Abstract
Plasma DNA methylation SEPTIN9, Syndecan 2 (SDC2), and Branched Chain Amino Acid Transaminase 1 (BCAT1) tests have served as valuable diagnostic, prognostic, and predictive markers for colorectal cancer (CRC). In this study, we analyzed data including 104 eligible CRC patients, 138 colorectal benign diseases, and 106 healthy subjects in our hospital from January 2019 to May 2023. This study was approved by the Medical Ethics Committee of Henan Cancer Hospital (Approval No.2018156). A real-time polymerase chain reaction-based gene panel was used to detect the methylation of SEPTIN9, SDC2, and BCAT1. The composite score (P) was calculated according to the cycle threshold (Ct) values of the three methylated genes using the logistic regression equation. The consistency of assay and pathological diagnosis were evaluated with kappa analyzed by IBM SPSS Statistics. The median survival time was obtained by Kaplan-Meier survival analysis. Statistical figures were all carried out using Origin software. The three genes were found to be significantly methylated in ctDNA of CRC patients compared to patients with colorectal benign diseases and healthy controls. The sensitivity was 86.1%, the specificity was 97.6%, and the area under the curve of 0.929. Positive predictive value (PPV) was 57.2%, and Negative predictive value (NPV) was 99.5%. No statistically significant differences in diagnostic efficiency were observed in relation to different types of stages. Moreover, there was a significant difference in the expression of composite scores between survival periods greater than 1 year and less than 1 year (p < 0.01). The composite score (P) derived from the ctDNA methylation levels of SEPTIN9, SDC2, and BCAT1 can be used for CRC diagnosis with high sensitivity and specificity. A combination of ctDNA methylation was proved to be an effective diagnostic, prognostic, and predictive biomarker in colorectal cancer.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) has been the third most prevalent cancer and the second leading cause of cancer-related mortality globally1. Among all kinds of cancer, the incidence rate of CRC has ranked second in China, accounting for 10.72%. The mortality rate has ranked fourth in China, accounting for 9.32%2. The development of CRC has involved a complex, multistep progression of genetic, histological, and morphological transformations with accruing over time3. The diagnosis of CRC has played a crucial role in understanding cancer development, aiding in prevention, disease assessment, and prognosis. Presently, CRC diagnosis primarily has relied on colonoscopy to detect histologic and morphological changes, as well as analyzing genetic molecules like DNA, RNA, and antigenic proteins in fecal and blood samples. However, colonoscopy has been highly invasive and carried potential complications4. What’s more, the current genetic molecular markers in feces and blood demonstrated low sensitivity, specificity5, and patient compliance, especially fecal tests6, hindering clinical effectiveness and widespread implementation. Therefore, it is very necessary to discover a non-invasive, efficient, and well-tolerated diagnostic method.
The current non-invasive tests predominantly were focused on blood genetic or epigenetic molecular tests7. Epigenetic alterations manifest in early-stages of colorectal cancer, and also in various stages of colorectal cancer development and virtually all critical pathways3. These epigenetic alterations molecular footprint could enable precise evaluation of tumor-specific aberrant molecules’ oncogenic impact in colorectal malignancies. Importantly, epigenetic testing has shown high sensitivity and specificity8, with the potential to translate into clinical predictive, diagnostic, and prognostic markers. Currently, epigenetic biomarkers primarily focused on DNA methylation9. Circulating tumor DNA (ctDNA) is released from primary or metastatic tumor cells10, undergone methylation in specific gene regions11. SEPTIN9, SDC2, and BCAT1 methylation have been separately validated in numerous clinical trials with high specificity and sensitivity. SEPTIN9 was the first gene to be studied at the DNA methylation site for CRC detection, methylated in the gene promoter region, and involved in cytoplasmic division and cell cycle regulation. It was highly specific12, but its sensitivity remained controversial, reported at only 35.0% and 63.0% in phase I and phase II of a study13. SDC2 is a heparan sulfate proteoglycan regulating cell-matrix adhesion, migration, proliferation, and angiogenesis14, possessing good specificity and sensitivity, especially in early detection, showing potential for development15,16. Previous studies have shown that BCAT1 is closely related to the cell cycle, growth and apoptosis of a variety of malignant tumors and can be used as a biomarker for screening cancer17. In the study of Symonds EL et al., the methylation detection sensitivity of BCAT1 was comparable to fecal immunochemical test (FIT), but it had higher specificity18.
In this study, the methylation levels of SEPTIN9, SDC2, and BCAT1 were first compared among CRC, colorectal benign diseases, and healthy groups. These levels were compared to the positivity rates of current markers carcinoembryonic antigen (CEA), carbohydrate antigen 19 − 9 (CA19-9), carbohydrate antigen 72 − 4 (CA72-4), and carbohydrate antigen 125 (CA125). Differential expressions in staging were examined, followed by an analysis of their consistency with pathological examination. Most importantly, this study provided additional follow-up and prognostic information regarding the three ctDNA methylations. A comprehensive analysis of the methylation levels of SEPTIN9, SDC2, and BCAT1 throughout the diagnosis and prognosis of CRC aims to support their role as clinical markers for colorectal cancer.
Results
Clinicopathological information of subjects
As shown in Table 1; Fig. 1, study participants were stratified into three diagnostic cohorts via biopsy-based colonoscopy: CRC patients (n = 104), benign colorectal lesions patients (n = 138), and healthy controls (n = 106). Demographic analysis revealed a median age of 55 years (range: 27–75) in CRC patients, 51 years (24–77) in benign disease cases, and 47 years (23–67) in healthy individuals, with relatively balanced gender distributions across groups (CRC: 54.8% male, 45.2% female; benign: 61.6% male, 38.4% female; healthy: 52.8% male, 47.2% female). Among CRC patients, tumors were predominantly located in the rectum (51.9%) and colon (45.2%). Lymph node status analysis revealed that 50 CRC patients (48.1%) were node-negative, while 31 CRC patients (29.8%) presented with lymph node metastasis, with the remaining 23 CRC patients (22.1%) having undetermined nodal status due to incomplete clinical evaluation. Metastatic status analysis demonstrated that 64 CRC patients (61.5%) were free of distant metastasis, while 38 CRC patients (36.5%) presented with distant metastasis. Based on the combination of tumor staging, lymph node metastasis and distant metastasis indicators of different CRC patients, TNM staging criteria are used for clinical staging, including 42.3% early- stage (n = 44; stage I: n = 16, stage II: n = 28) and 51.9% late-stage (n = 54; stage III: n = 16, stage IV: n = 38). Post-treatment surveillance data indicated 44 CRC patients (42.3%) maintained documented recurrence-free status, while 52 CRC patients (50.0%) had undetermined recurrence status, with remaining cases lacking detailed recurrence records in clinical follow-ups. Survival analysis showed 21.2% mortality, with 7.7% surviving less one year and 10.6% surviving 1–3 years. Benign lesions primarily consisted of adenomas (41.3%), polyps (30.4%), and enteritis (15.9%). Notably, 77.9% of CRC patients underwent surgical intervention, while 22.1% received non-surgical management.
Evaluation of the ctDNA methylation of SEPTIN9, SDC2, BCAT1 in CRC diagnostic accuracy
Diagnostic efficiency analysis was shown in Fig. 2; Table 2, the area under the curve (AUC) of the combined detection of three genes methylation (Composite score P) was 0.929 (95% CI: 0.897–0.954), with 86.1% sensitivity, 97.6% specificity, 99.5% negative predictive value (NPV), and 57.2% positive predictive value (PPV). The AUC of SEPTIN9 methylation was 0.929 (95% CI: 0.896–0.954), with 84.2% sensitivity, 98.4% specificity. The AUC of SDC2 methylation was 0.912 (95% CI: 0.877–0.940), with 85.2% sensitivity, 93% specificity. The AUC of BCAT1 methylation was 0.919 (95% CI: 0.885–0.945), with 84.2% sensitivity, 98.4% specificity. Compared to a single gene, the diagnostic efficiency of panel had higher sensitivity and AUC. In addition, considering the clinical, pathological, and epidemiological characteristics of early-onset colorectal cancer, we analyzed ROC curve on different age groups in Supplementary Fig. S1, and found that the high values of AUC, sensitivity and specificity of were similar for three age groups, including < 50 years, ≥ 50 years and all age groups. High AUC and sensitivity suggested that this test could effectively exclude non-CRC patients (with a low false negative rate) and is suitable for large-scale screening. High specificity supported its reliability in auxiliary diagnosis, especially as an alternative when colonoscopy cannot be performed. What’s more, the pathological examination method of colonoscopy was still the gold standard for diagnosing CRC, and the kappa value of 0.827 indicated that the diagnostic efficiency of panel in colorectal cancer was highly consistent with pathological examination. These parameters directly informed panel as a screening tool, particularly when combined with imaging modalities for confirmatory diagnosis.
Comparative analysis of SEPTIN9, SDC2, BCAT1 and other tumor biomarkers
Participants were divided into the colon and rectal cancer group, the benign disease group, and the healthy group. The Mean ± SD values and positivity rates of the current biological markers CEA, CA19-9, CA72-4, CA125, ctDNA methylation of SEPTIN9, SDC2, BCAT1, and composite score P were summarized (Table 3). Comparative analysis was shown that the panel of three genes methylation had substantial advantages over conventional biomarkers. According to composite score (P), methylation positivity rates reached 89.4% in colon cancers and 83.3% in rectum cancers, versus 39.1% and 39.6%, 20.0%, 30.2%, 40.4% and 32.7%,15% and 16.7% for biological markers of CEA, CA19-9, CA72-4 and CA125 respectively in colon and rectum cancers. In Fig. 3, the methylation levels of three genes biomarkers were compared, and SEPTIN9, SDC2, BCAT1 and composite score (P) showed significant discriminatory power between colorectal cancer patients and non-malignant controls (p < 0.001). Intriguingly, this panel showed preliminary potential for CRC localization discrimination (colon and rectum cancer, p < 0.05), though current statistical power remains limited and requires validation in extended research. These results indicated that the combined detection could cover the heterogeneity of CRC and improve the diagnostic accuracy through the methylation signal of complementary genes. Meanwhile, methylated biomarkers were shown higher sensitivity in detecting ctDNA released during early tumorigenesis, while protein-based biomarkers such as CEA, CA19-9, CA72-4 and CA125 had limited detection effect, especially in clinical diagnosis characterized by low tumor burden, which was prone to false negative results.
Next, for benign diseases and healthy samples, the positive detection rates of biomarkers CEA, CA19-9, CA72-4 and CA125 were 11.8% and 5.6%, 12.9% and 7.7%, respectively. The composite score (P) showed that the positive detection rates of three genes methylation panel were 5.1% and 3.8%, which was much lower than the positive detection rate of traditional biomarkers. The false-positive rate of three genes methylation panel was lower compared with traditional biomarkers, which indicated that misdiagnosis could be effectively avoided in clinic. Meanwhile, the standard deviation of Ct value of three genes methylation in CRC group were much lower than CEA, CA19-9, CA72-4 and CA125. The lower coefficient of variation implied that the detection system was highly reproducible, while the high dispersion of traditional biomarkers was limited its clinical diagnostic consistency.
Levels of methylated SEPTIN9, SDC2, BCAT1, and composite score (P) of subjects with different tumor locations of CRC patients, colorectal benign diseases, and healthy persons. (a) Levels of methylated SEPTIN9. (b) Levels of methylated SDC2. (c) Levels of methylated BCAT1. (d) Values of composite score (P). * p < 0.05, ** p < 0.01, *** p < 0.001, NS, no significance.
Subtype performance of SEPTIN9, SDC2, and BCAT1 methylation biomarkers in CRC diagnosis
In Table 4, upon analyzing the specificity variations of three DNA methylations in the staging and histology of colorectal cancer, it was revealed that there were no distinct differences in specificity among colon, rectum, and other histological types. In addition, it was shown that the similar high positive detection rates of methylation biomarkers SEPTIN9, SDC2, BCAT1. Therefore, the statistical evaluation of various tumor stages showed no significant difference through χ2 test (P > 0.05; 0.60131, 0.70296, 0.46938, 0.90839). T1-T4 stages were shown 75.0%, 78.6%, 84.9%, and 90.0% overall positive rates, respectively. Node stages of all investigated samples (N0-N2) maintained 84.0-90.0% positivity, while metastatic (M1) and non-metastatic (M0) groups exhibited 89.5% and 84.4% positive rates. Although no accurate discrepancies were observed among the three ctDNA methylations in pathological tissues and stagings, the panel was displayed high positive detection rates across every tumor stage (ranging from 80 to 100%), indicating that the panel could stably detect CRC patients in early-stages.
SEPTIN9, SDC2, and BCAT1 methylation biomarkers for detection of CRC survival outcomes
The analysis of SEPTIN9, SDC2, and BCAT1 gene expression levels in relation to survival outcomes, including death, six-month survival time, one-year survival time, and the median survival period, was conducted to assess the correlation between the three ctDNA methylations and overall survival (Table 5). Among the 48 surviving patients, 8 false negative patients were removed.
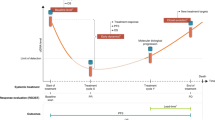
Studies had shown that the methylation levels of SEPTIN9, SDC2, and BCAT1 and composite score (P) are significantly correlated with the survival time of patients with CRC (Table 5; Fig. 4). There were significant differences in SEPTIN9, SDC2, BCAT1 and composite score (P) between patients with survival time ≤ 6 months and > 6 months. The methylation levels of SDC2 and BCAT1 were significantly different in patients with survival time ≤ 12 months and > 12 months. In addition, SDC2 methylation levels showed significant differences at various survival stages, including survival time ≤ 6 months, 6–12 months, and > 12 months. The significant difference in the expression levels of SDC2 between patients and controls suggested that it may reflect dynamic changes in tumor biological behavior. These markers can be supposed to identify high-risk patients, especially those with high short-term survival risk. For example, by continuously detecting methylation levels, the disease progression or treatment response could be evaluated in real-time. The composite score (P) was significantly higher in patients with shorter survival, which may reflect tumor load or invasiveness. The change of composite score (P) can be monitored longitudinally at multiple time points before, during and after treatment, and the treatment response was evaluated. The composite score (P) can also be incorporated into the existing staging system to train a prognostic model to guide the postoperative adjuvant therapy.
Discussion
This clinical trial investigated the diagnostic efficacy of SEPTIN9, SDC2, and BCAT1 circulating DNA methylation for colorectal cancer diagnosis. The findings revealed that the positivity rates of SEPTIN9, SDC2, BCAT1, and the composite score P in colorectal cancer were much higher than in benign diseases and normal groups. Additionally, the diagnostic efficacy of the three DNA methylation positivity tests was significantly higher than the traditional colorectal cancer biomarkers, like CEA, CA19-9, CA72-4, and CA125. Compared with traditional biomarkers, ctDNA methylation biomarkers directly reflected the early abnormalities of gene expression through epigenetic regulation mechanisms, and might provide more sensitive detection signals in the pre-tumorigenic stage19. Owing to the epigenetic regulation of the abnormal methylation of specific gene CpG islands, ctDNA methylation biomarkers could more accurately distinguish tumor sources and reduce the interference of non-tumor diseases20. Therefore, the three genes methylation panel could detect tumor gene promoter abnormal hypermethylation, enabling the identification of CRC with sensitivity up to 86.1% and specificity exceeding 97.6%. In contrast, conventional protein-based biomarkers like CEA, CA19-9, CA72-4, and CA125 exhibited lower sensitivity and higher uncertainty because of non-cancerous conditions such as inflammation21, metabolic disease22. The technical robustness of ctDNA methylation assays ensure reproducibility across multiple interferences clinical settings.
Comparing the diagnostic efficacy of the three DNA methylation positivity tests with the current gold standard colonoscopy yielded a kappa value of 0.827, indicating high consistency. Furthermore, the three ctDNA methylations demonstrated good diagnostic performance based on AUC, sensitivity, specificity, PPV, and NPV, with values of 0.929, 86.1%, 97.6%, 57.2%, and 99.5%, respectively. These results suggested the three ctDNA methylation tests had high diagnostic efficacy, indicating the potential for replacing colonoscopy and other current biomarker tests. In addition, considering the clinical, pathological, and epidemiological characteristics of early-onset colorectal cancer, we analyzed ROC curve on different age groups in Supplementary Fig. S1, and found that the high values of AUC, sensitivity and specificity of were similar for three age groups, including < 50 years, ≥ 50 years and all age groups. This study showed that three genes methylation panel exhibited high diagnostic efficacy (AUC > 0.9) in different age groups, but no significant inter group differences. Moreover, due to sample size limitations, imprecise age criteria and the absence of molecular subtyping, further exploration was needed to determine the impact of the unique biological characteristics of Early-onset colorectal cancer on methylation patterns. The study also revealed that the three ctDNA methylation panel performed high positive detection rates (80-100%) with every tumor stage, but unable to significantly distinguish differences specific CRC stages.
Moreover, the analysis of survival analysis revealed significant differences in SEPTIN9, SDC2, BCAT1 and composite score (P) between patients with survival time ≤ 6 months and > 6 months. The methylation levels of SDC2 and BCAT1 were significantly different in patients with survival time ≤ 12 months and > 12 months. In addition, SDC2 methylation levels showed significant differences at various survival stages, including survival time ≤ 6 months, 6–12 months, and > 12 months. These differences were statistically significant, highlighting the potential of the three ctDNA panel in assessing patients’ survival and compensating for the previous lack of prognostic analysis14. Noteworthy, the kit used in this study required only 2 mL of peripheral blood for measuring the methylation levels, showing higher efficiency compared to 3mL in other kits23. Moreover, our research results were consistent with previous studies, showing that the detection efficiency of the assay kit was higher when SEPTIN9 is combined with multiple biomarkers in the examination24.
However, the study also has some limitations. The current cohort size (104 CRC patients, 138 benign cases, and 106 healthy controls) meets initial exploratory requirements but may compromise generalizability. Subgroup analyses, particularly for the current sample size, were constrained by limited statistical power. For instance, the T0 stage group (n = 3) exhibited insufficient sample size to reliably detect methylation differences, causing uncertainty in subgroup-specific conclusions. Although the overall sensitivity (86.1%) and specificity (97.6%) were significant, these metrics may vary across diverse populations due to age, race, or comorbidity-related heterogeneity. The study identified no statistically significant differences in methylation marker profiles across CRC stages and metastatic statuses. This result may be limited by the uneven distribution of samples. Notably, the high proportion of advanced-stage patients (51.9%) likely obscured potential different stage-specific biomarker signatures, particularly in early-stage, where such markers could hold greater early diagnostic relevance. Furthermore, all samples were from a single medical institution, which introduced selection biases, including regional variations in genetic backgrounds, clinical practices, and treatment protocols. Such homogeneity limits the generalizability of findings to broader populations.
Although the current sample size and data limitations restrict the broader applicability of the results, this study preliminarily confirms the high value of SEPTIN9, SDC2, and BCAT1 methylation in the diagnosis and prognostic evaluation of CRC. It is necessary to expand the sample size (especially early cases) to improve the robustness of validating early diagnostic efficacy. CRC has high molecular heterogeneity25. The study did not analyze the association between methylation markers and molecular subtypes, which lead to the sensitivity of some subgroups being masked. Therefore, combined multi omics data could obtain with multi-level in-depth analysis to evaluate specific markers of CRC delicately26. In addition, it could be extended the follow-up periods to more than 5 years, analyzed the dynamic correlation between methylation level and overall survival to establish prognosis prediction model, which deepen the prognostic value. In the future, the large-scale, multi-disciplinary collaboration and longer follow-up periods will be essential to refine these biomarkers’ clinical utility and integrate them into non-invasive screening and precision oncology medicine.
Materials and methods
Study subjects
We retrospectively analyzed data passed the sample quality control acceptance criterion, including 104 eligible CRC patients, 138 colorectal benign diseases and 106 healthy subjects in the Affiliated Cancer Hospital of Zhengzhou University and Henan Cancer Hospital from January 2019 to May 2023. CRC patients were confirmed by pathological diagnosis of colonoscopy biopsy. Furthermore, all subjects underwent a blood draw before the pathological examination, and subsequent biopsy or surgery was performed. Demographic and clinical-pathological information of subjects including age, gender, pathological type, tumor stage, tumor location, metastasis status, and recurrence or survival of patients were collected for analysis (Table 1).
All participants signed the individual informed consent before samples collection, and were informed of the use of plasma and test results. This study was approved by the Medical Ethics Committee of Henan Cancer Hospital (Approval No.2018156) and all trails were carried out in according to the relevant guidelines and protocols, as well as the Declaration of Helsinki.
Sample collection and storage.
A 5 mL peripheral blood sample was collected with a K2EDTA-pretreated anticoagulant blood collection tubes (BD Biosciences, Franklin Lakes, NJ, USA) for the DNA extraction. The plasma was separated from the blood sample at 4000 rpm for 10 min and this process was duplicated only for supernatant. Then, the impurities-free plasma sample should be stored and transported under the instructions for the use of the Nucleic Acid Extraction Reagent (Excellen Medical Technology Co., Ltd.).
DNA isolation and bisulfite conversion
The DNA isolation and bisulfite conversion were performed with the Nucleic Acid Extraction Reagent (Excellen Medical Technology Co., Ltd.). Briefly, 3 mL Lysis Binding Buffer were added to 2 mL plasma following by 20 min incubation at room temperature. Added 100 µL mixing magnetic sufficient beads was bonded with DNA in 60 min incubation at 10-20 rpm in a rotator. Then, the precipitated beads were gathered and washed with Wash Buffer A and pipetted all supernatants carefully, following by dried by airing for 10 min.
At the beginning of DNA bisulfite conversion, 180 µL Bisulfite Solution and 20 µL Protection Buffer were added to the mixture with vortex magnetic beads completely. The mixture was transferred and incubated in a suitable thermostatic heater for 45 min at 85℃, in order to convert unmethylated cytosine residues to uracil residues. Utilizing Lysis Binding Buffer and Wash Buffer B were re-bonded between the magnetic beads and DNA entirely. Next, the obtained bond DNA was washed once with Wash Buffer A and twice with Wash Buffer B respectively, following by dried by airing for 10 min. In the last resort, the bisulfite-converted DNA (bisDNA) was eluted in 35 µL and ready for use in real-time PCR.
DNA methylation analysis
The obtained bisDNA was used as a template for fluorescence-based Real-Time PCR, as well as, performed with the Diagnostic Kit for Colorectal Cancer Genes Methylation (Excellen Medical Technology Co., Ltd.). Each sample was detected three parallel wells by Real-time PCR System (Fosun Diagnostics (Shanghai) Co., Ltd., SLAN-96P, Shanghai, China). In principle, these bisDNA subjects’ samples included patients, positive controls, negative controls and multiple water blanks. Furthermore, every reaction system contained 12.5 µL Reaction Buffer, 2.5 µL of Primer Mixture, and 10 µL of bisDNA. Amplifications were executed the thermal profile: 98℃ for 5 min, followed by 45 cycles at 95℃ for 10 s and 63℃ for 5 s to 58℃ for 30 s. In this reverse transcription-polymerase chain reaction (RT-PCR) process, the methylated target sequences can be exclusively identified from unmethylated DNA.
Real-time PCR data were analyzed using the Colorectal Cancer Analysis software v2.2 (Excellen Medical Technology Co., Ltd.). Positive values (composite score (P)) were defined using cut-off (P ≥ 1.2). The software calculated a composite score (P) based on the cycle threshold (Ct) values of the three methylated genes through logistic regression.
CEA, CA19-9, CA72-4, and CA125 quantification
For all plasma samples, CEA, CA19-9, CA72-4, and CA125 were measured using a Cobase 801 automatic electrochemical luminescence instrument and supporting reagents (Roche, Switzerland). The cut-off value of CEA, CA19-9, CA72-4, and CA125 is 3.5 ng/mL, 30 U/mL, 6.9 U/mL, 35 U/mL, respectively.
Statistical analysis
The performance of assay was observed with receiver-operating-characteristic (ROC) curves, calculation of area under the curve (AUC), estimates of sensitivity, specificity, and 95% confidence intervals (CIs) by the ROC curves analysis of MedCacl. The consistency of assay and pathological diagnosis were evaluated with kappa analyzed by IBM SPSS Statistics. All statistical tests were calculated with Chi-square test (χ2 test) or t-test, and P < 0.05 was considered statistically significant. The median survival time was obtained by Kaplan-Meier survival analysis. Statistical figures were all carried out using Origin.
Conclusions
This study confirmed that SEPTIN9, SDC2, and BCAT1 exhibited high sensitivity and specificity in colorectal cancer screening at various stages, including prevention, screening, and colorectal cancer staging. The three genes methylation panel can also predict prognosis and serve as potential clinical biomarkers for CRC screening.
Data availability
The datasets analyzed in this study are accessible from the corresponding author upon reasonable request.
Abbreviations
- SDC2:
-
Syndecan 2
- BCAT1:
-
Branched Chain Amino Acid Transaminase 1
- CRC:
-
Colorectal cancer
- P:
-
Composite score
- Ct:
-
Cycle threshold
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- ctDNA:
-
Circulating tumor DNA
- FIT:
-
Fecal Immunochemical Test
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9
- CA72-4:
-
Carbohydrate antigen 72-4
- CA125:
-
Carbohydrate antigen 125
- bisDNA:
-
Bisulfite-converted DNA
- ROC:
-
Receiver-operating-characteristic
- AUC:
-
Area under the curve
- CIs:
-
Confidence intervals
- χ2 test:
-
Chi-square test
- RT-PCR:
-
Reverse transcription-polymerase chain reaction
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 73(3), 229–263 (2024).
Han, B. et al. Cancer incidence and mortality in China, 2022. Cancer Lett. 4(1), 47–53 (2024).
Dariya, B., Aliya, S., Merchant, N., Alam, A. & Nagaraju, G. P. Colorectal cancer biology, diagnosis, and therapeutic approaches. Crit. Rev. Oncog. 25(2), 71–94 (2020).
Marrugo-Ramírez, J., Mir, M. & Samitier, J. Blood-Based cancer biomarkers in liquid biopsy: A promising Non-Invasive alternative to tissue biopsy. Int. J. Mol. Sci. 19(10), 2877 (2018).
Huang, Z. et al. Plasma MicroRNAs are promising novel biomarkers for early detection of colorectal cancer. Int. J. Cancer 127(1), 118–126 (2010).
Constâncio, V., Nunes, S. P., Henrique, R. & Jerónimo, C. DNA Methylation-Based testing in liquid biopsies as detection and prognostic biomarkers for the four major cancer types. Cells 9(3), 624 (2020).
Carethers, J. M. Fecal DNA testing for colorectal cancer screening. Annu. Rev. Med. 71, 59–69 (2020).
Lech, G., Słotwiński, R., Słodkowski, M. & Krasnodębski, I. W. Colorectal cancer tumour markers and biomarkers: Recent therapeutic advances. World J. Gastroenterol. 22(5), 1745–1755 (2016).
Chen, R. et al. DNA methylation of miR-138 regulates cell proliferation and EMT in cervical cancer by targeting EZH2. BMC Cancer 22, 488 (2022).
Freitas AJAd, Causin, R. L. et al. Liquid biopsy as a tool for the diagnosis, treatment, and monitoring of breast cancer. Int. J. Mol. Sci. 23(17), 9952 (2022).
Müller, D. & Győrffy, B. DNA methylation-based diagnostic, prognostic, and predictive biomarkers in colorectal cancer. Biochim. Biophys. Acta. 1877(3), 188722 (2022).
Zhang, S-L. et al. Septin9 DNA methylation is associated with breast cancer recurrence or metastasis. J. Int. Med. Res. 52(1), 655685541 (2024).
Xu, F. et al. Detection of Circulating tumor DNA methylation in diagnosis of colorectal cancer. Clin. Translational Gastroenterol. 12(8), e00386 (2021).
Lei, R. et al. The methylation of SDC2 and TFPI2 defined three methylator phenotypes of colorectal cancer. BMC Gastroenterol. 22, 88 (2022).
Oh, T. J. et al. Feasibility of quantifying SDC2 methylation in stool DNA for early detection of colorectal cancer. Clin. Epigenetics. 9, 126 (2017).
Zeng, T. et al. Combining methylated SDC2 test in stool DNA, fecal immunochemical test, and tumor markers improves early detection of colorectal neoplasms. Front. Oncol. 13, 1166796 (2023).
Xu, M. et al. BCAT1 promotes tumor cell migration and invasion in hepatocellular carcinoma. Oncol. Lett. 12(4), 2648–2656 (2016).
Symonds, E. L. et al. A blood test for methylated BCAT1 and IKZF1 vs. a fecal immunochemical test for detection of colorectal neoplasia. Clin. Translational Gastroenterol. 7(1), e137 (2016).
Wang, M., Li, Q. & Liu, L. Factors and methods for the detection of gene expression regulation. Biomolecules 13(2), 304 (2023).
Zeng, H., He, B., Yi, C. & Peng, J. Liquid biopsies: DNA methylation analyses in circulating cell-free DNA. J. Genet. Genom. 45(4), 185–192 (2018).
Liu, L. et al. A preoperative serum signature of CEA+/CA125+/CA19-9 ≥ 1000 U/mL indicates poor outcome to pancreatectomy for pancreatic cancer. Int. J. Cancer 136(9), 2216–2227 (2014).
Zhou, J., Cao, C., Liu, T., Wu, L. & Miao, J. Association between free Triiodothyronine and carcinoembryonic antigen levels in type 2 diabetes mellitus patients. Diabetes Metabolic Syndrome Obesity: Targets Therapy. 17, 4267–4275 (2024).
Ren, Y. et al. Alterations of DNA methylation profile in peripheral blood of children with simple obesity. Health Inform. Sci. Syst. 12, 26 (2024).
Song, L., Yu, H., Jia, J. & Li, Y. A systematic review of the performance of the SEPT9 gene methylation assay in colorectal cancer screening, monitoring, diagnosis and prognosis. Cancer Biomarkers 18(4), 425–432 (2017).
Zhao, N., Lai, C., Wang, Y., Dai, S. & Gu, H. Understanding the role of DNA methylation in colorectal cancer: Mechanisms, detection, and clinical significance. Biochim. Biophys. Acta 1879(3), 189096 (2024).
Du, M. et al. Integrated multi-omics approach to distinct molecular characterization and classification of early-onset colorectal cancer. Cell. Rep. Med. 4(3), 21 (2023).
Acknowledgements
The authors acknowledge all contributing physicians, study nurses, and laboratories for their support in the study.
Funding
This work was supported by the Medical Science and Technique Foundation of Henan Province (No.SBGJ202301004), Young and Middle-aged Health and Technology Innovation Leading Talent Project of Henan Province (No.YXKC2020008), Henan provincial Medical Science and Technology Research Project (No.LHGJ20210172), Science and Technique Foundation of Henan Province (No.222102310424), and Natural Science Foundation of Henan Province (No.242300420091).
Author information
Authors and Affiliations
Contributions
Conception and design: B.B.C., H.Z. and X.B.C.; Development of methodology: H.H.H., H.L.S., H.W., Z.T.Y., J.X.H., H.F.L. and B.B.C.; Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): W.F.X., J.Z.W., C.Y.N., J.Z., Y.D.H. and H.Z.; Clinical sample procurement: S.Q.W., and B.B.C.; Writing, review, and/or revision of the paper: All authors. Study supervision: B.B.C., H.Z. and X.B.C.; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Written informed consents were provided by all participants. This study was approved by the Medical Ethics Committee of Henan Cancer Hospital (Approval No.2018156).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, B., Zhao, H., Hu, H. et al. Circulating DNA methylation-based diagnostic, prognostic, and predictive biomarkers in colorectal cancer. Sci Rep 15, 13577 (2025). https://doi.org/10.1038/s41598-025-95712-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95712-5