Abstract
Diabetic ketoacidosis (DKA) is the most common acute complication in people with diabetes. We aimed to assess the association of DKA with the risk of diabetic retinopathy (DR) and related ophthalmic interventions in individuals with type 2 diabetes (T2D). To ensure similar T2D management and severity at baseline between groups, we enrolled 1,007 T2D patients with and without DKA matched by anti-diabetic combination within the initial 3 months of diabetes diagnosis, gender, birth and diabetes diagnosis year in Taiwan National Health Insurance Research Database from 2000 to 2019. We employed Fine and Gray competing risk model to assess the risk of non-proliferative DR (NPDR), proliferative DR (PDR) and panretinal photocoagulation (PRP). Our results showed that patients with DKA had an increased risk of DR (adjusted subdistribution hazard ratio [SHR] 1.64 [95% CI, 1.34–2.01]) and PRP (SHR 1.43 [1.11–1.86]). The risk of NPDR is elevated when diabetes-to-DKA duration exceeded 24 months (SHR 2.15 [1.52–3.05]), while 1–24 months duration increased PDR risk (SHR 3.72 [1.76–7.88]). Patients with DKA onset at ages 46–55 and 56–65 showed specific PDR (SHR 1.82 [0.99–3.33]) and NPDR susceptibilities (SHR 6.52 [2.30–18.49]), respectively. Our study showed that DKA was associated with a higher risk of developing DR and requiring related ophthalmic interventions compared to a matched cohort with similar T2D baseline characteristics.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is the leading cause of preventable visual loss in adults aged 20–74 years and the seventh most common cause of blindness globally1,2. As diabetes prevalence increases to 10.9% by 2045 and diabetic retinopathy impacts more than a third of diabetic patients, DR is projected to affect one in 28 individuals worldwide1,3. Despite glycemic exposure being the main risk factor of DR, 18–21% of diabetic patients with intensive glycemic control (glycated hemoglobin [HbA1C] < 7.0) or duration less than 10 years still develop DR4. Hence, it is essential to identify other risk factors in the natural course of DR.
Unlike pure hyperglycemia, metabolic derangements in diabetic ketoacidosis (DKA) results from combined effects of elevated counterregulatory hormones (glucagon, epinephrine) and insulin deficiency5. Various contributing factors beyond poor compliance are acknowledged in DKA, such as stressors, newly diagnosed type 2 diabetes (T2D)6. Recent studies demonstrate that DKA has a distinct long-term impact on the central nervous system, including an increased incidence of Alzheimer’s disease and stroke7,8. Moreover, DKA recurrence at approximately 21.6% exposes patients to repeated insults9. Patients who manifest proliferative DR (PDR) 5 years after T2D diagnosis exhibit significantly higher proportion of DKA history than those without10. The presence of ketone bodies in the cerebrospinal fluid in patients with DKA underscores their ready penetration through blood-brain barrier (BBB) and their incomplete metabolism in central nervous system11. Subsequent neuroinflammation triggered by DKA after BBB breakdown shares pivotal chemokines in pathogenic pathway of DR12. Given the physical and functional similarities of BBB and blood-retinal barrier (BRB), and the crucial role of damaged BRB in DR development, evaluating the impact of DKA on DR risk and progression is essential for improving the cost-effectiveness of DR screening.
To our knowledge, this is the first study to investigate the influence of DKA on the development of DR in individuals with T2D, which accounts for over 99% of the diabetic population and 30–32% of DKA13,14,15. We aimed to study the effects of acidosis and ketosis on DR, while minimizing bias from variations in baseline diabetes status, using a national cohort matched for medication regimen, gender and birth and diabetes onset year. We also examined the DKA onset and the time from T2D to DKA in relation to DR severity.
.
Methods
Data source
We conducted a retrospective cohort study using data from the National Health Insurance Research Database (NHIRD), a comprehensive longitudinal dataset that covers over 99% of the Taiwanese population through mandatory enrollment16. This database provides reliable healthcare information, such as diagnosis codes (International Classification of Diseases, Ninth Revision and Tenth Revision, Clinical Modification [ICD-9-CM, ICD-10-CM]), prescription details (dosages and dates), ophthalmologic procedures. The high quality of NHIRD has been demonstrated through studies focusing on diabetes and DR17. Our study cohort consisted of a random subset of two million individuals from the NHIRD, also known as the Longitudinal Generation Tracking Database (LGTD). The follow-up period lasted two decades, from 2000 to 2019. This study was approved by the Ethics Institutional Review Board of Chang Gung Memorial Hospital (202201107B1).
Study design
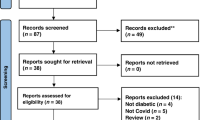
We identified newly-diagnosed T2D patients who had ≥ 1 hospitalization or ≥ 3 outpatient visits for T2D within a year (ICD-9-CM codes: 250 excluding 250.x1 or 250.x3; ICD-10-CM codes: E11) (Fig. 1, Supplementary Fig. 1)18,19. We excluded those with type 1 diabetes (ICD-9-CM codes: 250.x1, 250.x3; ICD-10-CM codes: E10), < 18 years of age, cancer history (ICD-9-CM codes: 140–208; ICD-10-CM codes: C00-C97), DKA preceding T2D, mortality during hospitalization due to DKA or within 3 months following the diagnosis of T2D or a lack of anti-diabetic prescription within the initial 3 months after T2D diagnosis. We matched each DKA patient having ≥ 1 DKA hospitalization (see Supplementary Table 1 for coding numbers) with one T2D patient without DKA by birth year, T2D diagnosis year, gender, and the initial pattern of anti-diabetic combination for 3 months at the outpatient department. Given the absence of biochemical data in NHIRD, this approach aimed to mitigate potential confounding related to baseline T2D status between groups and to better clarify the effect of DKA on DR at the population level. Glucose-lowering drugs were categorized by their mechanisms of action using the Anatomical Therapeutic Chemical code (ATC-code) before medication-matching (Supplementary Table 2). The three-month period was chosen as it aligns with HbA1C’s capacity to reflect average blood glucose levels over the same duration20. We analyzed and matched the initial anti-diabetic combination in the DKA group with the non-DKA group, considering only the medication classes from the prescription record ≥ 28 days, corresponding to one refill cycle for chronic disease prescriptions in NHIRD (Supplementary Fig. 2 A). The index date for the DKA group was the discharge date from DKA hospitalization if the duration from the initial diagnosis of T2D to DKA (T2D-to-DKA duration) exceeded 3 months; otherwise, it was 3 months after T2D diagnosis (Supplementary Fig. 2B)21. The non-DKA control had a pseudo-index date same as the matched individual with DKA to minimize immortal time bias. The matched pairs did not exhibit any outcomes or experience mortality before their respective index or pseudo-index dates.
The selection flow chart. LGTD: Longitudinal Generation Tracking Database. T2D: type 2 diabetes. T1D: type 1 diabetes. DKA: diabetic ketoacidosis. DME: diabetic macular edema. VH: vitreous hemorrhage. RD: retinal detachment. PDR: proliferative diabetic retinopathy. NPDR: nonproliferative diabetic retinopathy. IVI: intravitreal injection. PRP: panretinal photocoagulation. PPV: pars plana vitrectomy.
Outcomes
Our study aimed to evaluate DR and diabetes-related ocular complications (diabetic macular edema [DME] and retinal detachment [RD]) between DKA and non-DKA groups, which were recorded on ≥ 3 outpatient visits or ≥ 1 inpatient diagnosis (see Supplementary Table 1 for coding numbers). To better recognize the effect of DKA on different stages of DR, we classified DR into non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR), as the progression of NPDR to PDR was the main cause of visual decline and ophthalmologic complications (see Supplementary Table 1 for coding numbers). In cases where an individual received both PDR and NPDR diagnoses, we defined DR based on the first incidence to occur. Ophthalmologic procedures and surgical intervention that are performed to prevent advanced DR or at visual-threatening stage were also analyzed, including panretinal photocoagulation (PRP), pars plana vitrectomy (PPV) and intravitreal injection (IVI) (see Supplementary Table 3 for payment codes for surgery).
Statistical analysis
The study individuals were followed from T2D diagnosis until study outcomes, death or the end of 2019. Comorbidities that could affect DR progression were identified, including hypertension, coronary artery disease, chronic kidney disease (CKD), dialysis, chronic obstructive pulmonary disease (COPD), smoking, obesity, liver cirrhosis, autoimmune diseases (e.g. polymyositis, dermatomyositis, systemic lupus erythematosus, Sjogren’s disease, rheumatoid arthritis) (see Supplementary Table 1 for coding numbers)22,23. Additionally, We extracted medications previously demonstrated to either benefit DR prevention or be associated with a higher risk of vitreous hemorrhage, specifically if exposure ≥ 90 days within a year before index date was confirmed, such as statin, antiplatelets and anticoagulants17,24. Continuous variables were presented as means with standard deviation (SD) or median with lower and upper quartiles (Q1 and Q3), and categorical variables were reported as numbers and percentages. Categorical variables were assessed using Pearson’s χ2 test. To evaluate the subdistribution hazard ratio (SHR) between the two groups while considering death as a competing risk, we employed the Fine and Gray competing risk model25. Adjusted SHR were calculated to account for covariates showing significant differences between the two groups, including income level, CKD, COPD, smoking, obesity, use of antiplatelets/anticoagulation, and use of statins. To ensure model stability, multicollinearity diagnostics were performed: variance inflation factors (VIFs) for all covariates were < 5, and pairwise Cramer’s V coefficients for categorical variables were < 0.5, indicating no significant collinearity26. Covariates were retained based on clinical relevance, statistical significance, and absence of critical collinearity. Cumulative incidence of outcomes and statistical significance were assessed using Gray’s test. Furthermore, we used restricted cubic splines with four knots at fixed percentiles (5th, 35th, 65th, and 95th) to model continuous variables, including age at onset (or pseudo-onset) of DKA and the T2D-to-DKA duration, with DR, NPDR, PDR and PRP. Statistical significance was established for two-sided P values < 0.05. All analyses were conducted using SAS. Version 9.4 (SAS Inc., Cary, NC, USA).
Results
Demographics
A total of 288,542 patients with the diagnosis of T2D were enrolled for this study. Among those eligible patients, 1,815 were in the DKA group and 133,382 were in the non-DKA group. After one-to-one ratio matching, 1,007 patients enrollees in each group were analyzed (Table 1). The study population had a mean age of 52 years old at T2D diagnosis and 58.2% was male. The median follow-up duration for death was 6.4 years for the DKA group and 8.6 years for the non-DKA group. The mean duration from the diagnosis of T2D to DKA was 47.7 months. Baseline comorbidities were similar between groups, except CKD, COPD, smoking, and obesity. The predominance of CKD and COPD and/or smoking in DKA group may account for the fact that urinary tract infections and pneumonia commonly serve as most common precipitating factors for DKA27. Metformin was the most common glucose-lowering drug that > 60% of patients received during the first 3 months in both groups, aligning with the prevailing consensus of its status as a first-line therapy for diabetes. None of the patients in either group received glucagon-like peptide 1 (GLP-1) or sodium–glucose cotransporter 2 (SGLT2) inhibitors during the initial 3-month period following diagnosis. During the one-year period before the index/pseudo-index date, a higher proportion of non-DKA group patients were administered antiplatelets/anticoagulation and statins.
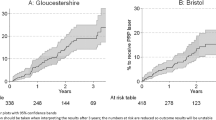
Association between DKA and risks of DR and PRP
The 2,014 patients had a total of 130 (12.9%) and 182 (18.1%) encounters of DR in non-DKA group and DKA group respectively (Table 2). Given the higher risk of death in DKA group (HR, 3.42; CI, 2.78–4.21; P < 0.001), which escalated with the onset age of DKA and T2D-to-DKA duration, the Fine-Gray SHR model was used to estimate outcome incidence considering competing risk over time (Supplementary Table 4, Supplementary Fig. 3). Cumulative incidence curves demonstrated an elevated risk of developing DR, PDR, NPDR and PRP in individuals with DKA (Fig. 2). The DKA group had significantly higher risk of developing DR (SHR, 1.71; CI, 1.43–2.05; P < 0.001), PDR (SHR, 1.35; CI, 1.07–1.69; P = 0.010) and NPDR (SHR, 1.62; CI, 1.31–2.01; P < 0.001). As for the ophthalmological intervention, patients with DKA had higher risk to receive PRP (SHR, 1.52; CI, 1.22–1.89; P < 0.001) and IVI (SHR, 1.64; CI, 1.11–2.41; P = 0.012). After adjusting for comorbidities that significantly differed between the two groups, the DKA group still had a higher cumulative risk for DR (SHR, 1.64; CI, 1.34–2.01; P < 0.001), PDR (SHR, 1.33; CI, 1.04–1.71; P = 0.026), NPDR (SHR, 1.51; CI, 1.20–1.91; P < 0.001), PRP (SHR, 1.43; CI, 1.11–1.86; P = 0.007) and IVI (SHR, 1.74; CI, 1.08–2.81; P = 0.024). The restricted cubic spline curve revealed a progressive rise in the adjusted SHR for DR, NPDR, PDR, and PRP in correlation with an increasing T2D-to-DKA duration (Supplementary Fig. 4A-D). However, these SHR markedly increase with the onset age of DKA from 46 to 55 years old, followed by a gradual decline from 56 to 65 years old (Supplementary Fig. 5A-D). Notably, the SHR for the DKA group surpassed that of the non-DKA group at all ages.
Cumulative incidence of (A) DR, (B) PDR, (C) NPDR, and (D) PRP in patients with and without DKA (Gray’s test P < 0.001 for all). DR: diabetic retinopathy. PDR: proliferative diabetic retinopathy. NPDR: nonproliferative diabetic retinopathy. PRP: panretinal photocoagulation. DKA: diabetic ketoacidosis.
Association between T2D-to-DKA duration and risks of PDR and NPDR
The median T2D-to-DKA duration was 28.3 months (IQR 0–79.2). Thus, we classified patients into three groups: 0 months, 1–24 months, and > 24 months (Table 3). Compared with the non-DKA group, the DKA group had a higher risk of PDR in the 1–24 months group (SHR, 2.50; CI, 1.42–4.39; P < 0.001) and of NPDR in the > 24 months group (SHR, 2.18; CI, 1.60–2.96; P < 0.001). This remained significant after adjusting for baseline differences. While the risk of receiving PRP was elevated in both the 1–24 months group (SHR, 1.77; CI, 1.07–2.91; P = 0.025) and the > 24 months group (SHR, 1.53; CI, 1.12–2.09; P = 0.008), this risk became statistically insignificant after adjustment (P = 0.077 and 0.153). Conversely, the 0-month group did not exhibit an increased risk for PDR (SHR, 1.41; CI, 0.90–2.20; P = 0.129) or NPDR (SHR, 1.00; CI, 0.65–1.55; P = 1.000).
Association between DKA onset age and risks of PDR and NPDR
Furthermore, we grouped the patients by age at DKA diagnosis: 18–45, 46–55, 56–65, and > 65 years, based on their median age of 54 years (IQR 45–66) (Table 3). After adjusting for baseline differences, the DKA group aged 46–55 had a higher risk of PDR (SHR, 1.82; CI, 0.99–3.33; P = 0.054), although not significant, and the one aged 56–65 had a higher risk of NPDR (SHR, 6.52; CI, 2.30–18.49; P < 0.001) than the non-DKA control. The risk of requiring PRP was only significantly elevated in the 56–65 years age group after adjustment (SHR, 2.52; CI, 1.11–5.75; P = 0.028). No significant risk of PDR or NPDR was observed in the > 65 years group.
Subgroup analysis of DKA patients
In our subgroup analyses focused on DKA patients only, we used 0 months of T2D-to-DKA duration and an age range of 18–45 years at DKA diagnosis as reference groups (Table 4). Following adjustment for baseline differences, we observed a 99% higher risk of PDR in patients with a duration of 1–24 months (SHR, 1.99; CI, 1.15–3.44; P = 0.013) compared to those with DKA duration of 0 month. Furthermore, the risk of NPDR was 77% higher in patients with a duration of 1–24 months (SHR, 1.77, 95% CI 1.00–3.15, P = 0.050) and 159% higher in patients with a duration of > 24 months than those with DKA duration of 0 month (SHR, 2.59, 95% CI 1.62–4.14, P < 0.001). While stratifying by age at DKA diagnosis indicated that the 46–55 and 56–65 age groups had a greater risk of developing PDR and NPDR than the 18–45 group, these differences did not reach statistical significance. In contrast, the > 65 years age group exhibited more than a 50% lower risk of PDR (SHR, 0.31; 95% CI, 0.13–0.71; P = 0.006), NPDR (SHR, 0.46; 95% CI, 0.23–0.91; P = 0.027), and PRP (SHR, 0.28; 95% CI, 0.13–0.62; P = 0.002) than the 18–45 years group after adjusting for baseline differences.
Discussion
We showed that DKA patients acquired higher risk of DR and related surgeries than controls matched with similar anti-diabetic medication, gender and birth and diabetes onset year. We also found that the risks of PDR and NPDR varied by the duration from T2D to DKA and by age at DKA diagnosis. Our study demonstrated that DKA as an important predictor of DR risk and identifies specific risk profiles is associated with DKA among similar T2D baseline characteristics.
Halting the progression from NPDR to PDR is crucial, as nearly half can result in severe vision loss without intervention. Both CLARITY and DRCR Retina Network studies have demonstrated efficacy of IVI with anti-vascular endothelial growth factor (VEGF) drugs in treating PDR, but their demanding schedules and adherence requirements pose substantial challenges to patients and make PRP indispensable28. Our study reveals that patients experiencing DKA face an elevated risk of requiring both IVI and PRP, aligning with the observed increased risk of DR. Patients who developed DKA within one month of their T2D diagnosis did not show an increased risk of DR. This subgroup represents individuals with DKA-prone diabetes, a milder form of T2D, who can often discontinue insulin and achieve normoglycemia through lifestyle modifications and oral hypoglycemic agents29. Furthermore, DKA recurrence appeared less likely in patients whose initial diabetes presentation was DKA30. Our findings also revealed a higher risk of PDR in DKA patients aged 46–55 years, with a T2D to DKA duration of 1–24 months. Conversely, the risk of NPDR and intervention with PRP were elevated in those aged 56–65 years with a T2D to DKA duration exceeding 24 months. The within group analysis of DKA also showed higher risk of PDR in 1–24 months group and of NPDR in > 24 months group. Numerous studies (SN-DREAMS-II, BISED II, SiMES, SINDI) have shown that PDR primarily develops from NPDR rather than absence of retinal diseases31. In addition, PDR progression links to younger age at diabetes diagnosis and can be mitigated by PRP32. Since individuals with more severe biochemical profiles of DKA also exhibit shorter diabetes durations and younger onset ages, we hypothesize that patients aged 46–55 years and with a duration of 1–24 months are at a higher risk of developing PDR due to more severe DKA33. PRP may provide protective effect on the progression from NPDR to PDR in patients aged 56–65 years and those with a T2D to DKA duration exceeding 24 months. Furthermore, individuals aged over 65 years demonstrated a higher risk of DR than their non-DKA counterparts; however, among DKA patients, those over 65 years had the lowest DR risk compared to patients aged 18–45 years, even after applying Fine-Gray competing risk models for mortality. This finding likely reflects survivor bias, as the > 65 year-old group experienced the highest mortality risk (HR, 4.67, 95% CI 3.57–6.12, P < 0.001; Supplementary Table 4), leading to truncated follow-up. The reduced DR incidence should therefore be interpreted in the context of limited survival time rather than a true protective association. Finally, our data revealed that DKA accelerates DR progression and the need for surgical intervention. The duration from T2D to DR was shorter in patients with DKA (median 7.7 years, IQR 4.8–11.9) compared to those without (median 9.8 years, IQR 5.8–14.2). Patients with DKA also required PRP sooner (median 7.7 years, IQR 4.6–11.0) than those without (median 9.4 years, IQR 5.9–13.3). Considering that HbA1C and diabetes duration together accounted for only approximately 11% of the risk of DR development, our study underscored the necessity of incorporating additional independent factors like DKA into DR screening protocols34. While the American Diabetes Association (ADA) and International Council of Ophthalmology (ICO) recommend a screening interval of 1–2 years for diabetes patients without DR at baseline in high-resource settings, our findings suggest that DKA patients might benefit from more frequent assessments to ensure timely detection and prevention strategies of PDR, given their unique risk profile35. Moreover, With the increasing use of sodium-glucose co-transporter-2 inhibitors in T2D, caution is necessary regarding their long-term use due to the heightened risk of euglycemic DKA in elderly patients36. Subsequent studies may need to explore whether this demographic faces an elevated risk of DR progression.
The increased risk of DR associated with DKA may be attributed to several mechanisms related to hyperglycemic crisis, ketonemia and acidosis. First, the high osmotic pressure during a DKA episode can disrupt the BBB, potentially damaging the integrity of the BRB37. Subsequently, the rapid decrease in extracellular osmolarity following treatment may lead to osmolyte stasis and protein accumulation, contributing to vascular hyperpermeability and endothelial cell leukostasis, the key factors in DR development38. Second, severe hyperglycemia in DKA can stimulate aerobic glycolysis in retinal pigmented epithelial cells, the key components of BRB, and lead to oxidative stress. Oxidative stress will activate Rac1-Nox2 pathway and cytosolic reactive oxygen species in the retina, further promoting DR39. Third, hyperglycemic crises in DKA are associated with elevated pro-inflammatory cytokines and C-reactive protein, creating a systemic pro-inflammatory state. Neuroinflammatory markers observed at the disrupted BBB of DKA patients are also elevated in the vitreous of diabetic patients and linked to the progression of PDR12,40,41. Finally, increased VEGF expression is detected in the retina of metabolic acidosis-induced rats, a key factor in neovascularization42. We propose that the breakdown of the BRB, oxidative stress, elevated inflammatory factors, and VEGF signaling in DKA collectively contribute to the intensified progression of DR.
Current ADA guidelines call for a dilated retinal exam at T2D diagnosis and at least annual follow‑up, with interval adjustments based on DR severity and glycemic control43,44. Our data—showing an early, steep rise in DR incidence after DKA (Fig. 2) and persistently higher SHR in the DKA group (Supplementary Fig. 4)—suggest that T2D patients with a DKA episode represent a distinct high‑risk subgroup. We therefore recommend adding a retinal evaluation at the time of DKA diagnosis, followed by more frequent surveillance than in the general T2D population (e.g., biennial without baseline retinopathy or annual with retinopathy). Additionally, intensive follow-up is advised for younger patients (age < 55) and those who experience a DKA episode within two years of their T2D diagnosis, as they warrant prioritized monitoring due to their heightened risk of developing PDR. Although the optimal interval requires validation in larger, multicenter cohorts, earlier and tighter monitoring after DKA is warranted to detect and treat emerging retinopathy promptly.
This study has some limitations. First, biochemical lab data (e.g., HbA1C, C-peptide, islet autoantibodies) were unavailable in the NHIRD, limiting our ability to assess glycemic control and accurately classify diabetes type. For example, cases of latent autoimmune diabetes in adults or monogenic diabetes may be misclassified as T2D in the absence of autoantibody or C-peptide testing45. Patients with severe insulin deficiency (low C-peptide) and poor glycemic control (elevated HbA1c) may experience more rapid progression of DR, potentially confounding associations between DKA and DR severity46.To address this limitation, we leveraged the NHIRD’s reimbursement policies to infer baseline glycemic control using initial three-month outpatient diabetic medication patterns, ensuring comparability across cohorts. Nevertheless, future studies incorporating linked laboratory data are warranted to improve diagnostic accuracy and enable adjustment for metabolic and immunologic variables. Second, DKA cases were identified solely by ICD codes. A recent validation study by Hodzic-Santor et al. reported high specificity (99.6%) and negative predictive value (99.7%) for ICD-coded DKA diagnoses, but only moderate positive predictive value (67.0%) and sensitivity (74.9%), suggesting potential for misclassification47. To reduce this risk, we restricted our analysis to DKA diagnoses documented during hospitalizations—where clinical confirmation and treatment are more likely—and excluded cases with DKA diagnoses preceding the diagnosis of T2D. For future research, we recommend combining ICD codes with laboratory criteria (e.g., pH ≤ 7.3, bicarbonate ≤ 18 mmol/L, anion gap > 10 mEq/L, ketonemia/ketonuria), medication records (e.g., insulin infusion), and confirmed hospitalization for DKA as the primary discharge diagnosis. This approach could improve case identification and causal inference in observational studies. Third, functional outcomes such as visual acuity changes were not evaluated, limiting our ability to assess DR progression. This limitation reflects the absence of clinical detail in claims data. Future studies should incorporate ophthalmologic data to better capture the functional impact of DR in patients with DKA. Fourth, the generalizability of our findings is limited by the ethnic composition of the NHIRD, which comprises over 95% Han Chinese, with small proportions of indigenous Taiwanese (∼2%), South Asians (∼1.3%), and Western residents (∼0.1%)48. Given that racial differences in DKA risk have been reported elsewhere, particularly among Black individuals in Western countries, future studies should examine similar associations using international or ethnically diverse datasets49,50. Fifth, antidiabetic medication use was assessed only during the initial 3-month period to ensure comparable baseline treatment, consistent with the landmark analysis design51,52. Fixing exposure at the index date mitigates immortal time bias but excludes post-landmark changes in treatment or disease status. While this strengthens causal inference for DKA effects, it precludes assessment of treatment modifications occurring after the landmark period, including later SGLT2 inhibitor initiation. Future studies with time-varying analyses are warranted to address these limitations. Finally, the wide confidence intervals observed in the stratified analyses likely reflect limited statistical power due to small sample sizes within subgroups, and these findings should be viewed as exploratory. This constraint is partly due to the substantial number of exclusions required to identify comparable initial diabetes regimens among individuals without DKA. To improve the robustness and inclusiveness of future analyses, we plan to examine the full population dataset to better support generalizable conclusions.
Conclusions
Our study revealed that DKA is associated with an increased risk of DR and a higher likelihood of receiving intervention in T2D patients with similar diabetic medication, year of birth, year of diabetes diagnosis, and gender, rather than the general T2D population. We also observed a shorter duration for DKA patients to develop DR and undergo surgical intervention following the onset of T2D. Furthermore, we elucidated that younger age at DKA onset or a shorter T2D-to-DKA duration is associated with a higher risk of developing PDR, a more severe form of the disease. Building on ADA guidelines, we propose incorporating DKA history into DR screening protocols by performing an initial retinal exam at the time of DKA diagnosis, with follow‑up thereafter more frequent than standard ADA recommendations to address the accelerated retinopathy risk in this population.
Data availability
Data are available from the corresponding author upon formal request.
References
Cheung, N., Mitchell, P. & Wong, T. Y. Diabetic retinopathy. Lancet 376, 124–136 (2010).
Flaxman, S. R. et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 5, e1221–e1234 (2017).
Saeedi, P. et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9(th) edition. Diabetes Res. Clin. Pract. 157, 107843 (2019).
Yau, J. W. et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 35, 556–564 (2012).
Umpierrez, G. E. et al. Hyperglycemic crises in adults with diabetes: A consensus report. Diabetes Care. 47, 1257–1275 (2024).
Elendu, C. et al. Comprehensive review of diabetic ketoacidosis: an update. Ann. Med. Surg. (Lond). 85, 2802–2807 (2023).
Chen, Y. L. et al. Diabetic ketoacidosis further increases risk of alzheimer’s disease in patients with type 2 diabetes. Diabetes Res. Clin. Pract. 147, 55–61 (2019).
Chen, Y. L. et al. Long-term risk of stroke in type 2 diabetes patients with diabetic ketoacidosis: A population-based, propensity score-matched, longitudinal follow-up study. Diabetes Metab. 43, 223–228 (2017).
Mays, J. A. et al. An evaluation of recurrent diabetic ketoacidosis, fragmentation of care, and mortality across chicago, Illinois. Diabetes Care. 39, 1671–1676 (2016).
Gange, W. S. et al. Incidence of proliferative diabetic retinopathy and other neovascular sequelae at 5 years following diagnosis of type 2 diabetes. Diabetes Care. 44, 2518–2526 (2021).
Ohman, J. L. Jr. et al. The cerebrospinal fluid in diabetic ketoacidosis. N Engl. J. Med. 284, 283–290 (1971).
Hoffman, W. H., Stamatovic, S. M. & Andjelkovic, A. V. Inflammatory mediators and blood brain barrier disruption in fatal brain edema of diabetic ketoacidosis. Brain Res. 1254, 138–148 (2009).
Sheen, Y. J. et al. Trends in prevalence and incidence of diabetes mellitus from 2005 to 2014 in Taiwan. J. Formos. Med. Assoc. 118 (Suppl 2), S66–S73 (2019).
Ebrahimi, F., Kutz, A., Christ, E. R. & Szinnai, G. Lifetime risk and health-care burden of diabetic ketoacidosis: A population-based study. Front. Endocrinol. (Lausanne). 13, 940990 (2022).
Wang, Z. H., Kihl-Selstam, E. & Eriksson, J. W. Ketoacidosis occurs in both type 1 and type 2 diabetes–a population-based study from Northern Sweden. Diabet. Med. 25, 867–870 (2008).
Hsieh, C. Y. et al. Taiwan’s National health insurance research database: past and future. Clin. Epidemiol. 11, 349–358 (2019).
Kang, E. Y. et al. Association of Statin therapy with prevention of Vision-Threatening diabetic retinopathy. JAMA Ophthalmol. 137, 363–371 (2019).
Chao, C. T. et al. The risk trajectory of different cardiovascular morbidities associated with chronic kidney disease among patients with newly diagnosed diabetes mellitus: a propensity score-matched cohort analysis. Cardiovasc. Diabetol. 20, 86 (2021).
Chung, Y. C. et al. Cost-effectiveness of diabetic retinopathy screening for newly diagnosed type 2 diabetic patients: A nationwide population-based propensity score-matched cohort study. Asia Pac. J. Ophthalmol. (Phila). 13, 100071 (2024).
Sherwani, S. I. et al. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark. Insights. 11, 95–104 (2016).
Hsu, C. N. et al. Continuity and completeness of electronic health record data for patients treated with oral hypoglycemic agents: findings from healthcare delivery systems in Taiwan. Front. Pharmacol. 13, 845949 (2022).
Kim, B. Y. et al. Prevalences of diabetic retinopathy and nephropathy are lower in Korean type 2 diabetic patients with non-alcoholic fatty liver disease. J. Diabetes Investig. 5, 170–175 (2014).
Wat, N., Wong, R. L. & Wong, I. Y. Associations between diabetic retinopathy and systemic risk factors. Hong Kong Med. J. 22, 589–599 (2016).
Kim, K. E. et al. Antithrombotic medication and the risk of vitreous hemorrhage in atrial fibrillation: Korean National health insurance service National cohort. Yonsei Med. J. 60, 65–72 (2019).
Huang, J. Y. et al. Prediabetes is associated with increased risk of heart failure among patients with atrial fibrillation. Diabetes Care. 46, 190–196 (2023).
Vatcheva, K. P., Lee, M., McCormick, J. B. & Rahbar, M. H. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiol. (Sunnyvale). 6, 226–227 (2016).
Cheng, Y. C. et al. Clinical outcomes of septic patients with diabetic ketoacidosis between 2004 and 2013 in a tertiary hospital in Taiwan. J. Microbiol. Immunol. Infect. 49, 663–671 (2016).
Jampol, L. M., Glassman, A. R. & Sun, J. Evaluation and care of patients with diabetic retinopathy. N Engl. J. Med. 382, 1629–1637 (2020).
Smiley, D., Chandra, P. & Umpierrez, G. E. Update on diagnosis, pathogenesis and management of ketosis-prone type 2 diabetes mellitus. Diabetes Manag (Lond). 1, 589–600 (2011).
Michaelis, M., Shochat, T., Shimon, I. & Akirov, A. Features and long-term outcomes of patients hospitalized for diabetic ketoacidosis. Diabetes Metab. Res. Rev. 37, e3408 (2021).
Sabanayagam, C. et al. Incidence and progression of diabetic retinopathy: a systematic review. Lancet Diabetes Endocrinol. 7, 140–149 (2019).
Harris Nwanyanwu, K. et al. Predicting development of proliferative diabetic retinopathy. Diabetes Care. 36, 1562–1568 (2013).
Wu, X. Y. et al. Clinical profiles, outcomes and risk factors among type 2 diabetic inpatients with diabetic ketoacidosis and hyperglycemic hyperosmolar state: a hospital-based analysis over a 6-year period. BMC Endocr. Disord. 20, 182 (2020).
Lachin, J. M. et al. Effect of glycemic exposure on the risk of microvascular complications in the diabetes control and complications trial–revisited. Diabetes 57, 995–1001 (2008).
Vujosevic, S. et al. Screening for diabetic retinopathy: new perspectives and challenges. Lancet Diabetes Endocrinol. 8, 337–347 (2020).
Liu, J. et al. Sodium-glucose co-transporter-2 inhibitors and the risk of diabetic ketoacidosis in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Diabetes Obes. Metab. 22, 1619–1627 (2020).
Burks, S. R. et al. Blood-brain barrier opening by intracarotid artery hyperosmolar mannitol induces sterile inflammatory and innate immune responses. Proc. Natl. Acad. Sci. U S A. 118 (18), e2021915118 (2021).
Hoorn, E. J. et al. Preventing a drop in effective plasma osmolality to minimize the likelihood of cerebral edema during treatment of children with diabetic ketoacidosis. J. Pediatr. 150, 467–473 (2007).
Duraisamy, A. J., Mishra, M., Kowluru, A. & Kowluru, R. A. Epigenetics and regulation of oxidative stress in diabetic retinopathy. Invest. Ophthalmol. Vis. Sci. 59, 4831–4840 (2018).
Aveleira, C. A. et al. TNF-alpha signals through PKCzeta/NF-kappaB to alter the tight junction complex and increase retinal endothelial cell permeability. Diabetes 59, 2872–2882 (2010).
Nawaz, M. I. et al. Autocrine CCL2, CXCL4, CXCL9 and CXCL10 signal in retinal endothelial cells and are enhanced in diabetic retinopathy. Exp. Eye Res. 109, 67–76 (2013).
Zhao, R. et al. Differential expression of Mir-1 26 and vascular endothelial growth factor in retinal cells of metabolic Acidosis-Induced neonatal rats. J. Nanosci. Nanotechnol. 15, 2088–2093 (2015).
American Diabetes Association Professional Practice C. 12. Retinopathy, neuropathy, and foot care: standards of care in Diabetes-2025. Diabetes Care. 48, S252–S265 (2025).
American Diabetes Association Professional Practice C. ; 48:S128-S145.6. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes-2025. Diabetes Care (2025).
American Diabetes Association Professional Practice C. 2. Diagnosis and classification of diabetes: standards of care in Diabetes-2025. Diabetes Care. 48, S27–S49 (2025).
Chung, J. O., Cho, D. H., Chung, D. J. & Chung, M. Y. Relationship between serum C-peptide level and diabetic retinopathy according to estimated glomerular filtration rate in patients with type 2 diabetes. J. Diabetes Complications. 29, 350–355 (2015).
Hodzic-Santor, B. et al. Validation of the diagnostic accuracy levels of international classification of diseases, 10th revision codes for diabetic ketoacidosis: A multicentre, Cross-sectional study of adults. Can. J. Diabetes. 48, 227–232 (2024).
Chung, T. L. et al. The association of socioeconomic status on kidney transplant access and outcomes: a nationwide cohort study in Taiwan. J. Nephrol. 37, 1563–1575 (2024).
Chen, I. C. et al. Association of antidiabetic medications with depression risk and All-Cause mortality in type 2 diabetes: A TriNetX-Based cohort study. Diabetes Res. Clin. Pract. 223, 112167 (2025).
McCoy, R. G. et al. Sociodemographic, clinical, and Treatment-Related factors associated with hyperglycemic crises among adults with type 1 or type 2 diabetes in the US from 2014 to 2020. JAMA Netw. Open. 4, e2123471 (2021).
Dafni, U. Landmark analysis at the 25-year landmark point. Circ. Cardiovasc. Qual. Outcomes. 4, 363–371 (2011).
Morgan, C. J. Landmark analysis: A primer. J. Nucl. Cardiol. 26, 391–393 (2019).
Acknowledgements
The authors thank the participating physicians, Health Information and Epidemiology Laboratory, and the patients involved in this study.
Funding
This study has been supported by grants from Chang Gung Memorial Hospital (CFRPG6M0021), Chiayi, Taiwan.
Author information
Authors and Affiliations
Contributions
Research idea, study design, data interpretation, first draft of the manuscript: YKC; data acquisition and statistical analysis: CPL; discussion of the work; CHL, NKW, WCW and CHL; review and revision of the manuscript: YHC and YHY.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have declared that no potential conflict of interest relevant to this article exists.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, YK., Lai, CH., Wang, NK. et al. Association of diabetic ketoacidosis and retinopathy in patients with type 2 diabetes: a nationwide cohort study. Sci Rep 15, 33594 (2025). https://doi.org/10.1038/s41598-025-18806-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18806-0