt youth substance use trajectories39.
Sex disparities persisted, with males exhibiting twice the ASIR (824.8 vs. 394.4 per 100,000 population) and ASDR (296.6 vs. 158.6 per 100,000 population) of females in 2021. These findings align with prior evidence of elevated rates of alcohol and drug use disorders in males41 and male predominance in substance-related emergency care or overdose mortality42. The observed disparities likely arise from interacting biological, psychosocial, and environmental mechanisms43. Delayed maturation of the male prefrontal cortex during adolescence may impair impulse control, increasing vulnerability to risk-taking behaviors43,44. Testosterone-mediated enhancement of dopaminergic neurotransmission may heighten reward sensitivity, promoting addictive behaviors45. Moreover, cultural constructs reinforcing male risk-taking through peer influence or media narratives may drive higher engagement in illicit substances46,47. Gender-responsive strategies including male-targeted prevention programs, stigma reduction, sex-stratified biomarker research, and longitudinal cohort analyses to identify risk pathways may be critical.
Age-specific patterns revealed escalating burdens with older cohorts. In 2021, global ASIR for 15–19-year-olds (682.3 per 100,000 population) exceeded rates in 10–14-year-olds (120.9 per 100,000 population) by fivefold, while 20–24-year-olds (1,109.9 per 100,000 population) surpassed the 10–14-year-olds by ninefold. This gradient, consistent across SDI quintiles, reflects neurodevelopmental and contextual shifts during adolescence and young adulthood. Early adolescence (10–14 years) may confer protection through limited substance access, whereas older cohorts face heightened risks from reward-system maturation, social-environmental exposures, and autonomy in high-risk settings5,15. Regional SDI disparities may further modulate risks via variable healthcare access and prevention infrastructure.
High SDI regions bore disproportionate burdens, with the high SDI quintile contributing 24.2% of global SUD incidence and 36.8% of DALYs in 2021. High-income North America alone accounted for 13.3% of incidence and 27.3% of DALYs. The SII and concentration indices confirmed this inequality, which aligns with prior GBD studies on SUDs48,49,50. High-income countries often exhibit greater SUD burden, which may be due to better healthcare access, higher purchasing power for substances, and cultural normalization of alcohol and drug use. In addition, higher SUD burden in high-income North America may also be attributable to opioid epidemics and cannabis legalization51. This contrasts with lower-SDI regions where underreporting persists which might be due to inadequate resources and limited surveillance systems52.
National surveillance efforts must prioritize countries with both the highest current SUD burdens and those experiencing marked incidence growth, as under-resourced nations remain particularly vulnerable to SUD-related public health crises. In 2021, Mongolia, Iran, Estonia, Samoa, Finland, New Zealand, Colombia, and Lebanon documented marked upticks in adolescent and young adult SUD incidence, underscoring the imperative for immediate intervention in these epidemiologically vulnerable settings.
Alcohol and cannabis dominated subtype burdens, though opioid disorders surged in high-SDI areas, which is consistent with prior research5,53. The multisystem harms of alcohol use disorders spanning hepatic, cardiovascular, oncologic, and psychiatric sequelae53, underscore the need for age-tailored prevention. Despite policy successes such as taxation, age limits for purchase, and marketing restrictions54,55, alcohol remains a leading contributor to early-life SUDs. Cannabis use disorders correlate with pulmonary sequelae56 and aberrant neurodevelopment in reward-processing, executive function, and attentional networks57,58. Heavy adolescent cannabis use impairs memory, learning, attention, and higher-order cognition59. A meta-analysis of 63 studies and 438,329 participants linked adolescent and young adult cannabis use to adverse educational outcomes including school absenteeism, reduced graduation rates, and diminished postsecondary attainment, as well as elevated unemployment risk60. Opioid-related harms extend beyond dependency: injection practices propagate bacterial infections and blood-borne viruses such as HIV and hepatitis C61, while opioid use itself induces nausea, constipation, hyperalgesia, and hypothalamic–pituitary–adrenal axis suppression53.
Sex, age, and region disparities in SUD burden underscore the imperative for sex-, age-and region- stratified management strategies. Urgent implementation of evidence-based prevention strategies is critical, particularly interventions to deter substance initiation in adolescents and young adults and prevent progression from experimental to addictive use5,15. First-line SUD therapies for adolescents and young adults emphasize family-based interventions, cognitive-behavioral therapy (CBT), and multicomponent programs integrating motivational interviewing (MI) and contingency management5,62. Clinicians, caregivers, guardians, and policymakers must collaborate to enhance early detection and prompt intervention. Policy priorities may include12,15,62,63,64: (1) school-based resilience programs targeting behavioral regulation and substance refusal skills for early adolescents; (2) implement of peer-delivered brief interventions integrated with digital follow-up systems; (3) community-driven harm reduction initiatives for older adolescents and young adults with established SUDs; (4) enhanced prescription drug monitoring coupled with pharmacist-led patient education; (5) development of gender-responsive interventions, particularly male-focused programs; (6) national surveillance systems reporting age-, sex-, and geography-stratified SUD outcomes to enable real-time policy optimization. Cross-sectoral integration of healthcare, education, and social services is essential for sustained impact.
The GBD 2021 dataset imposes inherent limitations. First, reliance on modeled estimates and data imputation for regions with sparse epidemiological surveillance may obscure local variations and underreporting, particularly in low-resource settings with weak surveillance systems. Second, global SUD rates in adolescents and young adults likely represent underestimates due to diagnostic and reporting biases. Third, exclusion of gender minorities in GBD study reduces generalizability. Fourth, our reliance on the GBD database excludes other relevant global data sources, such as the WHO Global Health Estimates. Future studies should update relevant epidemiological studies, strengthen epidemiological monitoring through multisource data integration, and evaluate effectiveness of early detection and intervention programs.
Conclusions
SUDs constitute a critical yet frequently underrecognized public health challenge among adolescents and young adults aged 10–24 years. In 2021, an estimated 29.7 million individuals in this age group were affected by SUDs, primarily alcohol, cannabis, and opioid use disorders, with disproportionately higher burdens observed in socioeconomically developed regions. Males and older individuals faced elevated risks. The GBD 2021 estimates highlight the imperative for life-course-oriented prevention and early intervention strategies. Prioritizing school-based substance use education and implementing routine SUD screening protocols are urgently needed. These findings provide valuable evidence for policymakers and clinicians to strengthen prevention frameworks and underscore the necessity of scalable, evidence-based interventions tailored to developmental and socioeconomic contexts.
Data availability
Data used for the analyses are publicly available from the Institute of Health Metrics and Evaluation (http://www.healthdata.org/; http://ghdx.healthdata.org/gbd-results-tool).
Change history
13 September 2025
The original online version of this Article was revised: The Supplementary Information file published with this Article contained unedited information. The original Article has been corrected.
Abbreviations
- GBD:
-
The Global burden of diseases, injuries, and risk factors study
- SUDs:
-
Substance use disorders
- PTSD:
-
Post-traumatic stress disorder
- SDI:
-
Socio-demographic index
- ASR:
-
Age-standardized rates
- YLLs:
-
Years of life lost due to premature mortality
- YLDs:
-
Years lived with disability
- ASIR:
-
Age-standardized incidence rate
- ASPR:
-
Age-standardized prevalence rate
- ASMR:
-
Age-standardized mortality rate
- ASDR:
-
Age-standardized rate of DALYs
- AAPC:
-
Average annual percent change
- DALYs:
-
Disability-adjusted life-years
- CBT:
-
Cognitive-behavioral therapy
- MI:
-
Motivational interviewing
References
Diagnostic and statistical manual of mental disorders. Fifth Edition. Am. Psychiatr. Assoc. 21(21), 591–643 (2013).
Grant, B. F. et al. Epidemiology of DSM-5 drug use disorder: Results from the national epidemiologic survey on alcohol and related conditions-III. Jama Psychiatr. 73(1), 39–47. https://doi.org/10.1001/jamapsychiatry.2015.2132 (2016).
Kieling, C. et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. Jama Psychiat. 81(4), 347–356. https://doi.org/10.1001/jamapsychiatry.2023.5051 (2024).
Castelpietra, G. et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990–2019: Findings from the global burden of disease study 2019. Lancet Reg. Health Eur. 16, 100341. https://doi.org/10.1016/j.lanepe.2022.100341 (2022).
Thomasius, R., Paschke, K. & Arnaud, N. Substance-use disorders in children and adolescents. Dtsch Arztebl Int. 119(25), 440–450. https://doi.org/10.3238/arztebl.m2022.0122 (2022).
GBD 2021 Diseases and injuries collaborators. Global incidence, prevalence, years lived with disability (YLDs) disability-adjusted life-years (DALYs) and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet.403(10440):2133–2161. https://doi.org/10.1016/s0140-6736(24)00757-8 2024
Mokdad, A. H. et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet 387(10036), 2383–2401. https://doi.org/10.1016/s0140-6736(16)00648-6 (2016).
Common comorbidities with substance use disorders research report. Bethesda (MD): National institutes on drug abuse (US) Apr. Available from: https://www.ncbi.nlm.nih.gov/books/NBK571451/. 2020
Schulte, M. T. & Hser, Y. I. Substance use and associated health conditions throughout the lifespan. Public Health Rev. https://doi.org/10.1007/bf03391702 (2014).
Yonek, J. C. et al. Factors associated with use of mental health and substance use treatment services by justice-involved youths. Psychiatr. Serv. 70(7), 586–595. https://doi.org/10.1176/appi.ps.201800322 (2019).
Gakh, M., Coughenour, C., Assoumou, B. O. & Vanderstelt, M. The relationship between school absenteeism and substance use: An integrative literature review. Subst. Use Misuse. 55(3), 491–502. https://doi.org/10.1080/10826084.2019.1686021 (2020).
Patton, G. C. et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 387(10036), 2423–2478. https://doi.org/10.1016/s0140-6736(16)00579-1 (2016).
Sawyer, S. M., Azzopardi, P. S., Wickremarathne, D. & Patton, G. C. The age of adolescence. Lancet child. & Adolesc. Health. 2(3), 223–228 (2018).
Diaz, T. et al. A call for standardised age-disaggregated health data. Lancet Healthy Longev. 2(7), e436–e443 (2021).
Simon, K. M., Levy, S. J. & Bukstein, O. G. Adolescent substance use disorders. NEJM Evid. 1(6), EVIDra2200051. https://doi.org/10.1056/EVIDra2200051 (2022).
Davis, A. et al. Psychiatric comorbidities of substance use disorders: Does dual diagnosis predict inpatient detoxification treatment outcomes?. Int. J. Ment. Heal. Addict. 21(6), 3785–3799. https://doi.org/10.1007/s11469-022-00821-1 (2023).
Meulewaeter, F., De Pauw, S. S. W. & Vanderplasschen, W. Mothering, substance use disorders and intergenerational trauma transmission: An attachment-based perspective. Front. Psychiatr. 10, 728. https://doi.org/10.3389/fpsyt.2019.00728 (2019).
Ram, D., Whipple, C. R. & Jason, L. A. Family dynamics may influence an individual’s substance use abstinence self-efficacy. J. Addict. Prev. Med. https://doi.org/10.19104/japm.2016.106 (2016).
Volkow, N. D. & Blanco, C. Substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatr. 22(2), 203–229. https://doi.org/10.1002/wps.21073 (2023).
Dick, D. M. Gene-environment interaction in psychological traits and disorders. Annu. Rev. Clin. Psychol. 7, 383–409. https://doi.org/10.1146/annurev-clinpsy-032210-104518 (2011).
Winter, J. J., Rodríguez-Acevedo, K. L., Dittrich, M. & Heller, E. A. Early life adversity: Epigenetic regulation underlying drug addiction susceptibility. Mol. Cell. Neurosci. 125, 103825. https://doi.org/10.1016/j.mcn.2023.103825 (2023).
Rose, E. J., Picci, G. & Fishbein, D. H. Neurocognitive precursors of substance misuse corresponding to risk, resistance, and resilience pathways: Implications for prevention science. Front. Psychiatr. 10, 399. https://doi.org/10.3389/fpsyt.2019.00399 (2019).
Institute for health metrics and evaluation. GBD protocol. Accessed October 1. https:// www.healthdata.org/gbd/about/protocol. 2024
Murray, C. J. L. The global burden of disease study at 30 years. Nat. Med. 28(10), 2019–2026. https://doi.org/10.1038/s41591-022-01990-1 (2022).
GBD 2021 Causes of death collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the global burden of disease study 2021. Lancet. 2024 403(10440):2100–2132. https://doi.org/10.1016/s0140-6736(24)00367-2
Stevens, G. A. et al. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet 388(10062), e19–e23. https://doi.org/10.1016/s0140-6736(16)30388-9 (2016).
WHO. Adolescent health. https://www.who.int/health-topics/adolescent-health#tab=tab_1 (accessed October 2, 2024).
WHO. Adolescent and young adult health. https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (accessed October 2, 2024).
WHO. WHO releases updated guidance on adolescent health and well-being. https://www.who.int/news/item/11-10-2023-who-releases-updated-guidance-on-adolescent-health-and-well-being (accessed October 2, 2024).
Kim, H. J., Fay, M. P., Feuer, E. J. & Midthune, D. N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 19(3), 335–351 (2000).
Zhang, J., Ma, B., Han, X., Ding, S. & Li, Y. Global, regional, and national burdens of HIV and other sexually transmitted infections in adolescents and young adults aged 10–24 years from 1990 to 2019: A trend analysis based on the global burden of disease study 2019. Lancet Child. Adolesc. Health. 6(11), 763–776. https://doi.org/10.1016/s2352-4642(22)00219-x (2022).
Liu, L. et al. Global, regional, and national burdens of blindness and vision loss in children and adolescents from 1990 to 2019: A trend analysis. Ophthalmology 130(6), 575–587. https://doi.org/10.1016/j.ophtha.2023.02.002 (2023).
World Health Organization, Handbook on health inequality monitoring with a special focus on low- and middle-income countries 39–45. Available at https://www.who.int/publications/i/item/9789241548632. 2013
R Core Team (2024). R: A language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria. https://www.R-project.org/.
Chadi, N., Bagley, S. M. & Hadland, S. E. Addressing adolescents’ and young adults’ substance use disorders. Med. Clin. North. Am. 102(4), 603–620. https://doi.org/10.1016/j.mcna.2018.02.015 (2018).
McCabe, S. E., Schulenberg, J. E., Schepis, T. S., McCabe, V. V. & Veliz, P. T. Longitudinal analysis of substance use disorder symptom severity at age 18 years and substance use disorder in adulthood. Jama Netw. Open. 5(4), e225324. https://doi.org/10.1001/jamanetworkopen.2022.5324 (2022).
Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use 1975–2016: Overview key findings on adolescent drug use. 2017
Center for behavioral health statistics and quality (CBHSQ). 2017 National survey on drug use and health: Detailed tables. Substance abuse and mental health services administration rockville, MD; 2018.
Miech RA, Johnston LD, Patrick ME, O'Malley PM. Monitoring the future national survey results on drug use, 1975–2024: Overview and key findings for secondary school students. Monitoring the future monograph series. Ann Arbor, MI: Institute for social research University of Michigan. Available at: https://monitoringthefuture.org/results/annual-reports/.
Taylor, S., Paluszek, M. M., Rachor, G. S., McKay, D. & Asmundson, G. J. G. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addict Behav. 114, 106754. https://doi.org/10.1016/j.addbeh.2020.106754 (2021).
McHugh, R. K., Votaw, V. R., Sugarman, D. E. & Greenfield, S. F. Sex and gender differences in substance use disorders. Clin. Psychol. Rev. 66, 12–23. https://doi.org/10.1016/j.cpr.2017.10.012 (2018).
National institute on drug abuse. Sex and gender differences in substance use. 1 April, 2020, https://nida.nih.gov/publications/research-reports/substance-use-in-women/sex-gender-differences-in-substance-use, Accessed 1 November. 2024.
Kuhn, C. Emergence of sex differences in the development of substance use and abuse during adolescence. Pharmacol. Ther. 153, 55–78. https://doi.org/10.1016/j.pharmthera.2015.06.003 (2015).
Heitzeg, M. M., Hardee, J. E. & Beltz, A. M. Sex differences in the developmental neuroscience of adolescent substance use risk. Curr. Opin. Behav. Sci. 23, 21–26. https://doi.org/10.1016/j.cobeha.2018.01.020 (2018).
Welker, K. M., Gruber, J. & Mehta, P. H. A positive affective neuroendocrinology approach to reward and behavioral dysregulation. Front. Psychiatr. 6, 93. https://doi.org/10.3389/fpsyt.2015.00093 (2015).
Wilkinson, A. L., Fleming, P. J., Halpern, C. T., Herring, A. H. & Harris, K. M. Adherence to gender-typical behavior and high frequency substance use from adolescence into young adulthood. Psychol. Men. Masc. 19(1), 145–155. https://doi.org/10.1037/men0000088 (2018).
Sudhinaraset, M., Wigglesworth, C. & Takeuchi, D. T. Social and cultural contexts of alcohol use: Influences in a social-ecological framework. Alcohol Res. 38(1), 35–45 (2016).
Danpanichkul, P. et al. The burden of alcohol and substance use disorders in adolescents and young adults. Drug Alcohol Depend. 266, 112495. https://doi.org/10.1016/j.drugalcdep.2024.112495 (2025).
Zhang, S., Qi, X., Wang, Y. & Fang, K. Global burden of drug use disorders by region and country, 1990–2021. Front. Public Health. 12, 1470809. https://doi.org/10.3389/fpubh.2024.1470809 (2024).
Shen, J. et al. Prevalence, incidence, deaths, and disability-adjusted life-years of drug use disorders for 204 countries and territories during the past 30 years. Asian J. Psychiatr. 86, 103677. https://doi.org/10.1016/j.ajp.2023.103677 (2023).
Bleyer, A., Barnes, B. & Finn, K. United States marijuana legalization and opioid mortality epidemic during 2010–2020 and pandemic implications. J Natl Med Assoc. 114(4), 412–425. https://doi.org/10.1016/j.jnma.2022.03.004 (2022).
Connery, H. S., McHugh, R. K., Reilly, M., Shin, S. & Greenfield, S. F. Substance use disorders in global mental health delivery: epidemiology, treatment gap, and implementation of evidence-based treatments. Harv. Rev. Psychiatr. 28(5), 316–327. https://doi.org/10.1097/hrp.0000000000000271 (2020).
Pace, C. A. & Samet, J. H. In the clinic substance use disorders. Ann. Intern Med. 164(7), Itc49–Itc64. https://doi.org/10.7326/aitc201604050 (2016).
Hingson, R. & White, A. New research findings since the 2007 surgeon general’s call to action to prevent and reduce underage drinking: A review. J. Stud. Alcohol Drugs. 75(1), 158–169. https://doi.org/10.15288/jsad.2014.75.158 (2014).
Elder, R. W. et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med. 38(2), 217–229. https://doi.org/10.1016/j.amepre.2009.11.005 (2010).
Volkow, N. D., Baler, R. D., Compton, W. M. & Weiss, S. R. Adverse health effects of marijuana use. N Engl J Med. 370(23), 2219–2227. https://doi.org/10.1056/NEJMra1402309 (2014).
Batalla, A. et al. Structural and functional imaging studies in chronic cannabis users: A systematic review of adolescent and adult findings. PLoS ONE 8(2), e55821. https://doi.org/10.1371/journal.pone.0055821 (2013).
Zalesky, A. et al. Effect of long-term cannabis use on axonal fibre connectivity. Brain 135(Pt 7), 2245–2255. https://doi.org/10.1093/brain/aws136 (2012).
Gould, T. J. Addiction and cognition. Addict. Sci. Clin. Pract. 5(2), 4–14 (2010).
Chan, O. et al. Cannabis use during adolescence and young adulthood and academic achievement: A Systematic review and meta-analysis. Jama. Pediatr. https://doi.org/10.1001/jamapediatrics.2024.3674 (2024).
Samet, J. H., Shevitz, A., Fowle, J. & Singer, D. E. Hospitalization decision in febrile intravenous drug users. Am. J. Med. 89(1), 53–57. https://doi.org/10.1016/0002-9343(90)90098-x (1990).
Fadus, M. C. et al. Adolescent substance use disorder treatment: An Update on evidence-based strategies. Curr. Psychiatr. Rep. 21(10), 96. https://doi.org/10.1007/s11920-019-1086-0 (2019).
Griffin, K. W. & Botvin, G. J. Evidence-based interventions for preventing substance use disorders in adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 19(3), 505–526. https://doi.org/10.1016/j.chc.2010.03.005 (2010).
Volkow, N. D. & Wargo, E. M. Association of severity of adolescent substance use disorders and long-term outcomes. Jama Netw Open. 5(4), e225656. https://doi.org/10.1001/jamanetworkopen.2022.5656 (2022).
Acknowledgements
This study used data from the Global Burden of Disease Study 2021 (GBD 2021). We sincerely thank the Institute for Health Metrics and Evaluation (IHME) and all GBD collaborators for their efforts in data collection and curation. The authors alone are responsible for the views expressed in this article.
Funding
This work was supported by the High-Level Chinese Medical Hospital Promotion Project (Grant HLCMHPP2023089), the Special Programme for Cultivation of Outstanding Young Scientific and Technological Talents (Innovation Category) under the Basic Scientific Research Fund of China Academy of Chinese Medical Sciences (Grant ZZ13-YQ-019), and the Fundamental Research Funds for Central Public Welfare Research Institutes (Grant ZZ-YQ2023004). The funders had no role in study design, data collection, analysis, interpretation, manuscript preparation, or submission decisions.
Author information
Authors and Affiliations
Contributions
He Chen and Sixing Liu contributed equally to this work and share first authorship. He Chen and Sixing Liu were responsible for the methodology, data analysis, and manuscript drafting. Weiming Wang, Hangyu Shi, and Shuai Gao accessed and analyzed the GBD data, and drafted the manuscript. Yan Yan, Jiufei Fang, and Ying Zhan participated in data analysis, visualization and interpretation, and manuscript editing. Zhishun Liu and Huan Chen supervised the project and reviewed the manuscript and are co-corresponding authors. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, H., Liu, S., Wang, W. et al. Global burden of substance use disorders in adolescents and young adults aged 10–24 years from 1990 to 2021. Sci Rep 15, 25971 (2025). https://doi.org/10.1038/s41598-025-11266-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-11266-6