Abstract
We previously demonstrated that the inability of primary endothelial cilia to sense fluid shear stress can lead to nitric oxide (NO) deficiency and cause hypertension (HTN). Decreased biosynthesis of NO contributes to cerebral amyloid angiopathy in Alzheimer’s disease (AD) patients through increased deposition of amyloid beta (Aβ). However, the molecular mechanisms underlying the pathogenesis of HTN and AD are incompletely understood. The objective of this study was to examine the pathophysiological roles of vascular primary cilia and muscarinic acetylcholine receptor 3 (CHRM3) in HTN and AD. We discovered, for the first time, that CHRM3 was localized to primary cilia of endothelial and cerebrovascular cells, and that CHRM3 expression was downregulated in cilialess cells. Moreover, CHRM3 activation enhanced cilia length and sensory function in terms of eNOS activation. To further examine the role of vascular CHRM3 in vivo, we showed that endothelial CHRM3 knockout was associated with increased BP and attenuated acetylcholine-mediated vascular relaxation. In addition, endothelial CHRM3 knockout resulted in altered fear behavior. This demonstrates the physiological significance of endothelial CHRM3 signaling and primary cilia-derived NO production as an important mechanism in the control of BP and cognition.
Similar content being viewed by others
Introduction
Primary cilia are solitary membrane-bound organelles emanating from the apical surface of most mammalian cells. They play pivotal roles in regulating various signaling pathways during embryonic development and adult homeostasis1. Ciliopathies, a group of genetic disorders characterized by disrupted cilia structure and/or function, present with a broad range of clinical symptoms, including HTN, developmental delays as well as cognitive and memory deficits, symptoms also observed in AD2,3,4. This suggests that cilia may regulate signaling cascades critical for vascular integrity and learning and memory5 and may also be important contributors to AD and HTN. Therefore, investigations of cilia function in the vascular system may reveal cilia-modulating mechanisms in neurodegenerative processes and suggest new treatments for HTN and AD.
AD, the fifth leading cause of death in the adult population, has a complex pathophysiological link with HTN6. HTN affects two-thirds of people aged > 60 years, and midlife HTN is the most decisive factor in all modifiable risk factors mediating AD development7. In fact, the structural and cellular injury and/or adaptations that occur in the neurovascular system in response to HTN have been shown to progressively disrupt the blood brain barrier (BBB) and exacerbate AD pathology8,9,10. A definite causative mechanism underlying the relationship between HTN and dementia, and particularly AD, has not yet been found. However, long-standing HTN, being closely related with endothelial dysfunction, arterial stiffness, and atherosclerosis, is linked with cerebral hypoperfusion11,12, leading in turn to the depletion of oxygen and nutrients in the brain parenchyma, oxidative stress on brain cells, increased permeability of the BBB, and impaired clearance of neurotoxic metabolites such as Aβ13.
We previously demonstrated that vascular endothelial primary cilia are fluid shear stress sensors14. In response to changes in blood flow/BP, they initiate the biosynthesis and release of NO15. We also demonstrated that cilia dysfunction is associated with diminished NO biosynthesis, decreased vascular reactivity, and increased BP15,16,17. It is well documented that diminished endothelial biosynthesis of NO and decreased vascular reactivity contribute to small cerebral artery constriction in AD patients through increased release and impaired clearance of Aβ, leading to the development of cerebral amyloid angiopathy (CAA)18. However, the possible mechanism by which loss of endothelial cilia function contributes to impaired vasoreactivity, increased BP, and cognitive impairment remains unexplored. Muscarinic acetylcholine receptors (CHRMs) comprise five subtypes, denoted as CHRM1-M519,20,21,22. The disruption of CHRM signaling contributes to several neurological disorders in the central nervous system (CNS) such as AD and schizophrenia23, and to cardiovascular diseases in the periphery such as HTN24 and heart failure25,26. ACh binding to CHRM3 triggers a signaling cascade that activates phospholipase Cβ leading to the mobilization of intracellular Ca+2 and eNOS activation27,28. CHRM3 is known as a regulator of the vascular system, consistent with its localization to the endothelial cell layer and vascular smooth muscle cells29. Interestingly, its distribution produces a response that is primarily endothelium dependent30,31.
Though both primary cilia and CHRM3 play important roles in NO biosynthesis, their relationship has never been explored, and cilium-associated CHRM3 functions have not been reported so far. Here, we utilized vascular and cerebrovascular endothelial cells to examine the localization and function of CHRM3 in the vascular system. We made the novel observation that CHRM3 and its downstream effector molecule phosphatidylinositol 4,5-bisphosphate (PIP2) are localized to primary cilia of vascular and cerebrovascular endothelial cells. We further demonstrated that the cholinergic system regulates cilia structure and sensory function in terms of NO release in part through CHRM3 activation. We also investigated a potential role for endothelial CHRM3 in BP and cognition. We found that the lack of CHRM3 in mouse vascular endothelia caused decreased vascular reactivity, increased BP, and impaired cognitive function. These findings reveal a critical involvement of primary cilia and CHRM3 in NO regulation and in cognitive impairment and vascular dysfunction.
Results
ACh regulates cilia length
Changes in cilia length can directly affect ciliary protein composition and consequently ciliary signaling output32. ACh treatment of endothelial cells derived from wildtype and Tg737Orpk/Orpk mice was associated with increased cilia length (Fig. S1a). Interestingly, cilia length was surprisingly restored in Tg737Orpk/Orpk cells (Fig. S1b).
CHRM3 localizes to primary cilia of mouse and human endothelial cells
Subcellular localization revealed that CHRM3 was predominantly localized to the ciliary axoneme in wildtype endothelial cells. CHRM3 ciliary localization in Tg737Orpk/Orpk endothelial cells could not be confirmed since these cells do not possess primary cilia (Fig. 1a,b). To further test if CHRM3 expression is dependent on normal primary cilia function or structure, CHRM3 expression was examined. Compared to wildtype cells, CHRM3 expression was significantly downregulated in Tg737Orpk/Orpk endothelial cells (Figs. 1c,S2). CHRM3 localization was also examined in human brain microvascular endothelial cells (HBECs) and was found to be abundantly expressed in primary cilia axoneme (Fig. 1d,f). PIP2, a major signaling molecule that is the target of CHRM3 activation, was colocalized with CHRM3 at the base of primary cilia (Fig. 1e,f). To confirm the localization CHRM3 to primary cilia, and to further validate our immunostaining data and our antibodies and to shed light on the physiological function of ciliary CHRM3 as well, HBEC cells were transfected with an expression vector containing Chrm3 gene fused to GFP (CHRM3-GFP). Immunostaining analysis with antibodies against acetylated α-tubulin confirmed CHRM3 ciliary localization (Fig. 1g). In addition, transfection of wildtype cells with CHRM3-GFP was associated with increased cilia length, but not ciliation frequency (Fig. 1h,i).
CHRM3 expression and localization to primary cilia. (a) Immunofluorescence staining with antibodies against acetylated α-tubulin and CHRM3 in wildtype and Tg737Orpk/Orpk endothelial cells. Images were captured at 60X magnification. (b) Ciliary localization of CHRM3 was confirmed by quantifying the number of ciliated cells in which CHRM3 is localized to primary cilia, to ciliary base, or to other cellular compartments (Other). CHRM3 localizations were examined from 3 preparations in each group, and at least 100–200 cilia were randomly selected in each preparation. (c) Western blot analysis to examine CHRM3 expression in wildtype and Tg737Orpk/Orpk endothelial cells. N = 6 cell preparations. Means are ± SEM. Unpaired two-tailed t-test, *P < 0.0296 denotes significant difference between CHRM3 expression in wildtype and Tg737Orpk/Orpk endothelial cells. t = 2.536, df = 10. Confocal immunofluorescence analysis of CHRM3 localization in HBEC cells stained with antibodies against (d) CHRM3 (green) and acetylated α-tubulin (red), e. Arl13b (green) and PIP2 (red), and f. CHRM3 (green) and PIP2 (red). g. Confocal immunofluorescence analysis of CHRM3 localization in HBEC cells transfected with expression vector containing Chrm3 gene fused to GFP (CHRM3-GFP) and stained with antibodies against acetylated α-tubulin (red) and GFP was imaged in green. (h) Cilia length and (i) ciliation frequency were quantified in wildtype cells transfected with CHRM3-GFP. N = 3 cell preparations with at least 50–100 cilia/preparation. Means are ± SEM. Unpaired two-tailed t-test, *P < 0.0028 denotes significant difference between cilia length in wildtype-CHRM3 and corresponding values in wildtype non-transfected cells. t = 3.009, df = 322. Images were captured at 60X and 40X magnifications. Scale bar, 5 μm.
CHRM modulation alters cilia length and sensory function
To investigate how a peripherally acting non-selective muscarinic agonist and antagonist would alter cilia structure and function, the stable CHRM agonist carbachol (CCh) and the antagonist hyoscyamine (Hyo) were used. Immunofluorescence staining indicated that CCh and surprisingly, Hyo treatments were both associated with a significant increase in cilia length in wildtype cells. (Fig. S3a,b). Since activation of CHRMs increased cilia length, we wanted to test whether CHRMs’ activity could bypass the dysfunctional mechano-ciliary complex through a mechanism that increases cilia length and cilia mechanosensory function. eNOS, the enzyme responsible for NO production, is acutely activated by various GPCRs and by physical stimuli such as hemodynamic shear-stress33. We subjected our cell lines to fluid-shear stress in the presence or absence of muscarinic agents. To assay for cilia function, we measured eNOS protein levels and eNOS enzymatic activity, which is regulated by phosphorylation at Ser1179 (p-eNOS). In both cell lines, total eNOS expression was relatively unaltered. In wildtype cells, CCh treatment was associated with a significant increase in p-eNOS expression under fluid flow compared to the vehicle-treated static group. Interestingly, p-eNOS expression was also significantly increased in the Hyo group under static conditions and in the co-treatment group (Hyo/CCh) under flow conditions (Fig. S3c). In Tg737Orpk/Orpk cells, CCh treatment was also associated with a significant increase in p-eNOS expression in the presence of fluid shear stress compared to vehicle-treated group (Fig. S3d).
CHRM3 modulation alters cilia length and sensory function
To examine the specific contribution of CHRM3 to cilia structure maintenance and function, the above experiments were repeated using cevimeline (CHRM3 agonist) and p-F-hexahydro-sila-difenidol (HHSiD; CHRM3 antagonist). In wildtype cells, cevimeline treatment was associated with a significant increase in cilia length and ciliation frequency in groups treated with 100–500 μM cevimeline compared to vehicle-treated group (Fig. 2a i–iii). In Tg737Orpk/Orpk cells, about 20% of the cells have stubby cilia; after treatment with cevimeline, cilia length and percent ciliation significantly increased in all treatment groups (Fig. 2b i–iii). Treatment of wildtype cells with 1–10 μM HHSiD was associated with a significant decrease in cilia length and ciliation frequency as compared to vehicle-treated cells (Fig. 2c i–iii). Tg737Orpk/Orpk cells were not tested due to the inability to measure cilia length decrease with high accuracy. To test whether the increase in primary cilia length associated with CHRM3 activation could enhance their sensory function; wildtype and Tg737Orpk/Orpk cells were treated with 500 μM cevimeline under static or fluid-shear stress conditions as described above and were assayed for eNOS and p-eNOS protein expression. In wildtype cells, cevimeline treatment further enhanced fluid shear stress-induced increase in p-eNOS expression. In Tg737Orpk/Orpk cells, p-eNOS expression was only increased under fluid shear stress and cevimeline treatment conditions (Figs. 3a,b, S4). In both cell lines, total eNOS expression was relatively unaltered (Figs. 3c,S4).
Selective CHRM3 modulation alters cilia length and ciliation frequency. Immunofluorescence using antibodies against acetylated α-tubulin (green) and pericentrin (red) was used to examine cilia length and ciliation frequency in response to 50–500 μM cevimeline treatment in (a i–iii) Wildtype (N = 1795, F(4,1791) = 140.7, P < 0.001), and (b i–iii) Tg737Orpk/Orpk (N = 1385, F(4,1381) = 74.21, P < 0.001) endothelial cells, or in response to 0.5–10 μM p-F–hexahydro-sila-difenidol, HHSiD treatment in (c i–iii) Wildtype (N = 1243, F(5,1238) = 14.95, P < 0.001) endothelial cells. 1-Way ANOVA with Tukey’s posthoc test, comparisons were made to control vehicle-treated cells. *P < 0.05, **P < 0.01, and ***P < 0.001. Individual data points represent cilia length measurements made from 4 preparations in each group, and cilia were randomly selected in each preparation. N represents number of cilia measured in each group. Images were captured at 60X magnification. Scale bar represents 5 μm. Means are ± SEM. Ciliation frequency is presented as whisker box with average value in the middle and minimum and maximum values as error bars.
Selective CHRM3 modulation enhanced cilia sensory function. (a–c) Western blot analysis was employed to assay total protein lysates from Wildtype and Tg737Orpk/Orpk endothelial cells for p-eNOS (N = 5–7, F(7,40) = 4.539, P < 0.0008) and eNOS (N = 3, F(7,16) = 0.1802, P < 0.9857) expression following treatment with cevimeline (Cev. 500 µM) under static or fluid shear stress conditions. GAPDH was used as a loading control. Bar graph represents averaged fold change in protein expression relative to wildtype control vehicle-treated cells. Means are ± SEM. N represents cell preparations. 1-Way ANOVA with Dunnett’s posthoc test. *P < 0.05, **P < 0.01, and ***P < 0.001.
CHRM3 ciliary localization is associated with cilia length
Since cilia length was altered after treatment with muscarinic drugs and since CHRM3 was localized to the primary cilia in endothelial cell lines, the possible link between CHRM3 ciliary localization and cilia length was further examined by quantifying cilia length and CHRM3 localization (ciliary base, ciliary axoneme, or “other” subcellular regions) in wildtype cells following treatment with cevimeline. Comparisons were made to vehicle-treated (control) cells in which CHRM3 is located to the ciliary base, followed by comparison between all groups. In wildtype cells, cevimeline treatment was associated with an increased cilia length in cells in which CHRM3 is localized to the ciliary base or to the axoneme, and a decreased cilia length in cells in which CHRM3 is localized to other subcellular regions. In addition, in cevimeline-treated cells in which CHRM3 is localized to the ciliary base or to the axoneme, primary cilia were always longer than their corresponding primary cilia in vehicle-treated groups (controls) and in “Other” cellular compartments groups (Fig. 4a i). Cevimeline treatment was also associated with a decreased CHRM3 localization to the ciliary base and no change in CHRM3 localization to axoneme or “Other” cellular compartments (Fig. 4a ii,iii). This result further confirms that CHRM3 activation and its ciliary localization are associated with cilia length. In HBEC cells, cevimeline treatment did not have any effect on CHRM3 ciliary axoneme or PIP2 ciliary base localization (Fig. 4b i,ii).
CHRM3 ciliary localization is associated with cilia length. (a) In wildtype cells, immunostaining using antibodies against acetylated α-tubulin and CHRM3 was used to examine (i.) cilia length in response to treatment with cevimeline (500 μM) in cells where CHRM3 was localized to the ciliary base, ciliary axoneme, or to “Other” non-ciliary compartments. N = 651 cells, 1-Way ANOVA with Bonferroni’s posthoc test, F(5,646) = 10.75, P < 0.0001 denotes significant difference in cilia length in all groups compared to cilia length where CHRM3 was localized to the ciliary base in vehicle-treated cells; #P < 0.05, ##P < 0.01, and ###P < 0.001denotes significant difference between cilia length in cevimeline-treated compared to all other groups. Individual data points represent cilia length measurements. Means are ± SEM, (ii.) CHRM3 localization frequency (%) to ciliary base, ciliary axoneme, or to “Other” non-ciliary compartments was quantified in response to cevimeline treatment (500 μM). N = 986 cells, unpaired two-tailed t-test, **P < 0.0081, t = 4.890, df = 4 significant difference in CHRM3 localization between cevimeline- and vehicle-treated cells, and (iii.) Immunostaining using antibodies against acetylated α-tubulin (red) and CHRM3 (green) was used to show representative images of CHRM3 localization to the ciliary base and axoneme. (b) In HBEC cells, immunostaining using antibodies against (i.) acetylated α-tubulin and CHRM3, and (ii.) PIP2 and CHRM3 was used to examine CHRM3 and PIP2 localization frequency (%) to ciliary base, axoneme, or to “Other” non-ciliary compartments in response to cevimeline treatment (500 μM). N = 658 cells, unpaired two-tailed t-test, NS non-significant difference in CHRM3 and PIP2 localization between cevimeline- and vehicle-treated (control) cells. None denotes no CHRM3 localization was found. Means are ± SEM.
Aβ treatment alters primary cilia structure and frequency
To determine whether elevated levels of Aβ affect cerebrovascular primary cilia structure, cilia length and ciliation frequency were examined in HBECs exposed to increasing concentrations of Aβ 1–42 (0.5–2.5 µM) and control Aβ 42–1 (2.5 µM) peptides. Exposure to 2.5 μM Aβ 1–42 was associated with a significant decrease in primary cilia length (Fig. S5a i–iii). Aβ causes increased levels of H2O2 and lipid peroxides to accumulate in cells34. To determine whether Aβ treatment altered cilia length through H2O2, HBECs were treated with H2O2 (100 µM) in the presence or absence of the γ-secretase inhibitor L-685,458 (2 µM), which inhibits Aβ generation35. As expected, H2O2 treatment was associated with significant decrease in cilia length and ciliation frequency, an effect that was abolished by L-685,458 (Fig. S5b i–iii). To test if Aβ deleterious effects on primary cilia length and ciliation frequency can be ameliorated by CHRM3 activation, HBECs were pre-treated with 2.5 μM Aβ 1–42 for 24 h followed by treatment with ACh (20 μM) or cevimeline (500 μM). Both, ACh and cevimeline treatments were associated with a significant increase in cilia length compared to Aβ 1–42 treatment, while only cevimeline treatment caused a significant increase in ciliation frequency (Fig. S5c i–iii).
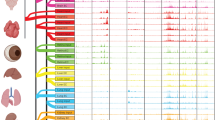
Vascular endothelial-specific CHRM3 knockout mice
Endothelial-specific recombination of the Chrm3 gene was confirmed by PCR (Fig. S6a i,ii). En-face immunofluorescence staining of artery sections revealed that CHRM3 is localized to primary endothelial cilia in Chrm3flox/flox, but not VECre:Chrm3flox/flox mice (Fig. S6bi,ii). Our immunofluorecscence staining data does not rule our CHRM3 localization to other cellular compartments. Furthermore, total proteins isolated from aorta, heart, brain, and liver confirmed diminished CHRM3 expression in aortas, but not in hearts, brains, and livers of VECre:Chrm3flox/flox compared to Chrm3flox/flox mice (Fig. S6c). This data further confirms CHRM3 ciliary localization and the endothelial selectivity of Chrm3 gene deletion. The mice were born in Mendelian frequencies with no gross developmental differences and no differences in organ weights.
Endothelial-CHRM3 knockout is associated with increased BP and attenuated ACh-mediated vasodilation
CHRM3 is expressed in the endothelial cell layer of the vascular system where it mediates vasodilation36. The role of endothelial CHRM3 in BP was examined in VECre:Chrm3flox/flox and Chrm3flox/flox mice over three days. Systolic BP was significantly higher in VECre:Chrm3flox/flox males on Days 1 and 3, and in VECre:Chrm3flox/flox females on Day 1 compared to respective Chrm3flox/flox controls. Average systolic BP was significantly higher in VECre:Chrm3flox/flox males and females than their respective Chrm3flox/flox controls (Fig. 5a,d). Diastolic BP was significantly higher in VECre:Chrm3flox/flox males on Day 3, and in VECre:Chrm3flox/flox females on Day 1 compared to respective Chrm3flox/flox controls. Average diastolic BP was not different between VECre:Chrm3flox/flox males and females and their respective Chrm3flox/flox controls (Fig. 5b,d). Mean arterial blood pressure (MAP) was significantly higher in VECre:Chrm3flox/flox males on Day 3, and in VECre:Chrm3flox/flox females on Day 1 compared to their respective Chrm3flox/flox controls. Average MAP was significantly higher in VECre:Chrm3flox/flox males compared to their Chrm3flox/flox controls (Fig. 5c,d). Heart rate was not different between VECre:Chrm3flox/flox and Chrm3flox/flox mice (data not shown). To examine whether the increased BP in VECre:Chrm3flox/flox is associated with the vasodilatory function of endothelial CHRM3, we examined endothelium-dependent vasodilation in response to ACh and endothelium-independent vasodilation in response to SNP in aortic segments. Wire myography revealed that endothelium-dependent vasodilation to ACh was markedly attenuated in VECre:Chrm3flox/flox compared to Chrm3flox/flox mice (Fig. 6a). Conversely, VECre:Chrm3flox/flox mice exhibited an increase in endothelium-independent vasodilation to SNP (at 10 nM), suggesting possible compensatory mechanism (Fig. 6b). SKA-31, a selective activator of Ca+2-activated K+ channels that mediate endothelium-dependent hyperpolarization, induced concentration-dependent dilations that were not significantly altered in VECre:Chrm3flox/flox mice (Fig. 6c). Together, these observations, support a key role for CHRM3s in ACh-mediated endothelial-dependent vasodilation.
Endothelial-CHRM3 contribute to high blood pressure. (a) Systolic, (b) Diastolic, and (c) MAP were monitored for three days in Chrm3f/f and VECre:Chrm3f/f male and female mice. (d) Averaged systolic, diastolic, and MAP were analyzed among Chrm3f/f and VECre:Chrm3f/f male and female mice. N = 16 male and female mice per genotype, a-c. repeated measures ANOVA with Bonferroni’s post hoc test, F(1,26) = 16.975, P < 0.001 (Systolic), F(1,26) = 8.774, P < 0.006 (Diastolic), and F(1,26) = 12.941, P < 0.001 (MAP) significantly different from corresponding values in Chrm3f/f mice. Individual data points (a-c) represent average BP measurements per 8 mice per day. Means are ± SEM. d. Unpaired two-tailed t-test, *P < 0.05 denotes significant difference between VECre:Chrm3f/f males and corresponding values in Chrm3f/f males, and *P < 0.05 denotes significant difference between VECre:Chrm3f/f females and corresponding values in Chrm3f/f females. Tail-cuff data points represent the average of approximately 15 BP measurements twice per day for three days per mouse. In a-d, red lines and bars represent females, and blue lines and bars represent males. Triangle signs and dotted bars represent knockout (VECre:Chrm3f/f) mice, and circle signs and clear bars represent control (Chrm3f/f) mice. Individual data points (d) represent average BP measurements per mouse.
Endothelial-CHRM3 contribute to ACh-mediated vasodilation. (a) Acetylcholine (ACh), (b) SNP, and (c) SKA-31 dose–response curves were assessed by wire myography in aortic segments preconstricted with phenylephrine (PE, 100 nmol/L) from Chrm3f/f and VECre:Chrm3f/f mice. N = 7–8 male and female mice per genotype, repeated measures ANOVA with Fisher’s LSD post hoc test, *P < 0.05 significantly different from corresponding values in Chrm3f/f mice. Red lines and squares represent knockout and black lines and circles represent control mice. Individual data points represent average aortic relaxation (as % of initial preconstriction) of 7–8 mice. Means are ± SEM.
Endothelial-CHRM3 knockout mice display altered fear behavior
The cued fear conditioning test was used to detect fear memory in Chrm3flox/flox, VECre:Chrm3flox/flox, and 3xTgAD mice subjected to three days of fear conditioning experiments, in which they associate an acoustic signal (tone) with a foot shock on Day 1, then on Days 2 and 3 were only given the tone with no shock for multiple trials (Fig. 7a). 3xTgAD mice were used as an AD model known to develop cognitive deficits over time and in which Aβ deposits appear by 6 months in the frontal cortex and become more extensive by 12 months37. For the 3–6- and 9–12-month-old age groups, there was a significant effect of genotype in the average freezing time during the habituation period (first 300 s of Day 1) with significantly higher habitual freezing for 3xTgAD than VECre:Chrm3flox/flox and Chrm3flox/flox mice (Fig. 7b i,ii). This habitual freezing measure is used as a movement control and suggests that 3xTgAD mice have a lower baseline level of movement compared to VECre:Chrm3flox/flox and Chrm3flox/flox mice.
Fear behavior in endothelial-CHRM3 knockout and 3xTgAD mice. (a) Schematic diagram of fear conditioning test. Freezing response in the 3–6- and 9–12-month-old Chrm3f/f, VECre:Chrm3f/f, and 3xTgAD mice measured as percent time spent freezing during (b i–ii) Habituation period (average of first 300 s) of Day 1. 1-Way ANOVA with Bonferroni’s post hoc test, F(2,29) = 15.19, P < 0.0001 for 3–6-month-old group, and F(2,20) = 7.259, P = 0.0043 for 9–12-month-old group, (c i–iv) Fear acquisition during the first 5 time points of Day 1 and average fear acquisition used as a proxy for learning memory rates between mouse genotypes. Repeated measures ANOVA with Bonferroni’s post hoc test, F(2,29) = 0.8840, P = 0.4240 for 3–6-month-old group, and F(2,19) = 20.75, P < 0.0001 for 9–12-month-old group, (d i,ii) Average fear recall/memory of the first 5 timepoints from Day 2 used as a proxy for fear memory. 1-Way ANOVA with Bonferroni’s post hoc test, F(2,29) = 1.067, P = 0.3573 for 3–6-month-old group, and F(2,20) = 0.8737, P = 0.4328 for 9–12-month-old group, (e i,ii) Fear extinction in response to all 30 tones of Days 2 and 3 used as a proxy for extinction learning. Repeated measures ANOVA with Bonferroni’s post hoc test, F(2,26) = 4.017, P = 0.030 for 3–6-month-old group, and F(2,17) = 3.209, P = 0.066 for 9–12-month-old group. #P < 0.022 significantly different from corresponding values in VECre:Chrm3f/f mice, (f i,ii) Fear extinction post hoc analysis representing the average of the last 5 timepoints of Day 3. 1-Way ANOVA with Bonferroni’s post hoc test, F(2,29) = 5.501, P = 0.0094 for 3–6-month-old group, and F(2,20) = 3.932, P = 0.0363 for 9–12-month-old group, and (g i,ii) Average fear extinction retention assessed by comparing freezing during the first 5 tones of Day 3 to freezing during the last 5 tones of Day 2. 1-Way ANOVA with Bonferroni’s post hoc test, F(2,29) = 0.8604, P = 0.4335 for 3–6-month-old group, and F(2,20) = 0.03907, P = 0.9618 for 9–12-month-old group. N = 8 for VECre:Chrm3f/f and 3xTgAD, and N = 16 for Chrm3f/f male and female mice. Means are ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 significantly different from corresponding values in Chrm3f/f mice and #P < 0.05, ##P < 0.01, and ###P < 0.001 significantly different from corresponding values in VECre:Chrm3f/f mice.
Fear acquisition is a measure of within-session learning, where mice acquire the fear response and associate the tone with the shock. In the 3–6-month-old group, the freezing time of the VECre:Chrm3flox/flox mice during the fear acquisition period (freezing during 5 tones of Day 1) was significantly lower than that of 3xTgAD mice during the first and second timepoints only, but not different from the Chrm3flox/flox mice; however, the average freezing time during the fear acquisition period was not different between Chrm3f/f, VECre:Chrm3f/f, or 3xTgAD mice (Fig. 7c i,ii). This suggests that there is no difference in the learning rates between the three genotypes in this age group. In the 9–12-month-old group, there was a significant effect of time, genotype, and a significant interaction between time and genotype. The freezing time of the VECre:Chrm3f/f mice during the fear acquisition period was significantly lower than that of 3xTgAD mice during the first four timepoints, but not different from the Chrm3f/f mice except during the third timepoint; however, the average freezing time during the fear acquisition period was significantly lower in the VECre:Chrm3f/f compared to Chrm3f/f and 3xTgAD mice (Fig. 7c iii,iv). This indicates that the VECre:Chrm3f/f mice learned at a different rate than the 3xTgAD and Chrm3f/f mice. Fear recall was analyzed as the freezing time during the first 5 tones of Day 2, a day after the acquisition training period, and was used as a proxy for consolidated fear memory. The average freezing time during the fear recall/memory period was not different between Chrm3f/f, VECre:Chrm3f/f, or 3xTgAD mice for both age groups (Fig. 7d i,ii).
Fear extinction assesses new learning that a conditioned stimulus no longer predicts an unconditioned stimulus following repeated exposures38. Extinction learning was analyzed by comparing freezing time during all 30 tones of Days 2 and 3. Surprisingly, in the 3–6-month-old group, the freezing time during fear extinction was higher for the VECre:Chrm3f/f at most timepoints compared to the Chrm3f/f mice (Fig. 7e i). More precisely, the 3xTgAD mice displayed plainly the worst fear extinction, with a nearly flat learning curve and a higher average freezing at the end of extinction. However, the VECre:Chrm3f/f mice have a different learning curve, with higher freezing (i.e. poor learning) at earlier time points, although they were not different from the Chrm3f/f mice at the end of 30 tones. This indicates that there was a significant effect of genotype and that the VECre:Chrm3f/f and 3xTgAD mice learned the extinction at different rates than the Chrm3f/f mice. For the 9–12-month-old group, the freezing time during fear extinction period was significantly higher for the 3xTgAD mice than the VECre:Chrm3f/f mice, but not different from the Chrm3f/f mice (Fig. 7e ii). In this age group, although there was no significant effect of genotype, pairwise comparisons indicated a significantly higher freezing percentage among 3xTgAD mice compared to VECre:Chrm3f/f mice. Average fear extinction post hoc analysis, examining the average of the last 5 time points of extinction, indicated that in the 3–6-month-old group, the freezing time during the fear extinction period was significantly higher for 3xTgAD than Chrm3f/f mice but not different from VECre:Chrm3f/f mice (Fig. 7f i). In the 9–12-month-old group, the freezing time during the fear extinction period was significantly higher for 3xTgAD compared to VECre:Chrm3f/f mice but not different from Chrm3f/f mice (Fig. 7f ii). This suggests that the VECre:Chrm3f/f mice were learning the extinction at a faster rate than the 3xTgAD mice. Extinction retention was then analyzed by comparing the freezing time during the first 5 tones of Day 3 to the freezing during the last 5 tones of Day 2 and was used as a proxy for extinction memory. A smaller difference between days indicates greater retention of extinction learning from the previous day. The average freezing time during the fear extinction retention period was not different between the genotypes in both age groups (Fig. 7 g I,ii).
Endothelial-CHRM3 knockout mice and spatial learning
Hippocampus-dependent spatial learning and memory were further evaluated using Barnes maze assay (Fig. 8a). For both age groups, the measures were the average latency to reach the escape hole on each training day, the primary latency on the probe day, and the percent of time in the correct quadrant of the maze on the probe day. For the 3–6-month-old mice, there was no significant difference in the average latency on all three training days between the genotypes (Fig. 8b i). However, the 9–12-month-old mice displayed a significant effect of time and genotype, with the 3xTgAD mice having a significantly higher training latency on each training day compared to the VECre:Chrm3f/f and Chrm3f/f mice (Fig. 8b ii). For primary latency, there was a significant effect of genotype in both age groups, specifically with 3xTgAD mice exhibiting a significantly higher latency than the Chrm3f/f mice (Fig. 8c i,ii). Lastly, the percentage of time the mice stayed in the quadrant that held the escape cage in the trail days was measured on the probe day. For both age groups, there was no significant difference between the genotypes (Fig. 8d i,ii).
Spatial learning in endothelial-CHRM3 knockout and 3xTgAD mice. (a) Schematic diagram of Barnes maze test in 3–6 and 9–12-month-old Chrm3f/f, VECre:Chrm3f/f and 3xTgAD mice to assess (b i,ii) Average latency per day across the three training days. Repeated measures ANOVA with Bonferroni’s post hoc test, F(2,24) = 1.675, P < 0.208 for 3–6-month-old group, and F(2,17) = 7.563, P < 0.004 for 9–12-month-old group, (c i,ii) Primary latency to enter the escape hole on the fourth day. 1-Way ANOVA with Bonferroni’s post hoc test, F(2,27) = 2.666, P = 0.0546 for the 3–6-month-old group, and F(2,17) = 2.666, P = 0.0797 for 9–12-month-old group, and (d i,ii) Time in each quadrant on the fourth day (as a measure of search strategy). 1-Way ANOVA with Bonferroni’s post hoc test, F(2,27) = 0.1269, P = 0.8814 for the 3–6-month-old group, and F(2,20) = 0.1950, P = 0.8244 for 9–12-month-old group. N = 8 for VECre:Chrm3f/f and 3xTgAD, and N = 16 for Chrm3f/f male and female mice. Means are ± SEM. *P < 0.05, and **P < 0.01 significantly different from corresponding values in Chrm3f/f mice and #P < 0.05, and ##P < 0.01 significantly different from corresponding values in VECre:Chrm3f/f mice.
Discussion
The regulation of cilia length is an important topic for the treatment of cilia-related diseases as many homeostatic mechanisms are dependent upon ciliary detection and translation of extracellular mechanical and chemical stimuli39. Often in disease states, ciliary length becomes dysregulated causing an overly elongated or shortened cilium40. However, in some diseases, the pathogenesis is attributed to excessively long cilia suggesting that cilia have a tissue specific “sweet spot” for optimum functioning and thus is tightly regulated and a required factor in maintaining homeostasis40. Here, we presented findings suggesting cholinergic involvement in primary cilia maintenance, BP, and AD.
The cholinergic system plays a central role in cognition, memory, and BBB permeability, whereas, peripherally, ACh regulates cardiac function and vascular contraction. Indeed, it has been reported that the vasodilator effects of muscarinic agonists are markedly reduced in CHRM3 knockout mice28. Thus, it is proposed that the vascular cholinergic system plays an important role in BP regulation through CHRM3. Primary cilia disruption in different tissues has been shown to induce changes in vascular function, BP41,42,43, and brain-related disorders44. Thus, despite the knowledge that primary cilia and proteins of the cholinergic system may play critical roles in BP41,45 and AD46, their relationship has never been explored. We provided strong evidence supporting the roles of CHRMs in altering the sensitivity and chemosensory function of primary endothelial cilia. This is supported by CHRM3 localization to primary cilia of wildtype endothelial cells. The downregulated expression of CHRM3 in Tg737Orpk/Orpk cilialess endothelial cells further suggested that normal cilia structure is an important determinant for CHRM3 expression. Our hypothesis about the important role of ciliary CHRM3 signaling in vascular and cognitive function was further supported by the strong and consistent localization of CHRM3 and its downstream signaling component PIP2 to primary cilia of HBECs. This finding demonstrated for the first time the importance of primary cerebrovascular cilia as discrete cellular domains for CHRM3 signaling. Signaling through GPCRs can be optimized by enriching receptors and downstream effectors in discrete cellular domains. The cilium is especially suited to propagate signaling cascades because of its small volume relative to the cell body and because signaling molecules, including GPCRs, localize dynamically to the cilium. This dynamic localization is critical as it enables rapid signaling alterations that tune pathway output47. Both, dynamic GPCR cilia localization and cilia length and shape changes have been implicated as key for signaling. It has been shown that cilia with specific GPCRs appear to dynamically alter their length, receptor occupancy, and ciliation frequency under different physiologic conditions and in different cell types. This suggests that dynamic cilia localization of GPCRs depends on properties of individual GPCRs and cells where they are expressed48. Our data suggests that CHRM3, like other ciliary GPCRs, is possibly delivered at the ciliary base where it docks at the transition fibers before being imported into the cilium49. Thus, ciliary localization enables a substantially higher local concentration of ciliary receptors to facilitate efficient signal detection and transduction, enabling the recognition of primary cilia as specialized signaling hubs or sensory antenna50. We propose that the CHRM3-mediated changes in primary cilia length in endothelial cells may alter the concentration and composition of ciliary membrane proteins or receptors to affect the function of primary cilia at the level of an organelle, which, in turn, could affect cellular behavior, ultimately leading to behavioral and/or physiological changes at the level of the organism. Although the role of cilia and CHRM3 in regulating endothelial NO release and BP have been heavily investigated in both clinical and experimental settings, yet we are just beginning to understand the precise signaling pathways mediated by ciliary GPCRs and how they impact cellular function and mammalian physiology.
Our studies on CHRM3 localization and expression, led us to investigate the involvement and relationship CHRM3 had with cilia structure and function. Expression studies of functional endpoints such as p-eNOS showed that CCh caused a statistically significant increase in p-eNOS expression in Tg737Orpk/Orpk cells when challenged with fluid flow. This suggests that CCh treatment could be associated with a rescue of cilia function in cilialess cells. Hyo, the non-selective antagonist also produced an increase in cilia length in wildtype cells and increased p-eNOS levels in wildtype cells only. It has been shown that biased GPCR signaling can cause antagonists to activate receptors leading to unexpected or opposite results/downstream signaling cascades which also may provide an explanation for Hyo results51. Interestingly, despite lacking intraflagellar transport molecule 88 (IFT88), a protein necessary for cilia formation, Tg737Orpk/Orpk cells showed a statistically significant increase in “stubby” cilia and cilia length after treatment with cevimeline. Unlike Hyo, treatment with CHRM3 selective antagonist, HHSiD caused a significant reduction in cilia length and ciliation frequency in wildtype cells, suggesting that CHRM3 activity may play an important role in regulating cilia structural dynamics. Western blot data assessing whether CHRM3 mediated increase in cilia length correlates to enhanced function showed that an upregulation in p-eNOS in endothelial cells. This is consistent with our hypothesis that CHRM3 activation could rescue cilia sensory function by bypassing the impaired NO release mechanism and yielding an increase in NO in the absence of functional cilia (Tg737Orpk/Orpk). Genetically modified animals in which primary cilia function or structure are perturbed show alterations in critical signaling pathways that are required for cellular homeostasis52. Our results demonstrated that exposure to high levels of Aβ can cause cilia length shortening and decreased ciliation frequency, postulating that Aβ levels observed inside blood vessels of AD patients and animal models might have similar effects on cilia structure, signaling, and ciliogenesis.
The essential role of eNOS in muscarinic-induced vasodilation is consistent with the significant reduction in the relaxation response to ACh observed in blood vessels obtained from eNOS knockout mice53,54. Our data demonstrated that endothelial-specific Chrm3 knockout mice had elevated baseline systolic and MAP in the absence of any HTN inducing agents such as angiotensin II or salt diet, suggesting that the elevated BP phenotype in Chrm3 knockouts may be due to diminished ability of the vasculature to release NO that mediate vessel dilation. This was further demonstrated by the inability of aorta segment isolated from VECre:Chrm3f/f to display relaxation response after treatment with ACh. This highlights the importance of the ACh-induced NO-mediated vascular relaxation in BP.
BP data from VECre:Chrm3f/f mice are in agreement with previous findings from Chrm3-/- knockout mice characterized by pronounced impairments in carbachol-mediated contractions of different smooth muscle preparations in vitro55,56,57. Interestingly, a recent study identified a missense mutation in the last intracellular domain of the Chrm3 gene in the Dahl salt-sensitive rat model that was functionally correlated with a rise in BP, an increased CHRM3 signaling, and an adrenal epinephrogenesis. Moreover, gene targeting that abolished the CHRM3 function caused a decrease in BP, suggesting that the CHRM3-mediated signaling promotes HTN via a central nervous system/adrenal mechanism58. On the other hand, a study reported that CHRM3 elicits endothelium-dependent dilation in response to ACh in arterioles in vivo, even though endothelial-specific deletion of CHRM3 did not affect overall cardiovascular homeostasis and BP59. In the later study, endothelial CHRM3 was knocked out using an inducible Cre‐recombinase driven by the VE‐cadherin promoter60, followed by BP measurement in 14–16 week-old male mice. The difference in the BP outcomes between our studies could be due to several factors including but not limited to the incomplete knockdown of the CHRM3 in the inducible tamoxifen-treated Cre model and the presence of sufficient fraction of CHRM3 in endothelial cells to prevent an increase in BP through ACh-mediated vasodilation. Our findings are also supported by studies using pharmacological and global CHRM3 deletion approaches concluding that CHRM3 is the most important among other CHRMs subtypes in mediating dilation in large and small arteries27,28,61,62. It was demonstrated that endothelial deletion of NOSTRIN impaired CHRM3 localization and its signaling function and selectively blunted ACh-induced dilations in the aorta and resistance vessels. This defect in CHRM3 function was also associated with an elevated BP and a diastolic cardiac dysfunction in vivo. Although endothelial CHRM3 knockout was not directly examined, these findings support the concept that endothelial CHRM3 and NOSTRIN are crucial for cardiovascular homeostasis and suggest a physiologic function for ACh on the endothelium63. Furthermore, a recent study postulated that ACh could act on the gastrointestinal CHRM3 to increase afferent vagal nerve activity, which decreases sympathetic nervous activity by autonomic reflex, suppressing noradrenaline release and lowering BP64. Taken together, these findings led us to conclude that endothelial CHRM3 contributes to ACh-mediated vascular relaxation in large arteries in vivo and suggest that neuronal or non‐neuronal ACh contributes to arterial pressure homeostasis through activation of CHRM3. Despite significant blunt in ACh-mediated aorta dilation in the VECre:Chrm3f/f knockout, BP was only moderately increased, suggesting that other factors could be counteracting endothelial CHRM3’s role in lowering BP. Thus, CHRM3 could be involved in BP regulation through its role in vascular relaxation in large arteries in response to ACh local release; however, CHRM3’s other roles (mainly CNS roles) in salt sensitivity, BP progression, and development of HTN, in addition to CHRM3-independent pathways in the endothelium and other BP-controlling mechanisms such as improved renal and cardiac activities, could be compensating its role in ACh-mediated endothelium-dependent vascular relaxation.
Despite the lack of mechanistic insight, HTN has been recognized as an important treatable condition that could potentially prevent or delay the onset of dementia-related cognitive deficits65. We investigated the effects of endothelial CHRM3 knockout on brain cognitive function, a major target of end-organ damage. The possible role of cerebrovascular CHRM3 in the pathogenesis of AD is supported by data demonstrating altered fear memory and behavior, a cognitive deficit characteristic of neurodegenerative diseases and AD, in the VECre:Chrm3f/f mice. This cognitive deficit was demonstrated in the difference in the learning rate between the VECre:Chrm3f.f/f and the Chrm3f/f mice when compared to the 3xTgAD AD model. The 3–6-month-old VECre:Chrm3f/f mice clearly displayed a slower rate of fear extinction, suggesting a more subtle learning deficit, possibly related to reversal learning or re-learning. By 9–12 months of age, the VECre:Chrm3f/f mice displayed worse fear acquisition, suggesting potent deficits in working memory. However, they do appear better at fear extinction, but this is probably due to decreased acquisition of conditioned fear as they acquired less of a fear response. Finally, the expected deficits in our positive control, 3xTgAD mice, appear most strongly in extinction learning and in the more challenging Barnes maze assay. While previous studies clearly implicated cerebrovascular endothelial dysfunction in the contribution to AD pathologies, the exact underlying signaling mechanism that leads to cognitive dysfunction is unknown. Endothelial CHRM3 is implicated in NO production through activation of eNOS, thus contributing to localized arterial dilatation, increased CBF, and lowering of BP. It is also well documented that decreased biosynthesis or availability of NO contributes to AD pathogenesis through increased deposition of Aβ in small cerebral arteries66. In addition, supplementation of NO attenuates increased expression of APP in cerebral microvessels of eNOS-deficient mice67. This suggests that activating pathways , such as the CHRM3 pathway, leading to NO release in the cerebral vasculature could play an important role in modulating expression and processing of APP. We hypothesize that the decreased NO availability could, in turn, be due to impaired ciliary CHRM3 signaling. In addition, in AD, Aβ accumulation can potentially lead to cilia sensory dysfunction and impaired CHRM3 signaling. Since HTN and diminished NO exacerbate AD pathology and cognitive decline, we postulate that there is a vicious cycle of mutually reinforcing damage between ciliary signaling impairment (vascular dysfunction) and Aβ-mediated pathology. Breaking this cycle by enhancing NO bioavailability through CHRM3 activation could slow the development and/or progression of AD by enhancing vascular function and diminishing Aβ accumulation. The current studies highlight both, the importance of endothelial ciliary signaling in AD as well as some unanswered questions regarding vascular dysfunction in the context of neurodegenerative diseases. A deeper mechanistic understanding of the microvascular dysfunction could facilitate the development of innovative therapies for AD.
To our knowledge, this is the first report to demonstrate CHRM3 localization to the primary cilium and to suggest a novel putative function for CHRM3 and its role in ciliopathy-associated cognitive impairment. Despite these strengths, several limitations of the study should be acknowledged. First, the study examined cilialess endothelial cells, but possibly in the future could examine the role of ciliary CHRM3. This would shed light on the importance of ciliary localization of GPCRs in relation to their activity and downstream signaling. Second, to confirm the involvement of CHRM3 in BP regulation, validation studies using HTN inducing agents may be conducted using VECre:Chrm3f/f mice. Finally, vascular contractility studies could be performed on cerebral blood vessels to confirm loss of ACh-mediated vascular relaxation in the cerebral vasculature.
Methods
Cell culture
The murine wildtype and Tg737Orpk/Orpk endothelial cell lines were previously established from 15.5-day embryonic mouse aortas. The cilia mutant, Tg737Orpk/Orpk (cilialess) line, does not respond to fluid shear stress, a characteristic of endothelial cells with abnormal cilia structure17. Human brain microvascular endothelial cells (HBEC-5i; ATCC CRL-3245™), were derived from small fragments of human cerebral cortex68. Endothelial cell lines were grown in Dulbecco’s Modification of Eagle’s (DMEM; Corning), or DMEM F-12 Medium (ATCC 30–2006, containing 2.5 mM L-glutamine, 15 mM HEPES, 0.5 mM sodium pyruvate, and 1200 mg/L sodium bicarbonate), containing 10% of fetal bovine serum (FBS; Sigma-Aldrich) and 1% penicillin/streptomycin (ThermoFisher Scientific) and maintained at 37 °C with 5% CO2 in a cell culture incubator. Prior to all experiments, cells were serum starved for 48–72 h to accurately quantify cilia structure and function in response to various pharmacological treatments. In some cases, fluid shear stress was applied to the surface of fully differentiated cells at 7.2 dynes for 1 hour17. Wildtype and HBEC cells were used for expression of synthetic gene encoding for wildtype CHRM3 created and inserted into the pEGFP-N3 vector (Clontech) and fused to GFP.
Pharmacological agents
Various pharmacological agents were used: ACh (20 µM; CHRM3 non-selective agonist), carbachol (CCh) (50 µM; CHRM3 non-selective agonist), L-hyoscyamine (250 nM; CHRM3 non-selective antagonist), cevimeline hydrochloride (50–500 µM; CHRM3-selective agonist), p-hexahydro-sila-difenidol (HHSiD, 0.5–10 µM; CHRM3-selective antagonist), Aβ peptide (1–42; 0.5–2.5 µM), Aβ control peptide (42–1; 2.5 µM), γ-secretase inhibitor (L-685,458; 2 µM) and H2O2 (100 µM). All chemicals were purchased from Sigma Aldrich and ThermoFisher Scientific. Cevimeline has been clinically used and considered as a relatively selective agonist of CHRM3s when compared with other muscarinic agonists69. HHSiD, is also a muscarinic antagonist which shows some selectivity for CHRM3 over others70.
Immunofluorescence staining
For en-face arterial immunofluorescence, arteries were cut longitudinally. Briefly, cells and arteries were fixed with 4% paraformaldehyde in 2% sucrose solution for 10 min at room temperature. All primary and secondary antibodies were diluted in a 10% FBS solution where primary antibodies against acetylated α-tubulin (Sigma Aldrich), CHRM3 (Alomone Labs and Novus Biologicals), pericentrin (Proteintech), PIP2 (Echelon), , CDD144 (VE-CAD, ThermoFisher Scientific), and Arl13b (Proteintech), were used at dilutions of 1:1,000. The FITC,Texas Red, and Alexa 647 secondary antibodies (ThermoFisher Scientific) were used at a 1:500 dilutions. Cells were then washed twice with 1X-PBS and mounted with DAPI (Vector Labs). Images were captured with Nikon TE2000-U microscope and analyzed with Nikon Imaging Software (NIS Elements). Outcome measures such as cilia length and localization quantification were analyzed by unpaired two-tailed t-test for single comparison, or by 1-Way ANOVA with Tukey’s, Bonferroni’s, or Dunnet’s multiple comparison test as appropriate and as indicated in the figure legends.
Immunoblotting
To examine whether the pharmacological agents modulate cilia sensory function, cells were treated with the pharmacological agent/s under static or fluid shear stress conditions. Cultured cells and various organs were lysed with RIPA buffer (ThermoFisher Scientific) containing protease inhibitor cocktail (Roche), and intracellular contents were collected after centrifugation for 20 min at 10,000 × g. After determination of protein concentration (BCA assay kit, ThermoFisher Scientific), total cell lysates were analyzed with SDS-PAGE. Primary antibodies against CHRM3 (Alomone Labs and Novus Biologicals), total eNOS (BD Biosciences), and p-eNOS (BD Bioscience, pS1177) were used at dilutions of 1:500–1:1000 and were incubated with the membrane at 4 °C overnight. GAPDH (1:1000; Cell Signaling) was used as a loading control. Membranes were then washed three times for 10 min each in 1X-TBS/T (100 mL of 10X Tris buffered saline in 900 mL dH2O) and incubated in a secondary anti-mouse or anti-rabbit IgG antibody (1:10,000) for 2 h at room temperature. The blots were washed in 1X-TBS/T and then incubated in chemiluminescent substrate (West Pico) for 2–5 min. Finally, the blots were developed via an x-ray film or Syngene G:box western blot imager (Syngene). Blots are sometimes cut into 2 or more pieces before hybridization with antibodies for consistency of results. Outcome measures such as protein expression quantification were analyzed by unpaired two-tailed t-test for single comparison, or by 1-Way, 2-Way, or 3-Way ANOVA with between-subjects factors of fluid flow, treatment, and group with Tukey’s, Bonferroni’s, or Dunnet’s multiple comparison test as appropriate and as indicated in the figure legends.
Generation of animal models
All animal studies were approved by the University of Toledo Institutional Animal Care and Use Committee (IACUC) and performed in accordance with the National Institutes of Health (NIH) Guide for the Care and Use of Laboratory Animals. Endothelial-specific Chrm3 knockout mice were generated by crossing endothelium constitutive Cdh5 (VECre) promoter driven Cre-transgenic mice (the Jackson Laboratory; Stock No: 006137, USA) with homozygous floxed Chrm3flox/flox mice (NIDDK, Bethesda, USA) to obtain VECre:Chrm3flox/+ mice. Further intercrossing of these mice resulted in VECre:Chrm3flox/flox mice and control littermates that did not harbor the Cre transgene. The 3xTgAD AD mouse model was purchased from the Jackson Laboratory (Strain # 004807).
Animal model characterization
Genomic DNA was prepared from mouse ear punch for genotyping by PCR. The Chrm3 floxed and wildtype alleles were identified using primers yielding bands of 230 bp and 200 bp, respectively. The presence of the Cre gene in the VECre endothelium-specific knockout lines was determined using primers (Table 1) yielding a single band of 700 bp71; for Cre-negative mice, no band was observed. Moreover, to confirm gene knockout and endothelial selectivity, mice were sacrificed at either 3, 6, or 9 months of age, and their organs were analyzed by immunohistochemistry and protein expression studies. For Western blotting studies, protein lysates from aorta, heart, brain, and liver of Chrm3flox/flox and VECre:Chrm3flox/flox mice were examined using specific antibodies against CHRM3. To further confirm the endothelial selectivity of the Chrm3 knockout, immunofluorescence staining was performed on artery segments from Chrm3flox/flox and VECre:Chrm3flox/flox mice using antibodies against acetylated α-tubulin and CHRM3. Please note that the endothelial selectivity and specificity of VECre mice have been well characterized before72.
Tail cuff blood pressure
Systolic, diastolic, MAP, and heart rate were measured using the CODA high throughput noninvasive blood pressure system (Kent Scientific Corporation). Mice were placed in small-size holders and secured to minimize movement using a nose cone73. The holder was then placed onto the warming platform where the tail was inserted into the VPR cuff. The mice were given at least 5 min to acclimate to the holder and cuff placement. CODA software was used to record BP for 15 s with 5 s between measurements for a total of 25 cycles, including 10 acclimation cycles and 15 measurement cycles. Measurements were taken twice daily for three consecutive days. Outcome measures such as blood pressure quantification over three days were analyzed by repeated measures ANOVA with Bonferroni multiple comparison post hoc test. Averaged blood pressure measurements were analyzed by unpaired two-tailed t-test for single comparison as indicated in the figure legends.
Wire myography
Wire myography was performed as previously described, with minor changes74. Briefly, aortic tissue segments (1–2 mm) were excised from anesthetized Chrm3flox/flox and VECre:Chrm3flox/flox mice and cleaned from the surrounding periadventitial fat and connective tissues in ice-cold oxygenated Kreb’s buffer (130 mM NaCl, 4.7 mM KCl, 1.17 mM MgSO4, 1.18 mM KH2PO4, 1.6 mM CaCl2, 25 mM NaHCO3, and 5.5 mM glucose; pH 7.4). Afterwards, the artery segments were mounted on multi-chamber DMT wire myographs (DMT-620 MA) and bathed in 37 °C oxygenated Kreb’s buffer. After an initial incubation period, artery segments were stretched to a prefixed tension of 5 mN and incubated for 45 min with multiple wash steps with fresh Kreb’s buffer. Aortic segments were challenged with KCl (120 mM) to test for viability. Cumulative dose response curves to multiple agonists, ACh (0.1–10 µM), SNP (0.01–10 µM), and SKA-31 (0.01–10 µM) were generated after an initial preconstriction period using phenylephrine (PE; 100 nM). Data was analyzed using PowerLab software (AD Instruments). Outcome measures such as average aortic relaxation (% of initial preconstriction) were analyzed using repeated measures ANOVA with Fisher’s LSD post hoc test.
Fear conditioning
Cognitive function was examined in Chrm3flox/flox, VECre:Chrm3flox/flox, and 3xTgAD mice at 3–6 and 9–12 months of age. Mice were trained on classic Pavlovian fear conditioning and assessed for contextual fear, cued fear, fear extinction, and extinction retention. Adult mice were placed in a conditioning chamber located within a sound attenuating box (Harvard Apparatus) monitored by FreezeFrame software (Actimetrics) with secondary sound attenuation provided by a sound attenuating booth (ROOM). Two contexts were used: cinnamon scent (McCormick) and house lights (Context A), or peppermint scent (McCormick) and infrared lights (Context B). On the first day, mice experienced a 300-s habituation period followed by five separate presentations of a tone (6 kHz, 30 s) paired with a light foot shock (0.5 mA, 0.5 s) at 30-s inter-trial intervals, all in Context A. On the second day, the animals were re-introduced to the conditioning chamber in Context B and exposed to 15 tones (6 kHz, 30 s) with 30-s inter-trial intervals. On the third day, the animals were re-introduced to the conditioning chamber and exposed to the same protocol as the previous day. The primary measure in all cases was freezing behavior, as assessed by Freezeframe software. Fear acquisition was assessed using freezing during each of the five tones of the training day (Day 1). Fear recall was assessed using freezing during the first five tones of the second day. Fear extinction was assessed using freezing during all 30 tones of the two extinction sessions (Days 2 and 3), with the post hoc analysis of fear extinction analyzing the last five tones on Day 3. Extinction retention was assessed by comparing freezing during the first five tones of Day 3 to freezing during the last five tones of Day 2. All outcome measures were analyzed using ANOVAs with between-subjects factors of group, age, and sex and within-subjects factor of time, followed by Bonferroni’s posthoc test.
Barnes maze
Mice were trained on a spatial memory task with negative reinforcement as previously described75. Briefly, mice were placed on a circular white table (92 cm across, 95 cm high) with 20 evenly spaced holes (5 cm) along the perimeter. A black plastic “escape cage” was located below one hole of the maze and colored paper shapes were mounted to the walls around the maze to act as visual cues. At the start of each trial, mice were placed under a black cylindrical cup at the center of the maze. After 30 s, the cup was lifted, and an alarm sound (100 dB) and a bright light (1800 lumens) were turned on. Mice were allowed to explore the maze for 3 min or until they entered the escape cage; mice that do not find the escape cage were placed under a clear cup and guided to the correct hole. Once in the escape cage, the lights and sound were turned off and the mouse rests for 1 min. Mice were trained using this procedure for five trials per day with 20-min inter-trial intervals for three consecutive days. On the fourth day, a final trial was performed as a probe test. The escape cage was removed, and the mice were given 3 min to find the correct hole. The test was recorded and analyzed using Noldus Ethovision XT, and the primary outcome measure was latency to enter the escape hole on the fourth day. Secondary outcome measures included the time in each quadrant on the fourth day (as a measure of search strategy), and the average latency per day across the three training days. Outcome measures were analyzed using ANOVAs with between-subjects factors of group, age, and sex (plus a within-subjects factor of time for latency per training day), followed by Bonferroni’s posthoc test.
Data analysis
Every effort was made to adhere to the essential 10 ARRIVE guidelines, including appropriate control groups, inclusion of all data from each experiment, randomization of treatments, and blinding of researchers to the identity of compounds for behavioral studies. All quantifiable data were reported as mean ± SEM. Distribution analyses were performed on all data sets to confirm normal data distribution. Homogeneity of variance (homoscedasticity) was also verified within each data set. When data set was not normally distributed or heterogeneous variance was detected, the distributions were normalized via log transformation. Sample size was determined according to power analysis. Intergroup differences were analyzed by unpaired two-tailed t-test for single comparison, or by 1-Way, 2-Way, or 3-Way ANOVA or repeated measures ANOVA with Tukey’s, Bonferroni’s, or Dunnett’s multiple comparison test as appropriate and as indicated under each method section and in the figure legends. Unless otherwise indicated, the difference between groups was statistically significant at P < 0.05, and it is indicated in the graphs by the asterisk (*) to denote comparison to the wildtype, control, vehicle-treated, non-induced or static group or by (#) to denote comparison between groups. The number of experimental replicates (N) is indicated in the figure legends. All statistical analyses were performed with GraphPad Prism version 5.0 or IBM SPSS Statistics 27.
Data availability
All data generated or analyzed in this study are included in this article and its supplementary information files. In addition, data from this study including raw data for cilia length, blood pressure, behavioral analyses, and original high-resolution images are available from the corresponding author upon reasonable request.
References
Hilgendorf, K. I., Myers, B. R. & Reiter, J. F. Emerging mechanistic understanding of cilia function in cellular signalling. Nat. Rev. Mol. Cell. Biol. https://doi.org/10.1038/s41580-023-00698-5 (2024).
Nauli, S. M., Jin, X. & Hierck, B. P. The mechanosensory role of primary cilia in vascular hypertension. Int. J. Vasc. Med. 2011, 376281. https://doi.org/10.1155/2011/376281 (2011).
Yoder, B. K. Role of primary cilia in the pathogenesis of polycystic kidney disease. J. Am. Soc. Nephrol. 18, 1381–1388. https://doi.org/10.1681/ASN.2006111215 (2007).
Singla, V. & Reiter, J. F. The primary cilium as the cell’s antenna: Signaling at a sensory organelle. Science 313, 629–633. https://doi.org/10.1126/science.1124534 (2006).
Berbari, N. F. et al. Hippocampal and cortical primary cilia are required for aversive memory in mice. PLoS One 9, e106576. https://doi.org/10.1371/journal.pone.0106576 (2014).
Yao, Q. et al. Pathophysiological association of Alzheimer’s disease and hypertension: A clinical concern for elderly population. Clin. Interv. Aging 18, 713–728. https://doi.org/10.2147/CIA.S400527 (2023).
Lennon, M. J., Koncz, R. & Sachdev, P. S. Hypertension and Alzheimer’s disease: Is the picture any clearer?. Curr. Opin. Psychiatry 34, 142–148. https://doi.org/10.1097/YCO.0000000000000684 (2021).
Toth, P. et al. Age-related autoregulatory dysfunction and cerebromicrovascular injury in mice with angiotensin II-induced hypertension. J. Cereb. Blood Flow Metab. 33, 1732–1742. https://doi.org/10.1038/jcbfm.2013.143 (2013).
Zlokovic, B. V. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron 57, 178–201. https://doi.org/10.1016/j.neuron.2008.01.003 (2008).
Kerkhofs, D. et al. Pharmacological depletion of microglia and perivascular macrophages prevents Vascular Cognitive Impairment in Ang II-induced hypertension. Theranostics 10, 9512–9527. https://doi.org/10.7150/thno.44394 (2020).
Qiu, C., Winblad, B. & Fratiglioni, L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 4, 487–499. https://doi.org/10.1016/S1474-4422(05)70141-1 (2005).
Katayama, T. & Hasebe, N. Angiotensin-receptor blockers, hypertension and Alzheimer disease–the entangled relationship. Circ. J. 77, 315–316. https://doi.org/10.1253/circj.cj-12-1550 (2013).
Yu, X., Ji, C. & Shao, A. Neurovascular unit dysfunction and neurodegenerative disorders. Front. Neurosci. 14, 334. https://doi.org/10.3389/fnins.2020.00334 (2020).
Nauli, S. M. et al. Non-motile primary cilia as fluid shear stress mechanosensors. Methods Enzymol. 525, 1–20. https://doi.org/10.1016/B978-0-12-397944-5.00001-8 (2013).
AbouAlaiwi, W. A. et al. Ciliary polycystin-2 is a mechanosensitive calcium channel involved in nitric oxide signaling cascades. Circ. Res. 104, 860–869. https://doi.org/10.1161/CIRCRESAHA.108.192765 (2009).
Mohieldin, A. M. et al. Vascular endothelial primary cilia: Mechanosensation and hypertension. Curr. Hypertens. Rev. 12, 57–67. https://doi.org/10.2174/1573402111666150630140615 (2016).
Nauli, S. M. et al. Endothelial cilia are fluid shear sensors that regulate calcium signaling and nitric oxide production through polycystin-1. Circulation 117, 1161–1171. https://doi.org/10.1161/CIRCULATIONAHA.107.710111 (2008).
Wang, J. Z. et al. Pin1, endothelial nitric oxide synthase, and amyloid-beta form a feedback signaling loop involved in the pathogenesis of Alzheimer’s disease, hypertension, and cerebral amyloid angiopathy. Med. Hypotheses 82, 145–150. https://doi.org/10.1016/j.mehy.2013.11.023 (2014).
Hammer, R. Muscarinic receptors in the stomach. Scand. J. Gastroenterol. Suppl. 66, 5–11 (1980).
Bonner, T. I., Buckley, N. J., Young, A. C. & Brann, M. R. Identification of a family of muscarinic acetylcholine receptor genes. Science 237, 527–532 (1987).
Caulfield, M. P. Muscarinic receptors–characterization, coupling and function. Pharmacol. Ther. 58, 319–379 (1993).
Caulfield, M. P. & Birdsall, N. J. International Union of Pharmacology. XVII. Classification of muscarinic acetylcholine receptors. Pharmacol Rev 50, 279–290 (1998).
Karam, C. S. et al. Signaling pathways in schizophrenia: Emerging targets and therapeutic strategies. Trends Pharmacol. Sci. 31, 381–390. https://doi.org/10.1016/j.tips.2010.05.004 (2010).
Gonzalez, S. A. et al. Sodium intake is associated with parasympathetic tone and metabolic parameters in mild hypertension. Am. J. Hypertens 25, 620–624. https://doi.org/10.1038/ajh.2012.10 (2012).
Lara, A. et al. Dysautonomia due to reduced cholinergic neurotransmission causes cardiac remodeling and heart failure. Mol. Cell Biol. 30, 1746–1756. https://doi.org/10.1128/MCB.00996-09 (2010).
Kakinuma, Y. et al. Acetylcholine from vagal stimulation protects cardiomyocytes against ischemia and hypoxia involving additive non-hypoxic induction of HIF-1alpha. FEBS Lett. 579, 2111–2118. https://doi.org/10.1016/j.febslet.2005.02.065 (2005).
Beny, J. L., Nguyen, M. N., Marino, M. & Matsui, M. Muscarinic receptor knockout mice confirm involvement of M3 receptor in endothelium-dependent vasodilatation in mouse arteries. J. Cardiovasc. Pharmacol. 51, 505–512. https://doi.org/10.1097/FJC.0b013e31816d5f2f (2008).
Khurana, S. et al. Vasodilatory effects of cholinergic agonists are greatly diminished in aorta from M3R-/- mice. Eur. J. Pharmacol. 493, 127–132. https://doi.org/10.1016/j.ejphar.2004.04.012 (2004).
He, X. et al. Activation of M3AChR (Type 3 muscarinic acetylcholine receptor) and Nrf2 (nuclear factor erythroid 2-related factor 2) Signaling by choline alleviates vascular smooth muscle cell phenotypic switching and vascular remodeling. Arterioscler Thromb. Vasc. Biol. 40, 2649–2664. https://doi.org/10.1161/ATVBAHA.120.315146 (2020).
Dauphin, F. & Hamel, E. Muscarinic receptor subtype mediating vasodilation feline middle cerebral artery exhibits M3 pharmacology. Eur. J. Pharmacol. 178, 203–213. https://doi.org/10.1016/0014-2999(90)90476-m (1990).
Harvey, R. D. Muscarinic receptor agonists and antagonists: Effects on cardiovascular function. Handb. Exp. Pharmacol. https://doi.org/10.1007/978-3-642-23274-9_13 (2012).
Avasthi, P. & Marshall, W. F. Stages of ciliogenesis and regulation of ciliary length. Differentiation 83, S30-42. https://doi.org/10.1016/j.diff.2011.11.015 (2012).
Ungvari, Z., Sun, D., Huang, A., Kaley, G. & Koller, A. Role of endothelial [Ca2+]i in activation of eNOS in pressurized arterioles by agonists and wall shear stress. Am. J. Physiol. Heart Circ. Physiol. 281, H606-612. https://doi.org/10.1152/ajpheart.2001.281.2.H606 (2001).
Behl, C., Davis, J. B., Lesley, R. & Schubert, D. Hydrogen peroxide mediates amyloid beta protein toxicity. Cell 77, 817–827. https://doi.org/10.1016/0092-8674(94)90131-7 (1994).
Shearman, M. S. et al. L-685,458, an aspartyl protease transition state mimic, is a potent inhibitor of amyloid beta-protein precursor gamma-secretase activity. Biochemistry 39, 8698–8704. https://doi.org/10.1021/bi0005456 (2000).
He, Y. et al. In utero hypoxia attenuated acetylcholine-mediated vasodilatation via CHRM3/p-NOS3 in fetal sheep MCA: Role of ROS/ERK1/2. Hypertens. Res. 45, 1168–1182. https://doi.org/10.1038/s41440-022-00935-y (2022).
Oddo, S. et al. Triple-transgenic model of Alzheimer’s disease with plaques and tangles: Intracellular Abeta and synaptic dysfunction. Neuron 39, 409–421. https://doi.org/10.1016/s0896-6273(03)00434-3 (2003).
Myers, K. M. & Davis, M. Mechanisms of fear extinction. Mol. Psychiatry 12, 120–150. https://doi.org/10.1038/sj.mp.4001939 (2007).
Marshall, W. F. & Nonaka, S. Cilia: Tuning in to the cell’s antenna. Curr. Biol. 16, R604-614. https://doi.org/10.1016/j.cub.2006.07.012 (2006).
Avalos, Y., Pena-Oyarzun, D., Budini, M., Morselli, E. & Criollo, A. New roles of the primary cilium in autophagy. Biomed. Res. Int. 2017, 4367019. https://doi.org/10.1155/2017/4367019 (2017).
Hu, C. et al. Sex-dependent effects of nephron Ift88 disruption on BP, renal function, and cystogenesis. J. Am. Soc. Nephrol. 32, 2210–2222. https://doi.org/10.1681/ASN.2020111571 (2021).
Reho, J. J., Guo, D. F., Morgan, D. A. & Rahmouni, K. Smooth muscle cell-specific disruption of the BBSome causes vascular dysfunction. Hypertension 74, 817–825. https://doi.org/10.1161/HYPERTENSIONAHA.119.13382 (2019).
Song, J. et al. Role of the primary cilia on the macula densa and thick ascending limbs in regulation of sodium excretion and hemodynamics. Hypertension 70, 324–333. https://doi.org/10.1161/HYPERTENSIONAHA.117.09584 (2017).
Ma, R., Kutchy, N. A., Chen, L., Meigs, D. D. & Hu, G. Primary cilia and ciliary signaling pathways in aging and age-related brain disorders. Neurobiol. Dis. 163, 105607. https://doi.org/10.1016/j.nbd.2021.105607 (2022).
Zhao, Y. & Rahmouni, K. BBSome: A new player in hypertension and other cardiovascular risks. Hypertension 79, 303–313. https://doi.org/10.1161/HYPERTENSIONAHA.121.17946 (2022).
Hu, L., Wang, B. & Zhang, Y. Serotonin 5-HT6 receptors affect cognition in a mouse model of Alzheimer’s disease by regulating cilia function. Alzheimers Res. Ther. 9, 76. https://doi.org/10.1186/s13195-017-0304-4 (2017).
Mykytyn, K. & Askwith, C. G-protein-coupled receptor signaling in cilia. Cold Spring Harb. Perspect. Biol. https://doi.org/10.1101/cshperspect.a028183 (2017).
Brewer, K. M. et al. Physiological condition-dependent changes in ciliary GPCR localization in the brain. eNeuro https://doi.org/10.1523/ENEURO.0360-22.2023 (2023).
Nachury, M. V. The molecular machines that traffic signaling receptors into and out of cilia. Curr. Opin. Cell Biol. 51, 124–131. https://doi.org/10.1016/j.ceb.2018.03.004 (2018).
Schou, K. B., Pedersen, L. B. & Christensen, S. T. Ins and outs of GPCR signaling in primary cilia. EMBO Rep. 16, 1099–1113. https://doi.org/10.15252/embr.201540530 (2015).
Sabbir, M. G. & Fernyhough, P. Muscarinic receptor antagonists activate ERK-CREB signaling to augment neurite outgrowth of adult sensory neurons. Neuropharmacology 143, 268–281. https://doi.org/10.1016/j.neuropharm.2018.09.020 (2018).
Tissir, F. & Goffinet, A. M. Cilia: Conductors’ batons of neuronal maturation. Nat. Neurosci. 15, 344–345. https://doi.org/10.1038/nn.3050 (2012).
Faraci, F. M. & Sigmund, C. D. Vascular biology in genetically altered mice: Smaller vessels, bigger insight. Circ. Res. 85, 1214–1225. https://doi.org/10.1161/01.res.85.12.1214 (1999).
Huang, T. et al. Detection of basal acetylcholine in rat brain microdialysate. J. Chromatogr. B Biomed. Appl. 670, 323–327. https://doi.org/10.1016/0378-4347(95)00181-6 (1995).
Matsui, M. et al. Mice lacking M2 and M3 muscarinic acetylcholine receptors are devoid of cholinergic smooth muscle contractions but still viable. J Neurosci 22, 10627–10632. https://doi.org/10.1523/JNEUROSCI.22-24-10627.2002 (2002).
Stengel, P. W., Yamada, M., Wess, J. & Cohen, M. L. M(3)-receptor knockout mice: Muscarinic receptor function in atria, stomach fundus, urinary bladder, and trachea. Am. J. Physiol. Regul. Integr. Comp. Physiol. 282, R1443-1449. https://doi.org/10.1152/ajpregu.00486.2001 (2002).
Matsui, M. et al. Multiple functional defects in peripheral autonomic organs in mice lacking muscarinic acetylcholine receptor gene for the M3 subtype. Proc. Natl. Acad. Sci. U S A 97, 9579–9584. https://doi.org/10.1073/pnas.97.17.9579 (2000).
Deng, A. Y. et al. Functional dosage of muscarinic cholinergic receptor 3 signalling, not the gene dose, determines its hypertension pathogenesis. Can. J. Cardiol. 35, 661–670. https://doi.org/10.1016/j.cjca.2018.12.029 (2019).
Rhoden, A. et al. Preserved cardiovascular homeostasis despite blunted acetylcholine-induced dilation in mice with endothelial muscarinic M3 receptor deletion. Acta Physiol. (Oxf) 226, e13262. https://doi.org/10.1111/apha.13262 (2019).
Stoehr, A. et al. Spontaneous formation of extensive vessel-like structures in murine engineered heart tissue. Tissue Eng. Part A 22, 326–335. https://doi.org/10.1089/ten.TEA.2015.0242 (2016).
Boulanger, C. M., Morrison, K. J. & Vanhoutte, P. M. Mediation by M3-muscarinic receptors of both endothelium-dependent contraction and relaxation to acetylcholine in the aorta of the spontaneously hypertensive rat. Br. J. Pharmacol. 112, 519–524. https://doi.org/10.1111/j.1476-5381.1994.tb13104.x (1994).
Gericke, A. et al. Role of M1, M3, and M5 muscarinic acetylcholine receptors in cholinergic dilation of small arteries studied with gene-targeted mice. Am. J. Physiol. Heart Circ. Physiol. 300, H1602-1608. https://doi.org/10.1152/ajpheart.00982.2010 (2011).
Kovacevic, I. et al. The F-BAR Protein NOSTRIN dictates the localization of the muscarinic M3 receptor and regulates cardiovascular function. Circ. Res. 117, 460–469. https://doi.org/10.1161/CIRCRESAHA.115.306187 (2015).
Yamaguchi, S. et al. Antihypertensive mechanism of orally administered acetylcholine in spontaneously hypertensive rats. Nutrients https://doi.org/10.3390/nu14040905 (2022).
Iadecola, C. & Gottesman, R. F. Neurovascular and cognitive dysfunction in hypertension. Circ. Res. 124, 1025–1044. https://doi.org/10.1161/CIRCRESAHA.118.313260 (2019).
d’Uscio, L. V., He, T. & Katusic, Z. S. Expression and processing of amyloid precursor protein in vascular endothelium. Physiology (Bethesda) 32, 20–32. https://doi.org/10.1152/physiol.00021.2016 (2017).
Austin, S. A., d’Uscio, L. V. & Katusic, Z. S. Supplementation of nitric oxide attenuates AbetaPP and BACE1 protein in cerebral microcirculation of eNOS-deficient mice. J. Alzheimers Dis. 33, 29–33. https://doi.org/10.3233/JAD-2012-121351 (2013).
Dorovini-Zis, K., Prameya, R. & Bowman, P. D. Culture and characterization of microvascular endothelial cells derived from human brain. Lab. Invest. 64, 425–436 (1991).
Yasuda, H. & Niki, H. Review of the pharmacological properties and clinical usefulness of muscarinic agonists for xerostomia in patients with Sjogren’s syndrome. Clin. Drug Investig. 22, 67–73. https://doi.org/10.2165/00044011-200222020-00001 (2002).
Hulme, E. C., Birdsall, N. J. & Buckley, N. J. Muscarinic receptor subtypes. Annu. Rev. Pharmacol. Toxicol. 30, 633–673. https://doi.org/10.1146/annurev.pa.30.040190.003221 (1990).
Alva, J. A. et al. VE-Cadherin-Cre-recombinase transgenic mouse: A tool for lineage analysis and gene deletion in endothelial cells. Dev. Dyn. 235, 759–767. https://doi.org/10.1002/dvdy.20643 (2006).
Mueller, K. B. et al. Endothelial mineralocorticoid receptors differentially contribute to coronary and mesenteric vascular function without modulating blood pressure. Hypertension 66, 988–997. https://doi.org/10.1161/HYPERTENSIONAHA.115.06172 (2015).
Wang, Y., Thatcher, S. E. & Cassis, L. A. Measuring blood pressure using a noninvasive tail cuff method in mice. Methods Mol. Biol. 1614, 69–73. https://doi.org/10.1007/978-1-4939-7030-8_6 (2017).
Pyla, R., Osman, I., Pichavaram, P., Hansen, P. & Segar, L. Metformin exaggerates phenylephrine-induced AMPK phosphorylation independent of CaMKKbeta and attenuates contractile response in endothelium-denuded rat aorta. Biochem. Pharmacol. 92, 266–279. https://doi.org/10.1016/j.bcp.2014.08.024 (2014).
Pitts, M. W. Barnes maze procedure for spatial learning and memory in mice. Bio Protocol https://doi.org/10.21769/bioprotoc.2744 (2018).
Acknowledgements
This work was supported by Grants R15HL140523, 3R15HL140523-01S1, 3R15HL140523-01S2, 3R15HL140523-01S3 to W.A., American Heart Association (AHA) Predoctoral Award #19PRE34430055 to H.S., American Foundation of Pharmaceutical Education (AFPE) Gateway to Research Award to R.B., and the University of Toledo Office of Research and Sponsored Programs. The support in part from the Alzheimer’s Association Grant AARGD-NTF-22-972749, from NIA through Grant 1R03AG080418-01, and from NHLBI through Grant 5R25HL105446-12 to W.A. is gratefully acknowledged. This work was also supported by an NHLBI award R00 HL153896 to I.O. We thank the University of California at Irvine and Dr. Frank LaFerla for providing the 3xTgAD mice under MTA#2022-089, and Dr. Jurgen Wess at the NIH/NIDDK for providing the Chrm3flox/flox mice. We thank Dr. Scott W. Crawley and Dr. Rafael Garcia-Mata at the University of Toledo Department of Biological Sciences for their support with Chrm3 cloning and CHRM3 overexpression studies.
Author information
Authors and Affiliations
Contributions
H.C.S., K.V.F., M.A.M., R.B., C.L.S., G.G., S.K., C.A.M., and A.M.M. contributed to the acquisition and analysis of data. W.S.M., I.A.O., J.P.B., and W.A.A contributed to the experimental design, analysis and interpretation of data, manuscript draft and revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests. Dr. W.S.M. is the founder and president of Psyneurgy Pharmaceuticals LLC.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Saternos, H.C., Forero, K.V., Meqdad, M.A. et al. Muscarinic acetylcholine receptor 3 localized to primary endothelial cilia regulates blood pressure and cognition. Sci Rep 15, 3745 (2025). https://doi.org/10.1038/s41598-025-87212-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87212-3