Abstract
Periodontitis has been linked to cardiovascular disease (CVD), suggesting that oral care may play a role in CVD prevention. In contrast, hypertension has been linked to oral health; however, its association with toothbrushing habits is unclear. Therefore, this study aimed to investigate the relationship between toothbrushing habits and hypertension. A total of 941 participants (361 men, mean age: 67 ± 11 years) from a 2019 community-based study conducted in Tarumizu City were included. Hypertension was defined as systolic BP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or use of antihypertensive medications. Toothbrushing habits were assessed using a questionnaire, and oral health was evaluated by dentists. The mean BP was 132 ± 17/78 ± 11 mmHg, with a hypertension prevalence of 56%. Participants reported toothbrushing rates of 33% upon waking, 8% before breakfast, 69% after breakfast, 48% after lunch, 4% before dinner, 42% after dinner, and 51% before sleeping. In the univariable analysis, both the timing of toothbrushing (after breakfast, after lunch, or before sleeping) and brushing frequency (≥ 3 times/day) were significantly associated with a lower prevalence of hypertension. Multivariable analysis revealed a significant association between toothbrushing after breakfast and hypertension. In conclusion, toothbrushing after breakfast was independently associated with a reduced risk of hypertension.
Similar content being viewed by others
Introduction
Hypertension is the leading risk factor for cardiovascular disease (CVD), making adequate blood pressure (BP) control crucial for CVD prevention1. Various strategies to decrease BP, including diet, exercise, and drug therapy, have been explored to achieve this goal. In Japan, BP control remains suboptimal, as some patients exhibit uncontrolled hypertension despite medications, while others remain untreated2. Therefore, identifying modifiable lifestyle factors associated with hypertension could help improve BP control.
The oral cavity harbors over 700 microbial species. As such, poor oral hygiene can lead to gum disease and periodontitis, a complex infection involving multiple gram-negative anaerobic bacteria that is associated with various systemic diseases, including rheumatism3, diabetes4, and non-alcoholic fatty liver5,6. Notably, oral health has been linked to CVDs, independent of other risk factors such as age, sex, and lifestyle (e.g., dyslipidemia, hypertension, diabetes, smoking)7,8,9.
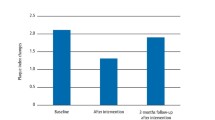
Periodontitis treatment has been shown to improve arterial function and prevent CVD. For example, patients with coronary artery disease demonstrated enhanced endothelial function, as evidenced by increased flow-dependent vasodilation 6 months following periodontal treatment10. A systemic review and meta-analysis demonstrated similar results, suggesting that periodontal disease treatment improves endothelial function and reduces atherosclerosis biomarkers11. Given the connection between periodontal disease and hypertension, oral care, particularly toothbrushing habits, becomes paramount in periodontitis prevention. A large cohort study in Scotland investigated the self-reported frequency of toothbrushing, reporting that low frequency was a risk factor for CVD development12. This was consistent with the findings of a study in Japan, which asserted that toothbrushing frequency and duration were associated with cardiovascular events13. Although few studies have explored the timing of toothbrushing and CVD, some evidence suggests that nighttime toothbrushing may reduce the CVD risk in patients ≥ 20 years admitted for surgery, testing, or medical treatment14.
While the relationship between periodontal diseases and hypertension has been established15, as reported by a randomized intervention trial showing that intensive periodontal treatment reduced systolic BP16, the influence of toothbrushing habits on BP control remains unclear. Thus, this study aimed to investigate the relationship between toothbrushing habits and hypertension.
Methods
Study population
A flowchart depicting the participant selection process is presented in Fig. 1. Since 2017, we have been conducting a regional study in Tarumizu, a city in Japan17,18. Study participants include residents over the age of 40 who live in Tarumizu and responded to our request to participate in the study. Participants were recruited through announcements such as the city bulletin, community notice boards, online announcements, local health programs, and postcards sent by mail. There are no other exclusion criteria. Of the participants in the 2019 Tarumizu study, 81 participants without teeth and three with missing data were excluded. Ultimately, 940 participants were included in the final analysis.
Written informed consent was obtained from all participants prior to the study. This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Ethics Committee of the Graduate School of Medical and Dental Sciences at Kagoshima University (No. 170351).
Data collection
Regarding the study participants’ medical history, we asked whether or not they were taking antihypertensive drugs, hypoglycemic drugs, or lipid-lowering drugs. Further, we asked them whether they were current smokers, have smoked in the past, or have never smoked. We defined both former and current smokers as smokers, and categorized participants into two groups: smokers and non-smokers. Educational history was obtained using a questionnaire, and nutritional intake was assessed using the Brief-Type Self-Administered Diet History Questionnaire (BDHQ)19. Body mass index (BMI) was calculated by dividing the weight (kg) by the square of height (m2).
BP measurement and definition of hypertension
Experimental health nurses measured BP using the oscillometric method during the community-based study. Measurements were taken in a seated position after a 5-min rest period. In cases where BP ≥ 180 mmHg (or higher than the usual value), a second measurement was obtained, and the average was used for analysis. Hypertension was defined as systolic BP ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or the use of antihypertensive medications.
Evaluation of toothbrushing habits and oral health
A questionnaire was administered to investigate toothbrushing habits. Participants reported timing and frequency of brushing at these specific times: upon waking, before and after breakfast, after lunch, before and after dinner, and before sleeping. Frequent toothbrushing was defined as brushing ≥ 3 times per day. In addition, participants indicated their brushing duration per session as follows: ≤ 30 s, 30–60 s, 1–2 min, 2–3 min, and ≥ 3 min. Long brushing duration was defined as brushing duration ≥ 2 min. Oral assessment with teeth enumeration was performed by an oral surgeon. Poor oral hygiene was evaluated based on the revised Tongue Coating Index (TCI)20, which involves visually inspecting the tongue coating. The tongue was divided into three regions (anterior, central, and posterior) for assessment and each section was evaluated using a 3-point scale, resulting in a total score of 9 points21.
Statistical analysis
Continuous variables were expressed as means ± standard deviation (SD), whereas categorical variables, including the proportion of participants receiving medication, were presented as numbers and percentages. Continuous and categorical variables were compared between the two groups using Student’s unpaired t-test and the chi-square test, respectively. The Wilcoxon rank-sum test was employed to compare the distribution of the number of teeth between the groups due to non-normal data distribution. Univariable logistic regression analysis was performed with hypertension as the dependent variable and timing and frequency of toothbrushing as independent variables. Multivariable logistic analyses were then adjusted for age and sex (Model 1) and further adjusted for age, sex, BMI, smoking history, and use of medications, years of education, and total energy intake per day, sugar and sodium intakes per 1000 kcal evaluated using BDHQ (Model 2). We carried out multivariable analyses with each toothbrushing timing or toothbrushing frequency ≥ 3 times per day and other factors as dependent variables for hypertension. Additionally, we also carried out multivariable analyses with all toothbrushing timings, toothbrushing frequency ≥ 3 per day, and other factors as dependent variables. Stratified analyses were conducted using separate multivariable logistic analysis models for older and non-older groups, with an age cut-off of 65 years. All statistical analyses were performed using the JMP Pro version 17 for Windows (SAS Institute Inc., Cary, NC, USA), with statistical significance set at P < 0.05.
Results
Participant characteristics
Table 1 summarizes the participant characteristics based on hypertension status. Among the 940 participants, 529 (56.3%) were in the hypertension group, while 411 (43.7%) were in the non-hypertension group. The overall mean BP was 132 ± 17/78 ± 11 mmHg, and the mean number of remaining teeth was 21.4 ± 7.8. The hypertension group was considerably older and comprised more men compared to the non-hypertension group. In addition, the hypertension group had a significantly higher BMI and fewer teeth (19.9 ± 8.2) than the non-hypertension group (23.2 ± 6.9).
Toothbrushing habits
Table 2 presents the toothbrushing habits of the participants. The overall toothbrushing rates were as follows: 33% upon waking, 8% before breakfast, 69% after breakfast, 48% after lunch, 4% before dinner, 42% after dinner, and 51% before sleeping. A total of 476 participants (51%) brushed their teeth three or more times. The hypertension group brushed less frequently after breakfast, after lunch, and before sleeping than the non-hypertension group. Similarly, the hypertension group had fewer participants who brushed their teeth frequently (≥ 3 times daily). Brushing duration was not significantly associated with hypertension. In addition, we performed a multivariable regression analysis adjusted for age and sex to assess the association between toothbrushing habits and oral environment. No significant associations were found between tongue coating scores and either toothbrushing timing or frequency of brushing (≥ 3 times per day).
Logistic analyses of hypertension
Univariable logistic regression analysis revealed that toothbrushing after breakfast (Odds ratio [OR] 0.577, 95% confidence interval [CI] 0.433–0.768, P < 0.001), after lunch (OR 0.571, 95% CI 0.441–0.741, P < 0.001), and before sleeping (OR 0.737, 95% CI 0.569–0.955, P = 0.021), as well as frequency of brushing ≥ 3 times per day (OR 0.554, 95% CI 0.427–0.719, P < 0.001) were all significantly associated with a lower risk of hypertension (Table 3). Multivariable logistic regression analyses are shown in Table 4. In Model 1 (adjusted for age and sex), toothbrushing after breakfast (OR 0.604, 95% CI 0.444–0.823, P = 0.001) and brushing ≥ 3 times per day (OR 0.735, 95% CI 0.554–0.973, P = 0.032) were significantly associated with a lower risk of hypertension (Table 5). After adjusting for age, sex, BMI, smoking history, and use of medications, years of education, and total energy intake per day, and sugar and sodium intakes per 1000 kcal as covariates (Model 2), only toothbrushing after breakfast was independently associated with reduced hypertension risk (OR 0.688, 95% CI 0.496–0.954, P = 0.025). Furthermore, in multivariable analyses using all toothbrushing timings, toothbrushing frequency, and other variables, toothbrushing after breakfast was independently associated with hypertension (Supplementary Table 1).
Stratified analyses divided by age
Stratified analysis was conducted by categorizing the participants by age with a cut-off of 65 years. Supplementary Table 2 shows the characteristics of study participants divided into older (age > 65 years) and non-older (age < 65 years) groups. The older group had a significantly higher rate of participants with hypertension than the non-older group (67% vs. 37%). Participants in the older group also had fewer remaining teeth. Additionally, the older group had fewer participants who brushed their teeth after lunch and before sleeping compared to non-older participants, but more participants who brushed their teeth after dinner (Supplementary Table 3). The number of participants who brushed their teeth ≥ 3 times per day in the non-older group was significantly higher than that in the older group. In older participants, multivariable analysis, adjusted for age and sex (Model 1), identified toothbrushing after breakfast and high toothbrushing frequency as independent factors associated with lower hypertension risk. Further adjustment for age, sex, BMI, smoking history, and the use of medications, years of education, and total energy intake per day, and sugar and sodium intakes per 1000 kcal (Model 2) revealed that only toothbrushing after breakfast was independently associated with a reduced risk of hypertension. In contrast, no specific variables or characteristics were associated with hypertension in non-older participants.
Discussion
This study investigated the association between toothbrushing habits and hypertension in the general population. Notably, only toothbrushing after breakfast was independently associated with lower hypertension risk. While brushing ≥ 3 times per day was initially associated with reduced hypertension after adjusting for age and sex, this association became non-significant after further adjusting for BMI, smoking, and use of antihypertensive, hypoglycemic, and lipid-lowering medications. This trend was also observed in those aged ≥ 65 years; however, no significant associations were identified in those aged < 65 years. While an association has been established between toothbrushing frequency and hypertension or cardiovascular diseases, the association between the timing of toothbrushing and hypertension has not yet been clarified. To our knowledge, this is the first study to demonstrate an association between toothbrushing after breakfast and hypertension.
Previous studies have linked inflammation to hypertension. Inflammatory biomarkers, such as C-reactive protein (CRP)22 and cytokines23, as well as white blood cell and platelet counts24, are often elevated in patients with hypertension. This established link strengthens the possibility of an association between oral inflammation and hypertension, as supported by several studies13,25,26. In a study involving Japanese university students, periodontal disease was reported to be significantly associated with hypertension27. Similarly, tooth loss, often associated with inadequate oral care, is linked with hypertension28,29,30,31,32. However, there is a lack of consensus on the specific number of missing teeth that defines an increased risk for hypertension. For example, a Korean study reported that tooth loss was strongly associated with hypertension, especially in women aged > 60 years28. In contrast, a French study identified poor masticatory function, poor oral hygiene, and oropharyngeal inflammation as risk factors for hypertension in participants aged < 65 years33. Regardless of age, these studies underscore the importance of maintaining a healthy oral environment and adopting appropriate toothbrushing habits.
Several reports have explored the association between toothbrushing habits and hypertension. A large Korean cohort study found that hypertension prevalence decreased with increasing toothbrushing frequency after adjusting for confounders, including periodontitis34. A previous meta-analysis also showed an association between toothbrushing frequency and hypertension35. In Kuwabara et al.’s large-scale epidemiological study on the association between toothbrushing and lifestyle-related diseases in the Japanese population36, less frequent toothbrushing was found to be associated with a higher hypertension prevalence. However, binary logistic regression analysis showed that toothbrushing frequency was independently associated with diabetes and dyslipidemia but not hypertension. In our study, the proportion of those brushing their teeth ≥ 3 times per day was significantly higher in the non-hypertension group than that in the hypertension group; however, this association became non-significant when other risk factors were added as additional covariates. The reason for the lack of association between toothbrushing frequency and hypertension in the multivariable analysis remains unclear, but there are several speculations. One possible explanation is that toothbrushing frequency is a general indicator of oral hygiene behavior but does not necessarily reflect the actual effect of plaque removal. Brushing technique including the use of interdental brushes, electric toothbrushes, water toothpaste, or other oral care items, and consistency are also important factors, and these were not captured in our study. Therefore, individuals who brush frequently may not necessarily achieve better oral hygiene or reduced inflammation. Another possibility is reverse causation. Participants who are more health-conscious or already diagnosed with hypertension may have adopted frequent toothbrushing as part of broader health behavior changes. Our detailed survey on toothbrushing frequency, which included the timing of toothbrushing, may have captured nuances that masked the association observed in other studies. Brushing the teeth at least thrice daily, especially after breakfast, may reduce the risk of developing hypertension.
This study identified toothbrushing after breakfast as an associated factor in lowering hypertension, which has not been identified in previous studies. Breakfast deposits food and drink in the oral cavity, which then affects the oral environment14. Therefore, not brushing after breakfast is likely to increase the risk of periodontal disease. The condition of the marginal tissue around the teeth has been shown to be associated with blood pressure37. Further, a significant correlation has been shown between high blood pressure and oral hygiene, while reducing plaque accumulation can prevent periodontal disease symptoms38,39. Plaque accumulation is significantly reduced among individuals who brush their teeth after breakfast40. It is believed that brushing teeth after breakfast to prevent plaque accumulation can help to maintain good oral hygiene, prevent periodontal disease, and even prevent hypertension. Furthermore, people who brush their teeth after breakfast may be more health conscious, and brushing their teeth after breakfast may be a contributing factor associated with hypertension. However, the specific association between toothbrushing, periodontitis prevention, and, ultimately, hypertension and CVDs remains unclear. Indeed, this study found that toothbrushing after breakfast was independently associated with hypertension, but oral hygiene status, as assessed by tongue coating score, was not associated with toothbrushing habits. While previous studies have demonstrated that tongue cleaning has an effect on tongue coating41, no reports were found regarding the influence of toothbrushing habits on tongue coating. It is possible that the results may have varied if a plaque score had been used to evaluate oral hygiene. The inclusion of detailed toothbrushing habits alongside comprehensive oral assessments for periodontal diseases in future large cohort studies could further clarify the association between toothbrushing timing and hypertension.
Despite the valuable insights shared in this study, it had some limitations. First, the cross-sectional design precludes establishing a causal relationship between toothbrushing habits and hypertension. Prospective longitudinal studies are needed to evaluate the effects of modifying toothbrushing habits on BP. Second, this study was conducted on health-examination participants; therefore, BP measurements were mostly taken once, which may not accurately reflect the true BP levels of the participants. Third, data on the use of interdental brushes, electric toothbrushes, water toothpaste, or other oral care items were not collected. Further research is necessary to clarify the relationships between these factors. Lastly, although the study targeted the general population of Tarumizu City, participation was voluntary, which may have introduced selection bias. Further studies, involving better recruitment processes, are warranted to validate our findings.
In conclusion, our study showed that toothbrushing after breakfast was independently associated with a lower risk of hypertension among individuals aged ≥ 65 years.
Data availability
Owing to privacy or ethical restrictions, the data are not publicly available. However, the datasets analyzed in this study will be made available by the corresponding author upon reasonable request, following ethical approval.
References
Ikeda, N. et al. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med. 9, e1001160 (2012).
Kawabata, T. et al. Insufficient blood pressure control is independently associated with increased arterial stiffness. Hypertens. Res. 45, 1861–1868 (2022).
Smolen, J. S., Aletaha, D. & McInnes, I. B. Rheumatoid arthritis. Lancet 388, 2023–2038 (2016).
Demmer, R. T., Jacobs, D. R. Jr. & Desvarieux, M. Periodontal disease and incident type 2 diabetes: results from the first national health and nutrition examination survey and its epidemiologic follow-up study. Diabetes Care 31, 1373–1379 (2008).
Kuroe, K. et al. Association between periodontitis and fibrotic progression of non-alcoholic fatty liver among Japanese adults. J. Clin. Periodontol. 48, 368–377 (2021).
Kim, J. Y. et al. Association between fatty liver index and periodontitis: the Korea national health and nutrition examination survey. Sci. Rep. 10, 3805 (2020).
Bahekar, A. A., Singh, S., Saha, S., Molnar, J. & Arora, R. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am. Heart J. 154, 830–837 (2007).
Tonetti, M. S. & Van Dyke, T. E. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J. Clin. Periodontol. Suppl 14, S24-29 (2013).
Kotronia, E. et al. Oral health and all-cause, cardiovascular disease, and respiratory mortality in older people in the UK and USA. Sci. Rep. 11, 16452 (2021).
Tonetti, M. S. et al. Treatment of periodontitis and endothelial function. N. Engl. J. Med. 356, 911–920 (2007).
Teeuw, W. J. et al. Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J. Clin. Periodontol. 41, 70–79 (2014).
de Oliveira, C., Watt, R. & Hamer, M. Toothbrushing, inflammation, and risk of cardiovascular disease: results from Scottish Health Survey. BMJ 340, c2451 (2010).
Matsui, S. et al. Poor toothbrushing behavior is associated with high risk of cardiovascular events: A prospective observational study. Int. J. Cardiol. 350, 111–117 (2022).
Isomura, E. T. et al. Not brushing teeth at night may increase the risk of cardiovascular disease. Sci. Rep. 13, 10467 (2023).
Muñoz Aguilera, E. et al. Periodontitis is associated with hypertension: a systematic review and meta-analysis. Cardiovasc. Res. 116, 28–39 (2020).
Czesnikiewicz-Guzik, M. et al. Causal association between periodontitis and hypertension: evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur. Heart J. 40, 3459–3470 (2019).
Makizako, H. et al. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr. Gerontol. Int. 19, 76–80 (2019).
Masumitsu, T. et al. Association of sleep duration and cardio-ankle vascular index in community-dwelling older adults. J. Atheroscler. Thromb. 29, 1864–1871 (2022).
Kobayashi, S. et al. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 14, 1200–1211 (2011).
Shimizu, T., Ueda, T. & Sakurai, K. New method for evaluation of tongue-coating status. J. Oral Rehabil. 34, 442–447 (2007).
Nakamura, M. et al. Association of oral hypofunction with frailty, sarcopenia, and mild cognitive impairment: A cross-sectional study of community-dwelling Japanese older adults. J. Clin. Med. 10, 1626 (2021).
King, D. E., Egan, B. M., Mainous, A. G. 3rd. & Geesey, M. E. Elevation of C-reactive protein in people with prehypertension. J. Clin. Hypertens. 6, 562–568 (2004).
Madhur, M. S. et al. Interleukin 17 promotes angiotensin II-induced hypertension and vascular dysfunction. Hypertension 55, 500–507 (2010).
Xu, J. P. et al. Systemic inflammation markers and the prevalence of hypertension: A NHANES cross-sectional study. Hypertens. Res. 46, 1009–1019 (2023).
Meng, R. et al. Effect of non-surgical periodontal therapy on risk markers of cardiovascular disease: a systematic review and meta-analysis. BMC Oral Health 24, 692 (2024).
Hanaoka, Y. et al. Level of serum antibody against a periodontal pathogen is associated with atherosclerosis and hypertension. Hypertens. Res. 36, 829–833 (2013).
Kawabata, Y. et al. Relationship between prehypertension/hypertension and periodontal disease: a prospective cohort study. Am. J. Hypertens. 29, 388–396 (2016).
Shin, H. S. Association between the number of teeth and hypertension in a study based on 13,561 participants. J. Periodontol. 89, 397–406 (2018).
Singh, A. et al. Association between tooth loss and hypertension among a primarily rural middle aged and older Indian adult population. J. Public Health Dent. 76, 198–205 (2016).
Da, D. et al. Association between tooth loss and hypertension among older Chinese adults: a community-based study. BMC Oral Health 19, 277 (2019).
Woo, H. G., Chang, Y., Lee, J. S. & Song, T. J. Tooth loss is associated with an increased risk of hypertension: A nationwide population-based cohort study. PLoS ONE 16, e0253257 (2021).
Abe, T. et al. Reduced masticatory performance and not using dentures are associated with hypertension in older adults with tooth loss: the Shimane CoHRE study. Hypertens. Res. 45, 1553–1562 (2022).
Darnaud, C., Thomas, F., Pannier, B., Danchin, N. & Bouchard, P. Oral health and blood pressure: the IPC cohort. Am. J. Hypertens. 28, 1257–1261 (2015).
Choi, H. M., Han, K., Park, Y. G. & Park, J. B. Associations among oral hygiene behavior and hypertension prevalence and control: the 2008 to 2010 Korea national health and nutrition examination survey. J. Periodontol. 86, 866–873 (2015).
Zou, L. et al. Meta-analysis on the association between the frequency of toothbrushing and hypertension risk. J. Clin. Hypertens. 24, 689–697 (2022).
Kuwabara, M. et al. Association between toothbrushing and risk factors for cardiovascular disease: a large-scale, cross-sectional Japanese study. BMJ Open 6, e009870 (2016).
Macedo Paizan, M. L. & Vilela-Martin, J. F. Is there an association between periodontitis and hypertension?. Curr. Cardiol. Rev. 10, 355–361 (2014).
Górska, R. et al. Correlation between the state of periodontal tissues and selected risk factors for periodontitis and myocardial infarction. Adv. Clin. Exp. Med. 26, 505–514 (2017).
Albardawel, L. H., Sultan, K., Hajeer, M. Y. & Maarouf, M. The effectiveness of probiotics on oral health during adult orthodontic treatment with fixed appliances. Cureus. 16, e73449 (2024).
Islam, Z. U., Shaikh, A. & Fida, M. Plaque index in multi-bracket fixed appliances. J. Coll. Physicians. Surg. Pak. 24, 791–795 (2014).
Choi, H. N., Cho, Y. S. & Koo, J. W. The effect of mechanical tongue cleaning on oral malodor and tongue coating. Int. J. Environ. Res. Public Health. 19, 108 (2021).
Acknowledgements
We appreciate the staff at the Tarumizu City Office and the members of the Tarumizu study contributing to this study. We would like to express our sincere gratitude to Professor Kanouchi, a registered dietitian and nutrition expert, for his valuable advice on interpreting the results of the BDHQ.
Author information
Authors and Affiliations
Contributions
Research idea and study design: A.T., T.K.; data acquisition: A.T., S.O., S.Y., Y.A., K.H., K.N, M.N., T.O.; data analysis/interpretation: A.T., T.K., S.K.; statistical analysis: A.T., S.K.; supervision or mentorship: S.K, T.T., M.O. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tezuka, A., Kubozono, T., Kawabata, T. et al. Association between toothbrushing habits and hypertension in the general population. Sci Rep 15, 35333 (2025). https://doi.org/10.1038/s41598-025-19217-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19217-x