Abstract
Patients with transfusion-dependent thalassemia (TDT) are vulnerable to neurotoxicity due to frequent blood transfusions and the subsequent iron overload (IO) and inflammation. This vulnerability may contribute to the development of depression, anxiety, and chronic fatigue syndrome (CFS). This case-control study aims to investigate central nervous system injury biomarkers, including neuron-specific enolase (NSE), glial fibrillary acidic protein (GFAP), neurofilament light (NFL) and nestin, neuro-immune markers, such as C-reactive protein (CRP), interleukin (IL)-6, and IL-10, calcium, magnesium, copper, zinc, hematocrit, hemoglobin, iron and ferritin in 126 children with TDT and 41 healthy children. We examined the associations between these biomarkers and the Fibro-Fatigue (FF) Rating Scale, the Children’s Depression Inventory (CDI), and the Spence Children’s Anxiety Scale (SCAS) scores. Children with TDT showed significantly elevated FF, CDI, and SCAS scores, IO (as assessed using iron and ferritin levels), and higher NSE, GFAP, NFL, CRP, IL-6 and IL-10, and lower magnesium, zinc, and calcium as compared with healthy children. There were significant correlations between the CDI score and NFL, NSE and GFAP, SCAS score and NFL, and FF score and NFL and GFAP. The neuronal damage biomarkers were significantly associated with biomarkers of IO (including iron and ferritin) and the erythron (including lowered hematocrit and hemoglobin). These results suggest that IO-associated neurotoxicity and inflammation in children with TDT may contribute to symptoms of depression, anxiety, and chronic fatigue and may serve as potential therapeutic targets.
Similar content being viewed by others
Introduction
Beta-thalassemia (β-TM) encompasses a group of hereditary conditions characterized by the absence or deficiency of the β-globin chain in the hemoglobin A molecule. This chain defect causes harm to the erythrocyte membrane and ultimately leads to anemia1. The aforementioned condition often presents with symptoms of hemolytic anemia and has a 15% mortality rate among the millions of children it impacts1,2. Individuals with β-TM necessitate long-term blood transfusions to maintain adequate hemoglobin levels and mitigate the adverse consequences of erythropoiesis inefficiency3.
Transfusion-dependent thalassemia (TDT) patients are at risk of developing various complications because of requiring frequent blood transfusions4. Prolonged blood transfusions have the potential to cause substantial iron excess (IO), which can result in toxicity affecting various organs such as the heart, liver, and endocrine glands5,6. Excess iron may be neurotoxic due to its capacity to trigger oxidative stress within central neurons7.
Thalassemia is associated with a heightened prevalence of neuropsychiatric disorders8. Around 65%8 to eighty-three%9. Children with thalassemia may suffer from anxiety disorders or depression. Anxiety symptoms are present in 32% of thalassemia patients and major depression (MDD) in 16–31% 10,11. MDD is associated with elevated IO and pro-inflammatory cytokine levels in the serum, such as interleukin (IL)-1β and tumor necrosis factor (TNF)-α12. Blood transfusions may induce depressive symptoms and MDD in TDT via the mediating effects of IO and subsequent activation of the immune-inflammatory response system (IRS)13.
MDD has been linked to alterations in iron metabolism, as indicated by elevated serum ferritin levels, decreased erythrocyte count, and decreased hematocrit and hemoglobin concentrations13,14. Additionally, evidence suggests that the impacts of activated IRS pathways on MDD12,15,16,17 and CFS is mediated by heightened neurotoxicity18. MDD is distinguished by increased serum concentrations of brain injury markers, including neurofilament light chain (NFL), glial fibrillary acidic protein (GFAP), P-tau217, and IRS markers such as C-reactive protein (CRP)19. NFL levels are elevated in patients with MDD and bipolar disorder12,20 and treatment-resistant depression21,22. Serum concentrations of NFL, nestin, CRP, and IL-10 are increased in association with depressive symptoms in patients with end-stage renal disease, while serum levels of zinc are reduced in comparison to the control group23.
NFL is a biomarker of neuronal injury and neurodegenerative processes in the central nervous system (CNS), whilst neurodegenerative diseases are frequently associated with elevated NFL plasma levels24,25. GFAP serves as an indicator of astrocyte functionality, and its upregulation is an index of neurodegeneration, ischemic stroke, and various other CNS disorders26,27,28. Nestin mediates radial axonal growth and is an additional intermediate filament protein that is expressed by neuronal progenitor cells, including those in the adult brain29,30. Neuron-specific enolase (NSE) is another neuronal marker that has been linked to neurodegenerative, inflammatory, hypoxic, and metabolic diseases26,31,32. Additionally, magnesium deficiency may contribute to neurodegenerative processes33and dysfunctional calcium signaling may be one of the essential processes in neurodegenerative processes34. This is significant because IRS activation is associated with decreased calcium, magnesium, and zinc levels and increased copper levels in MDD35,36. Neurodegenerative pathways, including aberrations in the Wnt/catenin pathway, oxidative stress pathways, and IRS activation, may be implicated in CFS18.
Nevertheless, there is no evidence that IO in children with TDT is associated with increased serum neuronal and astroglial projection biomarkers in association with the severity of depression, anxiety, and CFS. Therefore, the objective of the present investigation is to determine whether TDT is correlated with neuronal and astroglial injury indicators (as measured by serum GFAP, NSE, NFL, and nestin), as well as whether these indicators are associated with IRS biomarkers (as measured by CRP, IL-6, and IL-10), affective symptoms, and CFS.
Subjects and methods
Participants
A total of 167 children were enrolled in the present study; of these, 126 were children with TDT and 41 were healthy control children between the ages of 6 and 12, of both sexes. The recruitment process for TDT patients commenced in March 2023 and concluded in May 2023 at the Thalassemia Unit, which is situated at Al-Zahra’a Teaching Hospital in the Najaf Governorate of Iraq. The diagnosis of β-TM was ascertained through the utilization of the diagnostic criteria specified in the 2019 ICD-10-CM Diagnosis Code D56.1 by pediatricians and hematologists. The identification of β-TM was accomplished through the assessment of distinctive clinical manifestations, including aberrant bone growth, hepatosplenomegaly, and severe anemia. Hematological assessments were performed, including the measurement of hemoglobin (Hb) concentrations below 70 g/L and the identification of a high proportion of reticulocytes and hypochromic microcytic red blood cells with anisopoikilocytosis. Furthermore, the concentration of HbA2 was ascertained via high-performance liquid chromatography (HPLC) employing the VARIANT TM β-Thalassemia Short Program.
The control group comprised forty-one children who appeared to be in good health. There were no cases of anemia, immune-inflammatory disorders, any systemic medical diseases, affective disorders, and CFS among the controls. Healthy control children were selected to participate while accompanying their parents during a routine hospital examination. Informed consent was acquired from the parents, either the mother or father, who were informed that the outcomes of the study would be provided to them as complimentary and beneficial laboratory tests. Children (either TDT or normal controls) were excluded when they suffered from splenectomy, systemic diseases including renal failure, diabetes mellitus, liver disease and infectious disorders.
The determination of when to administer packaged red blood cells (RBCs) for blood transfusions was based on the Hb levels, which had to be maintained at or above 90 g/L. This was accomplished every two to four weeks. Furthermore, a protocol of iron-chelating therapy was implemented for the patients. This involved administering deferoxamine mesylate USP (brand name Desferal®) infusions at a rate ranging from 25 to 50 mg/kg/day for eight hours daily. The precise dosage that was administered to the patients was ascertained by analyzing their blood ferritin levels. To alleviate the symptoms of ineffective erythropoiesis, folic acid was administered to most patients undergoing TDT. Vitamin C was administered to patients who had received a diagnosis of TDT as a therapeutic intervention to support the iron chelation process when used in conjunction with deferoxamine.
The researchers obtained written informed consent from the first-degree relatives (either the father or mother) of the participating children after a comprehensive verbal explanation, in adherence to the tenets delineated in the Declaration of Helsinki. The research was granted approval by the Institutional Review Board (IRB) of the Najaf Health Directorate, Training and Human Development Center, Iraq (document number 4233/2023).
Clinical measurements
The Fibro-fatigue (FF) scale was administered by a senior psychiatrist to evaluate the severity of CFS in both patients and controls37. The assessment of depressive symptoms was conducted utilizing the Children’s Depression Inventory (CDI). This is a self-rating screening instrument consisting of 27 three-point scale statements. The child is requested to choose the response that most accurately characterizes his or her emotions over the past two weeks in relation to each given statement. The total CDI score is utilized as an indicator of depression severity in the present study. Negative self-esteem, interpersonal difficulties, ineffectiveness, anhedonia, and negative mood are the subscales that comprise the CDI. Having been validated in school-aged children, the CDI is one of the most widely utilized depression screening instruments for children. Depression in children may be diagnosed when the Child Depression Inventory (CDI) score is equal to or greater than 19. The children’s anxiety symptoms were assessed using the Spence Children’s Anxiety Scale (SCAS)38. The scales were validated in patients from Iraqi communities and used in previous Iraqi studies on TDT39,40,41.
Assays
Five milliliters of venous blood were drawn from all participants after an overnight fast. The patients’ samples were collected just before their blood transfusion session. Blood was left until complete clotting (about ten minutes) at room temperature. After centrifugation for five minutes at 3000 rpm, serum was separated and transported into Eppendorf tubes. Serum calcium, magnesium, albumin, copper, and zinc were measured by using ready-for-use kits purchased from Agappe Diagnostics® ready-to-use kit from Cham (Switzerland). Copper was determined spectrophotometrically using a kit from LTA Co. (Milano, Italy). The amount of iron in sera was determined by colorimetric kits purchased from Spectrum® (Cairo, Egypt). Commercial ELISA sandwich kits provided by Nanjing Pars Biochem Co., Ltd., Nanjing, China, were used to measure interleukin-6, Interleukin-10, GFAP, NSE, NF-L, and nestin. Serum ferritin levels were measured by using an ELISA kit purchased from Elabscience® (Wuhan, China). These kits were made for human samples depending on the biotin double antibody sandwich technology. Hematological parameters were measured by a five-part differential Mindray BC-5000 hematology analyzer (Mindray Medical Electronics Co., Shenzhen, China). The inter-assay CV% of all kits is lower than 10%. For samples with highly concentrated analytes, we employed sample dilutions. A C-reactive protein (CRP) latex slide test (Spinreact®, Barcelona, Spain) was used for CRP measurement in human serum. The approximate CRP concentration in the patient sample is calculated as follows: 6 x CRP Titer = mg/L.
Statistical analysis
Analysis of contingency tables (χ2 test) was employed to examine the relationships between nominal variables, whereas analysis of variance (ANOVA) was utilized to assess variations in continuous variables across groups. To determine the correlations between scale variables, Pearson’s product-moment correlation coefficients were applied. General linear models (GLM) were employed in the current investigation to assess the correlations between TDT (in contrast to the control group) and the biomarkers. Following that, evaluations of between-subject relationships and pairwise comparisons were performed across treatment groups. The researchers utilized a false-discovery rate (FDR) procedure to mitigate the impact of type I errors that may occur during multiple comparisons42. We matched the samples by age, gender, and BMI and used these confounders as covariates in GLM analyses. We then ran the analyses again, this time obtaining parameter estimates with robust standard errors (HC3) and their t values. Multiple regression analysis was utilized in the study, employing both manual and automatic stepwise techniques. A p-to-entry threshold of 0.05 and a p-to-remove threshold of 0.06 were applied. The purpose of the analysis was to determine which biomarkers could be used to predict the scores by assessing the variation in R2 (used as effect size). To identify (multi)collinearity issues, tolerance, and VIF were employed, Cook’s distance and leverage were utilized to assess multivariate normality, and the White and modified Breusch-Pagan tests were utilized to determine homoscedasticity. The results of the regression analyses were bootstrapped using 5,000 samples, and when there was an incongruity between the outcomes, the bootstrapped results were displayed. Four z-unit-based composite ratings were computed. (a) IRS activation was calculated as z IL-6 + z IL-10 + z CRP - z zinc – z albumin (referred to as Comp_IRS); (b) Disorders in the erythron were represented by z hemoglobin + z hematocrit (labeled as Comp_erythron); (c) z Iron + z ferritin constituted Comp_IO; and (d) an overall severity index was determined as z FF + z CDI + z SCAS (labeled as Comp_severity). We extracted the first principal component (PC) using the principal component (GFAP), NSE, and Nestin (NFL could not be included because it did not load highly enough on the first PC). The first principal component (PC) accounted for 50.3% of the variance, and all loadings exceeded 0.67. These results suggest that the PC score, designated PC_neuronal, potentially reflects neuronal injury. All statistical tests were two-tailed, and a p-value of 0.05 was used for statistical significance. For the analysis of the data, version 29 of IBM SPSS for Windows was utilized.
The primary statistical analyses are the multiple regression analyses with the rating scale scores as outcome variables and the biomarkers as explanatory variables. The a priori required sample size given alpha = 0.05, power = 0.8, five covariates, and an effect size of 0.18 (corresponding to 15% explained variance) is 79. The post-hoc achieved power of these analyses was at least 0.999.
Results
Socio-demographic data
Supplementary Table S1 shows the socio-demographic and clinical data of the children participating in the current study. The TDT patients have a duration of diseases (appearance of severe symptoms) of 8.84 ± 2.75 years. There were no significant differences in age, sex ratio, BMI, and education years between healthy children and TDT patients. The results showed significant increases (all p < 0.001) in total FF, CDI, and SCAS scores, ferritin, and iron in TDT patients compared with healthy children. There was a significant decrease in Hb and PCV% in patients compared with the controls.
Biomarkers in TDT and controls
Table 1 shows the results of the biomarkers in TDT and control groups. These data were analyzed using GLM analyses with age, sex, and BMI as covariates. The results showed a significant increase in the serum CRP, copper, IL-6, IL-10, NSE, GFAP, and NFL in the TDT group compared with the healthy children. The Comp_IRS and PC_neuronal scores were both significantly increased in TDT patients compared with the control group. Magnesium, calcium, and zinc are significantly decreased in TDT compared with the control group. These differences remained significant after FDR’s p-correction, including GFAP (FRR p = 0.0233). Serum albumin and nestin are not significantly different between the diagnostic groups. The aforementioned results remained unchanged when employing the HC3 robust standard error method.
Correlation matrix between clinical scores and biomarkers in TDT
Table 2 shows the correlation matrix of the neuropsychiatric rating scale scores and the iron status biomarkers in TDT patients. The results showed that FF is significantly correlated with CRP, copper, IL-6, IL-10, GFAP, and NFL, whilst there is a significant inverse correlation between FF and magnesium, calcium, and zinc. The results indicated that the CDI score is significantly correlated with CRP, IL-10, NSE, GFAP, and NFL, and inversely with magnesium, calcium, and zinc. The SCAS score is significantly correlated with CRP, copper, IL-10, and NFL, and inversely with calcium and zinc. The Comp_erythron index was significantly and inversely correlated with CRP, copper, IL-6, IL-10, NSE, GFAP, and NFL, and positively with magnesium, calcium, and zinc. Comp_IO is significantly correlated with CRP, copper, IL-6, IL-10, NSE, GFAP, and NFL, and inversely with magnesium and calcium.
There were significant correlations between Comp_severity and Comp_IRS (r = 0.349, p < 0.001), Comp_IO (r = 0.275, p < 0.001) and Comp_erythron (r=-0.221, p < 0.001).
Prediction of neuropsychiatric scores
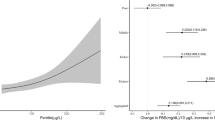
Table 3 shows the results of multiple regression analyses with the total FF, CDI, and SCAS scores as dependent variables and the neuronal damage biomarkers and other biomarkers as explanatory variables. The first regression shows that 42.9% of the variance in the FF score was predicted by CRP, copper, and NFL (all positively), and calcium and magnesium (both inversely associated). Regression #2 shows that the CDI total score was predicted by CRP, IL-10, and NFL (all three positively) and inversely with calcium. The third regression shows that 23.2% of the variance in the SCAS total score was explained by NFL, CRP, and copper (all positively correlated), and zinc (inversely associated). Figure 1 shows the partial regression of the total SCAS scale score on NFL levels.
Prediction of the neuronal damage biomarkers by the measured biomarkers in TDT patients
The results in Supplementary Table S2 reveal that neuronal damage biomarkers may be predicted by IRS biomarkers. Figure 2 shows the partial regression of PC_neuronal on Comp_IRS.
Partial regression plot of the principal component (PC) extracted from neuronal injury biomarkers, including glial fibrillary acidic protein, neuro-specific enolase, and nestin, on a composite score (comp) reflecting activation of the immune-inflammatory responses system (IRS) (p < 0.001, after adjusting for age, sex, and body mass index).
Regression #1 shows that 9.5% of the variance in the NSE could be explained by IL-10. In Regression #2, a part of the variance (12.6 7%) in GFAP is explained by IL-6 and IL-10. Supplementary Fig. S1 shows the partial regression of GFAP on Comp_IRS. The third regression shows that 16.5% of the variance in NFL is explained by copper (positively) and hemoglobin (inversely). Supplementary Fig. S2 shows the regression of the NFL levels on hemoglobin. Regression #4 shows that 10.6% of the variance in nestin is positively associated with IL-6 and inversely with calcium. In Regression #5, a moderate part of the variance (24.2%) in PC_neuronal was explained by IL-6, IL-10, and ferritin. Regression #6 shows that 27.1% of the variance in Comp_IRS could be explained by ferritin and inversely by PCV%. Supplementary Fig. S3 shows the partial regression of the inflammation component on Comp_erythron.
Discussion
IO, IRS activation, and affective and CFS symptoms due to TDT
The first major finding of this research is that children with TDT have higher total FF, CDI, and SCAS scores in comparison to healthy children. Additionally, there is a significant correlation between the integrated index of severity of affective and CFS symptoms and IRS activation, IO, and erythron disorders (low hematocrit and hemoglobin).
IRS activation in TDT was identified in the present study by elevated levels of CRP, IL-6, and IL-10 in the serum, in comparison to the control group. Previously, a wide spectrum of immune defects has been observed in patients with affective disorders and CFS18,43 and β-thalassemic patients44. Serum concentrations of IL-6, IL-10, and ferritin were all elevated in TDT patients45. TDT has been associated with altered cytokine profiles, modifications in innate immune functions, and the manifestation of a low-grade systemic inflammatory state46. Based on existing literature data, immunological abnormalities observed in thalassemia patients may be induced by the condition and its therapeutic interventions. IO, functional abnormalities of immune system cells caused by chronic inflammation, oxidative stress, multiple blood transfusions, iron chelation therapy, and splenectomy are the most significant contributors to these changes47.
Affective and CFS symptoms may result from peripheral activation of IRS pathways influencing the brain via humoral and neural pathways, thereby altering the functions of neural cells, structural and functional connectivity18,48,49. Neurotoxicity can be caused by various neuro-immune (M1, Th1, and Th17) and neuro-oxidative pathways which may disrupt crucial neuronal processes, including neurogenesis, neuroplasticity, axonogenesis, dendritic sprouting, and receptor expression17,50. Furthermore, IRS activation disrupts interoceptive signaling and the functional connectivity within the brain network, which may have ramifications for the etiology of MDD and CFS17,51. In addition, increased CRP production may further impair endothelial cells, increasing their permeability and exacerbating the progression of neurodegenerative and cerebrovascular disorders51,52,53,54.
Another hypothesis that connects TDT with the development of neuropsychiatric symptoms is that iron accumulation may have neurotoxic effects. Iron accumulation not only triggers oxidative stress but also exerts an impact on the turnover of neurotransmitters and the expression of neuroreceptors within the brain, consequently influencing behavioral responses12,55,56. Alternatively, psychological stressors may contribute to affective disorders in children with TDT57,58 through IRS activation and aggravating the oxidative stress59. Fear of separation from family, limited social interaction and isolation, physical and facial deformities, restricted life opportunities, fear of death, and restrictions in school and outdoor pursuits may contribute to such effects.
Neuronal and astroglial projection toxicity in TDT
The second major finding of the present study is that serum levels of various neuronal and astroglial damage biomarkers are elevated in TDT patients relative to the control group and that these CNS injury biomarkers are positively associated with the severity of affective and CFS symptoms. NFL, GFAP, and NSE were, in descending order of significance, the most pertinent CNS biomarkers. Moreover, there exists a substantial correlation between these markers of CNS injury and IRS biomarkers, as well as copper, IO, or erythron biomarkers.
Elevated NFL levels in patients with neuroinflammatory diseases are indicative of ongoing and acute disease processes as opposed to progressive brain injury60,61. Moreover, synaptic degeneration may be indicated by an increase in NFL62which is a biomarker of injury to cyto-axonal cell structures63 in neurodegenerative disorders. The correlation between serum NFL and cognitive performance in healthy individuals suggests that NFL has the capability to detect subclinical microstructural alterations64. Reactive astrogliosis and CNS trauma induce an increase in GFAP expression, which may be translocated into the peripheral circulation via blood-brain-barrier disruption27,28. Elevated serum GFAP is, therefore, a biomarker for neurotoxicity, specifically injury to neuronal and astroglial cells28. Variations in GFAP levels can manifest in response to traumatic injuries, neurodegenerative or neuroinflammatory processes65,66, neuropathology67, disruption of the blood-brain barrier68, and brain vascular inflammation. Serum and cerebrospinal fluid (CSF) NSE elevation is an effective biomarker for neuronal loss and impairment, brain injury, and neuroinflammation26,31,32. It is noteworthy that an increase in the release of neuronal biomarkers into the bloodstream69,70 through the glymphatic system may result from apoptosis of brain cells71,72.
Patients diagnosed with MDD and those experiencing affective and CFS symptoms because of ESRD exhibit elevated levels of neuronal and astroglial projection markers, as mentioned in the Introduction19,23. Cognitive function was found to be inversely correlated with increased NFL in patients with MDD73. This finding suggests that active neuropathological processes, specifically axonal and synaptic lesions, may be present in these patients74,75. CSF GFAP levels are elevated in patients with MDD76, and serum GFAP levels may increase as the severity of MDD worsens77. Additionally, individuals with neuropsychiatric disorders who do not exhibit any brain radiological abnormalities may have elevated plasma GFAP levels78. Serum GFAP has been proposed as a potential marker for monitoring astroglial pathology in MDD27,77,79. It was believed that NSE and GFAP served as prognostic indicators for high-risk suicide attempters26. Furthermore, elevated CRP levels were found to be strongly correlated with increases in these neuronal and astroglial projection injury biomarkers in MDD19. In summary, the findings indicate that the heightened neurotoxicity observed in affective and CFS symptoms might be the result of IRS activation, neuroimmune mechanisms, and IO. In the following paragraph, however, we explore additional potential pathways that connect TDT with CNS injury.
An overabundance of iron within the brain has been associated with the onset and progression of neurodegenerative diseases80,81. Elevated concentrations of iron stimulate the production of reactive oxygen species, which subsequently cause harm to cells and tissues82,83 as well as neurodegenerative disorders84,85. Iron toxicity can induce neurodegeneration, which in turn can trigger ferroptosis, a non-apoptotic cell death specific to iron86,87. In addition to heightened neuro-oxidative pathways, thalassemia disease may also induce neurodegeneration via mitochondrial dysfunctions88. Lowered calcium levels, in addition to peripheral inflammation, have the potential to induce neuro-glial projection toxicity19.
Limitations of the study
A first limitation of this study is its case-control design, which prevents causal inferences to be drawn. Consequently, potential causal relationships established here must be checked in prospective studies. Furthermore, to enhance the research, we should have assessed a comprehensive range of biomarkers associated with neuronal damage, cytokines, chemokines, oxidative and nitrosative stress, and neuronal damage in TDT patients in conjunction with neuropsychiatric ratings. Furthermore, there is always a possible reporting bias in self-report scales. Another potential limitation is that the unbalanced case-control study design may have influenced the statistical power in the comparative analyses, consequently leading to an increased type I error rate. Nonetheless, we have conducted a group-matching of the samples based on age, sex, and BMI. In addition, we employed Generalized Linear Model (GLM) analysis, incorporating these variables as covariates, and subsequently re-executed the analyses utilizing robust standard errors. The latter method yields more precise estimations of the standard errors associated with the coefficients in unbalanced case-control studies.
Conclusions
The current investigation showed heightened neurotoxicity among TDT patients, in which immune-inflammatory biomarkers and serum biomarkers of injury to neuronal and astroglial projections are correlated with the intensity of affective and CFS symptoms. IO may induce both immune activation and increased neurotoxicity in TDT. Activated IRS pathways, increased neurotoxicity, and subsequent injury to neuronal and astroglial projections may represent appropriate drug targets awaiting validation in longitudinal studies. Furthermore, neuroprotective agents may possess therapeutic potential to safeguard against heightened neurotoxicity. Routine screening for symptoms of depression, anxiety, and CFS in children with TDT may help early detection and intervention.
Data availability
The data that support these findings of the study are available upon request from the corresponding authors.
References
Raguram, A., Banskota, S. & Liu, D. R. Therapeutic in vivo delivery of gene editing agents. Cell (2022).
Crippa, S. et al. Bone marrow stromal cells from β-thalassemia patients have impaired hematopoietic supportive capacity. J. Clin. Investig. 129, 1566–1580 (2019).
Aydinok, Y. Treatment of thalassaemia: a review of the new approaches on transfusion safety and the novel therapeutics. ISBT Sci. Ser. 15, 102–109 (2020).
Shah, F. T., Sayani, F., Trompeter, S., Drasar, E. & Piga, A. Challenges of blood transfusions in β-thalassemia. Blood Rev. 37, 100588. https://doi.org/10.1016/j.blre.2019.100588 (2019).
Hamed, A. A., Elguindy, W., Elhenawy, Y. I. & Ibrahim, R. H. Early cardiac involvement and risk factors for the development of arrhythmia in patients with β-thalassemia major. J. Pediatr. Hematol. Oncol. 38, 5–11 (2016).
Daher, R., Manceau, H. & Karim, Z. Iron metabolism and the role of the iron-regulating hormone Hepcidin in health and disease. La. Presse Médicale. 46, e272–e278 (2017).
Schipper, H. M. Brain iron deposition and the free radical-mitochondrial theory of ageing. Ageing Res. Rev. 3, 265–301. https://doi.org/10.1016/j.arr.2004.02.001 (2004).
Sahu, S., Agrawal, A., Shrivastava, J. & Tonk, S. Psychiatric disorders and caregiver burden in children with transfusion dependent β-thalassaemia and their caregivers. World J. Clin. Pediatr. 12, 125–132. https://doi.org/10.5409/wjcp.v12.i3.125 (2023).
Shaligram, D., Girimaji, S. & Chaturvedi, S. Psychological problems and quality of life in children with thalassemia. Indian J. Pediatr. 74, 727–730 (2007).
Gan, G. G., Hue, Y. L. & Sathar, J. Factors affecting quality of life in adult patients with thalassaemia major and intermedia. Ann. Acad. Med. Singapore. 45, 520–523 (2016).
Shafiee, A., Nazari, S., Jorjani, S., Bahraminia, E. & Sadeghi-Koupaei, M. Prevalence of depression in patients with β-thalassemia as assessed by the beck’s depression inventory. Hemoglobin 38, 289–291. https://doi.org/10.3109/03630269.2014.929008 (2014).
Al-Hakeim, H. K., Najm, A. H., Al-Dujaili, A. H. & Maes, M. Major depression in children with transfusion-Dependent thalassemia is strongly associated with the combined effects of blood transfusion rate, iron overload, and increased Pro-inflammatory cytokines. Neurotox. Res. 38, 228–241. https://doi.org/10.1007/s12640-020-00193-1 (2020).
Trevisan, C. et al. Low hemoglobin levels and risk of developing depression in the elderly: results from the prospective PRO. VA study. J. Clin. Psychiatry. 77, 10882 (2016).
Rybka, J. et al. Interplay between the pro-oxidant and antioxidant systems and Proinflammatory cytokine levels, in relation to iron metabolism and the erythron in depression. Free Radic. Biol. Med. 63, 187–194 (2013).
Schiepers, O. J., Wichers, M. C. & Maes, M. Cytokines and major depression. Prog Neuropsychopharmacol. Biol. Psychiatry. 29, 201–217 (2005).
Maes, M. The cytokine hypothesis of depression: inflammation, oxidative & nitrosative stress (IO&NS) and leaky gut as new targets for adjunctive treatments in depression. Neuroendocrinol. Lett. 29, 287–291 (2008).
Maes, M. et al. The immune profile of major dysmood disorder: proof of concept and mechanism using the precision nomothetic psychiatry approach. Cells 11, 1183 (2022).
Maes, M., Kubera, M. & Kotańska, M. Aberrations in the Cross-Talks among redox, nuclear Factor-κB, and Wnt/β-Catenin pathway signaling underpin myalgic encephalomyelitis and chronic fatigue syndrome. Front. Psychiatry. 13, 822382. https://doi.org/10.3389/fpsyt.2022.822382 (2022).
Al-Hakeim, H. K., Al-Naqeeb, T. H., Almulla, A. F. & Maes, M. The physio-affective phenome of major depression is strongly associated with biomarkers of astroglial and neuronal projection toxicity which in turn are associated with peripheral inflammation, insulin resistance and Lowered calcium. J. Affect. Disord. 331, 300–312 (2023).
Chen, M. H. et al. Neurofilament light chain is a novel biomarker for major depression and related executive dysfunction. Int. J. Neuropsychopharmacol. 25, 99–105 (2022).
Domingues, R. B., Fernandes, G. B. P., Leite, F. & Senne, C. Neurofilament light chain in the assessment of patients with multiple sclerosis. Arq. Neuropsiquiatr. 77, 436–441. https://doi.org/10.1590/0004-282x20190060 (2019).
Spanier, S., Kilian, H. M., Meyer, D. M. & Schlaepfer, T. E. Treatment resistance in major depression is correlated with increased plasma levels of neurofilament light protein reflecting axonal damage. Med. Hypotheses. 127, 159–161. https://doi.org/10.1016/j.mehy.2019.03.022 (2019).
Al-Hakeim, H. K. et al. In end-stage kidney disease, inflammation, erythron abnormalities and declined kidney function tests are accompanied by increased affective symptoms, chronic-fatigue, and fibromyalgia. medRxiv, 2023.2001. 2012.23284460 (2023).
Maes, M. et al. Reactivity to neural tissue epitopes, Aquaporin 4 and heat shock protein 60 is associated with activated immune-inflammatory pathways and the onset of delirium following hip fracture surgery. MedRxiv (2022).
Yuan, A. & Nixon, R. A. Specialized roles of neurofilament proteins in synapses: relevance to neuropsychiatric disorders. Brain Res. Bull. 126, 334–346. https://doi.org/10.1016/j.brainresbull.2016.09.002 (2016).
Bagheri, M., Ghaneialvar, H., Oshnokhah, M. & Salari, S. GFAP and neuron specific enolase (NSE) in the serum of suicide attempters. Medical J. Islamic Repub. Iran 36 (2022).
Hol, E. M. & Pekny, M. Glial fibrillary acidic protein (GFAP) and the astrocyte intermediate filament system in diseases of the central nervous system. Curr. Opin. Cell Biol. 32, 121–130 (2015).
Yang, Z. & Wang, K. K. Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trend Neurosci. 38, 364–374 (2015).
Hendrickson, M. L., Rao, A. J., Demerdash, O. N. & Kalil, R. E. Expression of Nestin by neural cells in the adult rat and human brain. PloS One. 6, e18535 (2011).
Paquet-Durand, F. & Bicker, G. Human model neurons in studies of brain cell damage and neural repair. Curr. Mol. Med. 7, 541–554 (2007).
Park, D. W., Park, S. H. & Hwang, S. K. Serial measurement of S100B and NSE in pediatric traumatic brain injury. Child’s Nerv. Syst. 35, 343–348 (2019).
Haque, A., Polcyn, R., Matzelle, D. & Banik, N. L. New insights into the role of neuron-specific enolase in neuro-inflammation, neurodegeneration, and neuroprotection. Brain Sci. 8, 33 (2018).
Hlásný, J. Is magnesium deficiency the cause of neurodegeneration in animals and humans? 2nd part; alzheimer’s disease and BSE magnesium-ammonia theory connections. V´yzkum V Chovu Skotu. 2, 28–39 (2020).
Bezprozvanny, I. Calcium signaling and neurodegeneration. Acta Naturae. 2, 72–80 (2010).
Al-Dujaili, A. H., Al-Hakeim, H. K., Twayej, A. J. & Maes, M. Total and ionized calcium and magnesium are significantly Lowered in drug-naïve depressed patients: effects of antidepressants and associations with immune activation. Metab. Brain Dis. 34, 1493–1503. https://doi.org/10.1007/s11011-019-00458-5 (2019).
Al-Hakeim, H. K., Hadi, H. H., Jawad, G. A. & Maes, M. Intersections between copper, β-arrestin-1, calcium, FBXW7, CD17, insulin resistance and atherogenicity mediate depression and anxiety due to type 2 diabetes mellitus: A nomothetic network approach. J. Personal Med. 12, 23 (2022).
Zachrisson, O., Regland, B., Jahreskog, M., Kron, M. & Gottfries, C. G. A rating scale for fibromyalgia and chronic fatigue syndrome (the fibrofatigue scale). J. Psychosom. Res. 52, 501–509. https://doi.org/10.1016/s0022-3999(01)00315-4 (2002).
Spence, S. H., Barrett, P. M. & Turner, C. M. Psychometric properties of the spence children’s anxiety scale with young adolescents. J. Anxiety Disord. 17, 605–625. https://doi.org/10.1016/s0887-6185(02)00236-0 (2003).
Al-Hakeim, H. K., Najm, A. H., Al-Dujaili, A. H. & Maes, M. Major depression in children with transfusion-dependent thalassemia is strongly associated with the combined effects of blood transfusion rate, iron overload, and increased pro-inflammatory cytokines. Neurotox. Res. 38, 228–241 (2020).
Al-Hakeim, H. K., Najm, A. H., Moustafa, S. R. & Maes, M. Construction of an exposure-pathway-phenotype in children with depression due to transfusion-dependent thalassemia: results of (un) supervised machine learning. J. Affect. Disord. 282, 644–655 (2021).
Taher, A. et al. Validation of a patient-reported outcomes symptom measure for patients with nontransfusion‐dependent thalassemia (NTDT‐PRO©). Am. J. Hematol. 94, 177–183 (2019).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. Roy. Stat. Soc.: Ser. B (Methodol.). 57, 289–300 (1995).
Maes, M. & Carvalho, A. F. The compensatory Immune-Regulatory reflex system (CIRS) in depression and bipolar disorder. Mol. Neurobiol. 55, 8885–8903. https://doi.org/10.1007/s12035-018-1016-x (2018).
Bazi, A., Shahramian, I., Yaghoobi, H., Naderi, M. & Azizi, H. The role of immune system in thalassemia major: a narrative review. J. Pediatr. Rev. 6, 29–36 (2018).
Politou, M. et al. The effect of transfusion on immune responses in thalassemia. Blood Cells Molecules Dis. 83, 102425 (2020).
Elsayh, K. I., Mohammed, W. S., Zahran, A. M. & Saad, K. Leukocytes apoptosis and adipocytokines in children with beta thalassemia major. Clin. Experimental Med. 16, 345–350 (2016).
Gluba-Brzózka, A. et al. Pathomechanisms of immunological disturbances in β-Thalassemia. Int. J. Mol. Sci. 22, 9677 (2021).
Kubera, M., Obuchowicz, E., Goehler, L., Brzeszcz, J. & Maes, M. In animal models, psychosocial stress-induced (neuro)inflammation, apoptosis and reduced neurogenesis are associated to the onset of depression. Prog Neuropsychopharmacol. Biol. Psychiatry. 35, 744–759. https://doi.org/10.1016/j.pnpbp.2010.08.026 (2011).
Harrison, N. A. et al. A neurocomputational account of how inflammation enhances sensitivity to punishments versus rewards. Biol. Psychiatry. 80, 73–81 (2016).
Maes, M. et al. The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression. Metab. Brain Dis. 24, 27–53 (2009).
Aruldass, A. R. et al. Dysconnectivity of a brain functional network was associated with blood inflammatory markers in depression. Brain Behav. Immun. 98, 299–309 (2021).
Hsuchou, H., Kastin, A. J., Mishra, P. K. & Pan, W. C-reactive protein increases BBB permeability: implications for obesity and neuroinflammation. Cell. Physiol. Biochem. 30, 1109–1119. https://doi.org/10.1159/000343302 (2012).
Belin, C. et al. Description of neurotoxicity in a series of patients treated with CAR T-cell therapy. Sci. Rep. 10, 18997. https://doi.org/10.1038/s41598-020-76055-9 (2020).
Ge, X. et al. Relationships among serum C-reactive protein, receptor for advanced glycation products, metabolic dysfunction, and cognitive impairments. BMC Neurol. 13, 110. https://doi.org/10.1186/1471-2377-13-110 (2013).
Cutler, P. Iron overload and psychiatric illness. Can. J. Psychiatry. 39, 8–11 (1994).
Kim, J. & Wessling-Resnick, M. Iron and mechanisms of emotional behavior. J. Nutr. Biochem. 25, 1101–1107 (2014).
Shah, F. H. et al. Neurological deficits among beta-thalassemia patients and its possible therapeutic intervention: a comprehensive review. J. Dow Univ. Health Sci. (JDUHS). 14, 83–90 (2020).
Koutelekos, J. & Haliasos, N. Depression and thalassemia in children, adolescents and adults. Health Sci. J. 7, 239 (2013).
Maes, M., Galecki, P., Chang, Y. S. & Berk, M. A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro)degenerative processes in that illness. Prog Neuropsychopharmacol. Biol. Psychiatry. 35, 676–692. https://doi.org/10.1016/j.pnpbp.2010.05.004 (2011).
Cantó, E. et al. Association between serum neurofilament light chain levels and long-term disease course among patients with multiple sclerosis followed up for 12 years. JAMA Neurol. 76, 1359–1366 (2019).
Srpova, B. et al. Serum neurofilament light chain reflects inflammation-driven neurodegeneration and predicts delayed brain volume loss in early stage of multiple sclerosis. Mult Scler. J. 27, 52–60 (2021).
Zerr, I. et al. Cerebrospinal fluid neurofilament light levels in neurodegenerative dementia: evaluation of diagnostic accuracy in the differential diagnosis of prion diseases. Alzheimers Dement. 14, 751–763. https://doi.org/10.1016/j.jalz.2017.12.008 (2018).
Gaetani, L. et al. Neurofilament light chain as a biomarker in neurological disorders. J. Neurol. Neurosurg. Psychiatry. 90, 870–881. https://doi.org/10.1136/jnnp-2018-320106 (2019).
Beste, C. et al. How minimal variations in neuronal cytoskeletal integrity modulate cognitive control. NeuroImage 185, 129–139 (2019).
Bagheri, M., Rezakhani, A., Roghani, M., Joghataei, M. T. & Mohseni, S. Protocol for three-dimensional confocal morphometric analysis of astrocytes. JoVE (Journal Visualized Experiments), e53113 (2015).
Abdelhak, A. et al. Glial activation markers in CSF and serum from patients with primary progressive multiple sclerosis: potential of serum GFAP as disease severity marker? Front. Neurol. 10, 280 (2019).
Wang, Y. F. & Parpura, V. Central role of maladapted astrocytic plasticity in ischemic brain edema formation. Front. Cell. Neurosci. 10, 129 (2016).
Torres-Platas, S., Nagy, C., Wakid, M., Turecki, G. & Mechawar, N. Glial fibrillary acidic protein is differentially expressed across cortical and subcortical regions in healthy brains and downregulated in the thalamus and caudate nucleus of depressed suicides. Mol. Psychiatry. 21, 509–515 (2016).
Arslan, B. & Zetterberg, H. Neurofilament light chain as neuronal injury marker–what is needed to facilitate implementation in clinical laboratory practice? Clin. Chem. Lab. Med. (CCLM). 61, 1140–1149 (2023).
Negi, D. et al. Molecular biomarkers of neuronal injury in epilepsy shared with neurodegenerative diseases. Neurotherapeutics, 1–12 (2023).
Hablitz, L. M. & Nedergaard, M. The glymphatic system: a novel component of fundamental neurobiology. J. Neurosci. 41, 7698–7711 (2021).
Plog, B. A. et al. Biomarkers of traumatic injury are transported from brain to blood via the glymphatic system. J. Neurosci. 35, 518–526 (2015).
Bavato, F. et al. Altered neuroaxonal integrity in schizophrenia and major depressive disorder assessed with neurofilament light chain in serum. J. Psychiat Res. 140, 141–148. https://doi.org/10.1016/j.jpsychires.2021.05.072 (2021).
Douillard-Guilloux, G., Guilloux, J. P., Lewis, D. A. & Sibille, E. Anticipated brain molecular aging in major depression. Am. J. Geriat Psychiatry. 21, 450–460 (2013).
Dohm, K., Redlich, R., Zwitserlood, P. & Dannlowski, U. Trajectories of major depression disorders: a systematic review of longitudinal neuroimaging findings. Aust NZ J. Psychiatry. 51, 441–454 (2017).
Michel, M. et al. Increased GFAP concentrations in the cerebrospinal fluid of patients with unipolar depression. Transl Psychiatry. 11, 308. https://doi.org/10.1038/s41398-021-01423-6 (2021).
Steinacker, P. et al. Glial fibrillary acidic protein as blood biomarker for differential diagnosis and severity of major depressive disorder. J. Psychiat Res. 144, 54–58 (2021).
Esnafoglu, E. et al. Evaluation of serum Neuron-specific enolase, S100B, Myelin basic protein and glial fibrilliary acidic protein as brain specific proteins in children with autism spectrum disorder. Int. J. Dev. Neurosci. 61, 86–91 (2017).
Al Shweiki, M. R. et al. Major depressive disorder: insight into candidate cerebrospinal fluid protein biomarkers from proteomics studies. Expert Rev. Proteom. 14, 499–514 (2017).
Bartzokis, G. et al. In vivo evaluation of brain iron in alzheimer disease using magnetic resonance imaging. Arch. Gen. Psychiatry. 57, 47–53 (2000).
Rouault, T. A. & Cooperman, S. in Seminars in Pediatric Neurology. 142–148 (Elsevier, 2013).
Nandar, W., Neely, E. B., Unger, E. & Connor, J. R. A mutation in the HFE gene is associated with altered brain iron profiles and increased oxidative stress in mice. Biochim. Biophys. Acta. 1832, 729–741. https://doi.org/10.1016/j.bbadis.2013.02.009 (2013).
Tuomainen, T. P. et al. Body iron is a contributor to oxidative damage of DNA. Free Radic. Res. 41, 324–328. https://doi.org/10.1080/10715760601091642 (2007).
Honda, K., Casadesus, G., Petersen, R. B., Perry, G. & Smith, M. A. Oxidative stress and redox-active iron in alzheimer’s disease. Ann. N. Y. Acad. Sci. 1012, 179–182. https://doi.org/10.1196/annals.1306.015 (2004).
Xian-hui, D. et al. Age-related changes of brain iron load changes in the frontal cortex in APPswe/PS1∆E9 Transgenic mouse model of alzheimer’s disease. J. Trace Elem. Med Biol. 30, 118–123 (2015).
Kenkhuis, B. Iron-immune interactions in Alzheimer’s disease (Leiden University, 2022).
Zhang, P. et al. Ferroptosis was more initial in cell death caused by iron overload and its underlying mechanism in parkinson’s disease. Free Radic. Biol. Med. 152, 227–234 (2020).
Shaki, F. et al. The effect of epicatechin on oxidative stress and mitochondrial damage induced by homocycteine using isolated rat hippocampus mitochondria. Res. Pharm. Sci. 12, 119 (2017).
Acknowledgements
We thank the staff of the Thalassemia Unit at Al-Zahra’a Teaching Hospital-Najaf city-Iraq for their help in the collection of samples. We also acknowledge the work of the highly skilled staff of the Asia Laboratory in measuring the biomarkers.
Funding
There was no specific funding for this specific study.
Author information
Authors and Affiliations
Contributions
Maha Abdul Saheb Ridhaa: Data curation, investigation, writing-original draft.Hussein Kadhem Al-Hakeim: Conceptualization, investigation, methodology, resources, supervision, validation, writing-review & editing.Mohammed K.Kahlol: Data curation, investigation, project administration, writing-review & editing.Tabarek Hadi Al-Naqeeb: Data curation, investigation, project administration, writing-review & editing.Mengqi Niu: Writing-review & editing.Michael Maes: Formal analysis, supervision, validation, visualization, writing-review & editing.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ridhaa, M.A.S., Al-Hakeim, H.K., Kahlol, M.K. et al. In transfusion-dependent thalassemia, neuronal damage biomarkers are associated with affective and chronic fatigue symptoms. Sci Rep 15, 32721 (2025). https://doi.org/10.1038/s41598-025-16757-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-16757-0