Abstract
We investigated the effectiveness of Virtual Reality (VR) and three-dimensional (3D)-printed mannequins in replicating stress levels during pericardiocentesis training and compared their impact on learners’ emotional and physiological responses. A secondary analysis explored how demographic, lifestyle, and academic factors influence stress responses, providing deeper insights into the variability of physiological markers among medical trainees. We conducted a randomized study involving 108 final-year medical students (mean age: 23.6 years, 87% female) to compare stress responses during pericardiocentesis training using a 3D-printed mannequin and VR model as simulation modalities, both custom-designed by the research team. We investigated the influence of demographic, lifestyle, and academic factors, including medication use and perceived stress, on heart rate variability (HRV) markers. The two simulations showed similar HRV parameters, validating their effectiveness in replicating physiological stress levels associated with clinical scenarios. Secondary analysis revealed significant associations between the low frequency/high frequency ratio and family income and a trend-level effect for anxiolytic use, suggesting an interplay of socioeconomic and pharmacological factors on stress responses. Age and sex interacted significantly with HRV metrics, with younger students demonstrating heightened sympathetic activation. Our results suggest that the incorporation of VR into medical training programs may enhance learning outcomes and accessibility.
Similar content being viewed by others
Introduction
The field of medical education has been revolutionized by adopting simulation-based learning1, which aligns with the “learning by doing” philosophy. This approach enhances patient safety by allowing students to practice clinical procedures in safe environments, offering reproducible scenarios for consistent learning outcomes while accommodating various educational levels. Despite its widespread benefits, the application of simulation-based learning is often hampered by the high cost of advanced simulators and steep learning curves for instructors, which can exacerbate educational disparities, particularly in economically constrained settings2.
Advances in three-dimensional (3D) printing and virtual reality (VR) technology have addressed some of these challenges3. Three-dimensional printing offers a cost-effective way to create detailed medical models, enhancing the flexibility of simulations, whereas VR provides immersive environments that promote sensory and emotional engagement4.
Despite these advances understanding the emotional and physiological impact of simulations, particularly their ability to elicit authentic stress responses during high-stake medical procedures remains a significant challenge5. In this study we aimed to bridge this gap by focusing on pericardiocentesis—a complex and stress-inducing procedure. Specifically, we compared the efficacy of 3D-printed mannequins and VR simulations in generating realistic stress responses, measured through heart rate variability (HRV), a validated biomarker of autonomic activity.
Related work
HRV is a widely recognized biomarker for assessing psychophysiological stress, reflecting autonomic nervous system activity6. In medical simulations, HRV provides objective insights into stress responses which is valuable for tailoring training to enhance emotional preparedness for clinical emergencies. However, differences in stress dynamics between simulations and real-world scenarios, such as anticipatory effects and observer-biases, necessitate the refinement of simulation environments to better replicate clinical pressures7.
VR and mannequin-based simulations effectively induce physiological and psychological stress, albeit with varying intensities8. VR generally elicits slightly lower physiological stress than mannequins do; however, its immersive and realistic nature enhances learner engagement and motivation, leading to performance outcomes comparable to those of traditional methods. Despite this, VR alone may not fully replicate the intensity of real life stress, suggesting its optimal use is as part of a multimodal training strategy9.
Pericardiocentesis is a high-risk and stress-inducing procedure because of its complexity. Simulation-based training using VR and high-fidelity mannequins offers a safe environment for developing procedural skills and decision-making10. VR has been shown to induce moderate stress levels in other medical scenarios; however, its effectiveness in pericardiocentesis training remains unexplored, representing a critical gap in the current literature.
Stress responses in simulation-based learning are influenced by diverse demographic and lifestyle factors, many of which remain underexplored in this context. Prior studies have focused on variables such as sex and age, frequently observing heightened stress levels in female and younger participants11. We expand the scope by analyzing less commonly addressed parameters, including caffeine consumption, the use of cardiac medications, and physical activity habits. By incorporating these additional factors, this study provides a more nuanced understanding of individual variability in stress responses, highlighting the interplay between physiological predispositions and simulated stress conditions. This broader perspective underscores the need to integrate both traditional demographic variables and underexplored lifestyle factors to optimize training outcomes and educational interventions.
This study is unique in its simultaneous analysis of stress responses using biometric parameters across two distinct simulation environments —VR and high-fidelity mannequin-based simulations—in the context of a high-risk procedure like pericardiocentesis. Unlike previous research focusing on single simulation modalities or general procedures, we directly compared stress induction between VR and traditional methods in a complex clinical scenario. We also conducted a secondary analysis of demographic and lifestyle factors, including caffeine consumption, medication use, physical activity, and critical mental health parameters, such as suicidal ideation and thoughts of quitting the profession. These variables, which are rarely addressed in the context of medical training, provide a comprehensive perspective on the profound stressors medical students face. By combining these approaches, this study offers novel insights into the interplay between individual characteristics, simulation modalities, and physiological stress responses, contributing significantly to the development of more effective and supportive medical education strategies.
Methods
Objective
This validation study builds on previous pilot research to compare two simulation methods for pericardiocentesis training: a 3D-printed mannequin and a VR system developed by researchers using the Unity game engine. The primary objective of this study was to evaluate and compare the effectiveness of these methods in eliciting realistic emotional and physiological responses commonly encountered during medical procedures.
Randomization and participant grouping
A total of 132 final-year medical students from a Faculty of Medicine in Madrid were enrolled at the start of the academic year. Although no formal sample size calculation was performed due to the limited pool of available and willing participants, the sample size was sufficient to capture meaningful variations in stress responses across demographic and lifestyle factors. Before participation, the students completed demographic, lifestyle, and health behavior questionnaires. Participants were randomly assigned to two groups using a computer-generated sequence: one group began with VR training followed by the mannequin simulation, whereas the other group started in reverse order. This counterbalanced design minimized the potential order effects on learning outcomes and stress responses.
Development and validation of the training models
The 3D-printed mannequin was developed in-house by undergraduate students in the Medicine and Biology programs using free software, including Tinkercad and Adobe Fusion 360, to ensure accessibility and reproducibility. Slicing was performed using Ultimaker Cura, and the mannequin was printed on an Ender 3 device using cost-effective materials. This low-cost approach underscores the feasibility of creating high-quality educational tools in resource-limited settings. The VR simulation was developed in Unity 2018.4.36f1 with the TextMesh Pro 1.4.1 and OpenVR (Desktop) 1.0.5 plugins, targeting VR devices connected to a PC that are compatible with the SteamVR framework. To ensure a realistic representation of the room, the instruments and the patient, high-quality 3D models were sourced from third party professional 3D modelling professionals when possible. For some specific items that had low polygonal complexity and were not available in 3D asset stores (betadine bottle, glove box, cloth, finger pulse oximeter and electrodes), the models were created by researchers. The videos and sounds shown in the vital signs monitor pictured in the simulation were recorded by researchers from real medical devices. The full code of the VR application has been made available through an open-source license and can be freely downloaded from the GitHub code-sharing website, so they can be expanded by anybody for future research. The finished application can also be downloaded, together with a video showing the full procedure in the application, on the same website. Both simulations were validated by a panel of five clinical experts in critical care using the two-round Delphi method. The first round evaluated anatomical accuracy and design fidelity, whereas the second focused on usability and educational value. Although both models were highly praised for their realism, the lack of strong haptic feedback in the VR system (only slight vibrations on the controllers) was noted as a limitation. The participants also completed usability questionnaires following the simulations, which confirmed the highly perceived realism of the virtual model (a System Usability Score of 75.03).
Each participant completed two simulation sessions:
VR simulation: Students were exposed to an immersive VR environment running in a laptop with an Intel Core i7-7700HQ CPU, 16 GB of RAM, a NVIDIA GeForce GTX 1070 GPU with 8 GB of RAM, connected to an Oculus Rift S VR headset and running Windows 10 and SteamVRs. The simulation mirrored the anatomical features and procedural context of the 3D-printed mannequin. Tasks included the following.
-
Identifying anatomical landmarks.
-
Preparing the site for needle insertion.
-
Performing simulated pericardiocentesis.
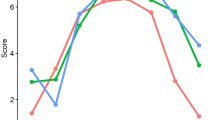
The VR environment used in this study is illustrated in Fig. 1.
Three-dimensional printed mannequin simulation: The participants were trained with a mannequin created using Tinkercad and Adobe Fusion 360. The pericardium mold was printed with an Ender 3 device using Ultimaker Cura. The tasks were identical to those in the VR simulation to ensure comparability. The 3D-printed mannequin used for simulation tasks is depicted in Fig. 2.
Each session lasted between 15 and 30 min, depending on the participants’ pace, followed by a 10-min rest period to allow for physiological recovery and mitigate carryover effects.
Ethical considerations and recruitment
The study was approved by the Research Ethics Committee of HM Monteprincipe University Hospital (Code: 18.12.1339.GHM) and spanned from November 7, 2023, to February 12, 2024 and conducted in accordance whit these regulations. All participants provided written informed consent, and their data were anonymized to ensure confidentiality.
Inclusion and exclusion criteria
All final-year medical students were eligible, except those on cardiac medication, excessive caffeine consumption (more than 3 cups per day), or simpaticomimetics, and those with incomplete data or improperly recorded signals (18.1% exclusion rate). The participants received standardized training through an instructional video of pericardiocentesis before the simulations.
Stress response measurement
Stress responses were assessed using the Biosignal Plux system, which continuously monitors heart rate through three electrodes placed on the participant’s torso. This setup was established before the simulation sessions to ensure consistent and reliable data collection. The system recorded HRV data with precise time-stamping, allowing for a detailed analysis of stress responses during specific phases of the simulation procedure. Data acquisition, processing, and conversion into values for statistical analysis were conducted using OpenSignals v.1.6.3 software.
HRV, a sensitive biomarker of autonomic nervous system activity, was chosen as the primary measure of physiological stress because it can quantify the balance between sympathetic and parasympathetic responses under stress-inducing conditions12. The HRV parameters analyzed included the following:
-
Frequency-domain parameters
-
Low frequency (LF): Reflects sympathetic activation, with some parasympathetic influence.
-
High frequency (HF): Indicates parasympathetic activity, associated with stress relief mechanisms.
-
LF/HF ratio: Reflects the balance between sympathetic and parasympathetic activity, with higher ratios indicating increased stress levels.
-
-
Time-domain parameters
-
Root Mean Square of Successive Differences (rMSSD): Measures short-term variability in heart rate, directly linked to parasympathetic control.
-
Percentage of successive NN intervals that differed by more than 20 ms (PNN20) and 50 ms (PNN50): Indicators of parasympathetic activity and HRV.
-
-
Non-linear parameters
-
SD1/SD2 ratio: This metric, derived from Poincarè plots, correlates with the LF/HF ratio and reflects the complexity of HRV patterns during stress.
-
These parameters provide a comprehensive profile of the participants’ stress responses, offering valuable insights into the impact of different simulation modalities on autonomic regulation.
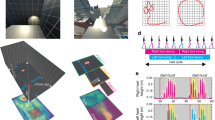
Figure 3 illustrates a participant equipped with the Biosignal Plux system. Figure 4 presents Poincaré plots depicting HRV patterns under basal conditions, rest conditions, mannequin-based simulation, and VR simulation.
Poincaré Plots illustrate the heart rate variability under four conditions: basal, rest, VR and mannequin-based simulations. Each scatter plot represents the relationship between consecutive NN intervals (NNi and NNi + 1, in ms) as measure of autonomic regulation, providing a visual depiction of autonomic regulation and stress responses.
Secondary analysis of stress indicators
A secondary analysis was performed to investigate the impact of external factors, including medication use, lifestyle habits, and academic pressures, on stress responses. This approach contextualized the physiological data, providing a deeper understanding of the multifactorial influences on stress levels during clinical training. Key variables such as the use of anxiolytics or antidepressants, caffeine consumption, physical activity, and self-reported academic and mental health challenges (e.g., suicidal ideation or thoughts of quitting) were included to offer a comprehensive perspective on stress regulation in medical students.
Data collection phases
Data collection was conducted in three distinct phases to ensure robust comparative analyses of the stress responses.
-
Baseline data collection: Stress data were initially recorded during a resting state to establish baseline physiological levels for each participant.
-
First training scenario: Students were assigned to either the mannequin-based or VR simulation, followed by a 10-min resting phase to minimize carryover effects between scenarios.
-
Second Training Scenario: Participants underwent training using the alternate method (VR or mannequin), enabling direct within-subject comparisons of stress responses across simulation modalities.
Statistical analysis
Stress parameters were analyzed using IBM SPSS software version 20, employing a combination of parametric and nonparametric tests to ensure robust and reliable results:
-
Normality testing: The Kolmogorov–Smirnov test was applied to assess the data distribution, guiding the selection of statistical tests.
-
Comparative analysis: The Friedman test was used to evaluate intragroup differences across conditions (baseline, simulation, rest, VR).
-
Paired comparisons: Friedman and Wilcoxon signed-rank tests were applied to identify significant differences between specific conditions.
-
Correlation analysis: Spearmans rank correlation coefficient was used to explore associations between HRV parameters and continuous demographic variables, such as hours of study and well-being scores.
-
Group comparisons: The Mann-Whitney U test was used to compare HRV parameters between the binary groups (e.g., use of anxiolytics, suicidal ideation, or thoughts of quitting).
-
Secondary analysis: Repeated-measures analysis of variance was performed to examine the influence of demographic and lifestyle factors on stress responses, with post hoc analyses conducted using Bonferroni and Tukey corrections for multiple comparisons.
Nonparametric tests were applied when the distributional assumptions for parametric tests were violated. This multifaceted statistical approach allowed for a detailed evaluation of physiological stress markers across simulation modalities, while also accounting for individual demographic and lifestyle variations.
Results
Demographic and lifestyle characteristics
Our study initially enrolled 132 medical students, with 108 (2 groups of 54 students each) included in the final analysis after applying the eligibility criteria. Most participants were female (87%), and the mean age of the participants was 23.6 years. Most students (78%) reported no prior experience with VR headsets. To contextualize the external influences on stress a comprehensive assessment of demographic and lifestyle factors was conducted. The variables included marital status, living arrangements, family income, work-study balance, and familial responsibilities (Table 1). The analysis also explored the impact of health-related behaviors, such as smoking, alcohol consumption, caffeine intake, physical activity, and medication use (Table 2). Additionally, academic and mental health variables—such as study hours, perceived stress, and thoughts of quitting or self-harm—were evaluated to understand the broader spectrum of influences on stress responses (Table 3).
Biological stress analysis
HRV parameters were analyzed across four simulation stages: basal, rest, mannequin-based simulation, and VR simulation. The Friedman test revealed significant differences in HRV parameters across these stages (p < 0.01), as shown in Table 4; Figs. 5 and 6. These results highlight the sensitivity of HRV markers in capturing dynamic stress responses and recovery phases in diverse simulation environments. For instance, rMSSD (χ2(3) = 27.30) increased significantly during both VR and mannequin-based simulations compared to the basal state, signaling heightened parasympathetic activity. Similarly, the LF/HF ratio (χ²(3) = 34.38) increased during simulations, reflecting a shift toward sympathetic dominance. These physiological changes underline the utility of HRV metrics for assessing stress under controlled conditions.
Figures 5 and 6 illustrate the variations in HRV markers, showing comparable stress responses in both VR and mannequin-based scenarios. The Poincaré plot values further confirmed this equivalence, demonstrating that VR effectively replicates the activation and relaxation patterns observed in traditional simulation methods, as seen in Fig. 4.
We next conducted a Wilcoxon signed-rank test to compare the HRV parameters between the two rest phases (basal and resting) and, more critically, between the VR and mannequin simulation phases. The analysis showed no significant differences between the stress responses elicited by the VR and mannequin simulations, indicating that both modalities effectively simulated the stress levels experienced in clinical scenarios. The absence of significant differences (p > 0.05) in the biometric parameters between VR and mannequin-based simulations supports the validity of both environments in inducing comparable physiological states during high-stakes simulations as shown in Table 5. This demonstrates the potential of VR to replicate activation and relaxation responses like those observed in traditional simulations. Additionally, the significant change observed in SD1/SD2 during the basal/rest phase (p = 0.002) suggests that this parameter may have greater sensitivity in detecting subtle physiological changes in certain stages. These findings underscore the utility of HRV metrics for objectively assessing stress responses in diverse simulation environments.
Bias and sequence effect analysis
An analysis was performed to address potential biases stemming from the sequence of simulation exposure (VR-first vs. mannequin-first). Tables 6 and 7 present HRV parameters stratified by exposure order, revealing that the sequence did not significantly affect stress responses. This finding reinforces the robustness of our experimental design and confirms the equivalence of both training modalities in eliciting stress responses.
Secondary analysis of the stress parameters
A secondary analysis explored the relationships between demographic, lifestyle, and mental health variables and HRV markers, with a focus on the LF/HF ratio. Table 8 summarizes the findings, revealing significant associations between LF/HF and factors such as family income (p = 0.020) and a trend-level effect for anxiolytic use (p = 0.082).
Following the univariate analyses, we performed a multivariate analysis to explore whether factors that appeared to suggest potential relationships with the LF/HF ratio—such as family income and the use of anxiolytics—might interact or amplify each other’s effects. This approach allowed us to evaluate the combined influence of multiple demographic, lifestyle, and mental health variables on autonomic stress responses. One of the objectives of this analysis was to identify high-risk profiles among medical students who may be more vulnerable to stress and burnout, enabling the development of tailored interventions to mitigate these risks. By examining potential synergies or compounding effects among these factors, we sought to uncover complex patterns that may not have been evident in the univariate analysis. This secondary analysis employed repeated-measures ANOVA with Bonferroni and Tukey’s post-hoc tests, ensuring a rigorous exploration of the intricate relationships between stress responses and the multifactorial determinants of physiological stress in medical students.
Age and sex influences: Significant interactions were observed between the HRV parameter RMSSD and the combined factors of age and sex (Table 9). These findings emphasize the importance of demographic variations in physiological stress responses during medical simulations. Specifically, differences in autonomic regulation between age groups and sexes suggest that stress is experienced differently across these demographics, which has potential implications for tailoring simulation-based training to individual needs.
Lifestyle dynamics: Our findings demonstrate that lifestyle factors, particularly family income and work-study balance, significantly influence stress responses (Table 10). The LF/HF ratio, an indicator of sympathetic activity, was strongly correlated with family income (p = 0.001) and showed a trend toward significance for its correlation with work-study balance (p = 0.057). These results suggest that economic pressures and the dual demands of work and study intensify stress levels among medical students.
Consumption habits: The impact of consumption habits such as smoking, alcohol consumption, and caffeine consumption on stress was less pronounced, with minimal influence on the primary stress markers.
Medication impact: The combined use of anxiolytics and antidepressants showed complex interactions that significantly affected stress biomarkers.
Academic and perceived stress: Contrary to initial expectations, our study revealed no significant correlations between study habits, perceived academic stress, and physiological stress markers among final-year medical students. This finding suggests that students, who have progressed through rigorous academic training over several years, may have developed effective coping mechanisms to manage and mitigate the physiological manifestations of stress. This adaptation may explain why academic demands and self-perceived stress did not markedly alter the physiological stress responses of the group. However, variations may exist in different student populations or distinct educational settings, indicating a potential area for further research to explore how stress coping mechanisms evolve throughout medical education. Certain interactions between lifestyle factors, such as family income and work-study balance, showed significant effects on the LF/HF ratio (p = 0.001), whereas interactions between many others did not (p > 0.05), as shown in Table 10 9. For example, marital status and living arrangements (p = 0.743) or their interaction with family income and responsibilities (p = 0.9) yielded nonsignificant results. These findings may reflect the nuanced and indirect influence of these variables, which could require larger sample sizes or alternative modeling approaches. Additionally, trends observed in variables with p-values near the threshold of significance (e.g., work-family balance, p = 0.051) highlight areas for further investigation, suggesting that these factors may still play a meaningful role in modulating stress responses. This underscores the importance of considering both statistically significant and non-significant trends when interpreting complex relationships between demographic and lifestyle factors in medical simulation training.
Discussion
Our results suggest that VR is comparable to traditional mannequin-based training in simulating stress responses during pericardiocentesis. Although VR offers an immersive and interactive environment, our findings cautiously support its equivalence rather than its superiority over traditional methods. This aligns with research by Mergen et al., who noted the capability of VR in procedural training without conclusively establishing its enhancement of clinical decision-making skills13. These findings underscore the importance of integrating VR with complementary training approaches to achieve comprehensive educational outcomes.
In line with Bolton et al.’s findings, VR has the potential to enhance access to medical training in low- and middle-income countries14. However, to maximize its impact, broader applications must prioritize sustainability and adaptability to local contexts, addressing challenges such as infrastructure limitations and economic barriers. Additionally, as Weissglass highlighted, the integration of emerging technologies such as medical artificial intelligence with VR necessitates robust policy frameworks to mitigate biases and ensure equitable access15.
We explored the integration of 3D modeling with VR and demonstrated its potential to enhance both the cost-effectiveness and accessibility of medical training. This approach aligns with the findings from Roh et al., who emphasized the benefits of using open-source software and photorealistic 3D models in surgical training16. Such advancements hold relevance for resource-limited settings, where cost-effective and scalable solutions can significantly improve the reach and impact of simulation-based education.
We also examined the psychological aspects of medical training. By incorporating 3D-printed mannequins and VR, we addressed the technical and emotional challenges healthcare professionals face. Similar findings by Towers et al. highlight the value of such methods in fostering emotional resilience17. Further, Rochlen et al. reported significant improvements in student confidence and procedural accuracy using VR and 3D technology18.
The application of VR in critical care settings, as discussed by Bruno et al., highlights its potential to enhance educational outcomes, while presenting challenges related to technology integration, cost, and ethical considerations19. These insights underscore the need to navigate technical and human factors to fully exploit the benefits of immersive technologies in high-stake environments.
Our secondary analysis revealed significant interactions between stress parameters and demographic variables, including age, sex, lifestyle, and medication consumption. Younger participants (< 23 years) exhibited higher LF/HF ratios during the simulations, indicating greater sympathetic activation compared with older participants. This finding is consistent with Helman et al.’s study, which indicated that younger individuals, who often have less clinical exposure, perceive simulations as more stressful, leading to greater physiological responses20.
Interestingly, the use of anxiolytics was somehow associated with alterations in HRV parameters, such as higher LF/HF ratios, suggesting that baseline autonomic regulation may be affected in individuals using these medications. These findings emphasize the need to consider medical treatments when designing and interpreting simulation-based training outcomes, because such treatments may independently modulate stress responses, irrespective of demographic or experiential variables.
No significant differences in HRV metrics were observed based on sex, which contrasts with existing literature reporting higher self-reported stress levels in female participants21. This divergence highlights the importance of using objective biometric measures, which may provide a more reliable understanding of stress responses than subjective assessments alone.
In terms of lifestyle, family income and work-study balance significantly influenced stress-related physiological responses, underscoring the complex interplay between socioeconomic factors and stress. These findings align with prior observations, such as Kreutz et al.’s work on the effects of lifestyle changes induced by the coronavirus disease pandemic on blood pressure and hypertension, further illustrating the interconnectedness of lifestyle factors and health outcomes22. However, other lifestyle habits, including caffeine consumption and physical activity, did not exhibit significant associations with HRV in this study.
Finally, including HRV analysis in VR simulations provides a novel approach for assessing stress responses, which is critical in preparing medical professionals to perform effectively under pressure. This aspect of our study aligns with the findings of Corrigan et al.23, who emphasized the ability of VR to replicate and manage real-world stress conditions effectively24.
These insights emphasize the complexity of physiological responses to stress and underscore the importance of personalized training approaches that account for demographic, pharmacological, and socioeconomic variability. Designing simulations that address these individual differences can improve medical students’ emotional and technical preparedness across diverse learner populations.
Several limitations should be considered when interpreting these findings. First, participant recruitment was based on voluntary enrollment without a formal sample size calculation. Although the sample size was adequate to detect meaningful variations in stress responses, this convenience sampling approach may restrict the generalizability of the findings to a wider population. Second, the study was conducted in a high-income country, which limits the applicability of our results to settings with different economic and healthcare conditions. Moreover, the participant group was limited to final-year medical students, raising questions about the generalizability of the findings to other populations. For instance, first-year medical students, who typically have less clinical exposure and underdeveloped stress management skills, may exhibit heightened physiological stress responses in similar simulations. Conversely, practicing healthcare professionals, equipped with advanced coping mechanisms and greater clinical expertise, may display more stable autonomic responses and perceive these simulations as less challenging. Additionally, the focus on pericardiocentesis, a complex and high-stakes procedure, may not fully capture the range of stress responses encountered across different medical scenarios. For instance, less invasive tasks, such as basic suturing, are unlikely to elicit similar levels of physiological activation. In contrast, highly dynamic and time-sensitive interventions, such as trauma resuscitation and advanced cardiac life support, may trigger more pronounced sympathetic responses. Future studies should explore how simulation-based training impacts stress responses across a wider spectrum of medical procedures to optimize educational strategies for various clinical contexts. Finally, our focus on a single VR platform and a specific 3D-printed mannequin limits the generalizability of the findings to other training models or technological implementations. Future research should explore the applicability of diverse VR platforms and 3D-printing technologies in various educational scenarios to provide a more comprehensive understanding of their potential in medical training.
This study makes a unique contribution to medical education by directly comparing stress responses in two distinct simulation modalities—VR and high-fidelity mannequins—within the context of pericardiocentesis. Employing objective biomarkers, such as HRV, enhances the reliability of the findings and provides valuable insights into the physiological and psychological impact of these educational tools.
A key strength of this work lies in the cost-effective development of the training models, both of which were designed and implemented by the research team, including medical and biotechnology students, using widely accessible software and hardware. The affordability of the 3D-printed mannequin and VR system makes this approach highly scalable and adaptable for institutions with limited financial resources, thereby promoting the democratization of access to simulation-based training. By reducing the financial barriers associated with advanced simulators, this study highlights a pathway for integrating innovative educational tools in diverse educational settings. By incorporating feedback from clinical experts during the validation process, this study ensures the clinical and educational relevance of the models, thereby setting a benchmark for future simulation-based research. The findings underscore the potential of VR as an effective and accessible training tool, particularly in resource-limited settings or when traditional training methods are impractical. Additionally, the study’s implications extend beyond medical students in their final year, offering a framework that can be adapted for other learner groups and procedures of varying complexity. Finally, the open accessibility of the VR model via GitHub promotes reproducibility and encourages further innovation in the development of simulation-based training tools.
Future research should prioritize evaluating the generalizability of these findings across diverse learner populations, such as first-year medical students, residents, and practicing healthcare professionals. Exploring how stress responses vary with levels of clinical experience and expertise could inform the design of tailored simulation programs that address specific training needs. In addition, broadening the scope of the analyzed procedures is essential for understanding the versatility of the simulation tools. Although this study focused on pericardiocentesis, future research could investigate stress responses in simulations of less invasive procedures, such as venipuncture, or highly dynamic interventions, including trauma resuscitation and advanced cardiac life support. Such studies would help to elucidate how stress dynamics differ across clinical scenarios with varying levels of complexity and urgency. Advancing the technological features of VR simulations is another promising direction for future research. Integrating haptic feedback and real-time biometric monitoring can significantly enhance the realism and educational value of VR environments. Evaluating the impact of these advancements on both stress induction and skill acquisition will provide a more nuanced understanding of how to optimize VR for medical training. Finally, longitudinal studies are needed to assess how repeated exposure to simulation-based training influences long-term stress management, skill retention, and clinical performance. Understanding the evolution of stress responses over time and their correlation with improved coping mechanisms could help to establish evidence-based guidelines for incorporating simulation into medical curricula. These studies provide valuable insights into how simulation training shapes not only technical competence but also emotional resilience in healthcare professionals.
Conclusions
This study highlights the effectiveness of 3D-printed mannequin and VR applications in simulating stress-related aspects of complex medical procedures, such as pericardiocentesis. By being compared to a mannequin, this demonstrates the capability of VR to replicate both technical challenges and emotional pressures in real-life medical scenarios, thereby significantly contributing to stress management training in medical education. Immersive VR environments and mannequins are instrumental to medical students’ preparation for the psychological demands they face in their careers and can complement each other.
The secondary analysis highlighted the significant influence of demographic and lifestyle factors on stress responses during training. These findings reinforce the potential of VR to deliver personalized and adaptive scenarios that address individual variability in stress responses. However, the study focus on undergraduate last-year medical students and the specific procedural context of pericardiocentesis may limit the generalizability of the results to other populations, such as practicing healthcare professionals or less experienced learners.
In conclusion, VR is an indispensable tool in medical education, particularly for integrating stress management into simulation-based training. Future research should focus on validating its effectiveness across diverse learner populations and exploring its application to a broader range of medical procedures. Additionally, further studies should integrate comprehensive stress analyses into VR training, and tailor simulations to address the specific educational needs of medical trainees worldwide. By bridging the gap between technical training and emotional preparedness, VR holds the potential to transform medical education and improve outcomes for both learners and patients.
Data availability
To support reproducibility and facilitate further research, we have made the following resources available: Biometric Data: The anonymized biometric data collected during the study, including heart rate variability (HRV) parameters (e.g., rMSSD, LF/HF ratio), is available through Fighshare at https://doi.org/10.6084/m9.figshare.26215184.v13D Pericardium Model: The 3D model of the pericardium, designed and used for this study, is available for download on https://doi.org/10.6084/m9.figshare.26219135. The model was created using Tinkercad and Adobe Fusion 360 (v. 15.3.0.1657) and can be utilized for educational or research purposes.VR Simulator Repository: The virtual reality simulator developed using Unity 2018.4.36f1 has its source code hosted on GitHub with an open source license, and the application itself can be downloaded freely: https://github.com/rgarciacarmona/VR-Pericardiocentesis.Virtual Simulation Video: A video demonstration of the virtual reality pericardiocentesis simulation, showcasing the immersive environment is hosted on YouTube: https://youtu.be/75eq2mssiRc? si=zlXWpPKFbl4_qwoVThese resources aim to promote transparency, reproducibility, and collaboration within the field of medical education.
Abbreviations
- VR:
-
Virtual reality
- HRV:
-
Heart rate variability
- 3D:
-
Three-dimensional
- LF:
-
Low frequency
- HF:
-
High frequency
- LF/HF ratio:
-
Low frequency/high hrequency hatio
- rMSSD:
-
Root mean square of successive differences
- PNN20:
-
Percentage of successive NN intervals that differ by more than 20 ms
- PNN50:
-
Percentage of successive NN intervals that differ by more than 50 ms
- SD1/SD2 Ratio:
-
Standard deviation 1/sStandard deviation 2 ratio
- ANS:
-
Autonomic nervous system
- SPSS:
-
Statistical package for the social sciences
- ANOVA:
-
Analysis of variance
References
Xu, M. et al. Game-based learning in medical education. Front. Public Health 11, 1113682 (2023).
Mahajan, A. & Hawkins, A. Current implementation outcomes of digital surgical simulation in low- and middle-income countries: Scoping review. JMIR Med. Educ. 9, (2023).
Lin, H.-C., Hwang, G.-J., Chou, K. R. & Tsai, C.-K. Fostering complex professional skills with interactive simulation technology: A virtual reality-based flipped learning approach. Brit. J. Educational Tech. 54, 622–641 (2023).
Urlings, J., de Jong, G., Maal, T. & Henssen, D. Views on augmented reality, virtual reality, and 3D printing in modern medicine and education: A qualitative exploration of expert opinion. J. Digit. Imaging 36, 1930–1939 (2023).
Brunzini, A., Papetti, A., Messi, D. & Germani, M. A comprehensive method to design and assess mixed reality simulations. Virtual Real. 26, 1257–1275 (2022).
Solhjoo, S. et al. Heart rate and heart rate variability correlate with clinical reasoning performance and self-reported Measures of cognitive load. Sci. Rep. 9, 14668 (2019).
Peek, R., Moore, L. & Arnold, R. Psychophysiological fidelity: A comparative study of stress responses to real and simulated clinical emergencies. Med. Educ. 57, 1248–1256 (2023).
Liaw, S. Y. et al. Desktop virtual reality versus face-to-face simulation for team-training on stress levels and performance in clinical deterioration: A randomised controlled trial. J. Gen. Intern. Med. 38, 67–73 (2023).
Mühling, T. et al. Virtual reality in medical emergencies training: benefits, perceived stress, and learning success. Multimed. Syst. 29, 2239–2252 (2023).
Lord, S., Lord, G. & Geary, S. P. A novel, low-cost, low-fidelity pericardiocentesis teaching model. West. J. Emerg. Med. 22, 931–936 (2021).
Amacher, S. A. et al. Influence of gender on the performance of cardiopulmonary rescue teams: a randomized, prospective simulator study. Crit. Care Med. 45, 1184–1191 (2017).
12. Dalmeida, K. M. & Masala, G. L. Hrv features as viable physiological markers for stress detection using wearable devices. Sensors 21, (2021).
Mergen, M., Meyerheim, M. & Graf, N. Reviewing the current state of virtual reality integration in medical education—A scoping review protocol. Syst. Rev. 12, 97 (2023).
Bolton, W. et al. A virtual reality training platform for surgeons, anaesthetists, and obstetricians in low and middle-income countries. Br. J. Surg. 109, znac242-018 (2022).
Weissglass, D. E. Contextual bias, the democratization of healthcare, and medical artificial intelligence in low- and middle-income countries. Bioethics 36, 201–209 (2022).
Roh, T. H. et al. Virtual dissection of the real brain: Integration of photographic 3D models into virtual reality and its effect on neurosurgical resident education. Neurosurg. Focus 51, E16 (2021).
Towers, A., Dixon, J., Field, J., Martin, R. & Martin, N. Combining virtual reality and 3D-printed models to simulate patient-specific dental operative procedures—A study exploring student perceptions. Eur. J. Dent. Edu. 26, 393–403 (2022).
Rochlen, L. R., Putnam, E., Levine, R. & Tait, A. R. Mixed reality simulation for peripheral intravenous catheter placement training. BMC. Med. Educ. 22, 876 (2022).
Bruno, R. R. et al. Virtual and augmented reality in critical care medicine: The patient’s, clinician’s, and researcher’s perspective. Crit. Care 26, 326 (2022).
Helman, T. J., Headrick, J. P., Stapelberg, N. J. C. & Braidy, N. The sex-dependent response to psychosocial stress and ischaemic heart disease. Front. Cardiovasc. Med. 10, 1072042 (2023).
Adjei, T., Xue, J. & Mandic, D. P. The female heart: Sex differences in the dynamics of ECG in response to stress. Front. Physiol 9, 1616 (2018).
Kreutz, R. et al. Lifestyle, psychological, socioeconomic and environmental factors and their impact on hypertension during the coronavirus disease 2019 pandemic. J. Hypertens. 39, 1077–1089 (2021).
Corrigan, S. L., Roberts, S., Warmington, S., Drain, J. & Main, L. C. Monitoring stress and allostatic load in first responders and tactical operators using heart rate variability: A systematic review. BMC Public Health 21, 1701 (2021).
Narciso, D. et al. Using heart rate variability for xomparing the effectiveness of virtual vs real training environments for firefighters. IEEE Trans. Vis. Comput. Graph. 29, 3238–3250 (2023).
Acknowledgements
The authors wish to express their sincere gratitude to all the students who participated in this study. Their involvement and dedication were essential to this research, and their contributions have greatly enhanced our understanding of virtual reality applications in medical training.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ARL designed the study, collected the data, performed the statistical analysis, and wrote the study as the principal investigator. RG participated in the development and correction of the virtual scenario.LZ performed the programming of the virtual scenario according to the created model.ARN participated in the performance tests and in the design and collection of biometric parametersAGP participated in the design and adaptation of the simulated scenariosPCF participated in proofreading and supervision of the study design, statistical analysis and writing of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rubio-López, A., García-Carmona, R., Zarandieta-Román, L. et al. Analysis of stress responses in medical students during simulated pericardiocentesis training using virtual reality and 3D-printed mannequin. Sci Rep 15, 7645 (2025). https://doi.org/10.1038/s41598-025-92221-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92221-3